Abstract
Obstetric hemorrhage, with its related complications, remains a significant and often preventable cause of maternal morbidity and mortality. The medical community has made strides in beginning to address the impact of obstetric hemorrhage as a cause of maternal morbidity and mortality with standardized bundles outlining key elements for hospitals to address in order to optimize hemorrhage prevention and management. Changes in definitions, an expansion of the spectrum of causes, variation in interventions and guidelines and lack of innovation are some of the issues that pose ongoing challenges for meaningful risk reduction. Opportunities to support risk reduction include helping to secure necessary resources, building team training and simulation programs, developing interventions targeted at minimizing cognitive biases, and facilitating patient and family support program development.
Keywords: obstetric hemorrhage, maternal morbidity, antepartum hemorrhage, postpartum hemorrhage, intrapartum hemorrhage
Introduction
The medical community has made great strides in thwarting the impact of obstetric hemorrhage as a cause of maternal morbidity and mortality. Large scale efforts at state and national levels have been undertaken such as the California Maternal Quality Care Collaborative (CMQCC),1 the New York State ACOG district II Safe Motherhood Initiative,2 and the National Partnership for Maternal Safety3 to eliminate preventable maternal death, with obstetric hemorrhage being a major area of focus. In the United States, a decline in pregnancy-related mortality from hemorrhage has been seen over the last 30 years with rates of maternal deaths resulting from hemorrhage going from 28.7% in 1987–1990 to 11.4% in 2011–2013.4 However, this rate has been relatively stagnant in the last reported 15 years. (12.5% 1998–2005, 11.4% 2006–2010, 11.4% 2011–2013).4
One wonders why obstetric hemorrhage remains resistant to risk reduction efforts despite many national and international efforts and its high degree of preventability as a cause of death. Without a doubt, the need for structural preparedness, such as access to care, proper training, and availability of a blood bank, remain essential. But even in well-resourced institutions, obstetric hemorrhage remains a quality concern with variations in definitions and management. In this manuscript, we will briefly review obstetric hemorrhage with a focus on areas that may be amenable to further risk reduction efforts.
Background
Obstetric hemorrhage can occur before birth (antepartum or intrapartum hemorrhage), or after birth (postpartum hemorrhage). Postpartum hemorrhage is most commonly early or primary (within the first 24 hrs after birth). Postpartum hemorrhage was traditionally defined as estimated blood loss in excess of 500 mL after a vaginal birth or a loss of greater than 1,000 mL after a cesarean birth.5 However, a current uniform definition of obstetric hemorrhage is lacking. Definitions vary by country, professional society, and specialty, and thresholds for severity and intervention vary as well.6 A recent definition was published by the American College of Obstetricians and Gynecologists’ (ACOG) reVITALize program as
cumulative blood loss greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours after the birth process (includes intrapartum loss) regardless of route of delivery.7
The new definition highlights the importance of cumulative blood loss and can be used to standardize management approaches and data collection. However, one challenge with the new definition should be acknowledged in that blood loss greater than 500 mL in a vaginal delivery is abnormal and should still trigger prompt attention and management. Kerr recommended different definitions for different purposes, such as for diagnosis, intervention, audit, or research.8 While this may seem helpful for each of these purposes, the authors believe that the current inability to capture the useful data for each purpose does not justify seeking different definitions for the same clinical entity. In addition, reaching a consensus on each of these alternative definitions would probably generate the same discord and will not allow meaningful comparisons of data retrieved based on multiple definitions. Reaching agreement on obstetric hemorrhage definitions remains an important issue to resolve.
Etiologies
Causes of primary postpartum hemorrhage have been commonly summarized using the mnemonic 4Ts that stands for Tone, Trauma, Tissue, and Thrombus.
Tone: stands for the lack of tone or atony i.e. uterine atony, which is by far the most common cause of postpartum hemorrhage. It accounts for the majority of PPH cases and is the leading cause of hemorrhage-related mortality (outside the first trimester) followed by uterine rupture, abruptio placenta, and placenta accreta spectrum.4
Trauma: refers to lacerations along the birth canal sustained during the birth process, most commonly in the perineum and vagina and less often in the cervix, or laceration of blood vessels (e.g. uterine artery) during cesarean section. It also includes uterine inversion that usually occurs with umbilical cord traction, before placental separation, causing the uterus to invert within the birth canal. The treatment of lacerations is most commonly suturing, and that of uterine inversion is often manual replacement.
Tissue: refers to retained placental tissue or membranes, and it requires identification through ultrasound or manual examination, and evacuation of that tissue often surgically via curettage of the uterus.
Thrombus: refers to the diminished ability of the blood to clot properly due to different constitutional deficits (e.g. hemophilia) or acquired disease (e.g. consumptive coagulopathy). This may be recognized prior to birth when preparations can be made accordingly or unknown in which case it should be raised in the differential diagnosis in a case where bleeding is not imputed to the 3 categories of causes listed above.
Secondary postpartum hemorrhage (after 24 hrs of birth until 12 weeks postpartum) is a rare but important contributor to morbidity and mortality.9 Its causes include the ones for primary hemorrhage in addition to subinvolution of the placental bed, endometritis, arteriovenous malformation and pseudoaneurysm. In some cases, a cause may not be identified. Primary postpartum hemorrhage will be the focus of the remainder of this manuscript.
Risk Reduction Opportunities
Obstetric hemorrhage remains the leading direct cause of maternal death worldwide. It is the fourth cause of pregnancy-related deaths in the United States. Data suggests that it is also on the rise in many countries.10 A primary prevention approach that targets risk factors at the national (e.g. reduction of cesarean section) level is considered ideal. However, these large scale efforts will be challenging and slow to implement, and the impact will be significantly delayed. While working on large scale efforts, primary prevention of hemorrhage and hemorrhage-related morbidities must remain a priority on a national, state-wide, local and institutional level. At the institutional level, primary prevention is subject to the challenges of quality improvement, from creating urgency and buy-in to issues of resources or team training and communication. Opportunities for risk reduction were examined by different entities; below 2 critical examinations are summarized: when examining cases of massive transfusion in the Anesthesia Closed Claims Project, obstetric hemorrhage accounted for 8% of cases in the database (National Anesthesia Clinical Outcome Registry) and it was the primary damaging event in 9.6% of obstetric cases.11 Most of the opportunities to improve care revolved around communication between the anesthesiologist and obstetric provider leading to delays in recognition, transfusion or return to the operating room.11
A recent quality improvement review of cases of maternal death from obstetric hemorrhage by the California Pregnancy-Associated Mortality Review Committee showed that all action domains, as defined by the Alliance for Innovation on Maternal Heath (see below) had opportunities for improvement. Readiness could be improved through practice standardization, better organization of equipment and planning for care of women with hemorrhage risk factors. Recognition could be improved through accurate assessment of blood loss and early clinical signs of deterioration. Response could be improved through reducing delays in administering blood, seeking consultations, transferring women to higher levels of care within or outside of the facility, and moving on to other treatments if a woman does not respond to current treatment.12 Adopting a framework for risk reduction, such as the example above, can be useful in the approach of these opportunities for improvement.
Consequences
There are multiple, varied potential clinical consequences of obstetric hemorrhage. Excessive blood loss can lead to severe anemia which contributes to tissue and organ hypoxia/ischemia. This can result in potential organ damage, need for transfusion and contributes to severe maternal morbidity and mortality. Recently, an obstetric comorbidity index was validated.13,14 It includes acute heart failure, acute liver disease, acute myocardial infarction, acute renal failure, acute respiratory failure, coagulopathy/ disseminated intravascular coagulation (DIC), coma, delirium, puerperal cerebrovascular disorders, pulmonary edema, pulmonary embolism, sepsis, shock, status asthmaticus, and status epilepticus. Using the co-morbidity index, Merriam et al showed that in the presence of postpartum hemorrhage and/or transfusion, maternal morbidity was higher, and it was increasing over time.15 Using the Centers for Disease Control and Prevention (CDC) measure of severe maternal morbidity (SMM) – an extensive collection of medical and surgical diagnosis and procedure codes - that they previously validated, Main et al demonstrated the association of hemorrhage with SMM at a baseline of 6.8 to 7.5 per 100 hemorrhage cases (transfusion excluded).16 More importantly, they showed that SMM was amenable to reduction through a state-wide collaborative effort.16 These publications highlight the fact that obstetric hemorrhage can have serious, sometimes irreversible, consequences and that further risk reduction efforts are paramount, feasible and impactful.
Triggers for Review and Quality Measures
Amount of Blood Loss
The lack of agreement on what constitutes an obstetric hemorrhage might be the first impediment to the proper capture of cases. Even if we agree on the amount of blood lost that defines obstetric hemorrhage (e.g. 1000 mL), the current way this loss is captured still commonly relies on estimation. Current efforts to quantify blood loss, by using calibrated collection bags, gravimetric or colorimetric techniques are laudable but to date no demonstrable improvement in outcomes has been clearly shown from these efforts.17 However, many benefits can be drawn from the quantification of blood loss including mitigation of the tendency to revise blood loss after an unexpected hematocrit is resulted, or avoiding inconsistent and subjective triggering of maternal hemorrhage interventions based on a total perceived blood loss.
Transfusion
Transfusion has commonly been used as an indicator of severity and as a quality measure. The lack of agreement on transfusion cut-offs except in extreme cases, and the variation in individual transfusion thresholds makes it difficult to adopt transfusion as a quality measure. However, transfusion can and should be used as a trigger for case review, followed by sound adjudication about the care provided, and a dissection of areas for improvement (e.g. issues with communication or readiness, delay in diagnosis or response).18
In summary, using a certain amount of blood loss to define severe hemorrhage (e.g. 1500 mL) or a predefined amount of blood transfusion (e.g. 4 RBCs) to trigger a review seems to be a reasonable approach. However, adjudication on the clinical care provided in these cases will be important to assess quality.19
Proposed Interventions for Risk Mitigation
Risk mitigation and quality improvement are often confounded. Despite having different goals, this overlap is often acceptable and even laudable as it fits a model of total quality improvement. Risk mitigation is often directed towards ensuring structural preparedness and a leveled playing field for institutions and providers. While the goals risk mitigation may be more restricted than those of quality improvement, the shared tools and strategies may have far-reaching effects and are often easily applied. In the following paragraphs, we will review some clinical and non-clinical strategies to mitigate risk in obstetric hemorrhage.
Clinical Strategies (Individual): Preparedness, Recognition, Response, Reporting
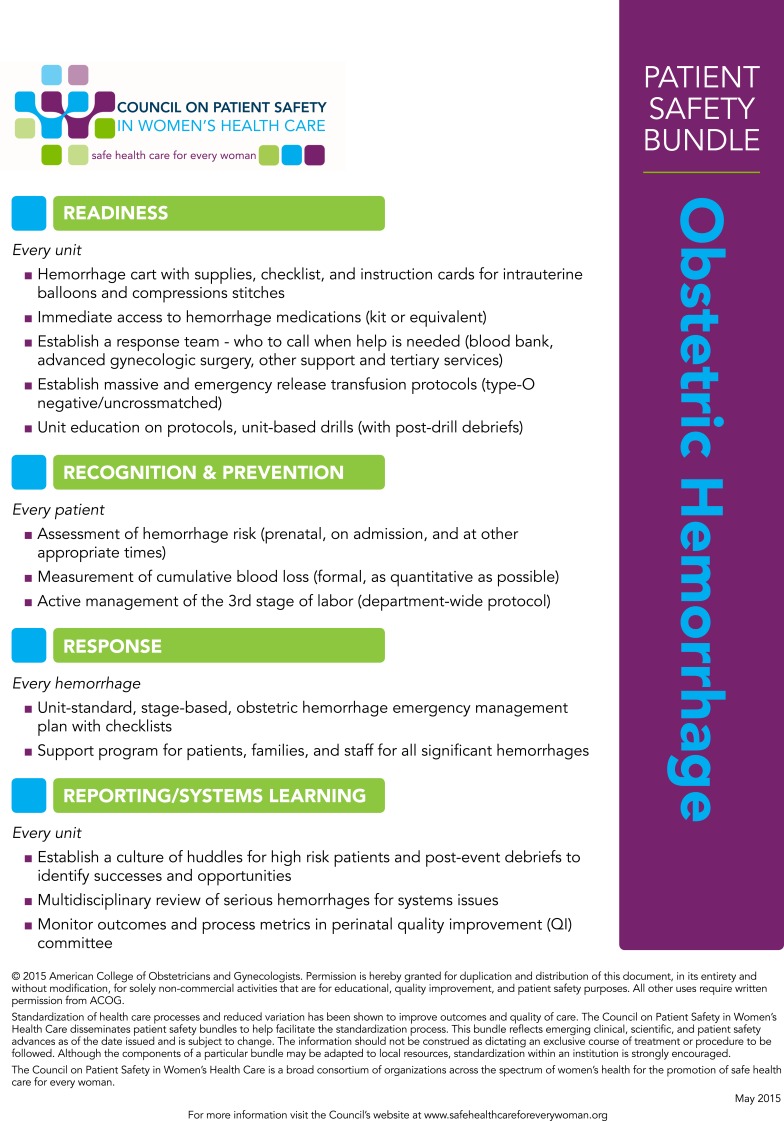
The Alliance for Innovation on Maternal Heath (AIM) is a national quality improvement initiative, within the Council on Patient Safety in Women’s Healthcare (safehealthcareforeverywoman.org), a multi stakeholder organization, whose goal is to eliminate preventable maternal mortality and severe morbidity across the United States.20 The main tools recommended by AIM are maternal safety bundles coupled with implementation guidance and educational opportunities using periodic webinars. The bundle on Obstetric hemorrhage includes key elements within four domains (Box 1): readiness, recognition and prevention, response, reporting and systems learning.
Box 1.
Obstetric hemorrhage safety bundle from the National Partnership for Maternal Safety, Council on Patient Safety in Women's Health Care.
Notes: Reprinted with permission from American College of Obstetricians and Gynecologists. Patient safety bundle: Obstetric hemorrhage. Council on Patient Safety in Women's Health Care. Washington, DC; American College of Obstetricians and Gynecologists: 2015. Available at: http:ljsafehealthcareforeverywoman.org/patient-safety-bundles/obstetrichemorrhage/. Retrieved December 5, 2019.
This bundle can serve as a template for risk reduction at the national, statewide, institutional and provider level. Implementation strategies can be applied for multiple key elements within the bundles. Specifically, certain topics may be more amenable to risk reduction tools than others, in view of less reliance on human judgment and/or interventions.
Within the readiness domain, structural preparedness elements such as the hemorrhage cart, a massive transfusion protocol, are a one-time investment in safety and should not be subject to any unjustified delay. The real investment in risk reduction would be in a meaningful local simulation based education that includes training on team response from trigger to use the stage-based emergency response plan through effective team debriefing. Investment in team training is crucial to promote an optimal, standardized response with a shared mental model.
Within the recognition and prevention domain, the institution of hemorrhage risk assessment can help incorporate risk assessment for all pregnant patients in outpatient and inpatient settings. This can be audited and enforced using hard-stop functions within the electronic medical record or at critical junctures in care (e.g. at the beginning of the second stage). More importantly, processes must be put in place to support the measurement of cumulative blood loss in order to help reduce underestimation, variation, and discrepancy in blood loss “measurement.”
Within the response domain, a standardized stage-based response still represents a challenge. Multidisciplinary efforts aimed at customization of existing resources and templates to the unit’s (and facility’s) specific setting, resources, clinical competencies of the team members is necessary. Once consensus has been achieved and buy in ensured, extensive training and practice are required to hardwire this type of organized team approach.
Within the reporting and systems learning domain, those focused on risk mitigation can learn much from this domain. Learning should be targeted at identifying the root causes of obstetric hemorrhage-related morbidity or mortality. Adopting a standard taxonomy for obstetric hemorrhage drivers and causes can improve the lessons learned and help target interventions. An adaptable and customized electronic medical record and trained chart abstractors can help to identify these drivers and causes in the chart and interpret them in the context of the setting and clinical picture. A multidisciplinary quality and patient safety team can help close the loop by disseminating lessons learned through various methods.
An illustrative example of the implementation of interventions that improve the domains explained above (though not reported in that framework) can be found in the study by Skupski et al in which a daily commitment to education, training, and systematic change lead to tangible results.21
Clinical Strategies (Global)
State-Wide Initiatives
Globally, reducing obstetric hemorrhage related morbidity and mortality can be mediated through large-scale interventions. State-wide initiatives such as the California Maternal Quality Care Collaborative and the Safe Motherhood Initiative/New York State Obstetric Hemorrhage Project are examples of what can be accomplished though learning collaboratives.1,2 A detailed description of their work is beyond the scope of this article but risk reduction strategies adopted in their work include setting goals, creating standards and ensuring widespread dissemination of these standards with support and data surveillance.
In addition to Quality Improvement initiatives, nearly thirty states have an active Maternal Mortality Review Committee (MMRC) in place or in development. Although these committees review all maternal deaths, hemorrhage remains an important contributor and a preventable outcome. A recent report from 9 MMRCs cited the need to enforce policies related to obstetric hemorrhage as a key recommended action.22
Standardization of Current Practices
There is a dire need for more standardization of obstetric hemorrhage risk assessment and management. There are no agreed upon screening tools, medications protocols (eg for oxytocin), approaches for assessing blood loss or time standards for laboratory assessment or initiating transfusion. This emanates primarily from the lack of studies of comparative effectiveness, but also from the reluctance to adopt one standard until studies prove one superior to another. Hence, the need for national and international societies to standardize whenever applicable will be important to minimize unnecessary variation. The efficacy of a standardized approach was demonstrated in obstetric hemorrhage: Shields et al showed that the implementation of a comprehensive protocol for maternal hemorrhage lead to earlier intervention, less transfusion, and quicker resolution of coagulopathy.23
Innovation in Treatment
There is a dearth of innovation in obstetric hemorrhage. Very few new medications have become available. Most recently tranexamic acid, though known and used in the trauma arena, has been shown to reduce mortality and return to the operating room in a large global study (WOMAN trial).24 Similarly, few tools or instruments are available to address advanced cases of hemorrhage, such as balloon- or vacuum-induced tamponade.25,26 Finally, the management of placenta accreta spectrum remains focused around hysterectomy as a definitive treatment while other treatments, such as conservative treatment, remain experimental.27
Hence, the opportunity for more innovation may be one of the ways to reduce risk beyond the usual audit and enforcement of best practices. Areas that can be served by further innovation include further investigation of hemostasis in pregnancy and potential applications for new tests (as currently seen with visco-elastography), devices, or medications, and the exploration of artificial intelligence to enhance prediction of obstetric hemorrhage and anticipatory interventions for prevention. Other areas of focus should include the refinement of the diagnosis and management of conditions such as placenta accreta spectrum and concealed bleeding and/or coagulopathy.
Non-Clinical Strategies
Dissemination, Audit and Feedback
The effectiveness of dissemination of clinical practice guidelines, protocols, and policies in improving practices has been found wanting. In addition, the fact that multiple interventions tend to be no more effective than a single one invites the investigation of other strategies.28
Audit and feedback is one approach that can be useful in providing an opportunity for reflection on one’s practice, and it can lead to change. While the effect seems modest, it may be
more effective when baseline performance is low, the source is a supervisor or colleague, it is provided more than once, it is delivered in both verbal and written formats, and when it includes both explicit targets and an action plan.29
The dependence of effectiveness on human factors highlights the need to explore other methods, such as team training, choice architecture, and use of adjuncts such as the judicious use of alerts, and checklists.30
Resources
Human and physical resources remain a major issue for the fight against hemorrhage-related morbidity and mortality. The response to obstetric hemorrhage requires an orchestra of providers and their tools to be deployed in a harmonious and timely fashion. One can make the argument that physical resources should not be an issue: that all providers should have the medications necessary within their armamentarium and that every primary response team has a contingency team in case a case becomes medically (e.g. a transfusion expert) or surgically (a gynecologic oncologist) complicated. Unfortunately, this may not be the case in all settings. Hence, the need to identify high-risk cases early and transfer them to settings with the appropriate level of maternal care resources is paramount.
Competencies: Teaming Training and Simulation
Assuming that resource needs are addressed, the deployment of these resources requires an orchestrated response. Building the competencies of the team members can be reinforced through simulation training. Simulation can be used to address clinical issues of screening, diagnosis, and management, but also non-technical issues such as communication between obstetricians and anesthesiologists, escalation triggers, communication with patients and families and many other unique challenges.31
Biases: In Diagnosis and Escalation
Bias pervades and permeates our clinical diagnostic and management processes.32 There are many biases that can affect these processes and listing them or addressing them is beyond the scope of this article, however, a few biases are particularly relevant for obstetric hemorrhage: one is confirmation bias in which confirming evidence may be prioritized over disconfirming evidence to support the thought of diagnosis (e.g. she is not bleeding because her urine output is fine, and her hypotension is likely due to her epidural bolus). The other bias is tolerance of ambiguity in which the ability of the provider to tolerate ambiguous situations or contradictory information is variable from one provider to another, thus leading to different management decisions (e.g. Providers with a high tolerance of ambiguity may wait longer to perform a cesarean section on an induction of labor, thus they may have a higher risk of chorioamnionitis and hemorrhage).33 While we are currently working to uncover and study these biases there is no effective way to eliminate them. One promising solution is through choice architecture and forcing functions (e.g. Calling a hemorrhage code is mandatory when the blood loss reaches a certain amount or a certain number of medications have been given or when a Bakri balloon is requested).
Patient and Family Support
The abrupt onset and the radical nature of certain treatments (e.g. Hysterectomy) in the case of obstetric hemorrhage make it a perfect setting for patients and their families to be ill-informed and psychologically unprepared to deal with the situation at the time of the treatment and thereafter. The permanent loss of function (e.g. fertility or kidney injury) or an organ (e.g. Uterus) can be quite detrimental on the biological and psychological state of the patient and her family.34 Supporting patients and families during and after obstetric hemorrhage is an essential component of taking holistic approach to patient care. Interventions targeted at teaching providers how to deliver bad news and help with the initial stages of grief can be helpful.35
Conclusion and Next Steps
Obstetric hemorrhage with its related morbidities remains a significant and often preventable cause of maternal morbidity and mortality. Changes in definitions, an expansion of the spectrum of causes, variation in interventions and guidelines and lack of innovation are some of the issues that pose ongoing challenges for meaningful risk reduction. Opportunities to further mitigate risk, while contributing to improved patient outcomes, include helping to secure necessary resources, building team training and simulation programs, developing interventions targeted at minimizing cognitive biases, and facilitating patient and family support program development. However, the road ahead remains long and winding. The need for innovation and practice-changing studies is dire. At this stage, performance improvement and risk mitigation for obstetric hemorrhage will require close coordination with clinicians and quality improvement teams. We must establish standardized approaches to diagnosis and treatment through team training and simulation that target both clinical and more importantly non-clinical challenges, such as communication, escalation and biases that can contribute to denial or delay in recognition or management of obstetric hemorrhage.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.California Maternal Quality Care Collaborative. OB hemorrhage toolkit V 2.0 Available from: https://www.cmqcc.org/resources-tool-kits/toolkits/ob-hemorrhage-toolkit. Accessed June19, 2019.
- 2.American College of Obstetricians and Gynecologists. Obstetric hemorrhage bundle Available from: https://m.acog.org/About-ACOG/ACOG-Districts/District-II/SMI-OB-Hemorrhage. Accessed June19, 2019.
- 3.Main EK, Goffman D, Scavone BM, et al., National Partnership for Maternal Safety; Council on Patient Safety in Women’s Health Care. National partnership for maternal safety: consensus bundle on obstetric hemorrhage. Obstet Gynecol. 2015;126(1):155–162. doi: 10.1097/AOG.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 4.Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011–2013. Obstet Gynecol. 2017;130(2):366–373. doi: 10.1097/AOG.0000000000002114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dahlke JD, Mendez-Figueroa H, Maggio L, et al. Prevention and management of postpartum hemorrhage: a comparison of 4 national guidelines. Am J Obstet Gynecol. 2015;213(1):76.e1–76.e10. doi: 10.1016/j.ajog.2015.02.023 [DOI] [PubMed] [Google Scholar]
- 6.Abdul-Kadir R, McLintock C, Ducloy AS, et al. Evaluation and management of postpartum hemorrhage: consensus from an international expert panel. Transfusion. 2014;54(7):1756–1768. doi: 10.1111/trf.12550. [DOI] [PubMed] [Google Scholar]
- 7.Menard MK, Main EK, Currigan SM. Executive summary of the revitalize initiative: standardizing obstetric data definitions. Obstet Gynecol. 2014;124(1):150–153. doi: 10.1097/AOG.0000000000000322 [DOI] [PubMed] [Google Scholar]
- 8.Kerr RS, Weeks AD. Postpartum haemorrhage: a single definition is no longer enough. BJOG. 2017;124(5):723–726. doi: 10.1111/1471-0528.14417 [DOI] [PubMed] [Google Scholar]
- 9.Dossou M, Debost-Legrand A, Déchelotte P, Lémery D, Vendittelli F. Severe secondary postpartum hemorrhage: a historical cohort. Birth. 2015;42(2):149–155. doi: 10.1111/birt.2015.42.issue-2 [DOI] [PubMed] [Google Scholar]
- 10.Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994–2006. Am J Obstet Gynecol. 2010;202(4):353.e1-6. doi: 10.1016/j.ajog.2010.01.011 [DOI] [PubMed] [Google Scholar]
- 11.Dutton RP, Lee LA, Stephens LS, Posner KL, Davies JM, Domino KB. Massive hemorrhage: a report from the anesthesia closed claims project. Anesthesiology. 2014;121(3):450–458. doi: 10.1097/ALN.0000000000000369 [DOI] [PubMed] [Google Scholar]
- 12.Seacrist M, Bingham D, Scheich B, Byfield R. Barriers and facilitators to implementation of a multistate collaborative to reduce maternal mortality from postpartum hemorrhage. J Obstet Gynecol Neonatal Nurs. 2018;47(5):688–697. doi: 10.1016/j.jogn.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 13.Bateman BT, Mhyre JM, Hernandez-Diaz S, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol. 2013;122(5):957–965. doi: 10.1097/AOG.0b013e3182a603bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metcalfe A, Lix LM, Johnson JA, et al. Validation of an obstetric comorbidity index in an external population. BJOG. 2015;122(13):1748–1755. doi: 10.1111/1471-0528.13254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merriam AA, Wright JD, Siddiq Z, et al. Risk for postpartum hemorrhage, transfusion, and hemorrhage-related morbidity at low, moderate, and high volume hospitals. J Matern Fetal Neonatal Med. 2018;31(8):1025–1034. doi: 10.1080/14767058.2017.1306050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Main EK, Cape V, Abreo A, et al. Reduction of severe maternal morbidity from hemorrhage using a state perinatal quality collaborative. Am J Obstet Gynecol. 2017;216(3):298.e1–298.e11. doi: 10.1016/j.ajog.2017.01.017 [DOI] [PubMed] [Google Scholar]
- 17.Diaz V, Abalos E, Carroli G. Methods for blood loss estimation after vaginal birth. Cochrane Database Syst Rev. 2018;13(9):CD010980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Joint Commission. Sentinel events Available from: https://www.jointcommission.org/assets/1/6/CAMH_24_SE_all_CURRENT.pdf. Accessed June19, 2019.
- 19.Atallah F, Bernstein PS, Diaz DA, Minkoff H. The adverse outcome index: putting quality into an outcome measure. Obstet Gynecol. 2018;132(3):750–753. doi: 10.1097/AOG.0000000000002791 [DOI] [PubMed] [Google Scholar]
- 20.Council on Patient Safety in Women's Health Care. Alliance for innovation on maternal health (AIM). Available from: https://safehealthcareforeverywoman.org/aim-program/. Accessed June19, 2019.
- 21.Skupski DW, Brady D, Lowenwirt IP, et al. Improvement in outcomes of major obstetric hemorrhage through systematic change. Obstet Gynecol. 2017;130(4):770–777. doi: 10.1097/AOG.0000000000002207 [DOI] [PubMed] [Google Scholar]
- 22.CDC Foundation. Report from nine mortality report committees Available from: https://www.cdcfoundation.org/sites/default/files/files/ReportfromNineMMRCs.pdf. Accessed September14, 2019.
- 23.Shields LE, Wiesner S, Fulton J, Pelletreau B. Comprehensive maternal hemorrhage protocols reduce the use of blood products and improve patient safety. Am J Obstet Gynecol. 2015;212(3):272–280. doi: 10.1016/j.ajog.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 24.WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105–2116. doi: 10.1016/S0140-6736(17)30638-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Said Ali A, Faraag E, Mohammed M, et al. The safety and effectiveness of Bakri balloon in the management of postpartum hemorrhage: a systematic review. J Matern Fetal Neonatal Med. 2019;24:1–8. doi: 10.1080/14767058.2019.1605349 [DOI] [PubMed] [Google Scholar]
- 26.Purwosunu Y, Sarkoen W, Arulkumaran S, Segnitz J. Control of postpartum hemorrhage using vacuum-induced uterine tamponade. Obstet Gynecol. 2016;128(1):33–36. doi: 10.1097/AOG.0000000000001473 [DOI] [PubMed] [Google Scholar]
- 27.Obstetric care consensus No. 7: placenta accreta spectrum. Obstet Gynecol. 2018;132(6):e259–e275. doi: 10.1097/AOG.0000000000002983 [DOI] [PubMed] [Google Scholar]
- 28.Squires JE, Sullivan K, Eccles MP, Worswick J, Grimshaw JM. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci. 2014;6(9):152. doi: 10.1186/s13012-014-0152-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;13(6):CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American College of Obstetricians and Gynecologists. Obstetric hemorrhage checklist Available from: https://www.acog.org/-/media/Districts/District-II/Public/SMI/v2/SMIHemorrhageChecklistREVISEDJUNE2019.pdf?dmc=1&ts=20190914T1242520709. Accessed September14, 2019.
- 31.Sheen JJ, Lee C, Goffman D. The utility of bedside simulation for training in critical care obstetrics. Semin Perinatol. 2018;42(1):59–63. doi: 10.1053/j.semperi.2017.11.010 [DOI] [PubMed] [Google Scholar]
- 32.Croskerry P. From mindless to mindful practice–cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445–2448. doi: 10.1056/NEJMp1303712 [DOI] [PubMed] [Google Scholar]
- 33.Yee LM, Liu LY, Grobman WA. The relationship between obstetricians’ cognitive and affective traits and their patients’ delivery outcomes. Am J Obstet Gynecol. 2014;211(6):692.e1-6. doi: 10.1016/j.ajog.2014.06.003 [DOI] [PubMed] [Google Scholar]
- 34.Zaat TR, van Steijn ME, de Haan-jebbink JM, Olff M, Stramrood CAI, van Pampus MG. Posttraumatic stress disorder related to postpartum haemorrhage: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2018;225:214–220. doi: 10.1016/j.ejogrb.2018.04.012 [DOI] [PubMed] [Google Scholar]
- 35.Powell SK. When things go wrong: responding to adverse events: a consensus statement of the Harvard hospitals. Lippincotts Case Manag. 2006;11(4):193–194. doi: 10.1097/00129234-200607000-00001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- California Maternal Quality Care Collaborative. OB hemorrhage toolkit V 2.0 Available from: https://www.cmqcc.org/resources-tool-kits/toolkits/ob-hemorrhage-toolkit. Accessed June19, 2019.