Abstract
Purpose
Circulating microRNAs (miRNAs) have shown the potential for non-invasive diagnosis of various types of malignancies at an early stage. The aim of the study was to explore the feasibility of a combination of 8 serum miRNAs related to non-small-cell lung cancer (NSCLC) with the corresponding serum exosomal miRNAs in early diagnosis for the patients with NSCLC.
Methods
We measured 8 serum miRNAs and the corresponding serum exosomal miRNAs including miR-21-5p, miR-126-3p, miR-141-3p, miR-146a-5p, miR-155-5p, miR-222-3p, miR-223-3p, and miR-486-5p in 48 patients with early NSCLC at stages I/II, 32 patients with lung benign lesion (LBL), and 48 healthy control (HC) by quantitative real-time polymerase chain reaction (qRT-PCR).
Results
The expression levels of 4 serum miRNAs including miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p, and 2 serum exosomal miRNAs including miR-146a-5p and miR-486-5p in the early NSCLC group were significantly different from that in the LBL group and the HC group (P < 0.01). The areas under the receiver operating characteristic curves (AUC) of the 4 serum miRNAs and 2 serum exosomal miRNAs in the early NSCLC group were ≥0.697, of which serum exosomal miR-146a-5p and miR-486-5p were 0.813 and 0.886, respectively, and higher than that of the 4 serum miRNAs. Additionally, a combination of 4 serum miRNAs with 2 serum exosomal miRNAs improved the AUC to 0.960 for the patients with NSCLC at early stages, with a sensitivity of 85.42% and a specificity of 92.50%.
Conclusion
This study suggests that serum exosomal miRNAs other than serum miRNAs might be preferable biomarkers for the patients with NSCLC at early stages, and a combination of serum miRNAs with serum exosomal miRNAs contributes to the further improvement of early diagnosis for NSCLC.
Keywords: serum, exosome, microRNA, non-small-cell lung cancer, early diagnosis
Introduction
Lung cancer is a malignant tumor with the highest morbidity and mortality worldwide, seriously endangering human health.1 As a predominant type of lung cancer, non-small-cell lung cancer (NSCLC) accounts for approximately 85% of all lung cancers, including adenocarcinoma (AC), squamous cell carcinoma (SCC), and large cell carcinoma (LCC).2 Due to the absence of apparent symptoms at an early stage, most patients with NSCLC miss the best opportunity for surgical treatment, leading to a dismal 5-year survival rate of 5–15%, while the 5-year survival rate of NSCLC patients receiving surgical resection at an early stage have been reported to be high for 50–70%.3 Therefore, improving the early diagnosis efficiency is very important for the prognosis of patients with NSCLC. However, the current routine screening programme has insufficient capacity for the early diagnosis of NSCLC and needs to be improved. For example, conventional-dose computed tomography (CT) in imaging has insufficient ability for screening and differentiating benign and malignant pulmonary nodules, while low-dose CT demonstrates problems such as high false positive rates and overdiagnosis.4,5 The current serum tumor antigen markers have rather deficient sensitivity or specificity for NSCLC, which limits their clinical application, especially in early diagnosis.6,7
MicroRNAs (miRNAs) are a class of small, endogenous, highly conserved non-coding RNAs with a length of approximately 19–25 nucleotides and which participate in the regulation of cell differentiation, proliferation, and apoptosis through the post-transcriptional regulation of gene expression.8,9 Studies have shown that some miRNAs may be aberrantly expressed in tumor tissues and are closely associated with the occurrence and development of malignancies. Additionally, miRNAs can be released into the sera, providing valuable markers for the non-invasive diagnosis of malignancies.10 Other than serum miRNAs, miRNAs existing in tumor-related serum exosomes have received extensive attention in recent years. As extracellular vesicles in body fluids including plasma, serum, urine, etc., exosomes are found to be rich with miRNAs and other biological molecules.11 Due to the protection of the lipid bilayer, exosomal miRNAs have higher stability compared with serum miRNAs. Therefore, whether serum exosomal miRNAs might be more valuable for the early diagnosis of various malignancies, such as NSCLC, is worth exploring.
In this study, 8 common serum miRNA markers related to NSCLC were selected: miR-21-5p, miR-126-3p, miR-141-3p, miR-146a-5p, miR-155-5p, miR-222-3p, miR-223-3p, and miR-486-5p. There have been many reports on the application of these 8 serum miRNAs for NSCLC diagnosis;12–17 however, there are few studies of the 8 serum miRNAs for the early diagnosis of NSCLC, while the diagnostic values of the corresponding serum exosomal miRNAs in patients with NSCLC at early stages have not yet been reported. This study aims to investigate the value of combined detection of two forms of miRNA in serum for the early diagnosis of NSCLC patients by simultaneous detection of 8 serum miRNAs and 8 corresponding serum exosomal miRNAs in early NSCLC patients.
Materials and Methods
Study Subjects
Forty-eight patients with NSCLC, 32 patients with benign lung lesions (LBL), and 48 healthy controls (HC) were recruited from March 2016 to July 2018 at Fujian Provincial Hospital. All patients met the diagnostic standards recognized by international or professional societies and none of the patients had accepted any treatment for the malignancy; the clinical and pathological data are shown in Table 1. There were 48 people in the HC group; participants in this group received health examinations from the physical examination centre of Fujian Provincial Hospital and showed no evidence of disease, including malignancies, LBL, etc. Each subject was informed about the study, and informed consent was obtained. Five milliliters of peripheral blood were collected before the surgery and the serum was separated immediately and stored at −80°C before use. This study was approved by the Institutional Review Board of Fujian Provincial Hospital, and all participants provided written informed consent.
Table 1.
Clinical Data for the Early NSCLC, LBL and HC Groups
| NSCLC (n = 48) |
LBL (n = 32) |
HC (n = 48) |
P value | |
|---|---|---|---|---|
| Age (years) | 59.42 ± 12.04 | 59.87 ± 12.76 | 51.01 ± 5.07 | 0.984 |
| Sex (%) | ||||
| Male | 33(68.75) | 20(62.50) | 27(56.25) | 0.449 |
| Female | 15(31.25) | 12(37.50) | 21(43.75) | |
| Smoking history (%) | 21(43.75) | 15(46.86) | 19(39.59) | 0.804 |
| Pathological classification (%) | ||||
| AC | 33(68.75) | |||
| SCC | 13(27.08) | |||
| LCC | 2 (4.17) | |||
| Staging (%) | ||||
| I | 36(75.00) | |||
| II | 12(25.00) | |||
| LBL (%) | ||||
| pneumonia | 16(50.00) | |||
| Lung abscess | 3 (9.38) | |||
| Pneumonia nodule |
8 (25.00) |
|||
| Tuberculosis | 4 (12.50) | |||
| Pulmonary hamartoma |
1 (3.12) |
Abbreviations: NSCLC, non-small-cell lung cancer; LBL, lung benign lesion; HC, healthy control; AC, adenomcarcinoma; SCC, squamous cell carcinoma; LCC, large cell carcinoma.
Serum miRNA Extraction
Serum RNA (including miRNA) was extracted using an extraction kit (CoWin Biosciences, Beijing). A total of 1 mL of TRIzol reagent was added into 200 µL of serum and mixed thoroughly. Extraction was in strict accordance with the kit instructions, and the extracted RNA was stored at −80°C before use.
Serum Exosome Extraction and Exosomal miRNA Purification
The serum exosome was extracted with an exosome extraction kit (Umibio Shanghai). A total of 500 µL serum was centrifuged at 3000 rpm for 10 min at 4°C. The supernatant was transferred to a new centrifuge tube and was centrifuged again at 12,000 rpm for 20 min at 4°C to remove impurities in the sample. Exosome concentration solution (250 µL) was added into the impurity-free supernatant, and extraction and purification were performed according to the instruction manual. The exosomal miRNA was extracted with an miRNA extraction kit (CoWin Biosciences, Beijing). TRIzol reagent (1 mL) was added to the purified exosomes; the mixture was vortexed thoroughly and then incubated at room temperature for 5 min. Chloroform (200 µL) was added; the mixture was vortexed thoroughly and then incubated at room temperature for 5 min. After centrifugation at 12,000 rpm for 15 min, the supernatant was transferred to an RM adsorption column. Ethanol (100%; 1/3 supernatant volume) was added; the mixture was vortexed thoroughly and then centrifuged at 12,000 rpm for 30 s. After centrifugation, the supernatant was transferred to an RS adsorption column, and 100% ethanol (2/3 supernatant volume) was added. The mixture was vortexed thoroughly and then centrifuged at 12,000 rpm for 30 s. After adding wash buffer, the mixture was centrifuged twice at 12,000 rpm for 30 s. RNase-free water (30 µL) was added to the RS adsorption column, and the mixture was centrifuged at 12,000 rpm for 30 s. The bottom solution was collected and stored at −80°C before use.
Transmission Electron Microscopy (TEM)
Purified exosomes were were treated with 2% glutaraldehyde at 4°C for 2 h. After being washed 4 times with PBS, exosomes were fixed with 1% osmium tetroxide for 2 h, and washed twice with ddH2O. Then, the exosomes were dehydrated with gradient ethanol and acetone, fixed in 2% glutaraldehyde at 4°C for 2 h, and washed with phosphate-buffered saline (PBS) 4 times. Finally, exosomes were immersed, embedded, and polymerized with ethoxyline resin to prepare slices at a thickness of 0.5 mm. After being stained with uranium acetate and lead citron citrate, exosomes were observed under a TEM.
Western Blot Assay
After determining the protein concentration of the purified exosome solution using a bicinchoninic acid (BCA) kit, protein samples were mixed with the same amount of loading buffer and denatured at 99°C for 5 min. Sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE, 12.5%) was performed, and the samples were transferred to a polyvinylidene fluoride (PVDF) membrane. The samples were blocked with 5% skimmed milk for 1 h and washed with Tris-buffered saline containing 0.2–0.4% Tween-20 (TBST) 3 times. Exosome-targeting antibodies CD9 (1:1000, ab92726), CD63 (1:1000, ab134045), and TSG101 (1:1000, ab125011) were added, respectively, and the membrane was incubated at 4°C overnight. After washing with TBST 3 times, horseradish peroxidase-conjugated goat anti-rabbit IgG was added and incubated at room temperature in the dark for 1 h. A chemiluminescence kit (Thermo Fisher, USA) was used for colour development, and a gel imager was used to take photos.
Nano Sight Detection
ZetaView (Particle Metrix, Germany) was used to detect the distribution of exosome size, and all parameters remained unchanged during the detection process. PBS (200 μL) was used to resuspend the exosome granules, and a 0.22-μm syringe was used to filter the sample. Each sample was diluted with distilled water to the appropriate detection range of the instrument to allow counting. ZetaView SP2 software was used for analysis and photography.
Expression Levels of Serum miRNAs and Serum Exosomal miRNAs by qRT-PCR
Mir-X miRNA First-Strand Synthesis and SYBR quantitative real-time polymerase chain reaction (qRT-PCR) kits (Takara, Japan) were used for the synthesis of complementary DNA (cDNA) and the real-time fluorescence quantitative PCR amplification, respectively. Synthesis of cDNA was conducted in strict accordance with the instruction manual. The PCR system was as follows (25 μL): SYBR Advantage Premix, 12.5 μL; forward primer, 0.5 μL; reverse primer, 0.5 μL; template DNA, 2 μL; ddH2O, 9 μL; and ROX Dye, 0.5 μL. The reaction conditions were as follows: pre-denaturation at 95°C for 10 s and 40 cycles of denaturation at 95°C for 5 s and annealing at 60°C for 20 s. For each sample, 3 duplicated wells were used for miRNA detection. U6 was used as an internal reference, and the expression level of miRNA was expressed as 2–ΔΔct, where ΔΔCt = experimental group (Cttarget gene − CtU6) − control group (Cttarget gene − CtU6). The primers were designed and synthesized by Shanghai Sanggong Biotech Co., Ltd.
Statistical Analysis
GraphPad Prism 5 was used to generate the figures, and IBM SPSS 23.0 software was used for statistical analysis. Quantitative data are expressed as the mean ± standard deviation (SD). The Mann–Whitney U-test, a non-parametric test, was used to compare quantitative data between groups. MedCalc version 12.0 software was used for the receiver operating characteristic (ROC) curve, and the area under the ROC curve (AUC) was used to evaluate the diagnostic efficacy of each indicator. P < 0.05 was considered statistically significant.
Results
Expression Levels of Serum miRNAs
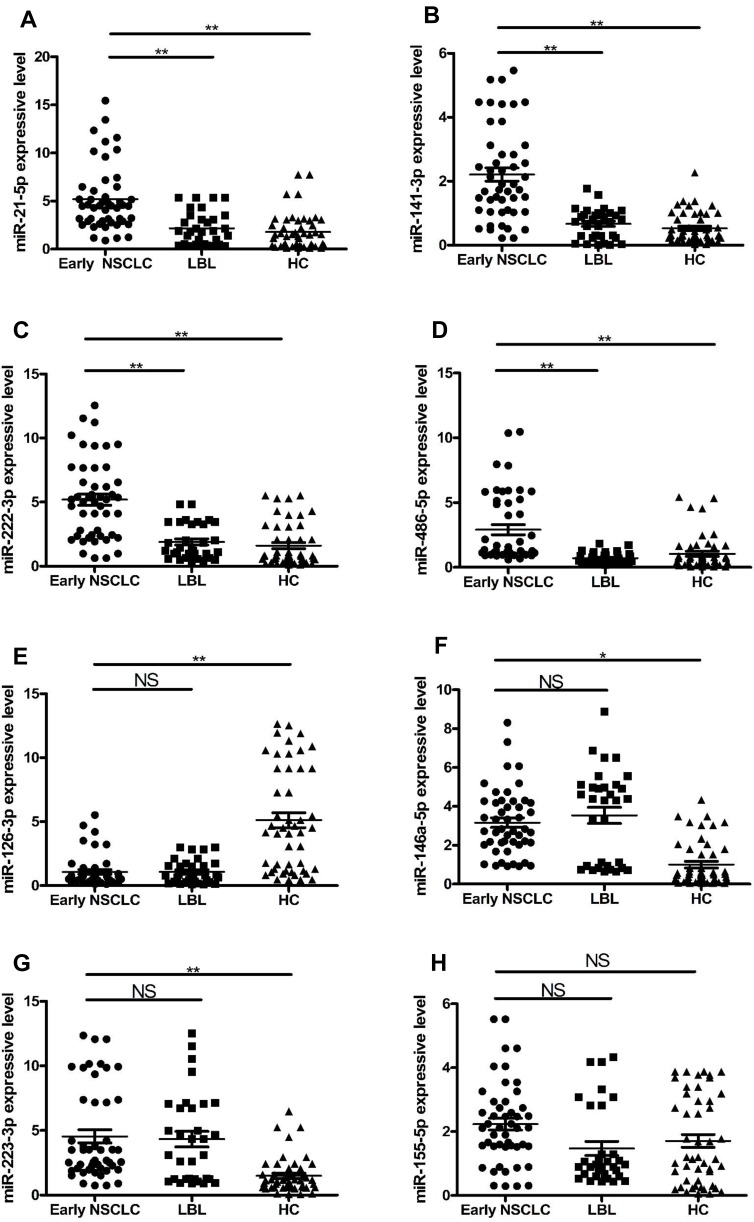
The qRT-PCR results showed that the levels of serum miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p in the early NSCLC group were significantly different from those in the LBL and HC groups (P < 0.01) (Figure 1). In the early NSCLC group, the expressions of serum miR-21-5p, miR-141-3p, and miR-222-3p, miR-486-5p were significantly upregulated. The levels of serum miR-146a-5p, and miR-223-3p in the early NSCLC group were significantly higher than those in the HC group (P < 0.05, P < 0.01), but not significantly different from those in the LBL group (P > 0.05). The levels of serum miR-126-3p were significantly lower than those in the HC group (P < 0.01), but not significantly different from those in the LBL group (P > 0.05). The level of serum miR-155-5p was not significantly different from those in the LBL and HC groups (P > 0.05).
Figure 1.
Expression levels of 8 serum miRNAs in early NSCLC, LBL and HC groups.
Notes: *, ** indicate P < 0.05, P < 0.01, respectively.
Abbreviations: NSCLC, non-small-cell lung cancer; LBL, lung benign lesion; HC, healthy control; NS, no significance.
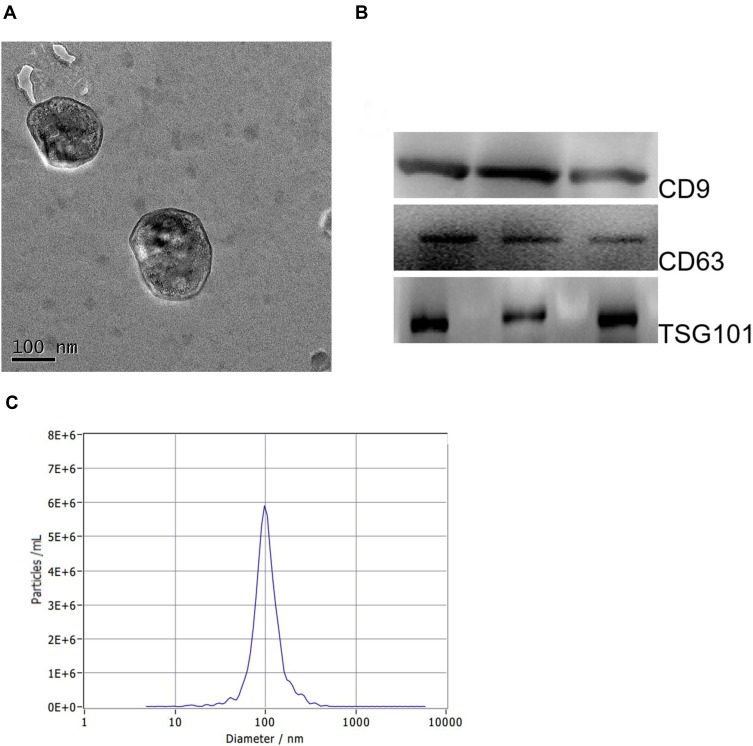
Identification of Exosomes
TEM showed that exosomes had a clear membrane structure with a diameter of about 100 nm (Figure 2A). The structural characteristics of the exosomes were consistent with previous reports. The presence of exosomal markers (CD9, CD63 and TSG101) was also confirmed by Western blot (Figure 2B). Nano Sight analysis indicated that the average diameter of the exosomes was 100 nm (Figure 2C).
Figure 2.
Identification of serum exosomes from early NSCLC group.
Notes: (A) The morphology of serum exosomes, TEM, scale 100 nm; (B) Western blot results show that the exosomal marker proteins TSG101, CD9, and CD63 are present in exosomes; (C) Nano Sight results show that the mean diameter of the exosome granules is approximately 100 nm.
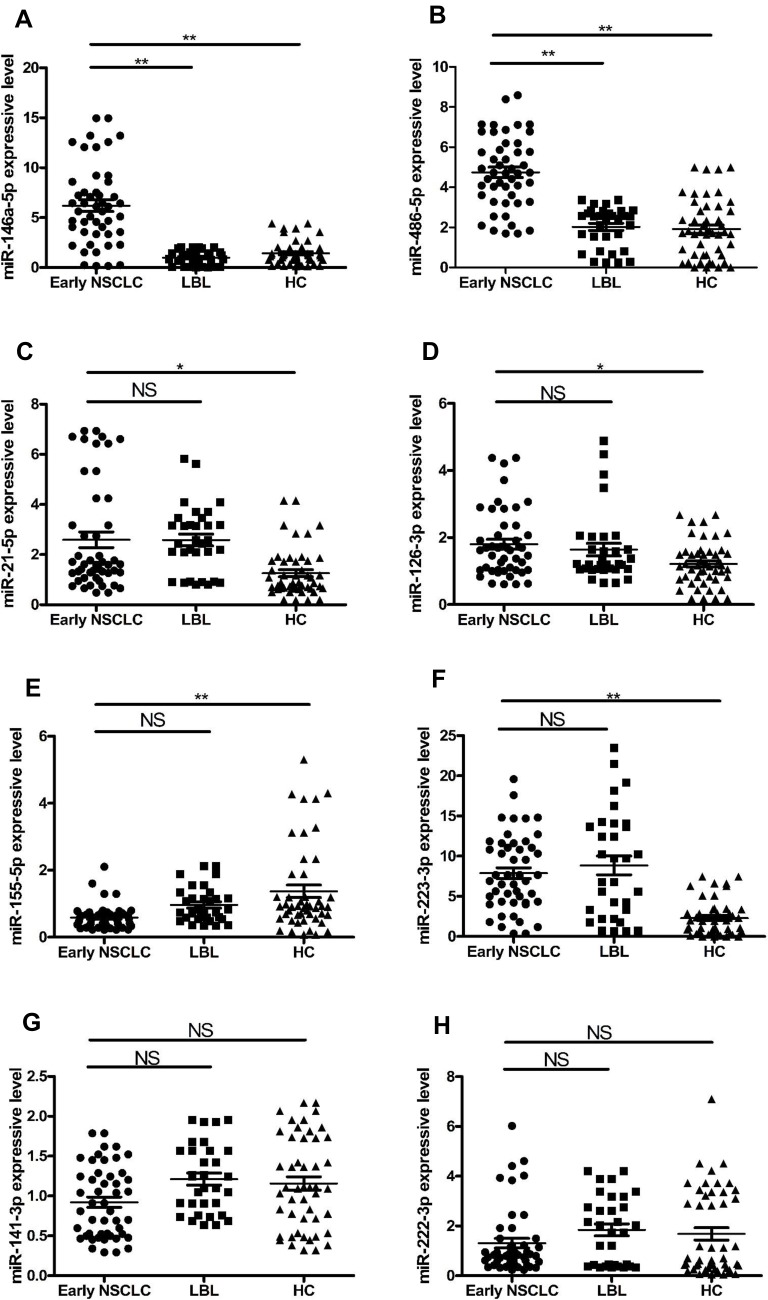
Expression Levels of Serum Exosomal miRNAs
The qRT-PCR results showed that the levels of serum exosomal miR-146a-5p and miR-486-5p in the early NSCLC group were significantly higher than those in the LBL and HC groups (P < 0.01) (Figure 3). The levels of serum exosomal miR-21-5p, miR-126-3p, and miR-223-3p in the early NSCLC group were significantly higher than those in the HC group (P < 0.05, P < 0.05, P < 0.01), but not significantly different from those in the LBL group (P > 0.05). The levels of serum exosomal miR-155-5p were significantly lower than those in the HC group (P < 0.01), but not significantly different from those in the LBL group (P > 0.05). The levels of serum exosomal miR-141-3p and miR-222-3p were not significantly different from those in the LBL and HC groups (P > 0.05).
Figure 3.
Expression levels of 8 serum exosomal miRNAs in early NSCLC, LBL and HC groups.
Notes: *, ** indicate P < 0.05, P < 0.01, respectively.
Abbreviations: NSCLC, non-small-cell lung cancer; LBL, lung benign lesion; HC, healthy control; NS, no significance.
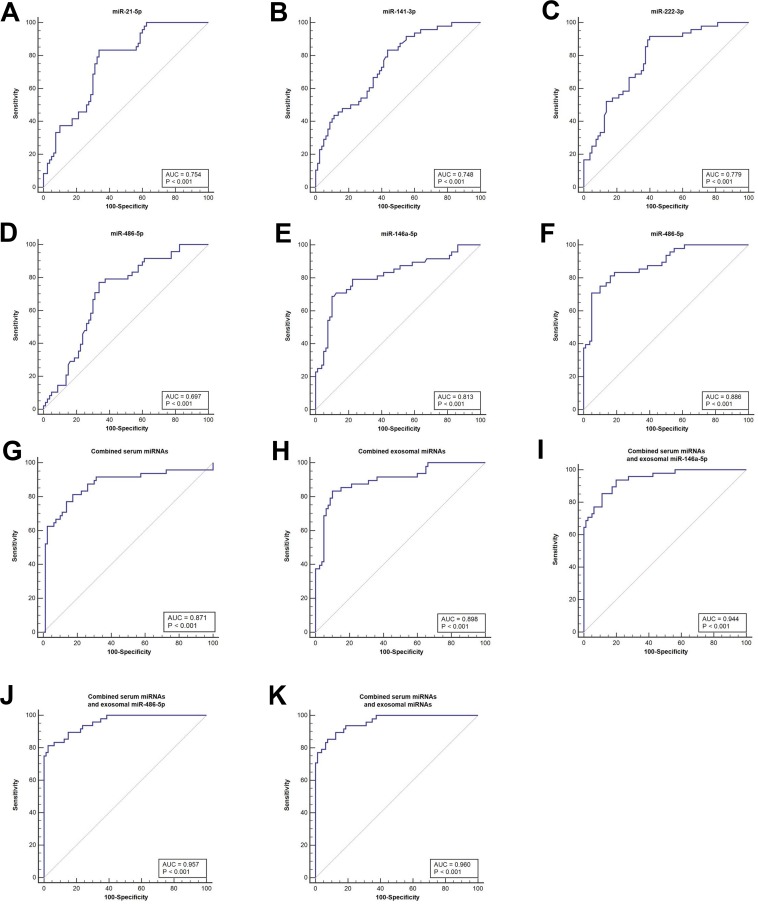
Diagnostic Performances of Serum and Exosomal miRNAs in Patients with Early NSCLC
The AUCs of the 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p) and 2 serum exosomal miRNAs (miR-146a-5p and miR-486-5p) in the early NSCLC group were ≥ 0.697. ROC analysis was conducted in the diagnostic performances of the aberrantly expressed 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p) and 2 exosomal miRNAs (miR-146a-5p and miR-486-5p) in the patients with NSCLC at early stages. ROC curves are shown in Figure 4, and the results are summarized in Tables 2 and 3. The data showed that for the patients with NSCLC at early stages, the AUC of serum miR-486-5p was 0.697, and the other 3 serum miRNAs were >0.700, of which miR-222-3p had the highest AUC of 0.779 (95% CI 0.697–0.847), with a sensitivity of 91.67% and a specificity of 60.00%. The AUC of the combination of 4 serum miRNAs was up to 0.871. The AUCs of serum exosomal miR-146a-5p and miR-486-5p were 0.813 and 0.886, respectively, and the AUC of the combination of 2 serum exosomal miRNAs was 0.898. Among 4 serum miRNAs and 2 serum exosomal miRNAs, the positive predictive value (PPV), negative predictive value (NPV) and agreement rate (AR) scores of serum exosomal miR-486-5p were the highest. Among the 3 combinations of 4 serum miRNAs with serum exosomal miR-146a-5p and/or miR-486-5p, the combination of 4 serum miRNAs with serum exosomal miR-146a-5p and miR-486-5p had the highest diagnostic performance for early NSCLC, with an AUC of 0.960, a sensitivity of 85.42% and a specificity of 92.50%, and the PPV, NPV and AR scores were 87.20%, 91.40% and 89.82%, respectively.
Figure 4.
ROC curves for aberrantly expressed miRNAs and ability to diagnose the patients with NSCLC at early stages.
Notes: (A–D) ROC curves for serum miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p. (E and F) ROC curves for serum exosomal miR-146a-5p and miR-486-5p. (G) ROC curve for the combined detection of 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, miR-486-5p). (H) ROC curve for the combined detection of 2 serum exosomal miRNAs (miR-146a-5p, miR-486-5p). (I) ROC curve for the combined detection of 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, miR-486-5p) with serum exosomal miR-146a-5p. (J) ROC curve for the combined detection of 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, miR-486-5p) with serum exosomal miR-486-5p. (K) ROC curve of the combined detection of 4 serum miRNAs (miR-21-5p, miR-141-3p, miR-222-3p, miR-486-5p) with serum exosomal miR-146a-5p and miR-486-5p. ROC, receiver operating characteristic.
Table 2.
Comparison of the Performance of Serum miRNAs and serum Exosomal miRNAs in Diagnosing the Patients with NSCLC at Early Stages
| Marker | AUC | SE | 95% CI | P Value |
|---|---|---|---|---|
| Serum miR-21-5p | 0.754 | 0.0423 | 0.670 - 0.825 | <0.0001 |
| Serum miR-141-3p | 0.748 | 0.0432 | 0.664 - 0.821 | <0.0001 |
| Serum miR-222-3p | 0.779 | 0.0408 | 0.697 - 0.847 | <0.0001 |
| Serum miR-486-5p | 0.697 | 0.0468 | 0.610 - 0.775 | <0.0001 |
| Combined serum miRNAs | 0.871 | 0.0374 | 0.800 - 0.923 | <0.0001 |
| Exosomal miR-146a-5p | 0.813 | 0.0421 | 0.735 - 0.877 | <0.0001 |
| Exosomal miR-486-5p | 0.886 | 0.0304 | 0.817 - 0.935 | <0.0001 |
| Combined exosomal miRNAs | 0.898 | 0.0301 | 0.832 - 0.945 | <0.0001 |
| Combined serum miRNAs + exosomal miR-146a-5p |
0.944 | 0.0193 | 0.889 - 0.977 | <0.0001 |
| Combined serum miRNAs + exosomal miR-486-5p |
0.957 | 0.0160 | 0.906 - 0.985 | <0.0001 |
| Combined serum miRNAs + exosomal miRNAs |
0.960 | 0.0152 | 0.910 - 0.987 | <0.0001 |
Notes: Combined serum miRNA=serum miR-21-5p+serum miR-141-3p+ serum miR-222-3p + serum miR-486-5p; Combined exosomal miRNA= exosomal miR-146a-5p+ exosomal miR-486-5p
Abbreviations: NSCLC, non-small-cell lung cancer; AUC, area under the curve; SE, standard error; CI, confidence interval.
Table 3.
Diagnostic Index of Serum miRNAs and serum Exosomal miRNAs in Diagnosing the Patients with NSCLC at Early Stages
| Marker | Sensitivity (%) | Specificity (%) | FPR (%) | FNR (%) | PPV (%) | NPV (%) | AR (%) |
|---|---|---|---|---|---|---|---|
| Serum miR-21-5p | 83.33 | 66.25 | 33.75 | 16.67 | 59.70 | 86.90 | 72.65 |
| Serum miR-141-3p | 83.33 | 56.25 | 43.75 | 16.67 | 53.30 | 84.90 | 66.41 |
| Serum miR-222-3p | 91.67 | 60.00 | 40.00 | 8.33 | 57.90 | 92.30 | 71.86 |
| Serum miR-486-5p | 77.08 | 66.25 | 33.75 | 22.92 | 57.80 | 82.80 | 70.31 |
| Exosomal miR-146a-5p | 68.75 | 90.00 | 10.00 | 31.25 | 80.50 | 82.80 | 82.03 |
| Exosomal miR-486-5p | 70.83 | 95.00 | 5.00 | 29.17 | 89.50 | 84.40 | 85.94 |
| Combined serum minRNAs | 81.25 | 82.50 | 17.50 | 18.75 | 73.60 | 88.00 | 77.34 |
| Combined exosomal miRNAs | 83.33 | 90.00 | 10.00 | 16.67 | 83.30 | 90.00 | 87.50 |
| Combined serum miRNAs + exosomal miR-146a-5p |
85.42 | 88.75 | 11.25 | 14.58 | 82.00 | 91.00 | 87.50 |
| Combined serum miRNAs + exosomal miR-486-5p |
81.25 | 97.50 | 2.50 | 18.75 | 95.10 | 89.70 | 91.41 |
| Combined serum miRNAs + exosomal miRNAs |
85.42 | 92.50 | 7.50 | 14.58 | 87.20 | 91.40 | 89.84 |
Notes: Combined serum miRNAs=serum miR-21-5p+serum miR-141-3p+ serum miR-222-3p + serum miR-486-5p; Combined exosomal miRNAs= exosomal miR-146a-5p+ exosomal miR-486-5p.
Abbreviations: FPR, false positive rate; FNR, false negative rate; PPV, positive predictive value; NPV, negative predictive value; AR, agreement rate.
Discussion
Currently, there is a lack of effective screening methods for early NSCLC in clinical practice, resulting in a poor 5-year survival rate in patients. However, detection of circulating miRNAs such as serum miRNAs can help diagnose various malignancies, indicating that circulating miRNAs might be a potential diagnostic marker for early NSCLC patients. Circulating miRNAs in serum include two forms: serum miRNAs and serum exosomal miRNAs. Compared with serum miRNAs, miRNAs in serum exosomes are more stable due to the protection of lipid bilayer. Therefore, whether the combined detection of serum miRNAs with serum exosomal miRNAs contribute to the improvement of diagnosis performance for early NSCLC is worth exploring.
Eight common serum miRNAs including miR-21-5p, miR-126-3p, miR-141-3p, miR-146a-5p, miR-155-5p, miR-222-3p, miR-223-3p, and miR-486-5p selected in this study have been reported to be closely associated with NSCLC diagnosis.12–17 By the simultaneous detection of 8 serum miRNAs and corresponding serum exosomal miRNAs, we found that 4 serum miRNAs including miR-21-5p, miR-141-3p, miR-222-3p, miR-486-5p and 2 serum exosomal miRNAs including miR-146a-5p and miR-486-5p showed good diagnostic values for patients with NSCLC at early stages, and levels in the early NSCLC group were significantly different from those in the LBL and HC groups (P < 0.01), and AUCs for early NSCLC patients were ≥ 0.697. Interestingly, the AUCs of serum exosomal miR-146a-5p and miR-486-5p for early NSCLC patients were 0.813 and 0.886, respectively, which were higher than that of 4 serum miRNAs. As the tumor suppressor genes of NSCLC, miR-146a-5p and miR-486-5p were reported to display aberrant expression in the tumor tissues and sera of NSCLC patients.13,15,18–20 Our study is the first to demonstrate that the performances of serum exosomal miR-146a-5p and miR-486-5p in diagnosing early NSCLC were superior to that of the 2 corresponding serum miRNAs and the other 6 serum miRNAs, suggesting that compared with serum miRNAs, serum exosomal miRNAs might be more valuable in diagnosing early NSCLC. It is believed that with further in-depth research, more serum exosomal miRNA markers with excellent diagnostic performance for early NSCLC patients will be found, applied and transformed clinically.
The sensitivity of a single miRNA is limited. It is worth investigating whether the combined detection of multi-miRNAs can help improve the diagnostic performance of early NSCLC patients. We further carried out combined detection and analysis of 4 serum miRNAs and 2 serum exosomal miRNAs, which demonstrated the diagnostic values for early NSCLC in our study. By comparison and analysis of several different combinations, the panel comprised of 4 serum miRNAs and 2 serum exosomal miRNAs was shown to improve the AUC for early NSCLC patients to 0.960, with sensitivity of 85.42% and specificity of 92.50%, indicating that the combination of serum miRNAs with serum exosomal miRNAs is helpful to further improve the diagnosis of early NSCLC.
Conclusion
Our study reveals the facts as follows: Serum miR-21-5p, miR-141-3p, miR-222-3p, and miR-486-5p and serum exosomal miR-146a-5p and miR-486-5p have good potentials for the early diagnosis of NSCLC. Other than serum miRNAs, serum exosomal miRNA might be preferable biomarkers for patients with NSCLC at early stages, and a combination of serum miRNAs with serum exosomal miRNAs contributes to the further improvement of early diagnosis for NSCLC.
Acknowledgments
This work was supported in part by the Scientific Joint Fund Of High Level Hospital Construction of Fujian Provincial Hospital (Grant No. 2017LHJJ04) to Y. Huang, the Joint Fund Of Science And Technology Innovation of Fujian province (Grant No. 2017Y9069) to Y. Huang, and the Natural Science Foundation of Fujian Province (Grant No. 2019J01176) to Y. Huang.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Freddie B, Jacques F, Isabelle S, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Travis W, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thoracic Oncol. 2011;6(2):244–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jantuslewintre E, Usó M, Sanmartín E, et al. Update on biomarkers for the detection of lung cancer. Lung Cancer. 2012;3(default):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shieh Y, Bohnenkamp M. Low-dose computed tomography for lung cancer screening: clinical and coding considerations. Chest. 2017;152(1):204–209. [DOI] [PubMed] [Google Scholar]
- 5.Aberle DR, Adams AM, Berg CD; National Lung Screening Trial Research Team. et al.. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma S, Shen L, Qian N, Chen K. The prognostic values of CA125, CA199, NSE, and SCC for stage I NSCLC are limited. Cancer Biomark. 2011;10(3–4):155–162. [DOI] [PubMed] [Google Scholar]
- 7.Fujita J, Ohtsuki Y, Bandoh S, et al. Elevation of cytokeratin 19 fragment (CYFRA 21-1) in serum of patients with radiation pneumonitis: possible marker of epithelial cell damage. Respir Med. 2004;98(4):294–300. [DOI] [PubMed] [Google Scholar]
- 8.Heller G, Weinzierl M, Noll C, et al. Genome-wide miRNA expression profiling identifies miR-9-3 and miR-193a as targets for DNA methylation in nonesmallcell lung cancers. Clin Cancer Res. 2012;18:1619–1629. [DOI] [PubMed] [Google Scholar]
- 9.Landi MT, Zhao Y, Rotunno M, et al. MicroRNA expression differentiates histology and predicts survival of lung cancer. Clin Cancer Res. 2010;16:430–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen X, Ba Y, Ma L, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18:997–1006. [DOI] [PubMed] [Google Scholar]
- 11.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2:569–579. [DOI] [PubMed] [Google Scholar]
- 12.Abd-El-Fattah Amal A, Sadik NAH, Shaker OG, et al. Differential microRNAs expression in serum of patients with lung cancer, pulmonary tuberculosis, and pneumonia. Cell Biochem Biophys. 2013;67:875–884. [DOI] [PubMed] [Google Scholar]
- 13.Fabrizio B, Francesco N, Matteo M, et al. A serum circulating miRNA diagnostic test to identify asymptomatic high-risk individuals with early stage lung cancer. EMBO Mol Med. 2011;3:495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernest N, Anna T, Asuka N, et al. A novel serum 4-microRNA signature for lung cancer detection. Sci Rep. 2015;5:12464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rui-Juan W, Yan-Hua Z, Ping W, et al. Serum miR-125a-5p, miR-145 and miR-146a-5p as diagnostic biomarkers in non-small cell lung cancer. Int J Clin Exp Pathol. 2015;8:765–771. [PMC free article] [PubMed] [Google Scholar]
- 16.Yanlong Y, Kai C, Yongchun Z, et al. Application of serum microRNA-9-5p, 21-5p, and 223-3p combined with tumor markers in the diagnosis of non-small-cell lung cancer in Yunnan in southwestern China. Onco Targets Ther. 2018;11:587–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen X, Hu Z, Wang W, et al. Identification of ten serum microRNAs from a genome-wide serum microRNA expression profile as novel noninvasive biomarkers for nonsmall cell lung cancer diagnosis. Int J Cancer. 2012;130(7):1620–1628. [DOI] [PubMed] [Google Scholar]
- 18.Yanaihara N, Caplen N, Bowman E, et al. Unique microRNA molecular profles in lung cancer diagnosis and prognosis. Cancer Cell. 2006;9:189–198. [DOI] [PubMed] [Google Scholar]
- 19.Yang S, Yu-Qing S, Yan-Li L, et al. Direct repression of the oncogene CDK4 by the tumor suppressor miR-486-5p-5p in non-small cell lung cancer. Oncotarget. 2016;7:34011–34021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fei T, Yanting S, Zhenzhu C, et al. Aberrant miR-181b-5p and miR-486-5p-5p expression in serum and tissue of non-small cell lung cancer. Gene. 2016;591:338–343. [DOI] [PubMed] [Google Scholar]