Abstract
Background
Supportive devices such as slings, wheelchair attachments and orthoses have been used to treat subluxation of the shoulder after stroke.
Objectives
To investigate the effect of supportive devices in preventing subluxation, re‐positioning the head of humerus in the glenoid fossa, decreasing pain, increasing function and adversely increasing contracture in the shoulder after stroke.
Search methods
We searched the Cochrane Stroke Group Trials Register (last searched on 22 March 2004). In addition, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, Issue 1, 2004), MEDLINE (1966 to March 2004), CINAHL (1982 to March 2004), EMBASE (1974 to March 2004), AMED (1985 to March 2004) and the Physiotherapy Evidence Database (PEDro, March 2004). We also handsearched conference proceedings and contacted authors for additional information.
Selection criteria
Studies were included if they were: randomised, quasi‐randomised or controlled trials; participants had a stroke; intervention was supportive devices; and subluxation, pain, function or contracture were measured.
Data collection and analysis
Two independent reviewers examined the identified studies which were assessed for methodological quality and analysed as (1) supportive devices versus no supportive devices or (2) two supportive devices.
Main results
Four trials (one on slings, three on strapping ‐ 142 participants) met the inclusion criteria. One trial testing a hemisling versus no device reported that no participants had subluxation greater than 10 mm, the same number had lost more than 30 degrees of shoulder external rotation (Peto odds ratio (OR) 1.00, 95% confidence interval (CI) 0.1 to 9.3), and more participants in the hemisling group had pain (Peto OR 8.7, 95% CI 1.1 to 67.1). The other three showed that strapping was effective in delaying the onset of pain (weighted mean difference (WMD) 14 days, 95% CI 9.7 to 17.8), but was ineffective in reducing pain severity (WMD ‐0.7 cm on a visual analogue scale, 95% CI ‐2.0 to 0.7), increasing upper limb function (WMD 0.8, 95% CI ‐1.5 to 3.1) or affecting the degree of contracture (WMD ‐1.4 degrees, 95% CI ‐10.9 to 8.1) at the shoulder.
Authors' conclusions
There is insufficient evidence to conclude whether slings and wheelchair attachments prevent subluxation, decrease pain, increase function or adversely increase contracture in the shoulder after stroke. There is some evidence that strapping the shoulder delays the onset of pain but does not decrease it, nor does it increase function or adversely increase contracture.
Plain language summary
Supportive devices for preventing and treating subluxation of the shoulder after stroke
There is insufficient evidence to conclude that supportive devices are effective in the prevention and treatment of subluxation of the shoulder after stroke. Shoulder subluxation is one of the most common secondary musculoskeletal problems after stroke which can cause pain and hinder the recovery of upper limb function. Supportive devices have traditionally been applied to treat shoulder subluxation. This review of four trials found insufficient evidence to conclude whether supportive devices prevent subluxation or not and found no evidence to conclude whether supportive devices can reposition the head of humerus in the glenoid fossa of an already subluxed shoulder.
Background
Inferior glenohumeral joint displacement, referred to as shoulder subluxation, is one of the most common musculoskeletal problems of the upper limb in individuals after stroke. Without muscle activity, the gravitational pull on the humerus causes stretching of the capsule of the shoulder joint resulting in shoulder subluxation (Moskowitz 1969). Proportional frequency of shoulder subluxation appears to be related to the recovery of muscles of the upper limb, i.e., the frequency of subluxation is related to the degree of the paralysis in the upper limb. For example, Najenson et al (Najenson 1971) reported an 81% proportional frequency, Smith et al (Smith 1982) reported a 60% proportional frequency while Miglietta et al (Miglietta 1959) reported a 56% proportional frequency in stroke patients who had no muscle activity of the upper arm. The proportional frequency was lower (40%) in stroke patients who had some activity in their upper arm (Linn 1999). Similarly, Chaco and Wolf (Chaco 1971) and Hurd et al (Hurd 1974) reported only a 15% and 7% proportional frequency in stroke patients who had activity of the upper arm muscles within one month.
Shoulder subluxation is considered a problem because it is believed to cause shoulder pain and hinder the recovery of upper limb function. It has been suggested that subluxation causes shoulder pain by overstretching the soft tissues (such as the shoulder capsule and muscles) surrounding the shoulder (Cailliet 1980; Chino 1981; Shai 1984). However, most studies report no significant correlation between subluxation and pain (Bohannon 1990; van Langenberghe 1988; Zorowitz 1996) indicating that subluxation is only one of several possible causes of shoulder pain following stroke. In contrast, there is more consistent evidence indicating that subluxation is associated with poor upper limb function (Hanger 2000) and reflex sympathetic dystrophy (a syndrome which presents with pain and tenderness of the affected part, associated with vasomotor instability or skin changes) (Dursun 2000). Therefore, prevention of shoulder subluxation should be an important focus of upper limb rehabilitation after stroke.
Since the 1950s, supportive devices such as slings, wheelchair attachments and external shoulder orthoses have been applied to counteract the downward pull of gravity on the humerus in an effort to treat shoulder subluxation. However, the effect of these supportive devices on subluxation, pain, function and adversely on contracture has not been systematically investigated.
Objectives
The main objectives of this systematic review were to investigate the following. (1) The effect of supportive devices (slings, attachments to wheelchairs/chairs and external shoulder orthoses) in preventing subluxation of the shoulder after stroke. (2) The effect of supportive devices in re‐positioning the head of the humerus in the glenoid fossa in a shoulder that is already subluxed after stroke. (3) The effect of supportive devices in preventing pain and improving function in the shoulder after stroke. (4) The adverse effect of supportive devices in increasing contracture in the shoulder after stroke.
Methods
Criteria for considering studies for this review
Types of studies
Truly randomised, quasi‐randomised, and controlled trials investigating the effect of two supportive devices or supportive devices versus no supportive devices were included in the review. Concealment, blinding and dropouts were noted for all studies but were not used to determine inclusion.
Types of participants
Studies which included patients of any gender and any age with a clinical diagnosis of stroke were included. Although it was envisaged that some trials would include participants with other types of upper motor neuron lesions, no mixed trials were identified. If trials of mixed participants had been identified, we would have attempted to obtain data for the stroke subgroup.
Types of interventions
Trials that evaluated the effect of any supportive device were included. Supportive devices were defined as any device designed to hold the head of humerus in the glenoid fossa by supporting the weight of the arm. It was planned to divide supportive devices into three categories: slings (such as Bobath sling or triangular sling), wheelchair attachments (such as lap‐trays or arm troughs), and external shoulder orthoses (such as strapping or the Functional Shoulder Orthosis). However, there were insufficient trials for this to be necessary.
Types of outcome measures
The primary outcome of interest was subluxation. Our intention was to analyse continuous variables (i.e., mm of subluxation measured from X‐ray) where possible, or dichotomous variables (i.e., presence or absence of subluxation). There was one trial examining the prevention of subluxation (Hurd 1974) in terms of the presence or absence of subluxation.
The other outcomes of interest were pain, function and contracture. For pain, our intention was to analyse continuous variables (i.e., cm of pain on a visual analogue scale) where possible, or dichotomous variables (i.e., presence or absence of pain). There was one trial which reported pain on a visual analogue scale (Hanger 2000). However, two other trials reported pain as number of pain free days after introduction of supportive devices (Ancliffe 1992; Griffin 2003) and these were pooled. Another trial (Hurd 1974) reported pain as presence or absence of pain. For function, our intention was to analyse continuous variables (i.e., normalised functional scales of upper limb activities). There was one trial (Hanger 2000) which reported function using the upper limb items of the Motor Assessment Scale (Carr 1985). For contracture, our intention was to analyse continuous variables (i.e., degrees of shoulder range of motion) wherever possible, or dichotomous variables (i.e., presence or absence of contracture). There was one trial (Hanger 2000) which reported contracture as degrees of shoulder external rotation and one trial (Hurd 1974) which reported the presence of contracture (i.e., loss of equal to or greater than 30 degrees of range of motion).
Search methods for identification of studies
See: 'Specialized register' section in Cochrane Stroke Group
We searched the Cochrane Stroke Group Trials Register, which was last searched by the Review Group Co‐ordinator on 22 March 2004. In addition, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, Issue 1, 2004) (Appendix 1), MEDLINE (1966 to March 2004) (Appendix 1), CINAHL (1982 to March 2004) (Appendix 2), AMED (1985 to March 2004) (Appendix 3), EMBASE (1974 to March 2004) (Appendix 4), and the Physiotherapy Evidence Database (PEDro: www.pedro.fhs.usyd.edu.au) (March 2004).
The database searches were supplemented by handsearching of the following conference proceedings. (1) International Congress of the World Confederation for Physical Therapy (World Confederation of Physical Therapy 1991 to 2003) (2) International Physiotherapy Congress (Australian Physiotherapy Association 1980 to 2002) (3) Australian Physiotherapy Conferences (APA 1980 to 2000) (4) Australian Neurological Physiotherapy Conference (APA 2003)
Data collection and analysis
Identification of relevant studies
One reviewer (AF) read the titles of the identified references and eliminated obviously irrelevant studies based on titles and, where available, abstracts. Two reviewers (AF and CC, physiotherapists with a background in neurological rehabilitation) independently examined potentially relevant studies using predetermined criteria. These criteria were: the study was a randomised, quasi‐randomised or controlled trial; participants were individuals who had had a stroke; interventions were a sling or a wheelchair attachment or an external shoulder orthosis; and subluxation or pain or function or contracture was measured as an outcome. Studies were ranked as excluded, or included or uncertain using a checklist. Disagreement was resolved by discussion between the reviewers (AF and CC). Trials that included participants that were less than two months from time of onset of stroke were investigated for the effect of supportive devices in preventing subluxation and pain, improving function and adversely increasing contracture in the shoulder. Trials that included participants with an already subluxed shoulder were planned to be investigated for the effect of supportive devices in repositioning the head of the humerus in the glenoid fossa, however, there were no trials identified in this category. There were no potentially‐relevant, non‐English trials requiring translation.
Assessment of methodological quality
The reviewers (AF and CC) scored the methodological quality of the included studies using the 11‐item PEDro scale (Moseley 2002), which is based on the Delphi List (Verhagen 1998) and available at The Physiotherapy Evidence Database (PEDro) (http://www.pedro.fhs.usyd.edu.au/scale_item.html). Items are: specification of eligibility criteria; random allocation to groups; concealed allocation; groups similar at baseline; blinding of participants, therapists and assessors; at least one outcome measurement obtained from more than 85% of participants initially allocated to groups; reporting of between‐group statistical comparisons; reporting of point measures and measures of variability. Disagreement was resolved by discussion between the reviewers.
Data extraction
Two reviewers (AF and CC) extracted descriptions of the studies including methods, inclusion criteria, participants' characteristics, description of the supportive devices, duration of intervention, and outcome measures reported. The number of participants as well as the means and standard deviations of outcome measures were extracted from each of the studies and recorded for analysis. The authors of the trials were contacted to provide clarification and/or missing data where possible.
Comparisons
Our intention was to compare (1) supportive devices versus no supportive devices or (2) two supportive devices. However, there were no trials identified in the latter category. Therefore, trials of supportive devices versus no supportive devices were analysed for the following outcomes. (1) Preventing subluxation (2) Re‐positioning the head of humerus (3) Decreasing pain (4) Increasing function (5) Increasing contracture However, there were no trials identified which investigated the outcome of repositioning the head of humerus.
Statistical analysis
If there were at least two studies that used the same outcome measurement, data was pooled. First, a test for heterogeneity and normality of continuous data was performed. Where there was homogeneity and normality, the effect sizes were reported as weighted mean differences (WMD) and 95% confidence intervals (CI), and a fixed‐effect model was used. Where there was significant heterogeneity (p < 0.1 using the Q‐test or chi‐square test) and lack of normality, the effect size were reported as standardised mean differences (SMD and 95% CI) and a random‐effects model was used. Peto odds ratios (Peto OR) and 95% CI were calculated for dichotomous data. All analyses were intention to treat wherever possible.
Results
Description of studies
Identification of relevant trials
Of the 270 studies retrieved from electronic database and hand searching, 244 obviously irrelevant studies were eliminated, leaving 26 potentially relevant studies. Examination of the reference lists of these potential studies and handsearching of conference proceedings added a further two studies making a total of 28 potentially relevant studies. Two independent reviewers (AF and CC) identified four studies for inclusion. Two reviewers (LA and CC) classified these four studies into the previously identified categories. Descriptions of the included studies can be found in the 'Characteristics of included studies' table and in Additional Table 2 (Methodological Quality of Included Studies).
1. Methodological quality of included studies.
| Study | Score | Randomisation | Concealment | Baseline compatible | Assessor Blinding | Drop‐outs = or < 15% | Intention to treat | Group comparisons | Point measures |
| Prevention trials | |||||||||
| Ancliffe 1992 | 3/8 | No, alternate allocation | No | No, unknown | Yes | Yes, 0% | No, unknown | Yes | Yes |
| Griffin 2003 | 8/8 | Yes | Yes, opaque envelope | Yes | Yes | Yes, 3% | Yes | Yes | Yes |
| Hanger 2000 | 8/8 | Yes | Yes, opaque envelope | Yes | Yes | Yes, 15% | Yes | Yes | Yes |
| Hurd 1974 | 2/8 | No, alternate allocation | No, unknown | No, unknown | No, unknown | Yes, 0% | No, unknown | No | Yes |
All four studies were classified as trials of supportive devices versus no supportive devices. One study (14 participants) examined the effect of supportive devices in preventing subluxation (Hurd 1974). Four studies (142 participants) examined the effect of supportive devices in decreasing pain (Ancliffe 1992; Griffin 2003; Hanger 2000; Hurd 1974). One study (98 participants) examined the effect of supportive devices in increasing function (Hanger 2000). Two studies (112 participants) examined the effect of supportive devices in adversely increasing contracture (Hanger 2000; Hurd 1974).
No studies examining the effect of supportive devices on repositioning the head of humerus in the glenoid fossa were identified.
Included studies comparing supportive devices with no supportive devices
Ancliffe 1992
This trial used alternate allocation to examine the effect of shoulder strapping on pain in eight participants after acute stroke (see 'Characteristics of included studies' for details) (Ancliffe 1992).
Griffin 2003
This trial used concealed random allocation to examine the effect of shoulder strapping on pain in 22 participants after acute stroke (see 'Characteristics of included studies' for details) (Griffin 2003).
Hanger 2000
This trial used concealed random allocation to examine the effect of shoulder strapping on pain, function and contracture in 98 participants after acute stroke (see 'Characteristics of included studies' for details) (Hanger 2000).
Hurd 1974
This trial used alternate allocation to examine the effect of a hemisling on subluxation, pain and contracture in 14 participants after acute stroke (see 'Characteristics of included studies' for details) (Hurd 1974).
Risk of bias in included studies
Details of the methodological quality are reported in the additional table (Table 2 'Methodological Quality of Included Studies'). For studies included in this review the maximum total PEDro score possible is 8 out of 10 since it is not possible to blind the participants or the physiotherapists to the intervention. The trials were variable in quality with two scoring highly (Griffin 2003; Hanger 2000) and two scoring poorly (Ancliffe 1992; Hurd 1974).
Effects of interventions
Comparison 01: Supportive devices versus no supportive devices
Preventing subluxation
There was one trial examining the effect of a hemisling in preventing subluxation (Hurd 1974. Hurd reports that only one participant (from the group that wore the hemisling) developed subluxation greater than 10 mm at the final follow up (five months) implying that no participants had greater than 10 mm of subluxation at initial follow up (four weeks).
Repositioning the head of humerus
There were no trials investigating the effect of supportive devices in repositioning the head of humerus in the glenoid fossa in a shoulder that is already subluxed.
Decreasing pain
There was one trial examining the effect of a hemisling in decreasing pain (Hurd 1974) where pain was reported as the number of participants who had nil, little or severe pain. There were significantly less participants who had pain at initial follow up (four weeks) in the no hemisling group (Peto OR 8.7, 95% CI 1.1 to 67.1, p = 0.04) (See Figure 01 Comparison 01 Outcome 01).
There were two trials examining the effect of strapping in decreasing pain (Ancliffe 1992; Griffin 2003) where pain was reported as the number of pain free days after admission to the study. Shoulder strapping significantly delayed the onset of shoulder pain by 14 days (WMD 14 days, 95% CI 9.7 to 17.8, fixed effect, p < 0.001) (See Figure 01 Comparison 01 Outcome 02). There was one trial examining the effect of strapping in decreasing pain (Hanger 2000) where pain severity was reported over the previous 24 hours on a visual analogue scale at six weeks after admission to the study. There was no difference in pain between the strapping group versus the no strapping group (WMD ‐0.7 cm, 95% CI ‐2.0 to 0.7, fixed effect, p = 0.34) (See Figure 01 Comparison 01 Outcome 03).
Increasing function
There was one trial examining the effect of strapping in increasing function (Hanger 2000) where function was reported as the summation of items 6, 7 and 8 of the Motor Assessment Scale. There was no difference in function between the strapping group versus the no strapping group (WMD 0.8, 95% CI ‐1.5 to 3.1, fixed effect, p = 0.48) (See Figure 01 Comparison 01 Outcome 04).
Increasing contracture
There was one trial examining the adverse effect of a hemisling in increasing contracture (Hurd 1974) where contracture was reported as the number of participants who had more than 30 degrees loss of shoulder external rotation. There was no difference in contracture between the hemisling group versus the no hemisling group (Peto OR 1.00, 95% CI 0.1 to 9.3, p = 1.00) (See Figure 01 Comparison 01 Outcome 05).
There was one trial examining the adverse effect of strapping in increasing contracture (Hanger 2000) where contracture was reported as range of shoulder external rotation at six weeks after admission to the study. There was no difference in contracture between the strapping group versus the no strapping group (WMD ‐1.4 degrees, 95% CI ‐10.9 to 8.1, fixed effect, p = 0.77) (See Figure 01 Comparison 01 Outcome 06).
Comparison 02: Two supportive devices
There were no studies comparing two different supportive devices.
Discussion
Musculoskeletal impairments of the shoulder, such as subluxation, pain and contracture, are common secondary problems after stroke. We are confident that our detailed search strategy of the electronic databases combined with hand searching of conference proceedings and references lists of published studies identified all relevant studies of supportive devices for prevention of these problems. It is therefore surprising to find only one clinical trial examining the effect of a sling (a routine intervention for the last 50 years) in preventing subluxation and pain as well as examining any adverse effect of increasing contracture. Furthermore, this trial was of disappointingly low quality. There were two high quality trials and one low quality trial examining the effect of strapping (a recently developed intervention) in preventing pain. However, these trials did not examine prevention of subluxation and only one examined prevention of contracture and improvement in function.
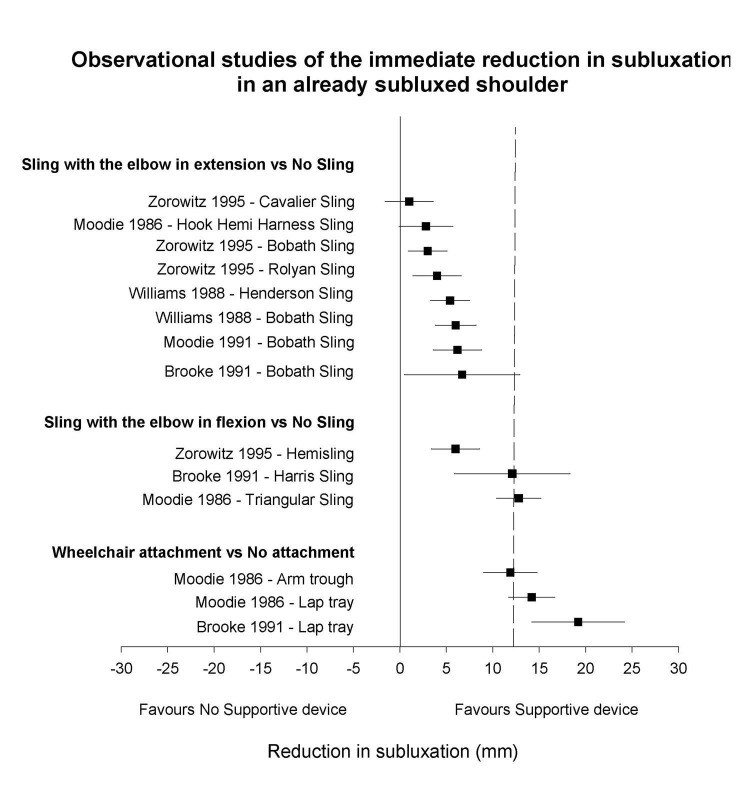
The only clinical trial examining the effect of a sling ‐ a hemisling ‐ reported no effect of wearing the sling for two to three weeks on subluxation or contracture. This is not surprising, since subluxation was considered to be clinically significant only when greater than 10 mm and contracture only when greater than 30 degrees. The development of these large amounts of subluxation and contracture within a month after stroke seems unlikely. Moreover, quite small amounts of subluxation cause malalignment of the humeral head and the glenoid fossa (Ada 2002; van Langenberghe 1988) which will interfere with function. Furthermore, if numbers of patients with clinically significant impairments are reported in future studies, then the period of intervention should be taken into account. For example, preventing 5 mm of subluxation and 15 degrees of loss of shoulder external rotation with a four‐week intervention would seem useful based on the amount of subluxation (Ada 2004; Linn 1999) and contracture (Ada 2004; Hanger 2000) developed in the control groups of previous clinical trials. There have been a number of observational studies which have examined the immediate effect of supportive devices in reducing subluxation in a shoulder that is already subluxed, i.e., subluxation of the shoulder was compared with a supportive device on and off (Brooke 1991; Moodie 1986; Williams 1988; Zorowitz 1995). Furthermore, although the order of measurement of subluxation (device on or off) was not randomised, in two of the studies (Williams 1988; Zorowitz 1995) the radiographers were blinded to device on or off and in the other two studies (Brooke 1991; Moodie 1986), the radiographers were not familiar with the supportive devices. Given the absence of prospective randomised controlled trials, these studies are worth examining in order to ascertain which devices are likely to have the potential to prevent subluxation. The four devices that produce an immediate reduction in subluxation are the lap tray, the arm trough, the triangular sling and the Harris sling (Figure 1) and it is, therefore, the ability of these devices to prevent subluxation that should be tested.
1.
Means and 95% CIs for the immediate reduction in subluxation (mm) with the use of supportive devices in an already subluxed shoulder. The vertical dotted line represents the average subluxation before applying supportive devices (calculated across the 4 studies)
Three clinical trials, two high quality and one low quality, examined the effect of strapping the shoulder. The application of strapping was found to be effective in delaying the onset of pain by 14 days based on the pooled analysis of one high and one low quality trial. However, the result from another high quality trial showed no difference in pain between strapping and no strapping after six weeks of intervention. There were slight differences in strapping technique between the studies but the trial with the strapping that appeared the most supportive (Hanger 2000) was the one which found no effect. It therefore seems reasonable to conclude that strapping is effective in delaying the onset of shoulder pain in the short term, but not in preventing pain in the longer term. Neither was strapping found to have any greater adverse effect in increasing contracture with loss of shoulder external rotation in both groups reaching nearly 30 degrees in two months. In addition, strapping did not increase function.
Authors' conclusions
Implications for practice.
Given that there is insufficient evidence from randomised controlled trials to conclude whether supportive devices are effective in preventing subluxation of the shoulder after stroke, at present, clinicians have to use other forms of evidence. In addition, since strapping the shoulder appears only to be effective in delaying the onset of, but not preventing pain in the shoulder, and it has no effect on contracture or function, at this stage it is not recommended.
Implications for research.
We suggest that there is a need for randomised controlled trials to evaluate the efficacy of supportive devices in preventing subluxation and pain, in increasing arm function, and evaluating any adverse effect of increasing contracture early after stroke. Supportive devices should be applied to these individuals early, i.e., as soon as they are allowed into the upright position, and continued for a period of time long enough for an effect to be detected, i.e., four to six weeks. Outcome measures should include subluxation of the shoulder (mean and standard deviation (SD) in mm as well as number of participants with more than 5 mm of subluxation), pain in the shoulder (mean and SD on a visual analogue scale), arm function and contracture of the shoulder (mean and SD in degrees of shoulder external rotation as well as number of participants with more than 15 degrees loss of shoulder external rotation).
What's new
| Date | Event | Description |
|---|---|---|
| 3 October 2008 | Amended | Converted to new review format. |
Acknowledgements
The authors would like to thank Carl Hanger, Jacqueline Ancliffe, Julie Bernhardt and Richard Zorowitz for providing us with information about their studies.
Appendices
Appendix 1. MEDLINE/CENTRAL search strategy
MEDLINE (OVID) 1966 to March 2004 and the Cochrane Central Register of Controlled Trials (CENTRAL) 2004 issue 1, employing the search strategy:
1. exp cerebrovascular disorders/ 2. (stroke$ or cerebrovascular or cerebral vascular or cva$).tw. 3. (cerebral or cerebellar or brain$ or vertebrobasilar).tw. 4. (infarct$ or isch?emi$ or thrombo$ or emboli$ or apoplexy).tw. 5. 3 and 4 6. (cerebral or brain$ or subarachnoid).tw. 7. (haemorrhage or hemorrhage or haematoma or hematoma or bleeding).tw. 8. 6 and 7 9. hemiplegia/ 10. (hemipleg$ or hemipar$ or poststroke or post‐stroke).tw. 11. 1 or 2 or 5 or 8 or 9 or 10 12. exp Orthotic Devices/ 13. Splints/ 14. (orthos$ or orthot$ or splint$ or sling$ or support$).tw. 15. (lapboard$ or lap board or laptray$ or lap tray$ or arm trough$).tw. 16. 12 or 13 or 14 or 15 17. shoulder dislocation/ 18. shoulder/ or shoulder joint/ or shoulder pain/ 19. (shoulder adj10 (sublux$ or dislocat$ or displace$ or malalign$ or misalign$)).tw. 20. 17 or 18 or 19 21. 11 and 16 and 20
Appendix 2. CINAHL search strategy
CINAHL (OVID) 1982 to March 2004, employing the search strategy:
1. exp cerebrovascular disorders/ 2. (stroke$ or cerebrovascular or cerebral vascular or cva$).tw. 3. (cerebral or cerebellar or brain$ or vertebrobasilar).tw. 4. (infarct$ or isch?emi$ or thrombo$ or emboli$ or apoplexy).tw. 5. 3 and 4 6. (cerebral or intracerebral or intracranial or parenchymal or brain$ or intraventricular or periventricular or cerebellar or infratentorial or supratentorial or subarachnoid).tw. 7. (Haemorrhage or hemorrhage or haematoma or hematoma or bleed$ or aneurysm).tw. 8. 6 and 7 9. hemiplegia/ 10. (aphasi$ or dysphasi$ or hemipleg$ or hemipar$).tw. 11. (hemipleg$ or hemipar$ or poststroke or post‐stroke).tw. 12. 1 or 2 or 5 or 8 or 9 or 10 or 11 13. exp Orthotic Devices/ 14. Splints/ 15. (orthos$ or orthot$ or splint$ or sling$ or support$).tw. 16. (lapboard$ or lap board or laptray$ or lap tray$ or arm trough$).tw. 17. 13 or 14 or 15 or 16 18. shoulder dislocation/ 19. shoulder/ or shoulder joint/ or shoulder pain/ 20. (shoulder adj10 (sublux$ or dislocat$ or displace$ or malalign$ or misalign$)).tw. 21. 18 or 19 or 20 22. 12 and 17 and 21
Appendix 3. AMED search strategy
AMED 1985 to March 2004, employing the search strategy:
1. cerebrovascular disorders/ 2. Hemiplegia/ 3. (stroke$ or poststroke or post‐stroke or cva$).tw. 4. (cerebrovascular or cerebral vascular or brain attack).tw. 5. (cerebral or cerebellar or brain$ or vertebrobasilar).tw. 6. (infarct$ or ischaemi$ or ischem$ or thrombo$ or apoplexy or emboli$ or insufficiency or occlusion).tw. 7. 5 and 6 8. (cerebral or intracerebral or intracranial or parenchymal or brain$ or intraventricular or cerebellar or infratentorial or supratentorial or subarachnoid).tw. 9. (haemorrhage or hemorrhage or haematoma or hematoma or bleed$ or aneurysm$ or vasospasm).tw. 10. 8 and 9 11. 1 or 2 or 3 or 4 or 7 or 10 12. exp Orthotic Devices/ 13. Splints/ 14. (orthos$ or orthot$ or splint$ or sling$ or support$).tw. 15. (lapboard$ or lap board or laptray$ or lap tray$ or arm trough$).tw. 16. 12 or 13 or 14 or 15 17. shoulder dislocation/ 18. shoulder/ or shoulder joint/ or shoulder pain/ 19. (shoulder adj10 (sublux$ or dislocat$ or displace$ or malalign$ or misalign$)).tw. 20. 17 or 18 or 19 21. 11 and 16 and 20
Appendix 4. EMBASE search strategy
EMBASE (ScienceDirect) 1974 to March 2004, employing the search strategy:
1. exp cerebrovascular disease 2. (stroke or poststroke or post stroke) 3. cerebrovascular 4. (cerebral or cerebellar or brainstem or vertebrobasilar) 5. (infarct! or ischemi! or thombo! or emboli!) 6. 4 and 5 7. (cerebral or intracerebral or intracranial or parenchymal or brain or intraventricular or brainstem or cerebellar or infratentorial or supratentorial or subarachnoid) 8. (haemorrhage or hemorrhage or haematoma or hematoma or bleeding or aneurysm) 9. 7 and 8 10. (hemiplegia or hemiparesis or hemipleg! or hemipar!) 11. 1 or 2 or 3 or 6 or 9 or 10 12. orthotic device 13. splint 14. (orthosis or orthotic or sling or support) 15. (lapboard or lap board or laptray or lap tray or arm trough) 16. 12 or 13 or 14 or 15 17. shoulder dislocation 18. (shoulder or shoulder joint or shoulder pain) 19. (shoulder subluxation or shoulder dislocation or shoulder displacement or shoulder malalignment or shoulder misalignment) 20. 17 or 18 or 19 21. 11 and 16 and 20
Data and analyses
Comparison 1. Supportive devices versus no supportive devices.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain (number of participants with pain) | 1 | 14 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 8.73 [1.14, 67.13] |
| 2 Pain (number of pain free days after admission to study) | 2 | 29 | Mean Difference (IV, Fixed, 95% CI) | 13.76 [9.68, 17.83] |
| 3 Pain (over previous 24 hours on a 10 cm visual analogue scale post intervention) | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐2.02, 0.70] |
| 4 Function (summation of Items 6, 7, 8 of the Motor Assessment Scale (score 0‐18) post intervention) | 1 | 83 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [‐1.46, 3.12] |
| 5 Contracture (number of participants with > 30° loss of shoulder external rotation) | 1 | 14 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.11, 9.34] |
| 6 Contracture (degrees of shoulder external rotation post intervention) | 1 | 81 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐10.90, 8.10] |
1.1. Analysis.
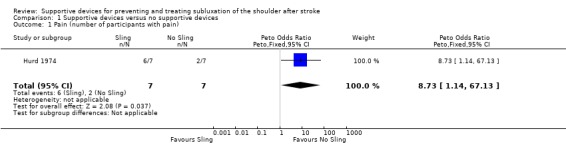
Comparison 1 Supportive devices versus no supportive devices, Outcome 1 Pain (number of participants with pain).
1.2. Analysis.
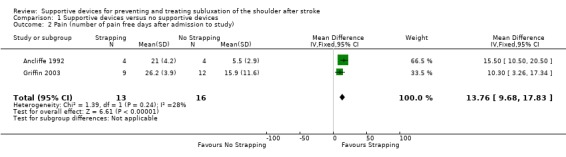
Comparison 1 Supportive devices versus no supportive devices, Outcome 2 Pain (number of pain free days after admission to study).
1.3. Analysis.
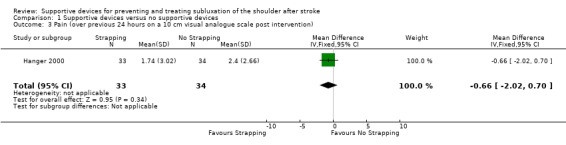
Comparison 1 Supportive devices versus no supportive devices, Outcome 3 Pain (over previous 24 hours on a 10 cm visual analogue scale post intervention).
1.4. Analysis.
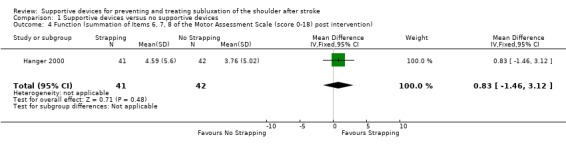
Comparison 1 Supportive devices versus no supportive devices, Outcome 4 Function (summation of Items 6, 7, 8 of the Motor Assessment Scale (score 0‐18) post intervention).
1.5. Analysis.
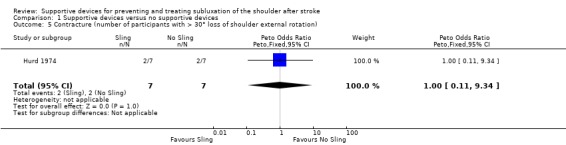
Comparison 1 Supportive devices versus no supportive devices, Outcome 5 Contracture (number of participants with > 30° loss of shoulder external rotation).
1.6. Analysis.
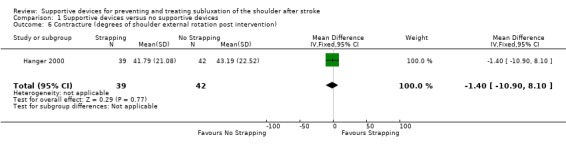
Comparison 1 Supportive devices versus no supportive devices, Outcome 6 Contracture (degrees of shoulder external rotation post intervention).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ancliffe 1992.
| Methods | Parallel group, single centre trial Exp: routine management (details not specified) + strapping C: routine management | |
| Participants | Inclusion criteria: no history of shoulder pain, upper arm paralysis Age (mean): Exp/C = 69/74 years Time after stroke: Exp/C = <2/2 days Number of participants: Exp/C = 4/4 Male/Female = 4/4 Right/Left hemiplegia = 1/7 Dropouts: Exp/C = 0/0 | |
| Interventions | Strapping: one protecting pad and two strapping tapes were used. First the protecting pad was positioned on the medial surface of the upper arm to protect the axilla and allow for application of the tape. The first strapping tape began at the middle of the clavicle, continued across the deltoid muscle in a diagonal direction, along the pad under the arm. Then, a slight stretch was applied in the direction of the posterior fibres of the deltoid with the tape terminating one quarter of the way along the spine of the scapula. The second strapping tape was applied in the same direction as the first, but 2 cms below. Strapping was left on day and night and changed every three or four days. | |
| Outcomes | Pain: number of pain‐free days (<1 Ritchie Articular Index: 0 = patient has no tenderness, 1 = patient complains of pain, 2 = patient complains of pain and winces, 3 = patient complains of pain, winces, and withdraws, Bohannon 1986) after admission to study | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Griffin 2003.
| Methods | Parallel group, single centre trial Exp: strapping + routine management (could include task‐specific re‐education for function, maintenance of ROM, provision of supportive devices for the arm) Placebo: placebo strapping + routine management C: routine management | |
| Participants | Inclusion criteria: within 4 weeks of stroke, no history of shoulder pain, score on Item 6 of the Motor Assessment scale of less than 4, score on Ritchie Articular Index of less than 2. Age (mean): Exp/P/C = 65/62/59 years Time after stroke (mean): Exp/P/C = 10/10/12 days Number of participants: Exp/P/C = 9/10/12 Male/Female = 22/10 Right/Left hemiplegia = 20/12 Dropouts: Exp/P/C = 1/0/0 | |
| Interventions | Strapping: one protecting pad and two strapping tapes were used. First the protecting pad was positioned on the medial surface of the upper arm to protect the axilla and allow for application of the tape. The first strapping tape began at the middle of the clavicle, continued across the deltoid muscle in a diagonal direction, along the pad under the arm. Then, a slight stretch was applied in the direction of the posterior fibres of the deltoid with the tape terminating one quarter of the way along the spine of the scapula. The second strapping tape was applied in the same direction as the first, but 2 cms below. Strapping was left on day and night and changed every three or four days. | |
| Outcomes | Pain: number of pain‐free days (< 2 on Ritchie Articular Index: 0 = patient has no tenderness, 1 = patient complains of pain, 2 = patient complains of pain and winces, 3 = patient complains of pain, winces, and withdraws, Bohannon 1986) after admission to study. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hanger 2000.
| Methods | Parallel group, single centre trial Exp: strapping + routine management (task‐specific re‐education for function, positioning, maintenance of ROM, provision of supportive devices for the arm when mobilising) C: routine management | |
| Participants | Inclusion criteria: within 4 weeks of stroke, no previous shoulder surgery precluding external rotation, unable to abduct shoulder to 90 degrees and hold for 2 seconds (upper arm function equivalent to a score of less than 4 on Item 6 of Motor Assessment Scale) Age (mean): Exp/C = 79/78 years Time after stroke (mean): Exp/C = 12/12 days Number of participants: Exp/C = 49/49 Male/Female = 39/59 Right/Left hemiplegia = 51/47 Dropouts: Exp/C = 8/7 | |
| Interventions | Strapping: three strapping and three under strapping tapes were used. The arm was supported under the elbow. First two tapes were applied longitudinally using a lifting action. One tape started from the front of the elbow and went up across the top of the shoulder and terminated past the spine of the scapula. The other tape started from the back of the elbow and went up across the top of the shoulder and terminated past the clavicle. These two tapes crossed at the top of the shoulder. The third tape was applied horizontally from the medial third of the clavicle around the surgical neck of the humerus and along the spine of the scapula to its medial third. Strapping was left on day and night and changed every two or three days. Duration of intervention: six weeks. | |
| Outcomes | Pain: pain over previous 24 hours on 10 cm vertical VAS (cm) Contracture: pain free passive shoulder external rotation (degrees) Function: summation of Items 6, 7, 8 (out of 18) of the Motor Assessment Scale (Carr 1985) | |
| Notes | Data for forest plots taken from unpublished data supplied by the author Note that there are different numbers of participants at the post‐intervention measurements due to missing data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hurd 1974.
| Methods | Parallel group, single centre trial Exp: routine management (details not specified) + sling C: routine management | |
| Participants | Inclusion criteria: first stroke, upper arm paralysis, no previous arm, shoulder or neck injury Age (range) = 22 to 87 years Time after stroke: 1 to 2 weeks Number of participants: Exp/C = 7/7 Male/Female = 4/10 Right/Left hemiplegia = unknown Dropouts: Exp/C = 0/0 | |
| Interventions | Sling: hemisling. Duration of intervention: 2 to 3 weeks | |
| Outcomes | Subluxation: number of participants with over 10 mm of subluxation Pain: number of participants who rated pain as nil, little or severe Contracture: number of participants who lost equal or greater than 30 degrees of shoulder external rotation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
C: control Exp: experimental P: placebo ROM: range of motion VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Brooke 1991 | Observational study |
| Brudny 1985 | Case report |
| Cool 1989 | No outcome of interest |
| Daviet 2002 | No outcome of interest |
| Egan 1990 | Descriptive study |
| Enstrom 1980 | Descriptive study |
| Ferreri 1974 | Descriptive study |
| Gracies 2000 | No outcome of interest |
| Krempen 1977 | Observational study |
| Moodie 1986 | Observational study |
| Morin 1997 | No outcome of interest |
| Patterson 1984 | No data available |
| Peters 2003 | Case report |
| Rajaram 1985 | No outcome of interest |
| Roy 1989 | Case report |
| Sodring 1980 | Descriptive study |
| Spaulding 1999 | No outcome of interest |
| Sullivan 1989 | Descriptive study |
| Walker 1983 | Descriptive study |
| Williams 1988 | Observational study |
| Zorowitz 1995 | Observational study |
| Zorowitz 1996 | No outcome of interest |
| Zorowitz 2001 | No outcome of interest |
Contributions of authors
Louise Ada (LA) contributed to the conception, design and approved the final manuscript of the protocol, helped extract trial and outcome data, guided the analysis and the interpretation of the data, contrituted to and approved the final manuscript of the review.
Anchalee Foongchomcheay (AF) contributed to the conception, design, drafted the protocol and searched electronic database and conference proceedings, screened titles and abstracts of references from the search, located, selected and assessed trials, extracted trials and outcome data, assessed the methodological quality of selected trials, contacted correspondents about unpublished data and also entered the data, carried out statistical analysis, helped with the interpretation of the data, drafted the review and approved the final manuscript of the review.
Colleen Canning (CC) contributed to screening the titles and abstracts of references from the search, located, selected and assessed trials, extracted trials and outcome data, assessed the methodological quality of selected trials, contributed to the interpretation of the data and contributed to and approved the final manuscript of the review.
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Ancliffe 1992 {published data only}
- Ancliffe J. Strapping the shoulder in patients following a cerebrovascular accident (CVA): a pilot study. Australian Journal of Physiotherapy 1992;38:37‐41. [DOI] [PubMed] [Google Scholar]
Griffin 2003 {unpublished data only}
- Griffin AL, Bernhardt J. Strapping of the hemiplegic shoulder prevents development of shoulder pain during rehabilitation. 1st Neruological Physiotherapy Conference of the National Neurology Group of the Australian Physiotherapy Association. 27‐29 November 2003:Sydney, Australia.
Hanger 2000 {published and unpublished data}
- Hanger HC, Whitewood P, Brown G, Ball MC, Harper J, Cox R, Sainsbury R. A randomized controlled trial of strapping to prevent post‐stroke shoulder pain. Clinical Rehabilitation 2000;14:370‐80. [DOI] [PubMed] [Google Scholar]
Hurd 1974 {published data only}
- Hurd MM, Farrell KH, Waylonis GW. Shoulder sling for hemiplegia: friend or foe?. Archives of Physical Medicine & Rehabilitation 1974;55:519‐22. [PubMed] [Google Scholar]
References to studies excluded from this review
Brooke 1991 {published data only}
- Brooke MM, Lateur BJ, Diana‐Rigby GC, Questad KA. Shoulder subluxation in hemiplegia: effects of three different supports. Archives of Physical Medicine & Rehabilitation 1991;72:582‐6. [PubMed] [Google Scholar]
Brudny 1985 {published data only}
- Brudny J. Functional impact of shoulder taping in the hemiplegic upper extremity. Orthotics and Prosthetics 1985;39:14‐20. [Google Scholar]
Cool 1989 {published data only}
- Cool JC. Biomechanics of orthoses for the subluxed shoulder. Prosthetics & Orthotics International 1989;13:90‐6. [DOI] [PubMed] [Google Scholar]
Daviet 2002 {published data only}
- Daviet JC, Preux PM, Salle JY, Lebreton F, Munoz M, Dudognon P, Pelissier J, Perrigot M. Clinical factors in the prognosis of complex regional pain syndrome type I after stroke: a prospective study. American Journal of Physical Medicine & Rehabilitation 2002;81:34‐9. [DOI] [PubMed] [Google Scholar]
Egan 1990 {published data only}
- Egan JM. An aid for the management of shoulder pain in hemiplegia. British Journal of Occupational Therapy 1990;53:362‐4. [Google Scholar]
Enstrom 1980 {published data only}
- Enstrom J, Davies J. Lapboard modification to help support a flaccid upper extremity. Physical Therapy 1980;6:795‐6. [DOI] [PubMed] [Google Scholar]
Ferreri 1974 {published data only}
- Ferreri J, Tumminelli J. A swivel cockup splint‐type armtrough. American Journal of Occupational Therapy 1974;28:359. [Google Scholar]
Gracies 2000 {published data only}
- Gracies JM, Marosszeky JE, Renton R, Sandanam J, Gandevia SC, Burke D. Short‐term effects of dynamic lycra splints on upper limb in hemiplegic patients. Archives of Physical Medicine & Rehabilitation 2000;81:1547‐55. [DOI] [PubMed] [Google Scholar]
Krempen 1977 {published data only}
- Krempen JF, Silver RA, Hadley J, Rivera V. The use of the Varney Brace for subluxating shoulders in stroke and upper motor neuron injuries. Clinical Orthopaedics & Related Research 1977;122:204‐6. [PubMed] [Google Scholar]
Moodie 1986 {published data only}
- Moodie NB, Brisbin J, Morgan AMG. Subluxation of the glenoidhumeral joint in hemiplegia: evaluation of supportive devices. Physiotherapy Canada 1986;38:151‐7. [Google Scholar]
Morin 1997 {published data only}
- Morin L, Bravo G. Strapping the hemiplegic shoulder: a radiographic evaluation of its efficacy to reduce subluxation. Physiotherapy Canada 1997;49:103‐8. [Google Scholar]
Patterson 1984 {published data only}
- Patterson JR, Zabransky R, Grabois M, Ferro P. Evaluation of the effectiveness of sling orthoses for the correction of glenohumeral subluxation in the hemiplegic. Archives of Physical Medicine & Rehabilitation 1984;65:635. [Google Scholar]
Peters 2003 {published data only}
- Peters SB, Lee GP. Functional impact of shoulder taping in the hemiplegic upper extremity. Occupational Therapy in Health Care 2003;17(2):35‐46. [DOI] [PubMed] [Google Scholar]
Rajaram 1985 {published data only}
- Rajaram V, Holtz M. Shoulder forearm support for the subluxed shoulder. Archives of Physical Medicine & Rehabilitation 1985;66:191‐2. [PubMed] [Google Scholar]
Roy 1989 {published data only}
- Roy CW, Blamire JG. The function shoulder orthosis in hemiplegic shoulder subluxation: a pilot study. Clinical Rehabilitation 1989;3:107‐9. [Google Scholar]
Sodring 1980 {published data only}
- Sodring KM. Upper extremity orthoses for stroke patients. International Journal of Rehabilitation Research 1980;3:33‐8. [DOI] [PubMed] [Google Scholar]
Spaulding 1999 {published data only}
- Spaulding SJ. Biomechanical analysis of four supports for the subluxed hemiparetic shoulder. Canadian Journal of Occupational Therapy 1999;66:169‐75. [DOI] [PubMed] [Google Scholar]
Sullivan 1989 {published data only}
- Sullivan BE, Rogers SL. Modified Bobath sling with distal support. American Journal of Occupational Therapy 1989;43:47‐9. [DOI] [PubMed] [Google Scholar]
Walker 1983 {published data only}
- Walker J. Modified strapping of roll sling. American Journal of Occupational Therapy 1983;37:110‐1. [DOI] [PubMed] [Google Scholar]
Williams 1988 {published data only}
- Williams R, Taffs L, Minuk T. Evaluation of two support methods for the subluxated shoulder of hemiplegic patients. Physical Therapy 1988;68:1209‐14. [PubMed] [Google Scholar]
Zorowitz 1995 {published data only}
- Idank DM, Zorowitz RD, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a pilot study comparing four slings. Archives of Physical Medicine and Rehabilitation 1993;74:1235. [DOI] [PubMed] [Google Scholar]
- Zorowitz RD, Idank D, Ikai T, Hughes MB, Johnston MV. Shoulder subluxation after stroke: a comparison of four supports. Archives of Physical Medicine & Rehabilitation 1995;76:763‐71. [Idank 1993] [DOI] [PubMed] [Google Scholar]
Zorowitz 1996 {published data only}
- Zorowitz RD, Hughes MB, Idank D, Ikai T, Johnston MV. Shoulder pain and subluxation after stroke: correlation or coincidence?. American Journal of Occupational Therapy 1996;50:194‐201. [DOI] [PubMed] [Google Scholar]
Zorowitz 2001 {published data only}
- Zorowitz RD. Recovery patterns of shoulder subluxation after stroke: a six‐month follow‐up study. Topics in Stroke Rehabilitation 2001;8:1‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Ada 2002
- Ada L, Foongchomcheay A. Efficacy of electrical stimulation in preventing or reducing subluxation of the shoulder after stroke: A meta‐analysis. Australian Journal of Physiotherapy 2002;48:257‐67. [DOI] [PubMed] [Google Scholar]
Ada 2004
Bohannon 1986
- Bohannon R, LeFort A. Hemiplegic shoulder pain measured with the Ritchie Articluar Index. International Journal Rehabilitation Research 1986;9:379‐81. [Google Scholar]
Bohannon 1990
- Bohannon RW, Andrews AW. Shoulder subluxation and pain in stroke patients. American Journal of Occupational Therapy 1990;44:507‐9. [DOI] [PubMed] [Google Scholar]
Cailliet 1980
- Cailliet R. The shoulder in hemiplegia. Philadephia: FA Davis Company, 1980:89‐106. [Google Scholar]
Carr 1985
- Carr JH, Shepherd RB, Nordholm L, Lynne D. Investigation of a new motor assessment scale for stroke patients. Physical Therapy 1985;65:175‐80. [DOI] [PubMed] [Google Scholar]
Chaco 1971
- Chaco J, Wolf E. Subluxation of the glenohumeral joint in hemiplegia. American Journal of Physical Medicine 1971;50:139‐43. [PubMed] [Google Scholar]
Chino 1981
- Chino N. Electrophysiological investigation on shoulder subluxation in hemiplegics. Scandinavian Journal of Rehabilitation Medicine 1981;13:17‐21. [PubMed] [Google Scholar]
Dursun 2000
- Durson E, Dursun N, Ural CE, Cakci A. Glenohumeral joint subluxation and reflex sympathetic dystrophy in hemiplegic patients. Archives of Physical Medicine & Rehabilitaiton 2000;81:944‐6. [DOI] [PubMed] [Google Scholar]
Linn 1999
- Linn SL, Granat MH, Lee KR. Prevention of shoulder subluxation after stroke with electrical stimulation. Stroke 1999;30(5):963‐8. [DOI] [PubMed] [Google Scholar]
Miglietta 1959
- Miglietta O, Lewitan A, Rogoff JB. Subluxation of the shoulder in hemiplegic patients. New York State Journal of Medicine 1959;1:457‐60. [PubMed] [Google Scholar]
Moseley 2002
- Moseley AM, Herbert R, Sherrington C, Maher C. Evidence for physiotherapy practice: A survey of the Physiotherapy Evidence Database (PEDro). Australian Journal of Physiotherapy 2002;48:43‐9. [DOI] [PubMed] [Google Scholar]
Moskowitz 1969
- Moskowitz H, Goodman CR, Smith E, Balthazar E, Mellins HZ. Hemiplegic shoulder. New York State Journal of Medicine 1969;15:548‐50. [PubMed] [Google Scholar]
Najenson 1971
- Najenson T, Yacubovich E, Pikielni SS. Rotator cuff injury in shoulder joints of hemiplegic patients. Scandinavian Journal of Rehabilitation Medicine 1971;3:131‐7. [PubMed] [Google Scholar]
PEDro
- Centre for Evidence‐Based Physiotherapy. The Physiotherapy Evidence Database (PEDro). http://www.pedro.fhs.usyd.edu.au (accessed 21 August 2002).
Shai 1984
- Shai G, Ring H, Costeff H, Solzi P. Glenohumeral malalignment in the hemiplegic shoulder: an early radiologic sign. Scandinavian Journal of Rehabilitation Medicine 1984;16:133‐6. [PubMed] [Google Scholar]
Smith 1982
- Smith RG, Cruikshank JG, Dunbar S, Akhtar AJ. Malalignment of the shoulder after stroke. British Medical Journal Clinical Research Ed 1982;284:1224‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Langenberghe 1988
- Langenberghe HVK, Hogan BM. Degree of pain and grade of subluxation in the painful hemiplegic shoulder. Scandinavian Journal of Rehabilitation Medicine 1998;20:161‐6. [PubMed] [Google Scholar]
Verhagen 1998
- Verhagen AP, Vet HC, Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology 1998;51(12):1235‐41. [DOI] [PubMed] [Google Scholar]