Abstract
Most psychiatric disorders, when examined individually, are associated with a broad range of adverse outcomes. However, psychiatric disorders often co-occur and their co-occurrence is well explained by a limited number of transdiagnostic factors. Yet it remains unclear whether the risk of these adverse outcomes is due to specific psychiatric disorders, specific dimensions of psychopathology (i.e., internalizing and externalizing dimensions), a general psychopathology factor or a combination of these explanations. In a large nationally representative prospective survey, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), we used structural equation modeling to examine the shared and specific effects of common Axis I and Axis II disorders on the risk of ten adverse outcomes (unemployment; financial crisis; low income; poorer general health; worse mental and physical health; legal problems; divorce; problems with a neighbor, friend or relative; and violence) in the general adult population. Effects of psychiatric disorders were exerted mostly through a general psychopathology factor representing the shared effect across all disorders, independent of sociodemographic characteristics and the presence of the adverse outcomes at baseline. Violence and legal problems were further associated with the externalizing factor, but there were no independent associations of the internalizing factor or any individual psychiatric disorders with any of the adverse outcomes. Our findings reveal that associations between psychiatric disorders and adverse outcomes occur through broad psychological dimensions. Understanding the biological and psychological mechanisms underlying these dimensions should yield key intervention targets to decrease the individual suffering and societal burden associated with common psychiatric disorders.
Introduction
Persistently increasing national rates of suicide attempts1 and deaths2 and opioid overdoses3, 4 along with decreasing life expectancy5, 6 and quality of life7 in some demographic groups have reignited interest in relationships between psychiatric disorders and adverse outcomes. Most psychiatric disorders, when examined individually, are associated with a broad range of adverse outcomes.8–10 However, psychiatric disorders often co-occur and their co-occurrence is well explained by a limited number of underlying dimensions or transdiagnostic factors.11, 12 In a previous study, we found that the association of psychiatric disorders with increased risk of suicide attempt was mediated almost exclusively through a general psychopathology factor representing the shared effect across common psychiatric disorders.8 It is unknown, though, whether similar general associations exist for other adverse outcomes and whether the strength of such associations vary by adverse outcome.
This prospective study sought to generalize the findings of our study on risk of suicide attempt and address broader questions by examining the shared and specific associations of a wide range of DSM-IV Axis I and Axis II disorders with multiple adverse outcomes assessed in a large, nationally representative sample. Since dimensions underlying psychopathology are correlated,11, 12 we used a bifactor latent variable approach to disentangle the effects shared by all psychiatric disorders (i.e., general psychopathology), those specific to dimensions of psychopathology (e.g., internalizing dimension) and those specific to individual psychiatric disorders (e.g., major depressive episode). To our knowledge, this is the most extensive assessment in a nationally representative sample of associations between psychiatric disorders and adverse outcomes. Based on prior research,8–10 we hypothesized that psychiatric disorders would be associated with a broad range of adverse outcomes and that these associations would be mediated primarily by broad underlying dimensions of psychopathology.
Materials and Methods
Sample
Data were drawn from the wave 1 and wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative face-to-face survey of the U.S adult population, conducted in 2001–2002 (Wave 1) and 2004–2005 (Wave 2) by the National Institute on Alcoholism and Alcohol Abuse (NIAAA).13 The target population included the civilian noninstitutionalized population, aged 18 years and older, residing in the United States. The cumulative response rate at Wave 2 was 70.2%, resulting in 34,653 Wave 2 interviews.13 The Wave 2 NESARC data were weighted to be representative of the U.S. civilian population based on the 2000 census.13 The research protocol, including written informed consent procedures, received full human subjects review and approval from the U.S. Census Bureau and the Office of Management and Budget.
Measures
Assessments of DSM-IV Axis I and Axis II disorders
Psychiatric disorders were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV version (AUDADIS-IV), a valid and reliable structured diagnostic instrument.13,14–18 Axis I diagnoses included substance use disorders (alcohol use disorder, drug use disorder, and nicotine dependence), mood disorders (major depressive disorder, dysthymic disorder, and bipolar disorder), anxiety disorders (panic disorder, social anxiety disorder, specific phobia, and generalized anxiety disorder), and pathological gambling. All Axis I disorder diagnoses were based on the past 12 months prior to Wave 1. Axis II disorders (including avoidant, dependent, obsessive-compulsive, histrionic, paranoid, schizoid, and antisocial personality disorders) were assessed on a lifetime basis13.
Assessments of adverse outcomes
We included all adverse outcomes assessed in the demographic and background information section of the AUDADIS in Waves 1 and 2. Adverse outcomes included unemployment; financial crisis; income below the median; poorer general health; worse mental and physical health; legal problems; divorce/separation; having problems with a neighbor, friend or relative; and violence. In Wave 1, all outcomes were assessed using a past-year timeframe, except violence, which was assessed using a lifetime timeframe. In Wave 2, all outcomes were also assessed using a past-year timeframe, except violence, which included any occurrence since the Wave 1 interview.
Respondents were considered unemployed if they answered “yes” to either: “Were you fired or laid off from a job?” or “Were you unemployed and looking for a job for more than a month?” Having a financial crisis was assessed with the question: “Have you experienced a major financial crisis, declared bankruptcy or more than once been unable to pay your bills on time?”. Income was assessed by self-report. Participants also completed version 2 of the Short Form 12 Health Survey (SF-12v2),19 a 12-item measure that assesses life satisfaction and current functioning over the last four weeks and has demonstrated sensitivity to change in clinical status.10, 20. The SF-12v2 can be scored to generate a norm-based physical component summary score (PCS) and a norm-based mental component summary score (MCS). Higher scores indicate better functioning. General health perception was assessed with the following question: “In general, would you say your health is excellent, very good, good, fair or poor?” which was recoded as fair/poor, good, or very good/excellent.
Participants were considered to have had legal problems if they answered positively to any of the following 3 questions: “Did you or a family member have trouble with the police, got arrested or sent to jail?”, “Have you gotten arrested, held at a police station or had any other legal problems because of your drinking?” and ”Have you gotten arrested, held at a police station or had any other legal problems because of your medicine or drug use?”. Marital status was assessed by self-report. In accord with prior work21, violence was assessed using 9 questions (e.g. “Have you used a weapon like a stick, knife, or gun in a fight?”, “Have you hit someone so hard that you injured them or they had to see a doctor?”). Having problems with a neighbor was assessed by asking: “Have you had serious problems with a neighbor, friend or relative?” To examine whether selective loss to follow-up between waves could bias the results, we compared the distribution of adverse outcomes among all individuals who participated in Wave 1, versus those who participated in both waves. For all outcomes, the difference in prevalence was less than 2%, indicating that loss to follow-up did not substantially influence the distribution of adverse outcomes. Because the prevalence of psychiatric disorders differs by age group, sex and across ethnicities, all analyses were adjusted for these variables.8
Statistical Analysis
Odds ratios (ORs) were calculated between each pair adverse events. ORs, population attributable fractions (PAFs) and their 95% confidence intervals (CIs) were calculated between each psychiatric disorder at Wave 1 with each adverse outcome at Wave 1 at the bivariate level. While the OR assesses the strength of association between two variables, the PAF is the proportional reduction in population adverse outcome that would occur if exposure to a risk factor were eliminated. Thus, the magnitude of the PAF depends on the strength of association between the risk factor (in this case, each psychiatric disorder) and each adverse outcome, as well as the prevalence of the risk factor. For the analyses of ORs and PAFs, continuous variables (i.e., income, SF-12 scores and general health status) were dichotomized at the median.
Because bivariate analyses do not properly model comorbidity and can lead to an inflation of type I error due to multiple comparisons (i.e., each disorder times each outcome), we used confirmatory factor analysis (CFA) to identify the latent structure underlying individual mental disorders assessed at Wave 1, based on previous models used to examine the relationship of psychiatric disorders with suicide attempts in these data.8 Specifically, we performed a bifactor CFA model to determine whether a general psychopathology factor measured by all psychiatric disorders in addition to disorder-specific factors22, 23 fit the underlying structure of psychiatric disorders. We examined measures of goodness-of-fit, including the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root mean squared error of approximation (RMSEA). CFI and TLI values greater than 0.95 and values of RMSEA less than 0.06 are commonly used to indicate good model fit and were used as cut-offs.24
Finally, we used a structural equation model, based on our previous work on the relationship of psychiatric disorders to risk of suicide attempt8, to assess shared and specific associations of psychiatric disorders at Wave 1 on each Wave 2 adverse outcome, while controlling for demographic characteristics and each adverse outcome at Wave 1 and each corresponding outcome at Wave 2. Specifically, we examined three sets of relationships: 1) the association of the general psychopathology liability factor (representing the effects shared across all mental disorders) with adverse outcomes, 2) the associations of each dimension of psychopathology with adverse outcomes beyond its association with the general psychopathology factor, and 3) the associations of individual psychiatric disorders with the adverse outcomes above and beyond the shared effects of psychiatric disorders through the latent factors.
Since internalization and externalization dimensions are positively correlated,11, 12 an advantage of modeling a bifactor model is that a general psychopathology factor accounts for a substantial proportion of this correlation, is orthogonal to these dimensions and saturates each psychiatric disorder diagnosis directly.22, 23 The bifactor model allows a disambiguation from each of the other associations shared by all psychiatric disorders (represented by the general psychopathology factor), those shared by disorders within each dimension of psychopathology (e.g., externalizing dimension) and the specific associations of each psychiatric disorder per se.25
The relationships between the general psychopathology factor and adverse outcomes are interpreted as the association of the overall shared psychiatric disorder liability predictor with the risk of the adverse outcome. By contrast, the relationships examined between the specific dimensions of psychopathology or specific individual disorders and adverse events are interpreted as the direct associations, because they indicate associations that are not mediated through the general psychopathology factor. To determine if a particular psychiatric disorder is associated with an adverse outcome above and beyond the association attributable to the latent variables, modification indices (i.e. chi-square tests with 1 df.) were examined to test if any residuals associated with psychiatric disorders are correlated with the risk of the adverse outcome. To avoid including associations that could be significant due to multiple testing (3 factors and 18 disorders times 10 outcomes), we consistently used as threshold for inclusion in the model associations with Bonferroni-corrected p-value=0.05/210, i.e., p≤0.00024.26 To assess the robustness of our results and facilitate comparisons with other work, we conducted a sensitivity analysis using two additional parameterizations of the model used in our previous work on suicide attempts: one in which the internalizing factor is subdivided in to separate internalizing factors, and another using the distress-fear-externalizing model that includes antisocial personality disorder, but not other personality disorders.
Population-attributable fractions (PAF) were computed using the Punaf program27, 28 for STATA software (Svy routines in Stata, version 11.0; StataCorp).28, 29 This program implements the method for estimating PAFs recommended by Greenland and Drescher for cohort studies.30 All other analyses were conducted in Mplus Version 7.3.26 The default estimator for the analysis was the variance-adjusted weighted least squares (WLSMV), a robust estimator appropriate for ordered categorical and dichotomous observed variables such as the ones used in this study.26 All analyses accounted for the NESARC’s complex sampling design.
Results
Associations of mental disorders with adverse outcomes
All adverse consequences increased the odds of all other adverse consequences except the association of SF-12 physical component summary score and unemployment, which decreased the odds; and the associations of income with marital status, SF-12 physical component score and violence and SF-12 physical component score and legal problems, all of which had ORs that were not statistically significant (Supplementary Table 1).
The psychiatric disorders with the highest 12-month prevalence were nicotine dependence (12.4%) and major depressive disorder (7.0%). All psychiatric disorders, except alcohol use disorder and pathological gambling, were positively associated with all adverse outcomes examined. The largest ORs were for the association between drug use disorder and violence and for the association between dependent personality disorder and scoring below the mean in the mental component summary of the SF-12. Alcohol use disorder, drug use disorder and pathological gambling were also associated with increased ORs for most adverse outcomes, but had decreased ORs for having an income below the median and for having a score below the mean in the physical component summary of the SF-12. In addition, alcohol use disorder was associated with lower odds of having general health that was good, fair, or poor as opposed to very good or excellent. Drug use disorder had decreased odds of scoring below the mean on the physical component summary of the SF-12 (Table 1).
Table 1.
Associations of past-year Axis I disorders and lifetime personality disorders (assessed in Wave 1) on the occurrence of adverse outcomes in Wave 2 of the National Epidemiological Survey on Alcohol and Related Conditions (N=34653).
| Divorced or Separated | Problems with neighbor | Unemployment | Financial Crisis | Incomea | General Healthb | MCSc | Violence | PCSc | Legal Problems | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 disorders | OR | OR | OR | OR | OR | OR | OR | OR | OR | OR | |
| MDE | 2.20 | 3.20 | 2.00 | 3.04 | 1.64 | 1.67 | 3.34 | 3.02 | 1.49 | 2.29 | |
| Dysthymia | 3.10 | 3.68 | 1.80 | 3.79 | 2.26 | 2.63 | 4.98 | 1.91 | 2.78 | 1.99 | |
| GAD | 2.24 | 3.37 | 1.75 | 3.73 | 1.59 | 2.39 | 4.81 | 1.65 | 2.16 | 2.15 | |
| Panic Disorder | 1.83 | 3.37 | 1.70 | 2.79 | 1.89 | 2.00 | 2.76 | 2.21 | 2.00 | 2.03 | |
| SAD | 1.51 | 2.44 | 1.30 | 2.18 | 1.50 | 1.59 | 3.13 | 1.72 | 1.50 | 1.74 | |
| Specific Phobia | 1.23 | 2.14 | 1.20 | 1.83 | 1.44 | 1.23 | 1.83 | 1.66 | 1.32 | 1.62 | |
| Mania/ Hypomania | 1.74 | 3.45 | 2.23 | 3.54 | 1.96 | 1.80 | 3.66 | 5.13 | 1.43 | 3.39 | |
| Avoidant PD | 1.65 | 2.96 | 2.01 | 3.09 | 2.04 | 2.02 | 4.43 | 2.95 | 1.67 | 2.03 | |
| Dependent PD | 1.43* | 2.60 | 2.50 | 4.32 | 5.17 | 4.45 | 8.24 | 5.01 | 3.94 | 2.94 | |
| OCPD | 1.22 | 2.29 | 1.48 | 1.96 | 0.99* | 1.24 | 1.88 | 1.92 | 1.29 | 1.70 | |
| Paranoid PD | 1.99 | 3.91 | 2.37 | 3.65 | 1.95 | 1.98 | 3.14 | 4.50 | 1.62 | 2.75 | |
| Schizoid PD | 1.80 | 2.50 | 1.89 | 3.04 | 1.51 | 1.98 | 2.35 | 3.42 | 1.79 | 2.44 | |
| Histrionic PD | 1.50 | 3.13 | 2.46 | 3.23 | 1.49 | 1.29 | 2.92 | 5.94 | 1.16* | 3.09 | |
| AUD | 1.33 | 1.60 | 1.91 | 1.74 | 0.66 | 0.84 | 1.20 | 6.22 | 0.65 | 3.35 | |
| DUD | 1.33 | 2.66 | 3.11 | 3.44 | 1.34 | 1.13* | 2.06 | 10.08 | 0.73 | 5.32 | |
| Nicotine Dep | 1.93 | 1.86 | 2.09 | 2.75 | 1.15 | 1.67 | 1.68 | 4.08 | 1.42 | 2.48 | |
| Pathological Gambling | 2.12 | 1.98* | 3.64 | 2.91 | 0.74* | 1.26* | 1.69* | 4.31 | 0.75 | 2.99 | |
| Antisocial PD | 1.44 | 2.06 | 2.84 | 3.22 | 1.12* | 1.57 | 1.82 | 6.39 | 1.29 | 3.59 | |
The income variable is dichotomized as follows: under the median versus equal or over the median (median = $21,690).
The general health variable is dichotomized as follows: poor or good health versus very good or excellent health.
these variables are dichotomized as follows: under the mean versus equal or over the mean (mean = 50).
Results are not significant (two-sided p-value < 0.05) unless marked with the * sign.
Abbreviations: CI, confidence interval; GAD, generalized anxiety disorder; SAD, social anxiety disorder; MDE, major depressive episode; OCPD, obsessive-compulsive personality disorder; OR, odds ratio; PD, personality disorder; AUD, alcohol use disorder; DUD, drug use disorder; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score.
The PAFs followed a slightly different pattern because their magnitude depends both on the prevalence of the psychiatric disorders as well as on strength of the association between psychiatric disorders and adverse outcomes (Table 2). All psychiatric disorders, except alcohol use disorder, drug use disorder, pathological gambling and obsessive-compulsive personality disorder, were associated with increased PAFs for all adverse outcomes. The largest PAFs were for associations of alcohol use disorder and nicotine dependence with violence. The size of these PAFs indicate that although other associations were stronger (as measured by the ORs presented in Table 1), the higher prevalence of these disorders resulted in a greater impact at the population level (Table 2). Obsessive-compulsive personality disorder, alcohol use disorder and pathological gambling had small negative PAFs, indicating that at the population level, they were associated with increases in median income. Alcohol and drug use disorders were associated with negative PAFs on the physical component score of the SF-12 and alcohol use disorder was further associated with a negative PAF for general health.
Table 2.
Population attributable fractions (PAF) of the Axis I disorders and lifetime personality disorders (assessed in Wave 1) on the occurrence of adverse outcomes in Wave 2 of the National Epidemiological Survey on Alcohol and Related Conditions (N=34653).
| Divorced or Separated | Problems with neighbor | Unemployment | Financial Crisis | Incomea | General Healthb | MCSc | Violence | PCSc | Legal Problems | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 1 disorders | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | PAF (%) | |
| MDE | 4.75 | 12.18 | 5.12 | 8.94 | 1.83 | 1.89 | 6.01 | 11.71 | 1.70 | 6.95 | |
| Dysthymia | 1.48 | 2.52 | 0.57 | 1.96 | 0.64 | 0.77 | 1.47 | 1.23 | 1.00 | 0.99 | |
| GAD | 1.42 | 3.90 | 1.14 | 3.17 | 0.60 | 0.95 | 2.17 | 2.09 | 1.09 | 1.80 | |
| Panic Disorder | 1.23 | 4.02 | 1.11 | 2.48 | 0.69 | 0.78 | 1.59 | 2.42 | 0.98 | 1.72 | |
| SAD | 0.96 | 3.20 | 0.73 | 2.36 | 0.56 | 0.70 | 2.06 | 1.90 | 0.77 | 1.68 | |
| Specific Phobia | 0.99 | 6.30 | 0.90 | 3.82 | 1.18 | 0.89 | 2.86 | 4.38 | 1.16 | 3.26 | |
| Mania/ Hypomania | 1.31 | 5.39 | 2.66 | 4.16 | 0.95 | 0.81 | 2.31 | 8.88 | 0.63 | 4.58 | |
| Avoidant PD | 0.99 | 4.24 | 1.97 | 3.30 | 1.06 | 0.99 | 2.26 | 4.13 | 0.92 | 2.41 | |
| Dependent PD | 0.10 | 0.62 | 0.37 | 0.75 | 0.32 | 0.30 | 0.51 | 1.28 | 0.35 | 0.42 | |
| OCPD | 1.04 | 8.05 | 2.74 | 5.37 | −0.43* | 0.92 | 3.34 | 7.45 | 0.98 | 4.75 | |
| Paranoid PD | 2.77 | 9.87 | 4.52 | 7.20 | 1.59 | 1.73 | 3.72 | 13.69 | 1.36 | 5.80 | |
| Schizoid PD | 1.55 | 3.99 | 1.96 | 3.84 | 0.62 | 1.01 | 1.88 | 5.89 | 1.03 | 3.22 | |
| Histrionic PD | 0.58 | 3.25 | 1.61 | 2.66 | 0.21 | 0.29 | 1.22 | 6.85 | 0.14 | 3.00 | |
| AUD | 1.64 | 4.67 | 5.29 | 4.23 | −2.03* | −0.96* | 0.84 | 24.75 | −2.35* | 11.07 | |
| DUD | 0.22 | 2.65 | 2.44 | 2.42 | 0.27 | 0.06 | 0.76 | 11.13 | −0.34* | 4.66 | |
| Nicotine Dep | 6.22 | 9.32 | 8.30 | 12.27 | 1.03 | 3.13 | 4.23 | 24.33 | 2.25 | 11.81 | |
| Pathological Gambling | 0.11 | 0.21 | 0.24 | 0.22 | −0.03* | 0.05 | 0.07 | 0.62 | 0.03 | 0.25 | |
| Antisocial PD | 0.78 | 4.01 | 4.03 | 4.78 | 0.16 | 0.67 | 1.38 | 14.76 | 0.36 | 6.61 | |
The income variable is dichotomized as follows: under the median versus equal or over the median (median = $21,690).
The general health variable is dichotomized as follows: poor or good health versus very good or excellent health.
these variables are dichotomized as follows: under the mean versus equal or over the mean (mean = 50).
Results are not significant (two-sided p-value < 0.05) unless marked with the * sign.
Abbreviations: CI, confidence interval; GAD, generalized anxiety disorder; SAD, social anxiety disorder; MDE, major depressive episode; OCPD, obsessive-compulsive personality disorder; OR, odds ratio; PD, personality disorder; AUD, alcohol use disorder; DUD, drug use disorder; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score.
Association of transdiagnostic factors with adverse outcomes
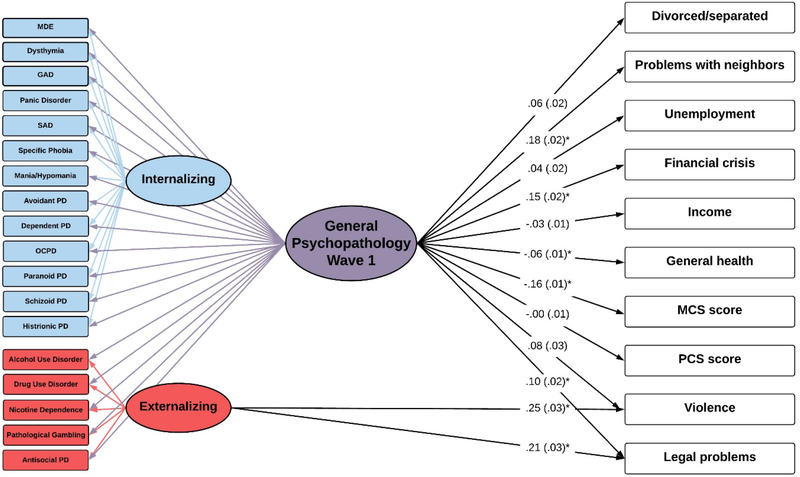
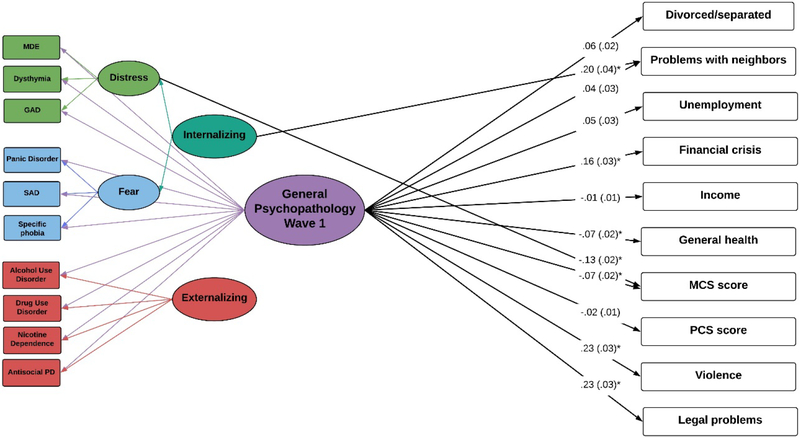
A bi-factor model (left side of Figure 1) of Wave 1 psychiatric disorders provided a good fit to the data (CFI=0.957, TLI=0.943, and RMSEA=0.013). After adjusting for sex, age and race/ethnicity and Wave 1 adverse outcomes, the general psychopathology factor at Wave 1 was significantly associated with all adverse outcomes at Wave 2, except divorce/separation, unemployment, income, violence, and PCS. In addition, the externalizing factor was associated with violence and legal problems in the last 12-months (non-significant paths from the internalizing and externalizing factors to the Wave 2 outcomes are shown in Supplementary Table 2). Furthermore, there were no direct associations with any individual psychiatric disorder with Wave 2 outcomes (Figure 1). Sex, age and race-ethnicity had significant associations with Wave 2 outcomes beyond that of the general psychopathology factor (Table 3) and the proportion of explained variance for each Wave 2 progressively increased from considering the general psychopathology alone to considering also the contribution of the specific factors, the Wave 1 outcomes, and the sociodemographic characteristics (Supplementary Table 3). In the sensitivity analysis, the model with two separate internalizing factors yielded nearly identical results to the main model (Supplemental Figure 1). The fear-distress-externalizing model results (Figure 2) were also very similar although there were direct effects from the internalizing factor to problems with neighbors and from the distress factor to the mental component summary of the SF-12 and there were no direct effects of the externalizing factor to any adverse outcome.
Figure 1. Bifactor model with one internalizing and one externalizing factors testing the shared and specific effects of past-year Axis I disorders and lifetime personality disorders (assessed in Wave 1) on the occurrence of adverse outcomes in Wave 2 of the National Epidemiological Survey on Alcohol and Related Conditions (N=34653).
Ellipses are used to denote latent constructs, rectangles are used to denote the observed variables measuring or impacting on these constructs. The bifactor model parses disorder variance into general variance (i.e., variance of the general psychopathology factor), variance of dimensions of psychopathology (e.g., variance of the externalizing dimension) and unique variance (variance of each mental disorder per se). Regression coefficients shown are standardized. Values in brackets indicate their standard errors. * indicate significant effects (two-sided p<0.05/210, i.e., p<0.00024). All results are adjusted for sociodemographic characteristics (sex, age and race/ethnicity) and each adverse outcome at Wave 1. Abbreviations: MDE, major depressive episode; GAD, generalized anxiety disorder; SAD, social anxiety disorder; OCPD, obsessive-compulsive personality disorder; PD, personality disorder; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score. The Wave 1 outcomes (e.g. divorced/separated, problems with neighbors at Wave 1) were included as direct effects to each of the respective W2 outcomes and were allowed to freely correlate with one another at Wave 1 (arrows not shown). The Wave 2 outcomes were also allowed to freely correlate with one another (arrows not shown).
Table 3.
Effects of sex, age and race/ethnicity on the general psychopathology factor and adverse outcomes in the bifactor model.
| GPF | Divorced or Separated | Problems with neighbor | Unemployment | Financial Crisis | Income | General Health | MCS | PCS | Violence | Legal Problems | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| Age | −0.35 (0.02) | −0.03 (0.02)* | −0.07 (0.02) | −0.31 (0.02) | −0.21 (0.02) | −0.07 (0.01) | −0.20 (0.01) | 0.02 (0.01) | −0.21 (0.01) | −0.33 (0.02) | −0.19 (0.02) |
| Men | −0.08 (0.02) | −0.04 (0.01) | −0.08 (0.02) | 0.04 (0.01) | −0.05 (0.01) | 0.10 (0.01) | −0.06 (0.01) | 0.05 (0.01) | −0.01 (0.01)* | 0.17 (0.02) | 0.03 (0.01) |
| White | 0.12 (0.01) | −0.04 (0.01) | 0.03 0.02)* | −0.08 (0.01) | −0.10 (0.01) | 0.03 (0.01) | 0.10 (0.01) | 0.01 (0.01) | 0.01 (0.01) | −0.03 (0.02)* | −0.04 (0.01) |
Regression coefficients (β) are standardized.
Results are not significant (two-sided p<0.05) unless indicated by the * sign.
Abbreviations: SE, standard error; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score.
Figure 2. Bifactor model with fear, distress and externalizing factors testing the shared and specific effects of past-year Axis I disorders and antisocial personality disorder (assessed in Wave 1) on the occurrence of adverse outcomes in Wave 2 of the National Epidemiological Survey on Alcohol and Related Conditions (N=34653).
Ellipses are used to denote latent constructs, rectangles are used to denote the observed variables measuring or impacting on these constructs. The bifactor model parses disorder variance into general variance (i.e., variance of the general psychopathology factor), variance of dimensions of psychopathology (e.g., variance of the externalizing dimension) and unique variance (variance of each mental disorder per se). Regression coefficients shown are standardized. Values in brackets indicate their standard errors. * indicate significant effects (two-sided p<0.05/150, i.e., p<0.00033). All results are adjusted for sociodemographic characteristics (sex, age and race/ethnicity) and each adverse outcome at Wave 1. Abbreviations: MDE, major depressive episode; GAD, generalized anxiety disorder; SAD, social anxiety disorder; PD, personality disorder; MCS, Mental Component Summary Score; PCS, Physical Component Summary Score. The Wave 1 outcomes (e.g. divorced/separated, problems with neighbors at Wave 1) were included as direct effects to each of the respective W2 outcomes and were allowed to freely correlate with one another at Wave 1 (arrows not shown). The Wave 2 outcomes were allowed to freely correlate with one another (arrows not shown).
Discussion
In a large, nationally representative sample, we found that psychiatric disorders were prospectively associated with a broad range of adverse outcomes assessed three years later. These associations were primarily mediated by a general psychopathology factor representing the shared effects across all psychiatric disorders, independent of sociodemographic characteristics and the presence of the adverse outcomes at baseline. Violence and legal problems were further associated with the externalizing factor, but there were no independent associations of the internalizing factor or any individual psychiatric disorders with any of the adverse outcomes. Sensitivity analysis indicated that the results were generally robust to model specification, with small differences probably due to differences in parameterization and to the exclusion of most personality disorders from the fear-distress-externalizing model.
Although previous studies have shown that individual psychiatric disorders are associated with a broad range of adverse outcomes,1, 7, 9 our findings demonstrate that these associations are mostly mediated by a general liability to psychopathology rather than being specific to any single disorder. Our results help reconcile findings that both internalizing disorders (such as major depressive disorder) and externalizing disorders (such as substance use disorders) are associated with multiple adverse outcomes. These patterns, which are consistent with current dimensional models of psychopathology and highlight the role of comorbidity, replicate and extend prior analyses on the risk of suicide attempt.8 The new results generalize to a wide of adverse outcomes associations of psychiatric disorders with a broad range of adverse outcomes through a common psychological factor. Shared genetic31 and environmental influences32 may contribute to this common psychological factor, whose underlying neurocircuitry is being actively pursued.33, 34 It is also possible that the associations between psychopathology at Wave 1 and Wave 2 outcomes may be partially explained by shared genetic factors, given the substantial contribution of genetic influences to several of the adverse outcomes examined in the study35, 36.
To our knowledge, this is the first study to examine prospectively differential associations of multiple outcomes across a broad range of psychiatric disorders. Although the general psychopathology factor was associated with all adverse outcomes, the strength of this association varied across outcomes. Furthermore, the externalizing factor was independently associated with violence and legal problems beyond the effect of the general psychopathology factor. These findings suggest that there is some specificity in the associations of psychopathological dimensions and adverse outcomes. The risk of adverse outcomes likely depends to different degrees on influences other than psychopathology. A previous analysis of the NESARC that established the validity of the bifactor model of psychopathology examined four validators (personal income, disability income, pain and lifetime history of incarceration)37. It found large effects of the specific factors beyond the general factor, also suggesting specificity of associations between different psychopathological dimensions and adverse outcomes. Despite its valuable contribution, because this study combined current and lifetime outcomes and did not control for those outcomes at Wave 1, it did not assess the effects of psychopathology on the development of adverse outcomes.
The bivariate analyses showed a clear pattern of associations between all psychiatric disorders and adverse outcomes. Of the 180 ORs examined (18 disorders times 10 adverse outcomes), 166 (92.2%) were significantly above 1, which is greater than 18-fold the number of significant ORs (180*0.05=9) that would be expected by chance. Even in the rare cases where some disorders, such as alcohol or drug use disorders were associated with decreased odds of some adverse outcomes (physical component summary of the SF-12), these disorders were associated with increased risks for most adverse outcomes. Consistent with this pattern, there were no direct effects of individual disorders on adverse outcomes in the bifactor model, indicating that after taking into account the presence of other disorders and the broader dimensions of psychopathology, all psychiatric disorders were consistently associated with the adverse outcomes examined in this study.
From the clinical and preventive perspective, the results highlight the central role of comorbidity in accounting for associations between psychiatric disorders and their adverse functional consequences and the limitations of examining individual disorders in isolation. The findings raise the possibility that transdiagnostic interventions,38 which are directed at broad psychopathological dimensions, may have greater effects than those directed at individual disorders. The results are also consistent with the observation that remission of one disorder decreases the risk of new onset or relapse of other disorders39 and with evidence of transdiagnostic biomarkers.40 The recent identification of neurocircuitry associated with broad psychopathology factors is also consistent with the results and may suggest promising targets for therapeutic interventions.33, 34 Linking transdiagnostic domains such as affect, cognition and behavior and their underlying neurobiology with the adverse outcomes on which psychopathology exerts its strongest effects may also help identify novel therapeutic targets.
From the public health perspective, our findings suggest that studies which narrowly focus on disorder-specific outcomes may underestimate effects on functional outcomes. Some interventions may help improve several functional domains in addition to the individual’s symptoms. The study results further suggest that addressing public health crises as isolated disorder specific events may be less fruitful than addressing their shared neurobiological or environmental causes.
Our findings should be interpreted in light of some limitations. First, although Wave 1 of the NESARC examined a wide range of Axis I and Axis II psychiatric disorders, several disorders, including psychotic disorders and borderline personality disorder, were not included. However, the structure of psychiatric disorders seems to be robust to the inclusion of a broad range of disorders as indicators.8 Second, our list of adverse outcomes, although extensive and providing a consistent pattern of results, is not exhaustive. Third, despite its prospective design, because of the possibility of uncontrolled confounds, our study cannot establish causal relationships between psychiatric disorders and adverse outcomes. Last, our study examined associations between psychiatric disorders and adverse events over a 3-year period and the pattern of associations may differ over different time intervals.
Despite these limitations, the results underscore that associations between psychiatric disorders and adverse outcomes occur primarily through broad psychological dimensions. Understanding the biological and psychological mechanisms underlying these dimensions should yield important intervention targets to decrease the individual suffering and societal burden of psychiatric disorders.
Supplementary Material
Acknowledgments:
The National Epidemiologic Survey on Alcohol and Related Conditions was sponsored by the National Institute on Alcohol Abuse and Alcoholism and funded, in part, by the Intramural Program, NIAAA, National Institutes of Health. The sponsors had no additional role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies or the US government.
Footnotes
Conflict of Interest: The authors have no competing financial interests in relation to the work described in this manuscript.
References
- 1.Olfson M, Blanco C, Wall M, Liu SM, Saha TD, Pickering RP et al. National Trends in Suicide Attempts Among Adults in the United States. JAMA Psychiatry 2017; 74(11): 1095–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999–2014. NCHS Data Brief 2016; (241): 1–8. [PubMed] [Google Scholar]
- 3.O’Donnell JK, Gladden RM, Seth P. Trends in Deaths Involving Heroin and Synthetic Opioids Excluding Methadone, and Law Enforcement Drug Product Reports, by Census Region - United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017; 66(34): 897–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oquendo MA, Volkow ND. Suicide: A Silent Contributor to Opioid-Overdose Deaths. N Engl J Med 2018; 378(17): 1567–1569. [DOI] [PubMed] [Google Scholar]
- 5.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015; 112(49): 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Mortality and morbidity in the 21(st) century. Brookings Pap Econ Act 2017; 2017: 397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olfson M, Wall M, Liu SM, Schoenbaum M, Blanco C. Declining Health-Related Quality of Life in the U.S. Am J Prev Med 2018; 54(3): 325–333. [DOI] [PubMed] [Google Scholar]
- 8.Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F et al. Mental disorders and risk of suicide attempt: a national prospective study. Mol Psychiatry 2015; 20(6): 718–726. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, Hirschfeld RM et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry 2006; 163(9): 1561–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubio JM, Olfson M, Perez-Fuentes G, Garcia-Toro M, Wang S, Blanco C. Effect of first episode axis I disorders on quality of life. J Nerv Ment Dis 2014; 202(4): 271–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT et al. Mapping common psychiatric disorders: structure and predictive validity in the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry 2013; 70(2): 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry 1999; 56(10): 921–926. [DOI] [PubMed] [Google Scholar]
- 13.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry 2009; 14(11): 1051–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol 1999; 60(6): 790–799. [DOI] [PubMed] [Google Scholar]
- 15.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend 1997; 47(3): 171–185. [DOI] [PubMed] [Google Scholar]
- 16.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 2003; 71(1): 7–16. [DOI] [PubMed] [Google Scholar]
- 17.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend 1997; 44(2–3): 133–141. [DOI] [PubMed] [Google Scholar]
- 18.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend 1995; 39(1): 37–44. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE, QualityMetric I, New England Medical Center H, Health Assessment L. How to score version 2 of the SF-12 health survey (with a supplement documenting version 1). QualityMetric Inc. ; Health Assessment Lab: Lincoln RI; Boston Mass., 2005. [Google Scholar]
- 20.Rubio JM, Olfson M, Villegas L, Perez-Fuentes G, Wang S, Blanco C. Quality of life following remission of mental disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2013; 74(5): e445–450. [DOI] [PubMed] [Google Scholar]
- 21.Elbogen EB, Johnson SC. The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2009; 66(2): 152–161. [DOI] [PubMed] [Google Scholar]
- 22.Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res 2007; 16 Suppl 1: 19–31. [DOI] [PubMed] [Google Scholar]
- 23.Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. J Abnorm Psychol 2013; 122(4): 1142–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lt Hu, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal 1999; 6(1): 1–55. [Google Scholar]
- 25.Wall MM, Li R. Comparison of multiple regression to two latent variable techniques for estimation and prediction. Statistics in medicine 2003; 22(23): 3671–3685. [DOI] [PubMed] [Google Scholar]
- 26.Muthen LK, Muthen BO. Mplus User’s Guide Los Angeles, 1998–2006. [Google Scholar]
- 27.Hoertel N, Le Strat Y, Angst J, Dubertret C. Subthreshold bipolar disorder in a U.S. national representative sample: prevalence, correlates and perspectives for psychiatric nosography. J Affect Disord 2013; 146(3): 338–347. [DOI] [PubMed] [Google Scholar]
- 28.Newson R PUNAF: Stata module to compute population attributable fractions for cohort studies. http://ideas.repec.org/c/boc/bocode/s457193.html. Published October 15, 2010. Accessed September 14, 2018.
- 29.Crum RM, Mojtabai R, Lazareck S, Bolton JM, Robinson J, Sareen J et al. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry 2013; 70(7): 718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenland S, Drescher K. Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics 1993; 49(3): 865–872. [PubMed] [Google Scholar]
- 31.Gandal MJ, Haney JR, Parikshak NN, Leppa V, Ramaswami G, Hartl C et al. Shared molecular neuropathology across major psychiatric disorders parallels polygenic overlap. Science 2018; 359(6376): 693–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blanco C, Rubio J, Wall M, Wang S, Jiu CJ, Kendler KS. Risk factors for anxiety disorders: common and specific effects in a national sample. Depress Anxiety 2014; 31(9): 756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castellanos-Ryan N, Briere FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U et al. The structure of psychopathology in adolescence and its common personality and cognitive correlates. J Abnorm Psychol 2016; 125(8): 1039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry 2015; 72(4): 305–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goh KI, Choi IG. Exploring the human diseasome: the human disease network. Brief Funct Genomics 2012; 11(6): 533–542. [DOI] [PubMed] [Google Scholar]
- 36.Siever LJ. Neurobiology of aggression and violence. Am J Psychiatry 2008; 165(4): 429–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. Is there a general factor of prevalent psychopathology during adulthood? J Abnorm Psychol 2012; 121(4): 971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S et al. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA Psychiatry 2017; 74(9): 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blanco C, Wall MM, Wang S, Olfson M. Examining heterotypic continuity of psychopathology: a prospective national study. Psychol Med 2017; 47(12): 2097–2106. [DOI] [PubMed] [Google Scholar]
- 40.Pinto JV, Moulin TC, Amaral OB. On the transdiagnostic nature of peripheral biomarkers in major psychiatric disorders: A systematic review. Neurosci Biobehav Rev 2017; 83: 97–108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.