Abstract
We aim to predict the number of new HIV cases over the 11 years among men who have sex with men(MSM), under different voluntary medical male circumcision(VMMC) coverage rates in Beijing, China. Using a deterministic compartmental modeling procedure to fit prevalence from 2005-2015, we projected new HIV cases during 2016-2026 under different coverage rates ranging from 0.0001 (at baseline) to 0.15 (an optimistic assumption) with simulations on varying transmission rates, model calibration to match historical data, and sensitivity analyses for different assumptions. Compared with the baseline (λ=0.0001), we found the new HIV cases would reduce with the increase of coverage rates of the VMMC among MSM. The higher the coverage rate, the lower the new HIV incidence would be. The number of new HIV cases would keep decreasing by 0.15%, 0.80%, 1.6%, 7.1%, 12.4% and 16.3% compared to the baseline by the end of 2026, if we increase the annual coverage rate of VMMC to 0.01, 0.005, 0.01, 0.05, 0.1 and 0.15, respectively. As one of the first studies to model the potential impact of VMMC among MSM in China, our model suggested a modest to the significant public health impact of VMMC. Even at just 15% VMMC annual uptake rate, the reduction in new infections is substantial. Therefore, there is a strong need to determine the efficacy of VMMC among MSM, to improve the evidence base for its potential use among MSM in low circumcision settings. Only then can policymakers decide whether to incorporate VMMC into a package of HIV prevention interventions targeting MSM.
Keywords: Voluntary medical male circumcision, mathematical modeling, HIV, incidence, men who have sex with men, China
INTRODUCTION
Based upon a newly released report from the Chinese government, the reported number of people living with HIV/AIDS(PLWHA) in China was 575,000 by the end of 2015(ChinaDaily,2015). Although national HIV surveillance data suggest that China is a relatively low-prevalence country, the trend of increasing HIV prevalence among men who have sex with men(MSM) is daunting(NHFPC,2014,2015).
Few effective interventions are available and/or widely utilized for MSM in China (Guo, Li, & Stanton,2011). Condoms can effectively prevent HIV transmission, but only 20% of MSM consistently use condoms during sexual activities(Guo et al.,2011; Zheng,2009). Pre-exposure prophylaxis(PrEP) can be used by uninfected MSM, but uninfected individuals often fail to adhere to PrEP antiretroviral drug regimens when they are neither ill nor perceive themselves to be at high risk (Ogbuagu et al.,2018). PrEP adherence may also be compromised by drug side effects or other barriers (e.g., cost, access, stigma)(Huang et al.,2014; Okwundu, Uthman, & Okoromah, 2012; Zhang, McMahon, et al.,2019). Voluntary medical male circumcision (VMMC) might serve as a biomedical tool to provide lifelong protection after a single surgical procedure for MSM, as has been demonstrated effective for heterosexual men (Vermund & Qian,2008).
Although evidence on the relationship between VMMC and HIV risk among MSM has been inconclusive, protective effects of VMMC have more often been observed among men who practiced insertive sex (Beyrer,2010; Wiysonge et al.,2011; Zhou et al.,2012). A study published in 2015 among MSM in Beijing suggested a remarkably strong protective effect among Chinese MSM who predominately practice insertive sex(adjusted odds ratio[aOR]=0.15; 95%confidence interval[CI]=0.04-0.65) (Qian et al.,2016). This study confirmed all circumcisions by physical examination and suggested a strong beneficial trend for MSM with versatile or receptive sexual positioning as well, providing the strongest evidence to date that VMMC might be a useful biomedical tool for HIV risk reduction among MSM. However, VMMC has been considered as a medical practice that specifically applied to men with phimosis and redundant prepuce in China for a long time. Neonatal circumcision is also rarely practiced in China, approximately 8% of boys aged 3-6 were circumcised (Ben et al.,2008). When considering medical or religious (e.g., Muslims) reasons, only about 2% of the population were circumcised, which is much fewer compared with Western countries (Ben et al.,2008; Lou, Wu, Chen, Ruan, & Shao,2009). On the other hand, with the increasingly scaling-up educational programs launched, many people have recognized its protective effects for HIV and other sexually transmitted diseases (STD). Therefore, circumcision may prove to be an overlooked and potentially feasible biomedical tool for HIV prevention among MSM.
To date, only one paper adopting a stochastic network-based model employing hypothetical sex-role preferences has been published which concluded that the roll-out of VMMC among MSM would be unlikely to reduce new HIV infection in Peru substantially (Goodreau et al.,2014). However, Goodreau et al. (2014) employed less optimistic assumptions using simulated data as to VMMC protective efficacy (e.g., odds ratio=0.8), not compatible with Chinese MSM populations (Qian et al.,2016). For instance, the Peru and China MSM epidemics are different in several epidemiological and social characteristics, limiting their model’s relevance for Chinese settings(Goodreau et al.,2012; Zhang, Penson, Qian, Webb, Lou, Shepherd, et al.,2019). Lou et al have assessed the impact of a few behavioral intervention approaches (e.g., condom use, partner reduction, HIV testing and ART) among Chinese MSM in Beijing using mathematical modeling strategies (Lou et al.,2014; Lou et al.,2009). However, it did not examine the putative impact of VMMC among MSM in China.
We sought to model the extent to which VMMC could alter the MSM epidemic in Beijing, China, employing a deterministic compartmental modeling strategy to project new HIV cases from 2016 to 2026 among MSM under different assumptions about the uptake rates of VMMC and the degree of protective efficacy of VMMC. We hypothesized that projected HIV incidence among MSM in Beijing would be reduced by greater coverage of VMMC. In the current study, we aimed to establish a more general mathematical model that can be generalizable to other settings with comparable social and cultural characteristics.
METHODS:
Study design
We used a deterministic compartmental model for simulating and projecting the HIV epidemic among MSM in Beijing. Deterministic compartmental models can specify transmission rates between compartments (e.g., susceptible, infectious) and they fit well large populations (Barnabas, 2016; Trottier & Philippe,2000 ). This model is usually used to describe and explain transmission patterns of certain infectious diseases at the population scale (Trottier & Philippe,2000 ). In the current study, we did not employ the sex-role-preference model as the sex position was too dynamic to capture (Goodreau et al.,2014; Lou et al.,2009; Wiysonge et al.,2011). Although some MSM in Beijing have female sexual partners, they were less likely to engage in risky sexual behaviors with their female partners(Lou et al.,2014; Lou et al.,2009). Therefore, we only considered the HIV infection as the result of homosexual contacts with male partners, and no other routes of transmission were considered (Fan et al.,2012; Lou et al.,2014). Model parameters (e.g., demographics, behavioral, and population-level) of the compartmental ordinary differential equation model were informed by key factors identified in published literature and available datasets.
To capture the randomness of transmission rates, we further simulated the transmission rates, repeated 50 times, using linear coefficients to capture all possible possibilities. We also assumed that the active age of sexual activities ranges from 18-65 years among MSM in Beijing (D.-I. Li, Liang, & Yang,2008; Lou et al.,2014).
Model structure:
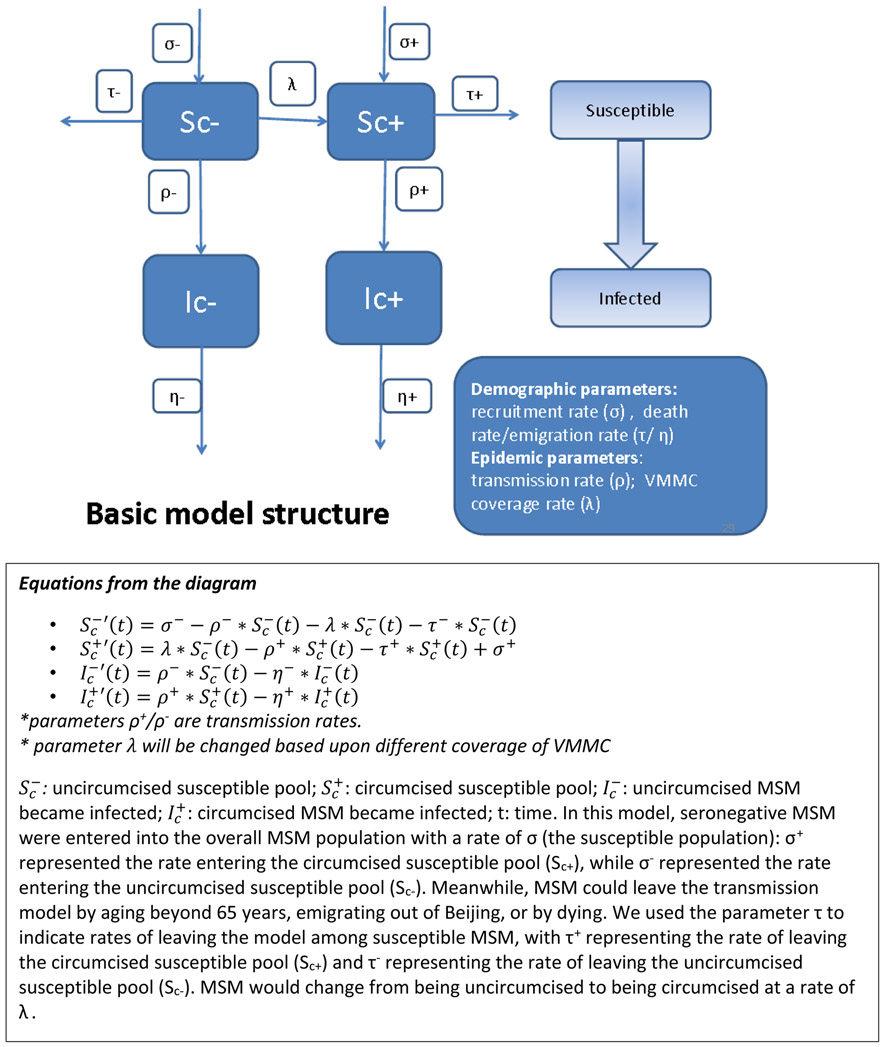
As being circumcised may change the risk of HIV transmission significantly among MSM (Goodreau et al., 2014; Goodreau et al., 2012; Qian et al., 2015), the study population was divided into two mutually exclusive subgroups:1) circumcised MSM(Sc+) and 2) uncircumcised MSM(Sc−) (Figure.1). Circumcised MSM became infected and entered the compartment of HIV-infected(Ic+) at an HIV transmission rate of ρ+, and uncircumcised MSM became infected(Ic−) at a transmission rate of ρ−. Both circumcised and uncircumcised MSM could leave the infectious pool at a rate of η+ (for circumcised) and η− (for uncircumcised) for the following reasons:1) progression to AIDS, 2) death due to HIV infection, 3) having undetectable viral loads due to either being an elite immunologic controller (a small group of HIV-infected patients who can maintain a high level of CD4+ cell counts without progressing immunologically towards AIDS over years in absence of ART)(Pantaleo et al.,1995) or adhering to an effective ART regime. When possible, parameters were estimated from the published literature or available unpublished data sources(Lou et al.,2014; Lou & Smith,2011; Lou et al.,2009); a few parameters (e.g., natural removal rate from each compartment) were calculated and calibrated within the model itself (Table.1).
Figure.1:
Schematic diagram for the HIV transmission model and voluntary medical male circumcision among men who have sex with men
Table 1:
Parameters for model building to assess HIV transmission model and the potential effect of male circumcision at varying levels of coverage among Chinese men who have sex with men
| Parameters | Description | Types | Sources |
|---|---|---|---|
| σ+ | Recruitment rate into circumcised per year | actual number /year | Lou et al., 2009, 2014 |
| σ− | Recruitment rate into uncircumcised per year | actual number/year | Lou et al., 2009, 2014 |
| τ+/τ− | Natural removal rate from susceptible circumcised MSM | Fraction | Lou et al., 2009, 2014 |
| Death rate per year | 0.01 | actual number/year | Lou et al., 2009, 2014 |
| emigration rate out of Beijing per year | 0.06 | actual number/year | Lou et al., 2009, 2014 |
| ρ+ | Transmission rate from susceptible to HIV positive among circumcised MSM-overall | Fraction | Surveillance data from China CDC; Zhang et al., under review |
| ρ− | Transmission rate from susceptible to HIV positive among uncircumcised MSM-overall | Fraction | Surveillance data from China CDC |
| Λ | Rate of circumcision among susceptible MSM per year | Fraction | Based upon different values given to λ |
| η+/η− | Rate of removal from the infected circumcised/uncircumcised MSM group | Fraction | Lou et al., 2009, 2014; model adjustment* |
| yearly mortality rate due to AIDS | Yearly death rate | yearly mortality rate | Lou et al., 2009, 2014; model adjustment* |
| undetectable rate after ART | Effective treatment that moves MSM out of the infectious pool | undetectable rate | Lou et al., 2009, 2014; expert opinion |
| undetectable rate due to elite immunological control | Inherent ability of the host immune system to reduce viral load | undetectable rate | OKulicz& Lambotte 2011 |
| emigration rate out of BJ | Demographic factors of mobility after HIV infection | emigration rate out of BJ | Lou et al., 2009, 2014; expert opinion |
| Scm | Susceptible uncircumcised MSM (C-minus) | Actual Number | Model predictions |
| Scp | Susceptible circumcised MSM (C-plus) | Actual Number | Model predictions |
| Ichp | Infected circumcised MSM (C-plus) | Actual Number | Model predictions |
| Ichm | Infected uncircumcised MSM (C-minus) | Actual Number | Model predictions |
Parameter was adjusted in order that the model could predict historical data
Model calibration
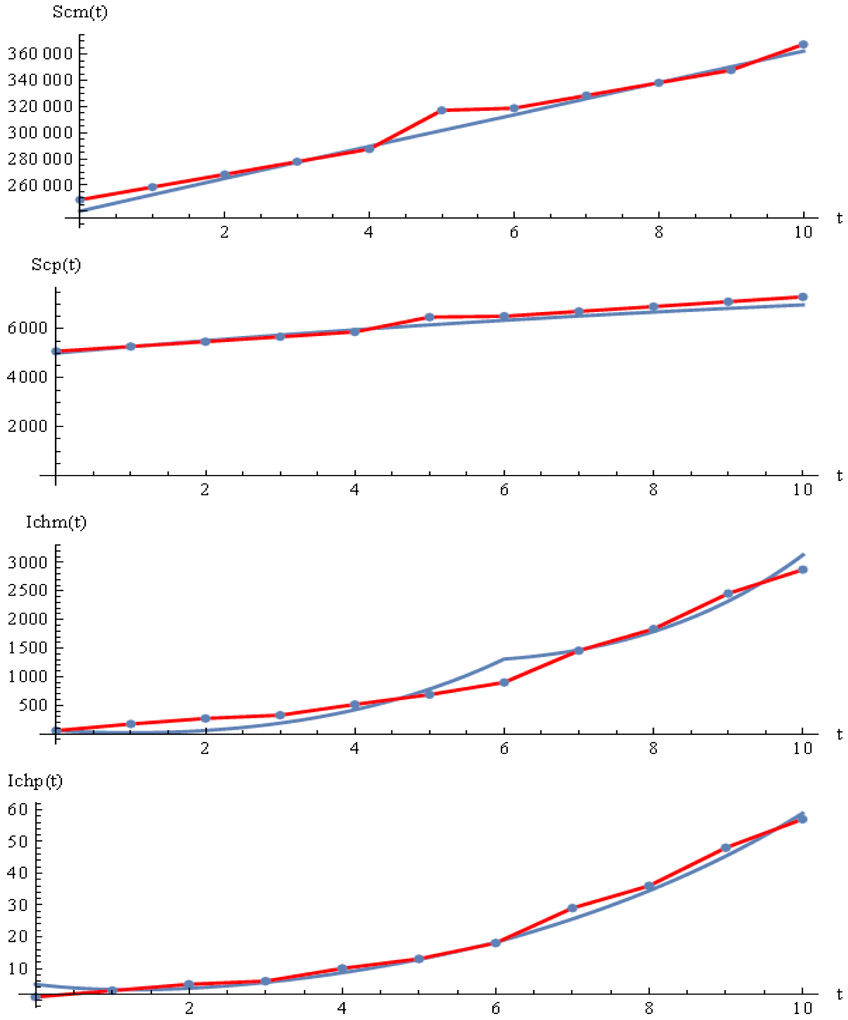
To refine the model to provide the most valid predictions, we used data to calibrate the model parameters to enable the model to predict historical surveillance data. At the initial stage, we used 2005-2015 surveillance data for HIV prevalence in Beijing to compare trends with those predicted by our model (Figure.2). In this model calibration process, parameters were adjusted until the prediction lines best overlapped with lines that reflected the historical surveillance data. When the prediction model overlapped with the surveillance data, using plausible and defensible parameter estimations, we considered the generated model to serve well for predictions forward in time.
Figure.2: Compare the model-predicted and historical trends (surveillance statistics) among four groups of men who have sex with men in China (2005-2015).
NOTE: Figure 2 compares 2005-2015 surveillance data of the number of new HIV cases in Beijing (red line) with the numbers predicted by our model (blue line); Scm: susceptible circumcised, Scp: susceptible uncircumcised, Ichp: infected circumcised, Ichm: infected uncircumcised; t: in years (from the year of 2005 to the year of 2015). In Figure 2, we presented the prediction model that we used for further calculations; the predicted and historical lines among four groups of MSM (susceptible circumcised [Scm], susceptible uncircumcised [Scp], infected circumcised [Ichp], and infected uncircumcised [Ichm]) overlapped well with each other. After this initial model calibration, we used the numbers generated by the model for 2015 (e.g., ρ−= 0.0099861, ρ+= 0.0093921, Scm=362,476, Scp=6,970, Ichp=59, and Ichm=3,129) as the baseline initial state to predict numbers of infected and susceptible MSM from 2016 to 2026 (see Appendix 1 for detailed formulas).
Data sources and estimation
Calculation of HIV incidence rates among both circumcised and uncircumcised MSM (2005-2015): To calculate incidence rates among circumcised and uncircumcised MSM for 2005-2015, we used a pooled adjusted odds ratio from a recently updated meta-analysis (Zhang, Qian, Liu, & Vermund, 2019) as well as the Beijing HIV surveillance data provided by China CDC. We calculated the HIV incidence from 2005-2015 among circumcised and uncircumcised MSM in Beijing (Table.2;Appendix.2).
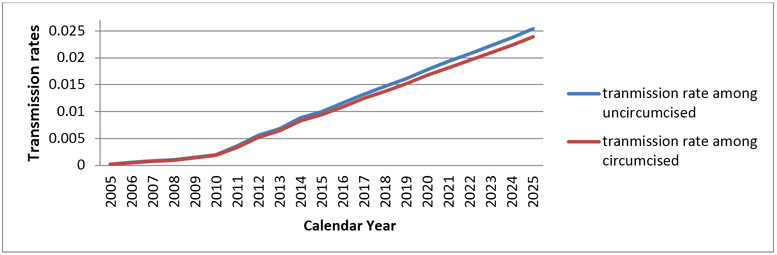
Simulation for incidence rates of HIV among both circumcised and uncircumcised MSM (2016-2025): To simulate HIV incidence from 2016 through 2025, we used existing incidence data among circumcised and uncircumcised MSM (2005-2015). We conducted a series of simulations for transmission rates of HIV among circumcised (ρ+) and among uncircumcised (ρ−) men (Figure.3;Table.3).
Prediction of new HIV cases: Using the calibrated model as well as the simulated data, we calculated new HIV cases among MSM for each prediction year (2016-2026) by varying the annual coverage rates of VMMC from 0.0001 to 0.15. We compared the new HIV cases for each hypothetical scenario with the new HIV cases at the baseline (λ=0.0001). The reduced proportion of HIV-infected men was defined as “the ‘total number of HIV cases in each hypothetical scenario minus the total number of cases at baseline’ divided by the ‘total cases at baseline’”. This was used as the indicator for each hypothetical coverage rate comparing with the baseline.
Sensitivity analyses: We conducted sensitivity analyses, by setting the transmission rates at the same level as the incidence rate seen in 2015, for both circumcised and uncircumcised MSM. If the transmission rate remains the same as of 2015, it represents a lower bound for the transmission rate (SFigure1). Besides, we calculated new HIV cases with a range of protective efficacies ranging from 0.07(95%CI=0.01-0.12) to 0.47(95%CI=−0.02-0.73), as suggested by the literature (Qian et al.,2016; Zhang, Qian, et al.,2019).
Table 2:
HIV Prevalence and incidence among circumcised and uncircumcised MSM in Beijing, China (2005-2015)
| Year | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uncircumcised MSM | Incidence | 0.00019 | 0.00054 | 0.00084 | 0.00099 | 0.00152 | 0.00197 | 0.00361 | 0.00563 | 0.00684 | 0.00883 | 0.00999 |
| Prevalence | 0.00306 | 0.00868 | 0.0135 | 0.01588 | 0.02432 | 0.0315 | 0.05784 | 0.09009 | 0.10939 | 0.14134 | 0.15978 | |
| Circumcised MSM | Incidence | 0.00018 | 0.0005 | 0.00079 | 0.00092 | 0.00142 | 0.00184 | 0.00338 | 0.00527 | 0.00641 | 0.0083 | 0.00939 |
| Prevalence | 0.00294 | 0.00833 | 0.01297 | 0.01525 | 0.02337 | 0.03028 | 0.05565 | 0.0868 | 0.10548 | 0.13646 | 0.15437 |
Figure.3:
HIV transmission rates among circumcised (circ+) and uncircumcised (circ−) men who have sex with men in China
Table 3:
Predicted HIV transmission rates among circumcised and uncircumcised men who have sex with men in China (2016-2025)
| Year | Transmission rate for circ− (uncircumcised MSM) |
Transmission rate for circ+ (circumcised MSM) |
|
|---|---|---|---|
| Predicted transmission rates for 2016-2025 | 2016 | 0.0116(0.0095,0.0137) | 0.0109(0.0090,0.0129) |
| 2017 | 0.0133(0.0111,0.0155) | 0.0125(0.0104,0.0145) | |
| 2018 | 0.0147(0.0124,0.0170) | 0.0138(0.0117,0.0160) | |
| 2019 | 0.0161(0.0135,0.0187) | 0.0152(0.0127,0.0176) | |
| 2020 | 0.0178(0.0151,0.0206) | 0.0168(0.0142,0.0194) | |
| 2021 | 0.0193(0.0166,0.0221) | 0.0182(0.0156,0.0208) | |
| 2022 | 0.0207(0.0179,0.0236) | 0.0195(0.0168,0.0222) | |
| 2023 | 0.0223(0.0194,0.0251) | 0.0209(0.0182,0.0237) | |
| 2024 | 0.0237(0.0207,0.0268) | 0.0223(0.0194,0.0252) | |
| 2025 | 0.0254(0.0221,0.0287) | 0.0239(0.0208,0.0270) |
RESULTS
New HIV cases at each different VMMC coverage rate
Compared with the baseline (λ=0.0001), we found the new HIV cases were reduced proportionally with increasing coverage rates of the VMMC among MSM. Higher coverage rates are associated with lower numbers of new HIV cases and result in a more substantial impact on the new cases by the end of 2026. The number of newly infected cases decreases by 0.03%, 0.09%, 0.46%, 0.92%, 4.18%, 7.44%, and 10.02% compared to the baseline (λ=0.0001) if we increase the annual coverage rate of VMMC to 0.0005, 0.001, 0.005, 0.01, 0.05, 0.1 and 0.15, respectively (Table.4).
Table 4.
The number of newly infected HIV cases among men who have sex with men in China with different coverage rates of voluntary medical male circumcision (2016-2026)
| λ1=0.0001 | λ1=0.0005 | λ1=0.001 | λ1=0.005 | λ1=0.01 | λ1=0.05 | λ1=0.1 | λ1=0.15 | |
|---|---|---|---|---|---|---|---|---|
| 2016 | 6344 (6344,6344) |
6344 (6344,6344) |
6344 (6344,6344) |
6343 (6343,6343) |
6343 (6343,6343) |
6337 (6337,6337) |
6330 (6330,6330) |
6324 (6324,6324) |
| 2017 | 9816 (9069,10561) |
9816 (9069,10561) |
9815 (9068,10560) |
9812 (9065,10557) |
9809 (9062,10553) |
9779 (9037,10519) |
9744 (9008,10479) |
9711 (8980,10442) |
| 2018 | 13581 (12129,15026) |
13580 (12128,15025) |
13580 (12127,15024) |
13570 (12119,15014) |
13560 (12111,15001) |
13476 (12040,14906) |
13380 (11959,14795) |
13292 (11884,14694) |
| 2019 | 17547 (15431,19648) |
17546 (15429,19646) |
17543 (15427,19643) |
17524 (15412,19622) |
17501 (15391,19595) |
17322 (15240,19391) |
17122 (15069,19162) |
16943 (14917,18957) |
| 2020 | 21688 (18852,24497) |
21685 (18848,24493) |
21679 (18845,24488) |
21644 (18816,24448) |
21603 (18778,24398) |
21279 (18503,24028) |
20923 (18201,23620) |
20614 (17939,23266) |
| 2021 | 26104 (22587,29578) |
26099 (22580,29572) |
26090 (22575,29563) |
26031 (22524,29496) |
25961 (22462,29413) |
25427 (22006,28805) |
24853 (21516,28151) |
24368 (21101,27596) |
| 2022 | 30694 (26584,34742) |
30687 (26574,34731) |
30673 (26566,34718) |
30582 (26486,34615) |
30472 (26390,34489) |
29656 (25685,33565) |
28800 (24947,32597) |
28094 (24337,31796) |
| 2023 | 35397 (30743,39966) |
35386 (30728,39951) |
35366 (30716,39932) |
35233 (30600,39783) |
35073 (30458,39600) |
33897 (29434,38280) |
32696 (28387,36928) |
31726 (27543,35836) |
| 2024 | 40242 (35097,45276) |
40225 (35078,45255) |
40199 (35059,45229) |
40013 (34896,45021) |
39788 (34696,44768) |
38170 (33273,42963) |
36553 (31852,41156) |
35279 (30734,39731) |
| 2025 | 45190 (39562,50676) |
45167 (39537,50648) |
45132 (39510,50613) |
44881 (39289,50335) |
44577 (39019,49997) |
42431 (37118,47612) |
40331 (35263,45279) |
38716 (33837,43483) |
| 2026 | 50301 (44182,56243) |
50270 (44150,56206) |
50224 (44115,56160) |
49897 (43823,55798) |
49499 (43468,55357) |
46724 (41001,52288) |
44074 (38648,49355) |
42081 (36881,47147) |
| Reduction in proportion HIV-infected with increasing circumcision coverage (%) | Baseline | 0.03 (0.038,0.044) |
0.087 (0.085,0.087) |
0.46 (0.459,0.463) |
0.92 (0.915,0.922) |
4.18 (4.169,4.185) |
7.44 (7.429,7.445) |
10.02 (10.009,26.312) |
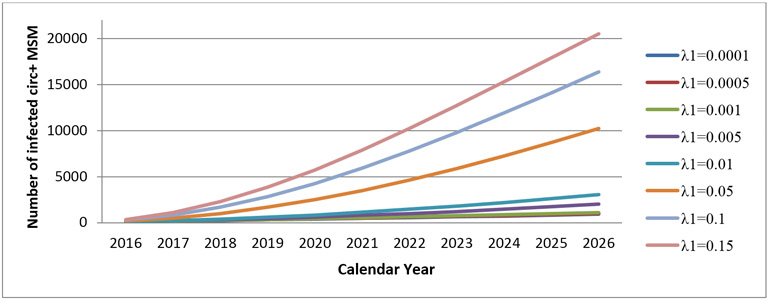
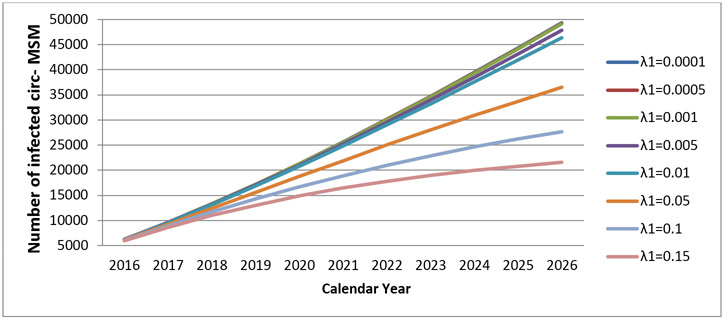
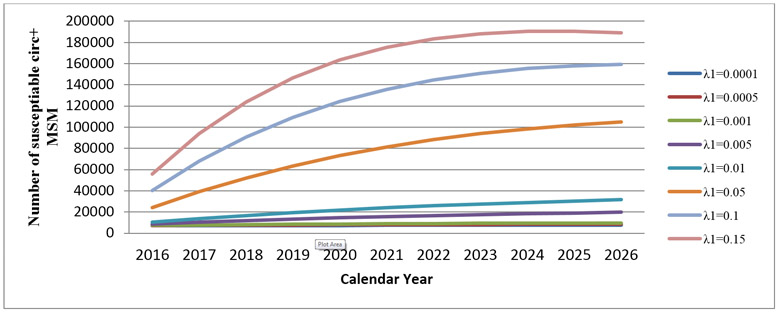
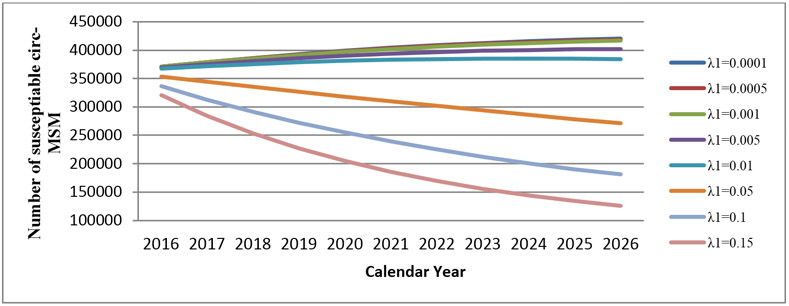
With the increased coverage rates of VMMC, the mean number of infected circumcised MSM increases (Figure.4a), while the mean number of infected uncircumcised MSM decreases over the same period (Figure.4b). With the increased coverage rates of VMMC, the mean number of susceptible circumcised MSM increases each year, given the larger pool of circumcised men (Figure.5a), while the mean number of susceptible uncircumcised MSM decreases over the same period (Figure.5b).
Figure.4a:
Cumulative number of infected circumcised men who have sex with men in Beijing by years (2016-2026)
Figure.4b:
Cumulative number of infected uncircumcised men who have sex with men in Beijing by years (2016-2026)
Figure.5a:
Cumulative number of susceptible circumcised men who have sex with men in Beijing (2016-2026)
Figure.5b:
Cumulative number of susceptible uncircumcised men who have sex with men in Beijing (2016-2026)
Prevalence of VMMC among MSM
We also examined the prevalence of VMMC among all MSM in Beijing. With a higher coverage rate, the prevalence of VMMC naturally increased correspondingly. By the year 2026, the prevalence increased from 1.75% when the baseline coverage rate was 0.0001, to 58.8% when the VMMC coverage rate increased to 0.15 per annum (Table.5).
Table 5.
Prevalence of voluntary medical male circumcision among all men who have sex with men in Beijing by years (2016-2026) (%)
| Coverage rates↓/year→ |
2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | 2025 | 2026 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| λ1=0.0001 | 1.87 | 1.85 | 1.83 | 1.82 | 1.80 | 1.79 | 1.78 | 1.77 | 1.76 | 1.75 | 1.74 |
| λ1=0.0005 | 1.90 | 1.92 | 1.93 | 1.94 | 1.95 | 1.95 | 1.96 | 1.97 | 1.97 | 1.98 | 1.98 |
| λ1=0.001 | 1.95 | 2.00 | 2.05 | 2.09 | 2.13 | 2.16 | 2.19 | 2.21 | 2.23 | 2.26 | 2.27 |
| λ1=0.005 | 2.31 | 2.69 | 3.02 | 3.30 | 3.56 | 3.79 | 3.99 | 4.17 | 4.33 | 4.47 | 4.60 |
| λ1=0.01 | 2.77 | 3.54 | 4.21 | 4.80 | 5.32 | 5.78 | 6.19 | 6.56 | 6.88 | 7.17 | 7.43 |
| λ1=0.05 | 6.32 | 10.06 | 13.25 | 15.98 | 18.33 | 20.37 | 22.14 | 23.68 | 25.03 | 26.20 | 27.23 |
| λ1=0.1 | 10.58 | 17.61 | 23.36 | 28.13 | 32.10 | 35.44 | 38.24 | 40.61 | 42.61 | 44.30 | 45.72 |
| λ1=0.15 | 14.64 | 24.52 | 32.29 | 38.49 | 43.49 | 47.53 | 50.81 | 53.47 | 55.63 | 57.37 | 58.76 |
Results of the sensitivity analyses
We found the patterns of HIV-infected and susceptible MSM by circumcision status as well as the proportion of circumcised men were similar when the transmission rates were set at the same incidence rate seen in 2015 (STable.1;SFigure.2a-d). We also assessed the HIV incidence using different protective efficacies ranging from being very conservative 7% to being optimistic 47%. The transmission rate of HIV was reduced among circumcised MSM with higher circumcision coverage rates (SFigure.3). The higher coverage rate, the fewer HIV cases would be observed in the projected years(STable.2).
Discussion
Our model predicts the magnitude of the impact of VMMC on HIV acquisition over 11 years by estimating the reduction in the proportion of HIV-infected cases (Kripke et al.,2016). By changing the coverage rates of VMMC from the very low baseline coverage (λ=0.0001) to a hypothetical scenario of an active VMMC program (λ=0.15), our model suggested a worthwhile potential public health impact of VMMC for MSM in China, depending on coverage assumptions, given an assumed efficacy of 7%. The reduction in the proportion of HIV-infected cases ranged from 0.06% when the VMMC coverage rate was low at 0.0001(corresponding to the prevalence of VMMC as 1.7%) to 16.3% when the VMMC coverage rate increased to 0.15 (corresponding to the VMMC prevalence of 58.8%) by the year of 2026. Meanwhile, we observed a big jump in the reduction in the proportion of the number of HIV cases (from 0.92% to 4.18%) when the VMMC coverage rate increased from 0.01 to 0.05. The big jump may indicate that a slight increase in the VMMC coverage rate may result in a significant reduction in new HIV cases among MSM in China, even when we use very conservative estimates of the efficacy of VMMC in protecting MSM.
Compared with modeling estimates using data from Peru and from more resource-rich settings (Anderson et al., 2009; Goodreau et al.,2014; Njeuhmeli et al.,2011), our model suggests a more optimistic efficacy of VMMC among MSM, even when using a low protective efficacy estimate (7%) for VMMC. In the MSM study in Peru, the authors observed fewer than 5-10% of HIV cases would have been averted if the VMMC coverage rate were to grow to 50% in the coming years (Goodreau et al.,2014). Two other studies posited that only if a 100% coverage rate of VMMC were achieved would such an incidence reduction be observed (Anderson et al.,2009; Londish, Templeton, Regan, Kaldor, & Murray,2010). The proportion of MSM who have a comparatively lower-risk profile, the low baseline VMMC prevalence, and the relatively recent expansion of the HIV epidemic among MSM in China may suggest, in part, why our model is more optimistic about the VMMC role for MSM in China (Lou et al.,2014; Vermund & Qian,2008; Zhang, Penson, Qian, Webb, Lou, Shephard, et al.,2019). VMMC offers lifelong protective benefits, and it might be embraced by the MSM community if advocated for by public health and community-based representatives (Grund et al.,2018).
The strengths of the current study include our employment of a deterministic compartmental model for predictions. The deterministic model has advantages compared to stochastic models for predicting the incidence of chronic infectious diseases such as HIV/AIDS (Lou et al.,2014). Although the output of a deterministic model was fully determined by values of included parameters and initial conditions, the simulation procedure for transmission rates can capture randomness properties better than can stochastic models (Vynnycky & White,2010). Additionally, we used sensitivity analyses to estimate new HIV cases at their lower bound when transmission rates remained the same as seen in 2015 as well as at different protective efficacies (7-47%), suggesting our findings to be robust and plausible. Our model may apply, too, to other settings with similar epidemic characteristics. The second strength of our study is that, unlike other modeling studies using hypothetical/simulated data (Goodreau et al.,2014), we used validated data sources to calculate parameters while adjusting initial conditions for the model (Lou et al.,2014). The simulation procedure used parameters estimated from HIV surveillance data in Beijing, improving the validity of the model and likely accuracy of context-specific predictions. Third, during the model building procedure, we gradually raised the hypothetical VMMC coverage rates from a baseline λ=0.0001 up to an annual λ=0.15. This procedure captures the gradual changes as the result of the increased VMMC coverage rate, providing a range of estimates and practical guidance for health professionals for future interventions of VMMC among MSM in China (Pan et al.,2018).
The major limitation of our prediction model is a simplification of the real epidemic in Beijing in our effort to balance parsimony and reality. For instance, unlike existing studies considering sexual role preferences (Goodreau et al.,2014; Lou et al.,2014), we did not stratify Chinese MSM by their sex role positioning due to the lack of population-based information. However, as our prediction model was built upon average transmission rates regardless of sexual positioning, it may capture average transmission patterns among MSM as a whole in Beijing. We did not incorporate other risk factors (e.g., types of partners, multiple partnerships, and condom use) in the model. With more availability of the epidemic information among this population, a more sophisticated model can emerge to assess the impact of VMMC on curbing HIV among Chinese MSM. Furthermore, indirect effects due to herd immunity (a form of indirect protection for susceptible people from an infectious disease when a relatively large proportion of a population has become immune to the given infection) (Fine, Eames, & Heymann,2011) of the VMMC may impact the HIV transmission among MSM in a long run, although a study has revealed minimum indirect effects of VMMC against HIV among heterosexual men (Boily, Desai, Masse, & Gumel,2008). In addition, we used the consecutive 11-year incidence rate data directly obtained from the China CDC, which was lower than published but sparse data (e.g., the HIV incidence rate estimates for 2009 was 40 times lower than the estimates from Li et al. 2012’s study(Li et al.,2012)). The discrepancy may be due to different sampling schemes and/or recruitment venues and strategies. Although the estimation may be affected using different data sources, our model is in the initial stage of modeling the epidemic effect of VMMC to date. Furthermore, the death and emigration rates may only consider MSM with formal Beijing residency status (Hukou) in the prediction, which may underestimate the numbers of susceptible MSM and comprise the precision of the estimation. Lastly, we only modeled MSM aged 18-65 years old, although studies have indicated that risk profiles have expanded the upper bound of the age range (Zhang et al.,2014). However, as we have limited data sources concerning VMMC among MSM who are older than 65 or younger than 18 years old, we call for future studies to examine how VMMC works among MSM beyond the age range of 18-65 years.
In conclusion, our model estimates the potential benefit of VMMC among MSM in China, using low to moderate estimates of the efficacy of VMMC for HIV prevention. VMMC may serve as a new tool to reduce HIV incidence among MSM in China. Although the optimal scenario of higher VMMC coverage rates can bolster HIV incidence reduction among MSM, the lack of an efficacy trial as well as pre-existing structural barriers in this population limits our ability to confidently assert the impact of VMMC on HIV, since protective efficacy of VMMC may vary greatly by epidemic context and relative frequency of predominantly insertive vs. receptive men. Without such efficacy data, promoting widespread VMMC in MSM is impractical (Sullivan et al.,2014).
Supplementary Material
Acknowledgments
Source of Support
This study was supported by grants from the U.S. National Institutes of Health (R01AI094562 and R34AI091446), and the Natural Science Foundation of China (No. 11771277). The content is solely the responsibility of the authors and does not necessarily represent the sponsor who had no role in the design or conduct of the study, the writing of this report, or its submission for publication.
References:
- Anderson J, Wilson D, Templeton DJ, Grulich A, Carter R, & Kaldor J (2009). Cost-effectiveness of adult circumcision in a resource-rich setting for HIV prevention among men who have sex with men. J Infect Dis, 200(12), 1803–1812. doi: 10.1086/648472 [DOI] [PubMed] [Google Scholar]
- Barnabas R (2016). Deterministic Compartmental Models: Application: Modeling the Potential Benefit of HPV Vaccines. In. [Google Scholar]
- Ben KL, Xu JC, Lu L, Yao JP, Min XD, Li WY, . . . Cao XM (2008). [Promoting male circumcision in China for preventing HIV infection and improving reproductive health]. Zhonghua Nan Ke Xue, 14(4), 291–297. [PubMed] [Google Scholar]
- Beyrer C (2010). Global prevention of HIV infection for neglected populations: men who have sex with men. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 50 Suppl 3, S108–113. doi: 10.1086/651481 [DOI] [PubMed] [Google Scholar]
- Boily MC, Desai K, Masse B, & Gumel A (2008). Incremental role of male circumcision on a generalised HIV epidemic through its protective effect against other sexually transmitted infections: from efficacy to effectiveness to population-level impact. Sex Transm Infect, 84 Suppl 2, ii28–34. doi: 10.1136/sti.2008.030346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ChinaDaily. (2015). China has 575,000 people with HIV/AIDS. Retrieved from http://www.chinadaily.com.cn/china/2015-12/01/content_22595361.htm
- Fan S, Lu H, Ma X, Sun Y, He X, Li C, . . . Ruan Y (2012). Behavioral and serologic survey of men who have sex with men in Beijing, China: implication for HIV intervention. AIDS Patient Care STDS, 26(3), 148–155. doi: 10.1089/apc.2011.0277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine P, Eames K, & Heymann DL (2011). “Herd immunity”: a rough guide. Clin Infect Dis, 52(7), 911–916. doi: 10.1093/cid/cir007 [DOI] [PubMed] [Google Scholar]
- Goodreau SM, Carnegie NB, Vittinghoff E, Lama JR, Fuchs JD, Sanchez J, & Buchbinder SP (2014). Can male circumcision have an impact on the HIV epidemic in men who have sex with men? PLoS One, 9(7), e102960. doi: 10.1371/journal.pone.0102960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodreau SM, Carnegie NB, Vittinghoff E, Lama JR, Sanchez J, Grinsztejn B, . . . Buchbinder SP (2012). What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One, 7(11), e50522. doi: 10.1371/journal.pone.0050522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grund JM, Chetty-Makkan CM, Ginindza S, Munyai R, Kisbey-Green H, Maraisane M, & Charalambous S (2018). Effectiveness of an “Exclusive Intervention Strategy” to increase medical male circumcision uptake among men aged 25-49 years in South Africa. BMC Public Health, 18(1), 868. doi: 10.1186/s12889-018-5729-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Li X, & Stanton B (2011). HIV-related behavioral studies of men who have sex with men in China: a systematic review and recommendations for future research. AIDS Behav, 15(3), 521–534. doi: 10.1007/s10461-010-9808-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W, Du S, Xu J, Zhou J, Liang S, Yu F, . . . Salazar LF (2014). Acceptability of Condoms, Circumcision and PrEP among Young Black Men Who Have Sex with Men: A Descriptive Study Based on Effectiveness and Cost. Biomed Res Int, 2(1), 129–137. doi: 10.1155/2014/49898710.3390/vaccines2010129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke K, Opuni M, Schnure M, Sgaier S, Castor D, Reed J, & Njeuhmeli E (2016). Age Targeting of Voluntary Medical Male Circumcision Programs Using the Decision Makers' Program Planning Toolkit (DMPPT) 2.0. 11(7), e0156909. doi: 10.1371/journal.pone.0156909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D-I, Liang H-Y, & Yang Y (2008). A Survey of Initial and Factors of Homosexual Intercourse Among Men Who Have Sex With Men. Journal of Preventive Medicine Information, 6, 008. [Google Scholar]
- Li D, Li S, Liu Y, Gao Y, Yu M, Yang X, . . . Shao Y (2012). HIV incidence among men who have sex with men in Beijing: a prospective cohort study. BMJ Open, 2(6). doi: 10.1136/bmjopen-2012-001829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Londish GJ, Templeton DJ, Regan DG, Kaldor JM, & Murray JM (2010). Minimal impact of circumcision on HIV acquisition in men who have sex with men. Sex Health, 7(4), 463–470. doi: 10.1071/sh09080 [DOI] [PubMed] [Google Scholar]
- Lou J, Blevins M, Ruan Y, Vermund SH, Tang S, Webb GF, . . . Qian HZ (2014). Modeling the impact on HIV incidence of combination prevention strategies among men who have sex with men in Beijing, China. PLoS One, 9(3), e90985. doi: 10.1371/journal.pone.0090985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou J, & Smith RJ (2011). Modelling the effects of adherence to the HIV fusion inhibitor enfuvirtide. J Theor Biol, 268(1), 1–13. doi: 10.1016/j.jtbi.2010.09.039 [DOI] [PubMed] [Google Scholar]
- Lou J, Wu J, Chen L, Ruan Y, & Shao Y (2009). A sex-role-preference model for HIV transmission among men who have sex with men in China. BMC Public Health, 9 Suppl 1, S10. doi: 10.1186/1471-2458-9-s1-s10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHFPC. (2014). 2014 China AIDS Response Progress Report. Retrieved from http://www.unaids.org/sites/default/files/documents/CHN_narrative_report_2014.pdf
- NHFPC. (2015). 2015 China AIDS Response Progress Report.
- Njeuhmeli E, Forsythe S, Reed J, Opuni M, Bollinger L, Heard N, . . . Hankins C (2011). Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS One, 8(11). doi: 10.1371/journal.pone.0153363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogbuagu O, Marshall BDL, Tiberio P, Ogunbajo A, Barakat L, Montgomery M, . . . Chan PA (2018). Prevalence and Correlates of Unhealthy Alcohol and Drug Use Among Men Who Have Sex with Men Prescribed HIV Pre-exposure Prophylaxis in Real-World Clinical Settings. AIDS Behav. doi: 10.1007/s10461-018-2260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okwundu CI, Uthman OA, & Okoromah CA (2012). Antiretroviral pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. Cochrane Database Syst Rev, 7, CD007189. doi: 10.1002/14651858.CD007189.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan SW, Carpiano RM, Li D, Zhang Z, Schechter MT, Spittal PM, & Ruan Y (2018). Ethnicity and HIV vulnerabilities among men who have sex with men in China. AIDS Care, 30(8), 1025–1030. doi: 10.1080/09540121.2018.1428727 [DOI] [PubMed] [Google Scholar]
- Pantaleo G, Menzo S, Vaccarezza M, Graziosi C, Cohen OJ, Demarest JF, . . . et al. (1995). Studies in subjects with long-term nonprogressive human immunodeficiency virus infection. N Engl J Med, 332(4), 209–216. doi: 10.1056/nejm199501263320402 [DOI] [PubMed] [Google Scholar]
- Qian HZ, Ruan Y, Liu Y, Milam DF, HM LS, Yin L, . . . Vermund SH (2015). Lower HIV risk among circumcised men who have sex with men in China: Interaction with anal sex role in a cross-sectional study. J Acquir Immune Defic Syndr. doi: 10.1097/qai.0000000000000856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian HZ, Ruan Y, Liu Y, Milam DF, Spiegel HM, Yin L, . . . Vermund SH (2016). Lower HIV Risk Among Circumcised Men Who Have Sex With Men in China: Interaction With Anal Sex Role in a Cross-Sectional Study. J Acquir Immune Defic Syndr, 71(4), 444–451. doi: 10.1097/qai.0000000000000856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, . . . Shau WY (2014). Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health, 17(1), 5–14. doi: 10.1016/j.jval.2013.08.2291 [DOI] [PubMed] [Google Scholar]
- Trottier H, & Philippe P (2000. ). Deterministic Modeling Of Infectious Diseases: Theory And Methods. The Internet Journal of Infectious Diseases, 1(2). [Google Scholar]
- Vermund SH, & Qian HZ (2008). Circumcision and HIV prevention among men who have sex with men: no final word. Jama, 300(14), 1698–1700. doi: 10.1001/jama.300.14.1698 [DOI] [PubMed] [Google Scholar]
- Vynnycky E, & White RG (2010). An introductory book on infectious disease modelling and its applications. New York: Oxford University Press. [Google Scholar]
- Wiysonge CS, Kongnyuy EJ, Shey M, Muula AS, Navti OB, Akl EA, & Lo YR (2011). Male circumcision for prevention of homosexual acquisition of HIV in men. Cochrane Database Syst Rev(6), Cd007496. doi: 10.1002/14651858.CD007496.pub2 [DOI] [PubMed] [Google Scholar]
- Zhang C, Li X, Su S, Zhang L, Zhou Y, Shen Z, & Tang Z (2014). Prevalence of HIV, syphilis, and HCV infection and associated risk factors among male clients of low-paying female sex workers in a rural county of Guangxi, China: a cross-sectional study. Sex Transm Infect, 90(3), 230–236. doi: 10.1136/sextrans-2013-051275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, McMahon J, Simmons J, Brown LL, Nash R, & Liu Y (2019). Suboptimal HIV Pre-exposure Prophylaxis Awareness and Willingness to Use Among Women Who Use Drugs in the United States: A Systematic Review and Meta-analysis. AIDS Behav. doi: 10.1007/s10461-019-02573-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Penson DF, Qian HZ, Webb GF, Lou J, Shephard BE, . . . Vermund SH (2019). Modeling economic and epidemiological impact of voluntary medical male circumcision among men who have sex with men in Beijing, China. Int J STD AIDS, 956462419831859. doi: 10.1177/0956462419831859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Penson DF, Qian HZ, Webb GF, Lou J, Shepherd BE, . . . Vermund SH (2019). Modeling economic and epidemiological impact of voluntary medical male circumcision among men who have sex with men in Beijing, China. Int J STD AIDS, 30(7), 630–638. doi: 10.1177/0956462419831859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C, Qian HZ, Liu Y, & Vermund SH (2019). Voluntary medical male circumcision and HIV infection among men who have sex with men: Implications from a systematic review. Sage Open Medicine, 7, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng T (2009). Red Lights: The Lives of Sex Workers in Postsocialist China. Minneapolis: Universityof Minnesota Press. [Google Scholar]
- Zhou C, Raymond HF, Ding X, Lu R, Xu J, Wu G, . . . Shao Y (2012). Anal Sex Role, Circumcision Status, and HIV Infection Among Men Who Have Sex with Men in Chongqing, China. Archives of sexual behavior. doi: 10.1007/s10508-012-0008-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.