Abstract
A 77‐year‐old woman presented with ophthalmic zoster and nasal tip involvement, consistent with Hutchinson's sign. Ocular examination disclosed a swollen upper eyelid, chemosis, conjunctival injection, pus, and mild corneal endothelial decompensation. The presence of Hutchinson's sign requires urgent consultation with an ophthalmologist due to the high risk of ocular complications.
Keywords: herpes zoster ophthalmicus, herpesvirus 3, human, trigeminal nerve
A 77‐year‐old woman presented with ophthalmic zoster and nasal tip involvement, consistent with Hutchinson's sign. Ocular examination disclosed a swollen upper eyelid, chemosis, conjunctival injection, pus, and mild corneal endothelial decompensation. The presence of Hutchinson's sign requires urgent consultation with an ophthalmologist due to the high risk of ocular complications.

1. CASE HISTORY
A 77‐year‐old woman (Table 1) presented with a 6‐day history of right‐sided facial pain, blurred vision, and photosensitivity. Physical examination showed crusted vesicles in the distribution of the right ophthalmic nerve (Figure 1). Findings were consistent with Hutchinson's sign of ophthalmic zoster. Ocular (including slit lamp and fundus) examination disclosed a swollen upper eyelid, chemosis, conjunctival injection, pus, and mild corneal endothelial decompensation (Figure 2). Visual acuity was limited to hand motion. There were no cells or flare in the anterior chamber, although the examination was complicated by the swollen eyelid. Oral acyclovir therapy was begun. Four days later, the patient was admitted due to confusion and malaise. Chest X‐ray showed a right‐sided pulmonary infiltrate. Staphylococcus aureus superinfection was identified in her zoster lesions. Although intravenous acyclovir as well as antibiotic and supportive therapy was initiated, the patient died due to respiratory complications.
Table 1.
Past medical history and list of medications at admission
| Past medical history |
|
| List of medications |
|
Figure 1.

Multiple crusted vesicles in the distribution of the right ophthalmic nerve, that is, the forehead, nasal bridge, and the nasal tip, consistent with Hutchinson's sign of ophthalmic zoster
Figure 2.
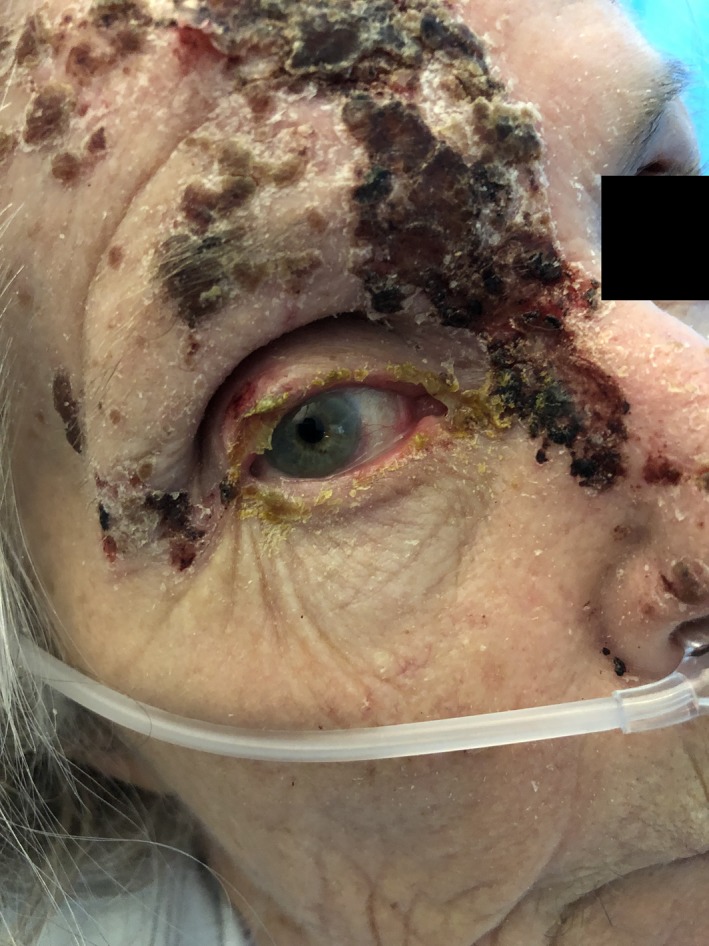
Ocular affection in ophthalmic zoster
Nasal tip, side, or root involvement during ophthalmic zoster represents the dermatome of the nasociliary nerve.1 Ocular involvement is more common in such cases.2 Accordingly, this requires urgent ophthalmological consultation. However, subsequent studies have found that even though the risk among these patients is much higher than those without, about a third of patients without nasociliary nerve involvement may also develop ocular complications.3
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
All authors: participated in collecting patient data (pictures and clinical history), reviewing the literature, interpretation of clinical findings, drafting the manuscript, critical revision of the manuscript for important intellectual content, and approval of the final version.
ACKNOWLEDGMENTS
We thank Dr Simon Persson Skibsted for his valuable contribution to the ophthalmological examination.
Frary J, Petersen PT, Pareek M. Hutchinson’s sign of ophthalmic zoster. Clin Case Rep. 2020;8:219–220. 10.1002/ccr3.2596
REFERENCES
- 1. Ting DSJ, Ghosh N, Ghosh S. Herpres zoster ophthalmicus. BMJ. 2019;364:k5234. [DOI] [PubMed] [Google Scholar]
- 2. Hutchinson J. A clinical report on herpes zoster frontalis ophthalmicus (shingles affecting the forehead and nose). R Lond Ophthalmic Hosp Rep. 1865;5:191‐215. [Google Scholar]
- 3. Harding SP, Lipton JR, Wells JC. Natural history of herpes zoster ophthalmicus: predictors of postherpetic neuralgia and ocular involvement. Br J Opthalmol. 1987;71:353‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]


