Abstract
Objective
To estimate the prevalence and incidence of self-reported diabetes and to study its association with medium- and long-term mortality from all causes in persons ≥65 years.
Design
A population-based cohort study begun in 1993.
Setting
“Envejecer en Leganés” cohort (Madrid).
Participants
A random sample of persons ≥65 years (n = 1277 in the 1993 baseline sample).
Methods
Participants were classified as having diabetes if they so reported and had consulted a physician for this reason within the last year. Diabetes history was categorized in <10 and ≥10 years in 1993. Incidence density was calculated in 2-year periods in non-diabetic individuals (1965 persons/2 years). Vital status was recorded on 31 December 2011. The association between diabetes history ≥10 years and mortality at 6 and 18 years follow-up was studied by the Kaplan–Meier and Cox regression analyses after adjusting for age, sex, heart disease and comorbidity.
Results
The prevalence of self-reported diabetes rose from 10.3% in 1993 to 16.1% in 1999 (p ≤ 0.001) and was higher in women than men (p ≤ 0.05). Total incidence density was 2.6 cases/100 persons/2 years (95% CI: 2.0–3.3). Medium- and long-term mortality was higher in persons with diabetes history ≥10 years than in non-diabetic individuals (HR: 2.0; 95% CI: 1.2–3.3 and HR: 1.7; 95% CI: 1.1–2.5, respectively). In diabetics with history <10 years the HR was 1.3 (95% CI: 0.9–1.9) and HR: 1.5 (95% CI: 1.2–1.9, respectively).
Conclusions
Although diabetes is clearly associated with increased risk of mortality, it is significant only for patients with ≥10 years’ history of diabetes.
Keywords: Diabetes, Elderly, Prevalence, Incidence, Mortality, Cohort studies
Resumen
Objetivos
Calcular la prevalencia y la incidencia de diabetes autorreferida y analizar su asociación con la mortalidad general a medio y a largo plazo en personas ≥ 65 años.
Diseño
Estudio de cohortes de base poblacional iniciado en 1993.
Emplazamiento
Cohorte «Envejecer en Leganés» (Madrid).
Participantes
Muestra aleatoria de los ≥ 65 años (n = 1.277 en 1993).
Mediciones principales
Diabético: autorreferido y haber visitado al médico por este motivo el último año. Antigüedad de diabetes: más y menos de 10 años en 1993. Prevalencia en 1993, 1995, 1997 y 1999. Densidad de incidencia calculada para periodos bianuales (1.965 personas/2 años). Estado vital registrado a 31 de diciembre de 2011. La asociación entre diabetes y mortalidad a 6 y 18 años se estudió mediante Kaplan-Meier y regresión de Cox, ajustando por edad, sexo, enfermedades del corazón y comorbilidad.
Resultados
La prevalencia de diabetes autorreferida aumentó desde el 10,3% (1993) hasta el 16,1% (1999) (p ≤ 0,001), siendo superior en mujeres (p ≤ 0,05). La incidencia de diabetes fue de 2,66 casos por 100 personas/2 años (IC 95%: 1,9-3,3). La mortalidad a medio y a largo plazo fue mayor en diabéticos con ≥ 10 años que en no diabéticos (HR: 2,0; IC 95%: 1,2-3,3, y HR: 1,7; IC 95%: 1,1-2,5, respectivamente). En diabéticos < 10 años el HR para mortalidad fue 1,3 (IC 95%: 0,9-1,9) y 1,5 (IC 95%: 1,2-1,9), respectivamente.
Conclusiones
Aunque padecer diabetes se asocia a un aumento de la mortalidad, esta asociación es significativa solo para los pacientes con historia de diabetes igual o superior a 10 años.
Palabras clave: Diabetes, Mayores, Prevalencia, Incidencia, Mortalidad, Estudios de cohortes
Introduction
Over the past 20 years, there has been an explosive increase in the number of cases of diabetes mellitus in both developed and developing countries.1 The International Diabetes Federation (IDF) has recently estimated that in 2030, 9.9% of the adult population worldwide will have diabetes (552 million).2 Diabetes mellitus prevalence rates are rising. The prevalence of diagnosed diabetes among US adults aged 18 years and over increased from 5.1% in 1997 to 9.2% in 2010,3 and the number of individuals in the US with a new diagnosis of diabetes is expected to increase in the next decades, with the fastest increase occurring in older and minority subpopulations.4 In Europe, the prevalence of diabetes varies among studies.5 The reasons for this are multiple, and include the different methodologies used.6 The prevalence of diabetes in the adult population of Spain (aged 18 years and over) ranges from 6% to 12% based on self-reported data,7 and from 20% to 25% with measured data.8
Not only the prevalence of diabetes, but also its incidence is rising at an alarming rate. This increase is likely to have a significant public health impact given the high rates of acute myocardial infarction, heart failure, stroke, and death that follow diabetes,1 and implies a substantial burden on both the individual and the healthcare system.9 Yet little research has been conducted on diabetes in elderly populations. In addition, because diabetes is a silent disease, with no sudden or exact date of onset, it is difficult to design studies of disease incidence.10
Lastly, mortality is known to be higher in people with diabetes than in those without it,11 and diabetes accounts for considerable morbidity and mortality in the elderly population.9, 12 However, again, little information is available about how diabetes affects mortality when the diagnosis is made at an older age.13
The longitudinal study “Aging in Leganés”14 offers an opportunity to examine in greater depth the magnitude of diabetes and its association with all-cause mortality in a European Mediterranean population of people aged 65 years and over, an age group for which few data are available. Thus, the aims of this study are to estimate (1) the prevalence and incidence of diabetes and (2) the association between diabetes and medium- and long-term mortality in a population-based cohort of people aged 65 years or older in Spain.
Methods
Study subjects
This study used data from the population-based longitudinal study “Aging in Leganés” which began in 1993. The methodological characteristics of this study have been described elsewhere.14, 15 In brief, Leganés is a city located in a metropolitan area 8 km from Madrid (Spain). The census population in 1991 was 171,400 inhabitants, of whom 13,679 (8%) were over 64 years of age. “Aging in Leganés” was launched in 1993, starting with a gender- and age-stratified random sample obtained from the Leganés census of the population aged 65 years and over. In the baseline cohort 1283 persons completed the study.
Data were collected using a standardized questionnaire (a face-to-face home interview) that included sociodemographic variables, health status and history of chronic diseases.14, 15
The present study uses data from the 1993 baseline, as well as the 1995, 1997 and 1999 waves to know the prevalence and incidence of diabetes and the sociodemographic and clinical variables selected for this study. Mortality at 31/12/2011 was obtained from National Death Index.
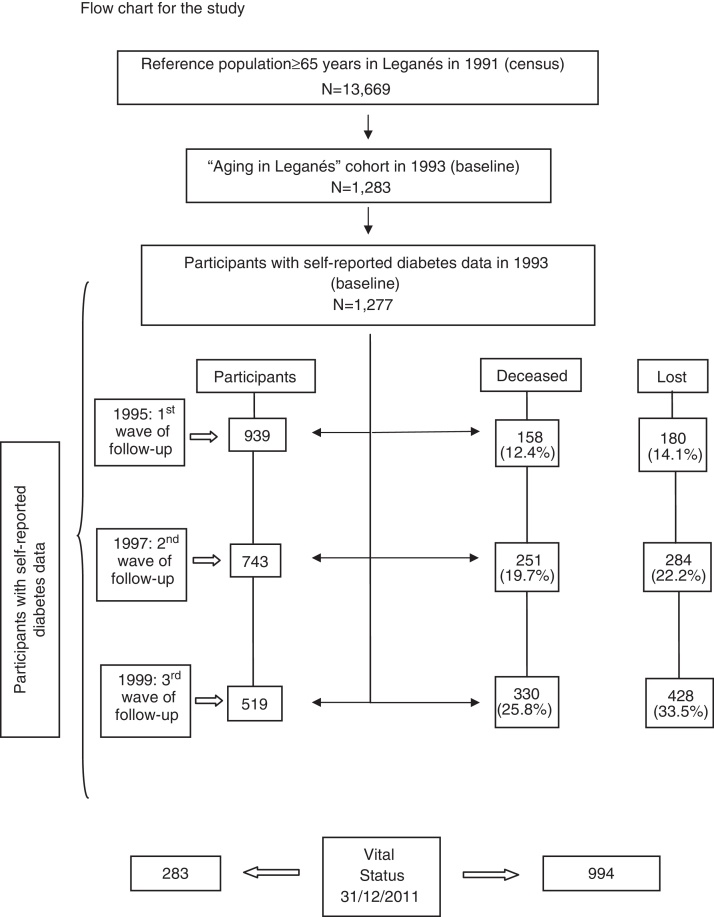
All individuals with available diabetes data were included in the analysis (1277 at baseline, 939 in 1995, 743 in 1997 and 519 in 1999) (see Flow chart for the study).
The local ethics committee approved the protocol for the Leganés study, and all participants signed an informed consent form.
Variables and procedures
History of diabetes was collected by self-reporting using two questions to the participants at baseline and in follow-up waves: “Do you have diabetes?” and “Did you have ever seen a physician in the last year for this problem?” People who answered “yes” to both the questions were considered to have diabetes and were asked to state the year when they became aware of their condition. Diabetes history was measured in years of diabetes at the time of incorporation of the individual in the baseline cohort (1993) and classified in three categories: no diabetes, less than 10 years of diabetes and 10 or more years of diabetes.
Mortality data were obtained from the National Death Index (NDI), a computerized database with information on the vital status of all residents in Spain. To compensate for the delay in updating mortality in the NDI, data were collected until June 2012. The cut-off date for the mortality analysis was 31/12/1999 (n = 330; 25.8%) for medium-term mortality (6 years) and 31/12/2011 (n = 994; 77.8%) for long-term mortality (18 years).
Age (years), sex, body mass index, heart disease, comorbidity, self-rated health and years of diabetes, obtained from the 1993 baseline Leganés questionnaire, were used as co-variables in the analysis.
Body Mass Index (BMI) in kg/m2 based on measures of weight and height.
Self-rated health (response to the question: “How would you describe your health at present?”: fair, poor or very poor versus good or very good).
Heart disease includes angina, myocardial infarction and/or heart failure.
Comorbidity was defined as having 4 or more chronic conditions of a list of 9 (heart disease, stroke, peripheral vascular disease (PVD), chronic respiratory disease (CRD), joint or bone pain, cancer, Parkinson's, genital or urinary pathology and gastrointestinal pathology). Chronic conditions were assessed by self-report of having been diagnosed by a medical doctor.
Statistical analysis
Due to the sampling design, prevalence and incidence figures are weighted using the age and sex distribution of the Leganés population in 1995. The data were weighted by assigning a specific weight (W) to each individual in the sample, calculated as W = N1/N:n1/n where N is the total population in Leganés, and n is the number of people in the cohort; N1 and n1 are the respective numbers in each age and sex group.
Fort the study of continuous variables, the goodness of fit to the normal distribution was analyzed using the Kolmogorov–Smirnov test; all cases fit the Gaussian curve, therefore the continuous variables were expressed as means ± standard deviation, and categorical variables as absolute and relative frequencies (n and %). A bivariate analysis was made for sex with distribution of variables in the baseline using χ2 test. The prevalence of diabetes was calculated by age group (65–74 and ≥75 years) and sex for each of the four waves (1993, 1995, 1997 and 1999). To study the change in the prevalence of diabetes over time, the χ2 tendency test was used.
For the calculation of incidence, all non-diabetic individuals in the previous waves were used: 978 persons in 1995, 783 in 1997, and 566 in 1999. The incidence density (incident cases/person-time periods) was calculated for biannual periods and expressed as the number of cases of diabetes per 100 persons by 2-year time periods. In total, 1965 persons/time periods were used.
Mortality analyses were conducted with the Kaplan–Meier analysis and adjusted by the Cox regressions. To evaluate the association between diabetes and general mortality, Cox regression was used at two moments: 31/12/1999 (6 years of follow-up) and 31/12/2011 (18 years of follow-up). Median survival was calculated, and the main results were summarized with hazard ratios (HRs) and their 95% CIs. Person follow-up time was calculated from the time people were incorporated into the study in 1993. Individuals were censored if they died or dropped out of the study.
Diabetes, as a principal variable, was used as a dummy variable (fictitious variable): (0) no diabetes, (1) less than 10 years of diabetes at baseline (1993), and (2) 10 or more years of diabetes at baseline (1993). Four multivariate Cox models were built: (1) crude diabetes data, (2) diabetes adjusted for age and sex, (3) additionally adjusted for heart disease and (4) additionally adjusted for comorbidity. Results with p less than 0.05 were considered statistically significant. SPSS version 19.0 and Epidat 3.1 were used for the analysis.
General outline of the study:
Results
Characteristics of the study subjects
Of the 1283 participating individuals in the baseline cohort (1993), diabetes self-reported data were available in 1277 individuals who participated in this wave, of which 50.4% were men and 49.6% were women. The flow chart for the study shows the number of participants in each of the waves, as well as the number of those who died or were lost to follow-up in each wave. The distribution of the variables studied in the baseline cohort is presented in Table 1. Women had a higher body mass index than men, as well as poorer self-rated health, a higher frequency and longer history of diabetes, and more comorbidity (p ≤ 0.001).
Table 1.
Distribution of variables in the baseline Leganés cohort (1993).
| Variables | Men (n = 644) | Women (n = 633) | Total (n = 1277) |
|---|---|---|---|
| Age [mean (SD)] | 75.6 (8.1) | 75.9 (8.1) | 75.8 (8.1) |
| Body mass index (BMI) [mean (SD)] | 26.3 (3.4) | 28.0 (4.8)*** | 27.1 (4.2) |
| Self-rated health fair, poor or very poor [n (%)] | 357 (55.4) | 432 (68.2)*** | 789 (61.8) |
| Diabetic patients [n (%)] | 47 (7.3) | 75 (11.8)** | 122 (9.6) |
| Patients with 10 or more years history of diabetes [n (%)] | 5 (0.8) | 28 (4.4)*** | 33 (2.6) |
| Heart disease [n (%)] | 163 (25.3) | 139 (22.0) | 302 (23.6) |
| Comorbidity (≥4 diseases) [n (%)] | 285 (44.3) | 388 (61.3)*** | 673 (52.7) |
p ≤ 0.05.
p ≤ 0.001.
Prevalence of diabetes
The prevalence of diabetes in the study population (weighted data) increased progressively over time, from 10.3% (95% CI: 8.6–11.9) in 1993 to 16.1% in 1999 (95% CI: 13.2–18.9), p ≤ 0.001. In the 1993 and 1995 waves, women had a significantly higher prevalence than men (p ≤ 0.05) (Table 2).
Table 2.
Age-specific prevalence of diagnosed diabetes by sex from 1993 to 1999.a
| 1993 (n = 1277) | 1995 (n = 939) | 1997 (n = 743) | 1999 (n = 519) | Tendency-p | |
|---|---|---|---|---|---|
| % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | ||
| Total | 10.3 [8.6–11.9] | 11.7 [9.7–13.6] | 14.5 [12.1–16.9] | 16.1 [13.2–18.9] | ≤0.001 |
| Men | 7.6 [5.4–9.8] | 9.2 [6.4–11.9] | 12.5 [9.1–15.9] | 15.6 [11.2–19.9] | ≤0.001 |
| Women | 12.3** [9.9–14.6] | 13.6** [10.8–16.4] | 16.1 [12.7–19.4] | 16.4 [12.5–20.3] | ≤0.005 |
| Age (years) | |||||
| 65–74 (total) | 10.1 [8.0–12.2] | 11.6 [9.0–14.2] | 14.0 [10.6–17.3] | 15.5 [10.9–20.0] | ≤0.005 |
| Men | 8.1 [5.3–10.9] | 9.6 [6.1–13.2] | 12.4 [7.7–17.1] | 15.8 [9.2–22.4] | ≤0.05 |
| Women | 11.8* [8.7–14.8] | 13.4 [9.5–17.2] | 15.5 [10.4–20.5] | 15.2 [8.7–21.6] | 0.148 |
| ≥75 (total) | 10.6 [7.9–13.2] | 12.2 [9.1–15.3] | 14.8 [11.5–18.2] | 16.7 [12.9–20.5] | ≤0.005 |
| Men | 6.5 [2.8–10.2] | 8.9 [4.5–13.4] | 12.7 [7.6–17.8] | 15.5 [9.5–21.5] | ≤0.002 |
| Women | 12.9 [9.2–16.7] | 14.2* [10.0–18.4] | 16.2 [11.7–20.8] | 17.5 [12.5–22.5] | 0.126 |
Weighted data.
p ≤ 0.05.
p ≤ 0.10.
The mean duration of diabetes in the 142 participants who had the disease at study baseline (1993) was 7.8 years (SD ± 6.8; range 0–30 years).
Incidence of diabetes
The total biannual incidence density of diabetes was 2.6 (95% CI: 1.9–3.3) cases per 100 persons at 2 years of follow-up, 2.8 (95% CI: 1.7–3.8) in men and 2.5 (95% CI: 1.6–3.4) in women. In general, the incidence density of diabetes decreased with increasing age, although this difference was not statistically significant. Differences between sexes were not statistically significant (Table 3).
Table 3.
Age-specific biannual incidence of diagnosed diabetes by sex (per 100 population) from 1993 to 1999.a
| Percentage | 95% confidence interval | |
|---|---|---|
| Total | 2.6 | 2.0–3.3 |
| Men | 2.8 | 1.7–3.8 |
| Women | 2.5 | 1.6–3.4 |
| Age (groups), years | ||
| 65–74 | 3.2 | 2.3–4.2 |
| Men | 3.3 | 1.9–4.8 |
| Women | 3.1 | 1.8–4.4 |
| ≥75 | 1.7 | 0.8–2.6 |
| Men | 1.7 | 0.2–3.2 |
| Women | 1.6 | 0.5–2.8 |
Weighted data.
Mortality associated with diabetes
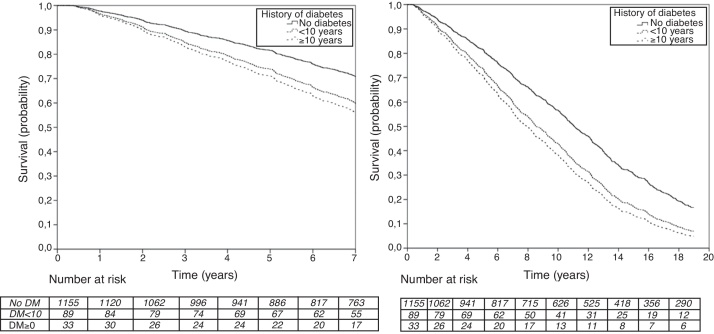
Our data show that survival time for older persons with 10 or more years history of diabetes is 2.7 years less than for non-diabetic individuals. The Kaplan–Meier medians in the medium-term models did not reach statistical significance. Median survival in the long term was 10.8 years (95% CI: 10.1–11.5) for non-diabetic persons; 9.0 (95% CI: 6.8–11.1) for persons with less than 10 years’ history of diabetes from baseline (1993); and 8.1 years (95% CI: 5.5–10.6) for those with 10 or more years’ history of diabetes from baseline (1993).
As can be seen in Table 4, the hazard ratio for medium- and long-term mortality in persons with 10 or more years’ history of diabetes was 2.0 (95% CI: 1.2–3.3) and 1.7 (95% CI: 1.1–2.5), respectively, after adjusting for age and sex, heart disease and comorbidity. Accordingly, it can be said that medium-term mortality is twice as high in persons with 10 or more years’ history of diabetes at baseline than in non-diabetic individuals, and is 70% higher in the long term.
Table 4.
Association of diabetes with all-cause mortality (Cox regression Hazard Model).a
| Medium-term mortality (1993–1999) |
Long-term mortality (1993–2011) |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Crude dataa | ||||||
| Less than 10 years of diabetes in 1993 | 1.2 | 0.8–1.6 | 0.394 | 1.4 | 1.1–1.7 | 0.007 |
| 10 or more years of diabetes in 1993 | 1.6 | 1.0–2.7 | 0.051 | 1.4 | 0.9–2.0 | 0.096 |
| Adjusted for age and sexa | ||||||
| Less than 10 years of diabetes in 1993 | 1.4 | 1.0–2.0 | 0.056 | 1.6 | 1.3–2.0 | <0.001 |
| 10 or more years of diabetes in 1993 | 2.1 | 1.3–3.5 | 0.003 | 1.8 | 1.2–2.6 | 0.003 |
| Additionally adjusted for heart diseasea | ||||||
| Less than 10 years of diabetes in 1993 | 1.3 | 0.9–1.9 | 0.095 | 1.6 | 1.2–2.0 | <0.001 |
| 10 or more years of diabetes in 1993 | 2.0 | 1.2–3.4 | 0.006 | 1.7 | 1.2–2.6 | 0.005 |
| Additionally adjusted for comorbiditya | ||||||
| Less than 10 years of diabetes in 1993 | 1.3 | 0.9–1.9 | 0.141 | 1.5 | 1.2–1.9 | 0.001 |
| 10 or more years of diabetes in 1993 | 2.0 | 1.2–3.3 | 0.009 | 1.7 | 1.1–2.5 | 0.009 |
The reference category in diabetes variable was NO DIABETES in baseline (1993).
The hazard ratio for medium- and long-term mortality in diabetic individuals with less than 10 years’ history of diabetes at baseline was 1.3 (95% CI: 0.9–1.9) and 1.5 (95% CI: 1.2–1.9), respectively. Thus, it can be said that in the medium term (6 years), those with less than 10 years’ history at baseline do not have higher mortality than non-diabetic persons, whereas their long-term mortality is almost 50% higher (Fig. 1).
Figure 1.
Medium- and long-term survival of diabetic patients and non-diabetic patients adjusted for age and sex, heart disease and comorbidity.
Discussion
Although increasing age is a risk factor for the development of diabetes and its vascular complications, few studies have focused specifically on the impact of diabetes in elderly populations.9, 12, 16 In our study, the prevalence of diabetes in individuals aged 65 years and over increased from 10.3% in 1993 to 16.1% in 1999. These data are consistent with other population studies: a Canadian study found that diabetes increased from 10.6% to 17.1% after 10 years of follow-up in a population over age 50,17 while a US study reported that the prevalence of diabetes increased from 12.5% to 17.7% in individuals aged 65 and over during 18 years of follow-up.18
In the DECODE study (Diabetes Epidemiology: Collaborative analysis of Diagnostic criteria in Europe),19 which measured plasma glucose in 13 European cohorts, in accordance with WHO recommendations for the diagnosis of diabetes, the prevalence of diabetes was 10–20% in individuals aged 60–79 years. In a recent study,20 conducted in subjects aged >60 years in Spain and with characteristics similar to ours, the overall prevalence of diabetes was 16.8%, slightly higher than ours (13.1%). This variation may be related to the methodology used to collect the information as well as the variability of results when they are self-reported by the patient. In a study in people older than 65 years in the United States using data from Medicare, the prevalence increased from 15.3% at baseline to 24.8% after 9 years of follow-up.12
In general, the prevalence of diabetes in the same age groups was much higher in 1999 than in the previous waves. Also in accordance with other studies17, 21 we found that most cases of diabetes occurred in the oldest individuals. One possible explanation for this could be a progressively greater awareness of diabetes on the part of both patients and medical professionals. Although most studies in the general population have found a higher prevalence of diabetes in men,6, 20, 22 some have found that the prevalence in people over age 65 is higher in women.23 The DECODE study has reported diabetes prevalence rates of 8.5% in men and 9.3% in women between the ages of 60 and 69 years, increasing to 12.4% in men and 15.4% in women between age 70 and 79 years, and to 12.9% in men and 22.4% in women between age 80 and 89.19 Our results are consistent with the aforementioned studies. The prevalence in 1993 was 7.6% in men and 12.3% in women, rising to 9.2% and 13.6% respectively, in 1995. The differences by sex found in 1997 and 1999 are not statistically significant.
Incidence of diabetes
Because diabetes has a silent course, without a sudden or exact date of onset, it is difficult to design studies of disease incidence.10
In Spain, the few studies that have estimated the incidence of diabetes are not consistent because they did not follow a standardized methodology.24 Moreover, most previous studies in Spain have provided diabetes incidence data in people under age 65 years, and therefore are not comparable with our data.10, 25 A recent study in Spain in persons aged 18–65 years25 found an annual diabetes incidence of 19.1 cases per 1000 person-years, slightly higher than that in our study. However, the annual incidence of diabetes in European studies conducted in the general population varies between 1.2 and 4.1 cases/1000 people,26, 27 which is lower than the figures published for the Spanish population.
Our results for diabetes incidence in persons aged 65 years and over show an incidence rate equivalent to 13.1 cases per 1000 person-years (2.6 cases per 100 persons-2 years of follow-up), which is between the 24 per 1000 person-years reported in a study made in US elderly12 and 9.4 cases per 1000 person-years for the population 65 years and over in Spain.28 In these two studies the incidence rates increased with increasing age. In our study the incidence is higher in the 65–74 years age group [3.2 (95% CI: 2.3–4.2)] than in those aged 75 years and over [1.7 (95% CI: 0.8–2.6)].
Mortality associated with diabetes
Diabetes has been associated with an average 10 years of life lost for individuals diagnosed during middle age.29 Individuals with diabetes have an excess mortality compared with people without diabetes.11 However, it is not clear how diabetes affects mortality when the diagnosis is made at an older age.13 Our data show that the survival time for people in the older population with 10 or more years history of diabetes is 2.7 years less than that for non-diabetic individuals.
Mortality in the medium term for persons with 10 or more years history of diabetes is almost double that of people without diabetes, while long-term mortality is almost 70% higher. Those with less than 10 years history of diabetes at baseline do not have higher mortality than non-diabetic individuals in the medium term, but long-term mortality is almost 50% higher. In a systematic review of observational studies11 reporting mortality in patients over age 60 diagnosed with type 2 diabetes, those with diabetes were found to have 40% higher mortality than non-diabetic persons, which is lower than found in our study.
Thus, our results show a clear association between diabetes and increased all-cause mortality, although this effect is statistically significant only in patients who have had diabetes for at least 10 years.
Strengths and limitations
The main strength of our study is the long follow-up time (18 years). Added to this is the fact that, to date, few studies of diabetes incidence and mortality have been made in Mediterranean populations.
One of the limitations of this study is that we used self-reported data to assess diabetes. Several authors point out that self-reported data could underestimate diabetes prevalence.10, 12, 20 Although this underestimation is possible, other authors have confirmed that self-reported diabetes is a reasonably reliable surrogate for diagnosed diabetes, based on their studies of the accuracy of patients’ self-reports compared with medical records.30, 31
In health care systems where general practitioners have a complete vision of their patients’ medical status and in which patients have easy and frequent access to medical services, patients are more likely to be well informed about their diseases, especially in the case of chronic diseases like diabetes. This is the case in Spain,32 where every community-dwelling person is registered in the patient list of a general practice, and access to other health care facilities, including outpatient clinics, is only possible through referral by a general practitioner.
Furthermore, in our study, individuals were classified as having diabetes not only based on their awareness of their condition, but also because they had seen a physician in the last year for this problem. The second question on medical consultations in the last year increases the validity of the self-report. In 1993 people in our sample averaged 8.3 consultations with general practitioners, similar to the current rate of general practitioner consultations in Spain.33
Our sample was drawn from a metropolitan area of Madrid, therefore this study may not be comparable to other non-Mediterranean population studies and cannot strictly be generalized to the whole older Spanish population.
Together with Sherwin R and Jastreboff AM,34 we can say that “today's message is that a diabetes tsunami is imminent, and the only way to minimize the damage is to create an early warning system and improve interventions to protect those in its path”. Effective public health interventions to prevent diabetes are needed, together with the resources required to manage the increasingly large number of people who are living longer with this debilitating disease.17 In accordance with Rose, we think that the “population strategy” with regard to prevention should always be the discovery and control of the causes of the incidence of chronic diseases.35 In the case of diabetes, important factors for prevention could be reducing obesity, increasing physical activity and maintaining a Mediterranean diet.
What is known about the topic
-
•
Diabetes mellitus is a chronic disease with major impact on health, and its prevalence and incidence are increasing.
-
•
Because diabetes is a silent disease, with no sudden or exact date of onset, it is difficult to design studies of disease incidence.
-
•
It is known that mortality is higher in diabetics than in non-diabetics, and diabetes in the elderly is responsible for a significant morbidity and mortality.
What brings the study
-
•
The article analyzes the prevalence of self-reported diabetes in Spain in a base population cohort of people over 65 years (Aging in Leganes cohort).
The prevalence of diabetes increased progressively over time, from 10.3% in 1993 to 16.1% in 1999. Women had a significantly higher prevalence than men.
-
•
The diabetes incidence in this population during the study period (1993–1999) was 13.1 cases per 1000 person-years (2.6 cases per 100 persons/2 years of follow-up). No differences were found between sexes neither between the age group 65–74 years and people over 75 years.
-
•
Although diabetes is clearly associated with increased risk of mortality, it is significant only for patients with ≥10 years history of diabetes. Mortality for persons with 10 or more years of history of diabetes is almost 70% higher than people without diabetes.
Funding sources
This work was supported by the Fondo de Investigaciones en Salud, FIS PI 05 1898, RETICEF RD06/0013/1013 and RD/12/0043/0019.
Conflict of interest
The authors declare no conflicts of interest.
Acknowledgements
We would like to thank the elderly people of Leganés for their generous participation in this study during many years as well as professors José Ramón Banegas and Juan José de la Cruz for their help in preparing the article.
References
- 1.Khan N.A., Wang H., Anand S., Jin Y., Campbell N.R., Pilote L. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care. 2011;34:96–101. doi: 10.2337/dc10-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.IDF Diabetes Atlas. Fifth edition; 2011. http://www.idf.org/diabetesatlas/news/fifth-edition-relese [accessed 20.08.12].
- 3.CDC/NCHS. Early release of selected estimates based on data from the 2010 National Health Interview Survey. Available from: http://www.cdc.gov/nchs/nhis/released201106.htm#6 [accessed November 2012].
- 4.Boyle J.P., Thompson T.J., Gregg E.W., Barker L.E., Williamson D.F. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaw J.E., Sicree R.A., Zimmet P.Z. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Soriguer F., Goday A., Bosch-Comas A., Bordiú E., Calle-Pascual A., Carmena R. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia. 2012;55:88–93. doi: 10.1007/s00125-011-2336-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministerio de Sanidad y Consumo. Estrategia en diabetes del Sistema Nacional de Salud. Madrid; June 2007. Available from: http://www.msssi.gob.es/organizacion/sns/planCalidadSNS/pdf/excelencia/cuidadospaliativos-diabetes/DIABETES/Estrategia_en_diabetes_del_SNS_Accesible.pdf [accessed July 2013].
- 8.Castell C., Tresserras R., Serra J., Goday A., Lloveras G., Salleras L. Prevalence of diabetes in Catalonia (Spain): an oral glucose tolerance test-based population study. Diabetes Res Clin Pract. 1999;43:33–40. doi: 10.1016/s0168-8227(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 9.Bethel M.A., Sloan F.A., Belsky D., Feinglos M.N. Longitudinal incidence and prevalence of adverse outcomes of diabetes mellitus in elderly patients. Arch Intern Med. 2007;167:921–927. doi: 10.1001/archinte.167.9.921. [DOI] [PubMed] [Google Scholar]
- 10.Goday A. Epidemiology of diabetes and its non-coronary complications. Rev Esp Cardiol. 2002;55:657–670. doi: 10.1016/s0300-8932(02)76674-8. [DOI] [PubMed] [Google Scholar]
- 11.Jansson S.P., Andersson D.K., Svärdsudd K. Mortality trends in subjects with and without diabetes during 33 years of follow-up. Diabetes Care. 2010;33:551–556. doi: 10.2337/dc09-0680. [Epub December 15, 2009] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sloan F.A., Bethel M.A., Ruiz D., Jr., Shea A.M., Feinglos M.N. The growing burden of diabetes mellitus in the US elderly population. Arch Intern Med. 2008;168:192–199. doi: 10.1001/archinternmed.2007.35. [discussion 199] [DOI] [PubMed] [Google Scholar]
- 13.Barnett K.N., McMurdo M.E., Ogston S.A., Morris A.D., Evans J.M. Mortality in people diagnosed with type 2 diabetes at an older age: a systematic review. Age Ageing. 2006;35:463–468. doi: 10.1093/ageing/afl019. [DOI] [PubMed] [Google Scholar]
- 14.Zunzunegui M.V., Béland F., Gutiérrez-Cuadra P. Loss to follow-up in a longitudinal study on aging in Spain. J Clin Epidemiol. 2001;54:501–510. doi: 10.1016/s0895-4356(00)00325-5. [DOI] [PubMed] [Google Scholar]
- 15.Zunzunegui M.V., Del Ser T., Rodríguez Laso A., García de Yebenes M.J., Domingo J., Otero A. Detección de la demencia y utilización de servicios sanitarios: implicaciones para la Atención primaria. Aten Primaria. 2003;31:581–586. doi: 10.1016/S0212-6567(03)79220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gregg E.W., Cheng Y.J., Saydah S., Cowie C., Garfield S., Geiss L. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care. 2012;35:1252–1257. doi: 10.2337/dc11-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipscombe L.L., Hux J.E. Trends in diabetes prevalence, incidence, and mortality in Ontario Canada 1995–2005: a population-based study. Lancet. 2007;369:750–756. doi: 10.1016/S0140-6736(07)60361-4. [DOI] [PubMed] [Google Scholar]
- 18.Cowie C.C., Rust K.F., Byrd-Holt D.D., Gregg E.W., Ford E.S., Geiss L.S. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care. 2010;33:562–568. doi: 10.2337/dc09-1524. [Epub January 12, 2010] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DECODE study group Age and sex specific prevalences of diabetes and impaired glucose regulation in 13 European cohorts. Diabetes Care. 2003;26:61–69. doi: 10.2337/diacare.26.1.61. [DOI] [PubMed] [Google Scholar]
- 20.Rosado Martín J., Martínez López MÁ, Mantilla Morató T., Dujovne Kohan I., Palau Cuevas F.J., Torres Jiménez R. MAPA. Prevalence of diabetes in an adult population in the region of Madrid (Spain). The Madrid Cardiovascular Risk study. Gac Sanit. 2012;26:243–250. doi: 10.1016/j.gaceta.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Gregg E.W., Cadwell B.L., Cheng Y.J., Cowie C.C., Williams D.E., Geiss L. Trends in the prevalence and ratio of diagnosed to undiagnosed diabetes according to obesity levels in the US. Diabetes Care. 2004;27:2806–2812. doi: 10.2337/diacare.27.12.2806. [DOI] [PubMed] [Google Scholar]
- 22.Gardete-Correia L., Boavida J.M., Raposo J.F., Mesquita A.C., Fona C., Carvalho R. First diabetes prevalence study in Portugal: PREVADIAB study. Diabet Med. 2010;27:879–881. doi: 10.1111/j.1464-5491.2010.03017.x. [DOI] [PubMed] [Google Scholar]
- 23.Durán Alonso J.C., investigadores del estudio Diagerca Prevalence of diabetes mellitus in geriatric patients in nursing homes of Cádiz. Diagerca study. Rev Esp Geriatr Gerontol. 2012;47:114–118. doi: 10.1016/j.regg.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Ruiz-Ramos M., Escolar-Pujolar A., Mayoral-Sánchez E., Corral-San Laureano F., Fernández-Fernández I. Diabetes mellitus in Spain: death rates, prevalence, impact, costs and inequalities. Gac Sanit. 2006;20(Suppl 1):15–24. doi: 10.1157/13086022. [DOI] [PubMed] [Google Scholar]
- 25.Soriguer F., Rojo-Martínez G., Almaraz M.C., Esteva I., Ruiz de Adana M.S., Morcillo S. Incidence of type 2 diabetes in southern Spain (Pizarra Study) Eur J Clin Invest. 2008;38:126–133. doi: 10.1111/j.1365-2362.2007.01910.x. [DOI] [PubMed] [Google Scholar]
- 26.Vilbergsson S., Sigurdsson G., Sigvaldason H., Hreidarsson A.B., Sigfusson N. Prevalence and incidence of NIDDM in Iceland: evidence for stable incidence among males and females 1967–1991. The Reykjavik Study. Diabetic Med. 1997;14:491–498. doi: 10.1002/(SICI)1096-9136(199706)14:6<491::AID-DIA365>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 27.Njolstad I., Arnesen E., Lund-Larsen P.G. Sex differences in risk factors for clinical diabetes mellitus in a general population: a 12-year follow-up of the Finnmark Study. Am J Epidemiol. 1998;147:49–58. doi: 10.1093/oxfordjournals.aje.a009366. [DOI] [PubMed] [Google Scholar]
- 28.Martín Martínez M.A., Carmona Alférez R., Prado Galbarro F.J., Sarría Santamera A. Incidence and prevalence of diabetes in an adult population of Madrid (Spain): a study using computerized medical records in primary care. Gac Sanit. 2013;27:284–285. doi: 10.1016/j.gaceta.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Narayan K.M., Boyle J.P., Thompson T.J., Sorensen S.W., Williamson D.F. Lifetime risk for diabetes mellitus in the United States. J Am Med Assoc. 2003;290:1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 30.Kriegsman D.M., Penninx B.W., van Eijk J.T., Boeke A.J., Deeg D.J. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49:1407–1417. doi: 10.1016/s0895-4356(96)00274-0. [DOI] [PubMed] [Google Scholar]
- 31.García del Campo M.M., Zunzunegui M.V., Béland F. La consulta por terceros en la atención primaria de las personas mayores. Aten Primaria. 1995;10:607–614. [PubMed] [Google Scholar]
- 32.García-Armesto S., Begoña Abadía-Taira M., Durán A., Hernández-Quevedo C., Bernal-Delgado E. vol. 12. 2010. Spain: health system review; pp. 1–295. (Health systems in transition). xix–xx. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21224176. [PubMed] [Google Scholar]
- 33.Actividad asistencial en Atención Primaria. Frecuentación general. Sistema Nacional de Salud. Año 2007-2011. Available from: http://www.msc.es/estadEstudios/estadisticas/estadisticas/estMinisterio/docs/Actividad_asist.pdf [accessed May 2013].
- 34.Sherwin R., Jastreboff A.M. Year in diabetes 2012: the diabetes Tsunami. J Clin Endocrinol Metab. 2012 doi: 10.1210/jc.2012-3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30:427–432. doi: 10.1093/ije/30.3.427. [discussion 433–4] [DOI] [PubMed] [Google Scholar]