Abstract
Objective:
Social media is a potentially engaging way to support adolescents and young adults in maintaining healthy diets and learning about nutrition. This review identifies interventions that use social media to promote nutrition, examines their content and features, and evaluates the evidence for the use of such platforms among these groups.
Material and methods:
We conducted a systematic search of 5 databases (PubMed, CINAHL, EMBASE, PsycINFO, and ACM Digital Library) for studies that included: 1) adolescents and/or young adults (ages 10–19; ages 18–25); 2) a nutrition education or behavior change intervention component, or outcomes related to nutrition knowledge or dietary changes; and 3) a social media component that allowed users to communicate or share information with peers.
Results:
16 articles were identified that included a social media component in a nutrition-related intervention for adolescents or young adults. Interventions included features in 7 categories: social media; communication; tracking health; education; tailoring; social support; and gamification. 11 out of the 16 studies had at least one significant nutrition-related clinical or behavioral outcome.
Conclusion:
Social media is a promising feature for nutrition interventions for adolescents and young adults. A limited number of studies were identified that included social media. A majority of the identified studies had positive outcomes. We found that most studies utilized only basic social media features, did not evaluate the efficacy of social media components, and did not differentiate between the efficacy of social media compared to other delivery mechanisms.
Keywords: Adolescent, Young adult, Nutrition Diet, Social media
1. Introduction
Maintaining healthy diets is a challenge for adolescents (ages 10–19) and young adults (ages 18–25) [1]. National health surveys classify over 80 percent of adolescents as not meeting recommendations for a healthy diet [2]. Dietary behaviors also tend to worsen during early adulthood, when young individuals transition into independent living [3]. Over time, this can lead to greater risks for cardiovascular disease, diabetes, and other chronic diseases [4]. This developmental stage, while historically overlooked in traditional nutrition interventions and considered a relatively healthy period of individuals’ lives, is receiving increasing attention as epidemiological evidence emerges showing poor outcomes for weight gain, physical activity, and dietary intake [5,6]. Interventions targeting adolescents and young adults, often conducted in high school and university settings, have seen moderate success with behavior-focused instruction, assessments with feedback, and the involvement of peers [7].
In recent years, nutrition education interventions have increasingly relied on computing and information technologies, particularly mobile platforms and social media [8,9]. Adolescents and young adults are particularly amenable to such solutions, as they exhibit high levels of smartphone and social media usage and, thus, are likely to be receptive to using these platforms for health [10-12]. Most already rely on smartphones to search for health information [13]. Novel computing and mobile-based platforms for health and nutrition leverage the popularity of mobile technologies among youth to deliver nutrition-related educational content, to facilitate counseling and communication with clinicians, and to encourage behavior logging and self-assessments [14]. Thus far, many of these efforts have focused on translating previous expert-developed programmatic content and interactions with professionals into experiences using technology.
An increasing number of technological interventions for nutrition leverage peer influence in social networks. Friends and social groups play influential roles during adolescence and young adulthood [15-17]. Particularly with dietary behaviors, research has found that eating habits of peers influence young adults’ consumption of snacks and fast foods [18-20]. Unhealthy habits can be modeled after friends’ behaviors and, long-term, peers can exert more influence than family on risks of obesity [21,22]. Previous nutrition interventions have leveraged social relationships to encourage healthy behaviors; however, most relied on in-person, peer group sessions and activities for providing support [23,24]. At the same time, social media—websites and applications that enable content creation, sharing, and participation in networking [25] -have been demonstrated to be an effective strategy for facilitating peer relationships in these target age groups [26].
To reflect a growing number of nutritional interventions with technological components, recent systematic literature reviews have included such interventions for adolescents and young adults. However, these previous reviews focused on broader age groups [27-34] and health conditions [9,30-32,34-37], or on specific behaviors and clinical outcomes such as vegetable intake or weight loss [38,39]. Others focused on theoretical foundations used to inform programmatic elements of the interventions [40,41]. In terms of technology, reviews have examined delivery methods such as computer, web, and mobile devices [42-45]. None, however, specifically examined the effect of nutrition and diet interventions for adolescents and young adults that incorporated social media. Thus far, only two reviews focused more generally on health and social media among adolescents and young adults. As a result, the effect of social media interventions on health outcomes remains unclear, with one review showing no significant outcomes and another describing the purpose of social media components in interventions (e.g. for recruitment; communication; etc.) but not examining outcomes [9,37].
The purpose of this review is to fill these gaps and to review the emerging evidence regarding the efficacy of interventions that utilize social media for improving nutrition among adolescents and young adults. Our specific goals are: 1) to identify technological features included in these interventions, 2) to evaluate evidence from randomized and non-randomized studies for using social media in nutrition interventions for these age groups, and 3) to identify areas that require further research.
2. Materials and methods
Our methods followed the PRISMA systematic review guidelines [45,46]. We searched five electronic databases: PubMed, CINAHL, EMBASE, PsycINFO, and ACM Digital Library between July and September 2016. Keywords included 1) age group (e.g.” adolescent” and “young adult”), 2) nutrition (e.g. “diet”, “food”, etc,) and 3) social media and technology (e.g. “social media”, “Facebook”, “Instagram”, “Internet”, “mobile applications”, “computer”, etc). Full search terms can be found in Supplementary Appendix A. In some cases, searches were further limited to having a social component (“social” or “peer (s)”) in the full-text. Papers retrieved were limited to those published in English from 2006 to 2016. Given the rapidly changing nature of social media technologies, this time period includes the most recent and still relevant interventions; it also captures the earliest references to “social media” in the literature. References from relevant articles were manually searched for citations, which were added for review.
We used the following inclusion criteria to select articles eligible for review: 1) targeted adolescents (10–19) and/or young adults (18–25) who are healthy, or have a health challenge, such as being overweight, obese, or have a chronic disease; 2) included a nutrition education or behavior change component, or outcomes related to improving nutritional knowledge or dietary changes (e.g. increase fruits/vegetable intake; reduce fast food/sugar-sweetened beverages intake); and 3) included a social media website, application, or homegrown technology that allows users to communicate or share information with peers. Exclusion criteria included interventions targeting eating disorders, families, or parents; or were not peer reviewed (e.g. dissertation/ thesis). We excluded studies without an evaluation component due to our interest in the impact of interventions on clinical or behavioral outcomes.
Two reviewers (MC and MB) conducted all article screenings with conflicts discussed and, if needed, adjudicated by a third reviewer (LM). An initial review was completed to screen database results based on title and abstract. Articles that did not fit inclusion criteria and duplicates were excluded. A full text review of articles was completed and reasons for exclusion were documented. Once final articles were determined, additional manuscripts from the research studies were added. The first author (MC) extracted study design characteristics, intervention features, measured outcomes, and significant outcomes from the final articles. Final articles were assessed for bias using the Downs Black Checklist for Measuring Quality in Health Care Intervention Studies [47] by two reviewers (MC and MB). The checklist is adaptable for study designs from experimental to non-experimental.
3. Results
3.1. Search results
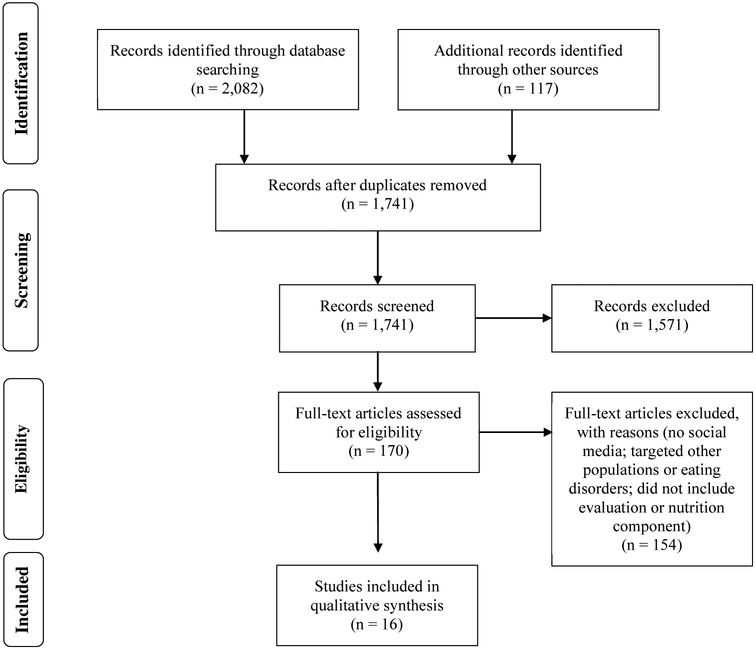
The initial database searches produced 2082 articles: 1234 from PubMed; 42 from CINAHL, 532 from EMBASE, 201 from PsycINFO; and 73 from ACM (Fig. 1). An additional 117 were included from other sources such as article references and known articles not captured with searches. After 458 duplicates were removed, 1741 articles were screened for titles and abstracts and 1571 were excluded. Articles were excluded for the following reasons: not including social media, including irrelevant age groups, targeting eating disorders, not including an evaluation component, and not including a nutrition component or outcomes. We excluded systematic reviews but searched the references. During full text screening, 170 articles were assessed for eligibility; of these 154 were excluded for reasons listed above. Our final qualitative analysis includes 16 studies.
Fig. 1.
PRISMA flow diagram of search strategy
3.2. Quality appraisal
Although the majority of studies were randomized control trials, study quality varied. Eleven studies met at least 60 percent of the Downs Black criteria indicating good quality [24,48-57]. Four studies were of fair quality meeting 50 percent of the checklist [58-61]. The remaining study did not sufficiently report key study characteristics to assess quality [62]. Full quality appraisal results are presented in Supplementary Appendix B.
3.3. Theoretical frameworks used to design interventions
Nearly all studies utilized theoretical frameworks to inform the design of application features and intervention content. This included individual behavior models like the transtheoretical model [48,56,63], theory of reasoned action [49], self-determination theory [24,49], transcontextual model of motivation [24], and theory of planned behavior [49,51]. One used the Attitude-Social Influence-Self-efficacy model based on the theory of planned behavior specific to fruit and vegetable consumption [63]. Seven studies used interpersonal beha-viors models such as control [48], social cognitive [24,49,55-57,64], and social network theories [64]. One accounted for broader influences using ecological models of health behavior [64]. Three studies described using general cognitive behavioral strategies [50,52,58] or behavioral change techniques [51] to design interventions. Technology use theories, such as the theory of interactive technology, were also used [57]. Three studies did not report using theoretical frameworks. One used a formative study with focus groups to solicit design ideas from participants [62]. The others did not describe the design process [60,61],
3.4. Intervention features
The analysis identified broad families of features included in the reviewed interventions: social media; communication mechanisms; health tracking; tailoring; education; social support; and gamification (Table 1).
Table 1.
Intervention features.
| Study (Last name, publication year) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Features | Allman-Farinelli 2016 | An 2013 | Chung 2016 | Doyle 2008 | Godino 2016 | Hutchesson 2016 | Jones 2014 | Kulik 2015 | Lana 2014 | Laska 2016 | Leme 2016 | Napolitano 2014 |
Nawi 2015 | Smith 2014 | Svetkey 2015 | Whittemore 2013 | Total of each feature |
| Significant nutrition outcomes |
✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||
| Social media | |||||||||||||||||
| Method of delivery | |||||||||||||||||
| ● | ● | ● | 3 | ||||||||||||||
| ● | 1 | ||||||||||||||||
| ● | 1 | ||||||||||||||||
| ● | 1 | ||||||||||||||||
| Homegrown mobile app | ● | ● | ● | ● | 4 | ||||||||||||
| Homegrown website | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | 11 | |||||
| Function | |||||||||||||||||
| Information dissemination & modules | ● | ● | ● | ● | ● | ● | ● | ● | 8 | ||||||||
| Online discussions forums & blogs | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | 10 | ||||||
| Post questions | ● | ● | 2 | ||||||||||||||
| Messaging | ● | ● | ● | ● | ● | ● | 6 | ||||||||||
| User profiles/avatars | ● | ● | ● | ● | 4 | ||||||||||||
| Peer assessments/support | ● | ● | ● | ● | ● | 5 | |||||||||||
| Nutrition and health resources | ● | ● | ● | 3 | |||||||||||||
| Prompts to track | ● | ● | 2 | ||||||||||||||
| Log/post goals and behaviors | ● | ● | ● | ● | ● | ● | 6 | ||||||||||
| Communication | |||||||||||||||||
| Generic messaging | ● | ● | ● | ● | 4 | ||||||||||||
| Messaging with clinicians/research staff | ○ | ● | ● | ● | ● | 5 | |||||||||||
| Tracking health | |||||||||||||||||
| Food diary | ● | ● | ● | ● | ● | ● | ● | ● | ● | ∎ | ● | ● | 12 | ||||
| Physical activity diary | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | ○ | 12 | ||||
| Other behavior tracking | ○ | ○ | ○ | ○ | 4 | ||||||||||||
| Goal setting | ● | ● | ● | ●○ | ● | ○ | ○ | ● | ● | 9 | |||||||
| Feedback/coaching | ∎ | ● | ● | ● | ● | ●○ | ● | ●○ | ● | ● | 10 | ||||||
| Prompts to track | ● | ● | ● | 3 | |||||||||||||
| Tailoring | |||||||||||||||||
| Messages | ● | ●○ | ● | ● | 4 | ||||||||||||
| Feedback or recommendations | ∎ | ● | ● | ∎ | ● | ● | ● | ● | ● | 9 | |||||||
| Goal setting | ● | ● | ● | 3 | |||||||||||||
| Education | |||||||||||||||||
| Method of delivery | |||||||||||||||||
| Workshops/classes | ■□ | ■□ | ■□ | □ | 4 | ||||||||||||
| Automated messages | ● | ●□ | ● | ● | ● | ●■ | ● | ● | 8 | ||||||||
| Static online information or links | ● | ● | ●□ | ● | ● | ● | ●○ | ● | 8 | ||||||||
| Emails / Newsletters | ● | ● | ●□ | ● | ■□ | 5 | |||||||||||
| Modules or videos or podcasts | ● | ●■ | ●□ | ● | ● | ● | ● | ● | 8 | ||||||||
| Content | |||||||||||||||||
| Recipes/meal planning/health tips | ●■ | ● | ● | ● | ■□ | ●■ | ● | 7 | |||||||||
| Peer support skills | ■□ | ● | □ | 3 | |||||||||||||
| Individual stress/coping skills | ■□ | ●■ | ● | ● | 4 | ||||||||||||
| Other lifestyle modification | ●■ | ■□ | ● | 3 | |||||||||||||
| Social support (not from social media) | |||||||||||||||||
| Family engagement | ■ | ■□ | ■□ | ■ | □ | 5 | |||||||||||
| Peers | ● | ● | ● | ● | □ | ● | 6 | ||||||||||
| Motivational messages | ● | ● | ● | 3 | |||||||||||||
| Gamification | |||||||||||||||||
| Behavioral challenges | ■ | ● | ○ | 3 | |||||||||||||
| Knowledge challenges (quizzes) | ● | ● | ● | ● | 4 | ||||||||||||
| Rewards | ● | ● | ● | 3 | |||||||||||||
| Total types of features per study | 12 | 16 | 14 | 10 | 15 | 12 | 9 | 10 | 8 | 22 | 11 | 15 | 2 | 13 | 17 | 9 | |
KEY● = tech-mediated, nutrition; ○=tech-mediated, not nutrition. ■ = in-person, nutrition; □=in-person, not nutrition.
3.4.1. Social media
Social media features were categorized based on the function, purpose or activity for which it was used and by specific platforms. The three main functions of social media in the interventions were 1) to facilitate communications and relationships among peers; 2) to support self-tracking and gamification; and 3) to share content among research staff and participants. We expand on these below.
One of the more common uses of social media was to facilitate communication, relationship building, and social support among peers. Blogs were used to disseminate information and allow commentary by community members [48,49]. More extensive interactions including support seeking, relationship building, problem solving, and behavior sharing were supported through online discussion forums [50,58,59,63,64]. Smaller group interactions were offered through private groups, messaging, and chats using Facebook, WhatsApp, Twitter and homegrown apps [52,60,65]. In some cases, interactions were open-ended to allow participants to organically discuss topics of interest [48,50,58,64]which in one case was monitored by a professional [58]. However, three interventions supplied topics [62] and structured activities with assigned partners [52,56] for discussion.
Social media was also used to support sharing of tracking activities and gamification. Public and selective sharing of goal setting, diet logging, and physical activities were included in five interventions [50,58,59,63,64] Two included assessments [24] or coaching [49] from peers. Diet and exercise related games and challenges were included [24,51,56] with one application enabling public results posting [24]. Homegrown applications or existing social media platforms such as Twitter [62] and Fitbit [62] were used for these activities.
Lastly, social media was used to share content among study staff and participants. This included educational information, messages [65], reminders [62], polls [60], and health-related event information [60]. Three studies supported multimedia content sharing including podcasts [60], photograph diary testimonials from peers [49], health-related images selected by study staff from Pinterest sent through Twitter [62], and video messages from peer coaches [49].
3.4.2. Other communication mechanisms
Communications outside of social media between study participants and research staff, professionals, and off-line with peers was another prominent feature. Technology-mediated private messaging [62,65], emails [48], and requests for online advice [63] with dietitians and research staff were available in three studies. Other studies relied on traditional communication methods such as phone calls [49,64] including coaching calls with dietitians [48].
3.4.3. Features for tracking health behaviors
Outside of social media, websites and apps were used to track health activities with goal setting, monitoring, and feedback for personal use and for review by experts. Monitored activities included diet, physical activity, screen time, and triggers of body dissatisfaction [50]. Private online journaling, self-monitoring, and reporting of behaviors was featured in nine studies [24,48-51,56,58,59,62]. In most cases, these required manual logging, particularly for diet. However one study autotweeted physical activities via FitBit [62]. Real-time location-based prompts were included in one study to encourage tracking [51]. Other interventions used paper diaries [65,66] and food recall surveys [63] submitted to study staff to assess diets. Goal review and feedback were provided in the form of phone calls [48], messaging [49], reports [60] from avatars [49], automated feedback [59], and research and clinical personnel [48,50,51,58,60,66]. One study offered online tracking bars for self review [49].
3.4.4. Tailoring
Ten studies utilized tailored or personalized content to provide specific, relevant information for study participants to change behaviors [24,48-51,56,58,60,62,64]. Interventions were customized for demographic characteristics like gender [48,50] or based on stages of change [48]. One application allowed users to set their own goals [51]. Tailored content most commonly included types of messages received [49], feedback [50,51,56,58,62], and educational materials [50]. In one case, personalized feedback reports with text and visuals were generated for participants [60].
3.4.5. Education
The most common educational component was diet and nutrition information for users. This included nutrition of foods [48], recommended daily servings and sizes [48,50,52,62], infographics and photos of healthy foods [62] and recipes [64]. Building skills associated with healthy eating such as meal planning [48,60], goal setting [52,60], monitoring diet [52,60], and contextualizing target behaviors [48] was included. Several included features for teaching how to understand situations that lead to unhealthy behaviors such as nutritional triggers [60], stress [60], and special occasions [60]. One extended this to teach cognitive approaches (problem solving, cognitive restructuring) to manage such issues [52]. Along with nutrition, interventions integrated educational content on physical activity such as daily recommendations and explanations of energy balance [24,48,50,52,58,62].
Most educational content was delivered using technology. App and website libraries of articles, links, videos were available to view [48,63,64]. One study used Facebook to house content [60]. In other cases, content was sent to users through text messages [55,58], messages from avatars [49], email [58], and Twitter [62]. Other interventions relied on non-technical modes of delivery such as in-person workshops [55], classes [55] and sessions [24,52] led by professionals or through printed materials [48,55].
3.4.6. Social support
Interventions included features to facilitate social support outside of the use of social media with peers. Parents were given information on children’s progress and how to support healthier lifestyles through periodic newsletters and meetings [24,50,55,59,66]. Peer support was leveraged through in-person and technology-mediated methods. These included mentoring [24], teaching support skills [66] and peer coaching with review tracking [49], and personalized video feedback, motivational messaging [55,56], and phone calls [49]. In some cases, participants were asked to seek support within existing social networks by sharing goals and results [51] or having non-study buddies [60].
3.4.7. Gamiflcation
Gamification, the use of game design elements in non-gaming contexts to engage participants [67], was used to encourage learning health information and practicing health behaviors. Quizzes were used to assess nutrition knowledge [59,63,64]. Behavioral dietary challenges were used to increase engagement and add competition to healthy eating [51]. Personal and group challenges promoted increases in physical activity [62]. Reward systems were popular for incentivizing intervention activities such as completing quizzes [58], viewing and reading content [63], playing games [63], and providing comments and feedback to other users [64]. In only one case, points were able to be redeemed for tangible prizes and gift cards [64].
3.5. Study characteristics
3.5.1. Target population
Participants included adolescents and young adults with individual studies focused on one of these subgroups (Table 2). Four studies targeted one gender—three for females and one for males [24,58,65,66]. Eight studies recruited students from secondary schools, colleges, and universities [24,54,57,59-62,65]. Minorities represented 27 to over 70% of the study populations in twelve studies [48-52,54,56,57,59,60,62,68]. Income levels were reported in six studies [24,48,54,57,58,65]; two studies [24,65] explicitly served lowincome populations and the remainder served broader income levels [48,54,57,58]. Typical inclusion criteria included: normal to obese body mass index (BMI); general good health; suboptimal diet or physical activity behaviors; and access to the internet and computer or mobile phone. Typical exclusion criteria were being pregnant; taking specific medications; in a weight loss program; and having medical conditions precluding them from intervention activities. One study included nutrition outcomes focused on participants who were quitting smoking [49].
Table 2.
Study characteristics(N=16).
| Author, year (Country) |
Interventi on name |
Target population | Study design | Sample size | Duration | Theoretical models |
Outcomes measured |
Significant nutrition related results |
Significant results | Social media feature |
Feasibility (selected findings) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Allman-Farinelli, 2016 (Australia) | TXT2BFit | Young adults aged 18-35 at risk overweight w BMI 23-24.9 with >2 kg weight gain in past 12 months, or BMI of 25-31.9. Also failing to meet key health behavior | Two-arm parallel randomized controlled trial (RCT) | n=250 | 12 weeks intervention; 9 month follow-up | Process of change; Control theory; Transtheoretical model | Primary: Measured and self-reported weight gain Secondary: daily fruit/vegetable intake; weekly sugar sweetened beverage (SSB) intake; weekly take-out meals; frequency and minutes of physical exercise | ✓ | Intervention group: weighed less at 9 months; had greater likelihoods of meeting fruit/veg/take-out food/SSB intake. | Smartphone app for self-monitoring; Community blog to talk with researchers and participants | 100% used coaching calls; 82.4% completed all. 90.9% reported using the text messages. Declines over time. Only 6.4% used the community blog. 74.5% did not access the mobile phone app. |
| An, 2013 (United States) | RealU2 | Young adults aged 18-30 who reported smoking at least once in the last 30 days | Three group RCT: general interest messages; tailored health messages; tailored health messages + online video peer support | n=1698 | 6 week intervention; 12 week follow-up | Theory of reasoned action and planned behavior, social cognitive theory, and self determination theory | Primary: Abstinence from smoking within 30 days Secondary: Number of days in last 30 days report eating breakfast, alcohol consumption, and exercise | ✓ | Abstinence from smoking (Tx1=11%, Tx2−=23%, Tx3=31%); Change in number of days: eating breakfast (Tx1=2.64, Tx2=6.51, Tx3=7.58), any drinking (Tx1=−.79, Tx2=−1.9, Tx3=−2.34), binge drinking (Tx1=−1, Tx2= −1.16, Tx3=−1.87), and exercise (Tx1=1.74, Tx2=4.57, Tx3=5.08) | Website with tailored messages + peer support online that included peer coach reviewing tracking, goals, and recording a video for the participants | In all groups, ~80% completed 4 out of 6 sessions. In tailored message + online peer support group, peer coaches completed 60% of calls; 48% of postings resulted in views. |
| Chung, 2016 (United States) | Tweeting to Health | College students who are healthy or overweight | Pre-post | n=12 | 2 month intervention and follow-up | Used formative study using focus groups to inform design | Height; Weight; Body fat percentage; self-reported intake of fruits/vegetables/SSBs; looked at Twitter messages; felt supported by group or study team; report any lifestyle changes | ✓ | Reported increased fruit (92%) /vegetable intake (58%); Decreased sugar sweet beverages (67%). Compliance with daily Fitbit wear (99%OW/73%HW of days) and dietary logging (82%OW/73%HW of days) | Log dietary intake via Twitter to Fitbit app; receive Twitter motivating messages; wear Fitbit; see others’ Fitbit; feed of healthy photos from Pinterest | Fitbit device wear was 99% OW and 78% of all days for OW and HW respectively. OW participants logged at least some dietary intake in Fitbit food diary on 82% of days versus 73% for HW participants. |
| Doyle, 2008 (United States) | Student Bodies 2 | Adolescents aged 12-18 who are at risk of overweight or overweight (≥85%) | RCT | n=83 | 16 weeks intervention and follow-up at 20 weeks | Cognitive behavioral strategies | Primary: Weight; height; eating disorder attitudes and behaviors Secondary: Dietary and physical activity related behaviors | ✓ | Difference in BMI post-intervention not sustained through follow-up. Decrease in shape concern (2.17-Tx; 1.96-Control). Intervention group greater use of dietary skills and physical activity related skills compared to control (no data reported). Report satisfied with discussion group but want more interaction. | Asynchronous moderated online discussion group with profiles; Private online journals | SB2 participants read 29.9% (SD, 27.3) of the Internet material (range, 0–90.7%), and 35% of the participants (n=14) viewed < 10% of the screens. 79% were satisfied with the program, 15.8% neither satisfied nor dissatisfied, and 5.3% dissatisfied. 63.2% were satisfied with the discussion group, 22.5% of the participants believed that there was not enough interaction |
| Godino, 2016 (United States) | Project SMART | Overweight or obese college students aged 18-35 | RCT | n=404 | 24 month intervention and follow-up | Michie’s taxonomy of twenty-six behavior change techniques. Intervention mapping and theory of planned behavior | Primary: Weight. Secondary: Weight, BMI (kg/ m2), waist circumference, arm circumference, systolic blood pressure, diastolic blood pressure, heart rate, and the level of engagement with intervention components. Physical activity, dietary intake, sedentary behaviors, eating behaviors, SSB consumption, eating away from home, quality of life, depression, self-esteem, psychosocial outcomes and social support. | Intervention group experienced greater weight loss at 6 months (−1·33 kg) and 12 months (−1·33 kg). However, at 24 months, there was no significant difference in weight loss. Significant difference between groups in proportion who lost 5% of their bodyweight at 6 months, waist circumference at 6 months, and systolic blood pressure at 24 months. | Facebook to connect participants; Smartphone sharing features to share goals, challenge participation, and health behaviors to Facebook; website with blog. | Defined as interactions with the intervention. Declined over time: 98 (9–265) interactions at 6 months, 76 (0–222) at 12 months, 41 (0–198) at 18 months, and 12 (0–161) at 24 months. | |
| Hutchesson, 2016 (Australia) | Be Positive, Be HealthE | Overweight female young adults aged 18-30 | Pre-post | n=18 | 3 months | Cognitive behavioral therapy strategies | Weight; waist circumference. | Significant reductions in weight, BMI, and waist circumference. | Online discussion group | Usage high for some features but declined over time. Other features had poor engagement. Discussion forum engagement poor throughout study. | |
| Jones, 2014 (United States) | StayingFit | Ninth grade students | Feasibility parallel, nonrandomized design | n=336 | None specified. | None specified. | Primary: Height and weight. Secondary: Weight and shape; | ✓ | BMI did not change. Significant changes in eating fruit, vegetables, consumption of soda for healthy weight. Significant changes in eating fruit for overweight. | Discussion board with questions posted for reaction. | Reported satisfaction with program content and implementation. |
| Kulik, 2015 (United States) | None specified. | Overweight girls aged 13-17 | Pilot randomized control intervention | n=41 | 16 weeks | Cognitive behavioral strategies | Social support and eating habits scale; social support and exercise scale; child and adolescent social support scale; adherence measured as number of brief check-ins and chat discussions; dietary intake; physical activity | Both groups experienced weight loss but no significant difference between groups (enhanced −6.4 vs control −6.47 lbs). Enhanced group experienced greater social support – friend encouragement for healthy eating (enhanced 15.05 vs control 9.24 pts; treatment effect 5.8) and friend support for exercise (enhanced 25.74 vs control 17.18pts; treatment effect 7.0). | Control include a standard cognitive behavioral weight loss program with 8 in-person meetings. Enhanced: standard program + peer support that included 8 inperson meetings (control) + small group activities+Facebook peer sessions. | High attendance of in-person sessions. Adherence to online support component low. 89% completed at least 4 sessions and had weight and questionnaire at Wk 16. Only 4 participants completed more than half the possible prescribed communications. 6/19 (32%) completed half of the chats with their Study Buddy and 4/19 (21%) completed half of the possible checkins with other group members. 32% (6/ 19) communicated with the group leader at least 75% or more of possible online contacts. | |
| Lana, 2014 (Spain and Mexico) | Prevencanadol | Adolescents aged 12-15 | Three group RCT: control; online intervention; online + SMS | n=2001 | 9 months | ASE Model;Transtheoretical model | Primary: Total behavioral cancer risk (smoking regularly; eating < 5 pieces of fruit or vegetables; eating ≥ 3 fat foods per day; quotient of cancer protecting to risk foods; obese or overweight; drinking excessively; physical activity less than 360 min per week; being in sun without sunscreen) | ✓ | 9 month outcomes: % not eating enough fruits decreased for all groups (−66.8 vs −62.6 vs −71.5). The enhanced "online + SMS" had a negative change in % who are overweight and obese (6.2 vs 23.8 vs −19.6). | Discussion group online | Not reported. 36.8% completed post-test. |
| Laska, 2016 (United States) | Choosing healthy options in college environments and settings (CHOICES) | Normal to overweight young adults aged 18-35 in two-year community and technical colleges | RCT | n=411 | 24 months | Ecological theories; social cognitive theory; social network theory | Diet: Weekly consumption of fast food, SSBs, breakfast, meals prepared at home; physical activity and screen time: energy expenditure leisure time, leisure time physical activity, television, computer use; sleep: total daily, days not getting enough rest, difficulty staying away more than 2 days, takes 30 minutes to fall asleep 3-7 nights per week. | ✓ | At 24 months, experimental group experienced reduction in fast food consumption (1.3 per week vs 1.4 in control) and increases in difficulty staying awake. | Social networking website to share behaviors. | Engagement in the website activities was also mixed with more than half of intervention participants logging onto the website during the first month, but then declining to 25–40% during the following 23 months of the intervention. |
| Leme, 2016 (Brazil) | Healthy Habits, Healthy Girls-Brazil program | Adolescent girls (mean age 16) | Cluster RCT in 10 public schools in low income communities | n=253 | 6 months | Michie's taxonomy of twenty-six behavior change techniques. Intervention mapping and theory of planned behavior | Body mass index; waist circumference; leisure time physical activity; sedentary behaviors (watching tv and using computers); dietary intake | ✓ | Intervention group: waist circumference (−2.28); screen time (−0.63 hr/day), sedentary activities (−0.92 hr/day, and veg(1.16 servings per day) /fruit intake (0.26 servings per day). | Includes twice weekly WhatsApp informational and motivational messages to users; group chat created for participants and moderator. | Intervention fidelity 60% for PA sessions; 53% for PE classes; and 80% for weekly nutrition and PA key messages. WhatsApp messages sent reported; not if they were read. |
| Napolitano, 2014 (United States) | None specified. | Young adults from a university aged 18-29 with BMI 25-50 | Three armed RCT: Facebook; Facebook + texts + feedback; control | n=52 | 8 weeks | None specified. | Height and weight. Physical activity behavior, goal setting and planning, physical activity self-efficacy, weight self-efficacy, adapted social support for diet and exercise, engagement/compliance, consumer satisfaction | ✓ | Facebook Plus group had significantly greater weight loss at 8 weeks (−2.4) vs Facebook (−0.63) vs control (−0.24) | Facebook delivered intervention with online content | Facebook group: 23.5% “liked” study-related posts; 41.2% posted or commented on study related content at least once; 88.2% responded to event invitations at least once. Facebook Plus: 22.2% “liked” the study-related posts on the Facebook group. 77.8% posted or commented on study-related content at least once. 72.2% responded to event invitations at least once. |
| Nawi, 2015 (Malaysia) | obeseGo! | Adolescents aged 16 with BMI > 25 | Cluster RCT in 6 secondary schools | n=108 | 12 weeks | None specified. | Height and weight. Waist circumference. Body fat. | No significant effects on outcomes. | Not reported | ||
| Smith, 2014 (Australia) | ATLAS | Adolescent boys aged 12-14 who are at risk for obesity | Cluster RCT in 14 schools in low income communities | n=361 | 8 months with 18 month follow up | Self-determination theory, social cognitive theory, transcontextual model of motivation | Height and weight. Body fat percentage. Physical activity. Muscular fitness. Resistance training skill competency. Recreational screen time. Sugar-sweetened beverage consumption. Physical self-concept. Subjective well-being. Pathological video gaming. Aggression. Daytime sleepiness. Motivation in school sports. Psychological needs satisfaction. Motivation to limit screen-time. Screen-time rules. Physical activity behavioral strategies. | ✓ | Reduced screen time (mean: −30 min/day), sugar sweetened beverages (mean: −0.6 glass/day). Increased muscular fitness (mean: 0.9 repetition) and training skills (mean: 5.7 units). | Smartphone with physical activity logging and peer assessments of resistance training skills | 95% of participants agreed or strongly agreed that the ATLAS program overall was enjoyable. 49% and 15% of participants had used the iPhone and Android apps. Did not report by feature. |
| Svetkey, 2015 (United States) | CITY | Young adults aged 18-35 with BMI > 25 | RCT: control; personal coaching + smartphone; mHealth | n=365 | 24 months | Social cognitive theory; and transtheoretical model | Weight change at 6, 12, and 24 months. Change in dietary pattern and physical fitness. | No significant weight loss across groups. | Smartphone app: Buddy system to send predetermined messages and basic profiles; challenge games; and tracking of diet, exercise, and weight. | Used the app 4.6 times/day in the first 6 months and 0.7 times/day in the final year | |
| n=384 | 6 months | ✓ | |||||||||
| Whittemore, 2013 (United States) | HEALTH [e]TEEN | Adolescents aged 14-17 | Cluster RCT in 3 schools: school based internet obesity prevention programs HEALTH [e]TEEN vs. HEALTH [e]TEEN + CST (coping skills training) | Theory of interactive technology; and social cognitive theory. | Sedentary behavior, nutrition behavior, physical activity, self-efficacy, satisfaction, and usage. | Significant increases in self-efficacy, healthy eating behaviors, fruit and vegetable intake, moderate and vigorous exercise, and stretching exercises. Decrease in sugary foods, junk food, and sedentary behaviors. | Included in all experimental groups: A blog for health coaching and social networking. | Usage used in statistical analysis but not reported. |
3.5.2. Study designs
The majority of studies, thirteen out of sixteen, used a randomized controlled trial design(Table 2) [24,48-52,54,56,57,60,61,63,65]. Two studies used non-experimental, pre/post design [58,62]. One used a parallel, non-experimental design [59].
3.5.3. Outcomes
Eleven studies had significant nutrition results (Table 2). Six studies showed improvements in clinical outcomes including weight [48,58,60], BMI [50,53,58], and waist circumference [58,65]. Dietary outcomes improved in eight studies including improvements in healthy eating behaviors [57] and fruit and vegetable intake [48,53,57,62,65] and reductions in unhealthy consumption of alcohol [49], sugar-sweetened beverages (SSBs) [24,48,62], sugary foods [57], junk food [57], and fast food [54]. Interventions improved physical activity with increases in exercise [49,57] and fitness and training skills [24]. Reductions were seen in screen time [24,65] and sedentary activities [57,65]. Lastly, in one study, users perceived enhanced peer support for healthy eating and exercise [66].
3.6. Feasibility and engagement
Limited measures of feasibility such as acceptability and demand are included in thirteen studies [24,48-51,55,56,58-60,62,66]. These included app and website usage, frequencies of feature interactions, reading/viewing content, participation in peer communication activities, and reported satisfaction. Limited and different sets of features were reported across studies. Five studies reported declines in interactions over time [48,51,56,58,69]. Among social media features, a community blog [48] and discussion board [58] reported low participation. Participants were happy with a different discussion board but wanted more interaction [50]. Peer communications’ participation was mixed, with some studies reporting low [66] participation [65], while others reporting high participation [48,70]. Fitbit had high adherence with 78–99% consistently wearing the device and food logging [62]. Facebook had high event invitations responses, moderate to high post commenting [60] but low response to recommended peer chats [66]. Among general features, high usage was reported with in-person sessions [65,66], text messaging [48], and online educational sessions [49,66]. Use of websites and apps was mixed [69] to low [24,48,50], often with declines over time [69,71] However, studies reported high satisfaction with content [24,50,59].
4. Discussion
The primary goal of our review was to evaluate available evidence regarding the use of social media in interventions designed to improve dietary behaviors and nutritional literacy among adolescents and young adults. This study fills an important gap in the existing knowledge regarding the efficacy of social media interventions in nutrition. Despite the growing recognition of social media’s potential to help young individuals improve health, few systematic reviews specifically examined this question. Previous reviews provide a partial account including descriptions of social media use without evaluation of outcomes [9,72] and featuring few interventions with no sustained outcomes [37]. While others have reviewed the use of social media for health [9], to the best of our knowledge, this review is the first to focus exclusively on use of social media for improving nutrition among adolescents and young adults.
The results show that use of social media in public health interventions for improving nutrition among adolescents and young adults is limited but promising. Of sixteen studies reviewed, eleven had significant nutrition outcomes suggesting social media may be valuable for delivering interventions for adolescents and young adults. The majority used high-quality study designs and showed clinical outcomes improvements, increases in healthy dietary behaviors, or reductions in unhealthy habits. Many studies were conducted in racially and ethnically diverse populations. Studies serving low income [24,65] populations and broader income levels [48,57,58,69] showed significant nutrition outcomes. All this suggests that interventions that incorporate digital technologies and, in particular, social media have a high potential of reaching diverse groups of adolescents and young adults.
However, together with these encouraging results, this review highlighted a number of limitations in the current research. First, while this review focused specifically on interventions that incorporate social media, it is important to note that the majority of reviewed interventions were complex, and included multiple features together with and often primary to social media. Many interventions included nutrition and behavior change features to help individuals better understand their dietary habits, make informed choices, and learn healthy eating skills. These included diet and activity tracking and feedback and educational content delivered using automated messages or online media. Several incorporated practical nutritional content, such as recipes and meal planning, helping to translate education into practical changes in diets. Finally, several included tailoring, such as personalized guidance on interpreting and modifying nutritional choices. Because these interventions were evaluated holistically, separating the impact of social media from the impact of other features remains a challenge. Further research is needed to compare the impact of social media with the impact of other interventions for healthy nutrition among adolescents and young adults, and to examine the relative contribution of social media to the impact of complex interventions.
Second, social media use in the included studies was conservative and engagement with social media was limited. Many interventions relied on traditional discussion boards and blogs to facilitate communication and disseminate information [73]. Others developed homegrown websites but incorporated similarly traditional discussion boards. While feasibility and usage of features were not uniformly reported, those studies that included data on user engagement showed mixed to low usage and decline in use overtime for these simpler forms of social media. These findings suggest that future interventions for healthy nutrition should consider leveraging newer and more innovative social media platforms that have new affordances and can inspire new health behaviors. These findings are further supported by studies that were screened, but did not qualify for the review. Many were not evaluated for clinical effectiveness but included innovative social media. For example, studies within this group found adolescents [74,76] and the general public [77-79] are using social media platforms to document and share meal photos, learn recipes, and showcase food preparation [78]. Though subject to reporting bias, taking photographs is perceived as faster and simpler than keeping standard food diaries [79,80]. In other such studies, researchers are using social media posts to learn about food choice influences [75], to incorporate photosharing of meals [81,82], and to allow users to collectively reflect on the food environment [83]. Though not targeted towards young people, others have explored social collaborative learning for collectively identifying healthy diet through food image tagging [84,85] and improving nutritional knowledge through crowdsourcing [86,87]. Another area that has received considerable attention outside the clinical domain is gamification. Studies in this review using online games saw limited long-term engagement [53,54,58]. However, behavioral challenges and reminders led to sustained engagement and diet logging in one study [62]. Others have used games to introduce heuristics for healthy eating [88,89]. Although these technologies are innovative in design, evaluation is needed to determine the effectiveness in improving nutrition.
Third, while some studies in this review did examine the efficacy of social media as a novel mechanism for delivery of behavioral interventions, many used social media to add social support component to a more traditional behavioral intervention. In many cases, the interventions required that the participants socialize with other users of the same intervention, rather than leverage their existing social connections and networks. Our review shows that while both of these approaches appear to have a positive impact on behaviors, adding social components to behavioral interventions does not always lead to high user engagement. This is consistent with findings of previous studies of social media usage patterns that suggest that individuals are more likely to use social media sites to maintain existing social networks, rather than to develop new relationships [90]. Consequently, leveraging existing social media platforms and existing social connections may help to increase low adoption and engagement barriers and help to more fully leverage the positive impact of social media on individuals’ health.
Further, there remain aspects of social media within the adolescent and young adult population not explored within studies included in this review. One notable trend is the popularity of platforms that support transient communication channels that leave no permanent traces like SnapChat and Whisper. Though young people increasingly seek an anonymous component in social media, reliance on anonymity in communication around nutrition may inadvertently reinforce unhealthy eating behaviors and facilitate the spread of misinformation [91]. Anonymity may remove barriers to sharing nutritional experience but, future research should examine dangerous unintended effects. Another area that has not received sufficient attention is tailoring of individuals’ access to social media about nutrition. Studies in this review tailored content to individuals’ characteristics [48,49] but, none tailored social media content. Such tailoring can further promote observational learning among individuals.
Finally, future research can address methodological issues in the current studies. Although most studies used randomized controlled trials, few included long-term follow up to examine sustainability. Feasibility and engagement of technical features also need to be consistently included and operationalized to understand their roles in affecting outcomes. Most included only clinical and behavioral outcomes. However, the influence of these interventions on social support and the possible effect of social support on intervention outcomes is unclear. Three studies examined social support but only one found adolescents to have greater feelings of healthy eating support [66]. Lastly, more evidence is needed to understand which features contribute to improved outcomes. Using study designs such as cross-over or factorial design could provide such insight.
Limitations to our study include potential exclusion of relevant articles. Our search strategy may have been missing useful keywords. For example, terms describing adolescents and young adults are not standardized across disciplines and some synonymous terms may have been missed.
5. Conclusion
This systematic literature review included studies that analyzed the impact of informatics interventions incorporating social media on nutritional literacy and eating behaviors among adolescents and young adults. Social media plays an integral role in the lives of adolescents and young adults [92,93] and this review suggests that it is a promising feature to include in nutrition interventions. We identified 11 out of 16 interventions for adolescents and young adults that included social media with short-term positive nutrition-related clinical or behavioral outcomes. The studies included in the review utilized a traditional, limited set of social media features. However, the functionality of social media is more comprehensive and expanding. More research should be conducted with innovative features and existing popular platforms to fully explore the potential of social media with adolescents and young adults.
Supplementary Material
Summary table.
What was already known on the topic:
A general scope of how social media is being used in health interventions and research with adolescents and young adults (e.g. for recruitment, information dissemination, etc).
The effect of social media on health outcomes among adolescents and young adults was unclear—one review found no significant outcomes within such interventions.
What this study added to our knowledge:
A general overview of how social media is being used in nutrition interventions with adolescents and young adults.
There is a growing body of nutrition interventions featuring social media that show positive clinical and behavioral outcomes within this age group.
The use of social media for nutrition interventions with adolescents and young adults is limited. Current social media interventions utilize only basic social media features, did not evaluate the efficacy of social media components, and did not differentiate between the efficacy of social media com-pared to other delivery mechanisms.
Acknowledgements
This work was supported by the National Library of Medicine [T15 LM00707] and the National Science Foundation Smart and Connected Health [1551708]
Footnotes
Statement on conflicts of interest
None.
References
- [1].Dick B, Ferguson BJ, Health for the world’s adolescents: a second chance in the second decade, J. Adolesc. Health 56 (January (1)) (2015) 3–6. [DOI] [PubMed] [Google Scholar]
- [2].Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM, Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005-2010, Circulation 127 (April (13)) (2013) 1369–1376. [DOI] [PubMed] [Google Scholar]
- [3].Niemeier HM, Raynor HA, Lloyd-Richardson EE, Rogers ML, Wing RR, Fast food consumption and breakfast skipping: predictors of weight gain from adolescence to adulthood in a nationally representative sample, J. Adolesc. Health 39 (December (6)) (2006) 842–849. [DOI] [PubMed] [Google Scholar]
- [4].Mikkilä V, Räsänen L, Raitakari OT, Pietinen P, Viikari J, Consistent dietary patterns identified from childhood to adulthood: the cardiovascular risk in young finns study, Br. J. Nutr. 93 (June (6)) (2005) 923–931. [DOI] [PubMed] [Google Scholar]
- [5].Arnett JJ, Emerging adulthood: a theory of development from the late teens through the twenties, Am. Psychol 55 (5) (2000) 469–480. [PubMed] [Google Scholar]
- [6].Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA, Emerging adulthood and College-aged youth: an overlooked age for weight-related behavior change, Obesity 16 (October 10) (2008) 2205–2211. [DOI] [PubMed] [Google Scholar]
- [7].HOELSCHER DM, EVANS A, PARCEL G, KELDER S, Designing effective nutrition interventions for adolescents, J. Am. Diet. Assoc 102 (March (3), Supplement) (2002) S52–63. [DOI] [PubMed] [Google Scholar]
- [8].DiFilippo KN, Huang W-H, Andrade JE, Chapman-Novakofski KM, The use of mobile apps to improve nutrition outcomes: a systematic literature review, J. Telemed. Telecare 12 (February) (2015) 1357633X15572203. [DOI] [PubMed] [Google Scholar]
- [9].Yonker LM, Zan S, Scirica CV, Jethwani K, Kinane TB, Friending” teens: systematic review of social media in adolescent and young adult health care, J. Med. Int. Res 17 (January 1) (2015) e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lenhart Amanda. Teens, Social Media & Technology Overview 2015 [Internet]. Pew Research Center: Internet, Science & Tech; 2015. [cited 2016 Mar 21]. Available from: http://www.pewinternet.org/2015/04/09/teens-social-media-technology-2015/. [Google Scholar]
- [11].Perrin Andrew. Social Media Usage: 2005–2015 [Internet]. Pew Research Center: Internet, Science & Tech; 2015. [cited 2016 Aug 9]. Available from: http://www.pewinternet.org/2015/10/08/social-networking-usage-2005-2015/. [Google Scholar]
- [12].Smartphone Ownership Highest Among Young Adults, Those With High Income/ Education Levels [Internet]. Pew Research Center: Internet, Science & Tech; 2015. [cited 2016 Sep 20]. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/pi_2015-04-01_smartphones_07/. [Google Scholar]
- [13].Young Adults Rely Heavily on Their Smartphones for Job Seeking, Educational Content, and Health Information [Internet]. Pew Research Center: Internet, Science & Tech; 2015. [cited 2016 Sep 20]. Available from: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/pi_2015-04-01_smartphones_15/. [Google Scholar]
- [14].Ajie WN, Chapman-Novakofski KM, Impact of computer-mediated, obesity-related nutrition education interventions for adolescents: a systematic review, J. Adolesc. Health 54 (June 6) (2014) 631–645. [DOI] [PubMed] [Google Scholar]
- [15].Ali MM, Amialchuk A, Heiland FW, Weight-related behavior among adolescents: the role of peer effects, PLoS One 6 (6) (2011) e21179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fortin B, Yazbeck M, Peer effects, fast food consumption and adolescent weight gain, J. Health Econ. 42 (July) (2015) 125–138. [DOI] [PubMed] [Google Scholar]
- [17].Lau RR, Quadrel MJ, Hartman KA, Development and change of Young adults’ preventive health beliefs and behavior: influence from parents and peers, J. Health Social Behav 31 (3) (1990) 240–259. [PubMed] [Google Scholar]
- [18].Ali MM, Amialchuk A, Heiland FW, Weight-related behavior among adolescents: the role of peer effects, PLoS One 6 (6) (2011) [Internet] Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L362012911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bruening M, Eisenberg M, MacLehose R, Nanney MS, Story M, Neumark-Sztainer D, Relationship between adolescents’ and their friends’ eating behaviors: breakfast, fruit, vegetable, whole-grain, and dairy intake, J. Acad. Nutr. Diet 112 (October 10) (2012) 1608–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wouters EJM, Geenen R, The influence of friendship groups and media on eating behavior and physical activity in adolescents, Int. J. Child Adolesc. Health 6 (3) (2013) 249–258. [Google Scholar]
- [21].Wouters EJM, Geenen R, The influence of friendship groups and media on eating behavior and physical activity in adolescents, Int. J. Child Adolesc. Health 6 (3) (2013) 249–258. [Google Scholar]
- [22].Christakis NA, Fowler JH, The spread of obesity in a large social network over 32 years, New Engl. J. Med. 357 (July 4) (2007) 370–379. [DOI] [PubMed] [Google Scholar]
- [23].Nguyen B, Shrewsbury VA, O’Connor J, Steinbeck KS, Hill AJ, Shah S, et al. , Two-year outcomes of an adjunctive telephone coaching and electronic contact intervention for adolescent weight-loss maintenance: the loozit randomized controlled trial, Int. J. Obes. (Lond.) 37 (March 3) (2013) 468–472. [DOI] [PubMed] [Google Scholar]
- [24].Smith JJ, Morgan PJ, Plotnikoff RC, Dally KA, Salmon J, Okely AD, et al. , Smart-phone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT, Pediatrics 134 (September 3) (2014) e723–731. [DOI] [PubMed] [Google Scholar]
- [25].social media: definition of social media in Oxford dictionary (American English) (US) [Internet], [cited 2016 Aug 8]. Available from: http://www.oxforddictionaries.com/us/definition/american_english/social-media.
- [26].Best P, Manktelow R, Taylor B, Online communication, social media and adolescent wellbeing: a systematic narrative review, Children Youth Serv. Rev 41 (June) (2014) 27–36. [Google Scholar]
- [27].Hebden L, Chey T, Allman-Farinelli M, Lifestyle intervention for preventing weight gain in young adults: a systematic review and meta-analysis of RCTs, Obes Rev. 13 (8) (2012) 692–710. [DOI] [PubMed] [Google Scholar]
- [28].Free C, Phillips Ct., Galli L, Watson L, Felix L, Edwards P, et al. , The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review Cornford T, editor, PLoS Med 10 (January 1) (2013) e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Wang Q, Egelandsdal B, Amdam Ct.V., Almli VL, Oostindjer M, Diet and physical activity apps: perceived effectiveness by app users, JMIR Mhealth Uhealth 4 (2) (2016) e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hamm MP, Shulhan J, Williams G, Milne A, Scott SD, Hartling L, A systematic review of the use and effectiveness of social media in child health, BMC Pediatr. 2 (June 14) (2014) 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Maher CA, Lewis LK, Ferrar K, Marshall S, De Bourdeaudhuij I, Vandelanotte C, Are health behavior change interventions that use online social networks effective? A systematic review, J. Med. Internet Res. 16 (2) (2014) e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Merolli M, Gray K, Martin-Sanchez F, Health outcomes and related effects of using social media in chronic disease management: a literature review and analysis of affordances, J. Biomed. Inf 46 (December 6) (2013) 957–969. [DOI] [PubMed] [Google Scholar]
- [33].Williams G, Hamm MP, Shulhan J, Vandermeer B, Hartling L, Social media interventions for diet and exercise behaviours: a systematic review and meta-analysis of randomised controlled trials, BMJ Open 4 (2) (2014) e003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Laranjo L, Arguel A, Neves AL, Gallagher AM, Kaplan R, Mortimer N, et al. , The influence of social networking sites on health behavior change: a systematic review and meta-analysis, J. Am. Med. Inf. Assoc. JAMIA (July) (2014) amiajnl-2014–002841-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Plotnikoff RC, Costigan SA, Williams RL, Hutchesson MJ, Kennedy SG, Robards SL, et al. , Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: a systematic review and meta-analysis, Int. J. Behav. Nutr. Phys. Act 12 (2015) 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Cushing CC, Steele RG, A meta-analytic review of eHealth interventions for pediatric health promoting and maintaining behaviors, J. Pediatr. Psychol. 35 (October 9) (2010) 937–949. [DOI] [PubMed] [Google Scholar]
- [37].Shaw JM, Mitchell CA, Welch AJ, Williamson MJ, Social media used as a health intervention in adolescent health: a systematic review of the literature, Digital Health 1 (January) (2015) 2055207615588395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nour M, Chen J, Allman-Farinelli M, Efficacy and external validity of electronic and Mobile phone-based interventions promoting vegetable intake in young adults: systematic review and meta-analysis, J. Med. Internet Res. 18 (4) (2016) e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Wickham CA, Carbone ET, Who’s calling for weight loss? A systematic review of mobile phone weight loss programs for adolescents, Nutr. Rev 73 (6) (2015) 386–398. [DOI] [PubMed] [Google Scholar]
- [40].Dute DJ, Bemelmans WJE, Breda J, Using mobile apps to promote a healthy lifestyle among adolescents and students: a review of the theoretical basis and lessons learned, JMIR Mhealth Uhealth 4 (2) (2016) e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Hackman CL, Knowlden AP, Theory of reasoned action and theory of planned behavior-based dietary interventions in adolescents and young adults: a systematic review, Adolesc. Health Med. Ther. 5 (2014) 101–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hamel LM, Robbins LB, Computer-and web-based interventions to promote healthy eating among children and adolescents: a systematic review, J. Adv. Nurs 69 (January 1) (2013) 16–30. [DOI] [PubMed] [Google Scholar]
- [43].Ajie WN, Chapman-Novakofski KM, Impact of computer-mediated, obesity-related nutrition education interventions for adolescents: a systematic review, J. Adolesc. Health 54 (6) (2014) 631–645. [DOI] [PubMed] [Google Scholar]
- [44].Chen J-L, Wilkosz ME, Efficacy of technology-based interventions for obesity prevention in adolescents: a systematic review, Adolesc. Health Med. Ther (August) (2014) 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Quelly SB, Norris AE, DiPietro JL, Impact of mobile apps to combat obesity in children and adolescents: a systematic literature review, J. Spec. Pediatr. Nurs 21 (1) (2016) 5–17. [DOI] [PubMed] [Google Scholar]
- [46].Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, PLOS Med 6 (July 7) (2009) el000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Downs SH, Black N, The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions, J. Epidemiol. Community Health 52 (June 6) (1998) 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Allman-Farinelli M, Partridge SR, McGeechan K, Balestracci K, Hebden L, Wong A, et al. , A Mobile health lifestyle program for prevention of weight gain in Young adults (TXT2BFiT): nine-month outcomes of a randomized controlled trial, JMIR Mhealth Uhealth 4 (2) (2016) e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].An LC, Demers MRS, Kirch MA, Considine-Dunn S, Nair V, Dasgupta K, et al. , A randomized trial of an avatar-hosted multiple behavior change intervention for young adult smokers, J. Natl. Cancer Inst. Monogr 2013 (47) (2013) 209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, Wilfley DE, Reduction of overweight and eating disorder symptoms via the internet in adolescents: a randomized controlled trial, J. Adolesc. Health 43 (2) (2008) 172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Godino JG, Merchant G, Norman GJ, Donohue MC, Marshall SJ, Fowler JH, et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2 year, parallel-group, randomised, controlled trial. The Lancet Diabetes & Endocrinology [Internet]. 2016. July [cited 2016 Jul 25]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S221385871630105X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kulik NL, Fisher EB, Ward DS, Ennett ST, Bowling JM, Tate DF, Peer support enhanced social support in adolescent females during weight loss, Am. J. Health Behav 38 (5) (2014) 789–800. [DOI] [PubMed] [Google Scholar]
- [53].Lana A, Faya-Ornia G, López ML , Impact of a web-based intervention supplemented with text messages to improve cancer prevention behaviors among adolescents: results from a randomized controlled trial, Preventive Med 59 (February) (2014) 54–59. [DOI] [PubMed] [Google Scholar]
- [54].Laska MN, Lytle LA, Nanney MS, Moe SG, Linde JA, Hannan PJ, Results of a 2-year randomized, controlled obesity prevention trial: effects on diet, activity and sleep behaviors in an at-risk young adult population, Preventive Med 89 (August) (2016) 230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Leme ACB, Philippi ST, The “healthy habits, healthy girls” randomized controlled trial for girls: study design, protocol, and baseline results, Cad Saude Publica 31 (7) (2015) 1381–1394. [DOI] [PubMed] [Google Scholar]
- [56].Svetkey LP, Batch BC, Lin P-H, Intille SS, Corsino L, Tyson CC, et al. , Cell phone intervention for you (CITY): a randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology, Obesity 23 (11) (2015) 2133–2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Whittemore R, Jeon S, Grey M, An internet obesity prevention program for adolescents, J. Adolesc. Health 52 (April 4) (2013) 439–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Hutchesson MJ, Morgan PJ, Callister R, Pranata I, Skinner G, Collins CE, Be positive be healthe: development and implementation of a targeted e-health weight loss program for young women, Telemed. J. E Health 22 (January 6) (2016) 519–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Jones M, Taylor Lynch K, Kass AE, Burrows A, Williams J, Wilfley DE, et al. , Healthy weight regulation and eating disorder prevention in high school students: a universal and targeted web-based intervention, J. Med. Internet Res. 16 (2) (2014) e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD, Using facebook and text messaging to deliver a weight loss program to college students, Obesity 21 (1) (2013) 25–31. [DOI] [PubMed] [Google Scholar]
- [61].Nawi AM, Jamaludin FIC, Effect of internet-based intervention on obesity among adolescents in Kuala Lumpur: a school-based cluster randomised trial, Malays J. Med. Sci. 22 (4) (2015) 47–56. [PMC free article] [PubMed] [Google Scholar]
- [62].Chung AE, Skinner AC, Hasty SE, Perrin EM, Tweeting to health a novel mHealth intervention using fitbits and twitter to foster healthy lifestyles, Clin. Pediatr 16 (June) (2016) 9922816653385. [DOI] [PubMed] [Google Scholar]
- [63].Lana A, del Valle MO, Lopez S, Faya-Ornia G, Lopez ML, Study protocol of a randomized controlled trial to improve cancer prevention behaviors in adolescents and adults using a web-based intervention supplemented with SMS, BMC Public Health 13 (2013) 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Lytle LA, Moe SG, Nanney MS, Laska MN, Linde JA, Designing a weight gain prevention trial for young adults: the CHOICES study, Am. J. Health Educ 45 (January 2) (2014) 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Leme ACB, Lubans DR, Guerra PH, Dewar D, Toassa EC, Philippi ST, Preventing obesity among Brazilian adolescent girls: six-month outcomes of the healthy habits, healthy girls-Brazil school-based randomized controlled trial, Prev. Med. 86 (2016) ((Leme A.C.B., acarolina@usp.br; Toassa E.C.; Philippi S.T.) Departamento de Nutrição, Faculdade de Saúde Pública, Universidade de São Paulo, São Paulo, Brazil):77–83. [DOI] [PubMed] [Google Scholar]
- [66].Kulik N, Ennett ST, Ward DS, Bowling JM, Fisher EB, Tate DF, Brief report: a randomized controlled trial examining peer support and behavioral weight loss treatment, J. Adolesc 44 (October) (2015) 117–123. [DOI] [PubMed] [Google Scholar]
- [67].Deterding S, Dixon D, Khaled R, Nacke L, From game design elements to gamefulness: defining “Gamification.”, Proceedings of the 15th International Academic MindTrek Conference: Envisioning Future Media Environments (2011) 9–15 [Internet] (MindTrek’ 11). Available from: http://doi.acm.org/10.1145/2181037.2181040. [Google Scholar]
- [68].Nawi AM, Jamaludin FIC, Effect of internet-based intervention on obesity among adolescents in Kuala Lumpur: a school-based cluster randomised trial, Malays J. Med. Sci 22 (4) (2015) 47–56. [PMC free article] [PubMed] [Google Scholar]
- [69].Laska MN, Sevcik SM, Moe SG, Petrich CA, Nanney MS, Linde JA, et al. , A 2-year young adult obesity prevention trial in the US: process evaluation results, Health Promot. Int 31 (December 4) (2016) 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].An LC, Demers MRS, Kirch MA, Considine-Dunn S, Nair V, Dasgupta K, et al. , A randomized trial of an avatar-hosted multiple behavior change intervention for young adult smokers, J. Natl. Cancer Inst. Monogr 2013 (December 47) (2013) 209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Svetkey LP, Batch BC, Lin P-H, Intille SS, Corsino L, Tyson CC, et al. , Cell phone intervention for you (CITY): a randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology, Obesity 23 (11) (2015) 2133–2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Park BK, Calamaro C, A systematic review of social networking sites: innovative platforms for health research targeting adolescents and young adults, J. Nurs. Scholarship 45 (3) (2013) 256–264. [DOI] [PubMed] [Google Scholar]
- [73].Anderson M, Jiang J, Teens, Social Media & Technology 2018 [Internet]. Pew Research Center: Internet, Science & Tech, [cited 2018 Jul 11]. Available from: (2018) http://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018/. [Google Scholar]
- [74].Holmberg CE, Chaplin J, Hillman T, Berg C, Adolescents’ presentation of food in social media: An explorative study, Appetite 99 (April 1) (2016) 121–129. [DOI] [PubMed] [Google Scholar]
- [75].Sharma SS, De Choudhury M, Measuring and characterizing nutritional information of food and ingestion content in instagram, Proceedings of the 24th International Conference on World Wide Web [Internet] (2015), 10.1145/2740908.2742754 [cited 2016 Oct 7]. p. 115–116. (WWW’ 15 Companion). Available from:. [DOI] [Google Scholar]
- [76].Mejova Y, Haddadi H, Noulas A, Weber I, #FoodPorn: obesity patterns in culinary interactions, Proceedings of the 5th International Conference on Digital Health 2015 (2015) [Internet] [cited 2017 Apr 3]. p. 51–58. (DH’ 15). Available from: http://doi.acm.Org/10.1145/2750511.2750524. [Google Scholar]
- [77].Abbar S, Mejova Y, Weber I, You Tweet What You Eat: Studying Food Consumption Through Twitter. In: Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, ACM, New York, NY, USA, 2015, pp. 3197–3206 [Internet] (CHI’ 15). Available from: http://doi.acm.org/10.1145/2702123.2702153. [Google Scholar]
- [78].Vaterlaus JM, Patten EV, Roche C, Young JA, #Gettinghealthy: the perceived influence of social media on young adult health behaviors, Comput. Human Behav 45 (April) (2015) 151–157. [Google Scholar]
- [79].Higgins JA, LaSalle AL, Zhaoxing P, Kasten MY, Bing KN, Ridzon SE, et al. , Validation of photographic food records in children: are pictures really worth a thousand words? Eur. J. Clin. Nutr 63 (August 8) (2009) 1025–1033. [DOI] [PubMed] [Google Scholar]
- [80].Martin CK, Nicklas T, Gunturk B, Correa JB, Allen HR, Champagne C, Measuring food intake with digital photography, J. Human Nutr. Diet 27 (s1) (2018) 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Park BK, Nahm E-S, Rogers VE, Development of a teen-friendly health education program on facebook: lessons learned, J. Pediatr. Health Care 30 (June 3) (2018) 197–207 2016. [DOI] [PubMed] [Google Scholar]
- [82].Yi-Frazier JP, Cochrane K, Mitrovich C, Pascual M, Buscaino E, Eaton L, et al. , Using instagram as a modified application of photovoice for storytelling and sharing in adolescents with type 1 diabetes, Qual. Health Res. 25 (10) (2015) 1372–1382 lip. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Parker AG, McClendon I, Grevet C, Ayo V, Chung W, Johnson V, et al I Am What I Eat: Identity & Critical Thinking in an Online Health Forum for Kids. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, [Internet] ACM, New York, NY, USA, 2013, 10.1145/2470654.2481338 [cited 2016 Oct 28]. p. 2437–2446. (CHI’ 13). Available from:. [DOI] [Google Scholar]
- [84].Mamykina L, Miller AD, Grevet C, Medynskiy Y, Terry MA, Mynatt ED, et al. , Examining the Impact of Collaborative Tagging on Sensemaking in Nutrition Management. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, [Internet] ACM, New York, NY, USA, 2011, pp. 657–666, 10.1145/1978942.1979037 (CHI’ 11). Available from:. [DOI] [Google Scholar]
- [85].Linehan C, Doughty M, Lawson S, Kirman B, Olivier P, Moynihan P, Tagliatelle: Social Tagging to Encourage Healthier Eating. In: CHI’ 10 Extended Abstracts on Human Factors in Computing Systems, [Internet] ACM, New York, NY, USA, 2010, pp. 3331–3336, 10.1145/1753846.1753980 (CHI EA’ 10). Available from:. [DOI] [Google Scholar]
- [86].Burgermaster M, Gajos KZ, Davidson P, Mamykina L, The Role of Explanations in Casual Observational Learning About Nutrition. In: Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, [Internet] ACM, New York, NY, USA, 2017, 10.1145/3025453.3025874 p. 4097–4145. (CHI’ 17). Available from:. [DOI] [Google Scholar]
- [87].Mamykina L, Smyth TN, Dimond JP, Gajos KZ, Learning from the crowd: observational learning in crowdsourcing communities, Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems, ACM, New York, NY, USA, 2016, pp. 2635–2644 (CHI’ 16). Available from: http://doi.acm.org/10.1145/2858036.2858560 [Internet].. [Google Scholar]
- [88].Khanana K, Law EL-C, Designing children’s digital games on nutrition with playability heuristics, CHI’ 13 Extended Abstracts on Human Factors in Computing Systems, ACM, New York, NY, USA, 2013. [cited 2014 Dec 23]. p. 1071–1076. (CHI EA’ 13). Available from: http://doi.acm.org/10.1145/2468356.2468548 [Internet].. [Google Scholar]
- [89].Mansour A, Barve M, Bhat S, Do EY-L, MunchCrunch: a game to learn healthy-eating heuristics, Proceedings of the 8th International Conference on Interaction Design and Children (2009) [cited 2014 Nov 5]. p. 166–169. (IDC’ 09). Available from: http://doi.acm.org/10.1145/1551788.1551818 [Internet].. [Google Scholar]
- [90].Heimlich R, Using Social Media to Keep in Touch, [Internet] Pew Research Center, 2011. [cited 2018 Jul 11]. Available from: http://www.pewresearch.org/fact-tank/2011/12/22/using-social-media-to-keep-in-touch/. [Google Scholar]
- [91].Syed-Abdul S, Fernandez-Luque L, Jian W-S, Li Y-C, Crain S, Hsu M-H, et al. , Misleading health-related information promoted through video-based social media: anorexia on YouTube, J. Med. Internet Res. 15 (February 2) (2013) e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].boyd d.. Why Youth (Heart) Social Network Sites: The Role of Networked Publics in Teenage Social Life [Internet]. Rochester, NY: Social Science Research Network; 2007. December [cited 2017 Apr 3]. Report No.: ID 1518924. Available from:https://papers.ssrn.com/abstract=1518924. [Google Scholar]
- [93].Pater JA, Miller AD, Mynatt ED, This digital life: a neighborhood-based study of adolescents’ lives online, Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems (2015) [cited 2017 Apr 3]. p. 2305–2314. (CHI’ 15). Available from: http://doi.acm.org/10.1145/2702123.2702534 [Internet]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.