Abstract
Background:
Health care career pipeline training programs are one solution to increasing the number of minority and underrepresented health care providers. The Chicago Cancer Health Equity Collaborative (ChicagoCHEC) Research Fellows Program, a tri-institutional effort between the University of Illinois at Chicago (UIC), Northeastern Illinois University (NEIU), and Northwestern University (NU), provides a holistic, 8-week summer research fellowship that facilitates self-reflection, professional development, and exposes and guides the novice undergraduate and postbaccalaureate student toward a health care career inclusive of research and scientific discovery.
Objectives:
The number of underrepresented students achieving health care careers is minimal. We outline curriculum development, innovation, lessons learned, and selected outcomes from the first three cohorts of the ChicagoCHEC Research Fellows program.
Methods:
A tri-institutional, collaborative curricular team was formed consisting of research faculty and staff at NEIU, UIC and NU. Once accepted, fellows experience a cohort model curriculum with particular emphasis to mindful inclusion of nontraditional students. The ChicagoCHEC Research Fellows Program uses evidence-based mentorship models, group reflection, and extensive program evaluation to continuously improve its program model.
Conclusions:
The 48 fellow alumni from the first 3 years reported high satisfaction with the program and will continued to be tracked for academic success. The ChicagoCHEC Research Fellows program will continue to provide academic and professional tools, sponsorship, and mentorship opportunities to underrepresented students as they progress toward health care careers. A program such as the ChicagoCHEC Fellows Program can serve as a useful model for increasing the number of minority researchers in health care careers.
Keywords: Pipeline program, health equity, partnership, health care career, underrepresented students
The Excellence Gap is defined as the “differences between subgroups of students performing at the highest level of achievement.”1 Inequity in education is pervasive across all academic levels as it pertains to the underrepresented minority student. The foundation for career pipeline inequity begins at the elementary school level. For example, public schools have been cited as overlooking and underestimating African American and Hispanic students in terms of their ability to demonstrate rigor, with African American third graders one-half as likely as White students to be included in gifted programs.2,3 Such low representation then fuels additional disparities in educational achievement at the middle and high school levels, and further exacerbates high rates of attrition for minority students in the postsecondary, graduate, and postgraduate studies. In a 2018 report released by the National Science Foundation, African Americans earned only 6.6% of all doctoral degrees, approximately one-half of their proportion of the U.S. population.4
In addition to the widening excellence gap, there is also inequity as it pertains to the representation of minority students in health care fields. Health care career pipeline programming are one potential solution; however, despite the efforts of existing pipeline programs, minority students remain underrepresented in health care professions.5–7 Firstgeneration students who reside in poverty and violenceplagued neighborhoods often face tremendous challenges, both in their neighborhood and in the classroom. While striving to achieve academic and career success they have to cope with socioemotional, economic, and familial stressors.8 Although it is important to acknowledge the complexity of stressors that accompany students residing in volatile environments, it is equally crucial to ensure that underrepresented students are provided the same opportunities as their nonminority peers to advance in fields of choice. A 2015 report released by the Association of American Medical Colleges addressing the representation of African American men in medical school reiterates that high school juniors in a 2007 study also listed limited knowledge of career pathways and poor access to African American role models as barriers to pursuing medical careers.9,10 Research teams that spearhead pipeline programming targeting underrepresented students must take into account the decades of educational inequality that applicants to their programs might have encountered. Thoughtful programming that focuses on leveraging underrepresented student stressors as strengths instead of deficits, can contribute to building resilience and self-efficacy as it relates to a successful career trajectory. In addition, the design of such programs should account for building social support and professional resilience, and use team science approaches in which students are part of a group and not just in a traditional laboratory experience.
Indeed, peer support is recognized as an important strategy to encourage minority students not only to excel in their academic endeavors but also to persist in their chosen career track.6 This and other best practices, for example, in admissions policy and institutional culture, have been shaped and further refined to foster diversity in the nation’s health care pipeline, in recognition of the importance of a diverse health care pipeline to realization of the goal of reducing health disparities in minority and other underrepresented populations.6, 11
CHICAGOCHEC RESEARCH FELLOWS PROGRAM
The National Cancer Institute’s (NCI) Comprehensive Partnership to Advance Cancer Health Equity program (PACHE) has positioned NCI-designated Cancer Centers and institutions that serve underrepresented minorities to form partnerships that work to increase minority representation in cancer research careers. The ChicagoCHEC, a PACHE partnership between the Robert H. Lurie Comprehensive Cancer Center of NU, NEIU, and the UIC, started the ChicagoCHEC Research Fellows Program in 2016. The ChicagoCHEC Research Fellows program is a comprehensive, paid, 8-week summer learning experience and pipeline program for undergraduate and postbaccalaureate students that aims to support underrepresented students’ aspirations to become cancer researchers and medical professionals. The program seeks to enhance, academic, research, and professional skills.
This article outlines the unique curriculum, program design elements, lessons learned, and selected outcomes from the first three years of the ChicagoCHEC Research Fellows Program. Particular emphasis will be placed on the program’s design, intentional mission to expose fellows to a variety of health care careers, and innovation in the program’s one cohort model.
METHODS
Program Development and Student Recruitment
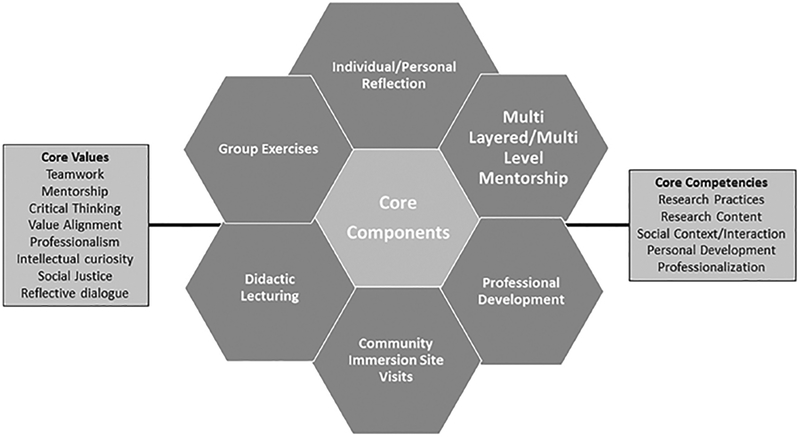
The ChicagoCHEC Research Fellows Program was designed to leverage the strengths of NU’s research community and rigor, UIC’s community engagement and pipeline programming, and NEIU’s strong foundation in education and access to diverse student populations. ChicagoCHEC’s program includes 1) the opportunity for students to engage in reflective dialogue and examine health inequities faced by their communities, 2) the leveraging of institutional resources to implement creative and didactic transdisciplinary lecturing, 3) encouraging participation of minority faculty and staff in multilayered/multilevel mentorship and sponsorship and near peer mentorship, 4) partnering with existing institutional programs, thus creating an even more expansive network for the fellows, and 5) community immersion site visits to help ensure students are able to envision successful health care careers that move beyond a clinical setting and into the field. A tri-institutional program planning team consisting of research faculty and staff was formed across institutional sites to collaboratively develop objectives, curricular elements, and components for the program in line with the program’s core values and competencies (Figure 1).
Figure 1.
ChicagoCHEC Research Fellows Program Elements
In an effort to remain consistent in targeting underrepresented undergraduate students, eligibility criteria for the program were specified and program spots were opened for NU, UIC, NEIU, and local community college students, with strong targeting of the Chicago community colleges. Emphasis was placed on moving students into successful and impactful health care careers, but also in moving students from a 2-year to a 4-year institution in the case of community college students. Eligibility criteria for the program specifies that students be a 1) rising sophomore, junior, or senior, at NEIU, UIC, or NU, or be enrolled at least half-time at one of the city colleges of Chicago or one of the community/junior colleges in the Chicago metropolitan area, or be a postbaccalaureate student within 2 years of graduation from their undergraduate institution. Students must also intend to apply to graduate or professional school. Community college students must intend to apply to a 4-year college and postbaccalaureate. Recruitment information was disseminated to a plethora of institutional and Chicago community partners, online job and internship boards at participating institutions, as well as the ChicagoCHEC website and social media. Staff attended on the ground campus recruitment via job fairs, and conducted recruitment application technical assistance workshops for participating institutions. To ensure individuals were well equipped for the application process, technical assistance application webinars were also developed and circulated to all program applicants.
Each student application was reviewed by at least one team member from each institution and a community partner, and were subsequently discussed by the entire review committee. Student finalists were invited for panel interviews and were required to participate in a 2-hour interview preparation workshop. To create a near-peer mentorship model and provide additional professional development, the committee also identified three ChicagoCHEC senior research fellows, one from each institution, to serve in a leadership role. In cohort 1, this role was filled by high-performing students who had just graduated from NU, NEIU, or UIC. In cohorts 2 and 3, this role was filled by fellows from the previous cohort. Before the program, accepted fellows are also required to complete pre-fellowship professional development modules via a free Massive Open Online Course entitled “Career 911: Your Future Job in Medicine and Healthcare.” This course was developed by Northwestern faculty and staff, and is geared toward preparing professionals that are interested in transitioning into health care fields. Curriculum from this online course is integrated in research fellows program professional development curriculum throughout the summer.
Evaluation and Tracking
With each cohort, data are collected at the time of application submission. Accepted fellows participate in pre–post program surveys that gauge confidence, interest, and noncognitive skills such as resiliency and leadership. Interim program qualitative interviews serve as an indicator for real-time program improvement efforts and have enabled program leaders to make quick, simple, and relatively burden-free changes to program structure and curriculum in real time. Fellows also complete speaker evaluations and are tracked after the program to ensure reporting of academic strides. ChicagoCHEC evaluators ensure that metrics are tracked to continually improve programming for the maximum benefit of students.
One Cohort Model
In contrast with many other health care career science, technology, engineering, and math (STEM) pipeline programs, where students individually progress through the program paired with one mentor, and are placed in a basic science research laboratory, ChicagoCHEC Research fellows advance through the summer as one cohort with exposure to a wide array of transdisciplinary researchers. This model was implemented purposefully to expose students to a variety of health care career options, and to facilitate and support the beginning of mentor relationships, social, and professional network development between fellows and program lecturers and leaders. This model also includes programming at all three academic sites, enabling students to get a well-versed array of academic exposures. This seemed to be a particularly enjoyed element by the community college students since many aim for 4-year acceptance at NEIU, NU, or UIC.
To continue fostering the one cohort model, students spend a full day in team building exercises and trust workshop dynamics facilitated by the program’s partnership with NEIU’s Center for College Access and Success. They are also assigned to smaller groups of four (with balanced representation from each institution or community college) throughout the summer to work on final projects, which included identifying a health inequity of choice and synthesizing information garnered from the summer experience to propose a hypothetical health intervention. Last, fellows are also given the opportunity to engage in mentor–mentee near peer relationships with the Lurie Children’s Hospital-Chase Foundation Chase Your Dreams high school program, in which local minority high school students from Chicago public high schools are introduced to health care careers. Weekly, the fellows presented information pertaining to college readiness, developing personal story, accessing valuable campus resources, financial planning, well-being, and health care career options in highly interactive workshops. Research fellows organically planned workshops that included expeditionary learning models, theater, and storytelling techniques. Facilitation of these workshops allowed fellows to enhance imperative and inherent leadership skills and nurtured the beginning of sustaining mentoring over time.
Inclusion of Nontraditional Students
In contrast with other STEM pipeline programs that initially focus on laboratory placements and wet laboratory activities, the research fellows program accepts students from various research backgrounds and seeks to prepare students for their first introduction to legitimate research laboratory placement post program. Approximately one-half of the fellows reported never having a research experience before gaining acceptance into the ChicagoCHEC Research Fellows program. As a result of students beginning the program at various academic levels and socioemotional strengths, it was considered valuable to expose the entire cohort to the same materials, activities, and curricular elements. Before the program began, antibias training occurred for all applicant interviewers. During the program, faculty and staff were careful not to assign students from the same institution to the same group, and differences in academic abilities were valued as an asset and not a deficit.
Innovative Programming
Through its Learning with Leaders series, the ChicagoCHEC Research Fellows program exposes fellows to advanced perspectives from more than 50 leaders in research, community organizations, clinical practice, and advocacy. These leaders meet with the research fellows to discuss their professional development journeys, current work and methodologies, relationship with cancer inequity and other health disparities, and provide insights into opportunities for the Research Fellows. ChicagoCHEC’s Journal Club has enabled fellows to share personal stories and reflect on times in their lives when they personally felt or have witnessed discrimination. Faculty and staff that specialize in social identity, social justice, health outcomes, and microaggression research are invited in to facilitate lectures that move these discussions forward. The journal club is complimented by required readings and reflective work into health equity and social justice, and local-level history into race, health, and medicine. Fellows work through a series of excerpts from texts such as Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to Present, The Death Gap: How Inequality Kills, and The Immortal Life of Henrietta Lacks. The program’s community site visits serve as a glimpse into the tangible life application of the knowledge and skills taught to the Research Fellows in guest lecture given by leading scholars and cancer researchers, health professionals, institutional leadership and community leaders across Chicago. Site visit hosts share the challenges to achieving cancer health equity in their communities owing to socioeconomic barriers such as violence, lack of education, lack of access to quality care, and lack of insurance. Last, fellows also have Development Fridays, in which time is dedicated to personal and professional development, and the building of crucial life skills. Past cohorts have had lectures on stress reduction, navigating the medical/graduate school application process, scientific writing, exposure to the life of a physician/researcher, presentation etiquette and scientific public speaking, and on networking and being a mentee.
RESULTS AND DISCUSSION
Two hundred forty individuals have applied to the ChicagoCHEC Research Fellows program to date, with 48 students having been an active fellow (including senior fellows). We report findings solely from cohorts 2 and 3 in this report. More than one-half of the fellows identify as a minority and a large majority (69% in cohort 2; 59% cohort 3) are first-generation college students (Table 1). Within the past year, we have paid close attention to improving recruitment of certain underrepresented minority groups, such as African American males, while also not jeopardizing the standards and integrity of our recruitment and acceptance process.
Table 1.
Characteristics of ChicagoCHEC Research Fellows Cohorts 2 and 3
| Cohort 2 (2017), n (%) | Cohort 3 (2018), n (%) | |
|---|---|---|
| Total, N (%) | 16(100) | 17(100) |
| Female sex | 11 (69) | 13(76) |
| Age, average (range) | 23.3 (19–33) | 24.9(19–48) |
| Race/ethnicity | ||
| Hispanic | 7(44) | 5(29) |
| Asian | 2(13) | 3(18) |
| NH African American/Black | 6(38) | 6 (35) |
| NH White | 1 (6) | 3(18) |
| Other | 0 | 5(29) |
| Parent’s highest level of education | ||
| High school | 4(25) | 5(29) |
| Associates degree | 4(25) | 4(24) |
| Some college | 3(19) | 1(6) |
| College (4-year) | 5(31) | 5(29) |
| Graduate/ID/PhD/MD | 0 | 2(12) |
| Has done research before | 8(50) | 11(65) |
| Has a mentor | 13(81) | 8(47) |
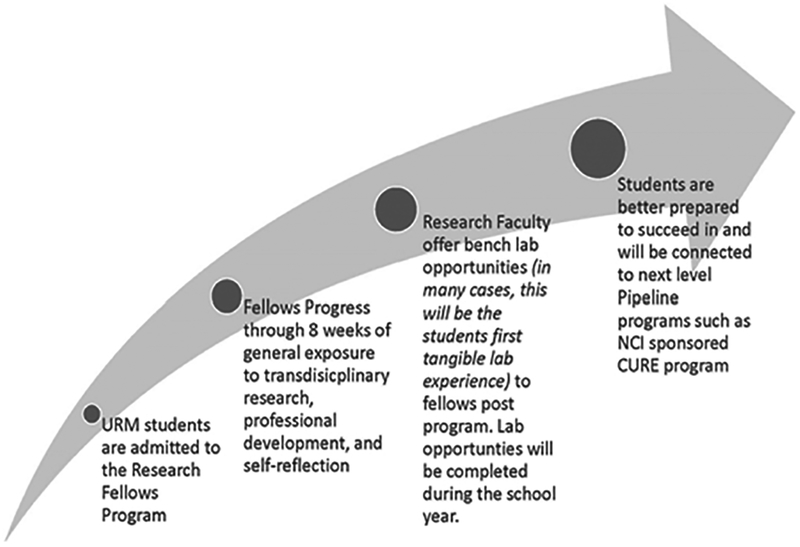
The program has noted some challenges as it pertains to the one cohort model. Although most students deeply value the group experience, some students have expressed frustration concerning the lack of consistent individual attention the program offers or the lack of traditional laboratory experiences. One fellow stated that they “expected more technical skills to be taught,” and another acknowledged that “different interests are hard to combine.” As we select and begin our fourth cohort, ChicagoCHEC’s one cohort model will be enhanced to include a much deeper mentoring component and postprogram laboratory immersion opportunities. Building on our current mentorship model, we are in the process of developing a multilayered, four-step approach for a ChicagoCHEC Mentoring Network (Figure 2), strongly inspired after the National Research Mentoring Network.12 This process will include the creation of a mentee profile, compiling engaging and transdisciplinary mentors from across our academic sites and community partners, and one-on-one meetings to facilitate meaningful mentor–mentee interactions, support, and guidance. In tandem, we will apply these practices to linking fellows with postprogram laboratory opportunities that will function as an extension of the program’s mentoring component. During the 8-week summer experience, fellows have the opportunity to tour various laboratories across partnering institutions. According to a study examining undergraduate characteristics that predicted persistence into graduate training, laboratory experiences that sparked the “curiosity to discover something new” was important for novice researchers.13–15 Owing to the overall mission of this program, the idea of laboratory experiences and placement remains a crucial component to our program. With the our enhanced mentor and placement model, we will equip students not only with the scientific knowledge to progress in the health care careers, but also with the skills to acquire their own professional experiences outside of the confines of the program and cohort.
Figure 2.
Proposed Design of Enhanced Post-Program Mentorship and Lab Placement Process
Research has found the importance of bridging trainees and community organizations in increasing educational excellence and increasing the number of minority researchers conducting health equity–focused research. This program will continue to serve as a catalyst between fellows and the many community organizations ChicagoCHEC works with on an annual basis. We believe this innovative component increases the understanding of cultural viewpoints, enhances the knowledge of fellows to better understand the neighborhoods and communities they work and play in, and increases knowledge of local-level health disparities. It also serves a mutually beneficial role in that community organizations are able to then work with fellows as volunteers, employees, and future health care leaders.
Overall, students have seemed to enjoy this program with high rates of satisfaction with the program (93% satisfied/highly satisfied in cohort 2; 100% in cohort 3) and with different program elements (Table 2). One fellow stated, “of all the programs I’ve ever done this one has been the most deliberate in introducing to people that could potentially take our careers to the next level,” and another fellow states, “this program has turned out to completely different than what I expected, I didn’t think ChicagoCHEC would turn into a family.” Students also show improvement in their confidence and increased interest in pursuing health-related careers in health equity and research (Table 3), and report changes in fellow attitudes toward their career trajectories. One fellow noted that ChicagoCHEC helped to “broaden [my] view of how to accomplish my goals in the health care field,” and another remarked on the dynamic nature our program can play by stating, that “many of [us] changed our goals in response to the things we learned about inequity and health.”
Table 2.
ChicagoCHEC Fellows’ Satisfaction with Different Program Componentsa
| Cohort 2 (2017), n (%) | Cohort 3 (2018), n (%) | |
|---|---|---|
| Program overall | ||
| Very dissatisfied/somewhat dissatisfied | 1(7) | 0 |
| No opinion | 0 | 0 |
| Satisfied/very satisfied | 14 (93) | 16(100) |
| Lectures | ||
| Very dissatisfied/somewhat dissatisfied | 4(27) | 0 |
| No opinion | 0 | 0 |
| Satisfied/very satisfied | 11(73) | 16(100) |
| Learning with leaders | ||
| Very dissatisfied/somewhat dissatisfied | 3(20) | 0 |
| No opinion | 1(7) | 0 |
| Satisfied/very satisfied | 11(73) | 16(100) |
| Near peer mentorship via Gear Up | ||
| Very dissatisfied/somewhat dissatisfied | 3(20) | 0 |
| No opinion | 1(7) | 0 |
| Satisfied/very satisfied | 11(73) | 16(100) |
| Journal club | ||
| Very dissatisfied/somewhat dissatisfied | 1(7) | 0 |
| No opinion | 3(20) | 3(19) |
| Satisfied/very satisfied | 11(73) | 13 (81) |
| Site visits | ||
| Very dissatisfied/somewhat dissatisfied | 2(13) | 0 |
| No opinion | 0 | 0 |
| Satisfied/very satisfied | 13 (87) | 16(100) |
| Project group work and final project | ||
| Very dissatisfied/somewhat dissatisfied | 4(27) | 0 |
| No opinion | 0 | 2(13) |
| Satisfied/very satisfied | 11(73) | 14 (88) |
Total cohort 2, N = 16; total cohort 3, N = 17. In both cohorts, one student was unable to complete the postprogram evaluation survey. Senior fellows do not complete these surveys.
Table 3.
ChicagoCHEC Fellows Self-report Fellow Interest and Confidence
| Cohort 2 (2017), n (%) | Cohort 3 (2018), n (%) | |||
|---|---|---|---|---|
| Pre (n = 16) | Post (n = 15) | Pre (n = 17) | Post (n = 16) | |
| I would enjoy a career that involves research. | ||||
| Strongly disagree/disagree | 1 (6) | 1 (7) | 0 | 0 |
| Neutral | 7 (44) | 0 | 2 (12) | 1 (6) |
| Agree/strongly agree | 8 (50) | 14 (93) | 15 (88) | 15 (94) |
| I feel confident in my ability to explore a career in research. | ||||
| Strongly disagree/disagree | 1 (6) | 0 | 1 (6) | 0 |
| Neutral | 6 (38) | 4 (27) | 5 (29) | 3 (19) |
| Agree/strongly agree | 9 (63) | 11 (73) | 11 (65) | 13 (81) |
| I would like to incorporate research into my future career. | ||||
| Strongly disagree/disagree | 1 (6) | 1 (7) | 0 | 0 |
| Neutral | 3 (19) | 1 (7) | 3 (18) | 1 (6) |
| Agree/strongly agree | 12 (75) | 13 (87) | 14 (82) | 15 (94) |
| How interested are you in pursuing a health-related career focused on reducing health disparities? | ||||
| Very uninterested/somewhat uninterested | 0 | 0 | 2 (12) | 0 |
| Neutral | 0 | 1 (7) | 1 (6) | 2 (13) |
| Somewhat interested/very interested | 16 (100) | 14 (93) | 14 (82) | 14 (88) |
| How interested are you in pursuing a research career focused on reducing health disparities? | ||||
| Very uninterested/somewhat uninterested | 0 | 0 | 2 (12) | 0 |
| Neutral | 2 (12) | 0 | 1 (6) | 0 |
| Somewhat interested/very interested | 14 (88) | 15 (100) | 14 (82) | 16 (100) |
| How confident are you in your ability to pursue a research career focused on reducing cancer disparities? | ||||
| Very unconfident/somewhat unconfident | 1 (6) | 0 | 2 (12) | 0 |
| Neutral | 4 (25) | 2 (13) | 2 (12) | 3 (19) |
| Somewhat/very confident | 11 (69) | 13 (87) | 13 (76) | 13 (81) |
Although the assessment of program impact on the trajectory of fellows, particularly in the beginning stages of a largescale program, is difficult, we will continue to place emphasis on evaluation and tracking and how to enhance our efforts in this area. An innovative feature to our annual tracking has been an alumni event that serves a dual purpose as a tracking touch point for all cohorts. Of 31 students in these first two cohorts, 50% of community college students have transitioned to 4-year universities, three students have transitioned to medical school, 13% of students have transitioned from 4-year universities to graduate-level training programs in health care, 26% of students have presented scholarly work after the fellowship, and 13% of students have obtained employment/internship opportunities in ChicagoCHEC affiliated projects/laboratories (Table 4). An emphasis in the ChicagoCHEC curriculum on networking with peers, mentors, and other role models is intended to encourage the trainees to forge lasting ties and thus build their network from the ChicagoCHEC experience onward. Indeed, based on our tracking, we have found that many of the trainees keep in contact with each other and with faculty who participate in the program and understand the importance of lifelong networking practices. They understand that adherence to networking fosters greater resilience and determination to stay the course in their career pipeline goals, even when faced with new barriers, whether personal or institutional.
Table 4.
Career and Educational Tracking of ChicagoCHEC Research Fellows from Cohorts 1 and 2
| Significant Transition Points in Education/Careers of ChicagoCHEC Fellowsa | Fellows Specific (N = 31), n |
|---|---|
| Transitioned from community college to 4-year college | 4 |
| Transitioned from 4-year college to medical school | 3 |
| Transitioned from 4-year college to graduate level program or other training in health care | 4 |
| Presented scholarly work after the fellowship | 8 |
| Obtained employment/internship in a ChicagoCHEC-affiliated project/laboratory | 4 |
Students listed above are not mutually exclusive. Includes tracking from cohorts 1 and 2. Tracking for cohort 3 has not started at the time of the writing of this article.
CONCLUSIONS
Leadership of the ChicagoCHEC Research Fellows Program recognizes that, although it is too early to determine whether or not the program’s current structure and curricular elements contribute to decreasing the overall excellence gap, the team is fundamentally committed to enhancing an experience that reaches beyond surface preparation of the underrepresented student for a health care career and places emphasis on the fundamental barriers underrepresented students face. Acknowledging previous personal and academic setbacks, while also allowing the underrepresented student space to reflect and journal about past struggles and victories allows the student to begin to garner needed elements of resilience and grit that will serve them immensely well as they progress through careers of choice.
ACKNOWLEDGMENTS
The authors thank our NCI Program Director Nelson Aguila, DVM, and NCI Deputy Director Mary Ann Van Duyn, PhD. We would like to acknowledge the exceptional ChicagoCHEC Research Fellows Program alumni. They have provided insight, valuable feedback, and immense integrity to this program. They will continue to guide the enhancement and success of this program. We thank the programs that have interacted with and ultimately impacted the ChicagoCHEC Fellows Program including Northwestern’s Lurie Children’s Hospital-Chase Foundation Chase Your Dreams, UIC’s ResearcHStart and GUIDE programs (P20CA202908). Last, we thank our community partners who have provided invaluable experiences in the field, and faculty across our three institutions who have served as ongoing guides to our fellows by providing advice, skill building activities, and connections. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This work was supported by the National Cancer Institute (U54CA202995, U54CA202997, U54CA203000).
REFERENCES
- 1.Plucker J, Burroughs N, Song R. Mind the (other) gap! The growing excellence gap in K–12 education [cited 2010. February 4]. Available from: https://eric.ed.gov/?id=ED531840 [Google Scholar]
- 2.Grissom JA, Redding C. Discretion and disproportionality: Explaining the underrepresentation of high-achieving students of color in gifted programs. AERA Open. 2016;2(1): 233285841562217. [Google Scholar]
- 3.Dynarski S. (2016. April 08). Why talented Black and Hispanic students can go undiscovered. Available from: www.nytimes.com/2016/04/10/upshot/why-talented-black-and-hispanic-students-can-go-undiscovered.html [Google Scholar]
- 4.National Science Foundation, National Center for Science and Engineering Statistics. Doctorate recipients from U.S. universities: 2016 [updated 2018]. Special Report NSF; 18–304. Alexandria, VA: Available from: www.nsf.gov/statistics/2018/nsf18304/ [Google Scholar]
- 5.Resources Health and Administration Services. The Rationale for Diversity in the Health Professions: A Review of the Evidence. Rockville, MD: HRSA, U.S. DHHS; 2006. Available from: http//bhpr.hrsa.gov/healthworkforce/reports/diversityreviewevidence.pdf [Google Scholar]
- 6.Smedley BD, Butler AS, Bristow LR. In the Nation’s Compelling Interest: Ensuring Diversity in the Health-Care Workforce. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 7.Agency for Healthcare Research and Quality. National healthcare disparities report, 2013. Publ. no. 14–0006. Rockville, MD: AHRQ; 2013. Available from: www.ahrq.gov/sites/default/files/publications/files/2013nhdr.pdf [Google Scholar]
- 8.Dennis JM, Phinney JS, Chuateco LI. The role of motivation, parental support, and peer support in the academic success of ethnic minority first-generation college students. Journal of College Student Development. 2005;46(3):223–36. [Google Scholar]
- 9.The Association of American Medical Colleges (AAMC). Altering the course: Black males in medicine [updated 2015]. Washington, DC. Available from: https://members.aamc.org/eweb/upload/Altering%20the%20Course%20-%20Black%20Males%20in%20Medicine%20AAMC.pdf [Google Scholar]
- 10.Rao V, Flores G. Why aren’t there more African-American physicians? A qualitative study and exploratory inquiry of African-American students’ perspectives on careers in medicine. J Natl Med Assoc. 2007;99:986–93. [PMC free article] [PubMed] [Google Scholar]
- 11.Grumbach K, Mendoza R. Disparities in human resources: Addressing the lack of diversity in the health professions. Health Aff (Millwood). 2008;27:413–22. [DOI] [PubMed] [Google Scholar]
- 12.Sorkness CA, Pfund C, Ofili EO, et al. A new approach to mentoring for research careers: The National Research Mentoring Network. BMC Proc. 2017;11(Suppl. 12), 22nd ser., 171–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mcgee R, Keller JL. Identifying future scientists: Predicting persistence into research training. CBE—Life Sciences Education. 2007;6(4):316–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson JC, Jayadevappa R, Taylor L, et al. Extending the pipeline for minority physicians. Acad Med. 1998;73(3):237–44. [DOI] [PubMed] [Google Scholar]
- 15.Smith SG, Nsiah-Kumi PA, Jones PR, et al. Pipeline programs in the health professions, part 1: Preserving diversity and reducing health disparities. J Natl Med Assoc. 2009;101(9):836–51. [DOI] [PubMed] [Google Scholar]