Abstract
Infants and children are at higher risk than adolescents and adults for exposure to environmental toxins via ingestion for a number of reasons: their smaller size (and proportionately larger dose of ingested toxins), their closer proximity to the ground, dirt, and indoor dust, their boundless curiosity and oral exploratory behaviors, pica habits that may persist into school-age for children with autism or other developmental delays, their proportionately larger daily water and milk intake, and food preferences that differ markedly from adolescents and adults. Children depend on adults to protect them and keep their home environment safe. Pediatric care providers can integrate environmental health topics into their well-child care practices, offering guidance and resources to parents concerned with reducing the risks to their children posed by hazards in their homes, daycare centers, preschools, schools, and the other environments in which they spend time.
Children are more vulnerable to the ingestion of environmental toxins than adults for a variety of reasons, including differences in size, behaviors, diet, and even where they spend their day. Children breathe more air, drink more water, and eat more food per kilogram of body weight than adults. This results in greater exposures per kilogram of body weight to any contaminants in the air, water, or food compared with adults. In the 2015 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS), there were 56,798 human exposure cases secondary to unintentional environmental exposures, representing 2.6% of all human exposure cases.1 Fifty (4%) deaths were secondary to unintentional environmental exposures, and 28% of these deaths were in people younger than age 20 years.1 Table 1 shows the typical environmental chemicals and metals that can be encountered every day by children living in hazardous environments.
TABLE 1.
Commonly Ingested Environmental Toxins and Their Household Sources
| Environmental Toxin | Household Source(s) |
|---|---|
| Bisphenols | Residues in foods |
| Flame retardants (polybrominated diphenyl ethers) | Foam-filled sofas, household interior dust |
| Formaldehyde | Compressed wood products |
| Lead | Paint, plaster, household dust, exterior dirt, plumbing, tap water, imported herbs and spices, imported cosmetics, ethnic home health remedies,“take-home” occupational lead |
| Methyl mercury | Fish and other seafood |
| Other metals (cadmium, mercury, arsenic) | Herbs and spices, ethnic home health remedies, well water (arsenic) |
| Perfluoroalkyl substances | Food, food packaging, carpeting finishes, contaminated water supplies, household dust, deteriorating nonstick-coated cookware |
| Pesticides | Insect sprays, cockroach killers, ant traps, rodent baits, residues in foods |
| Polychlorinated and polybrominated biphenyls, dioxin | Fish and other seafood |
INGESTED ENVIRONMENTAL TOXINS: WHY ARE CHILDREN AT HIGH RISK?
Ground-Level Size
Because infants and children are smaller than adolescents and adults, they will get a larger dose per unit size of chemicals they are exposed to in their environment. Crawling infants and toddlers live closer to the ground than older children and adults. They can be more exposed to chemical-containing household dust on their hands or feet from the floor or on carpeting. Indoor use of pesticides, for example, usually involves the spraying of chemicals along the edges of the floors, a place where infants and toddlers spend much of their time. Mouse baits and ant traps are placed in room corners, where infants and toddlers can grab and try to ingest them. In the 2015 NPDS report, pesticides accounted for the eighth and ninth most common category of substances for pediatric (age ≤5 years) and human exposure inquiries, respectively.1 In 2015, 42% of all human exposure cases involving pesticide (n = 83,483) exposure were in children age 5 years or younger.1
Oral Exploratory Behaviors
Infants and toddlers have “hard-wired” oral exploratory behaviors that include putting nonfood objects, including new toys, in their mouths. Thumb-sucking, a comfort-seeking behavior, is a common manifestation of the toddler’s oral habits. Such oral exploratory behaviors put them at high risk of ingesting foreign objects, such as paint or plaster chips (Figure 1), ant or rodent baits, or toxin-containing household dust. Such behaviors start to extinguish by age 3 to 4 years in otherwise typically developing children.
Figure 1.
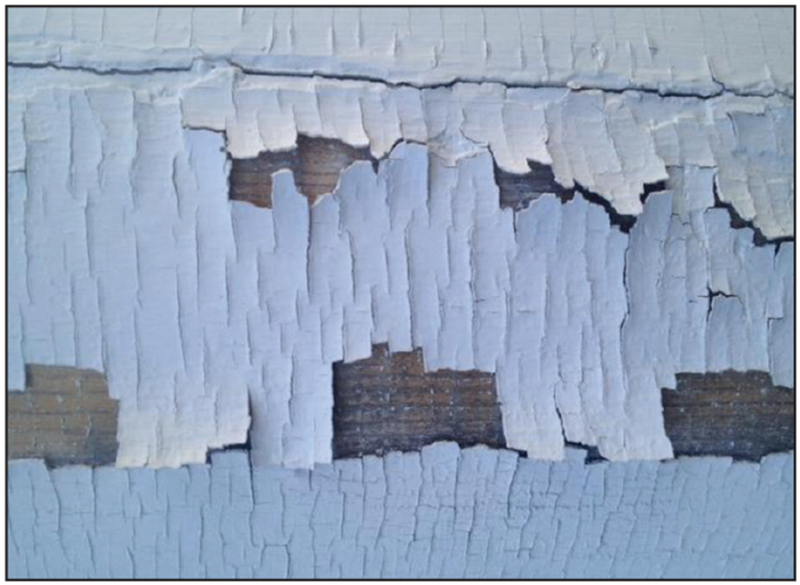
Example of peeling lead paint. The toxic chips can be ingested by infants and toddlers.
Pica
Toddlers lack the cognitive abilities to discriminate “food” from “nonfood” items to be put in their mouth, the condition known as pica. The Environmental Protection Agency (EPA) estimates that young children consume on average 200 to 800 mg of dirt daily.2 If playground dirt is contaminated with lead or other bioavailable contaminants, then children can be exposed while playing in bare dirt areas. Indoors, pica and mouthing behaviors lead to increased exposure to dust that may harbor lead, polybrominated diphenyl ethers (PBDEs), or perfluoroalkyl substances (PFAS).3 Persistent pica behaviors are linked to certain medical conditions, such as iron deficiency anemia and sickle cell disease. Children with developmental disorders such as autism may have a higher propensity for pica persisting into later childhood and even adolescence.
Water and Diet
Children drink proportionately more water per unit size than adolescents and adults. Older infants may drink up to 28 to 32 ounces of water daily if their powdered formula is reconstituted with tap water.4 Infants and toddlers drink much more milk as an important component of their nutrition than do adolescents or adults. Some environmental chemicals, such as PFAS, have been shown to pass into breast-milk and to the infant during lactation.5 Infants can also be exposed to contaminants if breast-feeding mothers are using certain imported breast creams that contain mercury. However, the American Academy of Pediatrics continues to recommend breast-feeding as the preferred choice for the first year of an infant’s life.6
Children also have different dietary preferences than do adults, eating proportionately more fruits and fruit juices and less meats and vegetables. Products containing rice, a typical first food and major ingredient in various infant foods, can often contain inorganic arsenic and may contribute to an infant’s arsenic exposure.7
Susceptible Populations
Some subgroups of children are especially susceptible to the ingestion of environmental chemicals. Children living at or below the poverty line who live in older housing are disproportionately at greatest risk of lead poisoning.8
Children with autism spectrum disorder or other developmental delays may have persistent mouthing behaviors and pica well into the school-age years. These children continue to be candidates for lead poisoning from eating paint chips, dirt, or mouthing home items laden with lead-containing dust.9
HOUSEHOLD SOURCES OF CONTAMINATION
Water
Access to safe drinking water is essential to the health of children, but water contamination events involving both public municipal supplies as well as private wells still occur. Well water can be contaminated by a number of naturally occurring chemicals, including arsenic, copper, and manganese. It can also be contaminated by man-made sources, such as lead in water mains, service pipes, school drinking fountains and bubblers, household indoor plumbing, pesticide run-off, perchlorates, nitrates from the agricultural use of fertilizers, and PFAS from contaminated groundwater. Municipal water supplies can also be contaminated by the above contaminants, notably lead, PFAS, and other organic and inorganic chemicals.
Diet
Food can be the source of trace chemical residues, such as bisphenols, metals, pesticides, polychlorinated biphenyls (PCBs), PFAS, and other contaminants. Arsenic has been detected in rice products and brown rice syrup, leading to new US Food and Drug Administration (FDA) guidance about limiting the intake of certain rice products in children and women who are pregnant.10 Fish can absorb and store toxins such as mercury, PCBs, and dioxins in their fatty flesh, with higher concentrations in larger predator fish (eg, tuna, swordfish) that are eaten by humans.11,12
Children in some families may be given herbs or ethnic home health remedies by parents who believe supplementation preserves the health of their child. However, some herbs and herbal remedies can be contaminated by metals (such as lead or mercury) or undeclared pharmaceuticals, thereby posing a health risk.13,14
Metals or pesticides can also contaminate imported herbs and spices used in food preparation. One study of Chinese raw herbs detected metals (lead and cadmium) and pesticides (chlorpyrifos) in the plant material itself.15 Another “market basket” study found that Indian spices imported into the United States, such as turmeric, could be contaminated with measurable amounts of lead.16
Environment
Children spend large amounts of their time at school or at play in places such as homes, public or private schools, nurseries or daycare centers, or outdoors in playgrounds where they are playing in bare dirt or sandboxes. It is estimated that preschool children ingest up to 800 mg of dirt during outdoor play.2 The “built environment” can be the source of a child’s toxic exposures if the homes or schools themselves are contaminated or if they are located in a hazardous location such as on or near toxic waste sites, smelters, electrical generation plants, or other industrial or agricultural concerns. All pose significant ingestion hazards to children from contamination by chemicals or other toxins. Residential surfaces and dust can be contaminated by lead, PFAS, indoor pesticides, and PBDEs, as detailed earlier in this review. Although lead-containing interior paints have long been banned in the US, until recently plumbing faucets and taps could contain up to 8% lead and still be labeled as “lead-free.”17 Outdoor soil can contain lead, arsenic, PCBs, and other toxins that can be absorbed through the gastrointestinal tract and become bioavailable when ingested. Lastly, there are limited regulations to identify, track, or remediate environmental hazards in school or childcare settings,18 and there is no federal agency to provide oversight.
Children’s toys or furniture (eg, pewter toys, older cribs containing lead-based paint) can be contaminated with lead. Some household products, such as shower weights (which can contain cobalt), bleach, cleaners and detergent pods, furniture oils and polishes, or button batteries (which may contain corrosive agents) may be accessible to a toddler. There are case reports of children who have been poisoned by lead after ingestion of gold-plated lead medallions, charms, or other lead-containing jewelry.19,20 Mothers wearing imported cosmetics, such as sindoor or kohl, contaminated with metals like lead or mercury may inadvertently put their infants at risk. Imported cookware may not be lead-safe and may contaminate food during cooking.
Parents can bring home lead or other metals in dust on their clothing, and such “take home” exposures pose a significant risk of contaminating both their vehicles and their homes.21–23 Certain adult hobbies, such as making pottery with leaded glazes, using lead solder in making stained glass windows, or handling lead bullets for hunting or marksmanship, can put children at high risk of exposure.24 Families who use ethnic home health remedies or religious practices that incorporate certain powders, cosmetics, or metal implements can risk exposing their children to metals such as lead or mercury.25
HEALTH EFFECTS OF COMMON ENVIRONMENTAL CONTAMINANTS
Arsenic
Arsenic is associated with anemia, gastrointestinal effects, poor appetite, weight loss, and neurotoxicity. It also can affect a developing fetus and cause adverse pregnancy outcomes.26,27
Bisphenol A, Phthalates, and Phytoestrogens
These chemicals are used in plastics, polyvinyl chloride plumbing, personal care products, and thermal/carbonless receipts. Children are exposed to them from ingestion (contaminated food and drink), inhalation, and dermal absorption. In animals, phthalates, bisphenol A, and other phenols interfere with the production and function of hormones. There is ongoing research to determine their health effects in humans.28,29
Flame Retardants (Polybrominated Diphenyl Ethers)
PBDEs are associated with endocrine disruptor and developmental effects in children, although the data are limited.30–32
Formaldehyde
Very low levels of formaldehyde off-gas from certain building materials comprised of pressed wood. This can cause eye, nose, throat, and skin irritation and can trigger asthma exacerbations in sensitized people.33
Lead
Lead is a known neurotoxin associated with developmental delays, lower cognitive function, attention deficits, poor executive function, learning disabilities, and neurobehavioral effects.34–37 It also causes anemia and has effects on bone growth, kidney function, immune competency, and high blood pressure.37
Mercury
Mercury (and methyl mercury) is a known neurotoxin that is associated with developmental delays, behavioral disorders, and learning problems.38,39
Perfluoroalkyl Substances
PFAS is labeled by the EPA as an “emerging pollutant” that in animal models can cause thyroid problems,40 metabolic changes,41 mammary gland abnormalities,42 and some tumors.43
It is also associated with elevated cholesterol and uric acid levels as well as increased rates of kidney and testicular cancers in adults.44 The possible health effects in children are not yet well understood.45,46
Pesticides
Many pesticides, such as organochlorines, organophosphates, and carbamates, are known to be neurotoxic in children.47,48 Others, such as rat baits, can cause bleeding.49 Pyrethrins and pyrethroid agents used indoors to kill cockroaches and ants can exacerbate childhood allergies and asthma and may themselves be neurotoxic.50
Polychlorinated (and Polybrominated) Biphenyls and Dioxin
PCBs, polybrominated biphenyls, and dioxin are known to be endocrine disruptors and associated with systemic effects in children.51
GIVING GUIDANCE TO PARENTS ABOUT THEIR CHILDREN’S HEALTH AND THE ENVIRONMENT
Pediatric health care providers play a pivotal role in educating parents about hazards in the environment of their children and how to avoid them. They also need to make sure that if treatment is warranted that it is done safely and by health care professionals with expertise in toxicology or environmental medicine. Table 2 provides some tips on best practices during routine medical care, and Table 3 gives guidance that primary care practitioners can incorporate into their counseling of families.
TABLE 2.
Tips for Practitioners: Screening for Environmental Toxins
| • Take a good environmental history – ask about family’s housing and age of construction, nearby industry, airports, agriculture, and toxic waste sites |
| • Ask about parental occupations and hobbies – consider“take-home”lead sources for parents engaged in lead-risk occupations (eg, home remodeling and construction, firearms range workers, bridge workers, smelter workers) |
| • Don’t just ask about foods in diet – also ask about the family’s use of imported herbs, dietary supplements, imported spices, and variety in diet, especially during infancy |
| • Don’t just ask about use of medicines – also ask about the family’s use of ethnic home health remedies, powders used in religious worship or rituals, imported cosmetics, cookware |
| • All children should be screened for risk of lead exposures. Follow Centers for Disease Control and Prevention guidance for testing preschool children with periodic blood lead levels |
| • Ask about source of household water, especially for younger formula-fed infants; where a private well is used, ask about frequency of well-water testing |
TABLE 3.
Guidance for Parents: Keep Kids Healthy, Avoid Environmental Toxins
| Possible Source of Toxins | How to Mitigate Exposure |
|---|---|
| Water | • Run tap for first-morning draw 3-5 minutes before using • Install water filtration/purification devices at point of use • Change out older lead-containing plumbing • Test your private well-water for contaminants annually • Clean out faucet aerators |
| Home furnishings | • Throw out old foam-filled furniture • Buy furniture without flame retardants |
| Indoor use of pesticides | • Avoid buying indoor pesticide“foggers”or“bombs” • Avoid using rodent/ant baits/sprays where infants crawl • Use integrated pest management strategies |
| Food | • Wash raw fruits and vegetables in soapy water • If affordable, buy selected organic fruits and vegetables, especially those whose skin is consumed. • If affordable, buy organically-raised, antibiotic-free meats • Eat a well-balanced diet and a variety of grains beyond rice and rice-containing products. • Maximize children’s dietary sources of iron, calcium, magnesium, vitamin D • Follow FDA guidance to limit children’s and pregnant women’s consumption of certain methyl mercury and PCB-containing fish and other seafood |
| Indoor paint, plaster, and dust | • Frequent dusting of window sills, baseboards, furniture • Frequent damp mopping of wood, linoleum, or tile floors • Wash plastic toys frequently • Use a HEPA vacuum on carpets and floors • Cover peeling interior paint or chipping plaster with duct tape or contact paper • Careful, frequent handwashing • Leave shoes at home’s threshold • Get your home or apartment inspected for lead • Use certified lead abatement contractor to remediate • Avoid starting renovation projects in pre-1970s homes/apartments until it has been inspected and determined to be free of lead contamination hazards |
Abbreviations: FDA, US Food and Drug Administration; HEPA, high efficiency particulate air; PCB, polychlorinated biphenyl.
CONCLUSIONS
Children and families are often confronted with hazardous environmental chemicals in trace amounts, which can undermine feelings of safety in their own home. The challenges of everyday life include limiting the extent of childhood exposures to chemicals that can affect their health both now and in the future.
Acknowledgments
Grant: This article was supported by the cooperative agreement award U61TS000237-04 from the Agency for Toxic Substances and Disease Registry (ATSDR). The U.S. Environmental Protection Agency (EPA) supports the Pediatric Environmental Health Specialty Unit (PEHSU) by providing funds to ATSDR under Inter-Agency Agreement DW-75-95877701.
Footnotes
Publisher's Disclaimer: Disclaimer: The article contents are the responsibility of the authors and do not necessarily represent the official views of the ATSDR. Neither the EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications.
Disclosure: The authors have no relevant financial relationships to disclose.
Contributor Information
Marissa Hauptman, Harvard-wide Health Services Pediatrics Research Fellow; a Pediatrician and Pediatric Environmental Health Specialist, Region 1 New England Pediatric Environmental Health Specialty Unit (PEHSU) and Pediatric Environmental Health Center; and an Instructor of Pediatrics, Harvard Medical School.
Alan D. Woolf, Director, Region 1 New England Pediatric Environmental Health Specialty Unit, and the Medical Director, Pediatric Environmental Health Center; and a Professor of Pediatrics, Harvard Medical School.
REFERENCES
- 1.Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd annual report. Clin Toxicol (Phila). 2016;54(10):924–1109. doi: 10.1080/15563650.2016.1245421. [DOI] [PubMed] [Google Scholar]
- 2.Binder S, Sokal D, Maughan D. Estimating soil ingestion: the use of tracer elements in estimating the amount of soil ingested by young children. Arch Environ Health. 1986;41(6):341–345. [DOI] [PubMed] [Google Scholar]
- 3.Lanphear BP, Roghmann KJ. Pathways of lead exposure in urban children. Environ Res. 1997;74(1):67–73. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics. Amount and schedule of formula feedings. https://www.healthychildren.org/English/ages-stages/baby/feeding-nutrition/Pages/Amount-and-Schedule-of-Formula-Feedings.aspx. Accessed November 28, 2017.
- 5.Mogensen UB, Grandjean P, Nielsen F, Weihe P, Budtz-Jorgensen E. Breastfeeding as an exposure pathway for perfluorinated alkylates. Environ Sci Technol. 2015;49(17):10466–10473. doi: 10.1021/acs.est.5b02237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. Policy statement: breastfeeding and the use of breast milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 7.Karagas MR, Punshon T, Sayarath V, Jackson BP, Folt CL, Cottingham KL. Association of rice and rice-product consumption with arsenic exposure early in life. JAMA Pediatr. 2016;170(6):609–616. doi: 10.1001/jamapediatrics.2016.0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raymond J, Wheeler W, Brown MJ. Lead screening and prevalence of blood lead levels in children aged 1-2 years – child blood lead surveillance system, United States, 2002-2010 and National Health and Nutrition Examination Survey, United States, 1999-2010 (supplement). MMWR Morb Mortal Wkly Rep. 2014;63(2):36–42. [PubMed] [Google Scholar]
- 9.George M, Heeney MM, Woolf AD. Encephalopathy from lead poisoning masquerading as a flu-like syndrome in an autistic child. Pediatr Emerg Care. 2010;26(5):370–373. doi: 10.1097/PEC.0b013e3181db2237. [DOI] [PubMed] [Google Scholar]
- 10.Lai PY, Cottingham KL, Steinmaus C, Karagas MR, Miller MD. Arsenic and rice: translating research to address health care providers’ needs. J Pediatr. 2015;167(4):797–803. doi: 10.1016/j.jpeds.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cladis P, Kleiner AC, Santerre CR. Mercury content in commercially available finfish in the United States. J Food Prot. 2014;77:1361–1366. doi: 10.4315/0362-028X.JFP-14-097. [DOI] [PubMed] [Google Scholar]
- 12.Manning TM, Roach AC, Edge KJ, Ferrell DJ. Levels of PCDD/Fs and dioxin-like PCBs in seafood from Sydney Harbour, Australia. Environ Poll. 2017;224:590–596. doi: 10.1016/j.envpol.2017.02.042. [DOI] [PubMed] [Google Scholar]
- 13.Boyer EW, Kearney S, Shannon MW, Quang L, Woolf A, Kemper K. Poisoning from a dietary supplement administered during hospitalization. Pediatrics. 2002;109(3):E49. [DOI] [PubMed] [Google Scholar]
- 14.Woolf AD, Hussain J, McCullough L, Petranovic M, Chomchai C. Infantile lead poisoning from an Asian tongue powder: a case report & subsequent public health inquiry. Clin Toxicol (Phila). 2008;46(9):841–844. doi: 10.1080/15563650801898536. [DOI] [PubMed] [Google Scholar]
- 15.Harris ES, Cao S, Littlefield BA, et al. Heavy metal and pesticide content in commonly prescribed individual raw Chinese herbal medicines. Sci Total Environ. 2011;409(20):4297–4305. doi: 10.1016/j.scitotenv.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin CG, Schaider LA, Brabander DJ, Woolf AD. Pediatric lead exposure from imported Indian spices and cultural powders. Pediatrics. 2010;125(4):e828–35. doi: 10.1542/peds.2009-1396. [DOI] [PubMed] [Google Scholar]
- 17.US Environmental Protection Agency. Basic information about lead in drinking water. https://www.epa.gov/ground-water-and-drinking-water/basic-information-about-lead-drinking-water. Accessed November 28, 2017.
- 18.Paulson JA, Barnett CL. Public health stops at the school house door. Environ Health Perspect. 2016;124(10):A171–A175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Lead poisoning of a child associated with use of a Cambodian amulet --- New York City, 2009. MMWR Morb Mortal Wkly Rep. 2011;60(3):69–71. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Death of a child after ingestion of a metallic charm--Minnesota, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(12):340–341. [PubMed] [Google Scholar]
- 21.Beaucham C, Page E, Alarcon WA, et al. Indoor firing ranges and elevated blood lead levels-United States, 2002-2013. MMWR Morb Mortal Wkly Rep. 2014;63(16):347–351 [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC). Occupational and take-home lead poisoning associated with restoring chemically stripped furniture—California, 1998. MMWR Morb Mortal Wkly Rep. 2001;50(13):246–248. [PubMed] [Google Scholar]
- 23.Staudinger KC, Roth VS. Occupational lead poisoning. Am Fam Physician. 1998;57(4):719–732. [PubMed] [Google Scholar]
- 24.Goldman RH, Woolf AD, Karwowski M. Gun marksmanship and youth lead exposure: a practice oriented approach to prevention. Clin Pediatr (Phila). 2017;56(11):1068–1071. doi: 10.1177/0009922817701177. [DOI] [PubMed] [Google Scholar]
- 25.Woolf AD, Hussain J, McCullogh L, Petranovic M, Chomchai C. Infantile lead poisoning from an Asian tongue powder: a case report and subsequent public health inquiry. Clin Toxicol (Phil). 2008;46(7):841–844. doi: 10.1080/15563650801898536. [DOI] [PubMed] [Google Scholar]
- 26.Farzan SF, Gossai A, Chen Y, Chasan-Taber L, Baker E, Karagas M. Maternal arsenic exposure and gestational diabetes and glucose intolerance in the New Hampshire birth cohort study. Environ Health. 2016;15(1):106. doi: 10.1186/s12940-016-0194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilbert-Diamond D, Emond JA, Baker ER, Korrick SA, Karagas MR. Relation between in utero arsenic exposure and birth outcomes in a cohort of mothers and their newborns from New Hampshire. Environ Health Perspect. 2016;124(8):1299–1307. doi: 10.1289/ehp.1510065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolff MS, Teitelbaum SL, McGovern K, et al. Phthalate exposure and pubertal development in a longitudinal study of U.S. girls. Hum Reprod. 2014;29(7):1558–1566. doi: 10.1093/humrep/deu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teitelbaum SL, Mervish N, Moshier EL, et al. Associations between phthalate metabolite urinary concentrations and body size measures in New York City children. Environ Res. 2012;112:186–193. doi: 10.1016/j.envres.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Herbstman JB, Sjodin A, Kurzon M, et al. Prenatal exposure to PBDEs and neurodevelopment. Environ Health Perspect. 2010;118(5):712–719. doi: 10.1289/ehp.0901340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eskenazi B, Chevrier J, Rauch SA, et al. In utero and childhood polybrominated diphenyl ether (PBDE) exposures and neurodevelopment in the CHAMACOS study. Environ Health Perspect. 2013;121(2)251–262. doi: 10.1289/ehp.1205597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harley KG, Rauch SA, Chevrier J, et al. Association of prenatal and childhood PBDE exposure with timing of puberty in boys and girls. Environ Int. 2017;100:132–138. doi: 10.1016/j.envint.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agency for Toxic Substances and Disease Registry. Formaldehyde - ToxFAQs. https://www.atsdr.cdc.gov/toxfaqs/tfacts111.pdf. Accessed November 28, 2017.
- 34.Canfield RL, Kreher DA, Cornwell C, Henderson CR Jr., Low-level lead exposure, executive functioning, and learning in early childhood. Child Neuropsychol. 2003;9(1):35–53. doi: 10.1076/chin.9.1.35.14496. [DOI] [PubMed] [Google Scholar]
- 35.Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nigg JT, Knottnerus GM, Martel MM, et al. Low blood lead levels associated with clinically diagnosed attention-deficit/hyperactivity disorder and mediated by weak cognitive control. Biol Psychiatry. 2008;63(3):325–331. doi: 10.1016/j.biopsych.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.President’s Task Force on Environmental Health Risks and Safety Risks to Children. Key federal programs to reduce childhood lead exposures and eliminate associated health impacts. https://ptfceh.niehs.nih.gov/features/assets/files/key_federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf. Accessed November 16, 2017.
- 38.Oken E, Radesky JS, Wright RO, et al. Maternal fish intake during pregnancy, blood mercury levels, and child cognition at age 3 years in a US cohort. Am J Epidemiol. 2008;167(10): 1171–1181. doi: 10.1093/aje/kwn034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Debes F, Budtz-Jorgensen E, Weihe P, White RF, Grandjean P. Impact of prenatal methylmercury exposure on neurobehavioral function at age 14 years. Neurotoxicol Teratol. 2006;28(5):536–547. doi: 10.1016/j.ntt.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 40.Chang SC, Thibodeaux JR, Eastvold ML, et al. Thyroid hormone status and pituitary function in adult rats given oral doses of perfluorooctanesulfonate (PFOS). Toxicology. 2008;243:330–339. doi: 10.1016/j.tox.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 41.White SS, Calafat AM, Kuklenyik Z, et al. Gestational PFOA exposure in mice is associated with altered mammary gland development in dams and female offspring. Toxicol Sci. 2007;96:133–144. doi: 10.1093/toxsci/kfl177. [DOI] [PubMed] [Google Scholar]
- 42.Hines EP, White SS, Stanko JP, Gibbs-Flournoy EA, Lau C, Fenton SE. Phenotypic dichotomy following developmental exposure to perfluorooctanoic acid (PFOA) in female CD-1 mice: low doses induced elevated serum leptin and insulin, and overweight in mid-life. Mol Cell Endocrinol. 2009;304:97–105. doi: 10.1016/j.mce.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy G, Butenhoff J, Olsen G, et al. The toxicology of perfluoro-octanoate. Crit Rev Toxicol. 2004;34(4): 351–384. [DOI] [PubMed] [Google Scholar]
- 44.Agency for Toxic Substances Disease Registry. An overview of perfluoroalkyl and perfluoroalkyl substances and interim guidance for clinicians responding to patient exposure concerns. https://www.atsdr.cdc.gov/pfc/docs/pfas_clinician_fact_sheet_508.pdf. Accessed November 16, 2017.
- 45.Fleisch AF, Rifas-Shiman SL, Mora AM, et al. Early-life exposure to perfluoroalkyl substances and childhood metabolic function. Environ Health Perspect. 2017;125(3):481–487. doi: 10.1289/EHP303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Braun JM, Chen A, Romano ME, et al. Prenatal perfluoroalkyl substance exposure and child adiposity at 8 years of age: the HOME study. Obesity (Silver Spring). 2016;24(1):231–237. doi: 10.1002/oby.21258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roberts JR, Karr CJ; Council on Environmental Health, American Academy of Pediatrics. Pesticide exposure in children. Pediatrics. 2012;130(6):e17645–e1788. doi: 10.1542/peds.2012-2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Council on Environmental Health. Policy statement: pesticide exposure in Children. Pediatrics. 2012;130(6):e1757–e1763. doi : 10.1542/peds.2013-0576. [DOI] [PubMed] [Google Scholar]
- 49.Kendrick DB. Mosquito repellents and superwarfarin rodenticides–are they really toxic in children? Curr Opin Pediatr. 2006;18(2):180–183. doi: 10.1097/01.mop.0000193273.54742.6f. [DOI] [PubMed] [Google Scholar]
- 50.Müller-Mohnssen H Chronic sequelae and irreversible injuries following acute pyrethroid intoxication. Toxicol Lett. 1999;107:161–175. [DOI] [PubMed] [Google Scholar]
- 51.Engel SM, Wolff MS. Causal inference considerations for endocrine disruptor research in children’s health. Annu Rev Public Health. 2013;34:139–158. doi: 10.1146/annurev-publhealth-031811-124556. [DOI] [PMC free article] [PubMed] [Google Scholar]


