Abstract
Background:
Recalcitrant greater trochanteric pain is increasingly recognized as an indication for surgical intervention. The arthroscopic approach has become rapidly more common than the open alternative.
Hypothesis:
Patients undergoing radiofrequency microdebridement (RFMD) as an adjunct to arthroscopic gluteal bursectomy (AGB) and iliotibial band release (ITBR) will experience better functional improvement than AGB and ITBR alone at 1 year.
Study Design:
Randomized controlled trial; Level of evidence, 2.
Methods:
A total of 33 patients with failed nonoperative treatment of gluteal tendinopathy were randomly allocated to undergo AGB/ITBR or AGB/ITBR + RFMD. Full-thickness tears were excluded. The primary outcome measure was the modified Harris Hip Score (mHHS) at 52 weeks. Secondary outcome measures included the mHHS, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analog scale (VAS) for pain, and 12-item Short Form Health Survey (SF-12), which were evaluated at 0, 6, 12, 24, and 52 weeks. Statistical significance was defined as P < .05.
Results:
A total of 33 participants (33 hips; 30 female and 3 male; mean age, 58 years) were randomized; 16 patients underwent AGB/ITBR + RFMD, and 17 underwent AGB/ITBR. Participants’ functionality improved in both groups at all time intervals. The mean mHHS score improved from 57.49 ± 10.61 to 77.76 ± 18.40 (P = .004) and from 58.98 ± 12.33 to 79.96 ± 18.86 (P = .001) at 52 weeks in the AGB/ITBR and AGB/ITBR + RFMD groups, respectively, although there was no statistically significant difference between groups. There were no device-related adverse events.
Conclusion:
AGB/ITBR led to significant improvements in patients with recalcitrant gluteal tendinopathy. In this small RCT, the addition of RFMD showed no additional benefit to AGB/ITBR but provided a safe adjunct for the surgical management of recalcitrant gluteal tendinopathy.
Registration:
NCT01562366 (ClinicalTrials.gov identifier).
Keywords: radiofrequency microdebridement, gluteal tendinopathy, greater trochanteric pain syndrome, hip arthroscopic surgery, bursitis, gluteal tendon tear
Gluteal tendinopathy, as a cause of greater trochanteric pain syndrome, remains a difficult clinical problem. Nonsurgical measures, including physical therapy, analgesics, and nonsteroidal anti-inflammatory drugs (NSAIDs), are considered first line, although with little supporting evidence.2,17,19 Despite the arguable presence of inflammation in the pathogenesis of tendinopathy, corticosteroid injections offer a good short-term effect in relieving symptoms.2 The increasing evidence for platelet-rich plasma (PRP) injections offers a promising nonsurgical option with longer lasting symptomatic benefits.11–13
There is currently a lack of high-quality research on the surgical treatment of gluteal tendinopathy. Surgery has been performed to repair full-thickness tears when nonoperative measures fail. Surgery for tendinopathy (including partial-thickness tears and tendinopathy) has been described as open techniques, including bursectomy, resection or release of the iliotibial band, and ostectomy of the greater trochanter.4,24 Arthroscopic bursectomy with or without iliotibial band release (ITBR) has been recently proposed as a treatment alternative, which may offer advantages over more invasive open surgical procedures.10,15
Arthroscopic radiofrequency microdebridement (RFMD) is a novel technique for the surgical treatment of tendinopathy. It has been proposed as an alternative to surgical debridement in the rotator cuff, Achilles tendon, and plantar fascia.7,18,20,25,26 Radiofrequency is thought to stimulate angiogenesis and promote the regeneration of tendon fibers.3,16 There is some evidence that pain relief is the result of radiofrequency-induced ablation of free nerve endings.22,26 To date, there have been no trials evaluating the safety or efficacy of microdebridement for gluteal tendinopathy.
The hypothesis of this study was that patients undergoing RFMD as an adjunct to arthroscopic gluteal bursectomy (AGB) and ITBR would experience better functional improvement than AGB and ITBR alone at 1 year.
Methods
This trial was registered with the Australian New Zealand Clinical Trials Registry and was approved by the Epworth HealthCare Human Research Ethics Committee (54512).
Study Design and Setting
This study was a 2-center, parallel-group, double-blind (participants and assessors) randomized controlled trial (RCT). Recruitment took place between May 2012 and January 2016. Patients between 40 and 70 years of age with recalcitrant gluteal tendinopathy (including partial-thickness tears) were invited to participate. Tendinopathy was confirmed radiologically by an experienced musculoskeletal radiologist at one center via either ultrasound or magnetic resonance imaging.
Failed nonoperative treatment, a prerequisite for recruitment into this trial, included at least 6 months of an initial period of rest and avoidance of aggravating activities, followed by physical therapy (≥6 sessions), analgesics, NSAIDs for ≥2 weeks, and at least 1 steroid injection. Some patients received either a second steroid injection or a PRP injection.
Patients were excluded preoperatively if they had a history of surgery to the hip, lumbar spine, or trochanteric region. They were also excluded if there were signs of femoroacetabular impingement, a labral tear was reported on radiological studies, any intra-articular procedure was concomitantly required, inflammatory arthropathy was present, there was long-term steroid use (>6 weeks), or they were simultaneously participating in another prospective study. Patients were excluded intraoperatively if an arthroscopic inspection demonstrated a full-thickness gluteal tendon tear.
Randomization
Treatment was allocated intraoperatively according to a computer-generated schedule by an independent member of the operating room staff. Randomization took place after ITBR and AGB had been completed so that those receiving RFMD had no other alteration in their procedure. Patients with full-thickness tears were excluded before randomization. Participants were allocated 1:1 to receive either our standard surgical care10 consisting of AGB/ITBR or AGB/ITBR + RFMD.
Surgical Procedure
The operative procedure was performed according to our routine practice. Antibiotics and thromboprophylaxis were given. Patients were in the lateral decubitus position using the McCarthy hip distractor, although no traction was applied. Ultimately, 2 peritrochanteric portals were used to access the lateral compartment, and AGB/ITBR was performed. First, the iliotibial band was cut in a cruciate pattern from its superficial surface and the corners then removed to leave a diamond-shaped defect in the iliotibial band overlying the greater trochanter. The trochanteric bursa was then excised using a combination of radiofrequency ablation and an arthroscopic shaver. Patients allocated to AGB/ITBR + RFMD subsequently underwent RFMD using a Topaz device (ArthroCare) (Figure 1). An average of 8 to 10 punctures were made into the gluteus medius and minimus tendons with the probe in a grid-like pattern at differing depths (see Video Supplement). Each RF “pulse” was controlled for a 0.5-s duration and generated a temperature of 40°C to 70°C. At the completion of surgery, all patients received a 20-mL injection of bupivacaine at 0.5%, adrenaline 0.020 mg, morphine 5 mg, and ketorolac 30 mg into the pre-existing bursal space. Portal closure with a single absorbable monofilament suture was performed in all patients.
Figure 1.
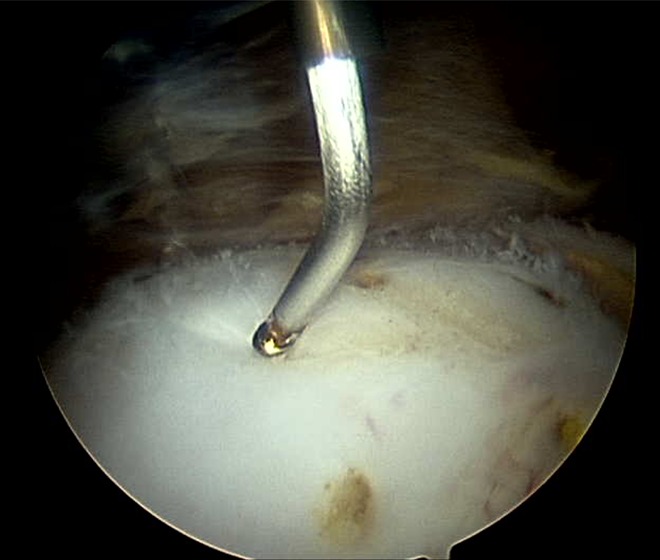
Arthroscopic radiofrequency microdebridement (RFMD) of the superior surface of the gluteal tendons of the hip.
Outcome Measures
Participants were screened preoperatively and assessed at 6, 12, 24, and 52 weeks. The primary outcome measure was the change in the modified Harris Hip Score (mHHS) between baseline and follow-up at 52 weeks. Because the mHHS has a maximum of 91 points, participants’ scores were multiplied by 1.1 to generate a range between 0 and 100, with a lower score representing more severe hip disability.5
The number of patients achieving the patient acceptable symptomatic state for the mHHS, defined as 74 points, was documented.6 Other secondary outcome measures included the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the visual analog scale (VAS) for pain, and the 12-item Short Form Health Survey (SF-12). Adverse events (AEs) were defined as any medical complication in a patient throughout the duration of the study.
Patients were blinded to the treatment arm throughout the study period. Outcome data were collected by an independent assessor who was blinded to the allocation of treatment. It was not possible to blind the surgeon, but the surgeon had no role in data collection or analysis.
Statistical Analysis
The study was conducted as a superiority trial, considering 15 points on the mHHS as a clinically significant change, with an estimated standard deviation of 20. To test the null hypothesis of no difference between treatment groups, the recruitment of 66 participants was planned to achieve a power of 90% and 5% significance.
Statistical analysis was performed using STATA (Version 13.1; StataCorp). Descriptive statistics were used to present continuous study variables. Independent-samples t tests compared primary and continuous secondary outcomes. All tests were 2-sided and performed at a 5% significance level.
Results
A total of 101 patients were screened for this study between May 2012 and January 2016. Of these, 65 were excluded, 36 enrolled, and 3 had full-thickness tears found intraoperatively, leaving 33 patients randomized. Moreover, 17 patients met the exclusion criteria because of full-thickness tears seen on imaging preoperatively. There were 3 participants who met the intraoperative exclusion criteria of full-thickness tendon tears, demonstrating the failure of preoperative imaging to identify full-thickness tears in this group. Participants were treated similarly regardless of whether they had partial-thickness tears. Enrollment was discontinued prematurely because of slow recruitment. The study flowchart is shown in Figure 2. All 33 patients were included in the analysis at 52 weeks.
Figure 2.
Flowchart of study patients. AGB, arthroscopic gluteal bursectomy; F-U, follow-up; ITBR, iliotibial band release; mHHS, modified Harris Hip Score; RFMD, radiofrequency microdebridement.
The groups were well balanced across demographic and baseline variables (Table 1). There were no important differences in the medical history between the treatment groups.
Table 1.
Baseline Demographicsa
| Patient Characteristics | AGB/ITBR + RFMD (n = 16) | AGB/ITBR (n = 17) |
|---|---|---|
| Female sex, n (%) | 15 (94) | 15 (88) |
| Age, y | 57.1 ± 8.53 | 58.4 ± 8.02 |
| Body mass index, kg/m2 | 29.2 ± 3.88 | 27.4 ± 4.47 |
| Smoker, n (%) | 1 (6) | 0 (0) |
| mHHS score | 58.98 ± 12.33 | 57.49 ± 10.61 |
aData are shown as mean ± SD unless otherwise indicated. P > .05 for all characteristics. AGB, arthroscopic gluteal bursectomy; ITBR, iliotibial band release; mHHS, modified Harris Hip Score; RFMD, radiofrequency microdebridement.
There was a significant improvement from baseline on the mHHS in both groups. Mean scores in the AGB/ITBR group improved from 57.49 ± 10.61 to 77.43 ± 20.02 and to 77.76 ± 18.40 at 24 and 52 weeks, respectively (P = .001 and .004, respectively). Mean scores in the AGB/ITBR + RFMD group improved from 58.98 ± 12.33 to 71.79 ± 17.75 and to 79.96 ± 18.86 at 24 and 52 weeks, respectively (P = .03 and .001, respectively). Differences between groups did not reach statistical significance at any time point (P = .75 at 52 weeks). The mHHS values at all time intervals are detailed in Figure 3.
Figure 3.
Modified Harris Hip Score (mHHS) at baseline and 6, 12, 24, and 52 weeks. AGB, arthroscopic gluteal bursectomy; ITBR, iliotibial band release; RFMD, radiofrequency microdebridement.
The patient acceptable symptomatic state for the mHHS (≥74/100) was achieved by 69% of patients in the AGB/ITBR + RFMD group versus 63% in the AGB/ITBR group (P = .72).
There was a significant improvement from baseline on the WOMAC and VAS in both groups. By 52 weeks, the mean WOMAC score had improved by 27.0 points in the AGB/ITBR + RFMD group and by 13.2 points in the AGB/ITBR group (95% CI, 11.99-38.37; P < .01 and 95% CI, 6.55-19.98; P = .038, respectively). The between-group difference at 52 weeks was 4.06 ± 7.49 (P = .59). The mean VAS score for pain had improved by 36.2 mm in the AGB/ITBR + RFMD group and by 30.4 mm in the AGB/ITBR group (95% CI, 21.58-50.84; P < .01 and 95% CI, 10.42-50.38; P < .01, respectively). The between-group difference at 52 weeks was 6.95 ± 9.68 (P = .48).
The physical component of the SF-12 improved by 11.3 points in the AGB/ITBR + RFMD group and by 8.3 points in the AGB/ITBR group. The psychological component remained almost unchanged from baseline. There was no significant difference in SF-12 scores between the groups at the end of follow-up (95% CI, –4.67 to 8.07; P = .59).
There were 24 AEs reported in 17 patients during the study period (Table 2). As anticipated in a surgical trial, postoperative pain was the most commonly reported AE. A total of 7 AEs (in 7 patients) were considered severe, with no difference between groups. No AE led to withdrawal from the study.
Table 2.
Reported Adverse Eventsa
| AGB/ITBR + RFMD (n = 16) | AGB/ITBR (n = 17) | Total (N = 33) | ||||
|---|---|---|---|---|---|---|
| n (%) | No. of Events | n (%) | No. of Events | n (%) | No. of Events | |
| System organ class/preferred term | ||||||
| All adverse events not related to treatment | 7 (43.8) | 11 | 10 (58.8) | 13 | 17 (51.5) | 24 |
| All treatment-related events | 0 | 0 | 0 | 0 | 0 | 0 |
| Musculoskeletal and connective tissue disorders | ||||||
| Arthralgia of hip joint | 4 (25.0) | 4 | 6 (35.3) | 7 | 10 (30.3) | 11 |
| Joint range of motion decreased | 0 | 0 | 1 (5.9) | 1 | 1 (3.0) | 1 |
| Worsening lateral hip symptoms | 0 | 0 | 1 (5.9) | 1 | 1 (3.0) | 1 |
| Surgical and medical procedures | ||||||
| Arthroscopic surgery of hip | 0 | 0 | 1 (5.9) | 1b | 1 (3.0) | 1 |
| Hip surgery | 0 | 0 | 1 (5.9) | 1b | 1 (3.0) | 1 |
| Knee surgery | 0 | 0 | 1 (5.9) | 1b | 1 (3.0) | 1 |
| Spinal fusion surgery | 0 | 0 | 1 (5.9) | 1b | 1 (3.0) | 1 |
| Injury, poisoning, and procedural complications | ||||||
| Foot fracture | 1 (6.3) | 1b | 0 | 0 | 1 (3.0) | 1 |
| Patellar fracture | 1 (6.3) | 1 | 0 | 0 | 1 (3.0) | 1 |
| General disorders and administration-site conditions | ||||||
| Adverse drug reaction | 1 (6.3) | 1 | 0 | 0 | 1 (3.0) | 1 |
| Immune system disorders | ||||||
| Drug hypersensitivity | 1 (6.3) | 1 | 0 | 0 | 1 (3.0) | 1 |
| Infections and infestations | ||||||
| Nasopharyngitis | 1 (6.3) | 1 | 0 | 0 | 1 (3.0) | 1 |
| Benign, malignant, and unspecified neoplasms (including cysts and polyps) | ||||||
| Breast cancer | 1 (6.3) | 1b | 0 | 0 | 1 (3.0) | 1 |
| Renal and urinary disorders | ||||||
| Renal injury | 1 (6.3) | 1b | 0 | 0 | 1 (3.0) | 1 |
aPercentages are based on the number of patients within each treatment group. AGB, arthroscopic gluteal bursectomy; ITBR, iliotibial band release; RFMD, radiofrequency microdebridement.
bSerious adverse event.
Discussion
Although many cases of gluteal tendinopathy can be treated nonoperatively with physical therapy, NSAIDs, or injections of corticosteroids or PRP,12,13 there are a group of patients who do not respond well to nonsurgical treatment. These patients are defined as having recalcitrant gluteal tendinopathy for whom surgical treatment may be beneficial.
This study showed significant improvement in functional (mHHS, WOMAC) and pain scores (VAS, physical component of SF-12) after arthroscopic treatment for this group of patients with recalcitrant gluteal tendinopathy, with or without the addition of RFMD. Although all of these measures showed greater improvement at 12 months with the addition of RFMD, these differences did not show a statistically significant benefit.
Our surgical results compare favorably with other published results of AGB/ITBR. Fox14 found good or excellent results in 23 of 27 patients undergoing bursectomy with no reported intervention to the iliotibial band. Drummond et al9 reported improvement on both the Oxford Hip Score and International Hip Outcome Tool (iHOT-33) 20 months after surgery in a retrospective analysis of 49 patients undergoing arthroscopic ITBR and bursectomy, although they included 7 cases that presented full-thickness tendon tears and were repaired, making the comparison between results more complex. Baker et al,1 in a prospective cohort study of 25 patients, reported an improvement of 26 points on the mHHS at 22 months.
This is one of the first prospective controlled trials to show improvement in multiple outcome scores after arthroscopic treatment for gluteal tendinopathy.
Despite the range of surgical interventions described for recalcitrant gluteal tendinopathy, the literature has consistently shown a lack of data to support one treatment over another.8,23 Often, combinations of treatment modalities are employed, and a variety of outcome measures are used. A comparison of treatment methods is therefore difficult.17
The use of RFMD as an independent treatment modality has been investigated in the supraspinatus tendon, with equivalent results to subacromial decompression.27 Used in isolation, this technique is designed to be a simpler and less involved procedure, reducing surgical time. In our study, RFMD was used as an adjunct to the usual care (AGB/ITBR). Further study would be required to use RFMD in isolation and determine surgical times.
It has been postulated that RFMD affects the tendon microstructure and might influence/reduce long-term symptomatic relapse.21,26 A longer term follow-up of our patients would allow us to assess whether patients undergoing adjunct RFMD have lower recurrence rates.
The major strength of this study is its strict RCT and double-blinded design using consistent diagnostic criteria and a standard surgical treatment with or without RFMD, thereby avoiding the confounding variables of multiple surgical interventions.
The study also has limitations: particularly, the sample size reduced from the planned 66 to 33 participants because of slow recruitment. The surgeons were not blinded but performed all surgery other than RFMD before randomization, and there were no objective measurements of structural change such as magnetic resonance imaging. The lack of statistical significance comparing the improvement between groups might be therefore caused by a lack of power (type II error). However, the study is of sufficient size to exhibit the safety of both AGB/ITBR and RFMD. The question regarding superiority remains to be answered definitively with larger sample studies. The other limitation is that results were not stratified according to the presence of partial-thickness tears.
Conclusion
AGB/ITBR led to significant improvements in patients with recalcitrant gluteal tendinopathy. In this small RCT, the addition of RFMD showed no additional benefit to AGB/ITBR but provided a safe adjunct for the surgical management of recalcitrant gluteal tendinopathy.
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967119895602.
Footnotes
Final revision submitted August 20, 2019; accepted September 11, 2019.
One or more of the authors declared the following potential conflict of interest or source of funding: J.O. has received consulting fees from Medacta and Smith & Nephew. J.F. has been on the medical advisory board for Bioventus Global. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Epworth HealthCare Human Research Ethics Committee.
References
- 1. Baker CL, Massie RV, Hurt WG, Savory CG. Arthroscopic bursectomy for recalcitrant trochanteric bursitis. Arthroscopy. 2007;23(8):827–832. [DOI] [PubMed] [Google Scholar]
- 2. Barratt PA, Brookes N, Newson A. Conservative treatments for greater trochanteric pain syndrome: a systematic review. Br J Sports Med. 2017;51(2):97–104. [DOI] [PubMed] [Google Scholar]
- 3. Bowden K, Ball S, Amiel D. Structural and angiogenic response to bipolar radiofrequency treatment of normal rabbit Achilles tendon: a potential application for the treatment of tendinosis. Trans Orthop Res Soc. 2003;28:819. [Google Scholar]
- 4. Brooker AF. The surgical approach to refractory trochanteric bursitis. Johns Hopkins Med J. 1979;145(3):98–100. [PubMed] [Google Scholar]
- 5. Byrd JWT, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2017;19(10):1055–1060. [DOI] [PubMed] [Google Scholar]
- 6. Chahal J, Van Thiel GS, Mather RC, 3rd, et al. The patient acceptable symptomatic state for the modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;43(8):1844–1849. [DOI] [PubMed] [Google Scholar]
- 7. Chou ACC, Ng SYC, Su DHC, Singh IR, Koo K. Radiofrequency microtenotomy is as effective as plantar fasciotomy in the treatment of recalcitrant plantar fasciitis. Foot Ankle Surg. 2017;22(4):270–273. [DOI] [PubMed] [Google Scholar]
- 8. Del Buono A, Papalia R, Khanduja V, Denaro V, Maffulli N. Management of the greater trochanteric pain syndrome: a systematic review. Br Med Bull. 2012;102:115–131. [DOI] [PubMed] [Google Scholar]
- 9. Drummond J, Fary C, Tran P. The outcome of endoscopy for recalcitrant greater trochanteric pain syndrome. Arch Orthop Trauma Surg. 2016;136(11):1547–1554. [DOI] [PubMed] [Google Scholar]
- 10. Farr D, Selesnick H, Janecki C, Cordas D. Arthroscopic bursectomy with concomitant iliotibial band release for the treatment of recalcitrant trochanteric bursitis. Arthroscopy. 2007;23(8):905.e1-5. [DOI] [PubMed] [Google Scholar]
- 11. Fitzpatrick J, Bulsara M, Zheng MH. The effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials. Am J Sports Med. 2016;45(1):226–233. [DOI] [PubMed] [Google Scholar]
- 12. Fitzpatrick J, Bulsara MK, O’Donnell J, McCrory PR, Zheng MH. The effectiveness of platelet-rich plasma injections in gluteal tendinopathy: a randomized, double-blind controlled trial comparing a single platelet-rich plasma injection with a single corticosteroid injection. Am J Sports Med. 2018;46(4):933–939. [DOI] [PubMed] [Google Scholar]
- 13. Fitzpatrick J, Bulsara MK, O’Donnell J, Zheng MH. Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2019;47(5):1130–1137. [DOI] [PubMed] [Google Scholar]
- 14. Fox J. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy. 2002;18(7):E34. [DOI] [PubMed] [Google Scholar]
- 15. Govaert LHM, van Dijk CN, Zeegers AVCM, Albers GHR. Endoscopic bursectomy and iliotibial tract release as a treatment for refractory greater trochanteric pain syndrome: a new endoscopic approach with early results. Arthrosc Tech. 2012;1(2):e161–e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gunes T, Bilgic E, Erdem M, et al. Effect of radiofrequency microtenotomy on degeneration of tendons: an experimental study on rabbits. Foot Ankle Surg. 2014;20(1):61–66. [DOI] [PubMed] [Google Scholar]
- 17. Lustenberger DP, Ng VY, Best TM, Ellis TJ. Efficacy of treatment of trochanteric bursitis: a systematic review. Clin J Sport Med. 2011;21(5):447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meknas K, Al Hassoni TN, Odden-Miland Å, Castillejo M, Kartus J. Medium-term results after treatment of recalcitrant lateral epicondylitis: a prospective, randomized study comparing open release and radiofrequency microtenotomy. Orthop J Sport Med. 2013;1(4):2325967113505433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mellor R, Bennell K, Grimaldi A, et al. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Br J Sports Med. 2018;52(22):1464–1472. [DOI] [PubMed] [Google Scholar]
- 20. Morrison RJM, Brock TM, Reed MR, Muller SD. Radiofrequency microdebridement versus surgical decompression for Achilles tendinosis: a randomized controlled trial. J Foot Ankle Surg. 2017;56(4):708–712. [DOI] [PubMed] [Google Scholar]
- 21. Ochiai N, Tasto JP, Ohtori S, Takahashi N, Moriya H, Amiel D. Nerve regeneration after radiofrequency application. Am J Sports Med. 2007;35(11):1940–1944. [DOI] [PubMed] [Google Scholar]
- 22. O’Donnell JM, Devitt BM, Arora M. The role of the ligamentum teres in the adult hip: redundant or relevant? A review. J Hip Preserv Surg. 2018;5(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reid D. The management of greater trochanteric pain syndrome: a systematic literature review. J Orthop. 2016;13(1):15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slawski DP, Howard RF. Surgical management of refractory trochanteric bursitis. Am J Sports Med. 1997;25(1):86–89. [DOI] [PubMed] [Google Scholar]
- 25. Sorensen MD, Hyer CF, Philbin TM. Percutaneous bipolar radiofrequency microdebridement for recalcitrant proximal plantar fasciosis. J Foot Ankle Surg. 2011;50(2):165–170. [DOI] [PubMed] [Google Scholar]
- 26. Takahashi N, Tasto JP, Ritter M, et al. Pain relief through an antinociceptive effect after radiofrequency application. Am J Sports Med. 2007;35(5):805–810. [DOI] [PubMed] [Google Scholar]
- 27. Taverna E, Battistella F, Sansone V, Perfetti C, Tasto JP. Radiofrequency-based plasma microtenotomy compared with arthroscopic subacromial decompression yields equivalent outcomes for rotator cuff tendinosis. Arthroscopy. 2007;23(10):1042–1051. [DOI] [PubMed] [Google Scholar]




