INTRODUCTION:
Over the past few decades, there has been an increase in the use of technology for the management of diabetes, primarily in the young and middle aged patients with type 1 diabetes (T1D). However, as technology has become more common, less expensive, and easier to use, its use has expanded to those with type 2 diabetes (T2D). In addition, in recent years, a growing number of older adults have started using technology to improve their diabetes. This phenomenon provides opportunities and challenges to understand the benefits and barriers in the use of technology in the aging population (Table 1). Currently, major advances in diabetes technology include: 1) insulin delivery systems as smart insulin pens and insulin pumps, 2) blood glucose monitoring as CGM, and 3) hybrid devices that combined glucose monitoring systems and insulin delivery systems1. The overall goal in the use of these technologies is to improve glycemic control, lower the risk of hypoglycemia, reduce the burden of living with diabetes, and improve quality of life2–7.
Table 1:
Diabetes Technology systems: Benefits and Challenges in Aging Population
| Technology Systems: | Benefits in Older Adults | Challenges in Older Adults |
| Insulin administration systems | ||
| Pump or CSII: |
|
|
| Bluetooth-enabled insulin pen: |
|
|
| Monitoring systems | ||
| CGM |
|
|
| Hybrid Systems |
|
|
In this article we review the evidence supporting the use of diabetes technologies in the older population and discuss recommendations based on current data and authors’ clinical knowledge and experience.
INSULIN DELIVERY SYSTEMS:
Insulin pens and Bluetooth enabled insulin pen:
Insulin pens have been a major advance in technology and have improved accuracy of insulin doses and ease of administration for patients who were using vial and syringe methods. Insulin pens are available as prefilled syringes, disposable or reusable with replaceable insulin cartridges that allow push-button injections. Some of these insulin pens have the ability to administer insulin by 0.5 Unit increment, improving the accuracy of dosing.
Recently, Bluetooth-enabled insulin pens (smart pens) have further improved this technology with their ability to record the dose and the time of the insulin delivery. In addition, some of these smart pens have built-in bolus calculators to help with insulin dosing calculations. . They also provide downloadable data reports to the clinicians and/or patients1. Until now, clinicians were adjusting insulin dosing based on blood glucose monitoring records, along with the assumption that the patient is taking their insulin as prescribed (both timing and dose). However, in patients with diabetes taking multiple insulin injection, omission or errors in doses and timing of insulin are fairly common8,9. The use of Bluetooth-enabled insulin pens in participants with T1D or T2D on insulin injection was shown to capture deviation from insulin prescriptions in a recent study10. Twenty two percent of the older sub-group in this study showed nonadherence with bolus insulin dosing, while 27% showed nonadherence with basal insulin administration. The study results also showed that the nonadherence measured by these methods was associated with poor glycemic control.
Benefits for older population:
Insulin pens are easier to use for older adults with vision impairment or dexterity problems compared to vial and syringes. Bluetooth-enabled pen can be used to assess missed or extra doses in patients with cognitive impairment. This information can be used by formal (aids or nurses) or informal (family members) caregivers to remind patients to take their insulin or eat meals on time. As mentioned above, some of the Bluetooth-enabled insulin pen systems has a built-in bolus calculator that can help with dosing calculation for those people who have difficulty with problem-solving. (Table 1)
Challenges in older adults:
Some older adults with cognitive decline have difficulty operating insulin pens, especially changing cartridges. There is also a problem with identifying missed or incorrect doses, as most pens do not have memory for given doses. The numbers on the pen are sometimes hard to read for visually-impaired patients. Although Bluetooth pens are better for some of these issues, they are much more expensive and some of the pens require the need for daily charging in order to keep system functioning. These additional steps add an extra level of complexity (Table 1 and 2)
Table 2:
Barriers to Technology Use in Older Adults
| Barriers | Glucose monitoring systems | Insulin delivery systems |
|---|---|---|
| Cognitive dysfunction |
|
|
| Dexterity problems |
|
|
| Visual impairment |
|
|
| Hearing impairment |
|
|
| Social Isolation / Lack of Support |
|
|
Insulin Pump or Continuous subcutaneous insulin infusion
Insulin pumps administer insulin continuously throughout the day. Most insulin pumps use tubing to deliver insulin through a cannula, while a few attach directly to the skin, without tubing (patch pump). This insulin delivery system is more accurate and precise than insulin administration via injections, and the amount of basal dose can be as small as 0.1U/hr. Insulin pumps have a bolus calculator that can determine bolus doses based on pre-programmed insulin to carbohydrate ratio, sensitivity factor, and set glucose target. Infusion sets are required to be changed every 2–3 days, requiring cannula insertion in the subcutaneous tissues and cartridge refill. Data can be downloaded from the pump and the reports can be reviewed by clinicians and can help identify problems such as missed doses or too many boluses causing stacking of insulin, often leading to hypoglycemia1.
Until recently, the use of insulin pump was mostly seen in younger adults and in those with type 1 diabetes. Large registry cohorts in this population have shown benefits of pump use by improvement in glucose control (A1C), reduction in hypoglycemia, and improvement in quality of life11,12. Several studies have evaluated the use of insulin pumps in the older population with T1D and T2D. A retrospective chart review to compare pump therapy in older and younger adults with T1D has shown similar benefits in both age groups in the risk of severe hypoglycemia and hospitalization13. Another retrospective study evaluating electronic medical records showed that the pump therapy can be used effectively and safely in carefully selected older adults with T1D14. A prospective, randomized study of older adults with T2D on either insulin pump or multiple daily injections (MDI) showed equal improvement in glucose variability over time with both modalities15. However, it did not show any difference between people using pump versus MDI in regards to glucose control, episodes of severe hypoglycemia, glucose variability, or treatment satisfaction.
Benefits in older adults:
Many older adults enjoy the convenience of insulin pumps, as they don’t need to carry multiple insulin pens with them. Although cost can be a problem, currently, all insulin pump systems are covered by Medicare, which is beneficial to the older population. (Table 1)
Challenges in older adults:
Obtaining and keeping up with various pump parts and supplies can be challenging at any age, but can be especially burdensome in older adults (Table 1 and 2). Although the Centers for Medicare & Medicaid Services (CMS) cover the expenses for insulin pump use in older adults with T1D, there is a caveat that the patients using the pump technology have a face-to-face encounter with a clinician every 3 months to receive disposable supplies needed for insulin pump use. A survey of older adults with T1D showed that obtaining supplies in a timely fashion remains a challenge16. More than 50% of the people interviewed in this study reported that because of these challenges, they changed pump-related behaviors such as leaving the infusion site in place longer than prescribed, reusing pump supplies, using injections to supplement pump use, or temporarily stopping the insulin pump use. As a consequence, there was an increased risk for adverse outcomes including more erratic blood glucose, irritation at insertion sites, and a greater number of episodes of hypoglycemia and hospitalizations.
Another major concern is the risk of diabetic ketoacidosis (DKA) associated with the insulin pump use. This risk is thought to be result of issues with infusion sets (dislodgement, occlusion). Although there are no studies specifically looking at the older population, risk of malfunction of pump and DKA needs careful consideration. (Table 1 and 2)
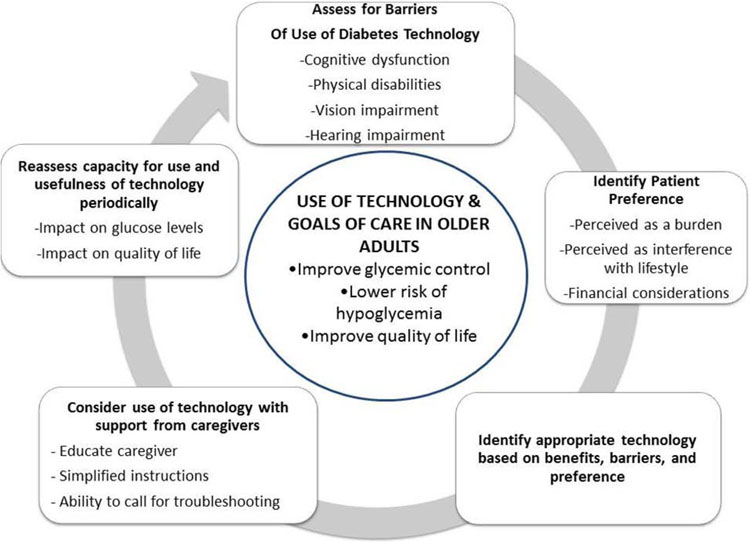
Aging is also associated with higher prevalence of number of conditions that interfere with diabetes self-care. Cognitive decline with aging is not uncommon and can impact mental flexibility and mental speed17. Patients with diminished mental flexibility and processing speed may do well with a simple regimen or technology, but may fail if the regimen is too complex or the technology requires multiple steps. In general, when patients develop cognitive dysfunction, they are less likely to be involved in diabetes self-care and glucose monitoring18. It is important to reassess patient’s ability to use inulin pumps periodically when cognitive decline is noted (Table 3 and Figure 1). Aging is associated with increased incidence of conditions such as osteoarthritis and tremors that can impact dexterity. A study conducted in people with T1D and T2D evaluating hand function and motoric performances showed that reduced skills are common in those people with diabetes, compared to the general population19. Assessment of dexterity in clinical practice is not part of diabetes-related clinical visit, and may result in a failure of insulin pump use if not considered beforehand. (Table 1 and 2). Vision and hearing impairment can also be barriers for many aspects of insulin pump use. Insulin pump screens may be difficult to see due to their small size and lack of magnification abilities. Alarms and alerts regarding malfunctions and reminders may be missed by those people with hearing difficulties.
Table 3:
Consideration for use of diabetes technology systems based on patient characteristics, health status, and glycemic goals
| Patient characteristics and Health status | Glycemic goal | Potential Benefits on Use of Diabetes Technology | Potential limitations of Use of Diabetes Technology |
|---|---|---|---|
| Healthy (few coexisting chronic illnesses, intact cognitive and functional status) | A1c goal 7.5% (58 mmol/mol) |
Bluetooth pen:
|
|
| Community-dwelling patients receiving care in a skilled nursing facility for short-term rehabilitation |
A1c is not a reliable measure, glycemic goal between 100–200 mg/dl (5.5–11 mmol/L) |
Pump:
|
Need to train staff at the facility |
| Very complex/poor health (long-term care or end stage chronic illnesses or moderate-to-severe cognitive impairment or 21 ADL dependencies) | A1c <8.5% (69 mmol/mol) |
Pump:
|
Need to train nursing home staff |
| Patients at end of life | avoid extreme of glucose level as hypo or hyperglycemia |
|
Figure 1.
Steps to consider in the Use of Diabetes Technology and Goals of Care in Older Adults to Improve Diabetes and Quality of Life Outcomes.
GLUCOSE MONITORING SYSTEMS
Self-monitoring of blood glucose (SMBG) is a key component of diabetes management. Older people with diabetes have been using SMBG values for several decades, however, this measure is a static value compared to the dynamic data obtained from the CGM, with information not only on the absolute value, but also trends. Over the last decade, CGM has dramatically improved in technology, ease of use, and accuracy. The real-time CGM (rtCGM), which continuously reports glucose levels and includes alarms for hypoglycemic and hyperglycemic excursions, is primarily used in the management of T1D. The professional CGM is used for pattern management and for assessment of glucose excursions in the management of both T1D and T2D. Two CGM devices are now approved by the FDA for making treatment decisions without SMBG confirmation, sometimes called non-adjunctive use1. A pivotal study conducted in 2008 showed that the use of CGM was associated with improved glycemic control, and lower risk of hypoglycemia in adults and children with T1D5. Similar results with improved glycemic control were also shown in two randomized controlled trials using CGM in adults with T1D and T2D using MDI7,20. A sub-analysis of this study evaluated the use of CGM versus usual self-monitoring in older adults (>60 years age) with T1D and T2D using MDI, and showed that 97% of the older participants used the CGM ≥ 6 days/week at 6 month, and the use of CGM was associated with improved glycemic control and glycemic variability21. Few small retrospective studies have evaluated use of CGM in older population in community setting. In 2014, a community endocrine practice looked at retrospective data on a small number of older adults (≥65 years of age) using CGM, at the time, when CGM was not covered by the Medicare, and found that the older patients using rtCGM had a lower A1c and fewer episode of severe hypoglycemia compared to non CGM users22.
Recently, the Wireless Innovation for Seniors With Diabetes Mellitus (WISDM trial) prospectively assessed the potential benefits and risks of CGM use in older adults (>60yrs) with T1D. The study showed a high retention rate up to 98% along with improvement in A1c, hypoglycemia (time spent < 70 mg/dl or 3.9 mmol/L) and severe hypoglycemia23.
A few studies have also evaluated the impact of CGM on quality of life by surveying patients using CGM. They have shown that in older adults with either T1D or T2D using CGM, rtCGM users had fewer moderate and severe hypoglycemic episodes, and greater reductions in severe hypoglycemia compared to non CGM users. The rtCGM users also reported significantly better well-being, less hypoglycemic fear, and less diabetes distress than non CGM users24,25.
Benefits in older adults:
rtCGM use in older adults has shown effectiveness in decreasing the risk of hypoglycemia. This is of particular importance, as hypoglycemia leads to poorer outcomes in older adults, due to its association with increased risks of falls and potential injury, myocardial infarcts, arrhythmias, temporary or permanent cognitive impairment, and death26–28. Older adults have a high risk of hypoglycemia unawareness and do not recognize many episodes of mild to moderate hypoglycemia, as they are asymptomatic29,30. Thus, alarms and alerts built in the CGM can help older patients to manage their hypoglycemia episodes in time and improve safety.
In addition, now there is an availability to use a smart device in conjunction with the CGM, which allows patients to enable mobile applications and use the SHARE feature. The SHARE application allows the user to share CGM data with up to five designated individuals who can monitor glucose levels remotely on compatible smart devices. This data-sharing capability can be helpful to caregivers of elderly and frail patients, especially if they have cognitive decline. (Table 1 and 2). In January 2017 the CMS had started providing coverage for rtCGM as durable medical equipment, which has helped to make this technology more affordable for older adults.
Challenges in older adults:
rtCGM provides an abundance of data, which sometimes creates challenges in troubleshooting and diabetes self-management decisions, especially in older adults. In addition, the constant problem-solving that is needed in interpreting and reacting to CGM readings can become a burden when other competing medical conditions or socio-economic problems arise.
In older adults with diabetes, Medicare covers the CGM, however, it requires limitation on the use of glucometer to only 3 fingerstick-checks per day. This limitation can be challenging in some, since SMBG has been used so diligently for many decades as a point of reference. Moreover, SMBG by glucometer are needed in certain situations e.g. CGM can have a warm-up period of a few hours where the patient does not have real time information regarding their glucose level, or when sensor glucose reads < 80 mg/dL or >250 mg/dL (<4.4 or >13.9 mmo/L) since CGM accuracy is reduced in these ranges.
As mentioned in the insulin delivery system discussion, cognitive decline and physical decline along with dexterity and visual impairment can be a challenge also in using CGM for older adults. In addition, hearing impairment, which is common in older subjects with diabetes, may interfere with hearing alarm and alert causing distress and impact appropriate use of the CGM system31 (Table 1 and 2). Some medications and comorbidities occurring frequently in older adults can also create problems. Older subjects are more likely to use medications that contain acetaminophen. The use of acetaminophen interferes with some of the sensors, making reading inaccurate (false hyperglycemic readings)32. Older adults with diabetes may also have altered renal function. However, thus far, CGM accuracy has not been tested for chronic kidney disease and eGFR <30 mg/ml/min.
GLUCOSE-RESPONSIVE INSULIN DELIVERY SYSTEM OR HYBRID SYSTEM
Two major class of glucose responsive insulin delivery system are currently on the market. The first is a sensor-augmented insulin pump that can automatically suspend insulin to prevent hypoglycemia33. The hybrid closed- loop systems (also called the artificial pancreas or automated insulin delivery systems) is the other one, that can modulate insulin delivery below and above the pre-set rate based on sensor glucose levels to mitigate both hyper- and hypoglycemia34. In the U.S., a system with predictive low glucose suspend (Tandem t:slim × 2 with Basal IQ) is approved by the Food and Drug Administration (FDA). Once covered by Medicare, this system will be available for use in older adults. The goal of the hybrid closed loop systems is to reduce the daily engagement by the person who wears it and provide help with the daily burden of diabetes decision-making, based on food intake (or lack thereof), exercise, and acute illnesses. There are no studies to assess the use of this technology in the older age group; however, a case-report highlights the potential power of this system in the older and frail population35. In this report, the use of closed loop insulin delivery systems was continued in a hospitalized individual during a period of terminal illness. Glucose control was kept within good range with minimal hypoglycemia while using a factory-calibrated CGM, which reduced the burden of SMBG measurements, and an insulin pump, which is less intrusive than insulin injections.
CONCLUSION:
Newer diabetes-related technologies, such as insulin pump and CGM, are being more commonly used in older adults with both T1D and T2D. Study data have shown that healthy older adults can use these technologies successfully and derive benefits through improvement of glycemic control and glucose variability, reduced hypoglycemia, and improvement of overall quality of life. However, aging brings challenges associated with competing medical conditions, comorbidities, polypharmacy, and cognitive and functional decline (Table 3). Careful evaluation and thoughtful discussion between clinicians, patients, and their caregivers should be performed to continually re-evaluate the use of technology and its benefits and burdens. If an older patient chooses to use technology, it is important to assess their support system and offer training and education to the caregivers. Figure 1 show the steps needed for successful use of technology with the overall goal of improved diabetes and quality of life outcomes.
KEY POINTS.
Recent studies have shown that the use of the technology for insulin administration (Insulin pump, insulin pens) and glucose monitoring (Continuous glucose monitoring (CGM)) can be used in older adults with type 1 and type 2 diabetes to improve glycemic control and quality of life, and reduce the risk of hypoglycemia.
Some medical conditions more commonly seen in older adults can act as barriers to the successful use of technology. These conditions, including cognitive and physical decline, can happen over time, or acutely after an illness.
Periodic assessment of cognitive and physical function, as well as overall health, is important in older adults using diabetes-related technologies.
Guidelines on the use of technology in older adults, impact of medical comorbidities, screening tests for these conditions, as well as educational material for clinicians, patients and caregiver are needed.
SYNOPSIS.
With successful aging of adults with type 1 diabetes, there is an increased opportunity to use technology for diabetes management. When used in appropriate patients, technology can ease the burden of self-care and provide a sense of security in older adults. However, age-related comorbidities, especially cognitive and physical decline, can make technology use difficult in older adults. Guidelines for the use of technology in the aging population are urgently needed, along with educational material for the clinicians caring for them and the caregivers helping them at home. In this article, we review the evidence supporting the use of diabetes-related technologies in the older population and discuss recommendations based on current data and authors’ clinical knowledge and experience.
Acknowledgment:
The authors thank Christine Slyne for editorial assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement: The authors have nothing to disclose.
Reference:
- 1.American Diabetes A. 7. Diabetes Technology: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019;42:S71–S80. [DOI] [PubMed] [Google Scholar]
- 2.Jeitler K, Horvath K, Berghold A, et al. Continuous subcutaneous insulin infusion versus multiple daily insulin injections in patients with diabetes mellitus: systematic review and meta-analysis. Diabetologia 2008;51:941–51. [DOI] [PubMed] [Google Scholar]
- 3.Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in Type 1 diabetes: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med 2008;25:765–74. [DOI] [PubMed] [Google Scholar]
- 4.Karges B, Schwandt A, Heidtmann B, et al. Association of Insulin Pump Therapy vs Insulin Injection Therapy With Severe Hypoglycemia, Ketoacidosis, and Glycemic Control Among Children, Adolescents, and Young Adults With Type 1 Diabetes. JAMA 2017;318:1358–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamborlane WV, Beck RW, Bode BW, et al. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–76. [DOI] [PubMed] [Google Scholar]
- 6.Lind M, Polonsky W, Hirsch IB, et al. Continuous Glucose Monitoring vs Conventional Therapy for Glycemic Control in Adults With Type 1 Diabetes Treated With Multiple Daily Insulin Injections: The GOLD Randomized Clinical Trial. JAMA 2017;317:379–87. [DOI] [PubMed] [Google Scholar]
- 7.Beck RW, Riddlesworth T, Ruedy K, et al. Effect of Continuous Glucose Monitoring on Glycemic Control in Adults With Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial. JAMA 2017;317:371–8. [DOI] [PubMed] [Google Scholar]
- 8.Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med 2012;29:682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brod M, Rana A, Barnett AH. Adherence patterns in patients with type 2 diabetes on basal insulin analogues: missed, mistimed and reduced doses. Curr Med Res Opin 2012;28:1933–46. [DOI] [PubMed] [Google Scholar]
- 10.Munshi MN, Slyne C, Greenberg JM, et al. Nonadherence to Insulin Therapy Detected by Bluetooth-Enabled Pen Cap Is Associated With Poor Glycemic Control. Diabetes Care 2019;42:1129–31. [DOI] [PubMed] [Google Scholar]
- 11.Fazeli Farsani S, Brodovicz K, Soleymanlou N, Marquard J, Wissinger E, Maiese BA. Incidence and prevalence of diabetic ketoacidosis (DKA) among adults with type 1 diabetes mellitus (T1D): a systematic literature review. BMJ Open 2017;7:e016587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sherr JL, Hermann JM, Campbell F, et al. Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: comparison of results from three large, transatlantic paediatric registries. Diabetologia 2016;59:87–91. [DOI] [PubMed] [Google Scholar]
- 13.Matejko B, Cyganek K, Katra B, et al. Insulin pump therapy is equally effective and safe in elderly and young type 1 diabetes patients. Rev Diabet Stud 2011;8:254–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Briganti EM, Summers JC, Fitzgerald ZA, Lambers LNJ, Cohen ND. Continuous Subcutaneous Insulin Infusion Can Be Used Effectively and Safely in Older Patients with Type 1 Diabetes: Long-Term Follow-up. Diabetes Technol Ther 2018;20:783–6. [DOI] [PubMed] [Google Scholar]
- 15.Johnson SL, McEwen LN, Newton CA, et al. The impact of continuous subcutaneous insulin infusion and multiple daily injections of insulin on glucose variability in older adults with type 2 diabetes. J Diabetes Complications 2011;25:211–5. [DOI] [PubMed] [Google Scholar]
- 16.Argento NB, Liu J, Hughes AS, McAuliffe-Fogarty AH. Impact of Medicare Continuous Subcutaneous Insulin Infusion Policies in Patients With Type 1 Diabetes. J Diabetes Sci Technol 2019:1932296819838292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Munshi MN. Cognitive Dysfunction in Older Adults With Diabetes: What a Clinician Needs to Know. Diabetes Care 2017;40:461–7. [DOI] [PubMed] [Google Scholar]
- 18.Sinclair AJ, Girling AJ, Bayer AJ. Cognitive dysfunction in older subjects with diabetes mellitus: impact on diabetes self-management and use of care services. All Wales Research into Elderly (AWARE) Study. Diabetes Res Clin Pract 2000;50:203–12. [DOI] [PubMed] [Google Scholar]
- 19.Pfutzner J, Hellhammer J, Musholt P, et al. Evaluation of dexterity in insulin-treated patients with type 1 and type 2 diabetes mellitus. J Diabetes Sci Technol 2011;5:158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous Glucose Monitoring Versus Usual Care in Patients With Type 2 Diabetes Receiving Multiple Daily Insulin Injections: A Randomized Trial. Ann Intern Med 2017;167:365–74. [DOI] [PubMed] [Google Scholar]
- 21.Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C, Group DS. Continuous Glucose Monitoring in Older Adults With Type 1 and Type 2 Diabetes Using Multiple Daily Injections of Insulin: Results From the DIAMOND Trial. J Diabetes Sci Technol 2017;11:1138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Argento NB, Nakamura K. Personal real-time continuous glucose monitoring in patients 65 years and older. Endocr Pract 2014;20:1297–302. [DOI] [PubMed] [Google Scholar]
- 23.Wireless Innovations for Seniors with Diabetes Mellitus—Primary Results of the WISDM Study The 79th scientific sessions of the American Diabetes Association. San Fransisco, CA2019. [Google Scholar]
- 24.Polonsky WH, Peters AL, Hessler D. The Impact of Real-Time Continuous Glucose Monitoring in Patients 65 Years and Older. J Diabetes Sci Technol 2016;10:892–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Litchman ML, Allen NA. Real-Time Continuous Glucose Monitoring Facilitates Feelings of Safety in Older Adults With Type 1 Diabetes: A Qualitative Study. J Diabetes Sci Technol 2017;11:988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah VN, Wu M, Foster N, Dhaliwal R, Al Mukaddam M. Severe hypoglycemia is associated with high risk for falls in adults with type 1 diabetes. Arch Osteoporos 2018;13:66. [DOI] [PubMed] [Google Scholar]
- 27.Thorpe CT, Gellad WF, Good CB, et al. Tight glycemic control and use of hypoglycemic medications in older veterans with type 2 diabetes and comorbid dementia. Diabetes Care 2015;38:588–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lipska KJ, Ross JS, Miao Y, Shah ND, Lee SJ, Steinman MA. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med 2015;175:356–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin-Timon I, Del Canizo-Gomez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes 2015;6:912–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bremer JP, Jauch-Chara K, Hallschmid M, Schmid S, Schultes B. Hypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetes. Diabetes Care 2009;32:1513–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bainbridge KE, Cowie CC, Gonzalez F, 2nd, et al. Risk Factors for Hearing Impairment among Adults with Diabetes: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). J Clin Transl Endocrinol 2016;6:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maahs DM, DeSalvo D, Pyle L, et al. Effect of acetaminophen on CGM glucose in an outpatient setting. Diabetes Care 2015;38:e158–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bergenstal RM, Garg S, Weinzimer SA, et al. Safety of a Hybrid Closed-Loop Insulin Delivery System in Patients With Type 1 Diabetes. JAMA 2016;316:1407–8. [DOI] [PubMed] [Google Scholar]
- 34.Forlenza GP, Li Z, Buckingham BA, et al. Predictive Low-Glucose Suspend Reduces Hypoglycemia in Adults, Adolescents, and Children With Type 1 Diabetes in an At-Home Randomized Crossover Study: Results of the PROLOG Trial. Diabetes Care 2018;41:2155–61. [DOI] [PubMed] [Google Scholar]
- 35.Boughton CK, Bally L, Hartnell S, et al. Closed-loop insulin delivery in end-of-life care: a case report. Diabet Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]