Abstract
Non-alcoholic fatty liver disease (NAFLD) has emerged as one of the main causes of chronic liver disease worldwide. NAFLD comprises a group of conditions characterized by the accumulation of hepatic lipids that can eventually lead to non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and hepatocellular carcinoma (HCC), the fifth most common cancer type with a poor survival rate. In this context, several works have pointed out perturbations in lipid metabolism and, particularly, changes in bioactive sphingolipids, as a hallmark of NAFLD and derived HCC. In the present work, we have reviewed existing literature about sphingolipids and the development of NAFLD and NAFLD-derived HCC. During metabolic syndrome, considered a risk factor for steatosis development, an increase in ceramide and sphigosine-1-phosphate (S1P) have been reported. Likewise, other reports have highlighted that increased sphingomyelin and ceramide content is observed during steatosis and NASH. Ceramide also plays a role in liver fibrosis and cirrhosis, acting synergistically with S1P. Finally, during HCC, metabolic fluxes are redirected to reduce cellular ceramide levels whilst increasing S1P to support tumor growth.
Keywords: Metabolic syndrome, NAFLD, NASH, cirrhosis, HCC, sphingolipids, ceramide, S1P, sphingomyelin, metabolomics, lipidomics
1. Non-Alcoholic Fatty Liver Disease and Derived Hepatocellular Carcinoma
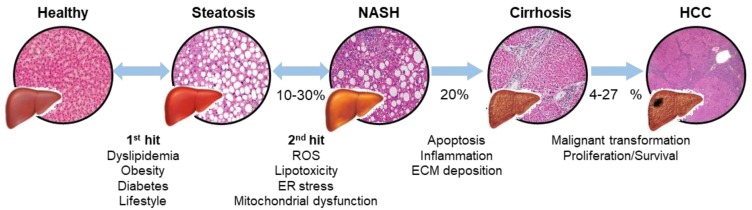
NAFLD is a term that encompasses a group of pathologies ranging steatosis, non-alcoholic steatohepatitis (NASH) and cirrhosis (Figure 1). This condition is particularly manifested in Western countries, with an incidence rate of about 20%–30% in the general population [1,2]. The most accepted explanation for NAFLD progression is the two-hit hypothesis [3], where an initial first hit induces lipid accumulation in the liver and increases liver vulnerability to different factors (second hits). As Sanyal notably reviewed, such second hits consist on an increased endoplasmic reticulum (ER) and oxidative stress, followed by a decreased antioxidant capacity that creates a pro-inflammatory environment and contributes to mitochondrial dysfunction [4].
Figure 1.
Liver disease progression: from steatosis to hepatocellular carcinoma. Schematic representation of the two-hit hypothesis and the progression of the disease, with characteristic H&E staining micrographs from each state of the pathology. A first hit leads an increased lipid accumulation in the liver, named steatosis. In a second hit reactive oxygen species (ROS), lipotoxicity, endoplasmic reticulum (ER) stress and mitochondrial dysfunction lead to non-alcoholic steatohepatitis (NASH) in 10%–30% patients. Sustained damage results in apoptosis, inflammation and extracellular matrix (ECM) deposition, leading to a fibrotic response and cirrhosis in 20% of patients. Finally, the 4%–27% of chronic patients can develop hepatocellular carcinoma (HCC).
On the other hand, lipotoxicity has also been pointed out as a second hit during NAFLD progression [5]. In this context, several works point out the convergence between metabolic pathways from triglycerides and sphingolipids. Indeed, steatosis has been correlated with an increased sphingolipid content, suggesting that lipid imbalance generates bioactive lipids that might act together with other second hits during NAFLD progression [6,7,8]. Steatosis progresses into NASH in 10%–30% cases with subsequent inflammation, hepatocyte death and fibrosis development [9]. Around 20% of NASH patients are estimated to develop cirrhosis if fibrosis development persists [10,11]. Although sometimes a compensated cirrhosis without symptoms can occur, it is often followed by complications leading to liver dysfunction [12].
Furthermore, cirrhosis can also evolve to hepatocellular carcinoma (HCC) with poorer survival rates [13]. HCC is the most prevalent form of presentation (70%–85%) of liver cancer, which is the fifth most common cancer type in the world and the second cause of cancer-related death [14,15]. Around 4%–27% of NAFLD patients are estimated to develop HCC development [16,17], and NAFLD is positioning as one of most leading causes of HCC and the most increasing one [18]. Improvement in understanding and diagnosing, particularly in NAFLD-derived HCC, is mandatory for finding suitable therapies and diagnosing methods against the disease.
2. Sphingolipid Metabolism: Ceramide as Central Molecule
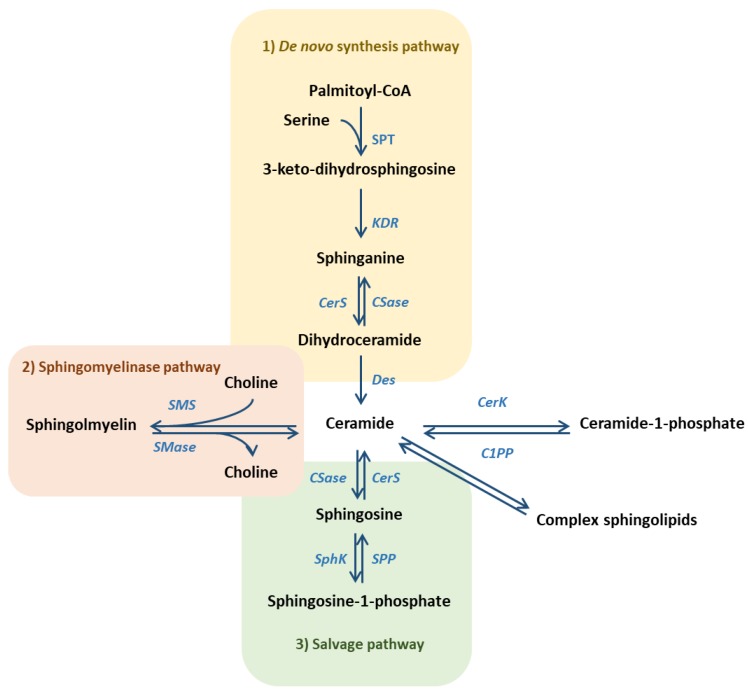
Sphingolipids are bioactive molecules that play a role in several cell functions and participate in tissue homeostasis [19,20,21]. Ceramide is considered as the central molecule in sphingolipid metabolism and it has been reported to play a pro-apoptotic and anti-proliferative role, regulating tissue homeostasis [22,23]. On one hand, ceramide can be synthetized from three different pathways (Figure 2): i) In the de novo pathway, by condensation of serine and palmitate, ii) through sphingomyelin (SM) catabolism in the sphingomyelinase (SMase) pathway, and iii) through the catabolism of complex sphingolipids in the salvage or catabolic pathway. The relationship between ceramide production and inflammation has been highly described by various authors [24,25]. Conversely, ceramide content can be reduced by its conversion into SM or complex glycosphingolipids (GSL), a common mechanism from cancer cells to block ceramide-induced cell death signaling [26]. Otherwise, ceramide can be directly phosphorylated into ceramide-1-phosphate (C1P), which mediates in many inflammatory processes through a specific membrane receptor [27,28,29].
Figure 2.
Ceramide is the central molecule in sphingolipid metabolism and can be synthesized by three different pathways: de novo synthesis pathway, sphingomyelinase pathway and salvage pathway. (SPT = serine palmitoyltransferase; KDR = 3-keto-dihydrosphingosine reductase; CerS = ceramide synthase; CSase = ceramidase; Des = desaturase; SphK = sphingosine kinase; SPP = S1P phosphatase; SMase = sphingomyelinase; SMS = sphingomyelin synthase; CerK = ceramide kinase; C1PP = ceramide-1-phosphate phosphatase).
Ceramidase catabolizes ceramide into sphingosine, which can be further phosphorylated into sphingosine-1-phosphate (S1P) (Figure 2), described as a pro-mitogenic and anti-apoptotic molecule [30]. There are two sphingosine kinase (SphK) isoforms 1 and 2 [31] that, together with phosphatases, control sphingosine/S1P turnover and make them exert intra- and extra-cellular functions [32,33]. Extracellular S1P can act through a specific G-protein coupled receptor family, named S1PR, closely linked with S1P-mediated inflammation [34,35].
Taking into account sphingolipid contribution to cell and tissue homeostasis and metabolism, as well as the combination of perturbations observed during NAFLD and derived HCC development, many studies have pointed out sphingolipids as potential triggers of the disease [25,36].
3. Sphingolipid Contribution to Metabolic Syndrome
Pathologies from metabolic syndrome (MetS) such as obesity, dyslipidemia and insulin resistance (IR) have been reported to induce first hits that induce steatosis development [37,38]. Noteworthy, diabetes and overweight increase the prevalence of the pathology from 20%–30% to 30%–50% and 80%–90% respectively, becoming almost universal when both are combined [37]. Metabolic perturbations during MetS may lead to alterations in the homeostasis of sphingolipids.
In this context, ceramide synthase (CerS), involved in ceramide production in the de novo and salvage pathways, has been described to promote weight gain, glucose intolerance [39,40] and the development of IR [41]. Meanwhile, CerS inhibition by fenretinide has also been demonstrated to prevent lipid-induced IR [42]. Moreover, an upregulation in de novo synthesis through serine-palmitoyltransferase (SPT) modulation has been reported to increase ceramide content in serum [43], whereas selective inhibition with myriocin decreases ceramide levels and ameliorates obesity-derived atherosclerosis [44,45], improves insulin sensitivity [40,43] and reduces body weight [46]. Remarkably, in the study performed by Park and colleagues they have observed a myriocin-induced reduction in hepatic de novo lipogenesis (DNL) that ameliorates serum hyperlipidemia and hypercholesterolemia [47]. It has been also reported an insulin sensitivity recovery through SPT inhibition in high-fat diet (HFD)-induced IR mouse models, which also lead to steatohepatitis and NASH [40,48].
Several works have also characterized the contribution of adipose tissue to sphingolipid content, where a fatty acid excess promotes ceramide synthesis through the de novo pathway. Furthermore, obesity-derived processes promote the release of pro-inflammatory cytokines, such as tumor necrosis factor (TNF), that stimulate ceramide synthesis [49,50] and contribute to NAFLD progression [5]. Indeed, reduced ceramide content by myriocin has been reported to promote adipose tissue beiging with a subsequent improvement in insulin sensitivity and resolution of hepatic steatosis [51]. Therefore, an increase of lipid content promotes ceramide synthesis, not only in the liver but also in adipocytes, contributing to a pro-inflammatory environment.
In relation to the mechanisms by which ceramides inhibit insulin signaling, Jebailey et al. indicates the reduction in the translocation of the glucose transporter type 4 (GLUT4) as a key one [52]. Furthermore, it has been also reported that ceramide interacts with protein kinase B (PKB/Akt) preventing its activation by insulin and inhibiting glucokinase activation, which inhibits glucose uptake and its conversion into glycogen [53,54]. Pertaining to Akt signaling, ceramide-induced inhibition has been described to be mediated by protein phosphatase 2 (PP2A) activation [55]. In a work from our laboratory, Zubiete-Franco et al. have already reported the effect of PP2A activation over autophagy dysregulation in the development of steatosis. Therein, an excess of S-adenosylmethionine (SAMe) inactivates PP2A resolving the pathology [56]. In this context, the dysregulation of autophagy caused by an activation of PP2A by ceramide could be another risk factor that, combined with PKB/Akt-mediated IR, contributes to steatosis.
As mentioned above, ceramide can be metabolized to S1P by the action of ceramidase and SphK, described to be increased in serum from obese patients that suggest a role of ceramide in MetS development [57,58]. An increased fatty acid uptake by the hepatocyte has been observed to stimulate C16-Ceramide and S1P synthesis with a direct effect on IR development [59,60,61]. Interestingly, the work from Shimabukuro also points a possible role of palmitate on promoting the apoptosis of pancreatic beta-cells [60]. Therefore, the effect of ceramide and S1P synthesis would act synergistically with beta-cells apoptosis and inhibiting downstream signaling for promoting insulin resistance.
Inhibition of SPT and CerS (particularly CerS6) presents an attractive target for avoiding MetS-derived steatosis and NASH development. In fact, type 2 diabetes mellitus (T2DM) has been reported to be reverted followed by a reduction on ceramide levels in patients [62] through a treatment that also resolves the NAFLD phenotype [63]. The correlation of MetS, the increase of sphingolipid content (particularly ceramide and S1P) and the development of steatosis and NASH prove to be strongly correlated.
4. Ceramide and Other Sphingolipids in Steatosis and NASH
As aforementioned, steatosis is characterized by an abnormal lipid accumulation, which can lead to NASH through the production of second hits [3]. Imbalances in sphingolipid homeostasis and IR are so relevant in NASH development that mice fed the HFD, the most extended model for IR, also develop NASH with a characteristic steatosis, inflammation, and fibrosis [64]. This may be due to the existing link between triglycerides and sphingolipids synthesis [65,66], combined to the fact that liver lipid content, and sphingolipids particularly, is higher than other tissues [67,68].
Several works have reported increased SM levels in liver [69] and serum [44] from HFD-fed mice, while SM reduction ameliorates both insulin sensitivity and steatosis [44,45]. Cano and colleagues have also reported elevated SM levels in methionine adenosyltransferase 1a (Mat1a)-deficient mice, which spontaneously develop NASH through a disrupted hepatic very-low density lipoprotein (VLDL) assembly [70,71]. Relevantly, around 50% of human NASH patients present a serum metabolic profile associated to Mat1a-/- mice [72], which suggests that SM might also be upregulated in NASH patients. Regarding another NASH animal model, an elevated sphingolipid content has been also characterized in mice overexpressing diacylglyceride-transferase 2 (Dgat2), where an increased lipogenesis leads to lipid accumulation without IR [73].
SMase is a family of enzymes that can be distinguished by their pH optima [74]. In this context, acid SMase (A-SMase) has been reported to be upregulated in NAFLD [6] and its deficiency has been related to the prevention of lipid accumulation in the liver [75]. Likewise, elevated ceramide levels, product of SM catabolism, have been related to the pathology [76,77] as they can promote mitochondrial ROS production by interfering in the electron transport chain, thus leading to an oxidative stress increase [78]. Oxidative stress is one of NASH hallmarks and responsible for inflammation and fibrosis development, so that ceramide could play a role in NAFLD progression by enhancing the effect on other second hits [7]. Moreover, some studies have characterized the relevance of ceramide fatty acid composition in their biological effect, pointing C16-ceramides as mediators in NASH [39,79]. In fact, when CerS6, the enzyme responsible of C14/C16-ceramide synthesis, is downregulated, there is a prevention of steatosis as ceramide also acts as a negative regulator of β-oxidation [39]. Interestingly, the supplementation with Vitamin E also improves NASH development with a subsequent ceramide reduction [71], so that enrichment with this compound in patients offers a compelling therapy.
Inflammation has been widely reported to play a key role during NASH progression into further stages by promoting hepatocyte cell death, Kupffer cell (KC) activation and hepatic stellate cell (HSC)-mediated fibrosis development [5,80]. In this context, cytokines such as TNF and other interleukins are also associated with NAFLD progression from NASH to further stages and, remarkably, they have been reported to upregulate ceramide production [25]. Relating to this, Chang and collaborators have reported that TNF and interleukin-1 (IL-1) activate SPT [81], while inhibiting its effect reduces ceramide content and reverts NASH development [82]. TNF-mediated biological effect has been reported to be through its binding with tumor necrosis factor receptor 1 (TNFR1) and SMases (A-SMase and possibly neutral N-SMase) activation [83], together with the promotion of ROS production [84]. In the meantime SMases also downregulate reduced glutathione (GSH) content in the hepatocyte, reducing the antioxidant capacity of the cell and promoting the effect exerted by ROS excess [85,86]. The treatment with adiponectin, besides improving insulin sensitivity and ameliorating lipid accumulation in the liver, also mitigates the effect of TNF in the hepatocyte while it promotes the anti-inflammatory cytokine IL-10 secretion by KCs [87].
Ceramide has been reported to accumulate in lipid droplets forming acyl-ceramide by the DGAT2-CerS-ACSL5 complex [88]. Considering the pro-apoptotic effect of the sphingolipid in the hepatocyte [89], this could explain the ceramide accumulation observed in steatosis and initial stages of NASH with absent cell death. However, at later stages, ceramide accumulation could be so high that the complex DGAT2-CerS-ACSL5 would be unable to conjugate all ceramide, so that the molecule would be present in its free form triggering hepatocyte cell death and leading to fibrosis development [88,89,90]. It would be interesting to perform an exhaustive study in order to determine whether the ceramide effect in each stage of the pathology depends on its conjugation into lipid droplets and if this process mediates in NAFLD progression.
Current routine methods are a key challenge for accurate correct NASH diagnose, and research is focused on finding adequate markers that allow to identify the pathology in a cost-effective way [1,91]. In this context, the lipidomic profile characterization of serum from NASH patients has identified an upregulation of ceramide levels [39,58]. Correlated to this, Alonso and another authors have also based on metabolomics analysis of serum to point ceramide and SM as key promoters of the transition between steatosis and NASH [72,77]. Therefore, ceramides may present a suitable method to identify the development and progression of NAFLD.
In summary, the high-fat hepatic content during MetS might lead to the observed hepatic SM accumulation. Meanwhile, enhanced SM catabolism through A-SMase upregulation could lead to the observed ceramide increase in NASH. Regarding NASH lean patients, more research needs to be performed for characterizing sphingolipid contribution to the pathology, as ceramide could be somehow mediating in the development of hepatic IR.
5. Ceramide and S1P Role in Fibrosis and Cirrhosis Development
During fibrosis development, hepatocyte cell death activate KCs that release pro-inflammatory cytokines, activating HSCs [80,92]. Once activated, HSCs secrete extracellular matrix (ECM) that fills the space of Disse and proliferate, replacing dead hepatocytes by fibrotic scar tissue which turns into fibrosis under chronic deposition [90,93,94].
Regarding their effect in the hepatocyte, both an upregulated A-SMase expression and ceramide content have been related to cell death [89] through activation of death receptors as fatty acid synthase (FAS) and TNFR1 [95]. The induction of necrosis in CCl4-treated mice, a fibrosis model widely studied [13,96], has been also correlated with an increase of ceramide content both in serum and liver [97]. Correlated with TNF, previously cited to deplete GSH levels in the cell during NASH, hepatocytes have been described to be more susceptible for cell death in that context [98,99]. Additionally, in mice that lack A-SMase ceramide levels are reduced and lowered TNF-mediated effect is lowered [99]. A-SMase has been also described to activate HSCs which, in the absence of the hepatocyte, promote the development of fibrogenesis through migration and extracellular matrix secretion [100].
Not only ceramide has been reported to be upregulated during liver fibrosis and cirrhosis, but also S1P has been pointed out to play a role [94]. It has been characterized that this molecule promotes fibrosis development in cholestatic liver injury by the recruitment of bone-marrow-derived myofibroblasts through S1PR3, where an agonist reverts the pathology [101]. The research of the mechanism of action of S1P has been further investigated in another work that characterizes S1P upregulation in human liver fibrosis, as well as the expression of its receptors S1PR1 and S1PR3 [102], whereas the receptor isoform 2 appears to be downregulated. Indeed, the effect of S1P on myofibroblast migration is also characterized for each receptor, finding a correlation between their expression and their pro-/anti-migratory activity (S1PR1 and S1PR3 promote migration while S1PR2 inhibits) [101]. This work agrees with the study by Liu and colleagues, where the role of S1P in human HSC motility and activation is elucidated [103]. Likewise, S1PR2 has been related to regulate and mitigate the fibrotic and regenerative response after liver injury [104]. This could explain the biological effect of S1P in myofibroblasts, where the molecule has been described to exert an anti-proliferative and a pro-survival role [105]. More research is required in order to define the signaling of S1P through each receptor and their regulation.
Despite liver fibrosis being historically considered irreversible, several treatments have proved to improve the pathology [106,107]. Necessarily, the development of a suitable therapy passes through characterizing the main underlying mechanism. Although liver biopsy is the most reliable technique, it presents an elevated cost and risk, resulting in the development of alternative methods, with sphingolipids emerging as a potential diagnosis tool. Changes in metabolic profile have been characterized in fibrosis animal models, such as previously mentioned CCl4, with a response to an anti-fibrotic therapy [97,108]. Chang and collaborators have also identified key metabolic changes in a fibrosis rat model, where lactosylceramide levels are increased along the progression of the disease [109]. Such alterations in sphingolipid profile also allow for classification of cirrhosis patients into compensated and non-compensated, relating it with their survival rate [6,110] or associating with another serum marker such as low-density lipoprotein (LDL) levels [111]. Ceramide levels have also been characterized to be altered during necroinflammation in patients with normal alanine aminotransferase (ALT) levels [112], the routine diagnose method in monitoring liver health.
The research performed in sphingolipid metabolomics has placed these molecules as a potential tool for diagnose cirrhosis patients, stratifying them or determining their survival prognosis. Additionally, targeting S1P-related proteins offers an attractive research line as they reduce the migration and activation of myofibroblasts or HSCs.
6. Hepatocellular Carcinoma and Ceramide Metabolism
As aforementioned, NAFLD increases the risk of developing HCC [16,17]. The absence of symptomatology allows diagnosis mostly at advanced stages, leading to a poor prognosis and difficulties during treatment [113,114]. Moreover, recurrence may be enhanced by metabolic reprogramming and different signaling pathways that contribute to the malignant transformation of the HCC and reduce the efficacy of systemic therapies [115]. In order to achieve a more accurate prognosis, an effective diagnostic methods and treatments are required.
6.1. Cancer Development Implies a Reduction of Ceramide Content
Although there is a ceramide increase during NAFLD development at all the stages [76,77,89], ceramide content has been reported to be reduced in HCC leading to a decrease in apoptosis [116] that correlates with the highly proliferative capacity of the disease [117]. Such reduction is caused by the metabolism of ceramide into other bioactive compounds. Despite being mainly characterized in other cancer cell types, the existence of common pathways prompts to expect a similar biological function in liver cancer [118].
Ceramide content is reduced through deacetylation and phosphorylation into S1P [119], which plays a proliferative role, especially during DNA damage repair (DDR) mechanisms [120]. Glucosylceramide production, which also reduces ceramide content, acts promoting drug resistance mechanisms during tumor development [121]. Moreover, ceramide phosphorylation into C1P and A-SMase inhibition have been reported to reduce ceramide content [122,123]. Although this ceramide metabolism into C1P has been only reported in macrophages [29], a similar activity of the molecule is expected in KCs from the liver. Furthermore, ceramide transfer protein (CERT), which plays a role during complex sphingolipids synthesis by transferring ceramide from the endoplasmic reticulum to Golgi, has been described to be induced in cancer [124] so related therapies sensitize cells to the treatment [125].
Modulators of ceramide-related enzymes have been emerged as an attractive approach for various cancer types [126]. Anthracyclines have been characterized to increase ceramide content by stimulating CerS triggering apoptosis [127], while Gemcitabine activates A-SMase reaching a similar effect [128]. Cisplatin has been also described to activate A-SMase [129], while the action of S1P-related enzymes (such as S1P lyase [130] or SphK and CerS isoforms [131]) modulates cell sensitivity to the treatment. Focusing on liver-targeting treatments for HCC, Vinblastine has been characterized to activate CerS increasing ceramide content inside the liver [132]. Interestingly, when ceramide is combined with the treatment, an induction of autophagy with the autophagosome maturation is reached, achieving a more powerful antitumor effect [6,118,133]. Another combined treatment with sorafenib and A-SMase promotes cell death relative to the treatment alone [134]. However, despite of sorafenib efficiency being proven, the loss of efficacy, resistance development and side effects [135] make more research required to achieve a better efficacy.
6.2. DDR and S1P as Potential Targets for HCC Therapies
The relationship between NAFLD progression and inflammation has been widely reported, with ROS overproduction and mitochondrial dysfunction leading to the release of pro-inflammatory cytokines as TNF [4,136]. Such ROS overproduction also mediates DNA-involved reactions, causing perturbations that activate DNA damage response (DDR) mechanisms reported to be relevant during HCC development [137]. Despite the exact pro-carcinogenic role of sphingolipids in NASH being poorly understood, some research works have found that S1P upregulates p27 [138], a cell-cycle regulator and a possible prognosis marker as it shows a positive correlation with tumor size [8,139]. Another work from Yin et al., also demonstrate that the alkaline ceramidase ACER3 isoform promotes the proliferation of HCC cells through the formation of S1P [140].
Remarkably, S1P implication has been characterized both in DDR mechanisms and DNA damage [120] while it controls lipid metabolism [8]. Osawa and collaborators have characterized the effect of SphK in hepatoma cell differentiation by promoting the pro-tumor phenotype [141]. In his work they characterize the differentiation effect of inhibiting SphK in Huh-7 cells, an in vitro cell model of human HCC widely used in the study of the disease [142,143]. Particularly, the isoform SphK1 has been related to poor prognosis among cancer patients by having a pro-metastatic role [144,145]. S1P has been pointed out as a key molecule in stimulating invasiveness, angiogenesis, lymphangiogenesis and cell survival against chemotherapy-induced ROS [146,147]. One of S1P-mediated actions is mediated through histone deacetylases (HDACs). The HDAC4 isoform has been described to promote fibrotic liver injury in a prohibitin 1-knockout (Phb1-/-) animal model which also develops HCC [148,149], suggesting a possible contribution of S1P to the observed effect in tumor development. Taking presented results into account, together with the highly proliferative and angiogenic capacity of HCC [150], S1P emerges as a potential anti-HCC treatment so more research would be interesting to perform.
In summary, most research about sphingolipid contribution to cancer development has not been performed in HCC, so it would be interesting to further characterize the existing turnover from ceramide to S1P in this type of cancer. Compounds targeting this process, as well as the combination with current treatments, seems an attractive approach against the pathology.
7. Concluding Remarks
The aim of this work is to point out the relevance of sphingolipids in the development of NAFLD and NAFLD-derived HCC. Presented studies characterize sphingolipids’ (particularly ceramide, SM, and S1P) contribution to NAFLD progression, in each stage of the pathology and its related conditions: MetS, steatosis and NASH, fibrosis/cirrhosis and HCC. Indeed, therapies targeting ceramide- or S1P-related enzymes have been proven to alleviate the condition. Metabolomics and sphingolipid determination in serum also presents an attractive approach for developing diagnostic methods, as these kind of molecules appear to be dysregulated in each pathology.
Ceramide is considered the central molecule in sphingolipids metabolism and its modulation plays a key role in the development of several pathologies. In an early steatosis condition, ceramide accumulation could be only a direct consequence of an imbalance, mainly determined by a perturbation in hepatic lipid content, as it is not exerting its biological pro-apoptotic function. This might be due to the ACSL5-DGAT2-CerS complex, which would somehow “buffering” ceramide effect by converting it into acylceramide. In more advanced stages, the complex could not afford such ceramide overproduction so ceramide would be mainly in its free form, promoting hepatocyte death and its metabolism into S1P. Meanwhile, S1P activates HSCs contributing to fibrosis development by ECM secretion and replacement of death hepatocytes. Finally, at the last stage of chronic disease such as HCC, an activation of the enzymes that reduce ceramide content in the cell is stimulated. This ceramide reduction prevents the cells from the anti-proliferative effect, so that this would favor tumor growth. Therein, S1P is the most abundant sphingolipid in the liver and plays a role in proliferation, invasiveness and angiogenesis capacity of the tumor (See graphical abstract).
Author Contributions
Conceptualization: J.S., A.O., M.L.M.-C.; Investigation: J.S., A.O., N.P.; Writing—Original Draft Preparation: J.S., A.O., L.A.-I., N.P.; Writing—Review and Editing: J.S., A.O., L.A.-I., N.P., T.C.D., M.L.M.-C.; Visualization: J.S., A.O., T.C.D., M.L.M.-C.; Funding acquisition: T.C.D., M.L.M.-C.; Supervision: M.L.M.-C.; Project Administration: J.S., M.L.M.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from Ministerio de Economía, Industria y Competitividad: SAF2017-87301-R (M.L.M.-C.), Gobierno Vasco-Departamento de Salud 2013111114 (to M.L.M.-C.), BIOEF (Basque Foundation for Innovation and Health Research: EiTB Maratoia BIO15/CA/016/BD (M.L.M.-C.), ELKARTEK 2016, Departamento de Industria del Gobierno Vasco (to M.L.M.-C.), Asociación Española contra el Cáncer (to T.C.D. and M.L.M.-C.), Daniel Alagille award from EASL (to T.C.D.), Fundación Científica de la Asociación Española Contra el Cancer (AECC Scientific Foundation) Rare Tumor Calls 2017 (to M.L.M.-C.), La Caixa Foundation Program (to M.L.M.-C.). We thank Gobierno Vasco-Departamento de Educación for the pre-doctoral grants from 2014 (to N.P.) and 2015 (to J.S.) and the post-doctoral grant from 2017 (to A.O.). We thank MINECO for the Severo Ochoa Excellence Accreditation (SEV-2016-0644).
Conflicts of Interest
María Luz Martínez-Chantar advises for Mitotherapeutix LLC. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of nonalcoholic fatty liver disease—Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 2.Bellentani S., Scaglioni F., Marino M., Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig. Dis. 2010;28:155–161. doi: 10.1159/000282080. [DOI] [PubMed] [Google Scholar]
- 3.Day C., James O. Steatohepatitis: A tale of two “Hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/S0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 4.Sanyal A.J. Mechanisms of Disease: pathogenesis of nonalcoholic fatty liver disease. Nat. Clin. Pract. Gastroenterol. Hepatol. 2005;2:46–53. doi: 10.1038/ncpgasthep0084. [DOI] [PubMed] [Google Scholar]
- 5.Day C.P. From fat to inflammation. Gastroenterology. 2006;130:207–210. doi: 10.1053/j.gastro.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Grammatikos G., Ferreiros N., Waidmann O., Bon D., Schroeter S., Koch A., Herrmann E., Zeuzem S., Kronenberger B., Pfeilschifter J. Serum sphingolipid variations associate with hepatic decompensation and survival in patients with cirrhosis. PLoS ONE. 2015;10:1–15. doi: 10.1371/journal.pone.0138130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasumov T., Li L., Li M., Gulshan K., Kirwan J.P., Liu X., Previs S., Willard B., Smith J.D., McCullough A. Ceramide as a mediator of non-alcoholic fatty liver disease and associated atherosclerosis. PLoS ONE. 2015;10:1–26. doi: 10.1371/journal.pone.0126910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagahashi M., Matsuda Y., Moro K., Tsuchida J., Soma D., Hirose Y., Kobayashi T., Kosugi S.I., Takabe K., Komatsu M., et al. DNA damage response and sphingolipid signaling in liver diseases. Surg. Today. 2016;46:995–1005. doi: 10.1007/s00595-015-1270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mishra A., Younossi Z.M. Epidemiology and Natural History of Non-alcoholic Fatty Liver Disease. J. Clin. Exp. Hepatol. 2012;2:135–144. doi: 10.1016/S0973-6883(12)60102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farrell G.C., Larter C.Z. Nonalcoholic fatty liver disease: From steatosis to cirrhosis. Hepatology. 2006;43:99–112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 11.Harrison S.A., Torgerson S., Hayashi P.H. The natural history of nonalcoholic fatty liver disease: a clinical histopathological study. Am. J. Gastroenterol. 2003;98:2042. doi: 10.1111/j.1572-0241.2003.07659.x. [DOI] [PubMed] [Google Scholar]
- 12.Samonakis D.N., Koulentaki M., Coucoutsi C., Augoustaki A., Baritaki C., Digenakis E., Papiamonis N., Fragaki M., Matrella E., Tzardi M., et al. Clinical outcomes of compensated and decompensated cirrhosis: A long term study. World J. Hepatol. 2014;6:504–512. doi: 10.4254/wjh.v6.i7.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zubiete-Franco I., Fernandez-Tussy P., Barbier-Torres L., Simon J., Fernandez-Ramos D., Lopitz-Otsoa F., Gutierrez-de Juan V., de Davalillo S.L., Duce A.M., Iruzubieta P., et al. Deregulated neddylation in liver fibrosis. Hepatology. 2017;65:694–709. doi: 10.1002/hep.28933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Govaere O., Roskams T. Pathogenesis and prognosis of hepatocellular carcinoma at the cellular and molecular levels. Clin. Liver Dis. 2015;19:261–276. doi: 10.1016/j.cld.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 15.Jemal A., Bray F., Ferlay J. Global Cancer Statistics. CA Cancer J. Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 16.McGlynn K.A., London W.T. The global epidemiology of hepatocellular carcinoma: present and future. Clin. Liver Dis. 2011;15:223–243. doi: 10.1016/j.cld.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mittal S., El-Serag H.B. Epidemiology of hepatocellular carcinoma: consider the population. J. Clin. Gastroenterol. 2013;47:S2–S6. doi: 10.1097/MCG.0b013e3182872f29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michelotti G.A., Machado M.V., Diehl A.M. NAFLD, NASH and liver cancer. Nat. Rev. Gastroenterol. Hepatol. 2013;10:656–665. doi: 10.1038/nrgastro.2013.183. [DOI] [PubMed] [Google Scholar]
- 19.Hannun Y.A., Obeid L.M. Principles of bioactive lipid signalling: lessons from sphingolipids. Nat. Rev. Mol. Cell Biol. 2008;9:139–150. doi: 10.1038/nrm2329. [DOI] [PubMed] [Google Scholar]
- 20.Gangoiti P., Camacho L., Arana L., Ouro A., Granado M.H., Brizuela L., Casas J., Fabriás G., Abad J.L., Delgado A., et al. Control of metabolism and signaling of simple bioactive sphingolipids: Implications in disease. Prog. Lipid Res. 2010;49:316–334. doi: 10.1016/j.plipres.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Gomez-Munoz A. Ceramide 1-phosphate/ceramide, a switch between life and death. Biochim. Biophys. Acta. 2006;1758:2049–2056. doi: 10.1016/j.bbamem.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Haimovitz-Friedman A., Kolesnick R.N., Fuks Z. Ceramide signaling in apoptosis. Br. Med. Bull. 1997;53:539–553. doi: 10.1093/oxfordjournals.bmb.a011629. [DOI] [PubMed] [Google Scholar]
- 23.Mullen T.D., Obeid L.M. Ceramide and apoptosis: exploring the enigmatic connections between sphingolipid metabolism and programmed cell death. Anticancer Agents Med. Chem. 2012;12:340–363. doi: 10.2174/187152012800228661. [DOI] [PubMed] [Google Scholar]
- 24.Albeituni S., Stiban J. Roles of Ceramides and Other Sphingolipids in Immune Cell Function and Inflammation. Adv. Exp. Med. Biol. 2019;1161:169–191. doi: 10.1007/978-3-030-21735-8_15. [DOI] [PubMed] [Google Scholar]
- 25.Holland W.L., Bikman B.T., Wang L.P., Yuguang G., Sargent K.M., Bulchand S., Knotts T.A., Shui G., Clegg D.J., Wenk M.R., et al. Lipid-induced insulin resistance mediated by the proinflammatory receptor TLR4 requires saturated fatty acid-induced ceramide biosynthesis in mice. J. Clin. Investig. 2011;121:1858–1870. doi: 10.1172/JCI43378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morad S.A., Cabot M.C. Ceramide-orchestrated signalling in cancer cells. Nat. Rev. Cancer. 2012 doi: 10.1038/nrc3398. in press. [DOI] [PubMed] [Google Scholar]
- 27.Arana L., Ordonez M., Ouro A., Rivera I.-G., Gangoiti P., Trueba M., Gomez-Munoz A. Ceramide 1-phosphate induces macrophage chemoattractant protein-1 release: involvement in ceramide 1-phosphate-stimulated cell migration. AJP Endocrinol. Metab. 2013;304:E1213–E1226. doi: 10.1152/ajpendo.00480.2012. [DOI] [PubMed] [Google Scholar]
- 28.Granado M.H., Gangoiti P., Ouro A., Arana L., González M., Trueba M., Gómez-Muñoz A. Ceramide 1-phosphate (C1P) promotes cell migration. Involvement of a specific C1P receptor. Cell. Signal. 2009;21:405–412. doi: 10.1016/j.cellsig.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Ouro A., Arana L., Rivera I.G., Ordoñez M., Gomez-Larrauri A., Presa N., Simón J., Trueba M., Gangoiti P., Bittman R., et al. Phosphatidic acid inhibits ceramide 1-phosphate-stimulated macrophage migration. Biochem. Pharmacol. 2014;92:642–650. doi: 10.1016/j.bcp.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Lee M.J., Van Brocklyn J.R., Thangada S., Liu C.H., Hand A.R., Menzeleev R., Spiegel S., Hla T. Sphingosine-1-phosphate as a ligand for the G protein-coupled receptor EDG-1. Science. 1998;279:1552–1555. doi: 10.1126/science.279.5356.1552. [DOI] [PubMed] [Google Scholar]
- 31.Taha T.A., Hannun Y.A., Obeid L.M. Sphingosine kinase: biochemical and cellular regulation and role in disease. J. Biochem. Mol. Biol. 2006;39:113–131. doi: 10.5483/BMBRep.2006.39.2.113. [DOI] [PubMed] [Google Scholar]
- 32.Mandala S.M. Sphingosine-1-phosphate phosphatases. Prostaglandins Other Lipid Mediat. 2001;64:143–156. doi: 10.1016/S0090-6980(01)00111-3. [DOI] [PubMed] [Google Scholar]
- 33.Johnson K.R., Johnson K.Y., Becker K.P., Bielawski J., Mao C., Obeid L.M. Role of human sphingosine-1-phosphate phosphatase 1 in the regulation of intra- and extracellular sphingosine-1-phosphate levels and cell viability. J. Biol. Chem. 2003;278:34541–34547. doi: 10.1074/jbc.M301741200. [DOI] [PubMed] [Google Scholar]
- 34.Vestri A., Pierucci F., Frati A., Monaco L., Meacci E. Sphingosine 1-Phosphate Receptors: Do They Have a Therapeutic Potential in Cardiac Fibrosis? Front. Pharmacol. 2017;8:296. doi: 10.3389/fphar.2017.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goetzl E.J., Wang W., McGiffert C., Huang M.C., Graler M.H. Sphingosine 1-phosphate and its G protein-coupled receptors constitute a multifunctional immunoregulatory system. J. Cell. Biochem. 2004;92:1104–1114. doi: 10.1002/jcb.20053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grammatikos G., Mühle C., Ferreiros N., Schroeter S., Bogdanou D., Schwalm S., Hintereder G., Kornhuber J., Zeuzem S., Sarrazin C., et al. Serum acid sphingomyelinase is upregulated in chronic hepatitis C infection and non alcoholic fatty liver disease. Biochim. Biophys. Acta - Mol. Cell Biol. Lipids. 2014;1841:1012–1020. doi: 10.1016/j.bbalip.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 37.Loomba R., Sanyal A.J. The global NAFLD epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013;10:686–690. doi: 10.1038/nrgastro.2013.171. [DOI] [PubMed] [Google Scholar]
- 38.Vernon G., Baranova A., Younossi Z.M. Systematic review: The epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharmacol. Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 39.Turpin S.M., Nicholls H.T., Willmes D.M., Mourier A., Brodesser S., Wunderlich C.M., Mauer J., Xu E., Hammerschmidt P., Brönneke H.S., et al. Obesity-induced CerS6-dependent C16:0 ceramide production promotes weight gain and glucose intolerance. Cell Metab. 2014;20:678–686. doi: 10.1016/j.cmet.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Holland W.L., Brozinick J.T., Wang L.P., Hawkins E.D., Sargent K.M., Liu Y., Narra K., Hoehn K.L., Knotts T.A., Siesky A., et al. Inhibition of Ceramide Synthesis Ameliorates Glucocorticoid-, Saturated-Fat-, and Obesity-Induced Insulin Resistance. Cell Metab. 2007;5:167–179. doi: 10.1016/j.cmet.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 41.Cinar R., Godlewski G., Liu J., Tam J., Jourdan T., Mukhopadhyay B., Harvey-White J., Kunos G. Hepatic cannabinoid-1 receptors mediate diet-induced insulin resistance by increasing de novo synthesis of long-chain ceramides. Hepatology. 2014;59:143–153. doi: 10.1002/hep.26606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bikman B.T., Guan Y., Shui G., Siddique M.M., Holland W.L., Kim J.Y., Fabriàs G., Wenk M.R., Summers S.A. Fenretinide prevents lipid-induced insulin resistance by blocking ceramide biosynthesis. J. Biol. Chem. 2012;287:17426–17437. doi: 10.1074/jbc.M112.359950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watson M.L., Coghlan M., Hundal H.S. Modulating serine palmitoyl transferase (SPT) expression and activity unveils a crucial role in lipid-induced insulin resistance in rat skeletal muscle cells. Biochem. J. 2009;417:791–801. doi: 10.1042/BJ20081149. [DOI] [PubMed] [Google Scholar]
- 44.Chun L., Junlin Z., Aimin W., Niansheng L., Benmei C., Minxiang L. Inhibition of ceramide synthesis reverses endothelial dysfunction and atherosclerosis in streptozotocin-induced diabetic rats. Diabetes Res. Clin. Pract. 2011;93:77–85. doi: 10.1016/j.diabres.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 45.Glaros E.N., Kim W.S., Wu B.J., Suarna C., Quinn C.M., Rye K.A., Stocker R., Jessup W., Garner B. Inhibition of atherosclerosis by the serine palmitoyl transferase inhibitor myriocin is associated with reduced plasma glycosphingolipid concentration. Biochem. Pharmacol. 2007;73:1340–1346. doi: 10.1016/j.bcp.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 46.Yang G., Badeanlou L., Bielawski J., Roberts A.J., Hannun Y.A., Samad F. Central role of ceramide biosynthesis in body weight regulation, energy metabolism, and the metabolic syndrome. Am. J. Physiol. Endocrinol. Metab. 2009;297 doi: 10.1152/ajpendo.91014.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park T.S., Panek R.L., Rekhter M.D., Mueller S.B., Rosebury W.S., Robertson A., Hanselman J.C., Kindt E., Homan R., Karathanasis S.K. Modulation of lipoprotein metabolism by inhibition of sphingomyelin synthesis in ApoE knockout mice. Atherosclerosis. 2006;189:264–272. doi: 10.1016/j.atherosclerosis.2005.12.029. [DOI] [PubMed] [Google Scholar]
- 48.Zabielski P., Daniluk J., Hady H.R., Markowski A.R., Imierska M., Gorski J., Blachnio-Zabielska A.U. The effect of high-fat diet and inhibition of ceramide production on insulin action in liver. J. Cell. Physiol. 2019;234:1851–1861. doi: 10.1002/jcp.27058. [DOI] [PubMed] [Google Scholar]
- 49.Samad F., Badeanlou L., Shah C., Yang G. Adipose tissue and ceramide biosynthesis in the pathogenesis of obesity. Adv. Exp. Med. Biol. 2011;721:67–86. doi: 10.1007/978-1-4614-0650-1_5. [DOI] [PubMed] [Google Scholar]
- 50.Chaurasia B., Summers S.A. Ceramides - Lipotoxic Inducers of Metabolic Disorders. Trends Endocrinol. Metab. 2015;26:538–550. doi: 10.1016/j.tem.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 51.Chaurasia B., Kaddai V.A., Lancaster G.I., Henstridge D.C., Sriram S., Galam D.L.A., Gopalan V., Prakash K.N.B., Velan S.S., Bulchand S., et al. Adipocyte Ceramides Regulate Subcutaneous Adipose Browning, Inflammation, and Metabolism. Cell Metab. 2016;24:820–834. doi: 10.1016/j.cmet.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 52.JeBailey L., Wanono O., Niu W., Roessler J., Rudich A., Klip A. Ceramide- and oxidant-induced insulin resistance involve loss of insulin-dependent Rac-activation and actin remodeling in muscle cells. Diabetes. 2007;56:394–403. doi: 10.2337/db06-0823. [DOI] [PubMed] [Google Scholar]
- 53.Ribaux P.G., Iynedjian P.B. Analysis of the role of protein kinase B (cAKT) in insulin-dependent induction of glucokinase and sterol regulatory element-binding protein 1 (SREBP1) mRNAs in hepatocytes. Biochem. J. 2003;376:697–705. doi: 10.1042/bj20031287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Holland W.L., Summers S.A. Sphingolipids, insulin resistance, and metabolic disease: New insights from in vivo manipulation of sphingolipid metabolism. Endocr. Rev. 2008;29:381–402. doi: 10.1210/er.2007-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Summers S.A. Ceramides in insulin resistance and lipotoxicity. Prog. Lipid Res. 2006;45:42–72. doi: 10.1016/j.plipres.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 56.Zubiete-Franco I., Garcia-Rodriguez J.L., Martinez-Una M., Martinez-Lopez N., Woodhoo A., Juan V.G.-D., Beraza N., Lage-Medina S., Andrade F., Fernandez M.L., et al. Methionine and S-adenosylmethionine levels are critical regulators of PP2A activity modulating lipophagy during steatosis. J. Hepatol. 2016;64:409–418. doi: 10.1016/j.jhep.2015.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kowalski G.M., Carey A.L., Selathurai A., Kingwell B.A., Bruce C.R. Plasma Sphingosine-1-Phosphate Is Elevated in Obesity. PLoS ONE. 2013;8:1–7. doi: 10.1371/journal.pone.0072449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Turner N., Kowalski G.M., Leslie S.J., Risis S., Yang C., Lee-Young R.S., Babb J.R., Meikle P.J., Lancaster G.I., Henstridge D.C., et al. Distinct patterns of tissue-specific lipid accumulation during the induction of insulin resistance in mice by high-fat feeding. Diabetologia. 2013;56:1638–1648. doi: 10.1007/s00125-013-2913-1. [DOI] [PubMed] [Google Scholar]
- 59.Fayyaz S., Henkel J., Japtok L., Krämer S., Damm G., Seehofer D., Püschel G.P., Kleuser B. Involvement of sphingosine 1-phosphate in palmitate-induced insulin resistance of hepatocytes via the S1P2 receptor subtype. Diabetologia. 2014;57:373–382. doi: 10.1007/s00125-013-3123-6. [DOI] [PubMed] [Google Scholar]
- 60.Shimabukuro M., Zhou Y.T., Levi M., Unger R.H. Fatty acid-induced β cell apoptosis: A link between obesity and diabetes. Proc. Natl. Acad. Sci. USA. 1998;95:2498–2502. doi: 10.1073/pnas.95.5.2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hu W., Bielawski J., Samad F., Merrill A.H., Cowart L.A. Palmitate increases sphingosine-1-phosphate in C2C12 myotubes via upregulation of sphingosine kinase message and activity. J. Lipid Res. 2009;50:1852–1862. doi: 10.1194/jlr.M800635-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kasumov T., Huang H., Chung Y.M., Zhang R., McCullough A.J., Kirwan J.P. Quantification of ceramide species in biological samples by liquid chromatography electrospray ionization tandem mass spectrometry. Anal. Biochem. 2010;401:154–161. doi: 10.1016/j.ab.2010.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Takahashi H., Kotani K., Tanaka K., Egucih Y., Anzai K. Therapeutic approaches to nonalcoholic fatty liver disease: Exercise intervention and related mechanisms. Front. Endocrinol. (Lausanne) 2018;9:1–17. doi: 10.3389/fendo.2018.00588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stephenson K., Kennedy L., Hargrove L., Demieville J., Thomson J., Alpini G., Francis H. Updates on dietary models of nonalcoholic fatty liver disease: Current studies and insights. Gene Expr. 2018;18:5–17. doi: 10.3727/105221617X15093707969658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bektas M., Laura Allende M., Lee B.G., Chen W.P., Amar M.J., Remaley A.T., Saba J.D., Proia R.L. Sphingosine 1-phosphate lyase deficiency disrupts lipid homeostasis in liver. J. Biol. Chem. 2010;285:10880–10889. doi: 10.1074/jbc.M109.081489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aguilera-Romero A., Gehin C., Riezman H. Sphingolipid homeostasis in the web of metabolic routes. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2014;1841:647–656. doi: 10.1016/j.bbalip.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 67.Kotronen A., Seppänen-Laakso T., Westerbacka J., Kiviluoto T., Arola J., Ruskeepää A.L., Yki-Järvinen H., Orešič M. Comparison of lipid and fatty acid composition of the liver, subcutaneous and intra-abdominal adipose tissue, and serum. Obesity. 2010;18:937–944. doi: 10.1038/oby.2009.326. [DOI] [PubMed] [Google Scholar]
- 68.Llacuna L., Marí M., Garcia-Ruiz C., Fernandez-Checa J.C., Morales A. Critical role of acidic sphingomyelinase in murine hepatic ischemia-reperfusion injury. Hepatology. 2006;44:561–572. doi: 10.1002/hep.21285. [DOI] [PubMed] [Google Scholar]
- 69.Chocian G., Chabowski A., Żendzian-Piotrowska M., Harasim E., Łukaszuk B., Górski J. High fat diet induces ceramide and sphingomyelin formation in rat’s liver nuclei. Mol. Cell. Biochem. 2010;340:125–131. doi: 10.1007/s11010-010-0409-6. [DOI] [PubMed] [Google Scholar]
- 70.Cano A., Buqué X., Martínez-uña M., Aurrekoetxea I., Menor A., García-rodriguez J.L., Lu S.C., Martínez-chantar M.L., Mato J.M. Methionine adenosyltransferase 1A gene deletion disrupts hepatic VLDL assembly in mice. Hepatology. 2011;54:1975–1986. doi: 10.1002/hep.24607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Presa N., Clugston R.D., Lingrell S., Kelly S.E., Merrill A.H., Jana S., Kassiri Z., Gómez-Muñoz A., Vance D.E., Jacobs R.L., et al. Vitamin E alleviates non-alcoholic fatty liver disease in phosphatidylethanolamine N-methyltransferase deficient mice. Biochim. Biophys. Acta - Mol. Basis Dis. 2019;1865:14–25. doi: 10.1016/j.bbadis.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 72.Alonso C., Fernández-Ramos D., Varela-Rey M., Martínez-Arranz I., Navasa N., Van Liempd S.M., Lavín Trueba J.L., Mayo R., Ilisso C.P., de Juan V.G., et al. Metabolomic Identification of Subtypes of Nonalcoholic Steatohepatitis. Gastroenterology. 2017;152:1449–1461.e7. doi: 10.1053/j.gastro.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Monetti M., Levin M.C., Watt M.J., Sajan M.P., Marmor S., Hubbard B.K., Stevens R.D.D., Bain J.R., Newgard C.B., Farese R.V., et al. Dissociation of Hepatic Steatosis and Insulin Resistance in Mice Overexpressing DGAT in the Liver. Cell Metab. 2007;6:69–78. doi: 10.1016/j.cmet.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 74.Goni F.M., Alonso A. Sphingomyelinases: enzymology and membrane activity. FEBS Lett. 2002;531:38–46. doi: 10.1016/S0014-5793(02)03482-8. [DOI] [PubMed] [Google Scholar]
- 75.Deevska G.M., Rozenova K.A., Giltiay N.V., Chambers M.A., White J., Boyanovsky B.B., Wei J., Daugherty A., Smart E.J., Reid M.B., et al. Acid sphingomyelinase deficiency prevents diet-induced hepatic triacylglycerol accumulation and hyperglycemia in mice. J. Biol. Chem. 2009;284:8359–8368. doi: 10.1074/jbc.M807800200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Puri P., Mirshahi F., Cheung O., Natarajan R., Maher J.W., Kellum J.M., Sanyal A.J. Activation and dysregulation of the unfolded protein response in nonalcoholic fatty liver disease. Gastroenterology. 2008;134:568–576. doi: 10.1053/j.gastro.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 77.Gorden D.L., Myers D.S., Ivanova P.T., Fahy E., Maurya M.R., Gupta S., Min J., Spann N.J., McDonald J.G., Kelly S.L., et al. Biomarkers of NAFLD progression: A lipidomics approach to an epidemic 1. J. Lipid Res. 2015;56:722–736. doi: 10.1194/jlr.P056002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.García-Ruiz C., Colell A., Marí M., Morales A., Fernández-Checa J.C. Direct effect of ceramide on the mitochondrial electron transport chain leads to generation of reactive oxygen species: Role of mitochondrial glutathione. J. Biol. Chem. 1997;272:11369–11377. doi: 10.1074/jbc.272.17.11369. [DOI] [PubMed] [Google Scholar]
- 79.Raichur S., Wang S.T., Chan P.W., Li Y., Ching J., Chaurasia B., Dogra S., Öhman M.K., Takeda K., Sugii S., et al. CerS2 haploinsufficiency inhibits β-oxidation and confers susceptibility to diet-induced steatohepatitis and insulin resistance. Cell Metab. 2014;20:687–695. doi: 10.1016/j.cmet.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 80.Higuchi H., Gores G. Mechanisms of Liver Injury: An Overview. Curr. Mol. Med. 2003;3:483–490. doi: 10.2174/1566524033479528. [DOI] [PubMed] [Google Scholar]
- 81.Chang Z.Q., Lee S.Y., Kim H.J., Kim J.R., Kim S.J., Hong I.K., Oh B.C., Choi C.S., Goldberg I.J., Park T.S. Endotoxin activates de novo sphingolipid biosynthesis via nuclear factor kappa B-mediated upregulation of Sptlc2. Prostaglandins Other Lipid Mediat. 2011;94:44–52. doi: 10.1016/j.prostaglandins.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nikolova-Karakashian M.N., Rozenova K.A. Ceramide in stress response. Adv. Exp. Med. Biol. 2010;688:86–108. doi: 10.1007/978-1-4419-6741-1_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Marí M., Fernández-Checa J.C. Sphingolipid signalling and liver diseases. Liver Int. 2007;27:440–450. doi: 10.1111/j.1478-3231.2007.01475.x. [DOI] [PubMed] [Google Scholar]
- 84.Schwabe R.F., Brenner D.A. Mechanisms of liver injury. I. TNF-α-induced liver injury: Role of IKK, JNK, and ROS pathways. Am. J. Physiol. Gastrointest. Liver Physiol. 2006;290:583–589. doi: 10.1152/ajpgi.00422.2005. [DOI] [PubMed] [Google Scholar]
- 85.Clarke C.J., Snook C.F., Tani M., Matmati N., Marchesini N., Hannun Y.A. The extended family of neutral sphingomyelinases. Biochemistry. 2006;45:11247–11256. doi: 10.1021/bi061307z. [DOI] [PubMed] [Google Scholar]
- 86.Nikolova-Karakashian M., Karakashian A., Rutkute K. Role of neutral sphingomyelinases in aging and inflammation. Subcell. Biochem. 2008;49:469–486. doi: 10.1007/978-1-4020-8831-5_18. [DOI] [PubMed] [Google Scholar]
- 87.Polyzos S.A., Toulis K.A., Goulis D.G., Zavos C., Kountouras J. Serum total adiponectin in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Metabolism. 2011;60:313–326. doi: 10.1016/j.metabol.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 88.Senkal C.E., Salama M.F., Snider A.J., Allopenna J.J., Rana N.A., Koller A., Hannun Y.A., Obeid L.M. Ceramide Is Metabolized to Acylceramide and Stored in Lipid Droplets. Cell Metab. 2017;25:686–697. doi: 10.1016/j.cmet.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tsugane K., Tamiya-Koizumi K., Nagino M., Nimura Y., Yoshida S. A possible role of nuclear ceramide and sphingosine in hepatocyte apoptosis in rat liver. J. Hepatol. 1999;31:8–17. doi: 10.1016/S0168-8278(99)80158-5. [DOI] [PubMed] [Google Scholar]
- 90.Bataller R., Brenner D.A. Liver fibrosis. J. Clin. Investig. 2005;115:209–218. doi: 10.1172/JCI24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.NICE Guideline [NG49] Non-alcoholic Fatty Liver Disease: Assessment and Management. [(accessed on 9 October 2019)];2016 Volume 34 Available online: https://www.nice.org.uk/guidance/ng49. [Google Scholar]
- 92.Pessayre D., Mansouri A., Fromenty B., Mansouri A. Nonalcoholic Steatosis and Steatohepatitis V. Mitochondrial dysfunction in steatohepatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2002;282:193–199. doi: 10.1152/ajpgi.00426.2001. [DOI] [PubMed] [Google Scholar]
- 93.Schuppan D., Afdhal N.H. Liver Cirrhosis. Lancet. 2008;371:838–851. doi: 10.1016/S0140-6736(08)60383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shea B.S., Tager A.M. Sphingolipid Regulation of Tissue Fibrosis. Open Rheumatol. J. 2012;6:123–129. doi: 10.2174/1874312901206010123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Malhi H., Guicciardi M.E., Gores G.J. Hepatocyte death: a clear and present danger. Physiol. Rev. 2010;90:1165–1194. doi: 10.1152/physrev.00061.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fernandez-Ramos D., Fernandez-Tussy P., Lopitz-Otsoa F., Gutierrez-de-Juan V., Navasa N., Barbier-Torres L., Zubiete-Franco I., Simon J., Fernandez A.F., Arbelaiz A., et al. MiR-873-5p acts as an epigenetic regulator in early stages of liver fibrosis and cirrhosis. Cell Death Dis. 2018;9:958. doi: 10.1038/s41419-018-1014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ichi I., Nakahara K., Fujii K., Iida C., Miyashita Y., Kojo S. Increase of ceramide in the liver and plasma after carbon tetrachloride intoxication in the rat. J. Nutr. Sci. Vitaminol. (Tokyo) 2007;53:53–56. doi: 10.3177/jnsv.53.53. [DOI] [PubMed] [Google Scholar]
- 98.Mari M., Caballero F., Colell A., Morales A., Caballeria J., Fernandez A., Enrich C., Fernandez-Checa J.C., Garcia-Ruiz C. Mitochondrial free cholesterol loading sensitizes to TNF- and Fas-mediated steatohepatitis. Cell Metab. 2006;4:185–198. doi: 10.1016/j.cmet.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 99.Mari M., Colell A., Morales A., Caballero F., Moles A., Fernandez A., Terrones O., Basanez G., Antonsson B., Garcia-Ruiz C., et al. Mechanism of mitochondrial glutathione-dependent hepatocellular susceptibility to TNF despite NF-kappaB activation. Gastroenterology. 2008;134:1507–1520. doi: 10.1053/j.gastro.2008.01.073. [DOI] [PubMed] [Google Scholar]
- 100.Moles A., Tarrats N., Morales A., Domínguez M., Bataller R., Caballería J., García-Ruiz C., Fernández-Checa J.C., Marí M. Acidic sphingomyelinase controls hepatic stellate cell activation and in vivo liver fibrogenesis. Am. J. Pathol. 2010;177:1214–1224. doi: 10.2353/ajpath.2010.091257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Changyong L., Xiangming J., Lin Y., Xihong L., Shi Y., Liying L. Involvement of sphingosine 1-phosphate (SIP)/S1P3 signaling in cholestasis-induced liver fibrosis. Am. J. Pathol. 2009;175:1464–1472. doi: 10.2353/ajpath.2009.090037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li C., Zheng S., You H., Liu X., Lin M., Yang L., Li L. Sphingosine 1-phosphate (S1P)/S1P receptors are involved in human liver fibrosis by action on hepatic myofibroblasts motility. J. Hepatol. 2011;54:1205–1213. doi: 10.1016/j.jhep.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 103.Liu X., Yue S., Li C., Yang L., You H., Li L. Essential roles of sphingosine 1-phosphate receptor types 1 and 3 in human hepatic stellate cells motility and activation. J. Cell. Physiol. 2011;226:2370–2377. doi: 10.1002/jcp.22572. [DOI] [PubMed] [Google Scholar]
- 104.Ikeda H., Watanabe N., Ishii I., Shimosawa T., Kume Y., Tomiya T., Inoue Y., Nishikawa T., Ohtomo N., Tanoue Y., et al. Sphingosine 1-phosphate regulates regeneration and fibrosis after liver injury via sphingosine 1-phosphate receptor 2. J. Lipid Res. 2009;50:556–564. doi: 10.1194/jlr.M800496-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Davaille J., Li L., Mallat A., Lotersztajn S. Sphingosine 1-phosphate triggers both apoptotic and survival signals for human hepatic myofibroblasts. J. Biol. Chem. 2002;277:37323–37330. doi: 10.1074/jbc.M202798200. [DOI] [PubMed] [Google Scholar]
- 106.Ratziu V., Goodman Z., Sanyal A. Review Current efforts and trends in the treatment of NASH. J. Hepatol. 2015;62:S65–S75. doi: 10.1016/j.jhep.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 107.Benyon R., Iredale J. Is liver fibrosis reversible? Gut. 2000;46:443–446. doi: 10.1136/gut.46.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang G., Li Z., Li H., Li L., Li J., Yu C. Metabolic profile changes of CCl4-liver fibrosis and inhibitory effects of Jiaqi Ganxian granule. Molecules. 2016;21:698. doi: 10.3390/molecules21060698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chang H., Meng H.Y., Liu S.M., Wang Y., Yang X.X., Lu F., Wang H.Y. Identification of key metabolic changes during liver fibrosis progression in rats using a urine and serum metabolomics approach. Sci. Rep. 2017;7:1–12. doi: 10.1038/s41598-017-11759-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mücke V.T., Thomas D., Mücke M.M., Waidmann O., Zeuzem S., Sarrazin C., Pfeilschifter J., Vermehren J., Finkelmeier F., Grammatikos G. Serum sphingolipids predict de novo hepatocellular carcinoma in hepatitis C cirrhotic patients with sustained virologic response. Liver Int. 2019:1–10. doi: 10.1111/liv.14178. [DOI] [PubMed] [Google Scholar]
- 111.Krautbauer S., Wiest R., Liebisch G., Buechler C. Associations of systemic sphingolipids with measures of hepatic function in liver cirrhosis are related to cholesterol. Prostaglandins Other Lipid Mediat. 2017;131:25–32. doi: 10.1016/j.prostaglandins.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 112.Duan Z.P. Plasma sphingolipids as potential indicators of hepatic necroinflammation in patients with chronic hepatitis C and normal alanine aminotransferase level. PLoS ONE. 2014;9:e95095. doi: 10.1371/journal.pone.0095095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Attwa M.H., El-Etreby S.A. Guide for diagnosis and treatment of hepatocellular carcinoma. World J. Hepatol. 2015;7:1632–1651. doi: 10.4254/wjh.v7.i12.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.El-Serag H.B., Marrero J.A., Rudolph L., Reddy K.R. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology. 2008;134:1752–1763. doi: 10.1053/j.gastro.2008.02.090. [DOI] [PubMed] [Google Scholar]
- 115.Forner A., Llovet J.M., Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245–1255. doi: 10.1016/S0140-6736(11)61347-0. [DOI] [PubMed] [Google Scholar]
- 116.Li Z., Guan M., Lin Y., Cui X., Zhang Y., Zhao Z., Zhu J. Aberrant lipid metabolism in hepatocellular carcinoma revealed by liver lipidomics. Int. J. Mol. Sci. 2017;18:2550. doi: 10.3390/ijms18122550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Takashima Y., Horisawa K., Udono M., Ohkawa Y., Suzuki A. Prolonged inhibition of hepatocellular carcinoma cell proliferation by combinatorial expression of defined transcription factors. Cancer Sci. 2018;109:3543–3553. doi: 10.1111/cas.13798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hajj C., Becker-flegler K.A., Haimovitz-friedman A. Novel mechanisms of action of classical chemotherapeutic agents on sphingolipid pathways. Biol. Chem. 2015;396:669–679. doi: 10.1515/hsz-2014-0302. [DOI] [PubMed] [Google Scholar]
- 119.Bonnaud S., Niaudet C., Legoux F., Corre I., Delpon G., Saulquin X. Sphingosine-1-Phosphate Activates the AKT Pathway to Protect Small Intestines from Radiation-Induced Endothelial Apoptosis. Ther. Targets Chem. Biol. 2010;70:9905–9915. doi: 10.1158/0008-5472.CAN-10-2043. [DOI] [PubMed] [Google Scholar]
- 120.Carroll B., Donaldson J.C., Obeid L. Sphingolipids in the DNA damage response. Adv. Biol. Regul. 2015;58:38–52. doi: 10.1016/j.jbior.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Liu Y., Yu-Teh L. Ceramide Glycosilation Catalyzed by Glucosylceramide Synthase and Cancer Drug Resistance. Adv. Cancer Res. 2013;117:59–89. doi: 10.1016/B978-0-12-394274-6.00003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gómez-muñoz A., Kong J.Y., Salh B., Steinbrecher U.P., Duffy P.A., Martin A., Brien L.O., Byun H., Pharmacol D.N.B.M., Frago L.M., et al. Ceramide-1-phosphate blocks apoptosis through inhibition of acid sphingomyelinase in macrophages. J. Lipid Res. 2004;45:99–105. doi: 10.1194/jlr.M300158-JLR200. [DOI] [PubMed] [Google Scholar]
- 123.Gangoiti P., Granado M.H., Wei S., Kong J.Y., Steinbrecher U.P., Gómez-muñoz A. Ceramide 1-phosphate stimulates macrophage proliferation through activation of the PI3-kinase/PKB, JNK and ERK1/2 pathways. Cell. Signal. 2008;20:726–736. doi: 10.1016/j.cellsig.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 124.Kolesnick R., Altieri D., Fuks Z. A CERTain Role for Ceramide. Cancer Cell. 2007:473–475. doi: 10.1016/j.ccr.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 125.Swanton C., Marani M., Pardo O., Warne P.H., Kelly G., Sahai E., Chang J., Temple J., Ahmed A.A., Brenton J.D., et al. Article Regulators of Mitotic Arrest and Ceramide Metabolism Are Determinants of Sensitivity to Paclitaxel and Other Chemotherapeutic Drugs. Cancer Cell. 2007;11:498–512. doi: 10.1016/j.ccr.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 126.Ogretmen B. Sphingolipid metabolism in cancer signalling and therapy. Nat. Rev. Cancer. 2018;18:33–50. doi: 10.1038/nrc.2017.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bose R., Verheij M., Haimovitz-friedman A., Scotto K., Fuks Z., Kolesnick R. Ceramide Synthase Mediates Daunorubicin-lnduced Apoptosis: An Alternative Mechanism for Generating Death Signals. Cell. 1995;82:405–414. doi: 10.1016/0092-8674(95)90429-8. [DOI] [PubMed] [Google Scholar]
- 128.Dumitru C.A., Sandalcioglu I.E., Wagner M., Weller M., Gulbins E. Lysosomal ceramide mediates gemcitabine-induced death of glioma cells. J. Mol. Med. 2009;87:1123–1132. doi: 10.1007/s00109-009-0514-8. [DOI] [PubMed] [Google Scholar]
- 129.Lacour S., Hammann A., Grazide S., Lagadic-Gossmann D., Athias A., Sergent O., Laurent G., Gambert P., Solary E., Dimanche-Boitrel M.-T. Cisplatin-induced CD95 redistribution into membrane lipid rafts of HT29 human colon cancer cells. Cancer Res. 2004;64:3593–3598. doi: 10.1158/0008-5472.CAN-03-2787. [DOI] [PubMed] [Google Scholar]
- 130.Min J., Stegner A.L., Alexander H., Alexander S. Overexpression of Sphingosine-1-Phosphate Lyase or Inhibition of Sphingosine Kinase in Dictyostelium discoideum Results in a Selective Increase in Sensitivity to Platinum-Based Chemotherapy Drugs. Eukaryot. Cell. 2004;3:795–805. doi: 10.1128/EC.3.3.795-805.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Min J., Mesika A., Sivaguru M., Van Veldhoven P.P., Alexander H., Futerman A.H., Alexander S. (Dihydro)ceramide Synthase 1 – Regulated Sensitivity to Cisplatin Is Associated with the Activation of p38 Mitogen-Activated Protein Kinase and Is Abrogated by Sphingosine Kinase 1. Mol. Cancer Res. 2007;5:801–813. doi: 10.1158/1541-7786.MCR-07-0100. [DOI] [PubMed] [Google Scholar]
- 132.Cabot M.C., Han T., Giuliano A.E. The multidrug resistance modulator SDZ PSC 833 is a potent activator of cellular ceramide formation. FEBS Lett. 1998;431:185–188. doi: 10.1016/S0014-5793(98)00744-3. [DOI] [PubMed] [Google Scholar]
- 133.Xie R., Nguyen S., Mckeehan W.L., Liu L. Acetylated microtubules are required for fusion of autophagosomes with lysosomes. BMC Cell Biol. 2010;11:89. doi: 10.1186/1471-2121-11-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Savic R., Xingxuan H., Fiel I., Schuchman E.H. Recombinant Human Acid Sphingomyelinase as an Adjuvant to Sorafenib Treatment of Experimental Liver Cancer. PLoS ONE. 2013;8:1–13. doi: 10.1371/journal.pone.0065620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Berasain C. Hepatocellular carcinoma and sorafenib: too many resistance mechanisms? Gut. 2013;62:1674–1675. doi: 10.1136/gutjnl-2013-304564. [DOI] [PubMed] [Google Scholar]
- 136.Freeman B.A., Crapo J.D. Biology of disease: free radicals and tissue injury. Lab. Investig. 1982;47:412–426. [PubMed] [Google Scholar]
- 137.Jackson S.P., Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461:1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kim D., Kim S., Kleuser B., Scha M., Kim K., Park K. Sphingosine-1-phosphate inhibits human keratinocyte proliferation via Akt / protein kinase B inactivation. Cell. Signal. 2004;16:89–95. doi: 10.1016/S0898-6568(03)00114-1. [DOI] [PubMed] [Google Scholar]
- 139.Matsuda Y., Wakai T., Hirose Y., Osawa M., Fujimaki S. p27 Is a Critical Prognostic Biomarker in Non-Alcoholic Steatohepatitis-Related Hepatocellular Carcinoma. Int. J. Mol. Sci. 2013;14:23499–23515. doi: 10.3390/ijms141223499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yin Y., Xu M., Gao J., Li M. Alkaline ceramidase 3 promotes growth of hepatocellular carcinoma cells via regulating S1P/S1PR2/PI3K/AKT signaling. Pathol. Res. Pr. 2018;214:1381–1387. doi: 10.1016/j.prp.2018.07.029. [DOI] [PubMed] [Google Scholar]
- 141.Osawa Y., Nagaki M., Banno Y., Nozawa Y., Moriwaki H., Nakashima S. Sphingosine Kinase Regulates Hepatoma Cell Differentiation: Roles of Hepatocyte Nuclear Factor and Retinoid Receptor. Biochem. Biophys. Res. Commun. 2001;286:673–677. doi: 10.1006/bbrc.2001.5451. [DOI] [PubMed] [Google Scholar]
- 142.Martínez-chantar M.L., García-Trevijano E.R., Latasa M.U., Martín-Duce A., Fortes P., Caballería J., Ávila M.A., Mato J.M. Methionine Adenosyltransferase II Beta Subunit Gene Expression Provides a Proliferative Advantage in Human Hepatoma. Gastroenterology. 2003;124:940–948. doi: 10.1053/gast.2003.50151. [DOI] [PubMed] [Google Scholar]
- 143.Zubiete-franco I., García-rodríguez J.L., Lopitz-otsoa F., Serrano-macia M., Simon J., Fernández-tussy P., Barbier-torres L., Fernández-ramos D., Gutiérrez-de-juan V., López S., et al. SUMOylation regulates LKB1 localization and its oncogenic activity in liver cancer. EBioMedicine. 2019;40:406–421. doi: 10.1016/j.ebiom.2018.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ruckhäveberle E., Rody A., Engels K., Gaetje R., von Minckwitz G., Schiffman S., Grösch S., Geisslinger G., Holtrich U., Karn T., et al. Microarray analysis of altered sphingolipid metabolism reveals prognostic significance of sphingosine kinase 1 in breast cancer. Breast Cancer Res. Treat. 2008:41–52. doi: 10.1007/s10549-007-9836-9. [DOI] [PubMed] [Google Scholar]
- 145.Liu S., Su Y., Qin M., Mao Y., Huang J., Tang G. Sphingosine kinase 1 promotes tumor progression and confers malignancy phenotypes of colon cancer by regulating the focal adhesion kinase pathway and adhesion molecules. Int. J. Oncol. 2013;42:617–626. doi: 10.3892/ijo.2012.1733. [DOI] [PubMed] [Google Scholar]
- 146.Nagahashi M., Ramachandra S., Kim E.Y., Allegood J.C., Rashid O.M., Yamada A., Zhao R., Milstien S., Zhou H., Spiegel S., et al. Sphingosine 1-phosphate produced by sphingosine kinase 1 promotes breast cancer progression by stimulating angiogenesis and lymphangiogenesis. Cancer Res. 2012;72:726–735. doi: 10.1158/0008-5472.CAN-11-2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Spiegel S., Milstien S. The outs and the ins of sphingosine-1-phosphate in immunity. Nat. Rev. Immunol. 2011;11:403–415. doi: 10.1038/nri2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Barbier-torres L., Beraza N., Fernández-tussy P., Lopitz- F., Fernández-ramos D., Zubiete-franco I., Varela-rey M., Teresa C., Gutiérrez V., Anguita J., et al. Histone Deacetylase 4 promotes cholectatic liver injury in the absence of Prohibitin-1. Hepatology. 2015;62:1237–1248. doi: 10.1002/hep.27959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Barbier-torres L., Delgado T.C., García-rodríguez J.L., Fernández-ramos D., Buqué X., Cano A., Boix L., Bruix J., Villa E., Castro A., et al. Stabilization of LKB1 and Akt by neddylation regulates energy metabolism in liver cancer. Oncotarget. 2015;6 doi: 10.18632/oncotarget.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Critelli R., Milosa F., Faillaci F., Condello R., Turola E., Marzi L., Lei B., Dituri F., Andreani S., Sighinolfi P., et al. Microenvironment inflammatory infiltrate drives growth speed and outcome of hepatocellular carcinoma: a prospective clinical study. Cell Death Dis. 2017;8:e3017. doi: 10.1038/cddis.2017.395. [DOI] [PMC free article] [PubMed] [Google Scholar]