Recently in Gut and elsewhere,1–3 rare and common hypomorphic sucrase-isomaltase (SI) gene variants have been linked to an increased risk of IBS. Similar to congenital SI deficiency (a form of carbohydrate malabsorption caused by homozygous SI loss-of-function mutations),4 reduced SI enzymatic activity may trigger IBS symptoms via colonic accumulation of undigested disaccharides from starch and sucrose, resulting in fermentation with gas production and osmotic diarrhoea. This information holds potential for patients’ stratification, and the identification of IBS subgroups better suited to benefit from specific dietary restrictions. For instance, diets low in short chain carbohydrates like the FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols that are poorly absorbed in the small intestine) have been shown to be effective in reducing GI symptoms in some patients with IBS,5 6 though this has not been studied in relation to SI genotype and/or function. While sucrose and, in part, starch are not specifically restricted in a standard low FODMAP diet, such a therapeutic approach may be less effective in individuals whose reduced SI activity contributes to symptoms. Hence, a low FODMAP diet may be less effective in patients with IBS carrying SI hypomorphic variants.
To test this hypothesis, we sought to re-evaluate results obtained in a previous randomised controlled trial of the low FODMAP diet in patients with IBS with diarrhoea (IBS-D),7on stratification of participants for SI genotype data. From the original study, 46 patients were selected for these new analyses (table 1), based on available full clinical information and high-quality genotype data from Illumina Infinium HumanCoreExome arrays, as previously reported.3 Endpoints of interest were IBS-D symptom relief (≥50%) and reduction of abdominal pain (30%), both studied and defined as in the original investigation.7 Based on available genotype data, we restricted the analysis to SI hypomorphic (pathogenic) variants as previously described,3 and three rare (Arg774Gly [rs147207752]; Tyr975His [rs146785675]; Glu1414Lys [rs145734588]) and one common (Val15Phe [rs9290264]) such variants were detected in the low FODMAP treated cohort (table 1). Due to the small sample size, we stratified patients into carriers and non-carriers of hypomorphic variants (either rare or common), and compared these groups for their response to dietary treatment. As shown in figure 1, while an overall 52.2% of patients experienced adequate IBS-D symptoms relief, SI carriers benefited significantly less than SI non-carriers from the low FODMAP diet, with respective response rates 43.5% vs 60.9% (p=0.031; OR=4.66). A similar trend was also observed for abdominal pain reduction, thought this did not reach statistical significance (50% in the whole cohort, 47.8% in SI carriers and 52.2% in SI non-carriers, p=0.231). Genotype data were also available for 39 patients (from the original study) who followed the modified National Institute for Health and Care Excellence (mNICE) dietary guidelines which also reduced carbohydrate consumption.7 While trends similar to the low FODMAP-treated group were observed in these patients (not shown), a combined FODMAP-mNICE analysis strengthened the evidence of association between SI genotype and response outcome: the increased sample size allowed further stratification of patients into individual genotype groups, and this revealed a correlation between SI hypomorphic copy number and response rates which were lowest in patients carrying two copies (16.7%) versus patients with one (42.1%) or no copies (56.1%) (p=0.0039; OR=3.33).
Table 1.
Demographic and clinical characteristics of low fermentable oligo-, di-, mono-saccharides and polyols treated IBS with diarrhoea patients, in relation to sucrase-isomaltase genotype
| Characteristic | Non-carriers n=23 |
Carriers n=23 |
| Average age (years) | 41.22±13.55 | 43.39±16.00 |
| Sex (female/male) | 14/9 | 17/6 |
| Race (white/other) | 19/4 | 17/6 |
| Average body mass index (kg/m2) | 26.28±5.72 | 28.38±6.71 |
| Abdominal pain (average score, baseline) | 5.03±1.43 | 5.27±1.61 |
| Bloating (average score, baseline) | 4.77±1.86 | 4.84±1.89 |
| Urgency score (baseline) | 5.02±1.79 | 4.90±2.18 |
| Stool frequency (average score at baseline) | 3.41±1.38 | 3.60±2.03 |
| Bristol Stool Form (average, baseline) | 5.15±0.51 | 5.29±0.71 |
| Rare hypomorphic variants (Arg774Gly; Tyr975His; Glu1414Lys) | 0 | 3 |
| Common hypomorphic variant (Val15Phe) | 0 | 20 |
Figure 1.
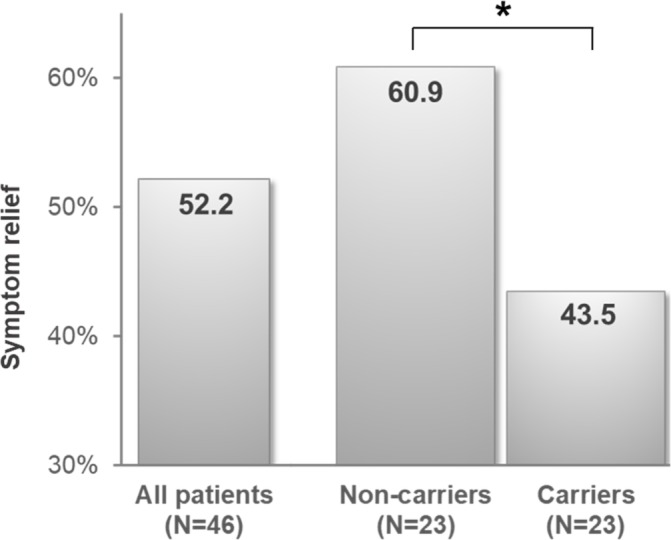
Decreased symptom relief in patients with IBS and diarrhoea carrying sucrase-isomaltase (SI) hypomorphic variants. Adequate symptom relief in low fermentable oligo-, di-, mono-saccharides and polyols treated individuals, stratified according to SI genotype into carriers and non-carriers of hypomorphic variants. *P=0.031 (one-tailed logistic regression analysis, adjusting for age, sex, body mass index and ethnicity).
In conclusion, we report initial evidence that carrying SI hypomorphic variants is associated with a threefold to fourfold reduction in the likelihood of responding to dietary approaches that restrict the intake of carbohydrates, particularly FODMAPs. While study limitations include small sample size and lack of mucosal disaccharidase measurements in patients, this may bear implications for the development of patient treatment stratification strategies in IBS.
Footnotes
WDC and MD’A contributed equally.
Contributors: MD’A and WDC: study design and supervision. SE, ALP, JLM and WDC: patients characterisation, data acquisition. TZ: statistical analyses. TZ, SE, WDC and MD’A: data analysis and interpretation. MD’A obtained funding and technical support, drafted the manuscript, with input and critical revision from all other authors. All authors approved the final draft of the manuscript.
Funding: This study was supported by grants from the Swedish Research Council (VR project nr 2017- 02403), and an unrestricted research grant from QOL Medical to MD’A. TZ is supported by the China Scholarship Council (CSC) programme.
Competing interests: The project has been partially supported by an unrestricted research grant from QOL Medical to MD’A.
Patient consent: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Henström M, Diekmann L, Bonfiglio F, et al. Functional variants in the sucrase-isomaltase gene associate with increased risk of irritable bowel syndrome. Gut 2018;67:263–70. 10.1136/gutjnl-2016-312456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thingholm L, Rühlemann M, Wang J, et al. Sucrase-isomaltase 15Phe IBS risk variant in relation to dietary carbohydrates and faecal microbiota composition. Gut 2019;68:177–8. 10.1136/gutjnl-2017-315841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Garcia-Etxebarria K, Zheng T, Bonfiglio F, et al. Increased prevalence of rare sucrase-isomaltase pathogenic variants in irritable bowel syndrome patients. Clin Gastroenterol Hepatol 2018;16:1673–6. 10.1016/j.cgh.2018.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gericke B, Amiri M, Naim HY. The multiple roles of sucrase-isomaltase in the intestinal physiology. Mol Cell Pediatr 2016;3:2 10.1186/s40348-016-0033-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Giorgio R, Volta U, Gibson PR, et al. gluten and FODMAPs in IBS: facts or fiction? Gut 2016;65:169–78. [DOI] [PubMed] [Google Scholar]
- 6. Dolan R, Chey WD, Eswaran S. The role of diet in the management of irritable bowel syndrome: a focus on FODMAPs. Expert Rev Gastroenterol Hepatol 2018;12:607–15. 10.1080/17474124.2018.1476138 [DOI] [PubMed] [Google Scholar]
- 7. Eswaran SL, Chey WD, Han-Markey T, et al. A randomized controlled trial comparing the low FODMAP Diet vs. Modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol 2016;111:1824–32. 10.1038/ajg.2016.434 [DOI] [PubMed] [Google Scholar]


