Abstract
Although diabetes education plays an important role in self-management for people living with diabetes, male health “help-seeking” lags far behind women. These gender-related “help-seeking” disparities often result in males being less engaged in their health care, which subsequently leads to poorer health outcomes among males. In this cross-sectional study, we used data from the 2017 Health Information National Trends Survey (HINTS) to identify factors that may contribute to communication inequalities between males and females. A hierarchical {linear/logistic} regression model was used to examine factors associated with online health information seeking among males living with diabetes. The results suggest that education, income, age, identifying as Hispanic, being a smoker, using a device to track progress toward a health-related goal, and using device to seek health information were all related to eHealth sum scores. Future research should consider testing applications among various at-risk groups to determine if the technology itself is becoming a barrier to eHealth.
Keywords: men’s health, digital technology, internet, help-seeking, diabetes
Gender-related disparities in health have been an essential focus for researchers who investigate males, masculinities, and mental health. In the United States, South Africa, and England, male health help-seeking (hereafter referred to as “help-seeking”) lags far behind women’s (Addis & Mahalik, 2003; Wang et al., 2007), and this carries with it enormous personal, relational, physical, mental, and economic costs (World Health Organization [WHO], 2016). Illustrating these costs, males are more likely than females to terminate therapy (e.g., patient counseling, physical therapy, prescription adherence) early and generally have negative attitudes toward help-seeking (Cottone et al., 2002; Doherty & Kartalova-O’Doherty, 2010; Nam et al., 2010). This hesitancy toward help-seeking persists despite important public health concerns related to mental health among males. For instance, males commit suicide more often than women (Oquendo et al., 2001) and experience higher levels of alcohol use and abuse (Karlamangla et al., 2006), stress (Reckelhoff, 2001), and sexual dysfunction (Laumann et al., 2005), all of which are related to mental health outcomes.
In the past decade, empowering patients to become proactive participants in their health care has become a priority of health-care providers in the United States (Kontos et al., 2014). This involves being able to make knowledgeable decisions regarding one’s illnesses, treatments, and health behaviors (Salmon & Hall, 2004). In company with this movement, information technology has continued to emerge with the advancement of highly interactive websites and applications creating an excess of opportunities for informational and communicative needs to be fulfilled through the internet (Kontos et al., 2014). According to 2019 Pew Research Center data, 90% of males in the United States use the internet followed by 89% of females (Pew, 2019). In the year 2018, approximately 92% of urban residents are internet users, 90% resided in suburban communities, and 78% resided in rural communities (Pew, 2019).
With the coaction of these two momentums, it is therefore unsurprising that considerable numbers of individuals residing in the United States are turning to the internet and mobile health (mHealth) to search for health information (Andreassen et al., 2007; Fox & Jones, 2009; Kontos et al., 2014).To date, the mass of related research examining the individual characteristics that correlate with online health information seeking has focused on sociodemographic factors. According to this research, being female (Carpenter et al., 2011; Hallyburton & Evarts, 2014; Powell et al., 2011; Stern et al., 2012; Thackeray et al., 2013), having a higher income and education (Cotten & Gupta, 2004; Kontos et al., 2014; Shahab et al., 2014), being married or in a de facto relationship (Hallyburton & Evarts, 2014), being of younger age (Andreassen et al., 2007; Bansil et al., 2006; Kontos et al., 2014), living outside of an urban area (Ruggiero et al., 2011), and having access to the internet both at work and home (Atkinson et al., 2009) are associated with online health information seeking.
Associations between some behavioral and health characteristics with online help-seeking have also been investigated, though to a lesser extent. Health information seeking behavior is referred to as an understanding how and why individuals who reside in the United States acquire health information, where they go to retrieve such information, what particular types of information they prefer, and how the health information sought is used (Lambert & Loiselle, 2007). Conversely, help-seeking behavior is referred to as the act of looking for or going in search of an alleviation or remedy to accomplish a need (Cornally & McCarthy, 2011). The existing evidence suggests that health status (hemoglobin A1c [HbA1c], body mass index, dietary behaviors, level of management education, and hypertension) is an important correlate of online health information seeking (Houston & Allison, 2002), as is online behavior, such as utilizing social media and social networking sites (Feng & Xie, 2015). Health-related behaviors, however, such as physical activity, diet, alcohol consumption, and smoking, have not consistently been reported to be associated with online health information seeking behavior (Shahab et al., 2014). While all people with chronic lifestyle conditions including diabetes are challenged by the long-term demands of managing their disease, there is an insufficient amount of male-centered research that centers on utilizing digital technology for chronic disease management. Such efforts could identify the unique social and cultural realities that either facilitate or impede the ability among males to seek or look for health information, including the use of the internet and devices that allow access to the internet.
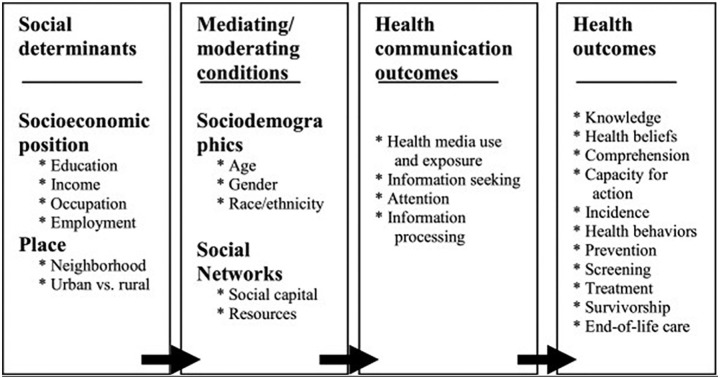
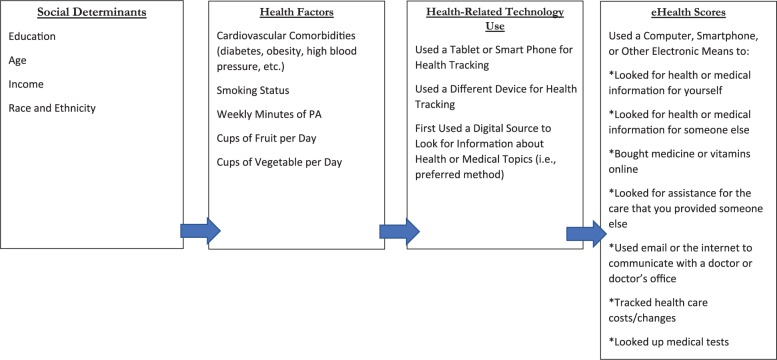
According to the model developed by Viswanath et al. (2007), structural influence model (Figure 1) posits that health communication inequality can be seen in terms of inequalities in health information seeking behavior, use, and/or exposure to health-related media content, motivation for and/or attention to health-related information, and information processing capacities. For the present study, we have developed a conceptual model (Figure 2) that illustrates where diabetic males and nondiabetic males search electronically for health-related information. Therefore, due to the potential impact digital technologies and mHealth could have on health education, social support, and self-management in the promotion of health among males living with chronic lifestyle conditions including diabetes, the present study investigates where male participants seek or look for health-related information. Additionally, the study will also investigate what predicts their use of digital health information and how they compare to those who are living without diabetes.
Figure 1.
Structural influence model.
Source: Viswanath et al. (2007).
Figure 2.
Conceptual model illustrating factors related to men’s eHealth scores.
Methods
Data Source
This cross-sectional study used data from the 2017 Health Information National Trends Survey (HINTS), a population-based survey that has been administered by the National Cancer Institute since 2003. Specifically, we used the data from the first data collection cycle of the fifth HINTS iteration, hereafter referred to as HINTS 5, Cycle 1 (2017). Data were collected from January to May 2017 via self-administered surveys that were mailed to a random stratified sample of addresses located in the United States. The Next Birthday Method was used to select one adult from each household sampled. Complete data were collected from 97% of survey respondents (n = 3,191/3,285). A survey was considered to be complete if at least 80% of the required questions were answered in the first two sections—that is, (a) Looking for Health Information and (b) Using the Internet to Find Information.
Participants
We included survey respondents who self-identified as “male” in response to the following question: Are you male or female? No other inclusion or exclusion criteria were used to derive our analytic subsample of 1,254 males, of which 865 males had complete data for all of the variables that were used in our study. The majority (n = 1,156, 93.8%) of participants reported being heterosexual, non-Hispanic White (n = 782, 66.7%), aged between 50 and 74 years (n = 722, 58.3%), with at least some college degree or more (n = 957, 76.8%). Most participants (n = 960, 77.2%) reported consuming less than two to three cups of vegetables per day and 1,057 (85.2%) said they had less than two cups of daily fruit intake; thereby failing to meet the federal fruit and vegetable recommendation guidelines for men. Over half the participants (n = 671, 54%) reportedly failed to meet the recommended, weekly 150 min of moderate physical activity guidelines for adults. A very small proportion (n = 167, 13.3%) said they were current smokers.
Almost half the participants (n = 607, 49%) reported being hypertensive. Based on participant responses, reportedly 430 (37.1%) were obese, 153 (12.4%) had a heart condition and 298 (24.2%) were diabetic. Additionally, over half (n = 613, 49%) of our sample reported using digital sources to seek health information. Over one third (n = 351, 33.9%) said they used tablets and smartphones to track progress on a health-related goal and 466 (37.3%) reported using devices, other than tablets and smartphones to track health. See Table 1 for all sample characteristics.
Table 1.
Sample Characteristics.
| Characteristic | Total N = 1,254 N (%) |
eHealth technology users N = 1,002 N (%) |
eHealth technology nonusers N = 195 N (%) |
χ2 test p Value |
|---|---|---|---|---|
| Socio-demographics | ||||
| Age | ||||
| 18–34 | 116 (9.4%) | 107 (10.8%) | 5 (2.8%) | .00 |
| 35–49 | 259 (20.9%) | 231 (23.2%) | 21 (11.2%) | |
| 50–64 | 431 (34.8%) | 343 (34.5%) | 68 (36.3%) | |
| 65–74 | 291 (23.5%) | 226 (22.7%) | 50 (26.7%) | |
| 75+ | 141 (11.4%) | 88 (8.8%) | 43 (23.0%) | |
| Race/ethnicity | ||||
| Non-Hispanic White | 782 (66.7%) | 657 (68.5%) | 102 (62.6%) | .00 |
| Non-Hispanic Black | 114 (9.7%) | 80 (8.4%) | 24 (14.7%) | |
| Other | 276 (23.6%) | 224 (23.1%) | 37 (22.7%) | |
| Annual household income | ||||
| $0–$9,999 | 62 (5.0%) | 31 (3.1%) | 25 (12.9%) | .00 |
| $10,000–$14,999 | 59 (4.7%) | 33 (3.3%) | 22 (11.4%) | |
| $15,000–$19,999 | 44 (3.5%) | 31 (3.1%) | 12 (6.2%) | |
| $20,000–$34,999 | 160 (12.8%) | 103 (10.3%) | 45 (23.3%) | |
| $35,000–$49,999 | 157 (12.6%) | 125 (12.5%) | 23 (11.9%) | |
| $50,000–$74,999 | 240 (19.2%) | 200 (20.0%) | 29 (15.0%) | |
| $75,000–$99,999 | 179 (14.3%) | 151 (15.1%) | 22 (11.4%) | |
| $100,000–$199,999 | 256 (20.5%) | 237 (23.7%) | 12 (6.3%) | |
| $200,000 or more | 93 (7.4%) | 89 (8.9%) | 3 (1.6%) | |
| Marital status | ||||
| Married | 758 (60.9%) | 645 (64.9%) | 84 (43.3%) | .00 |
| Living as married | 42 (3.3%) | 35 (3.5%) | 6 (3.1%) | |
| Divorced | 154 (12.4%) | 108 (10.9%) | 35 (18.1%) | |
| Widowed | 56 (4.5%) | 34 (3.4%) | 20 (10.3%) | |
| Separated | 33 (2.7%) | 22 (2.2%) | 9 (4.6%) | |
| Single | 202 (16.2%) | 150 (15.1%) | 40 (20.6%) | |
| Sexual orientation | ||||
| Heterosexual or straight | 1,156 (93.8%) | 929 (93.6%) | 173 (94.0%) | .29 |
| Homosexual or gay or lesbian | 44 (3.5%) | 38 (3.8%) | 6 (3.3%) | |
| Bisexual | 18 (1.5%) | 17 (1.7%) | 1 (0.5%) | |
| Other | 15 (1.2%) | 9 (0.9%) | 4 (2.2%) | |
| Education | ||||
| Less than high school | 74 (5.93%) | 40 (4.0%) | 28 (14.5%) | .00 |
| High school graduate | 215 (17.2%) | 130 (13.1%) | 71 (36.8%) | |
| Some college | 382 (30.6%) | 311 (31.2%) | 54 (28.0%) | |
| Bachelor’s degree | 320 (25.7%) | 286 (28.7%) | 24 (12.4%) | |
| Postbaccalaureate degree | 255 (20.5%) | 229 (23.0%) | 16 (8.3%) | |
| Employment status | ||||
| Currently employed | 662 (91.9%) | 571 (93.3%) | 63 (79.8%) | .00 |
| Unemployed | 59 (8.1%) | 41 (6.7%) | 16 (20.2%) | |
| Cardiovascular-related health behaviors | ||||
| Vegetable consumption | ||||
| None | 67 (5.4%) | 43 (4.3%) | 18 (9.3%) | .024 |
| 1/2 cup or less | 188 (15.1%) | 147 (14.9%) | 31 (16.0%) | |
| 1/2 to 1 cup | 312 (25.1%) | 249 (25.0%) | 50 (25.8%) | |
| 1 to 2 cups | 393 (31.6%) | 321 (32.3%) | 53 (27.3%) | |
| 2 to 3 cups | 192 (15.4%) | 161 (16.2%) | 26 (13.4%) | |
| 3 to 4 cups | 64 (5.1%) | 55 (5.5%) | 8 (4.1%) | |
| 4 or more cups | 28 (2.3%) | 18 (1.8%) | 8 (4.1%) | |
| Fruit consumption | ||||
| None | 129 (10.4%) | 91 (9.2%) | 33 (17.0%) | .03 |
| 1/2 cup or less | 245 (19.7%) | 197 (20.0%) | 34 (17.5%) | |
| 1/2 to 1 cup | 281 (22.7%) | 222 (22.4%) | 46 (23.7%) | |
| 1 to 2 cups | 402 (32.4%) | 334 (33.7%) | 50 (25.7%) | |
| 2 to 3 cups | 120 (9.7%) | 96 (9.7%) | 19 (9.8%) | |
| 3 to 4 cups | 38 (3.1%) | 31 (3.1%) | 7 (3.6%) | |
| 4 or more cups | 25 (2.0%) | 19 (1.9%) | 5 (2.7%) | |
| Smoking status | ||||
| Current smoker | 167 (13.3%) | 105 (10.5%) | 51 (26.1%) | .00 |
| Current nonsmoker | 1,087 (86.7%) | 897 (89.5%) | 144 (73.9%) | |
| Weekly minutes of moderate exercise | ||||
| <150 min (<2.5 h) | 671 (53.9%) | 474 (47.6%) | 117 (60.6%) | .03 |
| ≥150 min (≥2.5 h) | 574 (46.1%) | 521 (52.4%) | 76 (39.4%) | |
| Electronic health information seeking/tracking health via devices | ||||
| Using digital sources to seek health information | 641 (51.1%) | 613 (61.1%) | 11 (1.76%) | .00 |
| Not using digital sources to seek health information | 613 (48.9%) | 389 (38.9%) | 184 (94.4%) | |
| Using tablet/smartphone in tracking progress on a health-related goal | 351 (33.9%) | 333 (37.5%) | 10 (9.3%) | .00 |
| Not using tablet/smartphone in tracking progress on a health-related goal | 686 (66.1%) | 554 (62.5%) | 98 (90.7%) | |
| Using devices to track health (other than tablet/smartphone) | 466 (37.3%) | 426 (42.6%) | 26 (14.0%) | .00 |
| Not using devices to track health (other than tablet/smartphone) | 782 (62.7%) | 575 (57.4%) | 166 (86.0%) | |
| Chronic conditions | ||||
| Diabetic | 298 (24.2%) | 228 (22.80%) | 50 (25.64%) | .38 |
| Nondiabetic | 935 (75.8%) | 774 (77.20%) | 145 (74.36%) | |
| Obese (BMI ≥ 30.00) | 430 (37.10%) | 344 (36.95%) | 67 (38.0%) | .78 |
| Nonobese | 728 (62.9%) | 587 (63.05) | 109 (62.0%) | |
| Heart conditions | 153 (12.4%) | 119 (11.9%) | 26 (13.6%) | .53 |
| No heart conditions | 1,085 (87.6%) | 874 (88.1%) | 165 (86.4%) | |
| High blood pressure | 607 (49.0%) | 464 (46.9%) | 113 (58.6%) | .00 |
| Normal blood pressure | 631 (51.0%) | 526 (53.1%) | 80 (41.4%) | |
Note. BMI = body mass index.
Data Analysis
We analyzed the use of eHealth technologies in a sample of men using HINTS 5, Cycle 1 data. To assess variation in eHealth technology use, we regressed demographic variables (age, education, income, employment status, race, ethnicity), cardiovascular-related health behaviors (smoking, weekly exercise, consumption of fruits and vegetables) and comorbidities (whether someone indicated they had heart disease, diabetes, high blood pressure, or obesity), and technological device use (using a device to track progress toward a health-related goal and using a device to seek health-related information) onto an eHealth sum score, consistent of various ways a person can use technology to access health care. eHealth sum scores were calculated by combining the responses of seven items from the HINTS. Answers were in response to the stem, “In the past 12 months, have you used a computer, smartphone, or other electronic device as a means to:” and included items such as “bought medicine or vitamins online” and “used email or the internet to communicate with a doctor or doctor’s office.” See the eHealth Scores box in Figure 2 for all seven items summed to create the eHealth sum score.
SPSS version 24 (IBM, 2018) was used to perform all data analyses. Hierarchical linear regression analyses were conducted to determine the unique variance in eHealth scores explained by demographic variables alone, demographic variables + behavioral variables and comorbidities, and finally demographic variables + behavioral variables and comorbidities + device use variables.
Results
Pearson’s chi-square test was used to compare differences in the demographic, cardiovascular behaviors, chronic conditions, and electronic health information seeking/tracking variables between eHealth technology users (N = 1,002) and eHealth technology nonusers (N = 195). The p value of <.05 was considered statistically significant in all cases. Participants with an eHealth sum score of 1 or above were determined as eHealth users. Participants with an eHealth sum score of 0 were determined as eHealth nonusers.
Statistically significant differences between eHealth users and eHealth nonusers were observed in the majority of demographic variables, including age (p = .00), race/ethnicity (p = .00), annual household (p = .00), marital status (p = .00), education (p = .00), employment status (p = .00), fruit consumption (p = .03), vegetable consumption (p = .02), smoking status (.00), weekly minutes of moderate exercise (p = .03), using digital sources to seek health information (p = .00), using tablet/smartphone in tracking progress on a health-related goal (p = .00), using devices to track health (other than tablet/smartphone) (.00), and blood pressure (p = .00).
Differences were not statistically significant between eHealth users and eHealth nonusers regarding sexual orientation (p = .29), individuals with diabetes (p = .38), obesity (p = .78), and heart conditions (p = .53).
Hierarchical linear regression analyses suggest that education, income, age, identifying as Hispanic, being a smoker, using a device to track progress toward a health-related goal, and using device to seek health information were all related to eHealth sum scores (see Table 2 for complete regression models). Specifically, education (β = .133, t = 4.106, p < .001), income (β = .151, t = 4.327, p < .001), using a tablet or smartphone to track progress on a health-related goal (β = .126, t = 3.879, p < .001), using a device other than a tablet or smartphone to monitor/track health (β = .173, t = 5.507, p < .001), and using technology to seek health information (β = .227, t = 7.439, p < .001) were positively correlated to higher eHealth scores, while age (β = −.109, t = −2.986, p = .003), Hispanic ethnicity (β = −.103, t = −2.335, p = .020), and being a smoker (β = −.094, t = −3.507, p = .002) were related to lower eHealth sum scores.
Table 2.
Hierarchical Linear Regression Analysis Predicting eHealth Scores Among a Sample of Men (n = 865).
| Model 1 R2 = .167 |
Model 2 R2 = .190 |
Model 3 R2 = .293 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors | β | t | p | β | t | P | β | t | p |
| Education | .179 | 5.249 | <.001 | .177 | 5.516 | <.001 | .133 | 4.106 | <.001 |
| Age | −.177 | −4.912 | <.001 | −.210 | −5.637 | <.001 | −.109 | −2.986 | .003 |
| Income | .255 | 6.987 | <.001 | .221 | 5.910 | <.001 | .151 | 4.237 | <.001 |
| Employed | −.036 | −.959 | .338 | −.036 | −.959 | .338 | −.039 | −1.104 | .270 |
| Hispanic | −.095 | −2.016 | .044 | −.105 | −2.239 | .025 | −.103 | −2.335 | .020 |
| Non-Hispanic Black | −.053 | −1.231 | .219 | −.051 | −1.192 | .234 | −.059 | −1.490 | .136 |
| Non-Hispanic White | −.066 | −1.260 | .208 | −.069 | −1.317 | .188 | −.086 | −1.757 | .079 |
| Comorbidities | .075 | 2.211 | .027 | .013 | .411 | .681 | |||
| Current smoker | −.115 | −3.510 | <.001 | −.094 | −3.057 | .002 | |||
| Weekly minutes of PA | −.043 | −1.362 | .174 | −.027 | −.928 | .354 | |||
| Cups of fruit | −.005 | −.137 | .891 | −.002 | −.061 | .952 | |||
| Cups of vegetables | .051 | 1.411 | .159 | .029 | .848 | <.397 | |||
| Tablet or smartphone health tracking | .126 | 3.879 | <.001 | ||||||
| Other device health tracking | .173 | 5.507 | <.001 | ||||||
| Digital information seeking | .227 | 7.439 | <.001 | ||||||
Note. PA = physical activity.
When considering each level of the model, demographic variables alone explained 16.7% of the variance in eHealth scores, behavioral variables and comorbidities explained an additional 2.3% of the variance (R2 = .190), and device used added 10.3% to the variance explained (R2 = .293). Demographic variables held constant from model to model, suggesting a unique relationship between education, age, ethnicity, and income with eHealth scores. In the final model, seeking health information digitally was the strongest predictor of eHealth scores.
Discussion
In our study, most of the variance in eHealth technology use was explained by comorbidities and characteristics of the sample of participants. Our study’s findings underscore the importance of addressing communication equalities so that populations most affected by health disparities could increase use of eHealth technologies that could improve disease prevention and management (Carpenter et al. 2011; Fagan et al., 2004; Ophelia & Morey, 2007). More research efforts are needed to better discern which extent social determinants of health that also attribute to communication inequalities could be overcasting any effect chronic disease management. Similarly, more research is warranted to better understand eHealth technology use among healthy adults who may have less need compared to those who have been diagnosed with one or more chronic conditions. For example, one of the Healthy People 2020 diabetes objectives focuses on hypertension control among diabetics. Therefore should they choose to, men living with diabetes may perhaps turn to eHealth technology to monitor both blood glucose and blood pressure numbers, thereby creating a need for technology in a diseased population compared to that of a healthy population.
Our findings show that current smokers have lower eHealth use. This finding was unsurprising largely due to evidence suggesting smoking/tobacco-related disease burden is higher among low-income, underserved ethnic/racial minority populations (Do et al., 2018) who already face barriers to technology use (Cheatham et al., 2007). Thus, inadequate eHealth accessibility may worsen the existing disparity in smoking status (Naughton et al., 2014; Shahab et al., 2014). Further, the use of health monitoring/tracking devices, and seeking health information digitally, positively predicted eHealth use. Using health monitoring/tracking devices leads to better familiarity and comfort in utilizing technology for measuring health and fitness and also improving health behaviors (Alturki & Gay, 2016; Steinhubl et al., 2015; Williamson, 2015). For example, studies demonstrate the positive results of using web-based and mobile-based interventions for smoking cessation (Do et al., 2018; Nam et al., 2019; Naughton et al., 2014; Richardson et al., 2013). Overall, encouraging technology use for health promotion and intervention can effectively result in positive health outcomes.
Study Limitations
Although our cross-sectional study adds to the body of knowledge on men’s health, it is not without limitations. Our findings are based on self-reported data of the HINTS respondents. In the case of chronic disease status, we were not able to use medical chart data to confirm disease diagnosis or status. For example, we were not able to confirm diabetes diagnosis or assess how well diabetes was being managed (e.g., recent HbA1c result). There were also study limitations without outcome of interest because the inherent nature of the HINTS questions did not ask about specific topics for health information seeking or eHealth technology use. Further, while the sample size is large, HINTS data are largely represented by older, higher income, highly educated, and retired persons, which could directly influence use of digital devices. While we did control for this statistically, it is important that overgeneralizability of findings should be avoided. Future research could (a) focus on various groups less likely to use digital health resources (e.g., lower income) and (b) tailor survey questions to a specific health topic (e.g., diabetes) and related eHealth technology use (e.g., measuring blood glucose).
Implications for Future Research and Practice
According to Ball and Lillis (2001), advances in eHealth allow for people to become partners in their own health and redefines the patient/provider relationship. Because men are historically less likely to regularly see a physician or keep up with routine health care (Cheatham et al., 2007; Hammond et al., 2010), eHealth provides ways for men to be more active in their health, and perhaps reduce the number of preventable injuries, diseases, and deaths in this population (Jadad & Meryn, 2013; Ophelia & Morey, 2007). However, our study revealed there are subgroups of the male population that do not engage in eHealth, namely those that already face increased health disparities (e.g., lower education, lower income, ethnic minorities). Thus, research further investigating these differences in eHealth use is warranted, particularly if eHealth could potentially eliminate or reduce some health disparities (e.g., increased access to providers, more cost-effective health care).
The promotion of eHealth can happen in community settings, but also clinical settings, where persons less likely to utilize these resources can be educated and trained. Future research could experimentally test the effects of educating patients on eHealth use when in clinical settings and the impact of community outreach involving the promotion of eHealth. Our results also suggest that people already using technological devices (tablets, smartphones, etc.) for their health were more likely to engage in eHealth, despite any demographic variables. This is an important potential intervention point for health educators and health-care practitioners: capitalizing on how people are already using devices could improve their health care in the short and long term. Finally, because older adults and less educated persons were less likely to engage in eHealth, collaborating with developers to ensure user-friendly applications and devices will also help in increasing efficacy and usage related to eHealth in these groups. Researchers should consider testing applications among various at-risk groups to determine if the technology itself is becoming a barrier to eHealth.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the National Cancer Institute or any other health agency.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ledric D. Sherman  https://orcid.org/0000-0003-0858-9967
https://orcid.org/0000-0003-0858-9967
References
- Addis M. E., Mahalik J. R. (2003). Men, masculinity, and the contexts of help seeking. American Psychologist, 58(1), 5–14. [DOI] [PubMed] [Google Scholar]
- Alturki R. M., Gay V. (2016). A systematic review on what features should be supported by fitness apps and wearables to help users overcome obesity. International Journal of Research in Engineering and Technology, 5(9), 197–206. [Google Scholar]
- Andreassen H. K., Bujnowska-Fedak M. M., Chronaki C. E., Dumitru R. C., Pudule I., Santana S., Voss H., Wynn R. (2007). European citizens’ use of EHealth services: A study of seven countries. BMC Public Health, 7(147), 53. doi: 10.1186/1471-2458-7-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson N. L., Saperstein S. L., Pleis J. (2009). Using the internet for health-related activities: Findings from a national probability sample. Journal of Medical Internet Research, 11(1), e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball M. J., Lillis J. (2001). E-health: Transforming the physician/patient relationship. International Journal of Medical Informatics, 61(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Bansil P., Keenan N. L., Zlot A. I., Gilliland J. C. (2006). Health-related information on the web: Results from the HealthStyles Survey, 2002–2003. Preventing Chronic Disease, 3(2), A36. [PMC free article] [PubMed] [Google Scholar]
- Carpenter D. M., DeVellis R. F., Hogan S. L., Fisher E. B., DeVellis B. M., Jordan J. M. (2011). Use and perceived credibility of medication information sources for patients with a rare illness: Differences by gender. Journal of Health Communication, 16(6), 629–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheatham C. T., Barksdale D. J., Rodgers S. G. (2007) Barriers to health care and health-seeking behaviors faced by Black men. Journal of the American Academy of Nurse Practitioners, 20(11): 555–562. [DOI] [PubMed] [Google Scholar]
- Cornally N., McCarthy G. (2011). Help-seeking behaviour: A concept analysis. International Journal of Nursing Practice, 17(3), 280–288. [DOI] [PubMed] [Google Scholar]
- Cotten S. R., Gupta S. S. (2004). Characteristics of online and offline health information seekers and factors that discriminate between them. Social Sciences & Medicine, 59(9), 1795–1806. [DOI] [PubMed] [Google Scholar]
- Cottone J. G., Drucker P., Javier R. A. (2002). Gender differences in psychotherapy dyads: Changes in psychological symptoms and responsiveness to treatment during 3 months of therapy. Psychotherapy: Theory, Research, Practice, Training, 39(4), 297–308. [Google Scholar]
- Do H. P., Tran B. X., Le Pham Q., Nguyen L. H., Tran T. T., Latkin C. A., Dunne M. P., Baker P. R. (2018). Which eHealth interventions are most effective for smoking cessation? A systematic review. Patient Preference and Adherence, 12, 2065–2084. doi: 10.2147/PPA.S169397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty D. T., Kartalova-O’Doherty Y. (2010). Gender and self-reported mental health problems: Predictors of help-seeking from a general practitioner. British Journal of Health Psychology, 15(Pt 1), 213–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan P., King G., Lawrence D., Petrucci S. A., Robinson R. G., Banks D., Marable S., Grana R. (2004). Eliminating tobacco-related health disparities: Directions for future research. American Journal of Public Health, 94(2), 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Xie W. (2015). Digital divide 2.0: The role of social networking sites in seeking health information online from a longitudinal perspective. Journal of Health Communication, 20(1), 60–68. [DOI] [PubMed] [Google Scholar]
- Fox S., Jones S. (2009). The social life of health information (Pew Research Center). http://www.pewinternet.org/2009/06/11/the-social-life-of-health-Information
- Hallyburton A., Evarts L. A. (2014). Gender and online health information seeking: A five survey meta-analysis. Journal of Consumer Health on the Internet, 18(2), 128–142. [Google Scholar]
- Hammond W. P., Matthews D., Corbie-Smith G. (2010). Psychosocial factors associated with routine health examinations scheduling and receipt among African American men. Journal of the National Medical Association, 102(4), 276–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitlin P., Rainie L. (2019). Facebook algorithms and personal data. Pew Research Center. Retrieved January 16, 2019 from http://www.pewinternet.org/2019/01/16/facebook-algorithms-and-personal-data [Google Scholar]
- Houston T. K., Allison J. J. (2002). Users of internet health information: Differences by health status. Journal of Medical Internet Research, 4(2), e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. Released. (2018). IBM SPSS statistics for Windows, version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- Jadad A. R., Meryn S. (2013). The future of men’s health: Trends and opportunities to watch in the age of the internet. Journal of Men’s Health and Gender, 2(1), 124–128. [Google Scholar]
- Karlamangla A., Zhou K., Reuben D., Greendale G., Moore A. (2006). Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction, 101(1), 91–99. [DOI] [PubMed] [Google Scholar]
- Kontos E., Blake K. D., Chou W. Y., Prestin A. (2014). Predictors of eHealth usage: Insights on the digital divide from the Health Information National Trends Survey 2012. Journal of Medical Internet Research, 16(7), e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert S. D., Loiselle C. G. (2007). Health information-seeking behavior. Qualitative Health Research, 17(8), 1006–1019. [DOI] [PubMed] [Google Scholar]
- Laumann E. O., Nicolosi A., Glasser D. B., Paik A., Gingell C., Moreira E., Wang T. GSSAB Investigators’ Group. (2005). Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the global study of sexual attitudes and behaviors. International Journal of Impotence Research, 17(1), 39–57. [DOI] [PubMed] [Google Scholar]
- Nam S. K., Chu H. J., Lee M. K., Lee J. H., Kim N., Lee S. M. (2010). A meta-analysis of gender differences in attitudes toward seeking professional psychological help. Journal of American College Health, 59(2), 110–116. [DOI] [PubMed] [Google Scholar]
- Naughton F., Jamison J., Boase S., Sloan M., Gilbert H., Prevost A. T., Mason D., Smith S., Brimicombe J., Evans R., Sutton S. (2014). Randomized controlled trial to assess the short-term effectiveness of tailored web- and text-based facilitation of smoking cessation in primary care (iQuit in practice). Addiction, 109(7), 1184–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ophelia T., Morey M. L. S. (2007). Digital disparities. Journal of Consumer Health on the Internet, 11(4), 23–41. [Google Scholar]
- Oquendo M. A., Ellis S. P., Greenwald S., Malone K. M., Weissman M. M., Mann J. J. (2001). Ethic and sex differences in suicide rates relative to major depression in the United States. American Journal of Psychiatry, 158(10), 1652–1658. [DOI] [PubMed] [Google Scholar]
- Powell J., Inglis N., Ronnie J., Large S. (2011). The characteristics and motivations of online health information seekers: Cross-sectional survey and qualitative interview study. Journal of Medical Internet Research, 13(1), e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckelhoff J. F. (2001). Gender differences in the regulation of blood pressure. Hypertension, 37(5), 1199–1208. [DOI] [PubMed] [Google Scholar]
- Richardson A., Graham A. L., Cobb N., Xiao H., Mushro A., Abrams D., Vallone D. (2013). Engagement promotes abstinence in a web-based cessation intervention: Cohort study. Journal of Medical Internet Research, 15(1), e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero K. J., Gros D. F., McCauley J., de Arellano M. A., Danielson C. K. (2011). Rural adults’ use of health-related information online: Data from a 2006 national online health survey. Telemedicine Journal and E-Health, 17(5), 329–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon P., Hall G. M. (2004). Patient empowerment or the emperor’s new clothes. Journal of the Royal Society of Medicine, 97(2), 53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahab L., Brown J., Gardner B., Smith S. G. (2014). Seeking health information and support online: Does it differ as a function of engagement in risky health behaviors? Evidence from the health information national trends survey. Journal of Medical Internet Research, 16(11), e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhubl S. R., Muse E. D., Topol E. J. (2015). The emerging field of mobile health. Science Translational Medicine, 7(283), 283rv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern M. J., Cotten S. R., Drentea P. (2012). The separate spheres of online health: Gender, parenting, and online health information searching in the information age. Journal of Family Issues, 33(10), 1324–1350. [Google Scholar]
- Thackeray R., Crookston B. T., West J. H. (2013). Correlates of health-related social media use among adults. Journal of Medical Internet Research, 15(1), e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K., Ramanadhan S., Kontos K., Galea S. (2007). Mass media. In Galea S. (Ed.), Macrosocial determinants of population health (pp. 275–294). Springer. [Google Scholar]
- Wang P. S., Aguilar-Gaxiola S., Alonso J., Angermeyer M. C., Borges G., Bromet E. J., Bruffaerts R., de Girolamo G., de Graaf R., Gureje O., Haro J. M., Karam E. G., Kessler R. C., Kovess V., Lane M. C., Lee S., Levinson D., Ono Y., Petukhova M., . . . Wells J. E. (2007). Worldwide use of mental health services for anxiety, mood, and substance disorders: Results from 17 countries in the WHO World Mental Health (WMH) surveys. Lancet, 370(9590), 841–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson B. (2015). Algorithmic skin: Health-tracking technologies, personal analytics and the biopedagogies of digitized health and physical education. Sport, Education and Society, 20(1), 133–151. [Google Scholar]
- World Health Organization. (2016). Prevention and promotion in mental health. Author. [Google Scholar]