Abstract
Background:
Computer-delivered programs to reduce college drinking have strong appeal but are sometimes less efficacious than their in-person counterparts. Boosters may be an ideal way to strengthen and extend the effects of computerized interventions while maintaining low cost and easy dissemination. However, little is known about how they work. Consequently, the current study aimed to explore descriptive perceived drinking norms and use of protective behavioral strategies (PBS) as potential mediators of booster effects. We also examined norms and PBS as mediators of the main intervention. The present study was a follow-up analysis of data from a randomized controlled trial (Braitman & Lau-Barraco, 2018) testing the efficacy of emailed boosters containing personalized feedback after a computerized alcohol intervention.
Methods:
Participants were 537 (67.4% women) emerging adult college drinkers (M age = 19.65, SD = 1.67). They were randomly assigned to one of three conditions: general health education, alcohol intervention only, or alcohol intervention plus booster email. Participants completed assessments at baseline and follow-ups through 9 months.
Results:
Descriptive norms was a mediator of booster efficacy where receiving the booster yielded stronger reductions in alcohol use through reduced concurrent norms; however, fully longitudinal models did not reach significance. There was also an indirect effect for the intervention where those who received the intervention experienced an increase in drinking through increased concurrent norms. However, a stronger direct effect was found where those who received the intervention experienced a stronger decrease in drinking after controlling for norms. There was not support for PBS as a mediator of booster or intervention efficacy.
Conclusion:
The present study was the first, to our knowledge, to demonstrate a potential mechanism of change in booster interventions. A simple, succinct reminder via email lead to reductions in perceptions of how much peers drink and this led to reductions in alcohol consumption. Our findings support the promise of utilizing brief and easily implemented targeted messaging to enhance the potency of computerized interventions for college drinkers.
Keywords: brief alcohol intervention, boosters, college drinking, perceived descriptive norms, protective behavioral strategies
Drinking among college students is linked to academic problems (e.g., missed classes, poor grades; Bolin et al., 2017; Conway & DiPlacido, 2015), as well as physical consequences such as sexual assaults (Abbey et al., 2014; Testa & Hoffman, 2012). Although computer-delivered programs to reduce college drinking may have strong appeal for institutions, they are sometimes less efficacious than their in-person counterparts (Carey et al., 2009; Rodriguez et al., 2015). Boosters are an ideal way to strengthen and extend the effects of computerized interventions while maintaining low cost and easy dissemination (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018), but little is known about how they work. The current study is a follow-up examination of a randomized controlled trial (RCT) of delayed personalized feedback (i.e., boosters) for computer-delivered interventions (Braitman & Lau-Barraco, 2018) to examine potential mechanisms of behavior change.
Computer-delivered interventions (CDIs) targeting college drinking are linked to stronger reductions in alcohol use than assessment-only controls (Elliott et al., 2008). They can be a proactive tool to prevent negative consequences for students, are relatively inexpensive, can be quickly delivered, and are easily disseminated to large groups. Online programs are also more popular among students, and may have a greater reach than face-to-face interventions (Neighbors et al., 2018). Although CDIs have wide appeal, effects are often weaker than interventions delivered in-person (Carey et al., 2009; Rodriguez et al., 2015).
CDIs and Boosters
There is evidence of CDIs being as efficacious as in-person interventions in the short-term (up to 3 months; Barnett et al., 2007; Butler & Correia, 2009; Carey et al., 2009, 2011; Donohue et al., 2004; Murphy et al., 2010; Walters et al., 2009), but not longer-term (Carey et al., 2011, 2012). In addition, select indicators (such as peak drinking) have weaker intermediate reductions after CDIs than in-person interventions (Carey et al., 2012). A recent meta-analysis found reductions in alcohol outcomes among CDI recipients in the short-term (up to 6 weeks) and intermediate-term (7–26 weeks) but not for control participants (Cole et al., 2018). However, these effects were fairly small, and the two groups were almost indistinguishable by the long-term follow-ups (>27 weeks) across most drinking metrics. Thus, although CDIs may be far reaching, their effects are often weak and relatively short-lived.
Boosters, or brief, delayed follow-up sessions, may strengthen intervention efficacy or extend the duration of drinking reductions. Boosters may be an ideal solution for institutions using CDIs, capitalizing on easy dissemination and helping to strengthen relatively modest effects. However, research findings have been equivocal for intervention boosters targeting college drinkers. Four investigations failed to support the use of boosters in college settings, including a study of fraternity members receiving an additional skills-based training session, (Caudill et al., 2007), two studies delivering boosters to mandated students after in-person interventions (Carey et al., 2018; Linowski et al., 2016), and one study delivering boosters to mandated students in both CDI and in-person intervention conditions (Barnett et al., 2007).
However, three studies supported booster use with volunteer college drinker participants (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018; Neighbors, Lewis, et al., 2010). Gender-specific normative feedback led to drinking reductions relative to controls when they were delivered four times over two years, but not after only a single administration (Neighbors, Lewis, et al., 2010), and an emailed booster containing personalized feedback for norms and protective behavioral strategies (PBS; strategies to reduce harm associated with alcohol consumption) delivered 2 weeks after a CDI resulted in stronger drinking reductions at 4 weeks compared to intervention-only controls (Braitman & Henson, 2016). Finally, a third study examining the longer-term efficacy (up to 9 months) of an emailed booster providing normative and PBS feedback after a CDI was efficacious only among older emerging adult college drinkers (ages 21–24) and not those under legal drinking age (ages 18–20; Braitman & Lau-Barraco, 2018). Given the inconclusive pattern of findings, further exploration of how boosters may lead to drinking reductions among college drinkers is warranted.
Potential Booster Mechanisms
The content of boosters that were fully efficacious (Braitman & Henson, 2016; Neighbors, Lewis, et al., 2010) or partially supported (i.e., for emerging adults of legal drinking age only; Braitman & Lau-Barraco, 2018) included descriptive normative perceptions, or perceived alcohol consumption by a referent group. In addition, the two emailed boosters (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018) contained feedback regarding PBS. The current examination is a follow-up analysis of the data demonstrating select efficacy for emailed boosters (Braitman & Lau-Barraco, 2018), exploring descriptive norms and PBS as potential mechanisms of change for booster efficacy.
Descriptive normative feedback.
Descriptive norms, or perceptions of how much relevant others drink (such as students at the same campus), have strong and consistent associations with alcohol outcomes among college drinkers (Perkins, 2002, Borsari & Carey, 2003). Moreover, they have a demonstrated ability to influence those outcomes when misperceptions are corrected via personalized normative feedback (LaBrie et al., 2013; Lewis et al., 2007; Martens et al., 2013; Mattern & Neighbors, 2004; Neighbors, Lewis, et al., 2010). Personalized normative feedback is information provided to drinkers that includes: a) their own reported drinking, b) their reported perceptions of how much relevant others drink, and c) actual drinking rates for relevant others (Lewis & Neighbors, 2006). This is a common form of successful intervention (e.g., LaBrie et al., 2013; Lewis et al., 2007; Martens et al., 2013; Neighbors, Lewis, et al., 2010; see Lewis & Neighbors, 2006 for a review). Descriptive normative perceptions are the most commonly examined mediator among college drinking interventions, with extensive support (Reid & Carey, 2015). Of the 39 trials that examined this, the majority (64%) found support for norms as a mediator, with change in perceptions of drinking norms linked to changes in actual drinking. Support was stronger among trials where the norms feedback was gender-specific, and presented included local students rather than national norms, as in the current data. Moreover, a review of technology-based drinking interventions found that among the seven trials that examined norms as a mediator, a majority (85.7%) again supported norms as a mediator (Dallery et al., 2015). Although there is robust support for descriptive norms as a mediator of intervention efficacy, they have not been explored among booster research.
PBS.
The second feedback component for the current booster was PBS use. PBS are behaviors or techniques one could use to reduce alcohol consumption or related problems, such as avoiding drinking games, or eating before and during drinking (Martens et al., 2005; Sugarman & Carey, 2007). They are often associated with lower alcohol consumption and fewer related problems (see Pearson, 2013 and Prince et al., 2013 for reviews). Successful multi-component interventions often include promotion of PBS as a harm reduction strategy (e.g., Dimeff et al., 1999; Kivlahan et al., 1990).
The research support for PBS as a mechanism of change is equivocal, however. In their review of studies examining mediators of college drinking interventions, Reid and Carey (2015) found that six studies supported PBS as a mediator of intervention efficacy, while six did not. A more recent examination demonstrated that select types of PBS (i.e., avoidance of and seeking alternatives to drinking contexts) mediated reductions in both heavy drinking days and alcohol-related problems (Magill et al., 2017). Moreover, PBS-focused single-component interventions lead to increased PBS use and decreased alcohol consumption or related problems in select populations (i.e., among college women [Dvorak et al., 2017; Kenney et al., 2014], among those with stronger belief in the messages delivered [Dvorak et al., 2015]), and with limited support among students accessing mental health services (LaBrie et al., 2015). However, two studies administering PBS interventions to college drinkers found increases in PBS use were not associated with corresponding reductions in drinking or problems (Martens et al.,2013; Sugarman & Carey, 2009). Given that the current study is a follow-up examination after a multi-component intervention incorporating PBS, PBS holds promise as a potential mechanism of change.
The Current Study
The purpose of the current study was to explore descriptive norms and PBS as potential mediators of the intervention and booster effects for an emailed booster delivering personalized feedback after a CDI. We expected that receiving the intervention would be associated with an immediate reduction of descriptive norms and increase in PBS use, and that these changes will be associated with an immediate reduction in drinking. We expected a similar pattern after receiving the emailed feedback booster, corresponding with further reductions in drinking. We expect this to be true both immediately after receiving the booster (i.e., through week 4; shorter term effects) as well as through month 9 (i.e., longer term effects). Given that the efficacy of the emailed booster only held for emerging adults of legal drinking age in the original study (Braitman & Lau-Barraco, 2018), we examined age as a potential moderator of these mediation effects.
Method
Participants
Participants were N = 537 college student drinkers (consumed at least one alcoholic drink in the prior two weeks) between 18 and 24 years (M = 19.65, SD = 1.67) from a mid-size southeast public university. The sample was majority female (n = 362; 67.4%), and White (n = 262; 48.8%) or African-American or Black (n = 201; 37.4%).
All participants provided informed consent. The study was approved by the relevant Institutional Review Board and followed all American Psychological Association (2010) ethical guidelines. Participants received course credit for completing baseline, received up to $30 for completing the three short-term follow-up surveys, were entered into raffles for completing the longer-term follow-up surveys, and were entered into a raffle for additional money if they completed all phases of the study.
Procedure
In the parent study, an RCT design was used to assess the efficacy of an emailed personalized feedback booster after a CDI (Braitman & Lau-Barraco, 2018). Briefly, participants were randomized by sex to one of three conditions: general health education session (i.e., control condition), alcohol intervention-only, or alcohol intervention-plus-booster-email. Participants in both alcohol intervention conditions navigated through Alcohol 101 Plus™ for 60 minutes. It is a combination of several intervention components, focusing primarily on alcohol education and skills training. Some of the skills training components overlap with PBS, and some of the alcohol education touches on norms. However, it is a nonlinear environment, so participants can explore various areas and may not get all content. Participants in the control condition navigated through Health Education Answers by Lilly for Better Health®, a general health education session. See the original study for more details (Braitman & Lau-Barraco, 2018).
Emails were sent to all participants approximately 2 weeks after their participation (after the Week 2 assessments were sent). The decision to send the booster feedback at Week 2 was due to the demonstrated efficacy of emailed booster feedback at two weeks for the same intervention (Alcohol 101 plus™) in prior work (Braitman & Henson, 2016). Participants in the booster condition received personalized feedback; participants in other conditions were thanked for their participation so far and reminded of upcoming follow-up surveys. Booster content included sex-specific descriptive norms (i.e., drinks per week typically consumed by males and by females at the same institution), as well as feedback regarding PBS techniques the participant reported using and not using in their last survey. Normative information for college students of the same sex at the same institution, obtained through a separate survey at the participating institution, was chosen as the normative feedback for the current study given that closer referent groups are often more effective (Borsari & Carey, 2003; Lewis & Neighbors, 2006; Neighbors, LaBrie, et al., 2010; Neighbors, Lewis, et al., 2010).
Participants completed a baseline survey in the research lab, then interacted for 60 minutes with their assigned online session (alcohol intervention or general health). Participants were invited via email to complete the follow-up survey at 2 (n = 338; 63%), 4 (n = 284; 53%), and 6 weeks (n = 259; 48%) as well as 3 (n = 213; 40%), 6 (n = 173; 32%), and 9 months (n = 140; 26%) post-intervention.
Materials
Alcohol consumption.
Consumption was measured using a modified Daily Drinking Questionnaire (DDQ; Collins et al., 1985). Participants indicated how many standard drinks they consumed each day of the past two weeks, as well as how many hours passed while drinking. This was used to calculate total number of drinks (quantity), number of drinking days (frequency), and highest number of drinks on a single day (peak drinks). Estimated typical blood alcohol concentration (BAC) and highest BAC (peak BAC) were calculated as well (Matthews & Miller, 1979).
Descriptive norms.
Descriptive normative perceptions were assessed using two items. Participants reported the number of standard drinks they perceived a typical male student and a typical female student at their institution to consume each week. Reliability was good for the two items (α ranged from .91 to .92 across all timepoints).
PBS.
Harm reduction strategies were assessed using the 21-item Strategy Questionnaire (SQ; Sugarman & Carey, 2007) modified to reflect exact frequency. This value was divided by number of drinking days for relevant subscales (Braitman et al., 2015). This yields a precise measure of contingent frequency. The SQ total score was used to represent PBS. Reliability was excellent for all time waves (α’s from .93 to .98).
Demographics.
Self-reported demographic information was collected.
Analysis Approach
Consistent with prior work using these data (Braitman & Lau-Barraco, 2018), analyses were conducted using curve-of-factors second-order latent growth modeling. Alcohol consumption at each timepoint was operationalized as a latent variable defined by quantity, frequency, peak drinks, typical BAC, and peak BAC. Loadings for each item were constrained to equality across time. Norms were similarly operationalized as a latent variable defined by perceptions of male and female students. To operationalize growth over time, intercepts and slopes were fitted to consumption, norms, and PBS in a hybrid of piecewise and linear growth. Slopes 1 and 2 represent piecewise growth to Week 2 and to Week 4, respectively. Given that the booster email was sent after the Week 2 assessment, these two slopes are necessary to separately assess growth to Week 2 (the anticipated intervention effect) and growth to Week 4 (the anticipated booster effect). Slope 3 represents additional linear growth through Month 9 to assess maintenance over time. Condition was represented using two variables: intervention (coded as 0 = control session, 1 = alcohol intervention) and booster (coded as 0 = control email, 1 = personalized feedback email). Thus, the variables for intervention and booster were coded as 0,0 for the control condition (receiving neither the intervention or the booster), 1,0 for the alcohol intervention-only condition (receiving the intervention but not the booster email), and 1,1 for the alcohol intervention-plus-booster condition (receiving both the intervention and the booster email).
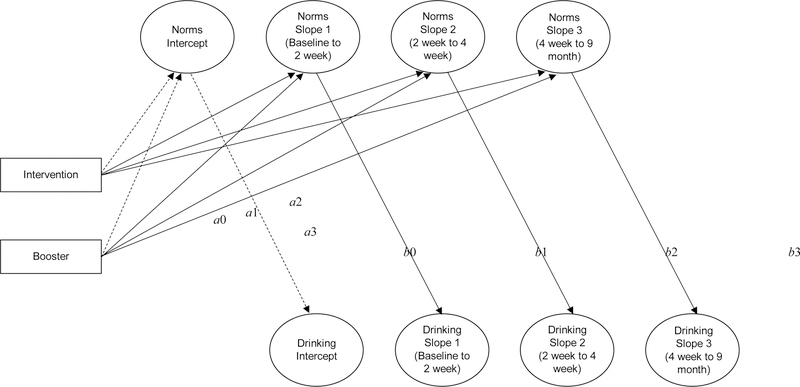
To assess the indirect effect of the intervention and booster on alcohol consumption through the mediator (i.e., norms or PBS), dual process latent growth models were used (see Figure 1). Two models were conducted: one assessing the indirect effect through descriptive norms (model 1), and one through PBS (model 2).
Figure 1.
Dual Process Latent Growth Models assessing the indirect effects of condition on alcohol consumption through descriptive norms. Though included in the model, direct effects are omitted from the figure for clarity. Dashed lines indicate effects prior to the relevant manipulation (i.e., before intervention effects, or before booster effects), and thus expected to be non-significant but included for definitional purposes. Note that intervention was coded 0 (control health session) or 1 (alcohol intervention), and booster was coded 0 (control email) or 1 (personalized feedback email).
To assess moderated mediation, a multigroup approach was used. Consistent with the original efficacy findings (Braitman & Lau-Barraco, 2018), the sample was split into emerging adults of legal drinking age (ages 21–24) versus those under legal drinking age (ages 18–20). A model with all measurement and structural paths constrained to equality across age groups was first conducted. In subsequent models, the effects of condition on mediator growth variables (the a paths), mediator growth on outcome growth (the b paths), and condition on outcome growth (c′ paths) were systematically freed one-by-one. Likelihood ratio tests for nested models indicated whether constraining these parameters yielded significantly worse model fit (i.e., moderation) or not (i.e., no moderation).
Sex was included as a covariate in all models. All models were conducted in Mplus (version 8; Muthén & Muthén, 1998–2017) using maximum likelihood estimation. To assess significance of indirect effects (MacKinnon, Lockwood, & Williams, 2004), bootstrapping using 5,000 draws was used. Significance was assessed using 95% bias-corrected bootstrap confidence intervals (BCCIs), with absence of 0 in the interval indicating significance at the p < .05 level.
Results
Preliminary Analyses
The data were examined for outliers, with extreme cases being Winsorized. Missingness on any follow-up survey was not significantly associated with any variables of interest for the current study (i.e., alcohol consumption, norms, PBS) nor any demographic characteristics, nor condition assignment. No constructs significantly varied across condition at baseline. Means and standard deviations at each timepoint are shown by condition in Table 1.
Table 1.
Descriptive Statistics for Study Variables over Time by Condition
| Baseline | Week 2 | Week 4 | Week 6 | Month 3 | Month 6 | Month 9 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | (SE) | M | (SE) | M | (SE) | M | (SE) | M | (SE) | M | (SE) | M | (SE) | |
| Drink quantity | ||||||||||||||
| Control | 16.93 | (1.10) | 14.21 | (1.26) | 13.20 | (1.22) | 12.17 | (1.46) | 12.07 | (1.50) | 14.55 | (2.14) | 12.55 | (1.85) |
| Int. Only | 17.99 | (1.28) | 12.50 | (1.29) | 12.59 | (1.69) | 12.25 | (1.81) | 13.77 | (2.27) | 12.62 | (2.11) | 11.27 | (2.26) |
| Int. + Booster | 18.04 | (1.22) | 15.42 | (1.54) | 13.70 | (1.71) | 15.88 | (2.14) | 14.92 | (1.78) | 16.10 | (2.69) | 12.23 | (2.80) |
| Total | 17.64 | (0.69) | 14.03 | (0.79) | 13.15 | (0.89) | 13.34 | (1.04) | 13.61 | (1.09) | 14.35 | (1.32) | 11.99 | (1.30) |
| Drink frequency | ||||||||||||||
| Control | 3.97 | (0.17) | 3.37 | (0.24) | 3.14 | (0.25) | 2.97 | (0.27) | 3.10 | (0.31) | 3.15 | (0.39) | 3.37 | (0.49) |
| Int. Only | 3.80 | (0.18) | 2.96 | (0.25) | 2.57 | (0.27) | 2.51 | (0.30) | 3.00 | (0.41) | 2.80 | (0.40) | 2.85 | (0.44) |
| Int. + Booster | 3.98 | (0.18) | 3.35 | (0.25) | 2.96 | (0.29) | 3.05 | (0.32) | 3.19 | (0.32) | 3.18 | (0.40) | 2.67 | (0.50) |
| Total | 3.92 | (0.10) | 3.23 | (0.14) | 2.89 | (0.15) | 2.84 | (0.17) | 3.10 | (0.20) | 3.04 | (0.23) | 2.99 | (0.27) |
| Peak drinks | ||||||||||||||
| Control | 5.80 | (0.28) | 4.99 | (0.36) | 4.90 | (0.35) | 4.55 | (0.41) | 4.29 | (0.47) | 4.98 | (0.61) | 4.57 | (0.41) |
| Int. Only | 6.35 | (0.31) | 5.00 | (0.38) | 5.07 | (0.48) | 4.85 | (0.56) | 5.08 | (0.61) | 4.29 | (0.63) | 4.08 | (0.63) |
| Int. + Booster | 6.14 | (0.28) | 5.27 | (0.43) | 5.07 | (0.49) | 5.38 | (0.58) | 5.22 | (0.52) | 4.90 | (0.62) | 4.31 | (0.86) |
| Total | 6.09 | (0.17) | 5.08 | (0.22) | 5.01 | (0.25) | 4.91 | (0.30) | 4.87 | (0.31) | 4.73 | (0.36) | 4.32 | (0.36) |
| Typical BAC | ||||||||||||||
| Control | 0.07 | (0.00) | 0.06 | (0.00) | 0.06 | (0.01) | 0.06 | (0.01) | 0.05 | (0.01) | 0.06 | (0.01) | 0.06 | (0.01) |
| Int. Only | 0.07 | (0.00) | 0.06 | (0.01) | 0.07 | (0.01) | 0.06 | (0.01) | 0.06 | (0.01) | 0.05 | (0.01) | 0.05 | (0.01) |
| Int. + Booster | 0.07 | (0.00) | 0.06 | (0.01) | 0.06 | (0.01) | 0.06 | (0.01) | 0.06 | (0.01) | 0.06 | (0.01) | 0.05 | (0.01) |
| Total | 0.07 | (0.00) | 0.06 | (0.00) | 0.06 | (0.00) | 0.06 | (0.00) | 0.06 | (0.00) | 0.06 | (0.01) | 0.05 | (0.00) |
| Peak BAC | ||||||||||||||
| Control | 0.10 | (0.01) | 0.09 | (0.01) | 0.09 | (0.01) | 0.09 | (0.01) | 0.08 | (0.01) | 0.10 | (0.01) | 0.09 | (0.01) |
| Int. Only | 0.11 | (0.01) | 0.10 | (0.01) | 0.11 | (0.01) | 0.10 | (0.01) | 0.10 | (0.01) | 0.09 | (0.02) | 0.08 | (0.01) |
| Int. + Booster | 0.12 | (0.01) | 0.10 | (0.01) | 0.10 | (0.01) | 0.10 | (0.01) | 0.10 | (0.01) | 0.09 | (0.01) | 0.08 | (0.01) |
| Total | 0.11 | (0.00) | 0.10 | (0.00) | 0.10 | (0.01) | 0.10 | (0.01) | 0.09 | (0.01) | 0.09 | (0.01) | 0.08 | (0.01) |
| Norms: Male Quantity | ||||||||||||||
| Control | 14.00 | (0.67) | 12.71 | (0.81) | 12.55 | (0.80) | 13.92 | (1.07) | 12.81 | (1.16) | 13.16 | (1.23) | 12.56 | (1.35) |
| Int. Only | 13.31 | (0.66) | 12.80 | (0.85) | 13.00 | (0.88) | 12.57 | (0.86) | 14.15 | (1.28) | 13.74 | (1.25) | 14.02 | (1.23) |
| Int. + Booster | 13.56 | (0.61) | 12.30 | (0.79) | 10.37 | (0.73) | 10.07 | (0.86) | 11.01 | (1.06) | 10.38 | (1.04) | 11.71 | (1.32) |
| Total | 13.63 | (0.37) | 12.61 | (0.47) | 12.01 | (0.47) | 12.29 | (0.55) | 12.67 | (0.68) | 12.55 | (0.70) | 12.85 | (0.75) |
| Norms: Fem. Quantity | ||||||||||||||
| Control | 8.79 | (0.43) | 7.97 | (0.50) | 8.47 | (0.54) | 8.87 | (0.68) | 8.30 | (0.67) | 8.77 | (0.79) | 8.11 | (0.85) |
| Int. Only | 8.30 | (0.43) | 8.15 | (0.54) | 7.94 | (0.54) | 7.99 | (0.51) | 9.27 | (0.78) | 8.40 | (0.76) | 8.98 | (0.75) |
| Int. + Booster | 8.77 | (0.39) | 8.04 | (0.56) | 7.04 | (0.52) | 6.74 | (0.54) | 7.51 | (0.66) | 6.81 | (0.61) | 7.91 | (0.94) |
| Total | 8.63 | (0.24) | 8.06 | (0.31) | 7.84 | (0.31) | 7.93 | (0.35) | 8.37 | (0.41) | 8.07 | (0.43) | 8.37 | (0.48) |
| PBS: Total | ||||||||||||||
| Control | 32.25 | (1.85) | 36.58 | (3.29) | 31.06 | (3.02) | 34.99 | (4.31) | 31.31 | (3.98) | 29.45 | (4.28) | 30.05 | (4.88) |
| Int. Only | 35.72 | (2.18) | 34.23 | (3.37) | 34.54 | (3.91) | 36.18 | (4.80) | 32.18 | (4.43) | 28.14 | (4.50) | 25.17 | (4.10) |
| Int. + Booster | 32.58 | (1.88) | 36.65 | (3.92) | 31.13 | (3.42) | 28.10 | (2.85) | 27.68 | (3.40) | 23.02 | (3.25) | 20.44 | (4.53) |
| Total | 33.48 | (1.14) | 35.83 | (2.03) | 32.23 | (1.99) | 33.27 | (2.40) | 30.40 | (2.29) | 27.17 | (2.40) | 25.64 | (2.63) |
Note. Int. = alcohol intervention, BAC = blood alcohol concentration, Fem. = female, PBS = protective behavioral strategies. Each cell represents means with standard errors in parentheses.
It should be noted that in the original analysis of these data using the full sample (Braitman & Lau-Barraco, 2018), there was not a significant intervention effect or booster effect on growth for any of the alcohol consumption slopes. However, moderation analyses revealed booster effects for legal age drinkers immediately after booster receipt (i.e., Slope 2, or growth to Week 4), but not for underage drinkers. Intervention non-significant findings were not moderated by age. Despite the lack of significance for intervention effects, however, tests of mediation are still appropriate as they can provide meaningful information, particularly in guiding program improvements (O’Rourke & MacKinnon, 2018).
Moderated Mediation
Moderation analyses were examined first, as they would determine if traditional mediation models were interpretable, or if simple effects mediation models separated by age were more appropriate. A series of likelihood ratio tests indicated that age was not a moderator for mediation via perceived descriptive norms (all p’s > .164). Although the likelihood ratio tests for mediation via PBS indicated that the a paths for the booster were significantly different across age, neither group was significantly different from zero, so the description of the mediation model for the full sample is appropriate (see below). Results available upon request.
Indirect Effects through Norms
The hypothesized paths for model 1 (descriptive norms) and model 2 (PBS) are included in Table 2. Consistent with terminology for indirect effects, the influence of the predictor on the mediator is referred to as the a path, the association between the mediator and the outcome is referred to as the b path, and the direct effect (controlling for the mediator) is referred to as c′ (see Figure 1). The indirect effect is conceptualized as the product of the a and b paths, or ab. For each predictor (i.e., intervention and booster), there are four a paths in the current models (i.e., the influence of the predictor on the mediator Intercept, Slope 1, Slope 2, and Slope 3, labeled a0 through a3, respectively). Similarly, there are four b paths (e.g., the mediator Intercept associated with the drinking Intercept, mediator Slope 1 associated with drinking Slope 1, etc., labeled b0 through b3). The a and b paths are both pictured in Figure 1 for the booster effect. There are also three indirect effects (ab) for each predictor, representing the product of the associated a and b paths. For example, the influence of the booster on mediator Slope 2 (a2) combined with the association between the mediator Slope 2 and drinking Slope 2 (b2) is the indirect effect of booster on Slope 2 drinking through Slope 2 norms (represented as ab2). Finally, there are four direct effects in the current models for each predictor (i.e., the influence of the predictor on the drinking Intercept, Slope 1, Slope 2, and Slope 3, labeled c′0 through c′3, respectively), controlling for the mediator. These paths are all described in Table 2, in addition to their labels.
Table 2.
Descriptive Norms and Protective Behavioral Strategies as Mediators of Intervention and Booster Effects
| Norms |
PBS |
||||||
|---|---|---|---|---|---|---|---|
| Path | b | β | 95% BCCI | B | β | 95% BCCI | |
| Intervention a paths | |||||||
| a0: Intervention → Med. Intercept | −0.38 | −0.04 | [−0.16, 0.08] | 3.44 | 0.08 | [−0.04, 0.23] | |
| a1: Intervention → Med. Slope 1 | 0.59 | 0.60* | [0.13, 1.49] | −6.54 | −0.24 | [−0.57, 0.11] | |
| a2: Intervention → Med. Slope 2 | −0.48 | −0.10 | [−0.33, 0.10] | 6.44 | 0.22 | [−0.06, 0.55] | |
| a3: Intervention → Med. Slope 3 | 0.04 | 0.09 | [−0.14, 0.31] | −0.28 | −0.73* | [−1.14, −0.12] | |
| Booster a paths | |||||||
| a0: Booster → Med. Intercept | 0.15 | 0.02 | [−0.10, 0.14] | −3.23 | −0.08 | [−0.20, 0.07] | |
| a1: Booster → Med. Slope 1 | −0.94 | −0.95* | [−8.84, −0.49] | 7.22 | 0.26 | [−0.05, 0.74] | |
| a2: Booster → Med. Slope 2 | −1.28 | −0.27* | [−0.51, −0.01] | −8.83 | −0.30 | [−0.59, 0.03] | |
| a3: Booster → Med. Slope 3 | 0.01 | 0.02 | [−0.23, 0.26] | −0.02 | −0.06 | [−0.89, 0.93] | |
| b paths | |||||||
| b0: Med. Intercept → Alcohol Int. | 0.10 | 0.40* | [0.27, 0.50] | −0.02 | −0.28* | [−0.37, −0.18] | |
| b1: Med. Slope 1 → Alcohol Slope 1 | 1.33 | 1.73* | [1.02, 34.78] | 0.02 | 0.95 | [−0.42, 1.79] | |
| b2: Med. Slope 2 → Alcohol Slope 2 | 0.09 | 0.27* | [0.01, 0.74] | 0.002 | 0.04 | [−0.55, 0.50] | |
| b3: Med. Slope 3 → Alcohol Slope 3 | 0.13 | 0.32* | [0.02, 0.65] | 0.61 | 1.53* | [0.89, 6.59] | |
| Intervention c′ paths | |||||||
| c′0: Intervention → Alcohol Intercept | 0.21 | 0.09 | [−0.02, 0.21] | 0.26 | 0.09 | [−0.03, 0.20] | |
| c′1: Intervention → Alcohol Slope 1 | −0.90 | −1.19* | [−36.08, −0.31] | −0.10 | −0.17 | [−1.06, 0.88] | |
| c′2: Intervention → Alcohol Slope 2 | 0.16 | 0.11 | [−0.15, 0.32] | 0.13 | 0.07 | [−0.27, 0.37] | |
| c′3: Intervention → Alcohol Slope 3 | −0.03 | −0.19 | [−0.47, 0.04] | 0.15 | 0.95 | [−0.27, 6.82] | |
| Booster c′ paths | |||||||
| c′0: Booster → Alcohol Intercept | 0.01 | 0.004 | [−0.11, 0.12] | −0.07 | −0.02 | [−0.14, 0.09] | |
| c′1: Booster → Alcohol Slope 1 | 1.19 | 1.57* | [0.31, 92.07] | −0.15 | −0.26 | [−1.16, 0.79] | |
| c′2: Booster → Alcohol Slope 2 | −0.06 | −0.04 | [−0.30, 0.27] | −0.10 | −0.06 | [−0.42, 0.26] | |
| c′3: Booster → Alcohol Slope 3 | −0.003 | −0.02 | [−0.26, 0.22] | 0.01 | 0.04 | [−1.88, 3.56] | |
| Intervention indirect effects | |||||||
| ab1: Intervention → Med. Slope 1 → Alcohol Slope 1 | 0.788 | 1.045* | [0.16, 35.72] | −0.130 | −0.223 | [−1.25, 0.12] | |
| ab2: Intervention → Med. Slope 2 → Alcohol Slope 2 | −0.041 | −0.027 | [−0.15, 0.01] | 0.014 | 0.008 | [−0.16, 0.25] | |
| ab3: Intervention → Med. Slope 3 → Alcohol Slope 3 | 0.005 | 0.031 | [−0.04, 0.17] | −0.174* | −1.118* | [−7.12, −0.004] | |
| Booster indirect effects | |||||||
| ab1: Booster → Med. Slope 1 → Alcohol Slope 1 | −1.247 | −1.649* | [−98.25, −0.39] | 0.143 | 0.245 | [−0.08, 1.71] | |
| ab2: Booster → Med. Slope 2 → Alcohol Slope 2 | −0.109 | −0.071* | [−0.32, −0.002] | −0.020 | −0.011 | [−0.27, 0.19] | |
| ab3: Booster → Med. Slope 3 → Alcohol Slope 3 | 0.001 | 0.007 | [−0.10, 0.11] | −0.015 | −0.095 | [−3.69, 1.91] | |
Note. Med. = Mediator, Int. = Intercept, 95% BCCI = 95% bias-corrected bootstrap confidence intervals for standardized estimates, PBS = protective behavioral strategies. Significant effects at the p < .05 level (as evidenced by BCCIs not containing zero) are indicated with bold text.
p < .05
Intervention effects.
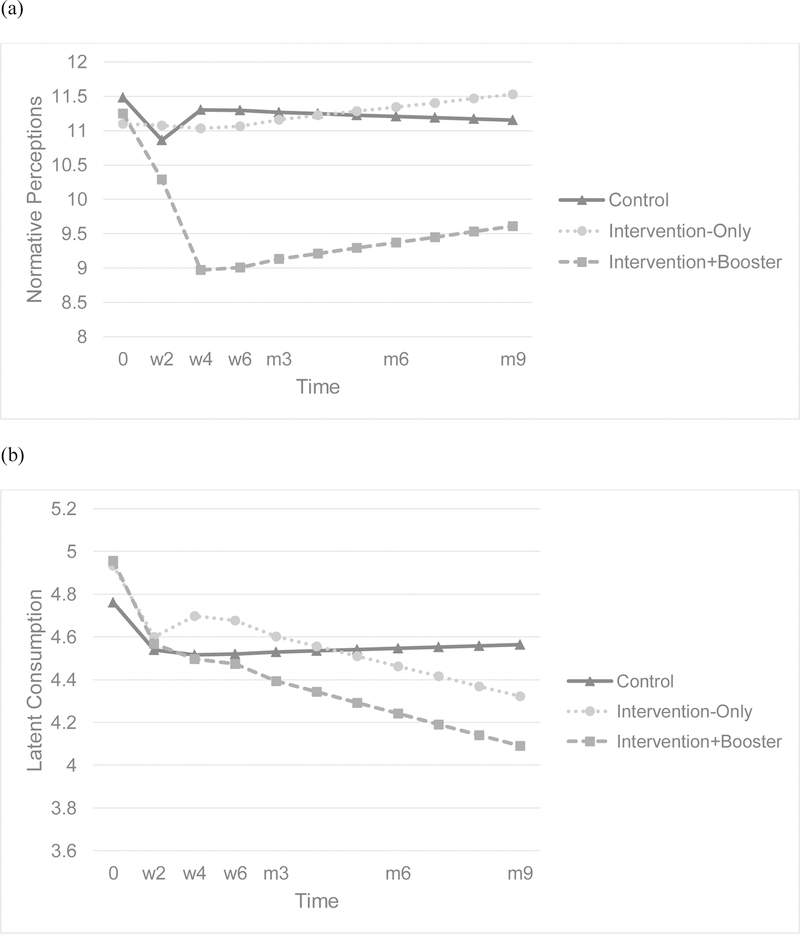
In the descriptive norms model, there was a significant, positive a path for the intervention (as seen in the left half of Table 2), β = 0.60, indicating that reductions in descriptive norms were not as strong for those who received the intervention as for those in the control group (as observed in panel a of Figure 2). Because changes in norms (growth to week 2; i.e., Slope 1) were significantly, positively associated with corresponding changes in drinking (also Slope 1), β = 1.73, the indirect effect of intervention on alcohol through norms (ab1) was significant, β = 1.045. This indicates that weaker norms reductions for those who received the intervention (compared to controls) were associated with weaker drinking reductions as well, through those weaker changes in norms. Despite this unfavorable indirect effect, there was also a significant, negative direct effect for the intervention on Slope 1, β = −1.19, indicating that those who received the intervention had significantly stronger reductions in their drinking relative to the control group, after controlling for descriptive norms (as observed in panel b of Figure 2). No other intervention effects (or associated indirect effects) were significant in the descriptive norms model.
Figure 2.
Descriptive norms (panel a) and standard drinks (panel b) over time by condition. Control = general health intervention only, Intervention-Only = alcohol intervention only, Intervention+Booster = alcohol intervention plus personalized feedback booster email, w2 = week 2, w4 = week 4, w6 = week 6, m3 = month 3, m6 = month 6, m9 = month 9.
Booster effects.
There were two significant paths for the booster. As expected, receiving the booster email led to a significantly stronger decrease in descriptive norms from week 2 to week 4 (a2; i.e., Slope 2), β = −0.27, as compared to receiving the intervention without a booster email. Surprisingly, the booster group also had significantly stronger decreases from baseline to week 2 (a1; i.e., Slope 1), β = −0.95, despite not yet having received the booster email. There was not a significant effect for Slope 3 (a3), indicating that maintenance trajectories for earlier changes were similar across conditions. All four b paths were significant, indicating that higher norms at baseline were associated with more drinking at baseline (b0), β = 0.40. In addition, changes in norms up to Week 2 (b1; post-intervention), Week 4 (b2; post booster email), and longer-term (b3) were associated with corresponding changes in drinking, or reduced norms were associated with reduced drinking.
The indirect effect (ab) of the booster email on alcohol (Slope 2) through norms (Slope 2; ab2) was significant, β = −0.071, indicating that the personalized feedback delivered via email yielded reductions in alcohol use through reduced descriptive norms. The size of this effect may be best expressed as the ratio of the indirect effect to the total effect, given that the indirect and direct effects are of the same direction (Wen & Fan, 2015). In this case, PM = .645, indicating the indirect effect accounts for 64.5% of the total effect, where the total effect b = −0.169 (β = −0.110). The anomalous booster effect on Slope 1 also has a significant corresponding indirect effect, β = −1.649, where the booster group’s stronger reductions in norms were associated with a stronger reduction in alcohol use. However, because the indirect effect and direct effect are of opposite valence, the majority of effect size approximations are inappropriate (Wen & Fan, 2015).
Finally, there was a significant direct effect for the booster for Slope 1 (c′1; again, before the booster email), β = 1.57, indicating a significantly weaker reduction in drinking for the booster group as compared to the intervention-only group, controlling for descriptive norms. This may be the counterpart to the anomalous finding regarding significantly stronger norm reductions (discussed further below). As seen in panel (b) of Figure 2, overall drinking was reduced. No other direct effects were significant. Model results are plotted in Figure 2. Panel (a) demonstrates condition effects on descriptive norms over time, which demonstrates a sharp decrease in descriptive norms for the booster group after receiving the personalized feedback booster email. Maintenance trajectories are similar across groups, demonstrating slight increases in norms over the maintenance period. However, norms are still substantially lower for the booster condition at month 9 as compared to any condition at baseline. Panel (b) demonstrates the effect of condition on drinking over time, incorporating both direct effects and indirect effects through norms. All three conditions experience a decline in drinking leading to week 2 (Slope 1; post-intervention), even the control group, though their decline is less steep. The control condition then levels off drinking, with a slight upward trajectory through month 9. After the initial drinking reduction, the intervention-only condition experiences an upward bump in drinking though week 4 (Slope 2) showing a slight change in the direction of returning to pre-intervention levels, before maintaining a long-term trajectory of mild declines through month 9 (Slope 3). After the initial drinking reduction, the intervention-plus-booster condition experiences another drop in drinking through week 4 (Slope 2; post-booster), before maintaining a similar long-term trajectory of continued mild declines through month 9 (Slope 3).
A similar model was run, but with alcohol-related problems (i.e., Young Adult Alcohol Consequences Questionnaire; Read et al., 2006) as the outcome of interest. Results for mediation were non-significant for both intervention and booster effects (details available upon request).
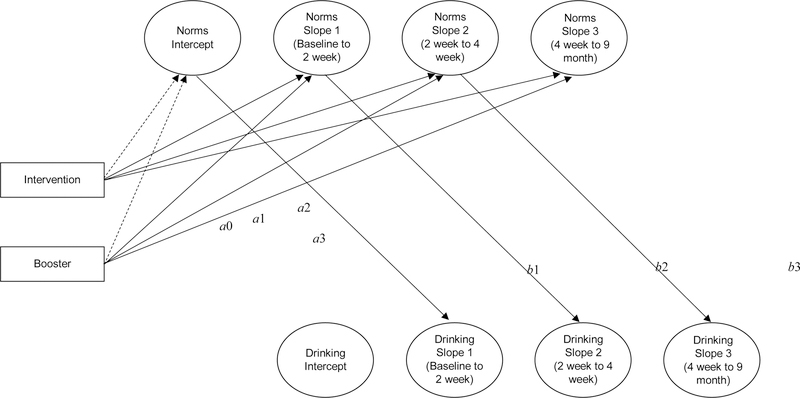
Fully Longitudinal Mediation
In the main model, slopes for alcohol consumption were regressed onto the slopes for the mediator within the same time period (e.g., drinking Slope 2 was regressed on norms Slope 2 to capture how changes in norms from Week 2 to Week 4 corresponded with changes in drinking from Week 2 to Week 4). An additional model was conducted to assess fully longitudinal mediation, regressing alcohol consumption slopes onto the slopes for the mediator for the prior time period (e.g., drinking Slope 2 was regressed on norms Slope 1 to capture how changes in norms from baseline to Week 2 corresponded with changes in drinking from Week 2 to Week 4; see Figure 3). This analysis allows for the assessment of whether changing norms are associated with subsequent, rather than simultaneous, behavior change. The variances of the norms latent variables were constrained to zero to aid in model convergence. As seen in Table 3, the only a path approaching significance was for a2, such that the decrease in norms to Week 4 (i.e., Slope 2) was stronger for the booster group, b = −1.15, β = −0.14, 90% BCCI [−2.15, −0.01], corresponding with p<.10. There were multiple significant b paths for the associations between norms and drinking, including: b1 such that having lower norms at baseline was associated with decreased drinking to Week 2 (i.e., Slope 1), b = 0.04, β = 0.94, 95% BCCI [0.02, 0.06]; b2 such that reduced norms to Week 2 was associated with decreased drinking to Week 4, b = 0.04, β = 0.24, 95% BCCI [0.01, 0.09]; and approaching significance for b3 such that reducing norms to Week 4 was associated with decreased drinking through month 9, b = 0.004, β = 0.18, 95% BCCI [0.000, 0.01]. The indirect effect of the booster on reduced longer-term drinking (alcohol Slope 3) through reduced Week 4 norms (norms Slope 2), ab3, approached significance, b = −0.004, β = −0.025, 95% BCCI [−0.01, 0.000]. No other effects were significant.
Figure 3.
Completely longitudinal mediation assessed via Dual Process Latent Growth Models, assessing the indirect effects of condition on alcohol consumption through descriptive norms. Though included in the model, direct effects are omitted from the figure for clarity. Dashed lines indicate effects prior to the relevant manipulation (i.e., before intervention effects, or before booster effects), and thus expected to be non-significant but included for definitional purposes. Note that intervention was coded 0 (control health session) or 1 (alcohol intervention), and booster was coded 0 (control email) or 1 (personalized feedback email).
Table 3.
Fully Longitudinal: Descriptive Norms as a Mediator of Intervention and Booster Effects
| Norms |
|||
|---|---|---|---|
| Path | b | β | 95% BCCI |
| Intervention a paths | |||
| a0: Intervention → Med. Intercept | −0.38 | −0.04 | [−1.52, 0.69] |
| a1: Intervention → Med. Slope 1 | 0.61 | 0.08 | [−0.27, 1.60] |
| a2: Intervention → Med. Slope 2 | −0.57 | −0.07 | [−1.65, 0.31] |
| a3: Intervention → Med. Slope 3 | 0.05 | 0.09 | [−0.04, 0.12] |
| Booster a paths | |||
| a0: Booster → Med. Intercept | 0.13 | 0.01 | [−0.88, 1.23] |
| a1: Booster → Med. Slope 1 | −1.07 | −0.12 | [−2.18, 0.19] |
| a2: Booster → Med. Slope 2 | −1.15† | −0.14 | [−2.36, 0.16] |
| a3: Booster → Med. Slope 3 | 0.01 | 0.01 | [−0.09, 0.11] |
| b paths | |||
| b1: Med. Intercept → Alcohol Slope 1 | 0.04* | 0.94 | [0.02, 0.06] |
| b2: Med. Slope 1 → Alcohol Slope 2 | 0.04* | 0.24 | [0.01, 0.09] |
| b3: Med. Slope 2 → Alcohol Slope 3 | 0.004† | 0.18 | [0.000, 0.01] |
| Intervention c′ paths | |||
| c′0: Intervention → Alcohol Intercept | 0.17 | 0.08 | [−0.12, 0.48] |
| c′1: Intervention → Alcohol Slope 1 | −0.09 | −0.22 | [−0.38, 0.27] |
| c′2: Intervention → Alcohol Slope 2 | 0.09 | 0.06 | [−0.28, 0.42] |
| c′3: Intervention → Alcohol Slope 3 | −0.02 | −0.14 | [−0.06, 0.01] |
| Booster c′ paths | |||
| c′0: Booster → Alcohol Intercept | 0.03 | 0.01 | [−0.27, 0.31] |
| c′1: Booster → Alcohol Slope 1 | −0.07 | −0.17 | [−0.39, 0.25] |
| c′2: Booster → Alcohol Slope 2 | −0.12 | −0.08 | [−0.47, 0.29] |
| c′3: Booster → Alcohol Slope 3 | 0.004 | 0.02 | [−0.03, 0.04] |
| Intervention indirect effects | |||
| ab1: Intervention → Med. Intercept → Alcohol Slope 1 | −0.014 | −0.033 | [−0.08, 0.02] |
| ab2: Intervention → Med. Slope 1 → Alcohol Slope 2 | 0.027 | 0.018 | [−0.01, 0.09] |
| ab3: Intervention → Med. Slope 2 → Alcohol Slope 3 | −0.002 | −0.012 | [−0.01, 0.001] |
| Booster indirect effects | |||
| ab1: Booster → Med. Intercept → Alcohol Slope 1 | 0.005 | 0.011 | [−0.03, 0.05] |
| ab2: Booster → Med. Slope 1 → Alcohol Slope 2 | −0.045 | −0.029 | [−0.15, 0.003] |
| ab3: Booster → Med. Slope 2 → Alcohol Slope 3 | −0.004† | −0.025 | [−0.01, 0.000] |
Note. Med. = Mediator, Int. = Intercept, 95% BCCI = 95% bias-corrected bootstrap confidence intervals for standardized estimates, PBS = protective behavioral strategies. Differences between this completely longitudinal mediation model (Figure 3) and the earlier mediation model (Figure 1) are indicated with underlined text. Significant effects at the p < .05 level (as evidenced by 95% BCCIs not containing zero) are indicated with bold text. Effects approaching significance are indicated with italic text, as evidenced by a 90% BCCI that does not contain zero, or a 95% BCCI that end with zero (p = .05).
p < .05
p < .10
Indirect Effects through PBS
Intervention effects.
There was one significant a path for the intervention, indicating that receiving the intervention resulted in a significantly different long-term trajectory through month 9 for PBS use (a3; Slope 3), β = −0.73. Whereas the control condition had a slight negative trajectory for PBS use long-term, this slope was steeper for conditions who received the intervention. The remaining a paths were not significant, indicating that receiving the intervention was not significantly associated with differences in initial PBS use (Intercept), or immediate changes in PBS use (Slopes 1 and 2).
Two b paths were significant for the associations between PBS use and alcohol consumption. The association between the PBS and alcohol intercepts was significant and negative, β = −0.28, indicating that higher PBS use at baseline was associated with less drinking at baseline (b0). In addition, long-term changes in PBS use were associated with similar changes in drinking (b3), β = 1.53. This effect was in the opposite of the hypothesized direction, such that decreased PBS use was associated with decreased drinking through month 9. The corresponding indirect effect was significant (ab3), β = −1.118, where intervention receipt was associated with decreased drinking through decreased PBS use, as seen in Table 2. Because the direct and indirect effects are of opposite signs, most effect size indicators are inappropriate (Wen & Fan; 2015).
No other b paths were significant, meaning changes in PBS use up to Week 2 (Slope 1; post-intervention; b1) and Week 4 (Slope 2; b2) were not associated with corresponding changes in drinking. Similarly, there were no other significant indirect effects, and there were no significant direct effects.
Booster effects.
There were no significant a paths for the effect of booster condition, indicating that there were no significant differences in PBS use for the booster condition at baseline, nor in subsequent growth. As seen in Table 2, there were no significant indirect effects for the influence of the booster on drinking through PBS use.
A similar model was run, but with alcohol-related problems as the outcome of interest. Results for mediation were non-significant for both intervention and booster effects (details available upon request). A fully longitudinal mediation model was not conducted given that PBS effects did not emerge until Slope 3.
Discussion
The current study was a follow-up analysis of data from an RCT assessing the efficacy of emailed boosters containing personalized feedback after a CDI targeting college drinking. It explored descriptive normative perceptions and PBS as potential mechanisms of change for intervention and booster effects. There was support for descriptive norms as a mediator of booster efficacy where receiving the booster yielded stronger reductions in alcohol use through reduced norms, as expected. Surprisingly, there was also an indirect effect for the intervention where those who received the intervention experienced a weakened decrease in drinking through weaker decreased norms. However, there was a stronger countering direct effect where those who received the intervention experienced a stronger decrease in drinking after controlling for norms. There was tepid support for norms as a longitudinal booster mediator and no support for PBS as a simultaneous mediator of booster or intervention efficacy. Although the original study found age moderated the booster such that it was more effective for emerging adult students of legal drinking age (ages 21–24) compared to underage students (ages 18–20; Braitman & Lau-Barraco, 2018), current analyses revealed that mediation models were not moderated by age.
Descriptive Normative Perceptions
The positive associations between norms and alcohol consumption for all time periods (i.e., initial reported levels as well as corresponding changes in growth over time) were as expected. Individuals with lower norms consumed less alcohol, and those who reduced their norms also reduced their consumption. Also as expected, there was a significant indirect effect for the booster’s influence on alcohol consumption through norms (i.e., the booster was associated with decreased norms, which was associated with deceased consumption). This effect approached but did not reach significance in the fully longitudinal mediation model. These findings are consistent with the literature, with robust associations between norms and drinking (Perkins, 2002, Borsari & Carey, 2003), and personalized normative feedback with norms reductions (LaBrie et al., 2013; Lewis et al., 2007; Martens et al., 2013; Mattern & Neighbors, 2004; Neighbors, Lewis, et al., 2010).
Surprisingly, there was an intervention indirect effect on drinking through norms that was positive, where reductions were not as strong for those receiving the intervention (for norms and consumption), though this was balanced with a stronger negative direct effect (where intervention recipients experienced reduced consumption, after controlling for this milder decrease in norms). In other words, the intervention was linked to reduced alcohol consumption after controlling for changes in norms, so the intervention yielded drinking reductions, but not through descriptive normative perceptions. This may imply that the unintended weaker decrease in descriptive norms for intervention recipients is being countered by a decrease in some other construct to produce the significant direct effect on drinking, with the two effects together producing a non-significant total effect for the intervention. Similarly, there was a significant, positive direct effect for the booster group for Slope 1 (before the booster email), indicating a weaker reduction in drinking for the booster group compared to the intervention-only group, controlling for descriptive norms. Again, this weaker effect controlling for norms (the direct effect) is countered by a stronger decrease in drinking through norms (the indirect effect), producing a non-significant total effect for the booster before it was sent. This non-significant total effect pre-booster is apparent in panel (b) of Figure 2, as is the stronger reduction in drinking for both intervention groups (intervention-only and intervention+booster). The pictured projected trajectories account for both effects simultaneously (the direct and indirect), and receiving the intervention still led to drinking reductions. This unexpected finding regarding the main intervention effect on norms may be due to the nature of how the norms were presented in the booster versus the intervention. The descriptive normative information presented in the intervention was not personalized (i.e., national college student drinking norms) while the booster presented descriptive norms that were personalized both for the institution as well as for sex (i.e., presenting typical drinking for males and females separately).
Moreover, the intervention used in the current study was not linear in nature, but instead was a virtual campus where the participant could choose to interact with different content. Normative information was presented in a specific “location” on the virtual campus; it is possible some participants did not visit that location or had other content competing for their attention, thus did not get the normative information. This ineffective presentation of normative descriptive information may partially explain the anomalous increase in norms as a main effect of the intervention. On the other hand, for the booster condition, the norms feedback was presented at the beginning of the email, and the email was relatively short; it is likely that the norms content was fully attended to by the recipients that read their emails. Unfortunately, that information was not tracked in the current study.
The finding that descriptive norms mediate the booster effect are consistent with findings that norms are a robust mechanism of change for college drinking interventions (Reid & Carey, 2015). They may be a potential mechanism of change for boosters as well. In a series of articles describing how an indirect effect can be established as a mechanism of change (MoC; Kazdin, 2007; Kazdin & Nock, 2003; Nock, 2007), Kazdin and Nock outline several criteria that must be met. Firstly, there must be strong associations for both the a and b paths. This was supported in the current study, as receiving the booster email was associated with a norms reduction of 1.28 drinks (β = −0.27), and the association between changes in norms and changes in drinking was of a similar size (β = 0.27). To be a MoC, the mediator must also be plausible as a mechanism, which is clearly supported. In addition, although an indirect effect through norms was identified, PBS was tested and found not to be a mediating factor, contributing to specificity of the relationship, another supporting indicator for norms as a MoC. Another required criterion for MoC status is that the mediator must be targeted by the booster in an experimental manipulation, which was supported in the current study, as norms were clearly presented in the booster email as part of an RCT. There also must be a temporal relationship between these changes. This is true for the a path; the booster was received prior to the corresponding reductions in norms. For the b path, the reductions in norms correspond with drinking reductions for the same time period (Slope 2, or growth to week 4), and in the fully longitudinal model the relevant change in growth was approaching significance (p=.05). However, two critical components are missing before one can conclude that descriptive norms are a MoC for the booster effect. Consistency across trials would provide further support for this supposition, suggesting more research is needed. In addition, gradient (i.e., establishing a dose–response relationship) was not examined in the current study. Future research might consider sending multiple booster messages with personalized feedback to determine if additional treatment is associated with further reductions in both norms and drinking.
PBS
As expected, more PBS use at baseline was associated with less drinking at baseline. However, there was an unexpected indirect effect for the intervention, where intervention receipt was associated with less PBS use longer-term (Slope 3), which in turn was associated with weaker inclines over time (also Slope 3). Thus, reduced alcohol use longer-term for the intervention group was through reduced PBS use, counter to the anticipated direction of the effect. There was not a main intervention effect on PBS for Slope 1. An examination of the intercept for Slope 1 for PBS use reveals a non-significant trend for PBS use to increase through week 2 (B = 3.51, β = 0.27, p = .253) for all groups, so this reduction in PBS use for the intervention group may reflect simply a return to original levels. In addition, PBS use was not supported as a mediator of the booster. Although counter to hypotheses, these findings are not surprising given prior literature. Although many studies have demonstrated drinking reductions after multi-component interventions including promotion of PBS use (e.g., Dimeff et al., 1999; Kivlahan et la., 1990), findings for PBS-focused interventions are more mixed. Studies using single-component PBS interventions reported increased PBS use and decreased alcohol consumption or related problems in select populations (Dvorak et al., 2015, 2017; Kramer, & Stevenson, 2017; Kenney et al., 2014). However, two studies focused on general college drinkers found increases in PBS use after a PBS-focused intervention were not associated with corresponding reductions in drinking or problems (Martens et al., 2013; Sugarman & Carey, 2009), contributing to ambiguity in the literature.
Examining PBS use as a mediator of intervention or booster effects may yield inconsistent findings due to imperfect assessment. Contingent response scales like the one used in the current study is the best choice of those available and has yielded theoretically-consistent associations with alcohol use (i.e., more PBS use linking to reduced consumption; Kite, 2013; Braitman et al., 2015). However, within the current study, even though PBS use was deconflated from frequency of drinking, consuming more within a single occasion may present more opportunities to use PBS (or, drinking less may limit opportunities, such as not needing a designated driving, no opportunities to decline drinks, etc.). So higher scores may naturally be associated with higher risk drinking situations simply because of more opportunities to use PBS. In addition, using one strategy effectively (such as choosing to engage in another activity besides drinking) could be more effective than using a higher number of other strategies. Thus, an effective intervention may help students recognize strategies that are most helpful and relevant for them, and so could use fewer strategies but choose them more effectively. Given the documented assessment issues across all available PBS measures, and questions of differing effectiveness of each strategy, it is difficult to identify whether prevention and intervention efforts should target strengthening the a path (booster/intervention influence on PBS use) or if the failure is in the b path (associations between PBS use and consumption). Future research should manipulate the presence of PBS items in the personalized feedback incorporated as part of the intervention or booster. This will permit directly assessing the impact of PBS feedback, without entangling with assessment issues. Significant changes in drinking based on the presence of PBS feedback could point to PBS as a promising active ingredient for booster feedback.
Limitations and Future Directions
There are several limitations in the current examination. Most notably, the study was powered for the parent study to detect booster efficacy, rather than indirect effects through potential mediators. Related, retention rates were low for the follow-up surveys, possibly due to changes in compensation type (from course credit, to payments, to raffles), which may limit the conclusions one may make. However, missingness for the follow-up surveys was not associated with demographic characteristics, baseline consumption, or condition assignment. Moreover, the use of maximum likelihood estimation allowed for the inclusion of all participants in analyses. In addition, in the fully longitudinal mediation model, the relevant b paths (post-intervention, and post-booster) were weaker. This is may be because the impact of drinking beliefs on behaviors may be strongest in the shorter term (e.g., same day, next day); detecting proximal sequential change may be better examined with a more fine-grained assessment. And as reviewed above, assessing PBS use can be problematic, so future research should manipulate the presence of PBS feedback in the booster to assess its impact. In addition, future research should explore the ideal timing of the booster feedback, as many studies indicate drinking reductions are still demonstrated at one month post-intervention (Carey et al., 2009). Moreover, assessing the impact of multiple booster emails would help to establish a dose-response relationship to support the gradient component of establishing norms as a MoC. Finally, the current investigation focused on general college drinkers. Results may not generalize to specific college populations that are common targets for intervention (e.g., mandated students, athletes, students involved in Greek life). In particular, future research should explore non-student emerging adults. Interventions are under-examined in this population, suggesting a strong potential for booster effects. However, in one study examining intervention impact among heavy drinking nonstudent emerging adults, descriptive norms were a mediator of intervention efficacy (Lau-Barraco et al., 2018), suggesting they could be a valuable target for booster feedback as well.
Conclusion
The current study was a follow-up analysis of an RCT examining efficacy of a booster email containing personalized feedback. The two booster components (descriptive norms and PBS use) were examined as mediators of the intervention and booster effects in the current examination. Although there was no support for PBS use, descriptive norms emerged as a significant mediator of the booster, where reductions in drinking after the booster were through simultaneous reduced descriptive norms. There was a similar but non-significant finding through lagged reduced descriptive norms. The present study was the first, to our knowledge, to explore and demonstrate a potential MoC in booster interventions. We demonstrated that a simple, succinct reminder via email lead to reductions in perceptions of how much their peers drink and this led to reductions in their alcohol consumption. Our findings support the promise of utilizing brief and easily implemented targeted messaging to enhance the potency of computerized interventions for college drinkers.
Acknowledgments
The project described was supported by award F32 AA021310 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; PI: Braitman). Preparation of this article was partially supported by a Career Development Award from the NIAAA (K01 AA023849; PI: Braitman).
Footnotes
All authors declare that they have no conflicts of interest.
References
- Abbey A, Wegner R, Woerner J, Pegram SE, Pierce J (2014) Review of survey and experimental research that examines the relationship between alcohol consumption and men’s sexual aggression perpetration. Trauma Violence Abus 15:265–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, Monti PM (2007) Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addict Behav 32:2529–2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolin RM, Pate M, McClintock J (2017) The impact of alcohol and marijuana use on academic achievement among college students. Soc Sci J 54:430–437. [Google Scholar]
- Borsari B, Carey KB (2003) Descriptive and injunctive norms in college drinking: a meta-analytic integration. J Stud Alcohol 64:331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, Henson JM (2016) Personalized boosters for a computerized intervention targeting college student drinking: The influence of protective behavioral strategies. J Am Coll Health 64:509–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, Henson JM, Carey KB (2015) Clarifying observed relationships between protective behavioral strategies and alcohol outcomes: The importance of response options. Psychol Addict Behav 29:455–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, Lau-Barraco C (2018) Personalized boosters after a computerized intervention targeting college drinking: A randomized controlled trial. Alcohol Clin Exp Res 42:1735–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler LH, Correia CJ (2009) Brief alcohol intervention with college student drinkers: Face-to-face versus computerized feedback. Psychol Addict Behav 23:163–167. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Henson JM, Maisto SA, DeMartini KS (2011) Brief alcohol interventions for mandated college students: Comparison of face-to-face counseling and computer-delivered interventions. Addiction 106:528–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Bolles JR, Carey MP (2009) Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction 104:1807–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, Carey MP (2012) Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clin Psychol Rev 32:690–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Walsh JL, Merrill JE, Lust SA, Reid AE, Scott-Sheldon LAJ, Kalichman SC, Carey MP (2018) Using e-mail boosters to maintain change after brief alcohol interventions for mandated college students: A randomized controlled trial. J Consult Clin Psych 86:787–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caudill BD, Luckey B, Crosse SB, Blane HT, Ginexi EM, Campbell B (2007) Alcohol risk-reduction skills training in a national fraternity: A randomized intervention trial with longitudinal intent-to-treat analysis. J Stud Alcohol Drugs 68:399–409. [DOI] [PubMed] [Google Scholar]
- Cole HA, Prassel HB, Carlson CR (2018) A meta-analysis of computer-delivered drinking interventions for college students: A comprehensive review of studies from 2010 to 2016. J Stud Alcohol Drugs 79:686–696 [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA (1985) Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psych 53:189–200. [DOI] [PubMed] [Google Scholar]
- Conway JM, DiPlacido J (2015) The indirect effect of alcohol use on GPA in first-semester college students: The mediating role of academic effort. J Coll Student Retention: Res Theory Pract 17:303–318. [Google Scholar]
- Dallery J, Jarvis B, Marsch L, Xie H (2015) Mechanisms of change associated with technology-based interventions for substance use. Drug Alcohol Depen 150:14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA (1999) Brief Alcohol Screening and Intervention for College Students (BASICS): A harm reduction approach, Guilford Press. [Google Scholar]
- Donohue B, Allen DN, Maurer A, Ozols J, DeStefano G (2004) A controlled evaluation of two prevention programs in reducing alcohol use among college students at low and high risk for alcohol related problems. J Alcohol Drug Educ 48:13–33. [Google Scholar]
- Dvorak RD, Kramer MP, Stevenson BL, Sargent EM, Kilwein TM (2017) An application of deviance regulation theory to reduce alcohol-related problems among college women during spring break. Psychol Addict Behav 31:295–306. [DOI] [PubMed] [Google Scholar]
- Dvorak RD, Pearson MR, Neighbors C, Martens MP (2015) Fitting in and standing out: Increasing the use of alcohol protective behavioral strategies with a deviance regulation intervention. J Consult Clin Psych 83:482–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Carey KB, & Bolles JR (2008) Computer-based interventions for college drinking: a qualitative review. Addict Behav 33:994–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Zha W, Weitzman ER (2009) Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs 16(Suppl.):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (2007) Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol 3:1–27. [DOI] [PubMed] [Google Scholar]
- Kazdin AE Nock MK (2003) Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol and Psyc 44:1116–1129 [DOI] [PubMed] [Google Scholar]
- Kenney SR, Napper LE, LaBrie JW, Martens MP (2014) Examining the efficacy of a brief group protective behavioral strategies skills training alcohol intervention with college women. Psychol Addict Behav 28:1041–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kite BA, Pearson MR, Henson JM. (2013) The assessment of protective behavioral strategies: Comparing the Absolute Frequency and Contingent Frequency Response Scales. Psychol Addict Behav 27:1010–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, Williams E (1990) Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. J Consult Clin Psych 58:805–810 [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Lewis MA, Atkins DC, Neighbors C, Zheng C, Kenney SR, … Grossbard J (2013) RCT of web-based personalized normative feedback for college drinking prevention: are typical student norms good enough? J Consult Clin Psych 81:1074–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Napper LE, Grimaldi EM, Kenney SR, Lac A (2015) The efficacy of a standalone protective behavioral strategies intervention for students accessing mental health services. Prev Sci 16:663–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau-Barraco C, Braitman AL, Linden-Carmichael A, Stamates AL (2018) Mediators and moderators of a personalized feedback alcohol intervention for nonstudent emerging adult drinkers. Alcohol Clin Exp Res 42:1756–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C (2006) Social norms approaches using descriptive drinking norms education: A review of the research on personalized normative feedback. J Am Coll Health 54:213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C, Oster-Aaland L, Kirkeby BS, Larimer ME (2007) Indicated prevention for incoming freshmen: Personalized normative feedback and high-risk drinking. Addict Behav 32:2495–2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linowski SA, DiFulvio GT, Fedorchak D, Puleo E (2016) Effectiveness of an electronic booster session delivered to mandated students. Int Quart Community Health Educ 36:123–129. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J (2004) Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar Behav Res 39:99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Colby SM, Orchowski L, Murphy JG, Hoadley A, Brazil LA, Barnett NP (2017) How does brief motivational intervention change heavy drinking and harm among underage young adult drinkers? J Consult Clin Psych 85:447–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A (2005) Development of the protective behavioral strategies survey. J Stud Alcohol 66:698–705. [DOI] [PubMed] [Google Scholar]
- Martens MP, Smith AE, Murphy JG (2013). The efficacy of single-component brief motivational interventions among at-risk college drinkers. J Consult Clin Psych 81:691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattern JL, Neighbors C (2004). Social norms campaigns: examining the relationship between changes in perceived norms and changes in drinking levels. J Stud Alcohol 65:489–493. [DOI] [PubMed] [Google Scholar]
- Matthews DB, Miller WR (1979) Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Addict Behav 4:55–60. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Martens MP, McDevitt-Murphy ME (2010) Computerized versus motivational interviewing alcohol interventions: impact on discrepancy, motivation, and drinking. Psychol Addict Behav 24:628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (1998–2017) Mplus User’s Guide (Eighth ed.). Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- Neighbors C, LaBrie JW, Hummer JF, Lewis MA, Lee CM, Desai S, Kilmer JR, Larimer ME (2010) Group identification as a moderator of the relationship between perceived social norms and alcohol consumption. Psychol Addict Behav 24:522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Lee CM, Larimer ME (2010) Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial. J Consult Clin Psych 78:898–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Rodriguez LM, Garey L, Tomkins MM (2018) Testing a motivational model of delivery modality and incentives on participation in a brief alcohol intervention. Addict Behav 84:131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK (2007) Conceptual and design essentials for evaluating mechanisms of change. Alcohol Clin Exp Res 31:4s–12s. [DOI] [PubMed] [Google Scholar]
- O’Rourke HP, MacKinnon DP (2018) Reasons for testing mediation in the absence of an intervention effect: A research imperative in prevention and intervention research. J Stud Alcohol Drugs 79:171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR (2013) Use of alcohol protective behavioral strategies among college students: A critical review. Clin Psychol Rev 33:1025–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins HW (2002) Social norms and the prevention of alcohol misuse in collegiate contexts. J Stud Alcohol 14(Suppl.):164–172. [DOI] [PubMed] [Google Scholar]
- Prince MA, Carey KB, Maisto SA (2013) Protective behavioral strategies for reducing alcohol involvement: A review of the methodological issues. Addict Behav 38:2343–2351. [DOI] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR (2006) Development and preliminary validation of the Young Adult Alcohol Consequences Questionnaire. J Stud Alcohol 67:169–177. [DOI] [PubMed] [Google Scholar]
- Reid AE, Carey KB (2015) Interventions to reduce college student drinking: State of the evidence for mechanisms of behavior change. Clin Psychol Rev 40:213–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez LM, Neighbors C, Rinker DV, Lewis MA, Lazorwitz B, Gonzales RG, Larimer ME (2015) Remote versus in-lab computer-delivered personalized normative feedback interventions for college student drinking. J Consult Clin Psych 83:455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman DE, Carey KB (2009) Drink less or drink slower: The effects of instruction on alcohol consumption and drinking control strategy use. Psychol Addict Behav 23:577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman DE, Carey KB (2007) The relationship between drinking control strategies and college student alcohol use. Psychol Addict Behav 21:338–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Hoffman JH (2012). Naturally occurring changes in women’s drinking from high school to college and implications for sexual victimization. J Stud Alcohol Drugs 73:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Jouriles EN (2009) Reactivity to alcohol assessment measures: an experimental test. Addiction 104:1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z, Fan X (2015) Monotonicity of effect sizes: Questioning kappa-squared as mediation effect size measure. Psychol Methods 20:193–203. [DOI] [PubMed] [Google Scholar]