Abstract
Objective
Our study assessed the effectiveness of Interpersonal Psychotherapy (IPT) tailored for biomedical patients with depression and pain. IPT was compared to enhanced treatment as usual (E-TAU) among women with co-occurring depression and chronic pain presenting for care at a women’s health or family medicine practice. We hypothesized that women presenting to urban medical practices with depression and chronic pain would benefit from IPT tailored to address their needs to a greater degree than from E-TAU.
Methods
We conducted a randomized controlled psychotherapy trial of 61 women from 2 urban medical practices who met criteria for major depressive disorder and chronic pelvic pain. Participants were assigned to receive either 8 sessions of IPT or a facilitated psychotherapy referral to a community mental health center, and assessed for depression, social interactions, and pain at 0-, 12-, 24-, and 36-weeks, with score on the Hamilton Rating Scale for Depression as the primary outcome. Both intent-to-treat (ITT) and causal modeling analyses correcting for treatment attendance were conducted.
Results
ITT analyses were not significant. In causal modeling analyses, participants assigned to IPT showed significantly more improvement for depression and social interactions, but not for pain.
Conclusion
IPT may be a viable option as part of a comprehensive treatment program for women in medical practices with depression and chronic pain.
Clinical Trials Registration
Keywords: chronic pain, depression, psychotherapy, socioeconomic disadvantage, women
Introduction
Reproductive-aged women are among those at greatest risk for both depression [1] and chronic pain [2]. Mood disorders and pain-related chronic medical conditions are the two leading causes of decreased quality of life [3], with annual costs of chronic pain and depression estimated at $215 billion and $80 billion respectively in the United States [4, 5]. Moreover, treatment engagement, adherence, and outcomes consistently are worse for those with depression and pain than for those with depression alone. Specifically, patients with depression and chronic pain have more severe depression, longer time to remission, poorer remission rates, and more partial response rates [6–13] compared to patients with depression only. Women who have the added burden of socioeconomic disadvantage face poverty, low educational attainment, multiple life stressors and limited resources, in addition to factors likely interfering further with their treatment engagement and response, such as trauma exposure, chronic life stress, and poor health [14–16]. To meet these challenges, tailored approaches that are responsive to the complex, concurrent difficulties facing women with pain and depression are required.
Women living with socioeconomic disadvantage and African American women often report using their medical doctors as their primary resource for both physical and mental health care [17, 18], and indicate a preference for psychotherapy over medication for treatment of depression [19–21]. Interpersonal Psychotherapy (IPT) is an evidence-based, time-limited psychotherapy that focuses on interpersonal issues associated with both the onset and maintenance of depression [22, 23]. IPT is an effective treatment for individuals with physical illnesses [24–27], and patients in primary care and women’s health settings [28–31]. IPT also has been found to be an excellent fit for low-income women and women of color with multiple social adversities and limited support [29, 30, 32]. Given the strong outcomes for IPT among socioeconomically disadvantaged women with health related concerns, we conducted a preliminary study for women with depression and pain, using specific treatment adaptations to address pain and treatment engagement [33], Interpersonal Psychotherapy for depressed patients with pain (IPT-P). Results from the study showed improvements in depression and social function [34], leading us to our next step: a controlled trial of our adapted IPT, with an active comparison condition.
In the current study, we compared IPT-P to enhanced treatment as usual (E-TAU), in which participants were provided with facilitated referrals for psychotherapy in a community mental health center. We hypothesized that IPT-P would prove more effective than E-TAU for depression outcomes among women with depression and pain presenting to primary care and obstetrics and gynecology practices. Our primary outcome was the severity score on the Hamilton Rating Scale of Depression. We also hypothesized that IPT-P would yield significant improvements in social interactions, pain, and daily function compared to E-TAU.
Method
Settings and Participants
Women from two urban medical practices (obstetrics and gynecology and family medicine) were recruited between February, 2009 and September, 2011. We targeted women with chronic pelvic pain for several reasons: their elevated risk for under-treatment of depression [35–36]; the lack of studies assessing what treatments are effective among women with pelvic pain [37]; to reduce the heterogeneity of the types of pain interference experienced among participants; and because of the focus on women’s health in this study. Thus, women with chronic pelvic pain seeking routine medical care were the focus of recruitment efforts. Moreover, given that screenings were held in health clinic settings, patients generally were not seeking depression care independently. Multiple recruitment strategies were employed. First, eligibility screens were conducted by research assistants while patients were waiting to be seen in exam rooms. Second, patients who had been diagnosed by their provider with chronic pelvic pain were sent letters inviting them to contact study staff if they were interested in learning more about a study for women trying to cope with the stress of chronic pelvic pain. Third, signs were posted in clinic exam rooms, waiting rooms, and bathrooms, inviting women who were having trouble living with chronic pelvic pain to contact study staff.
Potential participants received an initial screening to determine eligibility for the baseline assessment. The brief initial screening included: 1) the PHQ-2 [38] to determine if there was significant depressed mood and/or anhedonia defined as a score ≥ 3; and 2) the SF-36 pain scale [39, 40] to determine if there was moderate or greater pain intensity, defined as a score ≥ 3, and moderate or greater pain interference, defined as a score ≥ 2. Those who screened positive on both scales were evaluated by the research assistants to determine whether they met initial study inclusion and exclusion criteria. Self-reported pain in the pelvic region for a minimum of three months and within reproductive age range (18–50 years) were required for inclusion. Exclusion criteria were: pregnancy (due to potential complications for assessment of pain); currently receiving individual psychotherapy; residing more than 60-minutes away from the medical center; and inability to complete the baseline assessment in English. Literacy was not an inclusion criterion. Research assistants read the questions aloud to patients having difficulty reading the research materials.
Women who met initial inclusion criteria were invited to meet with the clinical research coordinator who obtained informed consent, completed the baseline assessment, and determined final study eligibility. Participants were required to meet criteria for major depression using the Structured Clinical Interview for the DSM-IV (SCID) [41], and score ≥ 15 on the Hamilton Rating Scale for Depression - 17 (HRSD) [42]. Participants were excluded if on interview they reported imminent suicidal intent, or met criteria for current psychotic disorder, current alcohol or substance dependence, or Bipolar I Disorder. Participants continued taking medications as prescribed by their health care providers for the duration of the study. Participants were randomized by their use of antidepressant medication at baseline to minimize likelihood of outcomes due to medication. All procedures were approved by the university research subjects review board.
Description of the interventions
Participants were randomly assigned by a research assistant using a computerized program to either IPT-P or E-TAU. Urn randomization was used to control for presence or absence of antidepressant medication use at baseline. Urn randomization randomizes subjects in a dynamic fashion, with the probability of being assigned to a treatment group determined by the balance of the treatment groups at the time of treatment assignment, rather than fixed a priori as in block randomization, decreasing likelihood of research staff predicting treatment assignment and thus reducing selection bias.
Interpersonal psychotherapy for depressed patients with pain (IPT-P)
Interpersonal Psychotherapy for depression is traditionally delivered weekly for 16 sessions by targeting improvement of social function and social support to reduce depressive symptoms [22, 23]. IPT-P includes modifications to fit the needs of patients with pain in a medical setting and is especially targeted to improve engagement and acceptability for patients with pain who may not identify as depressed. We created two categories of modifications: those to increase access and engagement; and those designed to target pain specifically. Accessibility and engagement adaptations included: 1) reducing the number of treatment sessions from 16 to 8, based on previous work showing brief IPT is still effective [43]; 2) holding therapy sessions in the health care clinic rather than in a mental health clinic; and 3) allowing patients up to 36 weeks to complete the 8 sessions since many were unable to attend appointments weekly or even biweekly due to their pain conditions. Three adaptations were made to address pain. In IPT, patients select a problem area to focus the work and to guide the therapist in determining which strategies may be most useful. Traditionally there are four problem areas considered: interpersonal dispute, grief, role transition, and interpersonal sensitivity. Our first change was to add a new problem area, “change in healthy self”, because of the recurrent themes of struggling to cope with changes of their physical status and subsequent changes in roles, relationships, and functioning among women with pain. Second, as in Brief IPT, the traditional IPT problem area of interpersonal sensitivity was dropped because it requires longer, more in-depth therapy than what could realistically be accomplished in 8 sessions. Third, traditional behavioral pain management strategies such as activity pacing and relaxation training could be used if they mapped on to patients’ treatment goals, and were applied using an interpersonal context. Examples include taking regular walks with a friend or talking with a partner about how to implement activity pacing to manage chores at home.
IPT-P therapists attended two days of didactic training in IPT-P and received weekly supervision with audio-recording review for the duration of the project to ensure treatment fidelity. IPT therapists were active clinicians in the community mental health center who volunteered to participate in the study; all sessions were completed on-site at the medical clinics. Two of the study therapists were doctoral-level clinical psychologists, and two had master’s degrees, one in counseling and one in marriage and family therapy.
Enhanced treatment as usual (E-TAU)
Patients assigned to E-TAU, or Enhanced Support and Connection to Care, met with a care coordinator, who was a graduate student in counseling, to discuss their personal concerns, needs, and priorities. Together with the care coordinator, the patient determined what local treatment facility and type of clinician would be the best match for her particular needs. The care coordinator then worked with the participant to facilitate connection, such as helping to schedule an initial appointment, calling to remind the participant of the appointment, and following up to see how the initial appointment went. Once the participant engaged in depression treatment, the care coordinator called monthly to assess her status and determine if any further assistance was needed to ensure she remained engaged in treatment. Frequency and intensity of treatment was determined by the treating clinician and tracked by study staff.
Consent and Assessment Procedures
Assessments were completed at baseline, 12, 24, and 36 weeks either at the medical clinic or in the patient’s home, depending on the patient’s preference. Transportation was provided for assessments when needed. Follow-up assessments were completed by telephone when participants were unable to meet in person. Monthly phone calls, birthday and holiday cards, and quarterly newsletters were used to encourage retention. Participants were reimbursed $40 for the baseline assessment and $25 for follow-up assessments.
Measures
In addition to the outcome measures described below, information about the women’s race, ethnicity, income, diagnoses, and medications was obtained. Satisfaction: The Client Satisfaction Questionnaire-8 [44] was used to assess participants’ satisfaction with the interventions.
Depression
In order to obtain a comprehensive assessment of depression, the clinician-rated Hamilton Rating Scale for Depression (HRSD) [42], the primary outcome, and the self-report Beck Depression Inventory (BDI) [45] were used to evaluate depressive symptom severity. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-IV) [41] was used to determine study eligibility by evaluating presence or absence of major depression diagnosis but was not used as an outcome. The complete SCID-IV was administered to ascertain presence or absence of other Axis I disorders. The assessors administering the HRSD and SCID were trained to criterion using standardized videotaped interviews, and inter-rater reliability of α ≥ .80 was obtained. Interviews were then audiotaped and reviewed by the PI to monitor reliability.
Social Interactions
Changes in social interactions were assessed by the Inventory of Interpersonal Problems (IIP) [46].
Pain
Pain severity and interference on the Multidimensional Pain Inventory (MPI) [47] was used to evaluate participants’ pain intensity and impact on daily pain function.
Data Analysis
Response to treatment was first investigated with an intent-to-treat (ITT) approach. Generalized estimating equations [48, 49] were used to compare change over time between the two treatment groups. We used GEE assuming an exchangeable correlation matrix to address the correlated responses in the data. If the subject is not assessed at a follow-up point, the outcome variable is assigned a missing value. The GEE approach is widely used due to its less stringent distributional assumptions and robustness properties, yielding valid inferences regardless of the data distribution. The significance level of statistical hypothesis tests was set as 0.05. Baseline antidepressant use (present/absent) was controlled in all analyses; pain and social interaction analyses only were adjusted for baseline HRSD scores.
ITT analyses, which include patients who received no treatment or incomplete treatment, run the risk of underestimating the effects of the intervention for those who were actually exposed to it [50]. To address the post-randomization confound of differences in treatment participation on treatment differences (51,52), we also conducted the potential outcome based causal models[49]. This approach accounts for varying degrees of participation in the intervention group. In contrast, the ITT approach ignores treatment participation variability and its influences on treatment effects. In this respect, causal models take into account individual-level treatment compliance at post-randomization and provide treatment effects at a higher granular level. We first modeled the level of IPT-P participation, or number of treatment sessions attended, using a generalized logit model with age, race, income, anti-depressants and education as predictors. Next, we imputed the level of participation for every subject in the E-TAU group based on the predictors above using this “dosage” model and compared the two groups within comparable participation strata. Thus, we defined the participation strata by the actual (for IPT-P) and predicted (for E-TAU) number of sessions attended. Then we incorporated all the weights into our causal models. Therefore, in the second stage of analyses, we conducted analyses with causal models that were weighted by participants’ actual or predicted treatment session dosage. Greater weight was assigned to participants who attended more treatment sessions and less weight was assigned to those who attended fewer sessions. This approach accounts for varying degrees of participation in the intervention group.
Results
Participants
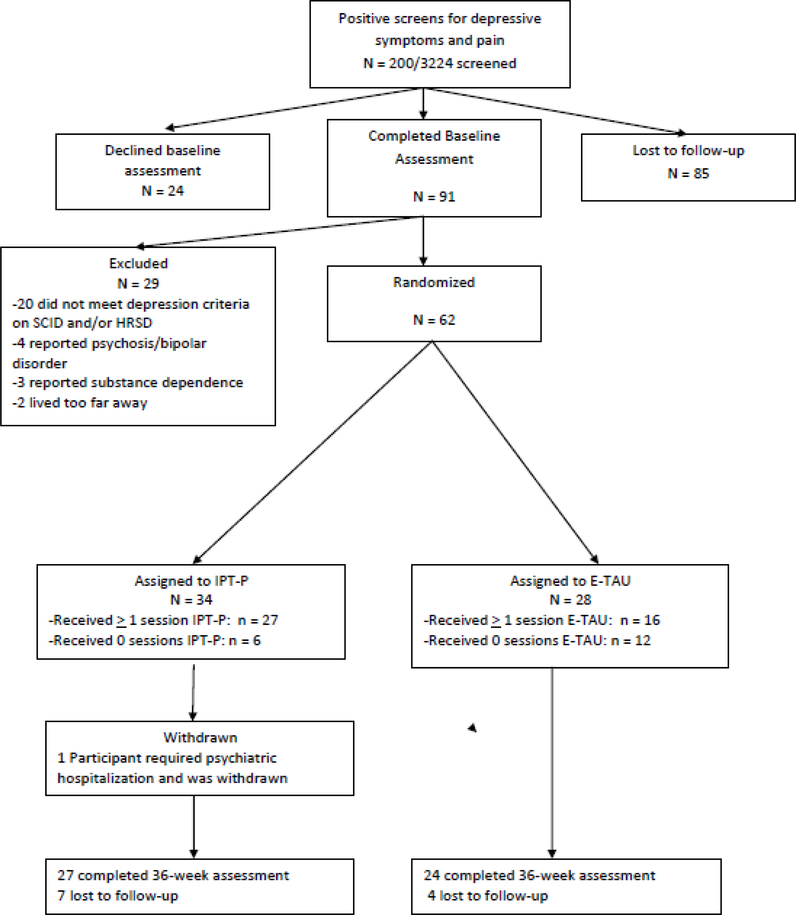
A total of 200 of 3224 (6.2%) women had positive screens and were referred for a baseline assessment (Figure 1). Of those, 85 (42.5%) failed to complete the baseline assessment and were not enrolled, and 24 (12.0%) declined to participate.
Figure 1:
CONSORT diagram
Of the remaining 93 women, 31 (33.3%) were excluded due to subthreshold depression symptoms (n = 20), psychotic or bipolar symptoms (n = 4), substance dependence (n = 3), or distance from the hospital interfering with their ability to attend regular psychotherapy appointments (n = 2). As a result, 62 enrolled, with 34 assigned to IPT-P and 28 assigned to E-TAU. One IPT-P participant was withdrawn from the study when she no longer met inclusion criteria due to reporting psychosis and she required hospitalization. Women in the IPT-P group reported a trend toward more pain interference at baseline compared to women in the E-TAU group (p=.06). No other differences were identified between the two treatment groups. Sociodemographics are reported in Table 1.
Table 1.
Descriptive information
| IPT-P | E-TAU | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N = 33 | n = 28 | n = 61 | ||||||||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||||||||||
| Age (years) | 36.3 (8.2) | 37.1 (9.8) | 36.7 (8.9) | |||||||||
| Race/Ethnicity | n (%) | n (%) | n (%) | |||||||||
| AA/Black | 22 (66.7) | 18 (64.3) | 40 (65.6) | |||||||||
| White/Caucasian | 3 (9.1) | 7 (25.0) | 10 (16.4) | |||||||||
| Hispanic | 6 (18.2) | 2 (7.1) | 8 (13.1) | |||||||||
| Biracial | 1 (3.6) | 1 (3.0) | 2 (3.3) | |||||||||
| Native American | . | 1 (3.0) | 1 (1.6) | |||||||||
| Marital Status | ||||||||||||
| Not partnered | 22 (66.7) | 21 (75.0) | 43 (70.5) | |||||||||
| Household Income | ||||||||||||
| <$20,000/year | 22 (66.7) | 16 (59.3) | 38 (63.3) | |||||||||
| Education | ||||||||||||
| < high school degree | 11 (33.3) | 10 (35.7) | 22 (34.4) | |||||||||
| High school degree or equivalent | 7 (21.2) | 7 (25.0) | 14 (23.0) | |||||||||
| Education beyond high school degree | 15 (45.5) | 11 (39.3) | 26 (42.6) | |||||||||
| Baseline antidepressant medication use | ||||||||||||
| 6 (18.2) | 7 (25.0) | 13 (31.3) | ||||||||||
| Baseline Depression Severity | ||||||||||||
| HRSD | 18.4 (3.5) | 18.3 (4.2) | 18.4 (3.8) | |||||||||
| BDI | 29.5 (9.3) | 29.4 (8.5) | 29.5 (8.9) | |||||||||
| Baseline Interpersonal Sensitivity | 1.8 (0.8) | 2.2 (0.8) | 2.0 (0.8) | |||||||||
| Baseline Pain Interference+ | 4.1 (0.8) | 3.7 (0.6) | 3.9 (0.7) |
Notes. HRSD = Hamilton Rating Scale for Depression; BDI = Beck Depression Inventory; Interpersonal Sensitivity measured on the Inventory of Interpersonal Problems; Pain Interference measured on the Multidimensional Pain Inventory
p<.10 difference between treatment groups at baseline.
Women generally reported depression in the moderate to severe range (BDI mean = 29.5, SD = 8.9; HRSD mean = 18.4, SD = 3.8). Women reported a diverse array of diagnoses potentially causing chronic pelvic pain. The most commonly reported were: fibroids (n = 13, 21.3%), endometriosis (n = 10, 16.4%), pelvic inflammatory disease (n = 6, 9.8%), pelvic adhesions (n = 5, 8.2%), and interstitial cystitis (n = 5, 8.2%). Many women also met criteria for co-occurring psychiatric diagnoses, including pain disorder (n = 44, 72.1%), specific phobia (n = 24, 39.3%), post-traumatic stress disorder (n = 22, 36.1%), panic disorder (n = 20, 32.8%), social phobia (n = 18, 29.5%), generalized anxiety disorder (n = 16, 26.2%), obsessive compulsive disorder (n = 6, 9.8%), and somatization disorder (n = 4, 6.6%).
Outcomes
Fifty-one women (83.6%; IPT-P n = 27; E-TAU n = 24) completed the 36-week post-treatment assessment. In terms of satisfaction at the final assessment, 14 of 20 (70.0%) of E-TAU participants and 17 of 19 (89.5%) IPT-P participants felt the intervention helped them somewhat or a great deal; 14 of 19 (73.6%) of E-TAU participants and 16 of 19 (84.2 %) of IPT-P participants reported that they were mostly or very satisfied with the treatment received. Four E-TAU and 8 IPT-P participants did not answer all the satisfaction questions. Descriptive results for outcome variables at each time point are presented in Table 2.
Table 2.
Descriptive outcomes of 61 women with chronic pelvic pain and depression using Interpersonal Psychotherapy for Depressed Patients with Pain (IPT-P) vs. Enhanced Treatment as Usual (E-TAU)
| IPT-P | E-TAU | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure and time point | M | SD | n | M | SD | n | ||||||||
| Depression | ||||||||||||||
| Hamilton Rating Scale for Depression | ||||||||||||||
| Baseline | 18.4 | 3.5 | 33 | 18.3 | 4.2 | 28 | ||||||||
| 12 weeks | 14.9 | 6.2 | 25 | 18.2 | 4.0 | 26 | ||||||||
| 24 weeks | 16.2 | 6.0 | 18 | 16.9 | 5.9 | 23 | ||||||||
| 36 weeks | 13.6 | 7.8 | 27 | 15.4 | 9.0 | 24 | ||||||||
| Beck Depression Inventory | ||||||||||||||
| Baseline | 29.5 | 9.3 | 33 | 29.4 | 8.5 | 28 | ||||||||
| 12 weeks | 23.9 | 10.2 | 25 | 27.9 | 10.2 | 25 | ||||||||
| 24 weeks | 23.4 | 9.7 | 19 | 25.4 | 9.4 | 23 | ||||||||
| 36 weeks | 21.9 | 13.3 | 26 | 23.6 | 12.3 | 24 | ||||||||
| Interpersonal Function | ||||||||||||||
| Interpersonal Sensitivity | ||||||||||||||
| Baseline | 1.8 | 0.8 | 33 | 2.2 | 0.8 | 28 | ||||||||
| 12 weeks | 1.6 | 0.8 | 24 | 2.0 | 0.9 | 24 | ||||||||
| 24 weeks | 1.6 | 0.9 | 19 | 1.9 | 1.1 | 23 | ||||||||
| 36 weeks | 1.3 | 0.7 | 22 | 1.8 | 1.0 | 23 | ||||||||
| Lack of Sociability | ||||||||||||||
| Baseline | 1.7 | 1.1 | 33 | 1.9 | 0.9 | 28 | ||||||||
| 12 weeks | 1.7 | 0.9 | 24 | 1.7 | 0.8 | 24 | ||||||||
| 24 weeks | 1.5 | 0.8 | 19 | 1.5 | 1.0 | 23 | ||||||||
| 36 weeks | 1.7 | 1.0 | 22 | 1.3 | 0.7 | 23 | ||||||||
| Interpersonal Ambivalence | ||||||||||||||
| Baseline | 1.1 | 0.9 | 33 | 1.7 | 0.9 | 28 | ||||||||
| 12 weeks | 1.4 | 1.1 | 24 | 1.6 | 0.8 | 24 | ||||||||
| 24 weeks | 1.3 | 1.0 | 19 | 1.8 | 1.0 | 23 | ||||||||
| 36 weeks | 1.1 | 0.7 | 22 | 1.5 | 0.7 | 23 | ||||||||
| Aggression | ||||||||||||||
| Baseline | 1.2 | 0.9 | 33 | 1.8 | 1.2 | 28 | ||||||||
| 12 weeks | 1.1 | 0.8 | 24 | 1.8 | 1.2 | 24 | ||||||||
| 24 weeks | 1.2 | 1.0 | 19 | 1.5 | 1.3 | 23 | ||||||||
| 36 weeks | 0.7 | 0.7 | 22 | 1.5 | 1.4 | 23 | ||||||||
| Need for Social Approval | ||||||||||||||
| Baseline | 1.6 | 1.0 | 33 | 2.1 | 0.9 | 28 | ||||||||
| 12 weeks | 1.9 | 0.9 | 24 | 1.8 | 0.9 | 24 | ||||||||
| 24 weeks | 1.6 | 1.0 | 19 | 1.7 | 0.9 | 23 | ||||||||
| 36 weeks | 1.4 | 0.9 | 22 | 1.7 | 0.9 | 23 | ||||||||
| Pain | ||||||||||||||
| Pain Severity | ||||||||||||||
| Baseline | 4.6 | 1.0 | 33 | 4.2 | 1.2 | 28 | ||||||||
| 12 weeks | 4.6 | 1.2 | 24 | 4.1 | 1.0 | 25 | ||||||||
| 24 weeks | 4.5 | 0.9 | 19 | 3.9 | 1.0 | 23 | ||||||||
| 36 weeks | 4.2 | 1.2 | 23 | 3.7 | 1.6 | 23 | ||||||||
| Pain Interference | ||||||||||||||
| Baseline | 4.1 | 0.8 | 33 | 3.7 | 0.6 | 28 | ||||||||
| 12 weeks | 3.9 | 0.8 | 24 | 3.7 | 0.9 | 25 | ||||||||
| 24 weeks | 4.1 | 0.6 | 19 | 3.6 | 0.8 | 23 | ||||||||
| 36 weeks | 3.9 | 1.0 | 23 | 3.5 | 1.2 | 23 |
Notes. Interpersonal function measured on the Inventory of Interpersonal Problems; Pain measured on the Multidimensional Pain Inventory.
Intent to treat analyses
Intent to treat analyses using Generalized Estimating Equations (GEE) showed no significant intervention effects for any of the outcomes assessed, including BDI, HRSD, MDD diagnosis, MPI pain, or IIP social interactions (specific results are not reported in the tables).
Causal modeling analyses
Consistent with our data analytic plan to address the potential post-randomization confound of differences in treatment participation, we next checked the distribution of number of treatment sessions for each treatment group. As anticipated, differences were noted in the amount of treatment received by women in the IPT-P group as compared to women in the E-TAU group and found they differed at p<.06 (Table 3). For example, 44.4% of E-TAU participants received no treatment, compared to 18.2% of IPT-P participants.
Table 3.
Sessions attended Interpersonal Therapy for Depressed Patients with Pain (IPT-P) compared to Enhanced Treatment as Usual (E-TAU) using repeated Analysis of Variance analyses.
| Weeks | IPT-P | E-TAU | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||||||
| 12 | 1.2 (0.7) | 0.9 (0.6) | 0.028 | ||||||
| 24 | 2.3 (1.3) | 1.7 (1.5) | |||||||
| 36 | 3.5 (1.6) | 2.3 (1.9) | |||||||
To address the post-randomization confound of differences in treatment participation, we then conducted causal models. We first modeled the level of IPT-P participation, or number of treatment sessions attended, using a generalized logit model with age, race, income, anti-depressants and education as predictors. Next, we imputed the level of participation for every subject in the E-TAU group based on the predictors above using this “dosage” model and compared the two groups within comparable participation strata. Intervention assignment was random, and therefore relationships between baseline predictors and participation are expected to be the same irrespective of assigned treatment condition [51]. Thus, we defined the participation strata by the actual (for IPT-P) and predicted (for E-TAU) number of sessions attended. Those with greater participation were then weighted more than those with less participation in comparing the two treatment groups, in order to calculate results that take the actual treatment received into consideration. Because of the trend found toward baseline differences in pain severity, we examined time X treatment group interaction effects for the pain outcomes only.
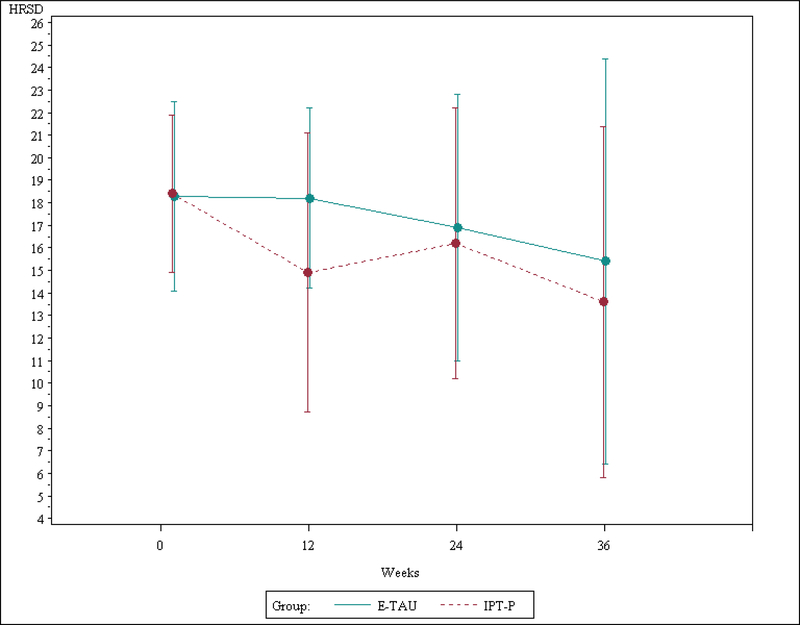
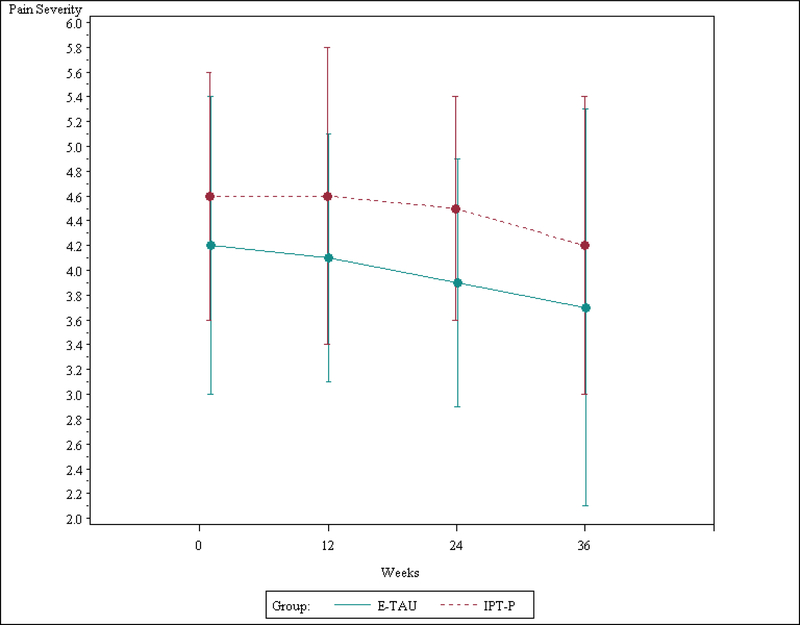
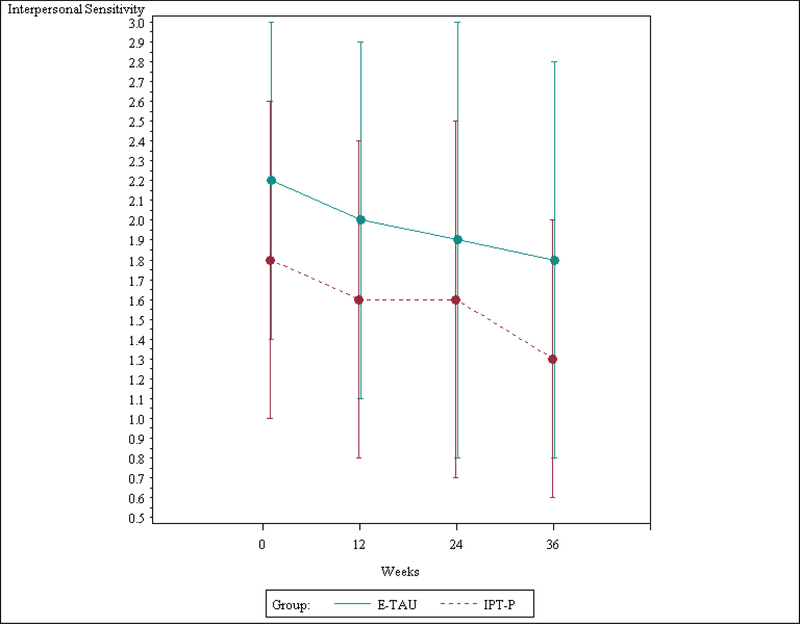
The causal models showed that at post-treatment, women assigned to IPT-P had significantly lower adjusted depression scores, significantly lower occurrence of major depressive disorder, and significantly less interpersonal sensitivity, interpersonal ambivalence, and aggression than women assigned to E-TAU (Table 4; Figures 2–4). The analyses did not find any significant differences by intervention for pain.
Table 4.
Causal model analyses comparing outcomes of Interpersonal Psychotherapy for Depressed Patients with Pain to Enhanced Treatment as Usual among 61 women with chronic pelvic pain and depression
| Causal Models | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | Standard Error | |||||||||
| Depression | ||||||||||
| Hamilton Rating Scale for Depression | ||||||||||
| Treatment group | 2.1533* | 1.048 | ||||||||
| Time | −0.012** | 0.004 | ||||||||
| Beck Depression Inventory | ||||||||||
| Treatment group | 3.887* | 2.186 | ||||||||
| Time | −0.022** | 0.007 | ||||||||
| Major Depressive Disorder Diagnosis | ||||||||||
| Treatment group | 0.187* | 0.098 | ||||||||
| Time | −0.001 | 0.000 | ||||||||
| Interpersonal Function | ||||||||||
| Interpersonal Sensitivity | ||||||||||
| Treatment group | 0.247* | 0.144 | ||||||||
| Time | −0.001* | 0.001 | ||||||||
| Lack of Sociability | ||||||||||
| Treatment group | −0.082 | 0.140 | ||||||||
| Time | −0.001 | 0.001 | ||||||||
| Interpersonal Ambivalence | ||||||||||
| Treatment group | 0.434** | 0.139 | ||||||||
| Time | −0.002** | 0.001 | ||||||||
| Aggression | ||||||||||
| Treatment group | 0.565** | 0.204 | ||||||||
| Time | −0.001* | 0.001 | ||||||||
| Need for Social Approval | ||||||||||
| Treatment group | 0.163 | 0.179 | ||||||||
| Time | −0.001* | 0.001 | ||||||||
| Pain | ||||||||||
| Pain Severity | ||||||||||
| Treatment group | −0.488 | 0.301 | ||||||||
| Time X Treatment Group | −0.001 | 0.002 | ||||||||
| Pain Interference | ||||||||||
| Treatment group | −0.331 | 0.198 | ||||||||
| Time X Treatment Group | −0.001 | 0.002 |
Notes.
p<.05 difference between treatment groups
p <.01 difference between treatment groups
Estimate for treatment group is interpreted as group difference; Estimate for time X treatment group is interpreted as group change over time; Reference group is the IPT-P group; All analyses controlled for age, baseline antidepressant medication use, and session attendance; social function and pain analyses also controlled for baseline Hamilton Rating Scale for Depression score; Interpersonal Function was measured on the Inventory of Interpersonal Problems; Pain was measured on the Multidimensional Pain Inventory.
Figure 2.
Outcomes on the Hamilton Rating Scale for Depression for Interpersonal Psychotherapy for Depressed Patients with Pain (IPT-P) vs. Enhanced Treatment as Usual (E-TAU).
Note. The bars above and below the means in the plot are standard deviations.
Figure 4.
Outcomes on the Multidimensional Pain Inventory Pain Severity scale for Interpersonal Psychotherapy for Depressed Patients with Pain (IPT-P) vs. Enhanced Treatment as Usual (E-TAU).
Note. The bars above and below the means in the plot are standard deviations.
Discussion
In sum, patients assigned to receive IPT-P demonstrated greater satisfaction and significantly better outcomes for depression and social interactions than patients assigned to receive E-TAU after correcting for variability in treatment attendance; no significant differences were found for pain outcomes. Moreover, results suggest IPT-P can be used effectively for patients who traditionally are under-represented in treatment: women with chronic pain presenting to medical settings and not seeking out depression treatment. These findings are notable given the generally poor outcomes similar patients have shown in response to other existing depression treatments [52–53]. Moreover, the findings suggest IPT-P may be a viable option for low-income, predominantly African American women. The variability in treatment engagement, and, consequently, the dose received, among participants in both groups highlights the challenges in engaging patients with depression and pain in psychotherapy. Yet our findings suggest that even with facilitated access and outreach, women with depression and chronic pain responded significantly better to IPT-P compared to conventional approaches to psychotherapy.
We were surprised to find pain did not improve despite improvements in depression and social interactions, as we expected these domains would be tightly linked. While it is possible that IPT has no effect on pain, there are several other potential interpretations as well. It may be that additional medical or rehabilitation treatments for pain are necessary in combination with IPT-P. Several other interpretations are also possible. Perhaps change in pain follows change in depression, and our follow-up phase was not sufficiently long to detect change. If this is the case, patients would be more likely to respond to pain-specific treatments once their depression and social interactions are improved. Another alternative explanation may be that the IPT-P received was not of high enough intensity and duration to achieve change in pain, which is notoriously difficult to improve [52–53].
Despite significant improvements in the IPT-P group, most participants received a limited dose of treatment and depression scores remained elevated in both groups after treatment. In other words, while IPT-P was more beneficial than E-TAU, it was not sufficient to lead to the remission of depression among most study participants. Our sample size was too small to determine if subgroups of patients were more or less likely to benefit from IPT-P. These positive yet modest findings are consistent with other studies of IPT for depression in predominantly low-income and racially diverse samples of adults [32, 54] and psychotherapy studies for patients with depression and chronic pain [7, 11]. Brief psychotherapy alone may not be sufficient to address the multiple issues contributing to the development and maintenance of depressive symptoms in the targeted sample of patients. Consistent with evolving patient-centered medical home models, patients with complex presentations, such as patients with comorbid depression and chronic pain, may benefit from comprehensive programs that include collaborative teams of physicians, social workers, outreach workers, and psychotherapists that include psychotherapies like IPT-P as one potential component of a treatment plan.
Several limitations of this study warrant comment. Generalizability of the findings is compromised in several ways. Our recruitment differed from most psychotherapy studies in that we targeted socioeconomically disadvantaged women in medical settings with pelvic pain who were not seeking mental health treatments; findings might be different if a treatment-seeking sample were studied. Our sample was small and quite heterogeneous in terms of pain diagnoses, psychiatric comorbidities, and onset and course of their disorders. Despite relatively broad inclusion/exclusion criteria, only 2% of patients at the two sites were eligible. Many women who screened positive for the study did not complete the eligibility process. Because changes in pharmacotherapies over the course of the trial were not controlled in an effort to improve external validity, changes in medications over the course of the study could be responsible, at least in part, for the outcomes. The E-TAU intervention was not standardized and varied between patients. Moreover, the additional outreach and support provided for E-TAU patients may have affected engagement and outcomes for this group. Randomization failed for pain levels at baseline, and patients in the IPT-P group started the trial with a trend toward more pain.
Conclusions
Study findings demonstrate IPT-P was acceptable and generate the hypothesis that it was effective for improvement of depression and social interactions among patients with depression and chronic pain. The study findings therefore suggest that IPT-P may be a viable option as part of a comprehensive treatment program for this patient population. These findings are also important because untreated depression can interfere with adherence and response to pain treatments [55, 56]. Thus, by identifying and treating depression among patients with pain, we may reduce the overall burden of disease in this population. Additional research is needed to determine how we can improve pain outcomes and decrease depression for this challenged, high-risk, underserved population.
Figure 3.
Outcomes on the Interpersonal Sensitivity Scale for Interpersonal Psychotherapy for Depressed Patients with Pain (IPT-P) vs. Enhanced Treatment as Usual (E-TAU).
Note. The bars above and below the means in the plot are standard deviations.
Highlights.
Two approaches to treating women with depression and chronic pelvic pain are compared.
Study participants reported both treatments to be acceptable.
Interpersonal Psychotherapy showed positive outcomes using causal modeling.
Acknowledgements
This work was supported by grant K23-MH079347 from the National Institute of Mental Health. We are grateful to Catherine Cerulli, JD, PhD, Yeates Conwell, MD, Hugh Crean, PhD, Tara Gellasch, MD, and Marsha Wittink, MD, for their suggestions on an earlier draft of this paper.
Footnotes
Competing Interest Statement: “All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf and declare that (1) [authors] received support from [name of company or other competing interest] for the submitted work; (2) [authors] have [specify relationships] with [name of companies or other competing interests] in the past three years that could be perceived to constitute a conflict of interest; (3) spouses, partners, or children of [authors] have [specified] financial relationships that may be relevant to the submitted work; and (4) [authors] have [specify type of relationship] non-financial interests that may be relevant to the submitted work.” If there are no competing interests to report, the authors should state: “The authors have no competing interests to report.”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Miranda J, & Green BL (1999). The need for mental health services research focusing on poor young women. Journal of Mental Health Policy and Economics, 2(2): p. 73–80. [DOI] [PubMed] [Google Scholar]
- 2.Poleshuck EL, & Green CR (2008). Socioeconomic disadvantage and pain. Pain, 136(3): 235–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandez A, et al. (2010). Burden of chronic physical conditions and mental disorders in primary care. British Journal of Psychiatry, 196: 302–309. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg PE, et al. (2003). The econmoic burden of depression in the Univted States: How did it change between 1990 and 2000? Journal of Clinical Psychiatry, 64(12): 1465–1475. [DOI] [PubMed] [Google Scholar]
- 5.American Academy, o.O.S. (1999). Musculoskeletal conditions in the United States. American Academy of Orthopaedic Surgeons Bulletin, 47: 34–36. [Google Scholar]
- 6.Poleshuck EL, et al. (2009). Pain as a predictor of depression treatment outcomes in women with childhood sexual abuse. Comprehensive Psychiatry, 50(3): 215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bair MJ, et al. (2004). Impact of pain on depression treatment response in primary care. Psychosomatic Medicine, 66(1): 17–22. [DOI] [PubMed] [Google Scholar]
- 8.Thielke SM, et al. (2007). Pain limits the effectiveness of collaborative care for depression. American Journal of Geriatric Psychiatry, 15(8): 699–707. [DOI] [PubMed] [Google Scholar]
- 9.Kroenke K, et al. (2008). Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain, 134(1–2): 209–15. [DOI] [PubMed] [Google Scholar]
- 10.Mavandadi S, et al. (2007). Effect of depression treatment on depressive symptoms in older adulthood: The moderating role of pain. Journal of the American Geriatrics Society, 55(2): 202–211. [DOI] [PubMed] [Google Scholar]
- 11.Karp JF, et al. (2005). Pain predicts longer time to remission during treatment of recurrent depression. Journal of Clinical Psychiatry, 66(5): 591–597. [DOI] [PubMed] [Google Scholar]
- 12.Leuchter AF, et al. (2010). Painful physical symptoms and treatment outcome in major depressive disorder: a STAR*D (Sequenced Treatment Alternatives to Relieve Depression) report. Psychological Medicine, 40(2): 239–251. [DOI] [PubMed] [Google Scholar]
- 13.DeVeaugh-Geiss AM, et al. (2010). The adverse effects of comorbid pain on depression outcomes in primary care patients: results from the ARTIST trial. Pain Medication, 11(5): 732–741. [DOI] [PubMed] [Google Scholar]
- 14.Almeida DM, et al. (2005). Do daily stress processes account for socioeconomic health disparities? Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60 Spec No 2: 34–39. [DOI] [PubMed] [Google Scholar]
- 15.Banks J, et al. (2006). Disease and disadvantage in the United States and in England. JAMA, 295(17): 2037–2045. [DOI] [PubMed] [Google Scholar]
- 16.Plichta SB, & Falik M (2001) Prevalence of violence and its implications for women’s health. Womens Health Issues, 11(3): 244–258. [DOI] [PubMed] [Google Scholar]
- 17.Miranda J, et al. (1998). Unmet mental health needs of women in public-sector gynecologic clinics. American Journal of Obstetrics and Gynecology, 178(2): 212–217. [DOI] [PubMed] [Google Scholar]
- 18.Scholle SH, et al. (2003). Addressing depression in obstetrics/gynecology practice. General Hospital Psychiatry, 25: 83–90. [DOI] [PubMed] [Google Scholar]
- 19.Alvidrez J, & Azocar F (1999). Distressed women’s clinic patients: preferences for mental health treatments and perceived obstacles. General Hospital Psychiatry, 21(5): 340–347. [DOI] [PubMed] [Google Scholar]
- 20.Cooper LA, et al. (2003). The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Medical Care, 41(4): 479–489. [DOI] [PubMed] [Google Scholar]
- 21.Dwight-Johnson M, et al. (2000). Treatment preferences among depressed primary care patients. Journal of General Internal Medicine, 15(8): 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stuart S, & Robertson M (2003). Interpersonal Psychotherapy: A clinician’s guide. New York: Arnold Publishers [Google Scholar]
- 23.Weissman MM, Markowitz JC, and Klerman GL (2000). Comprehensive Guide to Interpersonal Psychotherapy. New York: Basic Books. [Google Scholar]
- 24.Koszychi D, et al. (2004). An open-label trial of interpersonal psychotherapy in depressed patients with coronary disease. Psychosomatics, 45(4): 319–324. [DOI] [PubMed] [Google Scholar]
- 25.Markowitz JC, et al. (1998). Treatment of depressive symptoms in human immunodeficiency virus-positive patients. Archives of General Psychiatry, 55(5): 452–457. [DOI] [PubMed] [Google Scholar]
- 26.Miller MD, et al. (1996). Chronic medical illness in patients with recurrent major depression. American Journal of Geriatric Psychiatry, 4(4): 281–290. [DOI] [PubMed] [Google Scholar]
- 27.Ransom D, et al. (2008). Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons with depression: a pilot trial. Psychiatric Services, 59(8): 871–877. [DOI] [PubMed] [Google Scholar]
- 28.Wolf NJ, & Hopko DR (2008). Psychosocial and pharmacological interventions for depressed adults in primary care: a critical review. Clinical Psychology Review, 28(1):131–61. [DOI] [PubMed] [Google Scholar]
- 29.Spinelli MG, & Endicott J (2003). Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. American Journal of Psychiatry, 160(3): 555–562. [DOI] [PubMed] [Google Scholar]
- 30.Zlotnick C, et al. (2001). Postpartum depression in women receiving public assistance: Pilot study of an interpersonal-therapy-oriented group intervention. American Journal of Psychiatry, 158(4): 638–640. [DOI] [PubMed] [Google Scholar]
- 31.Schulberg HC, Raue PJ, and Rollman BL (2002). The effectiveness of psychotherapy in treating depressive disorders in primary care practice: clinical and cost perspectives. General Hospital Psychiatry, 24(4): 203–212. [DOI] [PubMed] [Google Scholar]
- 32.Grote NK, et al. (2009). A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatric Services, 60(3): 313–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poleshuck EL, Gamble SA, Cort N, Hoffman-King D, Cerrito B, Rosario-McCabe L, Giles DE (2010) Interpersonal psychotherapy for co-occurring depression and chronic pain. Professional Psychology: Research and Practice, 41: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poleshuck EL, et al. (2010). Interpersonal psychotherapy for women with comorbid depression and chronic pain. Journal of Nervous and Mental Disease, 198(8): 597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stones W, Cheong Y, and Howard F (2005). Interventions for treating chronic pelvic pain in women [review]. The Cochrane Database of Systematic Reviews, 4(31) Rosenthal R. Psychology of chronic pelvic pain. Obstetrics and Gynecology Clinics of North America, 20(4): 726–742. [Google Scholar]
- 36.Lorencatto C, Petta CA, Navarro MJ, Bahamondes L, and Matos A(2006). Depression in women with endometriosis with and without chronic pelvic pain. Acta Obstetricia et gynecologica Scandinavica, 85(1): 88–92. [DOI] [PubMed] [Google Scholar]
- 37.Meltzer-Brody S, & Leserman J (2011). Psychiatric comorbidity in women with chronic pelvic pain. CNS Spectrums, 16(2): ePub Ahead of Print [DOI] [PubMed] [Google Scholar]
- 38.Lowe B, Kroenke K, and Grafe K (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research, 58(2): 163–171. [DOI] [PubMed] [Google Scholar]
- 39.Ware JE, & Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Medical Care, 30: 473–483. [PubMed] [Google Scholar]
- 40.McHorney CA, Ware JE, and Raczek AE (1993). The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31: 247–263. [DOI] [PubMed] [Google Scholar]
- 41.First MB, Spitzer RL, Gibbon M, Williams JBW, and Benjamin L (1996).User’s Guide for the Structured Clinical Interview for DSM-IV Personality Disorders (SCID II). Washington DC: American Psychiatric Press Inc. [Google Scholar]
- 42.Hamilton M (1960).A rating scale for depression. Journal of Neurology, Nerosurgery and Psychiatry, 23: 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Swartz HA, et al. (2008). Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. American Journal of Psychiatry, 165(9): 1155–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Attkisson CC, Greenfield TC, and Maruish M (1994) The client satisfaction questionnaire-8 and the service satisfaction questionnaire-30The Use of Psychological Testing for Treatment Planning and Outcome Assessment, Erlbaum: Hillsdale, NJ. [Google Scholar]
- 45.Beck AT, et al. (1961), An inventory for measuring depression. Archives of General Psychiatry, 4: 561–571. [DOI] [PubMed] [Google Scholar]
- 46.Pilkonis PAK, Y., Proietti JM, and Barkham M (1996). Scales for personality disorders developed from the inventory of interpersonal problems. Journal of Personality Disorders, 10(4): 355–369. [Google Scholar]
- 47.Kerns RD, Turk DC, and Rudy TE (1985). The west haven-yale multidimensional pain inventory (WHYMPI). Pain, 23: 345–356. [DOI] [PubMed] [Google Scholar]
- 48.Liang KZ, SL. (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73: 13–22. [Google Scholar]
- 49.Tang W, He H and Tu XM (2012). Applied Categorical and Count Data Analysis. Florida: Chapman & Hall/CRC. [Google Scholar]
- 50.Dishion TJ, et al. (2008). The family check-up with high-risk indigent families: preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development, 79(5): 1395–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Frangakis CER, D. B. (2002). Principal stratification in causal inference. Biometrics, 58: 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.C de C Williams A, Eccleston C, and Morley S (2012). Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Pain, Palliative and Supportive Care Group Published Online: DOI: 10.1002/14651858.CD007407.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keller A, Hayden J, Bombardier C, and van Tulder M (2007). Effect sizes of non-surgical treatments of non-specific low-back pain. European Spine Journal, 16: 1776–1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Talbot NL, et al. (2011). A randomized effectiveness trial of interpersonal psychotherapy for depressed women with sexual abuse histories. Psychiatric Services, 62(4): 374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bair MJ, et al. (2003). Depression and pain comorbidity - A literature review. Archives of Internal Medicine, 163(20): 2433–2445. [DOI] [PubMed] [Google Scholar]
- 56.Detweiler-Bedell JB, et al. (2008). Integrating co-morbid depression and chronic physical disease management: identifying and resolving failures in self-regulation. Clinical Psychology Review, 28(8): 1426–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]