Abstract
Background:
There is no general consensus on the normal and pathological values for the posterior tibial slope (PTS).
Purpose/Hypothesis:
The primary aim of this study was to determine standard values for the PTS in healthy participants using 3-dimensional (3D) computed tomography (CT). A secondary aim was to determine the effect of demographic factors and coronal-plane lower limb alignment on the PTS measurement. The hypothesis was that the PTS would be significantly influenced by demographic factors and coronal-plane lower limb alignment.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A CT-based modeling and analytics system was used to examine and measure lower limb alignment and the PTS in 378 patients (193 male and 185 female; mean age, 58.3 ± 16.4 years [range, 18-92 years]; mean body mass index, 25.0 ± 4.4 kg/m2). The lateral, medial, and global PTS were measured for each patient. All measurements were constructed using algorithm-calculated landmarks, resulting in reproducible and consistent constructs for each specimen. The results were then evaluated based on ethnicity, sex, and hip-knee-ankle (HKA) angle.
Results:
The study population comprised 219 white and 159 Asian participants. The mean global, medial, and lateral PTS were 6.3° (range, –5.5° to 14.7°; 1% with ≥12°), 6.2° (range, –4.1° to 17.2°; 3% with ≥12°), and 5.3° (range, –4.7° to 16.2°; 2% with ≥12°), respectively. The lateral (Δ = –1.0° [95% CI, 0.6°-1.6°]; P < .0001) and global (Δ = –0.5° [95% CI, 0.0°-0.8°]; P = .0332) PTS were smaller in the female subpopulation. The global PTS was greater (Δ = 1.9° [95% CI, 1.5°-2.3°]; P < .0001) in the Asian subpopulation. The mean HKA angle was 179.6° (range, 170°-190°). The HKA angle was significantly correlated with the medial and global PTS. Specimens with a genu varum knee exhibited a significantly greater global (Δ = 1.2° [95% CI, 0.8°-1.7°]; P < .0001) and medial (Δ = 1.9° [95% CI, 1.3°-2.5°]; P < .0001) PTS.
Conclusion:
The present study gives a benchmark for the physiological values of the PTS in a healthy population and highlights several factors influencing the PTS, such as ethnicity, sex, and alignment. Anatomic variants with a PTS ≥12° were very uncommon (≤3%) in our Asian and white groups and thus could be considered as pathological. The PTS is a crucial anatomic factor for anterior cruciate ligament injuries and reconstruction. A general consensus is lacking regarding the cutoff for abnormal values, thus guiding standard of care. This study investigated the dispersion of global, medial, and lateral posterior plateau tibial angles in a large population representing a range of demographic diversity.
Keywords: tibial slope, anatomy, ACL injury, total knee replacement, morphometric study
The measurement of the posterior tibial slope (PTS) has been widely studied for its causal relationship to tibial translation,8 knee joint stability,20 and anterior cruciate ligament (ACL) injuries.30 While considerable research has been devoted toward exploring the former anatomic morphological characteristics,29 the PTS has only recently gained attention as an anatomic predictor of ACL tears. An increased PTS (≥12°) has been shown to be a risk factor for ACL ruptures2 and failure of ACL reconstruction31; because of this, some authors7,28 advocate performing osteotomy to correct the PTS after several failures of ACL reconstruction. However, data currently remain limited to support this approach.19,20,33,36
Numerous methods have been described for the PTS estimation,14,17 taking into account a number of different anatomic axes.3,9,35 Previous studies evaluated PTS values using radiography,32 computed tomography (CT),37 and magnetic resonance imaging.12 Despite the current availability of imaging modalities, the reliability and accuracy of PTS measurements reported in the literature are limited by the use of ex vivo analysis, inadequate sample sizes, or bias related to rotation of the lower limb on radiographic evaluations.14
Moreover, normative population statistics and demographics regarding the PTS have been sparsely documented. Weinberg et al,32 using a 3-dimensional (3D) digitizer apparatus, reported that the mean medial PTS was 6.9° ± 3.7°, which was greater than the mean lateral PTS of 4.7° ± 3.6° (P < .001), in 545 cadaveric specimens. Important sex- and race-based differences existing in the PTS were equally shown by their results.32 Women had higher values of the PTS compared with men: the medial slope was 7.5° ± 3.8° in the female group compared with 6.8° ± 3.7° in the male group, and the lateral slope was 5.2° ± 3.5° in the female group compared with 4.6° ± 3.5° in the male group. The group including black specimens had a greater mean medial slope of 8.7° ± 3.6° versus 5.8° ± 3.3° and a lateral slope of 5.9° ± 3.3° versus 3.8° ± 3.5° than white specimens.
The principal aim of this study was to determine standard values for the PTS in healthy participants using a reliable 3D CT method. The secondary aim was to determine the effect of demographic disparity and coronal-plane lower limb alignment. The hypothesis was that the PTS would be significantly influenced by demographic factors and lower limb alignment.
Methods
A CT-based modeling and analytics system (SOMA; Stryker) composed of scans of more than 19,000 bone segments was used for this institutional review board–approved study. These CT scans were originally obtained to explore vascular diseases or polytrauma in patients without orthopaedic clinical data. Using this system, the pelvis, bilateral femora, bilateral tibiae, and patellae of 378 patients (193 male and 185 female; mean age, 58.3 ± 16.4 years [range, 18-92 years]; mean body mass index, 25.0 ± 4.4 kg/m2) representing white (n = 219) and Asian (n = 159) participants were examined. The population characteristics are displayed in Table 1. CT scan selection was performed after radiographic inspection to rule out bone and joint anomalies, specimens with signs of osteoarthritis, bone deformities, or evidence of previous surgery. Patients with any of these anomalies were excluded from the study.
Table 1.
Population Characteristicsa
| Side, n (%) | |
| Right knee | 378 (50.0) |
| Left knee | 378 (50.0) |
| Ethnicity, n (%) | |
| White | 438 (57.9) |
| Asian | 318 (42.1) |
| Sex, n (%) | |
| Male | 386 (51.1) |
| Female | 370 (48.9) |
| Age, y | 58.3 (18-92) |
| Height, cm | 166.5 (140-189) |
| Weight, kg | 69.7 (39-110) |
| Body mass index, kg/m2 | 25.0 (15-41) |
| HKA angle, deg | 179.6 (170-190) |
aValues are reported as mean (range) unless otherwise indicated. HKA, hip-knee-ankle.
The posterior plateau tibial angle (PPTA) and hip-knee-ankle (HKA) angle4 were calculated for each patient and each knee. A total of 3 different estimations of the PTS were performed: the lateral PPTA (LPPTA), the medial PPTA (MPPTA), and the global PPTA (GPPTA)9 (Figure 1). All measurements were constructed using algorithm-calculated landmarks on the corresponding bone, which were then mapped to each chosen bone from the database. This resulted in reproducible and consistent constructs for each specimen. Previous accuracy and reproducibility analysis estimated that this system allows automated measurements of upper femoral anatomy with a margin of error of <2 mm and <1°.26
Figure 1.
Measurement method of the posterior tibial slope. (A) Mapping of the lateral plateau in the axial view. (B) Mapping of the lateral plateau in the coronal view. (C) Measurement of the global posterior tibial slope.
To define the HKA angle, the femoral and tibial mechanical axis landmarks were selected from the predefined landmarks available. These axes were defined from the knee center to the femoral head center and ankle center, respectively. The mechanical axis was then projected onto the coronal plane, and the angle between both axes was determined. Genu varum was considered for an HKA angle <178°, and genu valgum was considered for an HKA angle >182°.
A global proximal tibial plane was then created by fitting 35 points over the medial and lateral tibial plateaus. The intersection of the global proximal tibial plane and the sagittal plane defined the global sagittal tibial axis. The posterior angle between the global sagittal tibial axis and the tibial mechanical axis in the sagittal plane was determined as the GPPTA. Similarly, the lateral proximal tibial plane and medial proximal tibial plane were created by fitting 15 points over the lateral and medial articular surfaces, respectively. The intersection of each plane with the sagittal axis was established to determine the medial sagittal tibial axis and the lateral sagittal tibial axis. The posterior angle between each axis and the tibial mechanical axis in the sagittal plane was determined as the MPPTA and LPPTA, respectively.
Statistical Analysis
Means, standard deviations, and ranges were determined for each of the measurements made for the population as a whole and for various subpopulations based on sex, ethnicity, and mechanical axis values. Normal (Gaussian) distributions of different parameters of interest were determined. Univariate analysis was performed using t tests. Pearson product moment correlation coefficients were calculated to examine correlations among specimen demographic data and radiographic measurements. Multiple linear regression models were developed to establish the determinants for each of the variables that defined a difference between groups and subgroups. For each model, variables with a P value <.1 were kept in the final model. The sample size was calculated for a required level of statistical significance of α = .05 and a power of 1 – β = 0.95; in addition, 46 tibias would be required to detect >2° ± 3.5° between groups and/or subgroups, as Yoo et al35 examined 90 knees and found an average PTS of 10.6° ± 3.5°. A trained statistician performed statistical analysis using SPSS software (Version 22; IBM). All calculations assumed 2-tailed distributions.
Results
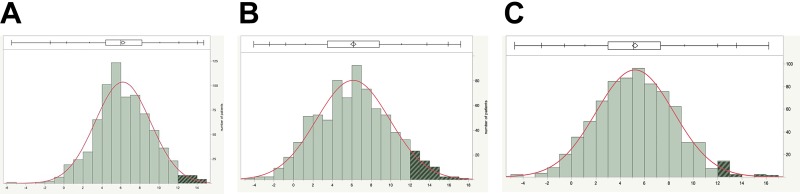
The mean global, medial, and lateral PTS were 6.3° (range, –5.5° to 14.7°), 6.2° (range, –4.1° to 17.2°), and 5.3° (range, –4.7° to 16.2°), respectively. Only a small percentage of measurements were ≥12°: 1% of global PTS, 3% of medial PTS, and 2% of lateral PTS. The mean MPPTA was significantly higher than the mean LPPTA (Δ = 0.9° [95% CI, 0.5° to 1.2°]; P < .0001). Results of the mean angles are displayed in Table 2 and depicted in Figure 2.
Table 2.
Posterior Tibial Slope According to Sex and Ethnicitya
| Overall | Sex | Ethnicity | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | P Value | White | Asian | P Value | ||
| GPPTA | 6.3 (–5.5 to 14.7) | 6.0 (5.8 to 6.3) | 6.5 (6.2 to 6.8) | .0332 | 5.4 (5.2 to 5.6) | 7.3 (7.0 to 7.6) | <.0001 |
| MPPTA | 6.2 (–4.1 to 17.2) | 6.3 (6.0 to 6.7) | 6.0 (5.6 to 6.4) | .27 | 4.8 (4.5 to 5.1) | 8.0 (7.6 to 8.4) | .0001 |
| LPPTA | 5.3 (–4.7 to 16.2) | 4.8 (4.5 to 5.1) | 5.8 (5.4 to 6.1) | <.0001 | 5.1 (4.8 to 5.4) | 5.4 (5.0 to 5.7) | .2 |
aValues are reported as mean (range) in degrees. Bolded P values indicate a statistically significant difference. GPPTA, global posterior plateau tibial angle; LPPTA, lateral posterior plateau tibial angle; MPPTA, medial posterior plateau tibial angle.
Figure 2.
Dispersion of posterior tibial slope values. (A) Global posterior plateau tibial angle. (B) Medial posterior plateau tibial angle. (C) Lateral posterior plateau tibial angle.
The white group exhibited a significantly lower GPPTA compared with the Asian group (Δ = –1.9° [95% CI, 1.5° to 2.3°]; P < .0001). While the MPPTA was significantly lower in the white versus Asian group (Δ = –3.2° [95% CI, 2.7° to 3.7°]; P < .0001), no significant difference related to the LPPTA (Δ = –0.3° [95% CI, –0.2° to 0.8°]; P = .2) was found. The male group showed a significantly greater GPPTA (Δ = 0.5° [95% CI, 0.0° to 0.8°]; P = .0332) and LPPTA (Δ = 1.0° [95% CI, 0.6° to 1.6°]; P < .0001) related to the female group. Laterality did not show any significant difference between the left and right knees: MPPTA (Δ = 0.0° [95% CI, –0.5° to 0.6°]; P = .895) and LPPTA (Δ = 0.4° [95% CI, –0.1° to 0.8°]; P = .09).
The HKA angle significantly influenced the GPPTA and MPPTA (Table 3). While genu varum knees (HKA angle <178°) were associated with a significant increase in the GPPTA (Δ = 1.2° [95% CI, 0.8° to 1.7°]; P < .0001) and MPPTA (Δ = 1.9° [95% CI, 1.3° to 2.5°]; P < .0001), genu valgum knees (HKA angle >182°) were associated with a decrease in the GPPTA (Δ = –0.7° [95% CI, 0.2° to 1.2°]; P = .0067) and MPPTA (Δ = –1.6° [95% CI, 1.0° to 2.3°]; P < .0001) (both compared with neutrally aligned knees).
Table 3.
Posterior Tibial Slope According to Alignmenta
| Genu Neutral | Genu Varum | P | Genu Valgum | P | |
|---|---|---|---|---|---|
| GPPTA | 6.1 (5.8-6.3) | 7.3 (6.9-7.7) | <.0001 | 5.4 (4.9-5.8) | .0067 |
| MPPTA | 6.0 (5.7-6.4) | 7.9 (7.4-8.4) | <.0001 | 4.4 (3.9-4.9) | <.0001 |
| LPPTA | 5.1 (4.7-5.4) | 5.5 (5.1-5.9) | .105 | 5.6 (5.1-6.0) | .0742 |
aValues are reported as mean (range) in degrees. Bolded P values indicate a statistical significance compared with genu neutral. GPPTA, global posterior plateau tibial angle; LPPTA, lateral posterior plateau tibial angle; MPPTA, medial posterior plateau tibial angle.
The multivariate analysis found that the GPPTA was correlated significantly with ethnicity (R 2 = 0.330 [95% CI, 0.266 to 0.392]; P < .0001), sex (R 2 = 0.077 [95% CI, 0.006 to 0.146]; P = .0332), and lower limb alignment (R 2 = –0.277 [95% CI, –0.341 to –0.277]; P < .0001).
This analysis confirmed that the MPPTA was correlated with ethnicity (R 2 = 0.395 [95% CI, 0.334 to 0.452]; P < .0001) and lower limb alignment (R 2 = –0.368 [95% CI, –0.427 to 0.306]; P < .0001), while the LPPTA was correlated with ethnicity (R 2 = 0.111 [95% CI, 0.041 to 0.179]; P = .002) and sex (R 2 = 0.156 [95% CI, 0.087 to 0.224]; P < .0001). Results of the multivariate analysis are displayed in Table 4.
Table 4.
Multivariate Analysis Concerning Ethnicity, Sex, Alignment, and Posterior Tibial Slopea
| Correlation Coefficient (R 2) | 95% CI | P | |
|---|---|---|---|
| GPPTA | |||
| Ethnicity | 0.330 | 0.266 to 0.392 | <.0001 |
| Sex | 0.077 | 0.006 to 0.146 | .0332 |
| HKA angle | –0.277 | –0.341 to –0.277 | <.0001 |
| MPPTA | |||
| Ethnicity | 0.395 | 0.334 to 0.452 | <.0001 |
| Sex | –0.0390 | –0.109 to 0.031 | .2769 |
| HKA angle | –0.368 | –0.427 to 0.306 | <.0001 |
| LPPTA | |||
| Ethnicity | 0.111 | 0.041 to 0.179 | .002 |
| Sex | 0.156 | 0.087 to 0.224 | <.0001 |
| HKA angle | –0.0018 | –0.072 to 0.068 | .9603 |
aBolded P values indicate a statistical significance. GPPTA, global posterior plateau tibial angle; HKA, hip-knee-ankle; LPPTA, lateral posterior plateau tibial angle; MPPTA, medial posterior plateau tibial angle.
Discussion
The present study confirmed our initial hypothesis and demonstrated that the PTS is significantly influenced by sex, ethnicity, and lower limb alignment. An estimation of the PTS was performed for a healthy population representing a range of demographic parameters (ethnicity, sex, and age) and lower limb alignment specificities. The mean GPPTA was 6.3° (range, –5.5° to 14.7°). The mean MPPTA (6.2° [range, –4.1° to 17.2°]) was significantly greater than the mean LPPTA (5.3° [range, –4.7° to 16.2°]) (Δ = 1.1° [95% CI, 0.5 to 1.2]; P < .0001). Our mean values for the global, medial, and lateral PTS were similar to those in previously published series32; we also noticed some important differences in comparison with other published series17 (Table 5). The explanations for these can be summarized as follows.
Table 5.
Posterior Tibial Slope Reported in the Literaturea
| Author (Year) | Population | Knee Disorder | Average Age, y | Imaging Technology | No. of Knees | Average MPPTA, deg | Average LPPTA, deg | Average GPPTA, deg | Tibial Reference Axis |
|---|---|---|---|---|---|---|---|---|---|
| Current study (2020) | White, Asian | None | 58 | CT | 756 | 6.2 ± 3.7 | 5.3 ± 3.2 | 6.3 ± 2.9 | Anatomic axis |
| Weinberg32 (2017) | Cadaveric: black, white | None | NR | 3D digitizer apparatus | 1090 | 6.9 ± 3.7 | 4.7 ± 3.6 | NR | Center of the first third of the tibial shaft |
| Zhang37 (2014) | Chinese | None | 31 | CT | 80 | 8.4 ± 3.1 | 7.6 ± 2.5 | NR | Proximal long axis, anterior cortices, posterior cortices |
| Mohanty23 (2013) | Indian | OA | 62 | Radiography | 100 | NR | NR | 11.6 ± 4.5 | Anatomic axis |
| Haddad10 (2012) | White, African, Asian | Soft tissue injury | 42 | MRI | 148 | 5.7 ± 3.8 | 5.6 ± 4.2 | NR | Tibial proximal anatomic axis |
| de Boer (2009)6 | Cadaveric: African, white, mixed | None | 56 | Handmade measurements | 105 | NR | NR | 8.4 ± 3.7 | Tibial shaft anatomic axis |
| Yoo35 (2008) | Korean (female) | OA | 67 | Radiography | 90 | NR | NR | 10.6 ± 3.5 | Anterior cortical line, proximal anatomic axis, central anatomic axis, posterior cortical line, fibular shaft axis |
| Kuwano17 (2005) | Japanese | OA | 71 | CT | 50 | 9.0 ± 5.0 | 8.1 ± 4.0 | NR | Longitudinal axis of the tibial shaft |
| Chiu5 (2000) | Cadaveric: Chinese | Healthy/OA | 68 | Radiography | 50 | 14.8 ± 4.2 | 11.8 ± 3.8 | NR | Anterior cortex |
a3D, 3-dimensional; CT, computed tomography; GPPTA, global posterior plateau tibial angle; LPPTA, lateral posterior plateau tibial angle; MPPTA, medial posterior plateau tibial angle; MRI, magnetic resonance imaging; NR, not reported; OA, osteoarthritis.
First, the PTS is deeply influenced by degenerative changes within the measured knees: Han et al11 reported greater PTS values with a mean MPPTA and LPPTA of 10.0° (range, 6.7°-13.3°) and 8.4° (range, 4.6°-12.2°), respectively. The authors11 evaluated 133 knees using preoperative CT for patients undergoing total knee arthroplasty (TKA) for osteoarthritis and concluded that PTS measurements were deeply influenced by degenerative changes. Mohanty et al23 evaluated the PTS value in a cohort of 100 Indian patients undergoing TKA. The global PTS was 11.6° (range, 2°-25°). In another study, Yoo et al35 described several ways of measuring the PTS in 90 knees (66 females) with osteoarthritis. The average global PTS in their series was 10.6° (range, 1.9°-19.6°). The values reported by Kuwano et al17 were similar to the ones reported by Han et al11: in a study including 50 knees for 32 patients, they found a mean MPPTA of 9.0° ± 5.0° and a mean LPPTA of 8.1° ± 4.0°. To clarify the difference between the slopes of healthy patients and the ones with osteoarthritis, Chiu et al5 compared 25 pairs of knees from Chinese cadaveric specimens. They found an average PTS of 13.1° ± 4.0° in the osteoarthritis group and 10.8° ± 3.5° in the nonosteoarthritis group. Another study performed by Meric et al22 included 13,546 CT scans of patients undergoing TKA, for whom they measured the global PTS. Their average finding was 7.2° ± 3.7°; this value comes close to our results, but 35% of their patients were outliers: 11.6% with <4° and 19.1% with >10°. This dispersion is different in our results and is most probably due to osteoarthritic changes in the knees before TKA.
Second, the radiographic evaluation of the PTS is biased by tibial and femoral positioning. Kiapour et al16 explained in their study that the radiography-based PTS estimation must account for knee flexion and thus the corresponding tibial rotation that occurs during the “screw-home” mechanism. Kessler et al14,15 showed that any rotation decreases horizontal displacement without influencing vertical displacement. Only perfect neutral axial rotation allows a reliable PTS value to be measured.29 The radiographic evaluation of the PTS, especially when the degrees of knee flexion and tilt are not considered, does not provide accurate and reproducible results.34
All these observations suggest that only anatomic landmarks, positioned over 3D bone models from a healthy population (without degenerative changes), are able to provide accurate and reliable PTS values. This position is confirmed by Amirtharaj et al,1 who performed measurements of the PTS on a new 3D model based on CT. They found an intraclass correlation coefficient of 0.999 for intraobserver reliability and 0.998 for interobserver reliability.
We found that the lateral and global PTS were significantly influenced by sex according to multivariate statistical analysis, with a decreased LPPTA and GPPTA in the female group. This is in line with trends observed in a previous study.13 Although Todd et al30 found an increased global PTS in female specimens with ACL ruptures, 9.8° ± 2.6° compared with 8.2° ± 2.4° in the noninjury group, they found no significant differences when comparing healthy men and women. This is probably because of the young age of their population: 24.9 ± 7.9 years. Weinberg et al32 demonstrated that women had a greater medial and lateral PTS when compared with men. The difference with our study could be that their measures were based on cadaveric bones. In the present study, univariate comparative analyses found a difference of <2° for lateral (1.0°) and global (0.5°) PTS according to sex.
The present study also showed that ethnicity was an independent predictor of the PTS. We confirmed that the white group exhibited a significantly decreased medial (P = .0001) and global (P < .0001) PTS compared with the Asian group.10 However, while the mean values reported in the literature demonstrated not so dissimilar medial PTS values for our Asian and white groups, other authors have reported a wide range of values for the lateral PTS, especially in the Asian population.17,35,37
Coronal-plane lower limb alignment was an independent factor of medial and global PTS values (P < .0001). The medial PTS was significantly decreased in genu valgum knees (4.4° MPPTA), while they were significantly increased in genu varum knees (7.9° MPPTA and 7.3° GPPTA) when compared with neutrally aligned knees. However, a difference of <2° in the medial or global PTS was reported according to coronal-plane lower limb alignment (genu varum or valgum). Puthumanapully et al24 reported a significant increase in the global PTS (3.5°) in genu valgum (P = .001) when considering 46 patients, even though their measurements might have been influenced by degenerative changes. Matsuda et al21 in 1999 compared 30 normally aligned lower limbs and 30 genu varum samples. They found an average medial PTS of 10.7° (range, 5°-15.5°) in healthy knees and 9.9° (range, 1.5°-19°) in genu varum knees. The lateral PTS was 7.2° (range, 0°-14.5°) in healthy knees and 6° (range, 1°-13°) in genu varum knees. Unfortunately, these differences were not statistically significant probably because of the lack of power in their statistical analysis.
This study has several limitations: foremost, its retrospective design did not allow us to assess limb dominance and activity level, factors that could potentially be correlated with the PTS. We only included participants without clear radiographic evidence of bony abnormalities, and our population did not represent the majority of patients requiring knee surgery, such as TKA or high tibial osteotomy. On the other hand, patients with knees with bony deformities, disease, previous surgery, or surgical hardware were excluded, as minor osteoarthritic or dysplastic abnormalities may have altered the bony anatomy. Methods of estimating the PTS are controversial and not consistent. The long anatomic axis of the tibia was used in our study,3,37 as in the studies of Kuwano et al17 and Mohanty et al.23 However, Weinberg et al32 took for reference the center of the first third of the tibial shaft, and Han et al11 published results with 4 different axes: mechanical axis, anatomic axis, anterior cortices, and fibular shaft axis. Yoo et al35 highlighted the wide difference of the PTS according to the chosen axis: anterior cortices (13.8°), proximal anatomic axis (10.8°), central anatomic axis (12.9°), posterior cortices (7.8°), and fibular shaft (9.5°). A comparison with other series needs to consider the fact that CT measurements could not be compared with radiographic measurements. Furthermore, we cannot comment on potential clinical consequences of PTS differences related to demographic factors and/or lower limb alignment because the risk of ACL injuries is a multifactorial issue and a detailed risk model incorporating other risk factors (eg, ligamentous laxity, hormone levels, quadriceps strength, and femoral notch anatomy) is most appropriate to determine the clinical importance of anatomic variations among race, sex, and mechanical axis deviation of the lower limbs.27 Finally, in our study, only white and Asian populations were studied; it might be interesting to enlarge this study to other ethnic groups.
Taking into account the limitations previously stated, the clinical relevance of our results should be considered in the controversy of the influence of the PTS on reruptures after ACL reconstruction. Lee et al18 recently reported on a series of 64 ACL reruptures at 37 months of follow-up compared with a control group of 64 ACL reconstruction procedures without reruptures. The average PTS in the rerupture group was 13.2° ± 2.5° (range, 8.5°-18.2°) compared with 10.9° ± 3.1° (range, 4.9°-13.6°) in the control group. The odds ratio of an ACL rerupture was 4.52 when the PTS was ≥12°. These values lead to the question of whether to perform high tibial osteotomy to correct the PTS in cases of reruptures, as made by Sonnery-Cottet et al28 and Dejour et al.7 To perform corrective slope-changing surgery, a cutoff value defining an abnormal PTS is needed. Schillhammer,25 in his most recent editorial commentary, challenged the “12° rule” recently proposed by some authors.1,18,35 In our series, only 1% (GPPTA) to 3% (MPPTA) of our participants exhibited a PTS value ≥12°, illustrating that this anatomic variant is very uncommon in the Asian and white populations.
Conclusion
The present study gives a benchmark for the physiological values of the PTS in a healthy population and highlights several factors influencing the PTS, such as ethnicity, sex, and alignment. Anatomic variants with a PTS ≥12° were very uncommon (≤3%) in our Asian and white groups and thus could be considered as pathological.
Footnotes
Final revision submitted September 23, 2019; accepted October 1, 2019.
One or more of the authors declared the following potential conflict of interest or source of funding: S.L., P.W., and A.F. are employees of Stryker. M.O. has received consulting fees from Arthrex, Newclip Technics, and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Assistance Publique–Hôpitaux de Marseille (approval No. 2018-12-234).
References
- 1. Amirtharaj MJ, Hardy BM, Kent RN, et al. Automated, accurate, and three-dimensional method for calculating sagittal slope of the tibial plateau. J Biomech. 2018;79:212–217. [DOI] [PubMed] [Google Scholar]
- 2. Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22(8):894–899. [DOI] [PubMed] [Google Scholar]
- 3. Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. [Evaluation of methods for radiographic measurement of the tibial slope: a study of 83 healthy knees]. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200. [PubMed] [Google Scholar]
- 4. Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am. 1994;25(3):379–386. [PubMed] [Google Scholar]
- 5. Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15(2):224–227. [DOI] [PubMed] [Google Scholar]
- 6. de Boer JJ, Blankevoort L, Kingma I, Vorster W. In vitro study of inter-individual variation in posterior slope in the knee joint. Clin Biomech (Bristol Avon). 2009;24(6):488–492. [DOI] [PubMed] [Google Scholar]
- 7. Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2846–2852. [DOI] [PubMed] [Google Scholar]
- 8. Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–749. [PubMed] [Google Scholar]
- 9. Genin P, Weill G, Julliard R. [The tibial slope: proposal for a measurement method]. J Radiol. 1993;74(1):27–33. [PubMed] [Google Scholar]
- 10. Haddad B, Konan S, Mannan K, Scott G. Evaluation of the posterior tibial slope on MR images in different population groups using the tibial proximal anatomical axis. Acta Orthop Belg. 2012;78(6):757–763. [PubMed] [Google Scholar]
- 11. Han HS, Chang CB, Seong SC, Lee S, Lee MC. Evaluation of anatomic references for tibial sagittal alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2008;16(4):373–377. [DOI] [PubMed] [Google Scholar]
- 12. Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kessler MA, Burkart A, Martinek V, Beer A, Imhoff AB. [Development of a 3-dimensional method to determine the tibial slope with multislice-CT]. Z Orthop Ihre Grenzgeb. 2003;141(2):143–147. [DOI] [PubMed] [Google Scholar]
- 15. Kessler OC, Jacob HAC, Romero J. Avoidance of medial cortical fracture in high tibial osteotomy: improved technique. Clin Orthop Relat Res. 2002;(395):180–185. [DOI] [PubMed] [Google Scholar]
- 16. Kiapour AM, Kiapour A, Goel VK, et al. Uni-directional coupling between tibiofemoral frontal and axial plane rotation supports valgus collapse mechanism of ACL injury. J Biomech. 2015;48(10):1745–1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kuwano T, Urabe K, Miura H, et al. Importance of the lateral anatomic tibial slope as a guide to the tibial cut in total knee arthroplasty in Japanese patients. J Orthop Sci. 2005;10(1):42–47. [DOI] [PubMed] [Google Scholar]
- 18. Lee CC, Youm YS, Cho SD, et al. Does posterior tibial slope affect graft rupture following anterior cruciate ligament reconstruction? Arthroscopy. 2018;34(7):2152–2155. [DOI] [PubMed] [Google Scholar]
- 19. Lee YS, Moon GH. Comparative analysis of osteotomy accuracy between the conventional and devised technique using a protective cutting system in medial open-wedge high tibial osteotomy. J Orthop Sci. 2015;20(1):129–136. [DOI] [PubMed] [Google Scholar]
- 20. Marriott K, Birmingham TB, Kean CO, Hui C, Jenkyn TR, Giffin JR. Five-year changes in gait biomechanics after concomitant high tibial osteotomy and ACL reconstruction in patients with medial knee osteoarthritis. Am J Sports Med. 2015;43(9):2277–2285. [DOI] [PubMed] [Google Scholar]
- 21. Matsuda S, Miura H, Nagamine R, et al. Posterior tibial slope in the normal and varus knee. Am J Knee Surg. 1999;12(3):165–168. [PubMed] [Google Scholar]
- 22. Meric G, Gracitelli GC, Aram L, Swank M, Bugbee WD. Tibial slope is highly variable in patients undergoing primary total knee arthroplasty: analysis of 13,546 computed tomography scans. J Arthroplasty. 2015;30(7):1228–1232. [DOI] [PubMed] [Google Scholar]
- 23. Mohanty SS, Rao NN, Dash KK, Bhosale SK. Correlation of posterior tibial slope with metaphysio-diaphyseal angle in total knee arthroplasty: a radiological study. Indian J Orthop. 2013;47(1):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Puthumanapully PK, Harris SJ, Leong A, Cobb JP, Amis AA, Jeffers J. A morphometric study of normal and varus knees. Knee Surg Sports Traumatol Arthrosc. 2014;22(12):2891–2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schillhammer C. Editorial commentary. Managing excessive posterior slope in anterior cruciate ligament reconstruction: where do we draw the line? Arthroscopy. 2018;34(7):2156–2157. [DOI] [PubMed] [Google Scholar]
- 26. Schmidt W, LiArno S, Khlopas A, Petersik A, Mont MA. Stryker Orthopaedic Modeling and Analytics (SOMA): a review. Surg Technol Int. 2018;32:315–324. [PubMed] [Google Scholar]
- 27. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature. Part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(1):69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sonnery-Cottet B, Mogos S, Thaunat M, et al. Proximal tibial anterior closing wedge osteotomy in repeat revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(8):1873–1880. [DOI] [PubMed] [Google Scholar]
- 29. Sturnick DR, Vacek PM, DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43(4):839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63–67. [DOI] [PubMed] [Google Scholar]
- 31. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 32. Weinberg DS, Williamson DFK, Gebhart JJ, Knapik DM, Voos JE. Differences in medial and lateral posterior tibial slope: an osteological review of 1090 tibiae comparing age, sex, and race. Am J Sports Med. 2017;45(1):106–113. [DOI] [PubMed] [Google Scholar]
- 33. Westermann RW, DeBerardino T, Amendola A. Minimizing alteration of posterior tibial slope during opening wedge high tibial osteotomy: a protocol with experimental validation in paired cadaveric knees. Iowa Orthop J. 2014;34:16–23. [PMC free article] [PubMed] [Google Scholar]
- 34. Yochum TR, Rowe LJ. Essentials of skeletal radiology. Radiology. 1987;243(2):348. [Google Scholar]
- 35. Yoo JH, Chang CB, Shin KS, Seong SC, Kim TK. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. J Arthroplasty. 2008;23(4):586–592. [DOI] [PubMed] [Google Scholar]
- 36. Zeng C, Yang T, Wu S, et al. Is posterior tibial slope associated with noncontact anterior cruciate ligament injury? Knee Surg Sports Traumatol Arthrosc. 2016;24(3):830–837. [DOI] [PubMed] [Google Scholar]
- 37. Zhang Y, Wang J, Xiao J, et al. Measurement and comparison of tibial posterior slope angle in different methods based on three-dimensional reconstruction. Knee. 2014;21(3):694–698. [DOI] [PubMed] [Google Scholar]