Abstract
Background
Selective beta‐adrenergic agonists for use in asthma are: short acting (2 to 6 hours) and long acting (> 12 hours). There has been little controversy about using short acting beta‐agonists intermittently, but long acting beta‐agonists are used regularly, and their regular use has been controversial.
Objectives
To determine the benefit or detriment of treatment with regular short‐ or long acting inhaled beta‐agonists in chronic asthma.
Search methods
We carried out a search using the Cochrane Airways Group trial register. We searched bibliographies of identified RCTs for additional relevant RCTs and contacted authors of identified RCTs for other published and unpublished studies.
Selection criteria
All randomised studies of at least two weeks duration, comparing a long acting inhaled beta‐agonist given twice daily with any short acting inhaled beta‐agonist of equivalent bronchodilator effectiveness given regularly in chronic asthma.
Data collection and analysis
Two reviewers performed data extraction and study quality assessment independently. We contacted authors of studies for missing data.
Main results
Thirty one studies met the inclusion criteria, 24 of parallel group and seven cross over design. Salmeterol xinafoate was used as long acting agent in 22 studies and formoterol fumarate in nine.
Salbutamol was the short acting agent used in 27 studies and terbutaline in five. The treatment period was over two weeks in 29 studies, and at least 12 weeks in 20.
25 studies permitted a variety of co‐intervention treatments, usually inhaled corticosteroid or cromones. One study did not permit inhaled corticosteroid.
Long acting beta‐agonists were significantly better than short acting for a variety of lung function measurements including morning highest forced expiratory flow measured with a peak flow meter (PEF) (Weighted Mean Difference (WMD) 33 L/min 95% CI 25 to 42) or evening PEF (WMD 26 L/min 95% CI 18 to 33); and had significantly lower scores for day and night time asthma symptom scores and percentage of days and nights without symptoms. They were also associated with a significantly lower use of rescue medication both during the day and night. Risk of exacerbations was not different between the two types of agent, but most studies were of short duration which limits the power to test for such differences.
Authors' conclusions
Long acting inhaled beta‐agonists have advantages across a wide range of physiological and clinical outcomes for regular treatment.
Plain language summary
Regular treatment with long acting beta agonists versus daily regular treatment with short acting beta agonists in adults and children with stable asthma
Patients with chronic asthma are generally treated with a 'preventer medication' to reduce the underlying airways inflammation but often require bronchodilators for their symptoms. Treatment with regular long acting Beta‐agonist bronchodilator agents, such as salmeterol (Serevent) or formoterol (Foradil, Oxis), leads to fewer asthma symptoms during the day and the night, less bronchodilator medication requirement for symptoms, better lung function measurements and better quality of life measurements compared to short acting Beta‐agonist bronchodilators such as salbutamol (Ventolin, Asmol, Airomir) or terbutaline (Bricanyl). There were no major adverse effects but there is little information on the effects in patients who do not use a 'preventer medication'.
Background
Asthma is a common respiratory disease among both adults and children (Pearce 2000), though there are large geographical differences in the prevalence of asthma (Janson 2001), and the prevalence is increasing in many countries. Estimates for asthma prevalence in 1990 varied from 8.5% in Australia to 4% in the USA and 3% in the United Kingdom (Sullivan 1996) and repeat estimates in Australia in 1999 (Woods 2001) gave rates for physician diagnosed asthma of 18% while 10% had used asthma medications in the past year.
As a chronic illness, asthma is responsible for significant economic costs, both direct medical costs and indirect costs. These have been measured and range from direct costs of US$ 250 million in Australia to US$ 3.6 billion for total costs. Costs per patient have been estimated at US$ 326 per patient per year in Australia and US$ 1,043 per patient per year in the United Kingdom (Sullivan 1996).
Pathophysiological studies have increasingly recognised asthma as an inflammatory airway disease over the past decade. National treatment guidelines for asthma were published in several countries including Britain, USA and Australia (BTS 1993; GINA 1995; BTS 1997; NAC 1998) recommending that doctors responsible for treating patients with asthma should make greater use of inhaled steroids in the management of asthma. In chronic asthma of moderate severity or greater, treatment with topical anti‐inflammatory corticosteroids or cromones is recommended as maintenance therapy.
In addition bronchodilator therapy is an essential component of treatment, traditionally used for relief of symptoms as needed. The most widely used bronchodilators are inhaled beta2‐agonists that are divided into two groups: those with a short duration of action (2 to 6 hours) and those, introduced more recently, with a longer duration of action (> 12 hours). The major representatives of the short acting beta2‐agonist agents in clinical use are salbutamol (known in North America as albuterol), terbutaline and orciprenaline, while the long acting beta2‐agonists in use are salmeterol and formoterol.
There has not been any controversy about using beta2‐agonists intermittently, for relieving acute asthma symptoms or preventing exercise induced asthma. However in chronic asthma, when used regularly three or four times daily, concerns have been raised (AAACI 1993). It was proposed that excessive use of beta2‐agonists might have contributed directly or indirectly to peaks in asthma mortality seen in the 1960's and late 1970's (Sears Rea 1986). A study by Campbell 1976 showed that in four Australian states there was a high correlation between the sales of adrenergic bronchodilator aerosols and the corresponding asthma mortality rates for the periods 1961 to 1963 and 1964 to 1966. Later in 1989 a case control study in New Zealand linked the use of inhaled fenoterol with increased risk of death from asthma (Crane 1989). This was followed soon after by a similar study in Saskatchewan that also showed an association between excessive use of beta2‐agonists and the risk of death or near death from asthma (Spitzer 1992).
Excessive use of beta2‐agonists in poorly controlled asthma may contribute to deaths (Abramson 2001) . This study showed significantly less use of asthma management plans and less use of inhaled corticosteroids in fatal cases.
Increased inflammation in the airways due to inhibition of anti‐inflammatory heparin release from mast cell degranulation by beta2‐agonists was proposed by Page 1993 as a mechanism for the worsening of asthma with regular use of these agents. Alternatively it was suggested that prolonged dilatation of the airways may allow more penetration of allergen.
The regular use of short acting beta‐2 agonist agents was the subject of a Cochrane review in 1999 ( Walters 1999). The conclusions were that there is little difference in using short‐acting beta2‐agonists regularly or as required, but with potentially some small clinical disadvantage to regular use. In general the frequency of use could therefore be left to patient preference.
The development of beta2‐agonists with long‐acting properties, such as salmeterol (Adkins 1997) and formoterol (Bartow 1998) has provided potential pharmacological advantages over short‐acting beta‐agonists, such as prolonged bronchodilation and protection against induced bronchospasm. However there remain concerns about adverse effects of regular use of long acting beta2‐agonists (Devoy 1995) on bronchial hyper responsiveness (Cockcroft 1993), the development of tolerance (Newnham 1995) and progressively reduced protection against provoking stimuli (Taylor 1997) and masking of deteriorating asthma (McIvor 1998).
Long acting beta‐agonists are more expensive than short acting beta agonists, and widespread use of long acting beta2‐agonist agents implies a significant increase in drug budgets for asthma. Whether there is any advantage in giving regular beta2‐agonist therapy as long or short acting drugs is therefore an important question (Kips 2001).
This review has addressed the comparative benefit or detriment of treatment in chronic asthma with regular short acting versus regular long acting inhaled beta2‐agonists.
Objectives
The objective of the review is to compare the effects of regular inhaled long acting beta agonists with regular use of inhaled short acting beta agonists in chronic asthma.
The specific purpose of the review is to assess whether there are any beneficial or harmful effects from the regular use of inhaled long acting beta agonists compared with inhaled short acting beta agonists on asthma control and symptoms, pulmonary function, airway hyper‐reactivity, rate of exacerbations of asthma, and quality of life.
Methods
Criteria for considering studies for this review
Types of studies
We considered all randomised studies, both open and blinded. Ideally, all studies would be blinded, and preferably double blind. The scoring system gives a lower score to open studies, which can be used to weigh the contribution of open studies, or exclude them from analyses. Studies could be either of parallel group or cross‐over design.
Types of participants
We included studies in which participants had a clinical diagnosis of asthma present for at least six months. We included both adults and children. We looked specifically for evidence of reversibility of airway obstruction to short‐acting inhaled beta(2)‐agonists as a diagnostic criterion. We sought to document the severity of participants' asthma at inclusion. Other asthma therapies could be used during the study, and we assessed the level and stability of the dose used. Studies that included some or all participants with other pulmonary diseases, and especially smoking related Chronic Obstructive Pulmonary Disease (COPD) were excluded unless the results for those with asthma alone were available separately.
Types of interventions
Participants in one treatment arm used a long acting inhaled beta agonist; either salmeterol or formoterol, twice daily administered via any inhalational device. The second treatment arm consisted of regular doses of any short acting inhaled beta agonist. The dose, inhalational device and frequency of administration were recorded, with the aim of having equivalence of bronchodilator effectiveness as far as possible. We excluded studies using oral administration of beta2‐agonists. The minimum period of treatment was two weeks, to fit the aim of assessing regular use in the chronic asthma setting.
Types of outcome measures
Outcome measures were chosen to reflect asthma control, balanced against side effects.
Planned outcome measures were daytime and night‐time asthma symptom scores, bronchodilator use for symptom relief, daily peak flow measurement (PEF), clinic measurements of airway function, airway hyper‐reactivity measurement, quality of life score, asthma exacerbation rates, adverse events.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Airways Group "Asthma and Wheez" trial register. This was derived from a comprehensive search of MEDLINE, EMBASE, CINAHL. In addition, hand searching of the 20 most productive respiratory care journals has been undertaken and relevant RCTs have been added to the register, including those published in a language other than English.
We searched this database using the following search strategy : (beta and agonist*) or bronchodilat* or salbutamol or albuterol or terbutaline or isoproterenol or reproterol or reproterenol or rimiterol or fenoterol or ventolin or orciprenaline or metaproterenol or pirbuterol) and (salmeterol or eformoterol or formoterol).
Searching other resources
We reviewed reference lists of all available primary studies and review articles to identify potentially relevant citations. We contacted researchers known to have an interest in the field to identify other relevant past or current studies.
Data collection and analysis
Selection of studies
From the abstracts or titles, two reviewers (JW and FR) independently reviewed literature searches to identify potentially relevant trials for full review. We carried out searches of bibliographies and texts to identify additional studies. Using the specified criteria, we decided inclusion of studies in the review by agreement between the reviewers (JW, EHW and FR).
Data extraction and management
Data were extracted by two authors and entered into Review Manager software by one author. We collected details of the study characteristics and outcomes assessed by seeking information presented in Appendix 1.
Assessment of risk of bias in included studies
The trials were scored using the Cochrane approach to assessment of allocation concealment: Grade A: Adequate concealment. Grade B: Unclear concealment. Grade C: Obviously not adequate concealment.
Each study was also assessed for validity using the method of Jadad 1996, on a 0 to 5 scale as follows: (1) Was the study described as randomised? (1 = yes, 0 = no) (2) Was the study described as double‐blind?(1 = yes, 0 = no) (3) Was there a description of withdrawals and drop outs? (1 = yes, 0 = no) (4) Was the method of randomisation well described and appropriate? (1 = yes, 0 = no) (5) Was the method of double‐blinding well described and appropriate? (1 = yes, 0 = no) (6) Deduct 1 point if methods of randomisation or blinding were inappropriate. Differences were resolved by discussion between the reviewers.
Dealing with missing data
An attempt was made to contact authors with data missing on relevant outcomes. We contacted a total of 17 principal authors of eligible studies. Five replied with data (Britton 1992; Pearlman 1992; D'Alonzo 1994; De Carli 1995; Bensch 2001) seven replied but were unable to provide data (Hermansson1995; Juniper 1995; Staehr 1995; Steffensen 1995; Leblanc 1996; Lipworth 1998; Taylor 1998) and no reply was received from the remainder.
Assessment of heterogeneity
For pooled effects a Breslow‐Day test of heterogeneity was carried out, and a p value < 0.05 was considered significant, indicating possible differences between studies. If heterogeneity was found an explanation was sought . Investigation of sources for heterogeneity included performing sensitivity analyses using the domains:
(1) Methodological quality ‐ Cochrane criteria A and B versus C ; Jadad score 3 to 5 versus 1 to 2. (2) Fixed effect versus random effects modelling.
Data synthesis
All included trials were combined using the Review Manager 4.1.1. We analysed data from parallel group and crossover studies separately.
For continuous outcomes, we calculated individual and pooled statistics as weighted mean differences (WMD) with 95% Confidence Intervals (CI) using both fixed and random effects models. Where different scales had been used to measure the outcome the pooled standardised mean differences (SMD), with 95% Confidence Intervals (CI) were calculated. The SMD is a statistic that expresses the difference in means between the two treatment groups in units of the pooled standard deviation. This applied particularly to measures of bronchial reactivity, symptom scores and diurnal variation in PEF.
For dichotomous outcomes, we calculated individual and pooled statistics as odds ratios (OR) with 95% Confidence Intervals (CI), using both fixed and random effects models.
Both a fixed effects model (Hasselblad 1995) and a random‐effects model (DerSimonian 1986) were used to pool the data, since there does not appear to be general consensus as to which method is superior. In general, the random effects method is a more conservative approach than the fixed effect method and results in larger CIs. The fixed effect result was reported unless a substantial difference was seen, when the random effects result was also quoted.
Funnel plots were used to examine the effects to investigate publication bias.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were planned to assess the effect of treatment in different populations of asthmatics; adults versus children, mild versus moderate asthma severity, asthmatics on regular inhaled corticosteroids versus asthmatics on no co interventions.
The following subgroup analyses were carried out:
Asthmatics using regular inhaled corticosteroids
Children
Severity of asthma (mild, mild‐moderate, moderate‐severe).
Subgroup analyses of studies over six months length was planned for the next version.
Results
Description of studies
Results of the search
We obtained a total of 868 references via a search performed in April 1999. These were assessed and we checked their reference lists in the full papers for further studies. The reference lists in 31 papers which were included in the earlier Cochrane review (Walters 1999), were also searched for relevant studies. A total of 208 papers were initially fully assessed. A repeat search, using the same criteria, was performed in February 2001 and we obtained a further 32 out of 459 references for full assessment. We assessed each paper and if it reported a study for inclusion, it was scored by at least two reviewers using the full text of the paper. Agreement on grading of quality was good. Kappa statistics showed 96% agreement on Cochrane grades and 86% on Jadad grades.
In these 240 papers there were: (1) 33 reviews, editorials and background studies (see additional reference list) (2) 53 which cited 31 studies meeting agreed inclusion criteria (see table of included studies) (3) 154 studies which were excluded for the following reasons (see table of excluded studies): (a) absence of a short‐acting beta(2)‐agonist group (96), (b) period of treatment less than 2 weeks (43), (c) dose of long‐acting beta(2)‐agonist varied during study (5), (d) oral short‐acting beta(2)‐agonist agent used (3), (e) not an RCT (5), (f) only published as an abstract without any further details available or obtainable(2).
Included studies
The long‐acting beta(2)‐agonist agent was salmeterol xinafoate in 22 studies. The dose used was 50 mcg given twice daily at 12 hour interval in 21 studies and 100 mcg twice daily in one study (Faurschou 1996). Two studies also used another dose in comparison‐ 25 mcg in one case and 100 mcg in another. Formoterol fumarate was the long‐acting beta(2)‐agonist agent used in nine studies, at a dose of 12 mcg twice daily in seven studies; one study used 6 mcg twice daily (Ekstrom 1998b) and one 24 mcg twice daily (Kozlik‐Feldman 1996). One had three treatment arms (Lipworth 1998), 6 mcg and 24 mcg in addition to 12 mcg. Where data from studies was combined, the dose of long‐acting beta(2)‐agonist used was the same or equivalent; salmeterol 50 mcg or formoterol 12 mcg (Campbell 1999). If another dose was used, the study was included, but the analysis performed with and without that study to assess the effect on the result.
The short‐acting inhaled beta(2)‐agonist agent used in 26 studies was salbutamol sulphate, at a dose of 200 mcg four times daily in 19 studies, a dose of 200 mcg twice daily in one study of children and a dose of 400 mcg four times daily in six studies. The drug was delivered in a dry powder form in studies using salbutamol 400 mcg, as this was considered by the maker as clinically equivalent to 200 mcg as a pressurised aerosol. Terbutaline sulphate 500 mcg four times daily was used in five studies.
The rescue agent used in 26 studies was salbutamol (albuterol); terbutaline in 2 studies; ipratropium ( an anticholinergic agent) in two studies, and in one study the patient's usual agent was continued (Castle 1993). Five studies in which the study drug was used as the rescue agent were excluded, on the basis that the dose of both the short‐acting beta(2)‐agonist agent and long‐acting beta(2)‐agonist agent was being varied in an unknown manner (Arvidsson1989; Wallin 1990; Midgren 1992; Newnham 1995; Tattersfield 2001).
INTERVENTION: TREATMENT PERIOD Any treatment period over two weeks was specified in the protocol and of the 31 included studies the treatment periods were:
2 weeks in 2 studies
4 weeks in 6 studies
6 weeks in 3 studies
12 weeks in 17 studies (four of these followed patients up for 12 months collecting limited data in the second period (Britton 1992; Lundback 1993; De Carli 1995; Lenney 1995)
16 weeks in 1 study
24 weeks in 2 studies
PARTICIPANTS: AGE Twenty eight studies used adult or adolescent subjects over the age of 12 and three used children younger than 12 years of age (Lenney 1995; Kozlik‐Feldman 1996; Byrnes 2000). There was little data available in these three publications with subjects aged less that 12 and they did not contribute to any of the major outcomes analyses.
PARTICIPANTS: ASTHMA SEVERITY Information on the severity of participants' asthma at entry to the study was sought from the paper‐ mild; mild ‐ moderate; moderate ‐ severe. If it was not directly specified then a grade of mild asthma was given where no preventive agent was used, mild to moderate if the majority of participants were on a preventive agent (usually inhaled corticosteroids or cromones), or moderate ‐ severe if participants were permitted to use oral steroids regularly. Those studies in which no details were available on the participants' asthma severity or any severity was permitted were classed as unknown or 'broad range'. The majority of studies, 23, used subjects with mild to moderate asthma. Two used subjects with mild asthma only ( Venables 1992; Kozlik‐Feldman 1996) and three used subjects with moderate to severe asthma (Lai 1995; Faurschou 1996; FitzGerald 1999) . Three were of unclear or a broad range of severity (Kesten 1991; Castle 1993; Steffensen 1995).
PARTICIPANTS: CO‐INTERVENTIONS Studies were assessed according to the co‐intervention treatment for asthma used by participants during the course of the study. The information was available for all studies, and in most cases the authors specified that the dose was kept constant during the course of the study treatment period.
The majority of studies, 25 of the 30 included, permitted a variety of co‐intervention treatments. The most frequently used were inhaled corticosteroid or cromones, but some of these studies also permitted oral steroids at low dose and theophyllines. Full details of treatments permitted in individual studies can be found in the table of included studies. In six studies all participants were required to use inhaled corticosteroids (Beach 1993; Lai 1995; Faurschou 1996; Lipworth 1998; FitzGerald 1999; Byrnes 2000). Only one study did not permit inhaled corticosteroid (Kozlik‐Feldman 1996).
METHODOLOGICAL QUALITY
OUTCOMES Results for parallel group studies have been analysed together, while those from studies with a cross‐over design have been grouped as a sub‐set. The statistical programme in Review Manager does not allow for the combining of results from studies with differing designs, unless the results from the first period are available alone, when this period only can be included.
Twenty three studies were of parallel group design and seven of cross‐over design. There were no cross‐over studies in which we were able to extract results independently from the first period.
All the results referred to below are from the twenty three parallel group studies, and are given as weighted mean differences, calculated using the fixed effect model, unless specified otherwise in the text. Results from these and other analyses can be found in additional tables Table 5.
1. Results by subgroup (WMD fixed 95%CI) *indicates non significant result.
| Outcome | All studies | #studies/ #pts | Heterogeneity chi2 | All on ICS | #studies/ #pts | Mild‐moderate asthma | #studies/ #pts | Mod‐severe asthma | #studies/ #pts |
| PEF am l/m | 32.93 (24.78,41.35) | 8/1881 | 8.61 df7 NS | 60.0 (0.8, 119.2) | 1/40 | 30.48 (23.72,37.24) | 6/1348 | ||
| PEF pm l/m | 25.62 (17.98,33.27) | 8/1878 | 14.04 df7, 7.37 df6 NS | 48.0 (13.77,109.77) | 1/40 | 18.3 (12.31,24.29) | 7/1872 | ||
| Change PEFam | 27.38 (22.98,31.77) | 6/1602 | 7.31 df5, 6.47 df4 NS | 29.6 (26.85,36.76) | 2/439 | 32.67 (26.89,37.26) | 4/1034 | 29.0 (12.13,45.87) | 1/190 |
| Change PEFpm | 11.94 (7.99,15.90) | 6/1603 | 7.31 df5, 6.47 df4 NS | 10.77 (3.5,18.05) | 2/438 | 13.29 (8.56,18.02) | 4/1035 | *10.0 (‐1.43,21.43) | 1/190 |
| FEV1 L | 0.22 (0.14,0.31) | 8/1397 | 14.79 df7 8.70 df6 NS | *0.18 (‐0.39,0.75) | 1/20 | 0.20 (0.13,0.28) | 6/1104 | *0.12 (‐0.13,0.37) | 1/180 |
| % pred FEV1 | *12.0 (‐1.06,25.06) | 1/22 | |||||||
| Change in FEV1 | 0.2 (0.12,0.28) | 3/844 | 8.6 df2, 5.45 df1 SIG | 0.14 (0.0, 0.28) | 1/248 | 0.2 (0.12, 0.28) | 3/844 | ||
| FVC L | 0.19 (0.09,0.30) | 4/760 | 8.45 df3 SIG | 0.24 (0.13,0.36) | 3/548 | ||||
| FEF 25‐75% l/sec | 0.42 (0.18,0.66) | 2/305 | 0.26 df1 NS | 0.42 (0.18,0.66) | 2/305 | ||||
| Sympt score ‐ 24hr | SMD ‐0.27 (‐0.11,‐0.43) | 3/604 | 2.12 df2 NS | ‐0.27 (‐0.11,‐0.43) | 3/604 | ||||
| Sympt score ‐ day | ‐0.15 (‐0.06,‐0.23) | 3/701 | 0.64 df2 NS | ‐0.14 (‐0.05,‐0.24) | 2/498 | ||||
| Sympt score ‐ night | ‐0.21 (‐0.1,‐0.31) | 3/701 | 0.8 df2 NS | ‐0.21 (‐0.09,‐0.33) | 2/498 | ||||
| % days no asthma symptoms | 10.34 (1.8,18.88) | 2/307 | 0.2 df1 NS | 10.34 (1.8,18.88) | 2/307 | ||||
| % nights no asthma awakenings | 12.12 (7.8,16.43) | 3/606 | 2.34 df2 NS | 12.12 (7.8,16.43) | 3/606 | ||||
| Rescue SABA 24hrs No. puffs | ‐0.48 (‐0.18,‐0.77) | 4/751 | 1.94 df3 NS | *‐1.10 (0.33,‐2.53) | 1/35 | ‐0.55 (‐0.19,‐0.9) | 3/606 | ||
| Rescue SABA daytime | ‐0.33 (‐0.16,‐0.5) | 4/1002 | 9.87 df3 SIG | ‐0.26 (‐0.09,‐0.44) | 3/799 | ||||
| Rescue SABA nighttime | ‐0.31 (‐0.19, ‐0.43) | 4/1002 | 1.02 df3 NS | ‐0.3 (‐0.17,‐0.42) | 3/799 | ||||
| QOL ‐overall score | SMD 0.54 (0.39, 0.69) | 2/647 | 8.23 df1 SIG | 0.32 (0.07, 0.57) | 1/539 | ||||
| QOL‐symptoms | 0.52 (0.39,0.65) | 1/539 | 0.52 (0.39,0.65) | 1/539 | |||||
| QOL ‐ emotions | 0.44 (0.32, 0.56) | 1/539 | 0.44 (0.32, 0.56) | 1/539 | |||||
| QOL ‐ exposure to environmental stimuli | 0.21 (0.11, 0.31) | 1/539 | 0.21 (0.11, 0.31) | 1/539 | |||||
| QOL ‐ activity limitation | 0.21 (0.11, 0.31) | 1/539 | 0.21 (0.11, 0.31) | 1/539 | |||||
| BHR (log PD20) | *0.37 (‐1.26, 0.51) | 1/20 | *0.37 (‐1.26, 0.51) | 1/20 | |||||
| Any adverse event | *OR 1.13 (0.8, 1.59) | 5/993 | 6.76 df4 NS | *OR 1.24 (0.53,2.95) | 1/180 | *OR 1.08 (0.66, 1.75) | 2/369 | *OR 1.24 (0.53, 2.95) | 1/170 |
| AE ‐ palpitations | *OR 1.04 (0.62,1.74) | 11/3239 | 8.94 df 10 NS | *OR 0.32 (0.01,8.03) | 1/190 | *OR 1.05 (0.61,1.78) | 9/2815 | *OR 0.96 (0.19,4.79) | 1/568 |
| AE ‐ headache | OR 1.28 (1.02,1.62) | 13/3737 | 14.5 df12 NS | *OR 0.64 (0.17,2.34) | 1/190 | OR 1.28 (1.01,1.61) | 11/3313 | *OR 0.64 (0.17,2.34) | 1/568 |
| AE ‐ tremor | *OR 0.68 (0.43,1.07) | 11/3546 | 13.33 df10 NS | *OR 1.48 (0.24,9.09) | 2/370 | *OR 0.64 (0.4, 1.03) | 10/3356 | *OR 1.48 (0.24,9.09) | 1/170 |
| AE ‐ cramps | *OR 2.12 (0.99,4.54) | 4/1234 | 3.38 df3 NS | *OR 0.48 (0.04,5.43) | 1/190 | OR 2.53 (1.07,5.97) | 2/910 | *OR 0.48 (0.04,5.43) | 1/170 |
| > 1 major exacerbation (similarly defined) | *OR 0.89 (0.75,1.06) | 9/2890 | 2.65 df8 NS | *OR 0.86 (1.48, 0.5) | 2/370 | *OR 0.82 (0.67,1.01) | 8/2279 | *OR 0.86 (0.5,1.48) | 2/370 |
| > 1 major exacerbation (definition less precise) | *OR 0.90 (0.78,1.03) | 14/28814 | 8.44 df13 NS |
Risk of bias in included studies
The methodological quality of the majority of trials was good and on the Jadad scoring method, three scored five while 23 scored four and one scored three. Four studies were given the lower score of two as they were not blinded by intervention. Lack of information in publications on the methods of randomisation used, meant that allocation concealment could not be confirmed in many cases, so only five studies were graded as confirmed adequate (A), and the remaining 26 were unclear (B).
Effects of interventions
AIRWAY CALIBRE MEASUREMENTS
There were significant advantages for the long acting beta agonist group compared with the regularly treated short acting beta agonist group for all indices of airway calibre.
The long acting beta agonist group showed an advantage of 32.93 L/min (95% CI 24.47 to 41.39, Analysis 1.1) for morning peak expiratory flow (PEF am). There was no significant heterogeneity.
1.1. Analysis.

Comparison 1 All studies, Outcome 1 Peak expiratory flow: morning l/min.
The evening peak expiratory flow (PEF pm) showed an advantage of 25.62 L/min (95% CI 17.98 to 33.27, Analysis 1.2) based on eight studies with 1881 subjects. There was significant heterogeneity however, chi2 was 14.04 df = 7, and on examination the heterogeneity was due to one study Ekstrom 1998b which used a lower dose of formoterol (6 mcg) than the other studies. When this was excluded from the calculation of the pooled effect, the chi2 value was not significant 7.37 df = 6.
1.2. Analysis.

Comparison 1 All studies, Outcome 2 Peak expiratory flow: evening l/min.
The mean difference in the change in PEF during treatment was 27.38 L/min (95% CI 22.98 to 31.77, Analysis 1.3) for morning PEF am and 11.94 L/min (95% CI 7.99 to 15.90, Analysis 1.4) for evening PEF, based on six studies with 1603 participants. There was no significant heterogeneity seen in this analysis.
1.3. Analysis.

Comparison 1 All studies, Outcome 3 Change in PEF morning.
1.4. Analysis.

Comparison 1 All studies, Outcome 4 Change in PEF evening.
There was only one study reporting usable data for participants who all used inhaled corticosteroids (Pearlman 1992) when the difference was larger for PEF am 60 L/min (CI 0.8 to 109.8), pm 48 L/min (CI 13.8 to 110). The result for participants with asthma of mild to moderate severity was very similar to the that in all studies combined.
Laboratory measures of lung function showed an advantage for long acting beta2‐agonists of 0.22 litres (95%CI 0.14 to 0.31) in FEV1 (based on eight studies with 2446 participants) and 0.24 Litres (95% CI 0.13 to 0.36) for FVC (based on three studies with 1118 participants). There was no heterogeneity. One study (De Carli 1995) had differences in FVC at baseline so this result was excluded.
Maximum mid‐expiratory flow (FEF 25‐75%) showed a difference of 0.42 L/sec (95% CI 0.18 to 0.66) based on two studies with 305 participants.
There was only one study with data on patients using inhaled corticosteroids and on participants classified as having moderate to severe asthma. The result in studies using participants classified as having mild to moderate asthma did not differ from the overall analysis (WMD 0.2 (CI 0.13 to 0.28).
SYMPTOM SCORES
There were significant advantages to the long acting beta agonist group compared with the regularly treated short acting beta agonist group for composite symptom scores, measured over the whole day and also day or night scores measured separately. The difference in whole day score was ‐0.27 units (SMD) (95%CI ‐0.11 to ‐0.43), based on three studies with 604 participants (Analysis 1.11).
1.11. Analysis.

Comparison 1 All studies, Outcome 11 Symptom score ‐ whole day.
For daytime only, the difference was ‐0.15 (95% CI ‐0.06 to ‐0.23), and for night time only score, the difference was ‐0.21 (95%CI ‐0.1 to ‐0.31), both in three studies with 701 subjects (Analysis 1.12).
1.12. Analysis.
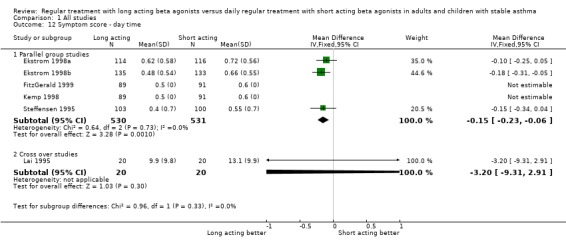
Comparison 1 All studies, Outcome 12 Symptom score ‐ day time.
There were also significant advantages to the long acting beta agonist group compared with the regularly treated short acting beta agonist group in the proportion of days and nights affected by asthma symptoms. The difference in the percentage of nights with no awakenings due to asthma was 12.12% (95%CI 7.8 to 16.43) in three studies with 606 participants (Analysis 1.15). The difference in percentage of days with no asthma symptoms was 10.34% (95%CI 1.8 to 18.88) in two studies with 307 participants (Analysis 1.14).
1.15. Analysis.
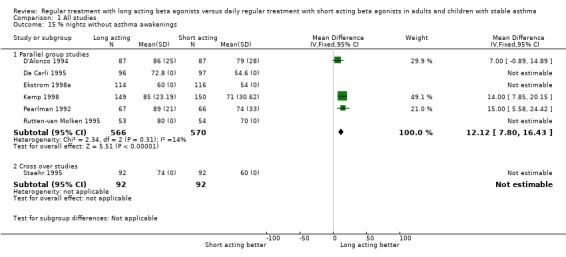
Comparison 1 All studies, Outcome 15 % nights without asthma awakenings.
1.14. Analysis.

Comparison 1 All studies, Outcome 14 %days without asthma symptoms.
There were no analyses possible in the subgroup of participants using inhaled corticosteroids or with asthma classified as moderate to severe owing to a lack of data. Those with asthma graded as mild to moderate showed very similar results to the overall analysis.
RESCUE BRONCHODILATOR USE
The long acting beta agonist group used significantly less rescue bronchodilator for symptoms compared with the regularly treated short acting beta agonist group during treatment. The amount of rescue medication being used by participants in most of the studies at the start was of the order of four to five puffs each day. This fell during study treatment period, and in three studies that reported figures, the mean change was ‐2.7 puffs per day in the long acting beta2‐agonist group and ‐2.0 puffs per day in the short acting beta2‐agonist group. The difference in mean decrease from baseline use was ‐0.69 puffs per day (95%CI ‐0.08 to ‐1.29) with the group treated with long acting agents showing a greater decrease in use of rescue agent (Analysis 1.19).
1.19. Analysis.

Comparison 1 All studies, Outcome 19 Change in use of rescue bronchodilator/day.
Over a 24 hour period the mean difference in number of puffs used was ‐0.48 puffs (95%CI ‐0.18 to ‐0.77) in four studies with 751 participants (Analysis 1.16). For daytime use of rescue agent, the difference between the long acting beta2‐agonist group and short acting beta2‐agonist group was ‐0.33 day time puffs/24 hrs (95%CI ‐0.16 to ‐0.5) in four studies with 1002 participants (Analysis 1.17). However this analysis showed significant heterogeneity (chi2 9,87 df = 3) , and on investigation, this was mainly due to one study (Steffensen 1995) in which the effect size was larger. This study did not specify the baseline severity of asthma in the participants and the WMD in studies on participants all with mild‐moderate asthma was ‐0.26 puffs/day (CI ‐0.09 to ‐0.44). There was no significant heterogeneity in this case (chi2 4.02 df = 2). The WMD for night time use of rescue short acting beta2‐agonist was ‐0.31 puffs/24 hrs (95%CI ‐0.19 to ‐0.43) in four studies with 1002 participants (Analysis 1.18).
1.16. Analysis.

Comparison 1 All studies, Outcome 16 Rescue bronchodilator use: whole day.
1.17. Analysis.

Comparison 1 All studies, Outcome 17 Rescue bronchodilator use: day time.
1.18. Analysis.

Comparison 1 All studies, Outcome 18 Rescue bronchodilator use: night time.
The majority of studies contributing to these results used asthmatics with mild to moderate asthma and there was no data available for subgroup analyses in more mild or more severe asthmatic participants.
QUALITY OF LIFE
Three studies (Juniper 1995; Rutten‐van Molken 1995; Wenzel 1998) measured quality of life changes with treatment, using the AQOL scale by Juniper 1992, which contains thirty two questions in four domains; activity limitation, symptoms, emotional function and environmental stimuli, but only in the case of Wenzel 1998 could the results be fully extracted for both treatment groups. De Carli 1995 used the Living with Asthma questionnaire to assess patient‐perceived quality of life. This gives a global score, based on 12 questions, with a reduction in score indicating better quality of life (Hyland 1991).
Combining the results from De Carli 1995 and Wenzel 1998 showed a significant advantage to the long acting beta agonist group compared with the regularly treated short acting beta agonist group in overall score, SMD 0.54 (95%CI 0.39, 0.69), N=647 for these two studies. There was significant heterogeneity in this analysis, (chi2 8.23 df = 1). The studies used different instruments to measure quality of life with different scales and the result is expressed as the SMD, however the different scales to some extent measure different aspects of quality of life and these may be affected in different ways by the study treatment.
The results from Wenzel 1998 for separate domains also gave a significant advantage to the long acting beta agonist group, with the mean difference for symptoms 0.52 (95%CI 0.39 to 0.65), emotions 0.44 (95%CI 0.32 to 0.56), exposure to environmental stimuli 0.21 (95%CI 0.11 to 0.31) and activity limitation 0.21 (95%CI 0.11 to 0.31) with 539 participants in the study. It is known that a mean difference of >= 0.5 for overall quality of life and each of the individual domains is clinically important (Juniper 1994). The result for symptoms of asthma reached this level of clinical importance, with that for emotional function approaching the level.
These differences were of similar magnitude to those seen in Juniper 1995, where in all four domains there was a significantly greater improvement in the long acting beta2‐agonist group compared to the short acting beta2‐agonist group. The magnitude was clinically important for symptoms and emotional function. In Rutten‐van Molken 1995 there was a significant improvement in all domains in the long acting beta2‐agonist group compared to the short acting beta2‐agonist group. This was clinically important in the domains of activity limitation and symptoms .
Subgroup analyses were not possible owing to lack of studies with data.
BRONCHIAL HYPER REACTIVITY
Three studies reported results for bronchial hyper reactivity (BHR), Beach 1993 and FitzGerald 1999, Byrnes 2000 but these used differing methods and timing. Only Beach 1993 had a wash out period after the previous dose of treatment, of 24 hours, to look at underlying changes in reactivity. FitzGerald 1999 tested reactivity two hours after the morning dose of trial medication, and Byrnes 2000 tested twelve hours after the previous dose.
Only Beach 1993 reported both mean and standard deviation, in a study on 20 participants, with a non significant difference in BHR measured as log PD20 methacholine 0.37 (95%CI ‐1.26 to 0.51) mg/ml. FitzGerald 1999 reported a non significant difference in degree of bronchoprotection of 1.38 fold (95%CI 0.88 to 2.15) at 12 weeks in 190 participants with moderate or greater asthma. Byrnes 2000, in a crossover study, tested 14 children and found no significant difference between treatments, the ratio of PC20 histamine being 1.54 (95%CI 0.65 to 3.7).
Lipworth 1998 studied the degree of bronchoprotection against methacholine challenge afforded by a long acting beta2‐agonist (formoterol 12 mcg) compared with a short acting agent (terbutaline 500 mcg), both after the first dose and after two weeks treatment, in participants on inhaled corticosteroids. The first dose of formoterol gave a two fold greater degree of protection compared to terbutaline, but after two weeks treatment there was no significant difference between the two treatments, and the residual degree of protection was 1.5 fold (95%CI 0.6 to 3.8) for formoterol 12 mcg BD and 1.6 fold (95%CI 0.8 to 4.9) for terbutaline 500 mg QID.
ADVERSE EVENTS
The majority of studies, twenty seven in total, reported on adverse events related to trial medication .The exceptions were Hekking 1990; Beach 1993, Rutten‐van Molken 1995, Lipworth 1998, Taylor 1998, and they stated that asthma related events and pharmacologically predicted events occurred at the same rate in both groups. Taylor 1998 reported extensively on asthma exacerbation rates, but this is reported later in the review.
For those studies which reported adverse events data, the odds ratio for any trial medication‐related adverse event occurring in the long acting beta agonist group compared with the regularly treated short acting beta agonist group was a non‐significant 1.13 (95%CI 0.8 to 1.59) in five studies with 993 participants (Analysis 1.27).
1.27. Analysis.

Comparison 1 All studies, Outcome 27 Adverse events‐all.
Specified pharmacologically predictable adverse effects of palpitations, headache, tremor and cramps were assessed and reported in 13 studies. A significant increase in odds ratio was found for headache in the regular long‐acting groups OR 1.28 (95%CI 1.02 to 1.62). The differences in other adverse effects were non‐significant: palpitations OR 1.04 (95%CI 0.62 to 1.74), tremor OR 0.68 (95% CI 0.43 to 1.07), and muscle cramps OR 2.12 (95%CI 0.99 to 4.54) where the increased odds ratio for the long acting beta agonist group approached statistical significance.
Subgroup analyses did not show any significant differences in the results from those studies using participants with more severe asthma or where all participants used inhaled corticosteroids.
ASTHMA EXACERBATIONS
Data on exacerbations of asthma were reported in fourteen studies. Exacerbations of asthma were defined in eight studies as worsening of asthma symptoms requiring treatment in addition to the study drug and rescue short acting inhaled beta ‐agonist agent. The number of participants experiencing at least one exacerbation was used as a comparative measure in these studies.
In Ekstrom 1998b the number of participants discontinuing participation in the study due to deterioration of asthma was recorded, and used as a measure of asthma exacerbations.
In FitzGerald 1999 the number of exacerbation days was measured. These were defined as days when more than eight puffs of rescue salbutamol were inhaled or the asthma symptoms score was at the maximum on the study scale. The number of patients requiring an increase in corticosteroid cover was recorded and this was used as the measure of major exacerbations for comparison.
In Steffensen 1995 data was collected on adverse events that were possibly drug related, including asthma exacerbations, though no definition of an exacerbation was given.
De Oliveira 1998 reported on withdrawals due to worsening asthma.
De Carli 1995 sent unpublished tables on exacerbations at time points from three to twelve months, but did not define an exacerbation. In Castle 1993 serious drug related adverse events were recorded and data on those that were respiratory and related to asthma were extracted.
Hekking 1990 measured an outcome called 'asthma attacks' with no definition of an attack, though discussion in the paper makes it clear that these were not synonymous with an exacerbation as defined by others. These data have not been combined with other data on exacerbations.
Taylor 1998 studied asthma control during long term treatment, and used a complex scoring system, based on PEF readings, symptoms scores, rescue bronchodilator use and presence of nocturnal wakening to define both minor and major exacerbations of asthma. A major exacerbation implied major deterioration over two or more days, with PEF 40‐60% of predicted value, increased asthma score and increased rescue use. The protocol stated that if this occurred, participants should commence a short course of oral prednisolone, in addition to increasing their inhaled corticosteroid dose according to their predefined action plan. Data was given as both the percentage of participants temporarily increasing their dose of inhaled corticosteroids and the percentage of participants who used one or more short courses of oral steroids. The outcome entered into the analysis was the number of participants who increased their dose of inhaled corticosteroid. This study also reported a corrected yearly exacerbation rate, for both major and minor exacerbations.
Overall, the odds ratio for experiencing at least one major exacerbation of asthma was lower in the long acting beta agonist group, OR 0.89 (95%CI 0.75 to 1.06) in nine studies with 2,890 participants (Analysis 1.32). These studies all used a highly comparable definition of an exacerbation. If the studies where the definition was imprecise or the data came from adverse events monitoring, were included in the analysis( N = 14) , there remained a lower risk of exacerbation, OR 0.90 (95%CI 0.78 to 1.03). Neither result achieved statistical significance.
1.32. Analysis.

Comparison 1 All studies, Outcome 32 Exacerbations asthma‐major.
Taylor 1998 was a crossover study design, and was therefore not combined for this outcome with other studies in the analysis, however he reported on the rate of exacerbations and there was a significant difference for the corrected rate of major exacerbations. There was an advantage towards the long acting beta agonist group , WMD ‐0.29 (95%CI ‐0.50 to ‐0.08) exac/patient/year.
In the two studies where all subjects were using inhaled corticosteroids (n = 370) the odds ratio for experiencing at least one major exacerbation was 0.86 (CI 0.5 to 1.84) . The result however was not statistically significant though it was similar to the result from all studies.
GLOBAL ASSESSMENT OF EFFICACY
Six studies reported results of the assessment of efficacy of study treatment, using scales offering the participant a range from very good or very effective to poor or poorly effective. Data was available in five studies for analysis and in Faurschou 1996 the authors stated that more participants rated treatment with salmeterol as effective or very effective when compared to salbutamol and the difference was statistically significant. The odds ratio of patients on long acting beta2‐agonists compared with short acting agents, in the five studies with data, for finding treatment very effective or effective was 2.54 (95%CI 1.92 to 3.36, Analysis 1.38) or as NNT 5 (95% CI 4 to 7).
1.38. Analysis.
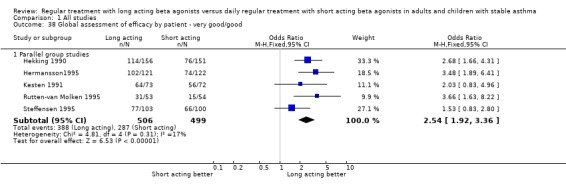
Comparison 1 All studies, Outcome 38 Global assessment of efficacy by patient ‐ very good/good.
Four of the studies also stated that investigator rated efficacy results were of similar direction and magnitude (Hekking 1990; Hermansson1995; Steffensen 1995; Faurschou 1996) . Only two of these studies quoted the results and the analysis showed significant heterogeneity.
Discussion
As a chronic disease, with no known cure, the accepted goals of management in chronic asthma are to minimise the adverse impact of the disease on a patient's physical and mental well being and to try, through good control, to minimise long term damage to the airways and prevent undue fixed airway obstruction. Treatment is therefore directed at improving physiological endpoints and patient perceived physical and mental health.
This review shows that for assessment of airway calibre, regular treatment with long acting inhaled beta2‐agonists gives significantly better results than regular therapy with short acting beta2‐agonists. The magnitude of the difference was moderately large: for morning PEF 32 L/min (95% CI 25 to 41) and evening PEF 25 L/min (95% CI 18 to 32). The change from pre‐treatment PEF values was also significantly greater for long acting inhaled beta2‐agonists, especially in morning values, 27 L/min (95% CI 23 to 31) reflecting the longer duration of action of 12 hours compared to the short acting agents of only 4 to 6 hours. The difference for evening PEF values was a more modest 12 L/min (95% CI 8 to 16), which reflects the diurnal variation of lung function in asthma, with the worst time being on waking or in the hours just prior to waking.
Clinic measured lung function also showed a significant and clinically important benefit for treatment with long acting inhaled beta2‐agonists, with an average increase in FEV1 of 220 ml (95% CI 140 to 310) , FVC 190 ml (95% CI 90 to 300) and FEF25‐75% 0.4 L/sec (95% CI 0.2 to 0.7).
Long acting inhaled beta2‐agonists also gave advantages over regular treatment with short acting agents in terms of patient assessed symptoms, and on a variety of scales. The difference in scores for the whole day, expressed using an SMD, was 0.3 (95% CI 0.1 to 0.4) (SMD), daytime alone 0.2 (95%CI 0.1 to 0.2) and night time 0.2 (95% CI 0.1 to 0.3). Interpretation of this improvement in quantitative terms is difficult, but when looking at the percentage of days with no asthma symptoms there was a significant benefit in the long acting inhaled beta2‐agonist group of 10% (95% CI 2 to 19), and nights with no asthma awakenings of 12% (95% CI 8 to 18).
The reduction in perceived symptoms was reflected in the amount of additional bronchodilator agent used, usually a short acting beta2‐agonist. It was significantly less in the long acting inhaled beta2‐agonist group. The amount of rescue medication being used by participants in most of the studies at the start of the study was of the order of four to five puffs each day. This fell during study treatment period in both the participants groups treated regularly with long acting and short acting agents, and in three studies which reported figures, the mean change was 2.7 puffs per day in the long acting beta2‐agonist group and 2.0 puffs per day in the short acting beta2‐agonist group. Over a 24 hour period the mean difference in number of puffs was used was 0.5 puffs (95% CI 0.2 to 0.8), 0.3 puffs (95% CI 0.2 to 0.5) for daytime use and 0.3 puffs (95% CI 0.2 to 0.4) for night time use. The difference in mean decrease from baseline use was 0.7 puffs per day (95% CI 0.1 to 1.3).
These commonly used clinical endpoints, forced expiratory volume in one second (FEV1), peak expiratory flow (PEF), symptom scores, use of rescue medication and sleep disturbance are not always good proxies for overall quality of life. Asthma specific measurement of the impact of asthma on patients' quality of life is now possible, using purpose ‐designed instruments, of proven reliability, validity and responsiveness. These provide a robust reliable measurement of this the global impact of aspect of efficacy of treatment. Two asthma specific measures were used in the studies included herein this review. The Living with Asthma Questionnaire (LWAQ) by Hyland 1991 and Asthma Quality Of Life Score (Asthma Quality Of Life Score (AQOL) based on Juniper 1992. Combining overall results from both studies showed a significantly better quality of life in those using long acting inhaled beta2‐agonists, SMD 0.6 (95%CI 0.4, 0.7). This was supported by results for all four domains of the AQLQ, i.e. activity limitation, symptoms, emotional function and environmental stimuli, from three studies, though in only one case were full results of available for both groups. The differences in AQLQ score for the separate domains varied in their clinical importance, with that for asthma symptoms being consistently at a level corresponding to the criterion for a small clinically significant improvement.
Data for underlying bronchial hyper reactivity (BHR) were limited to one study and two studies looked at bronchoprotection to challenge. Laboratory measures of airway reactivity can measure the bronchoprotection to various stimuli that is conferred by regular treatment with both long and short acting beta2‐agonists. The direct significance of these changes is not understood but they may provide explanations for adverse effects of treatment that may be observed or postulated from population data on mortality and severe life threatening asthma attacks.
The studies included in this review did not provide any evidence that regular treatment with either long or short acting beta2‐agonist agents adversely affects airway reactivity at a level likely to be of clinical importance. This is reassuring to those who have expressed concern over the past decade or more, that regular beta2‐agonist use would cause a worsening of underlying airway inflammation and thereby of BHR.
The development of tachyphylaxis to the bronchoprotective effects of beta2‐agonist agents to methacholine challenge seen in Lipworth 1998 occurred in spite of concomitant inhaled corticosteroid use. The clinical significance is not certain, and is probably slight at most but, but potentially this sub sensitivity could mean that long acting agents may not give full protection against a given bronchoconstrictor stimulus and extra doses of rescue agent might be required. It would argue against the use of long acting beta2‐agonist agents specifically as relief medication, which is now currently the case in some countries for formoterol.
Risks of treatment and deleterious effects must be taken into account in a comparison of effectiveness between these two treatments, especially any evidence of deterioration in asthma control, particularly in the light of historical concerns about regular use of beta2‐agonist agents. Evidence from a recent case control study from one group of patients dying from asthma did not show an increased risk of death with use of inhaled symptomatic medication for an attack, except that there was an increased risk of death (OR 4.1 95%CI 1.7 to 11) for the use of nebulised symptomatic medication for an attack or in the last month. Blood levels of salbutamol were significantly higher in asthma deaths than controls, even in a situation in which controls with life threatening asthma were usually given bronchodilator before assessment. Some of the blood levels detected in the deceased asthmatics were extremely high, suggesting that over reliance on relief beta2‐agonists for treatment of severe attacks could be cardio toxic (Abramson 2001).
Only one study (Castle 1993) looked at the safety of a long acting beta2‐agonist (salmeterol) compared with a short acting agent (salbutamol) when used regularly over sixteen weeks in a large number of participants. It was the only study reporting figures for mortality from asthma. There was a numerical excess of deaths in the salmeterol group; 0.07% compared with 0.02%, OR 3 (95%CI 0.67 to 13.41). The numbers were very small however, and the difference was not significant with a wide confidence interval. 17% of participants included in the study were classified as having severe asthma, 69% were using inhaled corticosteroids and 4.75 oral steroids, so they formed a more severe population than those included in most of the other studies reviewed the total population. The authors proposed that use of beta agonist was not causal in the deaths reported, but rather general under treatment of their asthma.
The risk of having at least one major exacerbation, (defined as requiring treatment in addition to study treatment, usually with oral steroids) in the long acting beta2‐agonist group was not reduced compared with the group using short acting agents, over the relatively short time scale of these studies; OR 0.89 (CI 0.75 to 1.06). There was a similar size difference OR 0.86 (CI 0.5 to 1.48) in the studies which only included participants on inhaled corticosteroids, however the number of participants in these studies was small. There was no evidence of an increased risk of exacerbation of asthma in those taking long acting beta2‐agonists regularly.
One study (Taylor 1998) was designed to look more comprehensively at the rate of all exacerbations of asthma, including minor exacerbations. These were defined as a fall in morning PEF to 60 to 75% of best run‐in value, with some increase in asthma symptoms or a fall to 40 to 60% of best PEF with no extra symptoms. There was a significantly lower rate of such episodes in the long acting beta2‐agonist group, the difference being 0.59 exacerbations/patient /year (95%CI 0.33 to 0.85). The acceptability of treatment to patients was assessed by patients rating the control of their asthma on treatment and results show a significantly higher odds ratio for assessment as good or very good by patients using long acting beta2‐agonists than those using short acting beta2‐agonists regularly, OR 2.5 (95%CI 1.9 to 2.4).
In recent times as healthcare resources have been increasingly constrained, treatment must be assessed not only to be clinically effective, acceptable to patients and safe but it must also be cost effective. There are currently few studies comparing the clinical and economic benefits of comparing alternate treatments in asthma, including the subject of this review, long acting with short acting inhaled beta2‐agonist agents. At this stage we are therefore unable to comment upon this.
Future studies should use a standardised approach to outcome measurement in addition to cost effectiveness analysis. Perhaps inevitably at this stage, we found that different studies reported lung function parameters in varying ways, and used symptom scores with different scales, so that direct comparisons were difficult. In general the length of intervention studies should be longer to allow more appropriate assessment of effectiveness and also to take into account dropouts from therapy. The burden of asthma is dependent on the severity of the condition, and there is a distinct lack of studies looking at asthma of defined severity at either end of the spectrum, mild or severe. Increasingly, the population of patients with chronic symptomatic asthma requiring regular symptom‐controller medication is going to be elderly, and studies are needed specifically in this group to determine both cost effectiveness and safety. The elderly, who might be more vulnerable to the adverse cardiovascular effects of systemic absorption of beta2‐agonists, tend to be poorly represented in the studies currently available.
Authors' conclusions
Implications for practice.
Long acting inhaled beta2‐agonists have advantages in clinical outcomes when used regularly over the effects of regular inhaled short acting beta2‐agonists. The increased cost of treatment if more long acting beta2‐agonists are prescribed will have implications for medical costs, which will only be partially offset by reduced symptom directed use of short acting beta2‐agonists.
Implications for research.
Increasingly studies are showing that long acting inhaled beta2‐agonists have anti‐inflammatory and other disease modifying effects, especially in combination with inhaled corticosteroids. Whether similar effects would be present if used without inhaled corticosteroids needs assessment. There are data suggesting that beta2‐agonists can enhance the translocation of the CS‐CS receptor complex into the nucleus where it can effect changes in transcription, but further work is required to document the full pathophysiological effects of long acting inhaled beta2‐agonists, independently and together with inhaled corticosteroids, and to more fully explain these effects.
Further cost effectiveness studies are also required.
What's new
| Date | Event | Description |
|---|---|---|
| 20 August 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 4, 2000
| Date | Event | Description |
|---|---|---|
| 24 April 2002 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Airways group staff especially Steven Milan and Toby Lasserson for logistic support, Jane Dennis and Karen Blackhall for searches, papers retrieval, and translation. Felix Ram for help with grading studies. Chris Cates for editorial input and advice.
Richard Wood Baker for advice and help with abstract writing.
Glaxo Smith Kline staff for unpublished data and authors who responded to requests for more information. Kirsty Olsen who copy edited this review.
Appendices
Appendix 1. Information collected from eligible studies
Methods‐study design, location and setting, method of randomisation and blinding, withdrawals/drop outs, compliance, confounders and quality score. Participants‐ total number of subjects (N), numbers of males and females, the mean age and range, baseline severity of asthma, inclusion and exclusion criteria. Interventions‐ the long acting beta agonist and short acting beta agonist used, with dose and frequency of dosing, the device used to administer drug, the treatment period, the additional rescue agent used if any, any co‐intervention used during study by participants, with its dose and whether dose remained stable. Outcomes‐ which outcomes were measured, which reported, in what form and whether they were complete, the standard deviation or other measure of variability. Studies could use a variety of measures of asthma control and we specifically extracted results for the following 35 outcomes where available: Peak expiratory flow (PEF): morning (PEF): evening % Predicted (PEF): morning % Predicted (PEF): evening Change in PEF: morning Change in PEF: evening Amplitude of diurnal variation in PEF FEV1 % Predicted forced expiratory flow in one second (FEV1) Change in FEV1 Forced Vital Capacity (FVC) FEF25‐75 (forced expiratory flow over the middle half of the FVC, that is the average flow from the point from where 25% of the FVC has been exhaled to the point where 75% has been exhaled. Symptom score: whole day Symptom score: day time Symptom score: night time %days without asthma symptoms % nights without asthma awakenings Rescue bronchodilator use: whole day Rescue bronchodilator use: day time Rescue bronchodilator use: night time Quality of life score: overall Quality of life score: symptoms Quality of life score: emotions Quality of life score: exposure to environmental stimuli Quality of life score: activity limitations Bronchial hyper reactivity Adverse events: all Adverse events: palpitations Adverse events: headache Adverse events: tremor Adverse events: cramps Exacerbations of asthma Deaths related to asthma Overall efficacy of treatment
We decided that measures of airway inflammation, obtained by bronchoscopy or sputum analysis would not be included in the review at this stage, because there were insufficient studies reporting them.
Data and analyses
Comparison 1. All studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peak expiratory flow: morning l/min | 14 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Parallel group studies | 12 | 3004 | Mean Difference (IV, Fixed, 95% CI) | 32.93 [24.47, 41.39] |
| 1.2 Cross over studies | 2 | 120 | Mean Difference (IV, Fixed, 95% CI) | 16.0 [‐55.90, 87.90] |
| 2 Peak expiratory flow: evening l/min | 12 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Parallel group studies | 10 | 2798 | Mean Difference (IV, Fixed, 95% CI) | 25.62 [17.98, 33.27] |
| 2.2 Crossover studies | 2 | 120 | Mean Difference (IV, Fixed, 95% CI) | 9.0 [‐62.90, 80.90] |
| 3 Change in PEF morning | 9 | 2117 | Mean Difference (IV, Fixed, 95% CI) | 27.38 [22.98, 31.77] |
| 3.1 Parallel group studies | 9 | 2117 | Mean Difference (IV, Fixed, 95% CI) | 27.38 [22.98, 31.77] |
| 3.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in PEF evening | 7 | 1991 | Mean Difference (IV, Fixed, 95% CI) | 11.94 [7.99, 15.90] |
| 4.1 Parallel group studies | 7 | 1991 | Mean Difference (IV, Fixed, 95% CI) | 11.94 [7.99, 15.90] |
| 4.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Amplitude PEF: diurnal variation (l/min or %) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Parallel group studies | 2 | 374 | Mean Difference (IV, Fixed, 95% CI) | ‐16.0 [‐21.66, ‐10.34] |
| 5.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐2.3 [‐5.84, 1.24] |
| 6 FEV1 (litres) | 13 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Parallel group studies | 11 | 2446 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [0.14, 0.31] |
| 6.2 Cross over studies | 2 | 122 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.56, 0.56] |
| 7 % Predicted FEV1 | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Parallel group studies | 1 | 22 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [‐1.06, 25.06] |
| 7.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Change in FEV (litres) | 5 | 1285 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.12, 0.28] |
| 8.1 Parallel group studies | 5 | 1285 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.12, 0.28] |
| 8.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Forced Vital Capacity (litres) | 4 | 1118 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.13, 0.36] |
| 9.1 Parallel group studies | 4 | 1118 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.13, 0.36] |
| 9.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 FEF25‐75 (litres/sec) | 2 | 305 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [0.18, 0.66] |
| 10.1 Parallel group studies | 2 | 305 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [0.18, 0.66] |
| 10.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Symptom score ‐ whole day | 3 | 606 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.43, ‐0.11] |
| 11.1 Parallel group studies | 3 | 606 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.43, ‐0.11] |
| 11.2 Cross over studies | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Symptom score ‐ day time | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Parallel group studies | 5 | 1061 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.23, ‐0.06] |
| 12.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐9.31, 2.91] |
| 13 Symptom score: night time | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Parallel group studies | 5 | 934 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.31, ‐0.10] |
| 13.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐6.39, 0.79] |
| 14 %days without asthma symptoms | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Parallel group studies | 4 | 601 | Mean Difference (IV, Fixed, 95% CI) | 10.34 [1.80, 18.88] |
| 14.2 Cross over studies | 1 | 184 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 % nights without asthma awakenings | 7 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 15.1 Parallel group studies | 6 | 1136 | Mean Difference (IV, Fixed, 95% CI) | 12.12 [7.80, 16.43] |
| 15.2 Cross over studies | 1 | 184 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Rescue bronchodilator use: whole day | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 16.1 Parallel group studies | 5 | 804 | Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐0.77, ‐0.18] |
| 16.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.86, 1.06] |
| 17 Rescue bronchodilator use: day time | 7 | 1469 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.50, ‐0.16] |
| 17.1 Parallel group studies | 7 | 1469 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.50, ‐0.16] |
| 17.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Rescue bronchodilator use: night time | 7 | 1468 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.43, ‐0.19] |
| 18.1 Parallel group studies | 7 | 1468 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.43, ‐0.19] |
| 18.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Change in use of rescue bronchodilator/day | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 19.1 Parallel group studies | 3 | 606 | Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.29, ‐0.08] |
| 20 Quality of life score: overall | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 20.1 Parallel group studies | 2 | 727 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.54 [0.39, 0.69] |
| 20.2 Cross over studies | 1 | 1545 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Quality of life score: symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 21.1 Parallel group studies | 1 | 539 | Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐0.65, ‐0.39] |
| 21.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Quality of life score: emotions | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 22.1 Parallel group studies | 1 | 539 | Mean Difference (IV, Fixed, 95% CI) | ‐0.44 [‐0.56, ‐0.32] |
| 22.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Quality of life score: exposure to environmental stimuli | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 23.1 Parallel group studies | 1 | 539 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.31, ‐0.11] |
| 23.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Qualtiy of life score: activity limitations | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 24.1 Parallel group studies | 1 | 539 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.31, ‐0.11] |
| 24.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Bronchial hyperreactivity‐ log PD20/PC20 methacholine or histamine | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 25.1 Parallel group studies | 2 | 200 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐1.26, 0.51] |
| 25.2 Cross over studies | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Bronchoprotection to methacholine challenge(protection ratio vs. baseline) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 26.1 Parallel group | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.03, 0.23] |
| 27 Adverse events‐all | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 Parallel group studies | 5 | 983 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.80, 1.59] |
| 27.2 Cross over studies | 2 | 264 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.34, 1.59] |
| 28 Adverse events‐ palpitations | 12 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 28.1 Parallel group studies | 11 | 3239 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.62, 1.74] |
| 28.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.69] |
| 29 Adverse events‐headache | 14 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 29.1 Parallel group studies | 13 | 3737 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [1.02, 1.61] |
| 29.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 30 Adverse events‐ tremor | 13 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 30.1 Parallel group studies | 12 | 3780 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.43, 1.07] |
| 30.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 31 Adverse events‐ cramps | 5 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 31.1 Parallel group studies | 4 | 1334 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.12 [0.99, 4.54] |
| 31.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 32 Exacerbations asthma‐major | 14 | 28814 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.78, 1.03] |
| 32.1 Exacerbations (similar definition) ‐ parallel group studies | 9 | 2889 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.75, 1.06] |
| 32.2 Exacerbations (less precise definition) ‐ parallel group studies | 5 | 25925 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.72, 1.12] |
| 33 Asthma attacks ‐ day | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 33.1 Parallel group studies | 1 | 301 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.26, 0.06] |
| 34 Asthma attacks ‐ night | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 34.1 Parallel group studies | 1 | 1652 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐2.66, ‐1.34] |
| 35 Major excerbation rate ‐ yearly (number/patient /year) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 35.1 Parallel group studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 35.2 Cross over studies | 1 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.50, ‐0.08] |
| 36 Minor exacerbation rate (number/patient/year) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 36.1 Cross over studies | 1 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐0.85, ‐0.33] |
| 37 Deaths related to asthma | 1 | 25180 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.00 [0.67, 13.41] |
| 38 Global assessment of efficacy by patient ‐ very good/good | 5 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 38.1 Parallel group studies | 5 | 1005 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.54 [1.92, 3.36] |
| 39 Global assessment of efficacy by investigator ‐ very good/good | 2 | 446 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.57, 3.66] |
| 39.1 Parallel group studies | 2 | 446 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.57, 3.66] |
| 39.2 Crossover studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.5. Analysis.
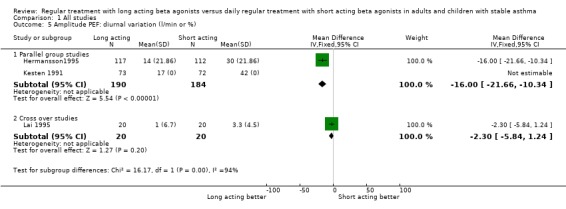
Comparison 1 All studies, Outcome 5 Amplitude PEF: diurnal variation (l/min or %).
1.6. Analysis.

Comparison 1 All studies, Outcome 6 FEV1 (litres).
1.7. Analysis.

Comparison 1 All studies, Outcome 7 % Predicted FEV1.
1.8. Analysis.
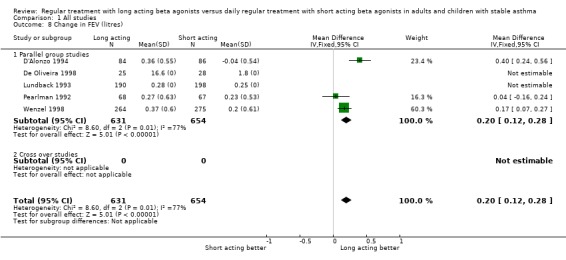
Comparison 1 All studies, Outcome 8 Change in FEV (litres).
1.9. Analysis.

Comparison 1 All studies, Outcome 9 Forced Vital Capacity (litres).
1.10. Analysis.

Comparison 1 All studies, Outcome 10 FEF25‐75 (litres/sec).
1.13. Analysis.

Comparison 1 All studies, Outcome 13 Symptom score: night time.
1.20. Analysis.

Comparison 1 All studies, Outcome 20 Quality of life score: overall.
1.21. Analysis.

Comparison 1 All studies, Outcome 21 Quality of life score: symptoms.
1.22. Analysis.

Comparison 1 All studies, Outcome 22 Quality of life score: emotions.
1.23. Analysis.
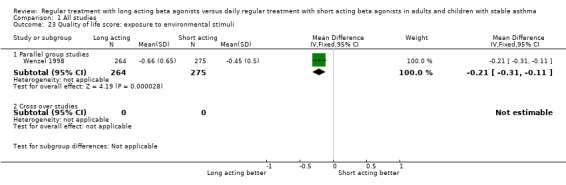
Comparison 1 All studies, Outcome 23 Quality of life score: exposure to environmental stimuli.
1.24. Analysis.

Comparison 1 All studies, Outcome 24 Qualtiy of life score: activity limitations.
1.25. Analysis.

Comparison 1 All studies, Outcome 25 Bronchial hyperreactivity‐ log PD20/PC20 methacholine or histamine.
1.26. Analysis.

Comparison 1 All studies, Outcome 26 Bronchoprotection to methacholine challenge(protection ratio vs. baseline).
1.28. Analysis.

Comparison 1 All studies, Outcome 28 Adverse events‐ palpitations.
1.29. Analysis.

Comparison 1 All studies, Outcome 29 Adverse events‐headache.
1.30. Analysis.

Comparison 1 All studies, Outcome 30 Adverse events‐ tremor.
1.31. Analysis.

Comparison 1 All studies, Outcome 31 Adverse events‐ cramps.
1.33. Analysis.

Comparison 1 All studies, Outcome 33 Asthma attacks ‐ day.
1.34. Analysis.

Comparison 1 All studies, Outcome 34 Asthma attacks ‐ night.
1.35. Analysis.

Comparison 1 All studies, Outcome 35 Major excerbation rate ‐ yearly (number/patient /year).
1.36. Analysis.

Comparison 1 All studies, Outcome 36 Minor exacerbation rate (number/patient/year).
1.37. Analysis.
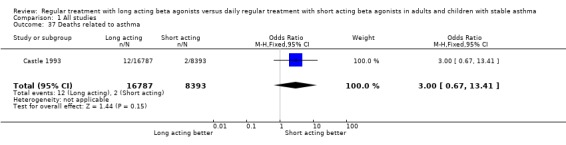
Comparison 1 All studies, Outcome 37 Deaths related to asthma.
1.39. Analysis.

Comparison 1 All studies, Outcome 39 Global assessment of efficacy by investigator ‐ very good/good.
Comparison 2. Studies with all subjects using ICS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peak expiratory flow: morning l/min | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Parallel group studies | 3 | 240 | Mean Difference (IV, Fixed, 95% CI) | 60.0 [0.80, 119.20] |
| 1.2 Cross over studies | 2 | 120 | Mean Difference (IV, Fixed, 95% CI) | 16.0 [‐55.90, 87.90] |
| 2 Peak expiratory flow: evening l/min | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Parallel group studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 48.0 [‐13.76, 109.76] |
| 2.2 Crossover studies | 2 | 120 | Mean Difference (IV, Fixed, 95% CI) | 9.0 [‐62.90, 80.90] |
| 3 Change in PEF morning | 2 | 438 | Mean Difference (IV, Fixed, 95% CI) | 29.60 [21.18, 38.02] |
| 3.1 Parallel group studies | 2 | 438 | Mean Difference (IV, Fixed, 95% CI) | 29.60 [21.18, 38.02] |
| 3.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Change in PEF evening | 2 | 438 | Mean Difference (IV, Fixed, 95% CI) | 10.77 [3.50, 18.05] |
| 4.1 Parallel group studies | 2 | 438 | Mean Difference (IV, Fixed, 95% CI) | 10.77 [3.50, 18.05] |
| 4.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Amplitude PEF: diurnal variation | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Parallel group studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐2.3 [‐5.84, 1.24] |
| 6 FEV1 litres | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Parallel group studies | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 0.18 [‐0.39, 0.75] |
| 6.2 Cross over studies | 2 | 122 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.56, 0.56] |
| 7 Change in FEV1 | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Parallel group studies | 1 | 248 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.00, 0.28] |
| 7.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Symptom score‐ day time | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Parallel group studies | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Symptom score: night time | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Parallel group studies | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐6.39, 0.79] |
| 10 Rescue bronchodilator use: whole day | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Parallel group studies | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐1.1 [‐2.53, 0.33] |
| 10.2 Cross over studies | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.86, 1.06] |
| 11 Rescue bronchodilator use: day‐time | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Parallel group studies | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Rescue bronchodilator use: night time | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Parallel group studies | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Quality of life score: overall | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Parallel group studies | 1 | 248 | Mean Difference (IV, Fixed, 95% CI) | ‐0.32 [‐0.57, ‐0.07] |
| 13.2 Cross over studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Bronchial hyperreactivity | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Parallel group studies | 2 | 200 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐1.26, 0.51] |
| 14.2 Cross over studies | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Adverse events ‐ all | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 Parallel group studies | 1 | 180 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.53, 2.95] |
| 15.2 Cross over studies | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.19, 1.44] |
| 16 Adverse events ‐ palpitations | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Parallel group studies | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.03] |
| 16.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.69] |
| 17 Adverse events ‐ headache | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Parallel group studies | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.17, 2.34] |
| 17.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 18 Adverse events ‐ tremor | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Parallel group studies | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.24, 9.09] |
| 18.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 19 Adverse events ‐ cramps | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Parallel group studies | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.04, 5.43] |
| 19.2 Cross over studies | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.26] |
| 20 Exacerbations asthma ‐ major | 2 | 370 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.48] |
| 20.1 Parallel group studies | 2 | 370 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.48] |
| 20.2 Cross over studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 1 Peak expiratory flow: morning l/min.
2.2. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 2 Peak expiratory flow: evening l/min.
2.3. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 3 Change in PEF morning.
2.4. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 4 Change in PEF evening.
2.5. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 5 Amplitude PEF: diurnal variation.
2.6. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 6 FEV1 litres.
2.7. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 7 Change in FEV1.
2.8. Analysis.
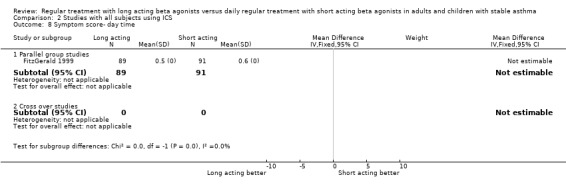
Comparison 2 Studies with all subjects using ICS, Outcome 8 Symptom score‐ day time.
2.9. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 9 Symptom score: night time.
2.10. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 10 Rescue bronchodilator use: whole day.
2.11. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 11 Rescue bronchodilator use: day‐time.
2.12. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 12 Rescue bronchodilator use: night time.
2.13. Analysis.
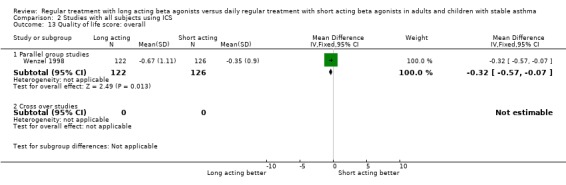
Comparison 2 Studies with all subjects using ICS, Outcome 13 Quality of life score: overall.
2.14. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 14 Bronchial hyperreactivity.
2.15. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 15 Adverse events ‐ all.
2.16. Analysis.
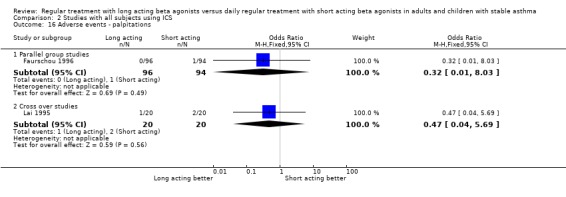
Comparison 2 Studies with all subjects using ICS, Outcome 16 Adverse events ‐ palpitations.
2.17. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 17 Adverse events ‐ headache.
2.18. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 18 Adverse events ‐ tremor.
2.19. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 19 Adverse events ‐ cramps.
2.20. Analysis.

Comparison 2 Studies with all subjects using ICS, Outcome 20 Exacerbations asthma ‐ major.
Comparison 3. Childrens studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse events ‐ palpitations | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Parallel group studies | 1 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.19, 4.79] |
| 1.2 Cross over studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Adverse events ‐ headache | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Parallel group studies | 1 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.85, 2.04] |
| 2.2 Cross over studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Adverse events ‐ tremor | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Parallel group studies | 1 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.19, 4.79] |
| 3.2 Cross over studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Exacerbations asthma ‐ major | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Parallel group studies | 1 | 568 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.74, 1.52] |
| 4.2 Cross over studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Adverse events‐all | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Parallel group studies | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Cross over studies | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.19, 1.44] |
| 6 Peak expiratory flow: morning l/min | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Parallel group studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Cross over studies | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Peak expiratory flow: evening l/min | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Parallel group studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Crossover studies | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 FEV1 litres | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Parallel group studies | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cross over studies | 1 | 82 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Bronchial hyperreactivity ‐ log PD/PC 20 methacholine or histamine | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Parallel group studies | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Cross over studies | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.1. Analysis.

Comparison 3 Childrens studies, Outcome 1 Adverse events ‐ palpitations.
3.2. Analysis.

Comparison 3 Childrens studies, Outcome 2 Adverse events ‐ headache.
3.3. Analysis.

Comparison 3 Childrens studies, Outcome 3 Adverse events ‐ tremor.
3.4. Analysis.
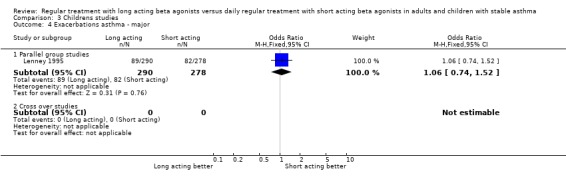
Comparison 3 Childrens studies, Outcome 4 Exacerbations asthma ‐ major.
3.5. Analysis.

Comparison 3 Childrens studies, Outcome 5 Adverse events‐all.
3.6. Analysis.

Comparison 3 Childrens studies, Outcome 6 Peak expiratory flow: morning l/min.
3.7. Analysis.

Comparison 3 Childrens studies, Outcome 7 Peak expiratory flow: evening l/min.
3.8. Analysis.

Comparison 3 Childrens studies, Outcome 8 FEV1 litres.
3.9. Analysis.
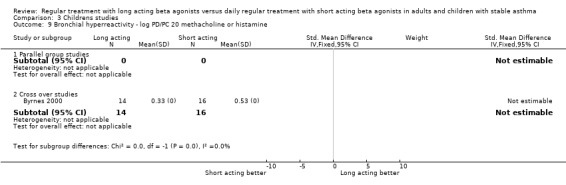
Comparison 3 Childrens studies, Outcome 9 Bronchial hyperreactivity ‐ log PD/PC 20 methacholine or histamine.
Comparison 4. Asthma severity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peak expiratory flow: morning l/min | 9 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Mild to moderate asthma | 8 | 2185 | Mean Difference (IV, Fixed, 95% CI) | 30.48 [23.72, 37.24] |
| 1.3 Moderate ‐ severe asthma | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Peak expiratory flow: evening l/min | 8 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Mild ‐ moderate asthma | 8 | 2460 | Mean Difference (IV, Fixed, 95% CI) | 18.30 [12.31, 24.29] |
| 2.3 Moderate ‐ severe asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Change in PEF morning | 8 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Mild ‐ moderate asthma | 7 | 1659 | Mean Difference (IV, Fixed, 95% CI) | 32.07 [26.89, 37.26] |
| 3.3 Moderate ‐ severe asthma | 1 | 190 | Mean Difference (IV, Fixed, 95% CI) | 29.0 [12.13, 45.87] |
| 4 Change in PEF evening | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Mild ‐ moderate asthma | 5 | 1533 | Mean Difference (IV, Fixed, 95% CI) | 13.29 [8.56, 18.02] |
| 4.3 Severe asthma | 1 | 190 | Mean Difference (IV, Fixed, 95% CI) | 10.0 [‐1.43, 21.43] |
| 5 Amplitude PEF: diurnal variation (l/min or %) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Mild ‐ moderate asthma | 2 | 231 | Mean Difference (IV, Fixed, 95% CI) | ‐16.0 [‐21.66, ‐10.34] |
| 5.3 Moderate ‐ severe asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 FEV1 (litres) | 9 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Mild asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Mild ‐ moderate asthma | 8 | 1909 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.13, 0.28] |
| 6.3 Moderate ‐ severe asthma | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.13, 0.37] |
| 7 % Predicted FEV1 | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Mild asthma | 1 | 22 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [‐1.06, 25.06] |
| 7.2 Mild ‐ moderate asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Moderate ‐ severe asthma | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Change in FEV (litres) | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Mild ‐ moderate asthma | 5 | 1285 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.12, 0.28] |
| 9 Forced Vital Capacity (litres) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Mild ‐ moderate asthma | 4 | 1118 | Mean Difference (IV, Fixed, 95% CI) | 0.24 [0.13, 0.36] |
| 10 FEF25‐75 (litres/sec) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Mild ‐ moderate asthma | 2 | 305 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [0.18, 0.66] |
| 11 Symptom score ‐ whole day | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Mild ‐ moderate asthma | 3 | 606 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.43, ‐0.11] |
| 12 Symptom score ‐ day time | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Mild ‐ moderate asthma | 3 | 678 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.24, ‐0.05] |
| 12.2 Severe asthma | 1 | 180 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Symptom score: night time | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Mild ‐ moderate asthma | 4 | 731 | Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.33, ‐0.09] |
| 14 %days without asthma symptoms | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Mild ‐ moderate asthma | 3 | 414 | Mean Difference (IV, Fixed, 95% CI) | 10.34 [1.80, 18.88] |
| 15 % nights without asthma awakenings | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 15.1 Mild ‐ moderate asthma | 5 | 943 | Mean Difference (IV, Fixed, 95% CI) | 12.12 [7.80, 16.43] |
| 16 Rescue bronchodilator use: whole day | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 16.1 Mild ‐ moderate asthma | 4 | 659 | Mean Difference (IV, Fixed, 95% CI) | ‐0.55 [‐0.90, ‐0.19] |
| 17 Rescue bronchodilator use: day time | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 17.1 Mild ‐ moderate asthma | 5 | 1086 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐0.44, ‐0.09] |
| 18 Rescue bronchodilator use: night time | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 18.1 Mild ‐ moderate asthma | 5 | 1086 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.42, ‐0.17] |
| 19 Quality of life score: overall | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 19.1 Mild ‐ moderate asthma | 1 | 248 | Mean Difference (IV, Fixed, 95% CI) | 0.32 [0.07, 0.57] |
| 20 Bronchial hyperreactivity | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 20.1 Mild ‐ moderate asthma | 1 | 20 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐1.26, 0.51] |
| 20.2 Moderate ‐ severe asthma | 1 | 180 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Adverse events ‐ all | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 21.1 Mild ‐ moderate asthma | 2 | 369 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.66, 1.75] |
| 21.2 Moderate ‐ severe asthma | 1 | 180 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.53, 2.95] |
| 22 Adverse events ‐ palpitations | 10 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 22.1 Mild ‐ moderate asthma | 9 | 2815 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.61, 1.78] |
| 22.2 Moderate ‐ severe asthma | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.03] |
| 23 Adverse events ‐ headache | 12 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 23.1 Mild ‐ moderate asthma | 11 | 3313 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [1.01, 1.62] |
| 23.2 Moderate ‐ severe asthma | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.17, 2.34] |
| 24 Adverse events ‐ tremor | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 24.1 Mild ‐ moderate asthma | 10 | 3356 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.40, 1.03] |
| 24.2 Moderate ‐ severe asthma | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.24, 9.09] |
| 25 Adverse events ‐ cramps | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 25.1 Mild ‐ moderate asthma | 2 | 910 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.53 [1.07, 5.97] |
| 25.2 Moderate ‐ severe asthma | 1 | 190 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.04, 5.43] |
| 26 Exacerbations asthma ‐ major | 11 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 26.1 Mild asthma | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Mild ‐ moderate asthma | 9 | 2847 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.73, 1.04] |
| 26.3 Moderate ‐ severe asthma | 2 | 370 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.48] |
| 27 Global assessment of efficacy by patient ‐ very good/good | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 27.1 Mild ‐ moderate asthma | 3 | 657 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.08 [2.19, 4.32] |
4.1. Analysis.

Comparison 4 Asthma severity, Outcome 1 Peak expiratory flow: morning l/min.
4.2. Analysis.

Comparison 4 Asthma severity, Outcome 2 Peak expiratory flow: evening l/min.
4.3. Analysis.

Comparison 4 Asthma severity, Outcome 3 Change in PEF morning.
4.4. Analysis.

Comparison 4 Asthma severity, Outcome 4 Change in PEF evening.
4.5. Analysis.
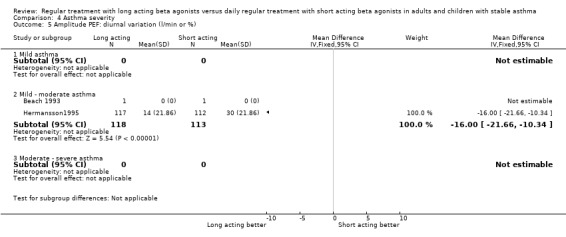
Comparison 4 Asthma severity, Outcome 5 Amplitude PEF: diurnal variation (l/min or %).
4.6. Analysis.

Comparison 4 Asthma severity, Outcome 6 FEV1 (litres).
4.7. Analysis.

Comparison 4 Asthma severity, Outcome 7 % Predicted FEV1.
4.8. Analysis.

Comparison 4 Asthma severity, Outcome 8 Change in FEV (litres).
4.9. Analysis.

Comparison 4 Asthma severity, Outcome 9 Forced Vital Capacity (litres).
4.10. Analysis.
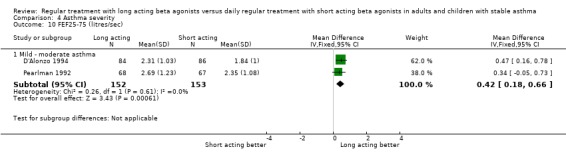
Comparison 4 Asthma severity, Outcome 10 FEF25‐75 (litres/sec).
4.11. Analysis.

Comparison 4 Asthma severity, Outcome 11 Symptom score ‐ whole day.
4.12. Analysis.

Comparison 4 Asthma severity, Outcome 12 Symptom score ‐ day time.
4.13. Analysis.

Comparison 4 Asthma severity, Outcome 13 Symptom score: night time.
4.14. Analysis.

Comparison 4 Asthma severity, Outcome 14 %days without asthma symptoms.
4.15. Analysis.

Comparison 4 Asthma severity, Outcome 15 % nights without asthma awakenings.
4.16. Analysis.

Comparison 4 Asthma severity, Outcome 16 Rescue bronchodilator use: whole day.
4.17. Analysis.

Comparison 4 Asthma severity, Outcome 17 Rescue bronchodilator use: day time.
4.18. Analysis.
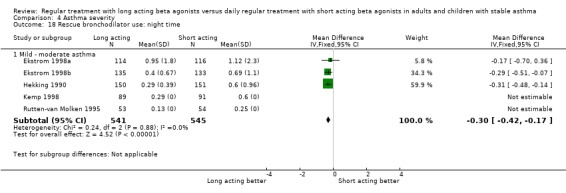
Comparison 4 Asthma severity, Outcome 18 Rescue bronchodilator use: night time.
4.19. Analysis.

Comparison 4 Asthma severity, Outcome 19 Quality of life score: overall.
4.20. Analysis.

Comparison 4 Asthma severity, Outcome 20 Bronchial hyperreactivity.
4.21. Analysis.

Comparison 4 Asthma severity, Outcome 21 Adverse events ‐ all.
4.22. Analysis.

Comparison 4 Asthma severity, Outcome 22 Adverse events ‐ palpitations.
4.23. Analysis.

Comparison 4 Asthma severity, Outcome 23 Adverse events ‐ headache.
4.24. Analysis.
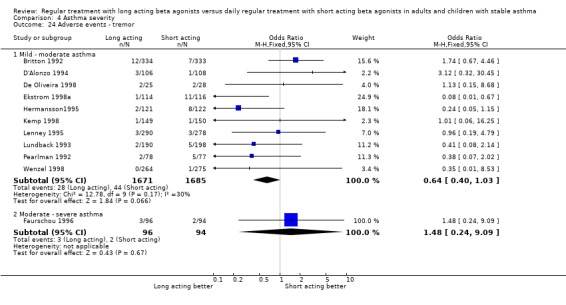
Comparison 4 Asthma severity, Outcome 24 Adverse events ‐ tremor.
4.25. Analysis.

Comparison 4 Asthma severity, Outcome 25 Adverse events ‐ cramps.
4.26. Analysis.
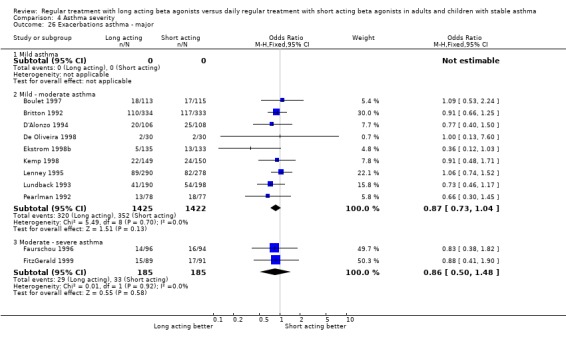
Comparison 4 Asthma severity, Outcome 26 Exacerbations asthma ‐ major.
4.27. Analysis.

Comparison 4 Asthma severity, Outcome 27 Global assessment of efficacy by patient ‐ very good/good.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beach 1993.
| Methods | STUDY DESIGN: Parallel group. 6 week treatment period. Single centre ‐ UK. RANDOMISATION: Yes, method not stated. BLINDING: Double blind using identical inhalers. WITHDRAWALS/DROP OUTS: All subjects completed study. COMPLIANCE: No details. CONFOUNDERS: None apparent. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 20 Adults M = 13,F = 7 Mean age 39 yrs BASELINE SEVERITY: Symptommatic asthma INCLUSION : Taking ICS regularly EXCLUSION:Oral beta agonist/theophylline, ipratropium | |
| Interventions | LONG ACTING BETA AGONIST: Salmterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400 mcg BD DEVICE: Diskhaler TREATMENT PERIOD: 6 weeks RESCUE: Short acting beta2 agonist‐ salbutamol 400 mcg inhalation PRN CO‐INTERVENTIONS: All on, ICS‐ mean dose 575 & 610 mcg. | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, PD20 Methacholine. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Bensch 2001.
| Methods | STUDY DESIGN: Parallel group. Multi centre, 26 in USA. 12 week treatment period. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, placebo controlled. Matching capsules and devices. WITHDRAWALS/DROP OUTS: 83described, 35 due to adverse events. COMPLIANCE: Assessed by counting capsules and weighing canisters, >80% in all gouprs. CONFOUNDERS: Baseline characteristics similar for all groups. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 541 randomised, 535 ITT M = 224, F = 317 ADULT Mean age 5.5 yrs (SD14.6) BASELINE SEVERITY: Mild‐moderate persistent asthma. INCLUSION : Diagnosis of asthma, requiring daily use of inhaled SABA. Baseline FEV1 40 to 80% predicted, > 15% reversibility to inhaled SABA EXCLUSION: URTI, hospitalization/asthma exacerbation < 4 weeks, serious illness. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12/ 24 mcg BD SHORT ACTING BETA AGONIST: Albuterol 180 mcg QDS PLACEBO: Placebo QDS DEVICE: LABA Aerolizer DP device & SABA MDI TREATMENT PERIOD: 12weeks RESCUE: Short acting beta2 agonist‐ albuterol 90 mcg inhalation PRN CO‐INTERVENTIONS: ICS 51%, Slow release theophylline 17%. | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25 to 75%, PEF, Rescue albuterol, asthma symptom score, asthma exacerbations, adverse events. | |
| Notes | Symptom Score‐ breathlessness, chest tightness, wheezing, cough; scaled 0‐4. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Boulet 1997.
| Methods | STUDY DESIGN: Parallel group. Multi centre, Canada. 12 week treatment period. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 21 described, 4 due to adverse events. COMPLIANCE: Not assessed objectively. CONFOUNDERS: Baseline characteristics similar for all groups. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 300 screened, 228 ITT M = 128, F = 100 ADULT Mean age39 yrs (SD16) BASELINE SEVERITY: Mild‐moderate persistent asthma. INCLUSION : Requiring daily use of inhaled SABA for 6 months. Symptoms in 4/7 days run in. Baseline FEV1 50‐80% predicted, >15% reversibility to inhaled SABA EXCLUSION: use of oral steroids, theophylline or ipratropium | |
| Interventions | LONG ACTING BETA AGONIST Salmeterol 50mcg BD SHORT ACTING BETA AGONIST: Albuterol 180 mcg QDS PLACEBO: Placebo BD DEVICE: MDI TREATMENT PERIOD: 12weeks RESCUE: Short acting beta2 agonist‐ salbutamol 100 mcg inhalation PRN CO‐INTERVENTIONS: ICS >70%, cromones, anti histamines, immunotherapy | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV25‐75%, PEF, Rescue albuterol, asthma symptom score, night awakenings, asthma exacerbations, adverse events. | |
| Notes | Symptom Score‐ breathlessness, chest tightness, wheezing, cough Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Britton 1992.
| Methods | STUDY DESIGN: Parallel group. Multi centre, Europe‐ 62 centres . 52 week treatment period. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 60 described during treatment , mainly due to asthma and poor compliance. COMPLIANCE: Recorded but no published. CONFOUNDERS: Baseline characteristics similar for all groups. QUALITY: Jadad 5. Cochrane A | |
| Participants | N = 796 screened, 667 randomised ( ITT) M = 332, F = 335 ADULT Mean age 49 yrs (range 18 to 81) BASELINE SEVERITY: Moderate persistent asthma. INCLUSION : Diagnosis of asthma with regular symptoms, symptoms score > 2 on 4/7 days run in, Baseline FEV1 > 50 predicted, > 15% reversibility to inhaled SABA EXCLUSION: LRTI, hospitalization with asthma < 14 days, use of oral steroids > 20 mg /day, theophylline or ipratropium | |
| Interventions | LONG ACTING BETA AGONIST Salmeterol 50mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: Placebo BD DEVICE: MDI TREATMENT PERIOD: 12weeks RESCUE: Short acting beta2 agonist‐ salbutamol 100 mcg inhalation PRN CO‐INTERVENTIONS: ICS >61%, OS 15%, cromones. | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV25‐75%, PEF, Rescue use, asthma symptom score, night awakenings, asthma exacerbations, adverse events. | |
| Notes | Symptom Score‐ 0 = none to 5 = severe. Exacerbations asthma defined as worsening of asthma symptoms recorded as an AE requiring change in therapy other than inhaled SABA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Study investigators unaware as to order of treatment group assignment (Cochrane Grade A) |
Byrnes 2000.
| Methods | STUDY DESIGN: Crossover, 3 way design. 4 week per treatment. Single centre UK. RANDOMISATION: Yes, computer generated random code. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 5 described during treatment , 1 due lack efficacy,3 FTA. COMPLIANCE: Assessed by counting unused blisters, >80%. CONFOUNDERS: no washout period at cross over, used second 2 week data only.. QUALITY: Jadad 5. Cochrane A | |
| Participants | N = 52 screened, 45 randomised ( ITT) CHILDREN. M = 31 F = 14 Mean age 9 yrs (sd 2.8) BASELINE SEVERITY: Symptomatic asthma on medium dose ICS. INCLUSION : Asthma requiring > 400mcg ICS . > 15% reversibility on PEF or FEV1 to inhaled SABA EXCLUSION: URTI/ use of OS/ hospitalization with asthma < 4 weeks, theophylline or ipratropium use. | |
| Interventions | LONG ACTING BETA AGONIST Salmeterol 50/ 100 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: Placebo BD DEVICE: Diskhaler TREATMENT PERIOD: 4 weeks RESCUE: Short acting beta2 agonist‐ salbutamol 200 mcg inhalation up to 6 times daily CO‐INTERVENTIONS: All on ICS >400 mcg. | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25‐75%, PEF, Rescue use, asthma symptom score, symptom free days, adverse events , BHR (in subgroup). | |
| Notes | No description of asthma score. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Study investigators unaware as to order of treatment group assignment (Cochrane Grade A) |
Castle 1993.
| Methods | STUDY DESIGN: Parallel group, general practice setting in UK‐ 3516 GPs. 16 weeks treatment. RANDOMISATION: Yes, computer generated random code, blocks of 6. BLINDING: double blind, double dummy, matching devices. Monitoring staff unblinded. WITHDRAWALS/DROP OUTS: 6481, causes fully described. COMPLIANCE: Not assessed/ reported. CONFOUNDERS: Groups well balanced by characteristics. Possibility of confounding by severity of asthma. QUALITY: Jadad 5. Cochrane A | |
| Participants | N = 25180 randomised (TT) Adults, M = 10479 F = 14701 Mean age not reported, range 18 to > 60 BASELINE SEVERITY: mild 17%, moderate 65%, severe 17% as categorised at randomisation by GP. INCLUSION : Clinical diagnosis of asthma requiring regular SABA EXCLUSION: Beta blocker use, serious uncontrolled diseases , pregnancy. | |
| Interventions | LONG ACTING BETA AGONIST Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: Placebo BD DEVICE: MDI TREATMENT PERIOD: 16 weeks RESCUE: Patients usual rescue agent PRN CO‐INTERVENTIONS: ICS 69%, OS 4.7%, Theophyllines, cromones, ipratropium‐ stable doses | |
| Outcomes | OUTCOMES: Deaths related to asthma, Admission to hospital‐ respiratory or asthma related. other serious adverse events related to asthma, withdrawals for respiratory or related to asthma. | |
| Notes | No definition of asthma exacerbation. Serious adverse event related to asthma= event requiring hospital admission, prolonging stay, life threatening or severely disabling. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Study investigators unaware as to order of treatment group assignment (Cochrane Grade A) |
D'Alonzo 1994.
| Methods | STUDY DESIGN: Three treatment parallel group, multicentre (11) study in USA, 12 wks RANDOMISATION: Yes, method not given. BLINDING:Double blind, double dummy, with 2 matching inhalers. WITHDRAWALS:42/322 , by groups ‐ 15 in salmeterol , 16 in albuterol, 11in placebo CONFOUNDERS: differential rates of ICS and cromone use in regular and prn group, use of theophyllines in run in period QUALITY: Jadad = 4, Cochrane B | |
| Participants | N = 322 Albuterol = 108, placebo =108, salmeterol = 106 AGE‐ means ‐albuterol 31(14), placebo 28(12), salmeterol 29(12) BASELINE SEVERITY: Chronic symptomatic asthma. INCLUSION: Diagnosis asthma by ATS criteria, requiring daily drug treatment for > 6 months. Baseline FEV1 50‐70% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: Smokers | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 42 mcg BD SHORT ACTING BETA AGONIST: Albuterol 180mcg QDS PLACEBO:placebo QDS DEVICE: MDI PERIOD:12 weeks RESCUE:albuterol 90mcg prn CO‐INTERVENTIONS: ICS ‐ used by 20% on placebo , 24% on albuterol, 21% on salmeterol ORAL STEROIDS ‐ not at randomisation CROMONES‐used by 9% on placebo , 6% on albuterol, 10% on salmeterol THEOPHYLIINES‐ used only during run in by 46% on placebo , 50% on albuterol, 43% on salmeterol ORAL BETA AGONISTS ‐ not permitted | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV25‐75%, PEF, Rescue use, asthma symptom score, symptom free days & nights, adverse events . | |
| Notes | Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. Symtom Score‐ composite based on individual scores for breathlessness, chest tightness, wheezing, cough. Scale : 0 = none to 5 = severe, activities cancelled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
De Carli 1995.
| Methods | STUDY DESIGN: Parallel group, multicentre, 27 in Italy. 12 weeks initially, with 12 month follow on. RANDOMISATION: Yes, used PACT computer code, allocation blocks of 2. BLINDING: open label, not blinded. WITHDRAWALS/DROP OUTS: 27 withdrawals detailed in 3mths, 1 in follow up period COMPLIANCE: Not assessed CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 3. Cochrane A | |
| Participants | N = 252 screened RANDOMISED/COMPLETED = 234 ITT, adult, M = 116 F = 118 Mean age: 45 (range 18 to 81) BASELINE SEVERITY: Mild to moderate asthma INCLUSION : Baseline FEV1 50 to 80% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: none specified. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: none DEVICE: MDI TREATMENT PERIOD: 12 weeks initial, 12 months follow on. RESCUE Salbutamol prn CO‐INTERVENTIONS: ICS 10%, OS < 20mg/day 4% | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events. Exacerbations. Efficacy score‐patient and investigator rated. Asthma QOL score | |
| Notes | Exacerbations‐ not defined. Symptom Score‐ Night‐time 0‐4 (none ‐ so severe that no sleep possible). Daytime Symptom Score‐ 0 = none to 5 = severe. LWAQ for QOL measure (Italian version) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Study investigators unaware as to order of treatment group assignment (Cochrane Grade A) |
De Oliveira 1998.
| Methods | STUDY DESIGN: Parallel group, single centre, Brazil, 4 wks. RANDOMISATION: Yes, method not stated. BLINDING: double blind, double dummy. WITHDRAWALS/DROP OUTS: 7 described after randomization. COMPLIANCE: No details CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 136 ENROLLED/ 60 RANDOMISED/53 COMPLETED, ADULT , M=17 F=43 Mean age: 37 (range 18‐64) BASELINE SEVERITY: Mild‐moderate symptomatic asthma INCLUSION : Diagnosis asthma by ATS criteria, Baseline FEV1 >50% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: Use of theophyllines or anticholinergic, except in acute attack. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: placebo BD DEVICE: MDI. TREATMENT PERIOD: 4 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS > 42%, | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events, | |
| Notes | Symptom Score‐ Night‐time 0‐4 (none ‐ so severe that no sleep possible). Day‐time 0‐4 (no symptoms ‐ symptoms so severe normal activities not possible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Ekstrom 1998a.
| Methods | STUDY DESIGN: Parallel group, 3 treatment arms; multicentre, 28 centres Scaninavia. 12 wks. RANDOMISATION: Yes, computer generated random order, balanced blocks.. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 32 described, due to asthma. COMPLIANCE: Not assessed/ reported. CONFOUNDERS: Groups well balanced by characteristics. QUALITY: Jadad 5. Cochrane A | |
| Participants | N = 343 Adults, M = 164 F = 179 Mean age 48 (RANGE 18 to 82) BASELINE SEVERITY: moderate stable asthma. INCLUSION : Diagnosis asthma by ATS criteria. Baseline FEV1 40 to 80% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: none stated in paper. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12 mcg BD SHORT ACTING BETA AGONIST: Terbutaline 500mcg QDS PLACEBO: Placebo QDS DEVICE: Dry powder device‐ turbuhaler. TREATMENT PERIOD: 12 weeks RESCUE: Terbutaline 250 mcg via turbuhaler PRN CO‐INTERVENTIONS: ICS 89%, cromones 2% ‐ stable doses OS 2 subjects | |
| Outcomes | OUTCOMES: FEV1, PEF, Rescue use, asthma symptom score, adverse events | |
| Notes | Symptom Score‐ breathlessness, chest tightness, wheezing, cough. Scale :0 ‐ 3 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Study investigators unaware as to order of treatment group assignment (Cochrane Grade A) |
Ekstrom 1998b.
| Methods | STUDY DESIGN: Parallel group, 3 treatment arms; multicentre, 25 centres Norway, Sweden, Spain, Italy. 12 wks. RANDOMISATION: Yes, method not given. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 38 described. 27 to asthma, 11 to adverse events. COMPLIANCE: Not assessed/ reported. CONFOUNDERS: Groups well balanced by characteristics. Excess withdrawals from SABA group, 10 subjects did not fully meet inclusion criteria. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 397 Adults, M = 232 F = 179 Mean age 47 (RANGE 18 to 79) BASELINE SEVERITY: mild ‐ moderate asthma. INCLUSION : Diagnosis asthma by ATS criteria. Baseline FEV1 50‐80% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: none stated in paper. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 6 mcg BD SHORT ACTING BETA AGONIST: Terbutaline 500mcg QDS PLACEBO: Placebo QDS DEVICE: Dry powder device. TREATMENT PERIOD: 12 weeks RESCUE: Terbutaline 250 mcg via turbuhaler PRN CO‐INTERVENTIONS: ICS 80%, cromones 5% (at stable dosages) | |
| Outcomes | OUTCOMES: FEV1, PEF, Rescue use, asthma symptom score, adverse events. asthma deterioration | |
| Notes | Symptom Score‐ breathlessness, chest tightness, wheezing, cough. Scale :0 ‐ 3. Asthma deterioration leading to withdrawal reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Faurschou 1996.
| Methods | STUDY DESIGN: Parallel group, multicentre, 20 centres UK, Norway, Denmark. 6 wks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 17 described. COMPLIANCE: Not assessed/ reported. CONFOUNDERS: Groups well balanced by characteristics. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 286 RECRUITED, 190 ENROLLED. Adults, M = 100 F=90 Mean age 51 (RANGE 18‐80) BASELINE SEVERITY: moderate to severe symptomatic asthma. INCLUSION : Baseline FEV1 30‐75% predicted, >15% FEV1 reversibility to SABA. Symptoms on 4/7 days run in, using > 1200mcg BUD or 1500mcg BDP EXCLUSION: URTI/ Change in asthma medication/ exacerbation asthma within 2 wks. Maintenance with OS. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 100 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400mcg QDS PLACEBO: Placebo BD DEVICE: Dry powder device‐ DISKHALER TREATMENT PERIOD: 6 weeks RESCUE: Salbutamol 200 mcg PRN CO‐INTERVENTIONS: ALL ON ICS . theophyline 18% Ipratroprium 10% | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25 to 75%, PEF, Rescue use, asthma symptom score, symptom free days & nights, adverse events . Efficacy rating | |
| Notes | Symptom Score‐ Night‐time 0 to 3 (none ‐ so severe that no sleep possible). Day‐time 0‐4 (no symptoms ‐ symptoms so severe normal activities not possible). Exacerbations asthma defined as worsening of asthma requiring a change in therapy . | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
FitzGerald 1999.
| Methods | STUDY DESIGN: Parallel group, multicentre, 15 centres Canada. RANDOMISATION: Yes, no method stated. 24 wks. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 54 described. COMPLIANCE: Not assessed/ reported. CONFOUNDERS: Groups well balanced by characteristics. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 374 RECRUITED, 271 RANDOMISED. Adults, M = 116 F = 155 Mean age 36 (SD 13) BASELINE SEVERITY: moderate to severe asthma. INCLUSION : Diagnosis asthma by ATS criteria. > 15% FEV1 reversibility to SABA. Using ICS 400 to 1200 mcg for > 1mth. PC20 methacholine < 8mg/ml EXCLUSION: URTI/ Change in asthma medication/ exacerbation asthma within 2 months. Smoking. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12 mcg BD SHORT ACTING BETA AGONIST: Albuterol 200mcg QDS PLACEBO: Placebo QDS DEVICE: Dry powder device. TEATMENT PERIOD: 24 weeks RESCUE:Albuterol 100 mcg PRN CO‐INTERVENTIONS: ALL ON ICS . Theophylinne, Ipratroprium, Cromones, antihistamines‐ at fixed doses. | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV25‐75%, PEF, Rescue use, asthma symptom score, exacerbations asthma, BHR, adverse events . | |
| Notes | Symptom Score‐ 0 = best to 4 = worst. Exacerbation defined as that requiring increase in corticosteroid cover. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Hekking 1990.
| Methods | STUDY DESIGN: Parallel group, multicentre, Holland. 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 45 described after randomization. COMPLIANCE: Not assessed / reported. CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 301 ENROLLED/ RANDOMISED, ADULT, M = 157 F=144 Mean age: 40 (SD 14) BASELINE SEVERITY: Stable phase asthma INCLUSION : Stable phase asthma, Baseline FEV1 <80% predicted, >15% FEV1 reversibility to SABA. EXCLUSION: Use of theophyllines, oral beta_2 agonists or anticholinergics. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200mcg QDS PLACEBO: placebo BD DEVICE: MDI TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: stable dose ICS, cromones. | |
| Outcomes | OUTCOMES: PEF, Rescue use, asthma attacks. Efficacy rating | |
| Notes | Asthma attacks not defined. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Hermansson1995.
| Methods | STUDY DESIGN: Parallel group, multicentre, 23 centres Europe. 4 wks. RANDOMISATION: Yes, no method stated. BLINDING: open label, not blinded. WITHDRAWALS/DROP OUTS: 15 after randomization. COMPLIANCE: 93 ‐ 96% reported. CONFOUNDERS: Groups well balanced by characteristics. QUALITY: Jadad 2. Cochrane B | |
| Participants | N = 243 RANDOMISED. Adults, M = 120 F = 123 Mean age 48 (RANGE 18 to 78) BASELINE SEVERITY: mild to moderate asthma. INCLUSION : Baseline FEV1 > 75% predicted, > 15% FEV1 reversibility to SABA. Symptom score >2 on 4/7 days run in EXCLUSION: LRTI/ exacerbation asthma within 1 mth. OS > 20mg/day | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Terbutaline 500mcg QDS PLACEBO: none DEVICE: Dry powder devices‐ diskhaler, turbuhaler. TREATMENT PERIOD: 4 weeks RESCUE:Salbutamol 400 mcg PRN CO‐INTERVENTIOS: ICS 73% . OS 3% Cromones, | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events . Efficacy rating | |
| Notes | Symptom Score‐ Night‐time 0 to 4 (none ‐ so severe that no sleep possible). Day‐time 0 to 5 (no symptoms ‐ symptoms so severe normal activities not possible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Juniper 1995.
| Methods | STUDY DESIGN: 3 way cross over, multicentre, 14 centres Canada, 4 wks. RANDOMISATION: Yes, no method stated. BLINDING: Double blind, double dummy, matching inhalers. WITHDRAWALS/DROP OUTS: 21 described after randomization. COMPLIANCE: >70% reported for all but 7 subjects. CONFOUNDERS: QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 140 RANDOMISED. Adults, M = 66 F = 74 Mean age 37.5 (sd 14.5) BASELINE SEVERITY: mild to moderate asthma. INCLUSION : Baseline FEV1 > 60% predicted, > 15% FEV1 reversibility to SABA. Symptom score > 2 on 4/7 days run in EXCLUSION: Exacerbation asthma within 1 mth, emergency room visit > 3 mths, uncontrolled illness, pregnancy. OS within 1mth. Theophylline . | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: placebo QDS DEVICE: MDI. TREATMENT PERIOD: 4 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS 77%. Cromones 15%, 30% none. | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25‐75%, PEF, Rescue use, asthma symptom score, symptom free days & nights, adverse events, AQOL scores. | |
| Notes | AQOL score measures‐symptoms, emotions, activity limitation, environment‐overall scores + individual domains | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Kemp 1998.
| Methods | STUDY DESIGN: Parallel group, multicentre, 14 centres Canada, 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: Double blind, double dummy, matching inhalers. WITHDRAWALS/DROP OUTS: 41 described after randomization. COMPLIANCE: > 70% reported for all but 7 subjects. CONFOUNDERS: QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 451 RANDOMISED. Adults, M = 262 F = 189 Mean age 31 (sd 14) BASELINE SEVERITY: mild ‐ moderate asthma. INCLUSION : Diagnosis asthma by ATS criteria. Baseline FEV1 50‐80% predicted, >15% FEV1 reversibility to SABA. Requiring daily drug treatment for > 6 mths. EXCLUSION: smoking. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Albuterol 180 mcg QDS PLACEBO: placebo QDS DEVICE: MDI & dry powder device. TREATMENT PERIOD: 12 weeks RESCUE: Albuterol 100 mcg PRN CO‐INTERVENTIONS: ICS 55 to 70 % . Cromones 7 to 12 % | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25‐75%, PEF, Rescue use, asthma symptom score, symptom free days & nights, adverse events, exacerbations. | |
| Notes | Symptom Score‐ breathlessness, chest tightness, wheezing, cough. Scale : 0 to 3. Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Kesten 1991.
| Methods | STUDY DESIGN: Parallel group, multicentre, 7 centres Canada & UK. 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: Double blind, double dummy, matching inhalers. WITHDRAWALS/DROP OUTS: 12 described after randomization. COMPLIANCE: assessed by diary card, not reported. CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 309 ENROLLED, 145 RANDOMISED. Adults, M = 60 F=85 Mean age NOT REPORTED BASELINE SEVERITY: stable, symptomatic asthma. INCLUSION : Baseline FEV1 >40% predicted, >15% FEV1 reversibility to SABA. Requiring > 2 puffs rescue/day in run in EXCLUSIONuse of OS, exacerbation asthma within 1mth | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12 mcg BD SHORT ACTING BETA AGONIST: Albuterol 200 mcg QDS PLACEBO: placebo BD DEVICE: MDI. TREATMENT PERIOD: 12 weeks RESCUE: Albuterol 100 mcg PRN CO‐INTERVENTIONS: None 32%, ICS 62 % . Cromones 7 % Theophylline 32% | |
| Outcomes | OUTCOMES: FEV1, FVC, FEV 25 to 75%, PEF, Rescue use, rate asthma attacks day & night, adverse events, exacerbations. Efficacy rating | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Kozlik‐Feldman 1996.
| Methods | STUDY DESIGN: Parallel group, single centre Germany, 12 weeks RANDOMISATION: Yes, no method stated. BLINDING: not stated and no details in paper WITHDRAWALS/DROP OUTS: All completed, no withdrawals. COMPLIANCE: Not assessed CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 2. Cochrane B | |
| Participants | N = 22 RANDOMISED/COMPLETED, children, M = 15 F = 7 Mean age: 9.7 (SD 3.5) BASELINE SEVERITY: Mild asthma, not requiring additional therapy other than SABA INCLUSION : Mild asthma, requiring no preventive therapy. EXCLUSION: Requiring additional therapy for asthma. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 24 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: none DEVICE: not specified TREATMENT PERIOD: 12 weeks RESCUE: none required CO‐INTERVENTIONS: none | |
| Outcomes | OUTCOMES: FEV1, FVC, histamine provocation, beta‐receptor binding sites on mononuclear leucocytes, adverse events | |
| Notes | Histamine provocation only until subjective endpoint, not 20% fall in FEV1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Lai 1995.
| Methods | STUDY DESIGN: cross over, single centre Hong Kong. 2weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 5 described after randomization. COMPLIANCE: Not assessed CONFOUNDERS: Not analysed by ITT QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 55 ENROLLED, 25 RANDOMISED, 20 COMPLETED. Adults, M = 14 F = 6 Mean age: 41.7 (SD 3.2) BASELINE SEVERITY: Moderate to severe asthma. INCLUSION : Baseline FEV1 > 30% predicted, > 15% FEV1 reversibility to SABA. Requiring ICS > 800MCG/DAY EXCLUSION: none stated | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Albuterol 400 mcg QDS PLACEBO: placebo BD DEVICE: Dry powder device‐ diskhaler TREATMENT PERIOD: 2 weeks RESCUE: Albuterol 400 mcg PRN CO‐INTERVENTIONS: ICS all 800‐2000 mcg/day , OS. | |
| Outcomes | OUTCOMES: FEV1, PEF, Rescue use, asthma symptom score, efficacy rating, adverse events. | |
| Notes | No details on Symptom Score‐ or scale. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Leblanc 1996.
| Methods | STUDY DESIGN: 3 way cross over, multicentre 15 Canada. 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 67 described after randomization. COMPLIANCE: 93% assessed by diary card. CONFOUNDERS: Smokers included QUALITY: Jadad 4. Cochrane B | |
| Participants | N = ENROLLED, 367 RANDOMISED. Adults, M = 164 F=203 Mean age: 39 (SD 13.9) BASELINE SEVERITY: mild to moderate asthma. INCLUSION : Baseline FEV1 > 60% predicted, > 15% FEV1 reversibility to SABA. Symptoms on 4/7 days run in. EXCLUSION: methylxanthines, anticholinergic, OS | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: placebo QDS DEVICE: MDI. TEATMENT PERIOD: 12 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS >80% , cromones 7% | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom free days & nights, adverse events . | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Lenney 1995.
| Methods | STUDY DESIGN: Parallel group, conducted as 2 separate studies, multicentre 91 in 17 countries. RANDOMISATION: Yes, no method stated. BLINDING: double blind, matching devices. WITHDRAWALS/DROP OUTS: 50 described after randomization. COMPLIANCE: Not assessed. CONFOUNDERS: QUALITY: Jadad 4. Cochrane B | |
| Participants | N = ENROLLED, 847 RANDOMISED. Children , M = 534 F = 313 Mean age: 10.2 (SD 2.9) BASELINE SEVERITY: Symptommatic asthma requiring inhaled SABA therapy. INCLUSION : > 15% FEV1/PEF reversibility to SABA. Symptoms on 5/7 days run in, requiring SABA 7/14 days. EXCLUSION: Exacerbation asthma requiring hospital/ LRTI within 1 mth, current OS. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 25 mcg BD or Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg BD PLACEBO: none DEVICE: MDI or Diskhaler. TREATMENT PERIOD: 52 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS > 60%, cromones 23% | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom free days & nights, exacerbations, adverse events. | |
| Notes | Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. Symptom Score‐ Night‐time 0 to 3 (none ‐ so severe that no sleep possible). Day‐time 0 to 3 (no symptoms ‐ symptoms so severe normal activities not possible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Lipworth 1998.
| Methods | STUDY DESIGN: Parallel group‐ 5 groups, 2 centres UK. 2 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 5 described after randomization. COMPLIANCE:. assessed by diary card & counting doses not used, >75% CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N= ENROLLED, 72 RANDOMISED.67 COMPLETED. ADULT , M = 38 F = 34 Mean age: 37 (range 16 to 65) BASELINE SEVERITY: Mild to moderate asthma INCLUSION : Diagnosis asthma by ATS criteria. Baseline FEV1 > 60% predicted, > 15% FEV1 reversibility to SABA, PD20 methacholine < 1000mcg EXCLUSION: LRTI within 1 mth, current OS. Smoking within 1 yr, current pollen allergy. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 6 mcg BD/ Formoterol 12 mcg BD/ Formoterol 24 mcg BD SHORT ACTING BETA AGONIST Terbutaline 500 mcg QDS PLACEBO: Placebo QDS DEVICE: Dry powder device‐ turbuhaler. TREATMENT PERIOD: 2 weeks RESCUE: Ipratropriium PRN CO‐INTERVENTIONS: All on ICS < 2000 mcg/day , cromones stable dose | |
| Outcomes | OUTCOMES: PEF, PD20 methacholine | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Lundback 1993.
| Methods | STUDY DESIGN: Parallel group‐ multicentre 47 in 11 countries. 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 85 described after randomization. COMPLIANCE:. Not assessed CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 460 ENROLLED, 388 RANDOMISED. ADULT , M = 187 F = 201 Median age: 44 (range 19 to 79) BASELINE SEVERITY: Mild to moderate asthma INCLUSION : Baseline FEV1 > 50% predicted, > 15% FEV1 reversibility to SABA. Symptoms on 4/7 days run in. EXCLUSION: OS 20mg/day, uncontrolled illness. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 200 mcg QDS PLACEBO: Placebo BD DEVICE: Dry powder device‐ diskhaler. TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol 200 mcg PRN CO‐INTERVENTIONS: ICS 55%, os 10%. cromones stable dose | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events . exacerbations | |
| Notes | Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Pearlman 1992.
| Methods | STUDY DESIGN: parallel‐group( 3), multicentre (8) in USA RANDOMIISATION: Randomised‐ means and methods not described. BLINDING: double‐blind, placebo controlled using 2 identical inhalers WITHDRAWALS: 33 DESCRIBED COMPLIANCE : Not reported in paper. CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad score = 4. COCHRANE = B | |
| Participants | N = 234, ADULT/ADOLESCENT M = 150, F = 84 Mean age = 27.3. range 12 to 73yr BASELINE SEVERITY: Mild‐moderate asthma INCLUSION: Baseline FEV150‐80% predicted. Diagnosis asthma by ATS definition,FEV1 reversiblility to albuterol >15%. Requiring daily beta agonist treatment during preceeeding 6 months. EXCLUSION: smoking, theophylline and oral beta agonist | |
| Interventions | LONG ACTING BETA AGONIST : Salmeterol 42 mcg bd SHORT ACTING BETA AGONIST :Albuterol 180 mcg qds PLACEBO: placebo qds DEVICE:MDI PERIOD TREATMENT: 12 weeks RESCUE: Albuterol 90 mcg PRN COINTERVENTIONS: ICSS 40%, cromones 7%, | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events . exacerbations | |
| Notes | Symtom Score‐ composite based on individual scores for breathlessness, chest tightness, wheezing, cough. Scale : 0=none to 5= severe, activities cancelled. Exacerbations defined as worsening of asthma symptoms that required treatment in addition to the study drug and rescue SABA. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Rutten‐van Molken 1995.
| Methods | STUDY DESIGN: Parallel group‐single centre , Holland. 6 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, matching devices. WITHDRAWALS/DROP OUTS: 13 described after randomization. COMPLIANCE:. Not assessed CONFOUNDERS: Groups well balanced by characteristics. Not ITT QUALITY: Jadad 4. Cochrane B | |
| Participants | N = ENROLLED, 120 RANDOMISED. 107 COMPLETED ADULT , M = 60 F = 47 Mean age: 53 (SD 14) BASELINE SEVERITY: Moderate asthma INCLUSION : Baseline FEV1 50 to 70% predicted, > 15% FEV1 reversibility to SABA. EXCLUSION: URTI/ LRTI < 6 WKS. OS, theophyllines, uncontrolled illness. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400 mcg BD PLACEBO: DEVICE: Dry powder device‐ diskhaler. TREATMENT PERIOD: 6 weeks RESCUE: Salbutamol 400 mcg PRN CO‐INTERVENTIONS: ICS 31%, cromones stable dose | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, efficacy score, AQOL/LWAQ scores, % days with no symptoms ,% nights with no asthma awakenings . Eficacy rating | |
| Notes | Symptom Score‐ Night‐time 0 to 4(none ‐ so severe that no sleep possible). Day‐time 0 to 5 (no symptoms ‐ symptoms so severe normal activities not possible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Staehr 1995.
| Methods | STUDY DESIGN: 2 period cross over, general practice setting, 29 GPs , Denmark. 4 week treatment period. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 36 pre‐randomisation, 10 described after randomization. COMPLIANCE:. Not assessed / reported. CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 128 ENROLLED/ 92 RANDOMISED, ADULT, M = 36 F=56 Mean age: 40 BASELINE SEVERITY: Mild‐moderate stable asthma INCLUSION : Stable phase asthma, run‐in PEF average >50% predicted, >15% PEF reversibility to SABA. EXCLUSION: uncontrolled disease, pregnancy, Use of theophyllines, oral beta_2 agonists or anticholinergics. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400mcg QDS PLACEBO: placebo BD DEVICE: Diskhaler TREATMENT PERIOD: 4 weeks RESCUE: Salbutamol 400 mcg PRN CO‐INTERVENTIONS: none 28%, ICS 72%, OS, cromones. | |
| Outcomes | OUTCOMES: PEF, Rescue use, asthma symptom score, adverse events. | |
| Notes | Symptom Score‐ Night‐time 0 to 4 (none ‐ so severe that no sleep possible). Day‐time 0 to 5 (no symptoms ‐ symptoms so severe normal activities not possible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Steffensen 1995.
| Methods | STUDY DESIGN: Parallel group‐multicentre , 20 Scandinavia.12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 42 described after randomization. COMPLIANCE:. Not assessed CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 362 ENROLLED, 304 RANDOMISED. ADULT , M = 60 F = 47 Mean age: 48 (SD 13) BASELINE SEVERITY: not specified, clinically stable. INCLUSION : Baseline FEV1 > 40% predicted, > 15% FEV1 reversibility to SABA. Requiring SABA. EXCLUSION: unstable asthma, altered dose medication. | |
| Interventions | LONG ACTING BETA AGONIST: Formoterol 12 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400 mcg QDS PLACEBO: placebo QDS DEVICE: Dry powder device. TREATMENT PERIOD: 12 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS 84%, OS 6%, cromones stable dose | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score. adverse events, including asthma exacerbations. Efficacy rating | |
| Notes | Symptom Score‐ Day: 0 = none, to 3 = very severe symptoms. Night: 0 = none to 3 = almost no sleep due to asthma. No definition of asthma exacerbation recorded as an adverse event given. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Taylor 1998.
| Methods | STUDY DESIGN: 3 way cross over, 2 centre, New Zealand. 24 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 35 described after randomization and 8 protocol violators. COMPLIANCE:. Assessed by counting blisters, > 87% CONFOUNDERS: Not analysed by ITT, Efficacy analysis similar. QUALITY: Jadad 4. Cochrane B | |
| Participants | N = ENROLLED, 165 RANDOMISED, 157 ANALYSED. ADULT , M = 73 F = 92 Mean age: 38 (range 18 to 64) BASELINE SEVERITY: Mild‐moderate asthma INCLUSION : > 15% FEV1 reversibility to SABA. PC20 methacholine < 8mg/ml. EXCLUSION: current smokers, requiring OS or theophyllines, SABA requirement > 10 puffs/day, significant illness. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Salbutamol 400 mcg QDS PLACEBO: placebo QDS DEVICE: Dry powder device‐ diskhaler. TREATMENT PERIOD: 24 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: None 8%, ICS 92%, cromones stable dose | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, exacerbations, daily asthma score. | |
| Notes | Exacerbations‐ Major = daily asthma score 3, PEF 40 to 60% predicted, requiring OS. Minor‐ Daily asthma score 2, PEF 61 to 75% predicted, increased rescue use. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Venables 1992.
| Methods | STUDY DESIGN: 2 way cross over, general practice setting, unspecified number practices in UK RANDOMISATION: Yes, no method stated. BLINDING: open, not blinded. WITHDRAWALS/DROP OUTS: 26 pre‐randomization, 16 post randomisation (adverse events etc) 28 non compliant. COMPLIANCE:. Assessed by diary card, 28 excluded for non compliance.. CONFOUNDERS: QUALITY: Jadad 2. Cochrane B | |
| Participants | N = 128 ENROLLED/ 102 RANDOMISED, 58 completed, ADULT, M = 54 F = 48 Mean age: 39 (range 18 to 71) BASELINE SEVERITY: Mild persistent asthma INCLUSION : Adult asthmatics, requiring daily bronchodilator treatment < 800mcg SABA/day. Baseline FEV1 > 75% predicted, > 15% FEV1 reversibility to SABA. Minimum symptom score 1:4 in 4 of 7 days run in. EXCLUSION: Serious uncontrolled diseases, URTI < 2 weeks, pregnancy, lactation, OS within 6 weeks, > 4 courses OS within 12 months. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 50 mcg BD SHORT ACTING BETA AGONIST: Terbutaline 500 QDS PLACEBO: none DEVICE: SABA turbuhaler, LABA diskhaler. TREATMENT PERIOD: 4 weeks RESCUE: Salbutamol 100 mcg PRN CO‐INTERVENTIONS: ICS < 400mcg /day 50%, cromones, theophyllines at constant dose | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, asthma symptom score, nights with asthma, patient assessment, adverse events | |
| Notes | Symptom Score‐ breathlessness, wheezing, cough. Scale :0 = none to3=symptoms most of day | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
Wenzel 1998.
| Methods | STUDY DESIGN: Parallel group, multicentre, 40, USA. 12 weeks. RANDOMISATION: Yes, no method stated. BLINDING: double blind, double dummy, matching devices. WITHDRAWALS/DROP OUTS: 15 described after randomization. COMPLIANCE:. Not assessed / reported. CONFOUNDERS: Groups well balanced by characteristics QUALITY: Jadad 4. Cochrane B | |
| Participants | N = 539 ENROLLED/ RANDOMISED, ADULT/ADOLESCENT , M = 272 F = 266 Mean age: 35.4 (range 12 to 83) BASELINE SEVERITY: Mild to moderate persistent asthma INCLUSION : Diagnosis asthma by ATS criteria, requiring daily bronchodilator treatment > 6 weeks. Baseline FEV1 40 to 80% predicted, > 15% FEV1 reversibility to SABA. EXCLUSION: CF, COPD, current smokers, hospitalized by exacerbation asthma < 6 weeks. Use of theophyllines or cromones. | |
| Interventions | LONG ACTING BETA AGONIST: Salmeterol 42 mcg BD SHORT ACTING BETA AGONIST: Albuterol 180mcg QDS PLACEBO: placebo BD DEVICE: MDI. TREATMENT PERIOD: 12 weeks RESCUE: Albuterol 90 mcg PRN CO‐INTERVENTIONS: ICS 46%, | |
| Outcomes | OUTCOMES: FEV1, FVC, PEF, Rescue use, asthma symptom score, adverse events, AQOL scores. | |
| Notes | Symptom Score‐ Night‐time 0‐3 (none ‐ woke > 3 times). Day‐time 0‐3 (no symptoms ‐ significant discomfort) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available (Cochrane Grade B) |
ICS = Inhaled corticosteroids. OS = oral corticosteroids. LABA = long‐acting beta2 agonist. SABA = Short‐acting beta 2 agonist. Short acting beta 2 agonist salbutamol known in USA as albuterol‐ dose measured at mouthpiece 90 mcg = 100mcg from inhaler . Bronchial hyperreactivity = BHR, measured as PD20 or PC20 in methacholine or histamine. BDP = beclomethasone dipropionate, BUD = budesonide , FP = fluticasone propionate. Cromones = sodium cromoglycate, nedocromil sodium . MDI = Metered dose inhaler. Dosages: QDS= 4 times daily, TDS= 3 times daily, BD= twice daily. AQOL score = Asthma quality of life score, based on Juniper 1992 (Juniper EF, Guyatt GH. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47:76‐83) value of 1 = maximum impairment, value 7 = no impairment. Results 0.5 = small change, 1.0 = moderate change, 1.5 = large change. LWAQ = Living with asthma questionnaire (Hyland M. The living with asthma questionnaire. Respir Med 1991;85 supp:13‐16.), lower score indicates better quality of life.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adinoff 1998 | Intervention‐ no short acting beta2‐agonist group |
| Akpinarli 1999 | Intervention‐ no short acting beta2‐agonist group |
| Arvidsson1989 | Intervention‐ dose of long acting beta2‐agonist varied during study |
| Aziz 1999 | Intervention‐ treatment period less than 2 weeks |
| Aziz 1998 | Intervention‐ treatment period less than 2 weeks |
| Aziz I Tan 1998 | Intervention‐ treatment period less than 2 weeks |
| Baki 1998 | Intervention‐ no short acting beta2‐agonist group |
| Becker Simons 1993 | Abstract only‐ no further publication or details on request |
| Becker 1989 | Intervention‐ treatment period less than 2 weeks |
| Bhagat 1995 | Intervention‐ treatment period less than 2 weeks |
| Bishop 1994 | Intervention‐ treatment period less than 2 weeks |
| Blake 1999 | Intervention‐ treatment period less than 2 weeks |
| Booth Bish 1996 | Intervention‐ no short acting beta2‐agonist group |
| Booth 1993 | Intervention‐ no short acting beta2‐agonist group |
| Boulet Cartier 1998 | Intervention‐ no short acting beta2‐agonist group |
| Boulet Turcot 1997 | Intervention‐ no short acting beta2‐agonist group |
| Bowers 1997 | Not RCT, Review of 8 previously published studies |
| Boyd 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Brambilla 1994 | Intervention‐ oral SR short‐acting beta(2)‐agonist |
| Busse 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Campbell 2000 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Carlsen 1995 | Intervention‐ treatment period less than 2 weeks |
| Charpin 1992 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Chervinsky 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Cheung 1992 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Clark 1993 | Not RCT, Case reports |
| Clauzel 1998 | Not RCT, intervention‐ no short‐acting beta(2)‐agonist group |
| Cockcroft 1997 | Intervention‐ treatment period less than 2 weeks |
| Dahl 1991 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Derom 1992 | Intervention‐ treatment period less than 2 weeks |
| Di‐Lorenzo 1995 | Intervention‐ treatment period less than 2 weeks |
| Droszcz 1999 | Not RCT, intervention‐ no short‐acting beta(2)‐agonist group |
| Faurschou 1991 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Faurschou 1992 | Abstract only‐ no publication details available |
| Faurschou Dahl 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Fitzpatrick 1990 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Fuglsang 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Gardiner 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Giannini 1995 | Intervention‐ treatment period less than 2 weeks |
| Giannini Bacci 1999 | Intervention‐ treatment period less than 2 weeks |
| Gong 1996 | Intervention‐ treatment period less than 2 weeks |
| Gotz 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Green 1992 | Intervention‐ treatment period less than 2 weeks |
| Greening 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Grove 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Grove Lipworth 1996 | Intervention‐ treatment period less than 2 weeks |
| Hacki 1993 | Not RCT, intervention‐ no short‐acting beta(2)‐agonist group |
| Hyland 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Jartti 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Jones 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Juniper 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Kalra 1996 | Intervention‐ treatment period less than 2 weeks |
| Kavuru 2000 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Kemp Cook 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Kemp 1993 | Intervention‐ treatment period less than 2 weeks |
| Kemp DeGraff 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Kemp Dockhorn 1994 | Intervention‐ treatment period less than 2 weeks |
| Kesten 1992 | Not RCT, intervention‐ no short‐acting beta(2)‐agonist group |
| Kia 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Kraft 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Langley 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Langton 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Li Ward 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Li 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Lipworth Aziz 2000 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Lipworth Demps 2000 | Intervention‐ treatment period less than 2 weeks |
| Lipworth Aziz 1999 | Intervention‐ treatment period less than 2 weeks |
| Lockey 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Lotvall 1992 | Not RCT, intervention‐ no short‐acting beta(2)‐agonist group |
| Mahajan 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Malo 1992 | Intervention‐ treatment period less than 2 weeks |
| Malozowski 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Mann 1996 | Not RCT, cohort study |
| Martin 1999 | Intervention‐ oral SR short‐acting beta(2)‐agonist group |
| McIvor 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Meijer 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Midgren 1992 | Intervention‐ dose of long acting beta2‐agonist varied during study |
| Molimard 2001 | Intervention‐ no regular short‐acting beta(2)‐agonist group, not DB |
| Nathan 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Nelson 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Nelson 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Newnham 1993 | Intervention‐ treatment period less than 2 weeks |
| Newnham 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Newnham 1995 | Intervention‐ dose of long acting beta2‐agonist varied during study |
| Nichol 1990 | Intervention‐ treatment period less than 2 weeks |
| Nielsen 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Nix 1990 | Intervention‐ treatment period less than 2 weeks |
| Norhaya 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Nowak 1992 | Intervention‐ treatment period less than 2 weeks |
| Palmer 1992 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Pauwels 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Pearlman 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Pearlman 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Pederson 1993 | Intervention‐ treatment period less than 2 weeks |
| Quebe‐Fehling 1996 | Intervention‐ treatment period less than 2 weeks |
| Rabe 1993 | Intervention‐ treatment period less than 2 weeks |
| Ramage 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Ramage Lipworth 1994 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Ramsdale 1991 | Intervention‐ treatment period less than 2 weeks |
| Ringbaek 1996 | Intervention‐ oral SR short‐acting beta(2)‐agonist group |
| Roberts 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Roberts 1992 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Rosenthal 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Rosenthal 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Russell 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Schaaning 1996 | Intervention‐ treatment period less than 2 weeks |
| Schreurs 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Self 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Shapiro 2000 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Shepherd 1991 | Not RCT‐ letter |
| Sichletidis 1993 | Intervention‐ treatment period less than 2 weeks |
| Siergiejko 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Simons 1992 | Intervention‐ treatment period less than 2 weeks |
| Simons 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Simons 2 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Simons Gerst 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Smyth 1993 | Intervention‐ treatment period less than 2 weeks |
| Starke 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Sussman 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Tan 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Tattersfield 2001 | Intervention‐ dose varied of short‐acting and long‐acting beta(2)‐agonist |
| Tattersfield 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Taylor 1992 | Intervention‐ treatment period less than 2 weeks |
| Totterman 1998 | Intervention‐ treatment period less than 2 weeks |
| Turner 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Twentyman 1990 | Intervention‐ treatment period less than 2 weeks |
| Ullman 1988 | Intervention‐ treatment period less than 2 weeks |
| Ullman 1990 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Van der Molen 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Van der Molen 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Verberne 1991 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Verberne 1996 | Intervention‐ treatment period less than 2 weeks |
| Verberne 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Verberne 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Verberne 2000 | Not RCT , review |
| Verini 1998 | Intervention‐ treatment period less than 2 weeks |
| Viskum 1990 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Von Berg 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Von Berg 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wallaert 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wallin 1999 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wallin 1990 | Intervention‐ dose of long acting beta2‐agonist varied during study |
| Walters 1992 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Weinstein 1997 | Intervention‐ treatment period less than 2 weeks |
| Weinstein 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wilding 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wolfe 2000 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wong 1997 | Intervention‐ treatment period less than 2 weeks |
| Woolcock 1996 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Wronska 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Yates 1995 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Yates 1997 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Zarkovic 1998 | Intervention‐ no short‐acting beta(2)‐agonist group |
| Zellweger 1994 | Intervention‐ treatment period less than 2 weeks |
Contributions of authors
Julia Walters cooperated in writing the protocol, carried out the initial study selection, study grading, data extraction and analysis, and writing of the first draft and subsequent revisions.
Haydn Walters cooperated in writing the protocol, grading studies, data checking and analysis, writing and revising drafts of the review.
Peter Gibson advised on protocol formulation and writing the first and subsequent revisions of the review.
Declarations of interest
E H Walters has taken part in collaborative clinical pharmacology studies with a number of pharmaceutical companies including GlaxoWellcome, Astra Zeneca, Pfizer, Boehringer, Schering Plough, SKB, and Novartis. He has, in the past, held consultancies with GlaxoWellcome, Pfizer and Zeneca. He has had sponsorship to meetings from a number of the companies listed over the past 15 years.
Edited (no change to conclusions)
References
References to studies included in this review
Beach 1993 {published data only (unpublished sought but not used)}
- Beach JR, Young CL, Harkawat R, Gardiner PV, Avery AJ, Coward GA, et al. Effect on airway responsiveness of six weeks treatment with salmeterol. Pulmonary Pharmacology 1993;6:155‐7. [DOI] [PubMed] [Google Scholar]
Bensch 2001 {published and unpublished data}
- Bensch G, Lapidus R, Levine B, Lumry W, Yegen U, Kiselev P, et al. A randomized, 12‐week, double‐blind, placebo‐controlled study comparing formoterol dry powder inhaler with albuterol metered‐dose inhaler. Annals of Allergy, Asthma, & Immunology 2001;86(1):19‐27. [DOI] [PubMed] [Google Scholar]
- Della Cioppa G, Kiseley P, Matos D, Yegen I, Townley RG. QID Albuterol worsens peak flow variability in asthma whereas BID Formoterol does not.(abstract). Annals of Allergy , Asthma & Immunology 1998;80:88. [Google Scholar]
Boulet 1997 {published data only (unpublished sought but not used)}
- Boulet LP, Laviolette M, Boucher S, et al. A Twelve week comparison of salmeterol and salbutamol in the treatment of mild to moderate asthma: a Canadian multicentre study. Journal of Allergy & Clinical Immunology 1997;99:13‐21. [DOI] [PubMed] [Google Scholar]
Britton 1992 {published and unpublished data}
- Britton MC, Earnshaw JS, Palmer JBD. A twelve month comparison of salmeterol with salbutamol in asthmatic patients. European Respiratory Journal 1992;5:1062‐67. [PubMed] [Google Scholar]
- Fuller R. Safety of salmeterol in the treatment of asthma. European Respiratory Journal 1995;5:133‐7. [Google Scholar]
Byrnes 2000 {published data only (unpublished sought but not used)}
- Byrnes C, Shrewsbury S, Barnes PJ, Bush A. Salmeterol in paediatric asthma. Thorax 2000;55(9):780‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes CA, Weber EA, Moorat A, Bush A. A Comparison of salmeterol 50mcg bd and 100mcg bd with salbutamol 200mcg qds in paediatric asthma. American Journal of Respiratory & Critical Care Medicine 1996;153(4):A408. [Google Scholar]
Castle 1993 {published data only}
- Castle W, Fuller R, Hall J. Serevent nationwide surveillance study:Comparison of salmeterol with salbutamol in asthmatic patients who require regular bronchodilator treatment. British Medical Journal 1993;306:1034‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Alonzo 1994 {published data only}
- Arledge T, Liddle D, Stahl E, Rossing T. Salmeterol does not cause tolerance during long term asthma therapy. Journal of Allergy & Clinical Immunology 1996;98:1116‐9. [DOI] [PubMed] [Google Scholar]
- D'Alonzo GE. Efficacy of inhaled salmeterol in the treatment of asthma. European Respiratory Review 1995;5:128‐32. [Google Scholar]
- D'Alonzo GE, Nathan RA, Henchowicz MD. Salmeterol xinafoate as maintenance therapy compared with albuterol in patients with asthma. The Journal of the American Medical Association 1994;271:1412‐6. [PubMed] [Google Scholar]
- Nathan R, Seltzer J, Kemp J, Chervinsky P, Alexander W, Liddle R, et al. Safety of salmeterol in the maintenance treatment of asthma. Annals of Allergy, Asthma, & Immunology 1995;75:243‐8. [PubMed] [Google Scholar]
- Pearlman DS. Long‐acting beta 2‐agonist salmeterol compared with albuterol in maintenance asthma therapy. Annals of Allergy, Asthma, & Immunology 1995;75:180‐4. [PubMed] [Google Scholar]
- Pearlman DS, Liddle R. Controlling asthma symptoms: Salmeterol compared with salbutamol in large‐scale multicentre studies. European Respiratory Review 1994;4:301‐5. [Google Scholar]
De Carli 1995 {published and unpublished data}
- Carli G, Arpinelli F, Irvine SH, Bamfi F, Ravinetto R, Recchia G. Change of quality of life induced by salmeterol and salbutamol in adult asthmatic patients. Therapie 1995;50 Suppl:N118. [Google Scholar]
De Oliveira 1998 {published data only}
- Oliveira M, Jardim J, Faresin S, Lucas S, Nery L. Efficacy of and tolerance to salmeterol compared to salbutamol in patients with bronchial asthma. Revista da Associacao Medica Brasileira 1998;44:169‐75. [PubMed] [Google Scholar]
Ekstrom 1998a {published data only}
- Ekstrom T, Ringdal N, Tukiainen P, Runnerstrom E, Soliman S. A 3 month comparison of formoterol with terbutaline via turbuhaler. A placebo controlled study. Annals of Allergy, Asthma, & Immunology 1998;81:225‐30. [DOI] [PubMed] [Google Scholar]
Ekstrom 1998b {published data only}
- Ekstrom T, Ringdal N, Sobradillo V, Runnerstrom E, Soliman S. Low‐dose formoterol Turbuhaler(TM) (Oxis(TM)) b.i.d., a 3‐month placebo‐controlled comparison with terbutaline (q.i.d.). Respiratory Medicine 1998;92(8):1040‐5. [DOI] [PubMed] [Google Scholar]
Faurschou 1996 {published data only}
- Faurschou P, Steffensen I, Jacques L. Effect of addition of inhaled salmeterol to the treatment of moderate‐to‐severe asthmatics uncontrolled on high‐dose inhaled steroids. asthmatics uncontrolled on high‐dose inhaled steroids. European Respiratory Journal 1996;9:1885‐90. [DOI] [PubMed] [Google Scholar]
FitzGerald 1999 {published data only (unpublished sought but not used)}
- FitzGerald J, Chapman K, Della Cioppa G, Stubbing D, Fairbarn M, Till M, et al. Sustained bronchoprotection, bronchodilatation, and symptom control during regular formoterol use in asthma of moderate or greater severity. Journal of Allergy & Clinical Immunology 1999;103(31):427‐35. [DOI] [PubMed] [Google Scholar]
Hekking 1990 {published data only}
- Hekking P, Maesen F, Greefhorst A, Prins J, Tan Y, Zweers P. Long term efficacy of formoterol compared with salbutamol. Lung 1990;168 Supp:76‐82. [DOI] [PubMed] [Google Scholar]
Hermansson1995 {published and unpublished data}
- Hermansson B, Jenkins R. A 4‐week comparison of salmeterol and terbutaline in adult asthma. Allergy 1995;50:551‐8. [DOI] [PubMed] [Google Scholar]
Juniper 1995 {published data only (unpublished sought but not used)}
- Juniper EF, Johnston PR, Borkhoff CM, Guyatt G, Boulet L‐P, Haukioja A. Quality of life in asthma clinical trials: a comparison of salmeterol and salbutamol. Am J Respir Crit Care Med 1995;151:66‐70. [DOI] [PubMed] [Google Scholar]
- Juniper EF, Johnston, Borkhoff C, Haukioja A. A multicentre comparison of salmeterol and salbutamol on asthma‐specific quality of life [abstract]. Quality of Life Research 1994;3:83. [Google Scholar]
Kemp 1998 {published data only}
- Arledge T, Liddle D, Stahl E, Rossing T. Salmeterol does not cause tolerance during long term asthma therapy. Journal of Allergy & Clinical Immunology 1996;98:1116‐9. [DOI] [PubMed] [Google Scholar]
- Kemp J, Wolfe J, Grady J, LaForce C, Stahl E, Arlidge T, et al. Salmeterol powder compared with albuterol aerosol as maintenance therapy for asthma in adolescent and adult patients. Clinical Therapeutics 1998;20(2):270‐82. [DOI] [PubMed] [Google Scholar]
- Wolfe J, LaForce C, Chervinsky P, Galant S, Lumry W, Noonan M, et al. Inhaled salmeterol powder compared with albuterol aerosol given regularly or as needed for asthma. Annals of Allergy, Asthma and Immunology 1995;74:52. [Google Scholar]
Kesten 1991 {published data only}
- Kesten S, Chapman KR, Broder I, et al. A three month comparison of inhaled formoterol versus four times daily inhaled albuterol in the management of stable asthma. American Review of Respiratory Disease 1991;144:622‐5. [DOI] [PubMed] [Google Scholar]
Kozlik‐Feldman 1996 {published data only}
- Kozlik‐Feldmann R, Berg A, Berdel D, Reinhardt D. Long‐term effects of formoterol and salbutamol on bronchial hyperreactivity and beta‐adrenoceptor density on lymphocytes in children with bronchial asthma. European Journal of Medical Research 1996;1:465‐70. [PubMed] [Google Scholar]
Lai 1995 {published data only}
- Lai C, Chan C, Ho S, Hui A, Lai K. Inhaled salmeterol and albuterol in asthmatic patients receiving high‐dose inhaled corticosteroids. Chest 1995;108:36‐40. [DOI] [PubMed] [Google Scholar]
Leblanc 1996 {published data only (unpublished sought but not used)}
- Leblanc P, Knight A, Kreisman H, Borkhoff CM, Johnston PR. A placebo controlled crossover comparison of salmeterol and salbutamol in patients with asthma. American Journal of Respiratory & Critical Care Medicine 1996;154:324‐8. [DOI] [PubMed] [Google Scholar]
Lenney 1995 {published data only (unpublished sought but not used)}
- Boner A. Salmeterol: long term studies in children. European Respiratory Journal 1992;5 Suppl:318. [Google Scholar]
- Lenney W, Pedersen S, Boner AL, Ebbutt A, Jenkins M. Efficacy and safety of salmeterol in childhood asthma. European Journal of Pediatrics 1995;154:983‐90. [DOI] [PubMed] [Google Scholar]
Lipworth 1998 {published data only}
- Lipworth B, Tan S, Devlin M, Aiken T, Baker R, Hendrick D. Effects of treatment with formoterol on bronchoprotection against methacholine. American Journal of Medicine 1998;104(5):431‐8. [DOI] [PubMed] [Google Scholar]
Lundback 1993 {published data only}
- Fuller R. Safety of salmeterol in the treatment of asthma. European Respiratory Journal 1995;5:133‐7. [Google Scholar]
- Lundback B, Rawlinson DW, Palmer JBD. Twelve month comparison of salmeterol and salbutamol as dry powder formulations in asthmatic patients. Thorax 1993;153:148‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearlman 1992 {published and unpublished data}
- Arledge T, Liddle D, Stahl E, Rossing T. Salmeterol does not cause tolerance during long term asthma therapy. Journal of Allergy & Clinical Immunology 1996;98:1116‐9. [DOI] [PubMed] [Google Scholar]
- D'Alonzo GE. Efficacy of inhaled salmeterol in the treatment of asthma. European Respiratory Review 1995;5:128‐32. [Google Scholar]
- Jenkins M, Hilton C, Kock J, Palmer J. Exacerbations of asthma in patients on salmeterol. Lancet 1991;337:913‐4. [DOI] [PubMed] [Google Scholar]
- Nathan R, Seltzer J, Kemp J, Chervinsky P, Alexander W, Liddle R, et al. Safety of salmeterol in the maintenance treatment of asthma. Annals of Allergy, Asthma, & Immunology 1995;75:243‐8. [PubMed] [Google Scholar]
- Pearlman DS. Long‐acting beta 2‐agonist salmeterol compared with albuterol in maintenance asthma therapy. Annals of Allergy Asthma Immunology 1995;75:180‐4. [PubMed] [Google Scholar]
- Pearlman DS, Chervinsky P, LaForce C, Seltzer JM, Southern DL, Kemp JP, et al. A comparison of salmeterol with albuterol in the treatment of mild‐to‐moderate asthma. New England Journal Of Medicine 1992;327:1420‐5. [DOI] [PubMed] [Google Scholar]
- Pearlman DS, Liddle R. Controlling asthma symptoms: Salmeterol compared with salbutamol in large‐scale multicentre studies. European Respiratory Review 1994;4:301‐5. [Google Scholar]
Rutten‐van Molken 1995 {published data only (unpublished sought but not used)}
- Rutten‐van Molken M, Custers F, van‐Doorslater EKA, et al. Comparison of performance of four instruments in evaluating the effects of salmeterol on asthma quality of life. European Respiratory Journal 1995;8:888‐98. [PubMed] [Google Scholar]
Staehr 1995 {published data only (unpublished sought but not used)}
- Staehr P, Vestbo I. Salmeterol improves control in asthmatic patients treated in general practice. A comparative study of salmeterol and salbutamol in patients with mild to moderate asthma. Ugeskrift for Laeger 1995;157:36‐40. [PubMed] [Google Scholar]
Steffensen 1995 {published and unpublished data}
- Steffensen I, Faurschou P. Formoterol as inhalation powder in the treatment of patients with reversible obstructive lung diseases. A 3‐month placebo‐controlled comparison of the effects of formoterol and salbutamol, followed by a 12‐month period with formoterol alone. Ugeskrift for Laeger 1996;158:7092‐6. [PubMed] [Google Scholar]
- Steffensen I, Faurschou P, Riska H, et al. Inhaled formoterol DP in the treatment of patients with ROAD. A 3month, placebo controlled comparison of the efficacy and safety of formoterol and salbutamol. Allergy 1995;50:657‐63. [DOI] [PubMed] [Google Scholar]
Taylor 1998 {published data only (unpublished sought but not used)}
- Taylor DR, Drazen JM, Herbison GP, Yandava CN, Hancox RJ, Town GI. Asthma exacerbations during long term beta agonist use: Influence of beta2 adrenoceptor polymorphism. Thorax 2000;55(9):762‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DR, Town GI, Herbison GP, Boothman‐Burrell D, et al. Asthma control during long term treatment with regular inhaled salbutamol and salmeterol. Thorax 1998;53:744‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Venables 1992 {published data only}
- Venables TA. A multicentre study in general practice to compare the efficacy and tolerability of inhaled salmeterol and terbutaline in the treatment of asthma. British Journal of Clinical Research 1992;3:125‐36. [Google Scholar]
Wenzel 1998 {published data only}
- Cox F, Goodwin B, Wenzel S, Rickard K, Kalberg C, Emmett A. Asthma specific quality of life in patients treated with salmeterol or albuterol. Journal of Allergy & Clinical Immunology. 1996; Vol. 97:256.
- Goodwin R, Cox F, Lumry W, Rickard K, Kalberg C, Emmett A. The impact of salmeterol versus albuterol on disease specific quality of life in mild to moderate asthmatics. Journal of Allergy & Clinical Immunology 1996;97(Part 3):256. [Google Scholar]
- Wenzel SE, Lumry W, Manning M, Kalberg C, Cox F, Emmett A, et al. Efficacy, safety, and effects on quality of life of salmeterol versus albuterol in patients with mild to moderate persistent asthma. Annals of Allergy 1998;80(6):463‐70. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adinoff 1998 {published data only}
- Adinoff A, Schwartz H, Rickard K, Yancey S, Swearingen B. Salmeterol compared with current therapies in chronic asthma. Journal of Family Practice 1998;47:278‐84. [PubMed] [Google Scholar]
Akpinarli 1999 {published data only}
- Akpinarli A, Tuncer A, Saraclar Y, Sekerel B, Kalayci O. Effect of formoterol on clinical parameters and lung functions in patients with bronchial asthma: A randomised controlled trial. [English]. Archives of Disease in Childhood 1999;81(1):45‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arvidsson1989 {published data only}
- Arvidsson P, Larsson S, Lofdahl CG, Melander B, Wahlander L, Svedmyr N. Formoterol, a new long acting bronchodilator for inhalation. European Respiratory Journal 1989;2:325‐30. [PubMed] [Google Scholar]
Aziz 1999 {published data only}
- Aziz I, Lipworth BJ. A bolus of inhaled budesonide rapidly reverses airway subsensitivity and beta2‐adrenoceptor down‐regulation after regular inhaled formoterol. Chest 1999;115(3):623‐8. [DOI] [PubMed] [Google Scholar]
Aziz 1998 {published data only}
- Aziz I, Hall IP, McFarlane LC, Lipworth BJ. Beta 2 adrenoceptor regulation and bronchodilator sensitivity after regular treatment with formoterol in subjects with stable asthma. Journal of Allergy & Clinical Immunology 1998;101:337‐41. [DOI] [PubMed] [Google Scholar]
Aziz I Tan 1998 {published data only}
- Aziz I, Tan KS, Hall IP, Devlin MM, Lipworth BJ. Subsensitivity to bronchoprotection against adenosine monophosphate challenge following regular once‐daily formoterol. European Respiratory Journal 1998;12(3):580‐4. [DOI] [PubMed] [Google Scholar]
Baki 1998 {published data only}
- Baki A, Karaguzel G. Short‐term effects of budesonide, nedocromil sodium and salmeterol on bronchial hyperresponsiveness in childhood asthma. Acta Paediatrica Japonica 1998;40:247‐51. [DOI] [PubMed] [Google Scholar]
Becker Simons 1993 {published data only}
- Becker AB, Simons FER. Formoterol, a new beta2 agonist, improves chronic airway hyperresponsiveness in children with asthma. Immunology and Allergy practice 1993;14(7):18‐9. [Google Scholar]
Becker 1989 {published data only}
- Becker AB, Simons F. Formoterol, a new long‐acting selective beta 2‐adrenergic receptor agonist: double‐blind comparison with salbutamol and placebo in children with asthma. Journal of Allergy & Clinical Immunology 1989;84(6):891‐5. [DOI] [PubMed] [Google Scholar]
Bhagat 1995 {published data only}
- Bhagat R, Kalra S, Swystun VA, Cockcroft DW. Rapid onset of tolerance to the bronchoprotective effect of salmeterol. Chest 1995;108:1235‐9. [DOI] [PubMed] [Google Scholar]
Bishop 1994 {published data only}
- Bishop AL, Chervinsky P, Liddle R, et al. Salmeterol for treatment of reversible obstructive airways disease in children. Journal of Allergy & Clinical Immunology 1994;93:248. [Google Scholar]
Blake 1999 {published data only}
- Blake K, Pearlman D, Scott C, Wang Y, Stahl E, Arledge T. Prevention of exercise‐induced bronchospasm in pediatric asthma patients: a comparison of salmeterol powder with albuterol. Annals of Allergy, Asthma, & Immunology 1999;82:205‐11. [DOI] [PubMed] [Google Scholar]
Booth Bish 1996 {published data only}
- Booth H, Bish R, Walters J, Whitehead F, Walters EH. Salmeterol tachyphylaxis in steroid treated asthmatic subjects. Thorax 1996;51:1100‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Booth 1993 {published data only}
- Booth H, Fishwick K, Harkawat R, Devereux G, Hendrick DJ, Walters EH. Changes in methacholine induced bronchoconstriction with the long acting beta2 agonist salmeterol in mild to moderate asthmatic patients. Thorax 1993;48(11):1121‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boulet Cartier 1998 {published data only}
- Boulet L, Cartier A, Milot J, Cote J, Malo JL, Laviolette M. Tolerance to the protective effects of salmeterol on methacholine‐induced bronchoconstriction: influence of inhaled corticosteroids. European Respiratory Journal 1998;11(5):1091‐7. [DOI] [PubMed] [Google Scholar]
Boulet Turcot 1997 {published data only}
- Boulet L, Turcotte H, Boutet M, Dube J, Gagnon M, Laviolette M. Influence of salmeterol on chronic and allergen‐induced airway inflammation in mild allergic asthma : A pilot study. Current Therapeutic Research ‐ Clinical and Experimental 1997;58:240‐59. [Google Scholar]
Bowers 1997 {published data only}
- Bowers BW, Cox FM, Kalberg C, et al. The impact of salmeterol on asthma specific quality of life in patients reporting nocturnal asthma awakenings due to asthma [abstract]. Annals of Allergy, Asthma, & Immunology 1997;78:110. [Google Scholar]
Boyd 1995 {published data only}
- Boyd G. Salmeterol xinafoate in asthmatic patients under consideration for maintenance oral corticosteroid therapy. UK Study Group. European Respiratory Journal 1995;8:1494‐8. [PubMed] [Google Scholar]
Brambilla 1994 {published data only}
- Brambilla C, Chastang C, Georges D, et al. Salmeterol compared with slow release terbutaline in nocturnal asthma: a multi center randomised double blind double dummy sequential clinical trial. Allergy 1994;49:421‐6. [DOI] [PubMed] [Google Scholar]
Busse 1998 {published data only}
- Busse WW, Casale TB, Murray JJ, Petrocella V, Cox F, Rickard K. Efficacy, safety, and impact on quality of life of salmeterol in patients with moderate persistent asthma. American Journal of Managed Care 1998;4(11):1579‐87. [PubMed] [Google Scholar]
Campbell 2000 {published data only}
- Campbell LM, Berggren F, Emmas C. The cost effectiveness of eformoterol via Turbohaler(TM) and salmeterol via pressurised metered dose inhaler and metered dose powder inhaler in mild to moderate asthma. Journal of Medical Economics 2000;3:49‐60. [Google Scholar]
Carlsen 1995 {published data only}
- Carlsen K, Roksund O, Olsholt K, Nja F, Leegaard J, Bratten G. Overnight protection by inhaled salmeterol on exercise‐induced asthma in children. European Respiratory Journal 1995;8:1852‐5. [DOI] [PubMed] [Google Scholar]
Charpin 1992 {published data only}
- Charpin D, Vervloet D. Quality of life in moderate chronic asthma: salmeterol versus current treatments [abstract]. Allergy 1992;47(12 Suppl):230. [Google Scholar]
Chervinsky 1999 {published data only}
- Chervinsky P, Goldberg P, Galant S, Wang Y, Arledge T, Welch MB, et al. Long‐term cardiovascular safety of salmeterol powder pharmacotherapy in adolescent and adult patients with chronic persistent asthma: A randomized clinical trial. Chest 1999;115(3):642‐8. [DOI] [PubMed] [Google Scholar]
Cheung 1992 {published data only}
- Cheung D, Timmers MC, Zwinderman AH, et al. Long term effects of a long acting beta adrenoceptor agonist in patients with mild asthma. New England Journal of Medicine 1992;327:1198‐203. [DOI] [PubMed] [Google Scholar]
Clark 1993 {published data only}
- Clark CE, Ferguson AD, Siddorn J. Respiratory arrests in young asthmatics on salmeterol. Respiratory Medicine 993;87:227‐8. [DOI] [PubMed] [Google Scholar]
Clauzel 1998 {published data only}
- Clauzel AM, Molimard M, Gros V, Lepere E, Febvre N, Michel FB. Use of formoterol dry powder administered for three months via a single dose inhaler in 1,380 asthmatic patients. Journal of Investigational Allergology and Clinical Immunology 1998;8:265‐0. [PubMed] [Google Scholar]
Cockcroft 1997 {published data only}
- Cockcroft DW, Swystun VA, Bhagat R. Salmeterol and airway response to allergen. Canadian Respiratory Journal 1997;4:37‐40. [Google Scholar]
Dahl 1991 {published data only}
- Dahl R, Earnshaw JS, Palmer JBD. Salmeterol: a 4 week study of a long acting beta2 adrenoceptor agonist for the treament of reversible airways disease. European Respiratory Journal 1991;4:1178‐84. [PubMed] [Google Scholar]
Derom 1992 {published data only}
- Derom EY, Pauwels RA, Straten MEF. The effect of inhaled salmeterol on methacholine responsiveness in subjects with asthma up to 12 hours. Journal of Allergy & Clinical Immunology 1992;89:811‐5. [DOI] [PubMed] [Google Scholar]
Di‐Lorenzo 1995 {published data only}
- Di‐Lorenzo G, Morici G, Norrito F, Mansueto P, Melluso M, Purello‐D'Ambrosio F, et al. Comparison of the effects of salmeterol and salbutamol on clinical activity and eosinophil cationic protein serum levels during the pollen season in atopic asthmatics. Clinical and experimental allergy 1995;25(10):951‐6. [DOI] [PubMed] [Google Scholar]
Droszcz 1999 {published data only}
- Droszcz P, Droszcz W. Results of 30 days and 12 months treatment with salmeterol in patients with asthma and COPD. Polske Merkuriusz Lekarski 1999;6:266‐7. [PubMed] [Google Scholar]
Faurschou 1991 {published data only}
- Faurschou P. Chronic dose‐ranging studies with salmeterol. European Respiratory Journal 1991;1(4):282‐87. [Google Scholar]
Faurschou 1992 {published data only}
- Faurschou P. Salmeterol and Salbutamol: long term efficacy and safety. European Respiratory Journal 1992;5 Supp (15):317‐8. [Google Scholar]
Faurschou Dahl 1997 {published data only}
- Faurschou P, Dahl R, Jeffery P, et al. Comparison of the anti‐inflammatory effects of fluticasone and salmeterol in asthma: A placebo controlled, DB CO with bronchoscopy, bronchial methacholine provocation and lavage. European Respiratory Journal 1997;10 Suppl:243. [Google Scholar]
Fitzpatrick 1990 {published data only}
- Fitzpatrick MF, MacKay T, Driver H, Douglas H. Salmeterol in nocturnal asthma: a double blind , placebo controlled trial of a long acting inhaled beta agonist. British Medical Journal 1990;301:1365‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fuglsang 1998 {published data only}
- Fuglsang G, Vikre‐Jorgensen J, Agertoft L, Pedersen S. Effect of salmeterol treatment on nitric oxide level in exhaled air and dose‐response to terbutaline in children with mild asthma. Pediatric Pulmonology 1998;25(5):314‐21. [DOI] [PubMed] [Google Scholar]
Gardiner 1994 {published data only}
- Gardiner PV, Ward C, Booth H, et al. Effect of eight weeks treatment with salmeterol on bronchoalveolar lavage inflammatory indices in asthmatics. American Journal of Respiratory & Critical Care Medicine 1994;150:1006‐11. [DOI] [PubMed] [Google Scholar]
Giannini 1995 {published data only}
- Giannini D, Carletti A, Dente FL, et al. Tolerance to salbutamol in allergen induced bronchoconstriction. American Journal of Respiratory & Critical Care Medicine 1995;151:A39. [Google Scholar]
Giannini Bacci 1999 {published data only}
- Giannini D, Bacci E, Dente FL, Franco A, Vagagginin B, Testi R, et al. Inhaled beclomethasone diproprionate reverts tolerance to the protective effect of salmeterol on allergen challenge. Chest 1999;115:629‐34. [DOI] [PubMed] [Google Scholar]
Gong 1996 {published data only}
- Gong H, Linn WS, Shamou DA, et al. Effect of inhaled salmeterol on sulfur dioxide induced bronchoconstriction in asthmatic subjects. Chest 1996;110:1229‐35. [DOI] [PubMed] [Google Scholar]
Gotz 1995 {published data only}
- Gotz MH, Taak NK. The efficacy and safety of inhaled salmeterol 50mcg bd compared with salbutamol 200mcg prn in children with asthma [abstract]. European Respiratory Journal 1995;8 Suppl (19):517. [Google Scholar]
Green 1992 {published data only}
- Green C, Price J. Prevention of exercise induced asthma by inhaled salmeterol xinafoate. Archives of Disease in Childhood 1992;67:1014‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greening 1994 {published data only}
- Greening AP, Ind PW, Norhtfield M, et al. Added salmeterol versus higher dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Lancet 1994;344:219‐24. [DOI] [PubMed] [Google Scholar]
Grove 1995 {published data only}
- Grove A, Lipworth BJ. Bronchodilator subsensitivity to salbutamol after twice daily salmeterol in asthmatic patients. Lancet 1995;346:201‐6. [DOI] [PubMed] [Google Scholar]
Grove Lipworth 1996 {published data only}
- Grove A, Lipworth BJ. Effects of prior treatment with salmeterol and formoterol on airway and systemic beta 2 responses to formoterol. Thorax 1996;51:585‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hacki 1993 {published data only}
- Hacki M, Ritter A, Medici T. Formoterol: three years therapy in asthma. European Respiratory Journal 1993;6 Suppl (17):529. [Google Scholar]
Hyland 1994 {published data only}
- Hyland ME, Kenyon CAP, Jacobs P. Sensitivity of quality of life domains and constructs to longitudinal change in a clinical trial comparing salmeterol and placebo in asthmatics. Quality of Life Research 1994;3:121‐6. [DOI] [PubMed] [Google Scholar]
Jartti 1998 {published data only}
- Jartti TT, Kaila TJ, Tahvanainen KUO, Kuusela TA, Vanto TT, Valimaki IAT. Altered cardiovascular autonomic regulation after salmeterol treatment in asthmatic children. Clinical Physiology 1998;18(4):345‐53. [DOI] [PubMed] [Google Scholar]
Jones 1994 {published data only}
- Jones K. Salmeterol xinafoate in the treatment of mild to moderate asthma in primary care. UK Study Group. Thorax 1994;49:971‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juniper 1999 {published data only}
- Juniper E, Svensson K, O'Byrne P, Barnes P, Bauer C, Lofdahl C‐G, et al. Asthma quality of life during 1 year of treatment with budesonide with or without formoterol. European Respiratory Journal 1999;14(5):1038‐43. [DOI] [PubMed] [Google Scholar]
Kalra 1996 {published data only}
- Kalra S, Swystun V, Bhagat R, Cockcroft DW. Inhaled corticosteroids do not prevent the development of tolerance to the bronchoprotective effect of salmeterol. Chest 1996;109:953‐6. [DOI] [PubMed] [Google Scholar]
Kavuru 2000 {published data only}
- Kavuru M, Melamed J, Gross G, LaForce C, House K, Prillaman B, et al. Salmeterol and fluticasone propionate combined in a new powder inhalation device for the treatment of asthma: A randomized, double‐blind, placebo‐controlled trial. Journal of Allergy & Clinical Immunology 2000;105(6):1108‐16. [DOI] [PubMed] [Google Scholar]
Kemp Cook 1998 {published data only}
- Kemp J, Cook D, Incaudo G, Corren J, Kalberg C, Emmett A, et al. Salmeterol improves quality of life in patients with asthma requiring inhaled corticosteroids. Salmeterol Quality of Life Study Group. Journal of Allergy & Clinical Immunology 1998;101:188‐95. [DOI] [PubMed] [Google Scholar]
Kemp 1993 {published data only}
- Kemp J, Bukstein D, Busse W. Effective salmeterol, salbutamol and placebo in the prevention of exercise induced bronchospasm. Chest 1993;104 Suppl:10. [Google Scholar]
Kemp DeGraff 1999 {published data only}
- Kemp J, DeGraff A, Pearlman D, Chervinsky P, Galant S, Goldberg P, et al. A 1‐year study of salmeterol powder on pulmonary function and hyperresponsiveness to methacholine. Journal of Allergy & Clinical Immunology 1999;104(6):1189‐97. [DOI] [PubMed] [Google Scholar]
Kemp Dockhorn 1994 {published data only}
- Kemp JP, Dockhorn RJ, Busse WW, et al. Prolonged effect of inhaled salmeterol against exercise induced bronchoconstriction after chronic dosing with salmeterol. American Journal of Respiratory & Critical Care Medicine 1994;150:1612‐5. [DOI] [PubMed] [Google Scholar]
Kesten 1992 {published data only}
- Kesten S, Chapman KR, Broder I, Cartier A, Hyland RH, Knight A, et al. Sustained improvement in asthma with long‐term use of formoterol fumarate. Annals of Allergy 1992;69(5):415‐20. [PubMed] [Google Scholar]
Kia 1997 {published data only}
- Kia Soong T, Grove A, McLean A, Gnosspelius Y, Hall IP, Lipworth BJ. Systemic corticosteroid rapidly reverses bronchodilator subsensitivity induced by formoterol in asthmatic patients. American Journal of Respiratory & Critical Care Medicine 1997;156(1):28‐35. [DOI] [PubMed] [Google Scholar]
Kraft 1997 {published data only}
- Kraft M, Wenzel SE, Bettinger CM, Martin RJ. The effect of salmeterol on nocturnal symptoms, airway function and inflammation in asthma. Chest 1997;111:1249‐54. [DOI] [PubMed] [Google Scholar]
Langley 1998 {published data only}
- Langley SJ, Masterson CM, Batty EP, Woodcock A. Bronchodilator response to salbutamol after chronic dosing with salmeterol or placebo. European Respiratory Journal 1998;11:1081‐5. [DOI] [PubMed] [Google Scholar]
Langton 1995 {published data only}
- Langton Hewer S, Hobbs J, French D, Lenney W. Pilgrim's progress: the effect of salmeterol in older children with chronic severe asthma. Respiratory Medicine 1995;89:435‐40. [DOI] [PubMed] [Google Scholar]
Li Ward 1999 {published data only}
- Li X, Ward C, Thien F, Bish R, Bamford T, Bao X, et al. An antiinflammatory effect of salmeterol, a long‐acting beta2 agonist, assessed in airway biopsies and bronchoalveolar lavage in asthma. American Journal of Respiratory & Critical Care Medicine 1999;160:1493‐9. [DOI] [PubMed] [Google Scholar]
Li 1998 {published data only}
- Li X, Bamford T, Ward C, et al. Influence of salmeterol on eosinophil inflammation in bronchial biopsies from asthmatics on inhaled steroid. European Respiratory Journal 1998;12 Suppl:157. [Google Scholar]
Lipworth Aziz 2000 {published data only}
- Lipworth B, Aziz I. Bronchodilator response to albuterol after regular formoterol and effects of acute corticosteroid administration. Chest 2000;117(1):156‐62. [DOI] [PubMed] [Google Scholar]
Lipworth Demps 2000 {published data only}
- Lipworth BJ, Dempsey OJ, Aziz I. Functional antagonism with formoterol and salmeterol in asthmatic patients expressing the homozygous Glycine‐16 beta2 adrenoceptor polymorphism. Chest 2000;118(2):321‐8. [DOI] [PubMed] [Google Scholar]
Lipworth Aziz 1999 {published data only}
- Lipworth BJ, Aziz I. A high dose of albuterol does not overcome bronchoprotective susbsensitivity in asthmatic subjects deceiving regular salmeterol or formoterol. Journal of Allergy & Clinical Immunology 1999;103:88‐92. [DOI] [PubMed] [Google Scholar]
Lockey 1999 {published data only}
- Lockey R, DuBuske L, Friedman B, Petrocella V, Cox F, Rickard K. Nocturnal Asthma. Effect of Salmeterol on Quality of Life and Clinical Outcomes. Chest 1999;115:666‐73. [DOI] [PubMed] [Google Scholar]
Lotvall 1992 {published data only}
- Lotvall J, Lunde H, Ullman A, Tornquist H, Svedmyr N. Twelve months, treatment with inhaled salmeterol in asthmatic patients. effects on b2receptor function and inflammatory cells. Allergy 1992;47:477‐83. [DOI] [PubMed] [Google Scholar]
Mahajan 1998 {published data only}
- Mahajan P, Stahl E, Arledge T. Quality of life in pediatric asthma patients treated with salmeterol and impact on the daily activities of their parents. Pediatric Asthma Allergy & Immunology 1998;12(1):21‐8. [Google Scholar]
Malo 1992 {published data only}
- Malo J‐L, Ghezzo H, Trudeau C. Salmeterol a new inhaled beta2 agonist, has a longer blocking effect than albuterol on hyperventilation induced bronchoconstriction. Journal of Allergy & Clinical Immunology 1992;89:567‐74. [DOI] [PubMed] [Google Scholar]
Malozowski 1998 {published data only}
- Malozowski S, Stadel BV, Pian LP, Simons FER. Comparison of beclomethasone, salmeterol, and placebo in children with asthma. New England Journal of Medicine 1998;339(10):704‐5. [DOI] [PubMed] [Google Scholar]
Mann 1996 {published data only}
- Mann RD, Kubota K, Pearce G, et al. Salmeterol: a study by prescription event monitoring in a UK cohort of 15,407 patients. Journal of Clinical Epidemiology 1996;49:247‐50. [DOI] [PubMed] [Google Scholar]
Martin 1999 {published data only}
- Martin R, Kraft M, Beaucher Wea. Comparative study of extended release albuterol sulfate and long‐acting inhaled salmeterol xinafoate in the treatment of nocturnal asthma. Annals of Allergy, Asthma, & Immunology 1999;83(2):121‐6. [DOI] [PubMed] [Google Scholar]
McIvor 1998 {published data only}
- McIvor RA, Pizzichini E, Turner MO, et al. Potential masking effects of salmeterol on airway inflammation in asthma. American Journal of Respiratory & Critical Care Medicine 1998;158:924‐30. [DOI] [PubMed] [Google Scholar]
Meijer 1995 {published data only}
- Meijer GG, Postma DS, Mulder PGH, et al. Long term circadian effects of salmeterol in asthmatic children treated with inhaled corticosteroids. American Journal of Respiratory & Critical Care Medicine 1995;152:1887‐92. [DOI] [PubMed] [Google Scholar]
Midgren 1992 {published data only}
- Midgren B, Melander B, Persson G. Formoterol, a new long acting beta2 agonist, inhaled twice daily in stable asthmatic subjects. Chest 1992;101:1019‐22. [DOI] [PubMed] [Google Scholar]
Molimard 2001 {published data only}
- Molimard M, Bourcereau V, LeGros V, Bourdeix I, Leynadier F, Duroux P. Comparison between formoterol 12mcg BID and on‐demand salbutamol in moderate persistent asthma. Respiratory Medicine 2001;95:65‐70. [DOI] [PubMed] [Google Scholar]
Nathan 1999 {published data only}
- Nathan R, Pinnas J, Schwartz H, Grossman J, Yancey S, Emmett A, et al. A six‐month, placebo‐controlled comparison of the safety and efficacy of salmeterol or beclomethasone for persistent asthma. Annals of Allergy 1999;82(6):521‐9. [DOI] [PubMed] [Google Scholar]
Nelson 1999 {published data only}
- Nelson H, Berkowitz R, Tinkelman D, Emmett A, Rickard K, Yancey S. Lack of Subsensitivity to Albuterol After Treatment with Salmeterol in Patients with Asthma. American Journal of Respiratory & Critical Care Medicine 1999;159:1556‐61. [DOI] [PubMed] [Google Scholar]
Nelson 1998 {published data only}
- Nelson J, Strauss L, Skowronski M, Ciufo R, Novak R, McFadden EJ. Effect of long‐term salmeterol treatment on exercise‐induced asthma. New England Journal of Medicine 1998;339(141‐6). [DOI] [PubMed] [Google Scholar]
Newnham 1993 {published data only}
- Newnham DM, Ingram CG, Earnshaw J, et al. Salmeterol provides prolonged protection against exercise induced bronchoconstriction in a majority of subjects with mild stable asthma. Respiratory Medicine 1993;87:439‐44. [DOI] [PubMed] [Google Scholar]
Newnham 1994 {published data only}
- Newnham DM, McDevitt DG, Lipworth BJ. Bronchodilator subsensitivity after chronic dosing with eformoterol in patients with asthma. American Journal of Medicine 1994;97(1):29‐37. [DOI] [PubMed] [Google Scholar]
Newnham 1995 {published data only}
- Newnham DM, Grove A, McDevitt DG, Lipworth BJ. Subsensitivity of bronchodilator and systemic beta 2 adrenoceptor responses after regular twice daily treatment with eformoterol dry powder in asthmatic patients. Thorax 1995;50(5):475‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nichol 1990 {published data only}
- Nichol G, Nix A, Barnes P, Chung K. Prolonged attenuation of BHR to methacholine by long acting b2adrenoceptor agonist formoterol. American Review of Respiratory Disease 1990;141:A 210. [Google Scholar]
Nielsen 1999 {published data only}
- Nielsen L, Pedersen B, Faurschou P, Madsen F, Wilcke J, Dahl R. Salmeterol reduces the need for inhaled corticosteroid in steroid‐dependent asthmatics. Respiratory Medicine 1999;93(12):863‐8. [DOI] [PubMed] [Google Scholar]
Nix 1990 {published data only}
- Nix A, Nichol G, Robson A, Barnes P, Chung K. Effect of formoterol, a long‐lasting beta2adrenoceptor agonist, against methacholine‐induced bronchoconstriction. British Journal of Clinical Pharmacology 1990;29:321‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norhaya 1999 {published data only}
- Norhaya M, Yap T, Zainudin B. Addition of inhaled salmeterol to inhaled corticosteroids in patients with poorly controlled nocturnal asthma. Respirology 1999;4(1):77‐81. [DOI] [PubMed] [Google Scholar]
Nowak 1992 {published data only}
- Nowak D, Jorres R, Rabe KF, et al. Salmeterol protects agonist hyperventilation induced bronchoconstriction over 12 hours. European Journal of Clinical Pharmacology 1992;43:591‐5. [DOI] [PubMed] [Google Scholar]
Palmer 1992 {published data only}
- Palmer JBD, Stuart AM, Shepherd GL, Viskum K. Inhaled salmeterol in the treatment of patients with moderate to severe ROAD‐ a 3 mth comparison of the efficacy and safety of bd salmeterol (100mcg) and salmeterol (50mcg). Respiratory Medicine 1992;86:409‐17. [DOI] [PubMed] [Google Scholar]
Pauwels 1997 {published data only}
- Pauwels RA, Lofdahl CG, Postma DS, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. New England Journal of Medicine 1997;337:1405‐11. [DOI] [PubMed] [Google Scholar]
Pearlman 1996 {published data only}
- Pearlman DS, Bronsky E, Chervinsky P, et al. Inhaled salmeterol powder compared with placebo administered over 12 weeks to children with mild to moderate asthma. American Journal of Respiratory & Critical Care Medicine 1996;153(4):A76. [Google Scholar]
Pearlman 1999 {published data only}
- Pearlman D, Stricker W, Weinstein S, Gross G, Chervinsky P, Woodring A, et al. Inhaled salmeterol and fluticasone: A study comparing monotherapy and combination therapy in asthma. Annals of Allergy 1999;82(3):257‐65. [DOI] [PubMed] [Google Scholar]
Pederson 1993 {published data only}
- Pederson B, Dahl R, Larsen BB, et al. The effect of salmeterol on the early and late phase reaction to bronchial allergen and post challenge variation in BHR, blood eosinophils, serum ECP and serum eosinophil protein X. Allergy 1993;48:377‐82. [DOI] [PubMed] [Google Scholar]
Quebe‐Fehling 1996 {published data only}
- Quebe‐Fehling E, Brambilla R, Bromly C L, Fishwick K, Walters E H, Hendrick DJ. The duration of action of inhaled formoterol dry powder. British Journal of Clinical Practice 1996;50(8):446‐9. [PubMed] [Google Scholar]
Rabe 1993 {published data only}
- Rabe KF, Jorres R, Nowak D, et al. Comparison of the effects of salmeterol and formoterol on airway tone and responsiveness over 24 hours in bronchial asthma. American Review of Respiratory Disease 1993;147:1436‐41. [DOI] [PubMed] [Google Scholar]
Ramage 1994 {published data only}
- Ramage L, Cree IA, Dhillon DP. Comparison of salmeterol with placebo in mild asthma: effect on peripheral blood phagocyte function and cytokine levels. International Archives of Allergy & Immunology 1994;105:181‐4. [DOI] [PubMed] [Google Scholar]
Ramage Lipworth 1994 {published data only}
- Ramage L, Lipworth BJ, Ingram CG, et al. Reduced protection against exercise induced bronchoconstriction after chronic dosing with salmeterol. Respir Med 1994;88:363‐8. [DOI] [PubMed] [Google Scholar]
Ramsdale 1991 {published data only}
- Ramsdale E, Otis J, Kline P, Gontovnick L, Hargreave F, O'Byrne P. Prolonged protection against methacholine induced bronchoconstriction by the inhaled b2 agonist formoterol. American Review of Respiratory Disease 1991;143:998‐1001. [DOI] [PubMed] [Google Scholar]
Ringbaek 1996 {published data only}
- Ringbaek TJ, Soes‐Petersen U, Christensen M, Iversen ET, Rasmussen FV. Salmeterol compared with salbutamol controlled release in patients with moderate bronchial asthma. Ugeskrift for Laeger 1996;158:3940‐3. [PubMed] [Google Scholar]
Roberts 1999 {published data only}
- Roberts J, Bradding P, Britten K, Walls A, Wilson S, Gratziou C, et al. The long‐acting beta2‐agonist salmeterol xinafoate: effects on airway inflammation in asthma. European Respiratory Journal 1999;14(2):275‐82. [DOI] [PubMed] [Google Scholar]
Roberts 1992 {published data only}
- Roberts B, Bradding P, Holgate S. Effects of a six week course of salmeterol on bronchial reactivity. Thorax 1992;47:230p. [Google Scholar]
Rosenthal 1997 {published data only}
- Rosenthal R, Chervinsky P, DeGraaf A, et al. Long term regular treatment with salmeterol is effective in protecting against bronchial hyperresponsiveness as measured by methacholine challenge in asthmatics [abstract]. Journal of Allergy & Clinical Immunology 1997;99 Suppl:323. [Google Scholar]
Rosenthal 1999 {published data only}
- Rosenthal R, Busse W, Kemp J, Baker J, Kalberg C, Emmett A, et al. Effect of long‐term salmeterol therapy compared with as‐needed albuterol use on airway hyperresponsiveness. Chest 1999;116(3):595‐602. [DOI] [PubMed] [Google Scholar]
Russell 1995 {published data only}
- Russell G, Williams DAJ, Weller P, Price JF. Salmeterol xinafoate in children on high dose inhaled steroids. Annals of Allergy, Asthma and Immunology 1995;75(5):423‐8. [PubMed] [Google Scholar]
Schaaning 1996 {published data only}
- Schaaning J, Vilsvik J, Henriksen AH. Efficacy and duration of salmeterol in protecting against exercise induced bronchoconstriction. Annals of Allergy, Asthma, & Immunology 1996;76:57‐60. [DOI] [PubMed] [Google Scholar]
Schreurs 1996 {published data only}
- Schreurs A, Sinninghe Damste H, Graaff C, Greefhorst A. A dose‐response study with formoterol Turbuhaler as maintenance therapy in asthmatic patients. European Respiratory Journal 1996;9(8):1678‐83. [DOI] [PubMed] [Google Scholar]
Self 1998 {published data only}
- Self T, Rumbak MJ, Kelso T, Eberle L, Abou‐Shala N, Learned CC, et al. Does salmeterol facilitate 'step‐down' therapy in patients with asthma receiving moderate to high doses of inhaled corticosteroids?. Current Therapeutic Research, Clinical & Experimental 1998;59:803‐11. [Google Scholar]
Shapiro 2000 {published data only}
- Shapiro G, Lumry W, Wolfe J, Given J, White M, Woodring A, et al. Combined salmeterol 50 mug and fluticasone propionate 250 in the diskus device for the treatment of asthma. American Journal of Respiratory & Critical Care Medicine 2000;161:527‐34. [DOI] [PubMed] [Google Scholar]
Shepherd 1991 {published data only}
- Shepherd G, Jenkins W, Alexander J. Asthma exacerbations in patients taking regular salmeterol, or salbutamol for symptoms. Lancet 1991;337(8754):1424. [DOI] [PubMed] [Google Scholar]
Sichletidis 1993 {published data only}
- Sichletidis L, Daskalopoulou E, Kyriakis G, et al. Comparative efficacy of salbutamol and salmeterol in exercise induced asthma. Journal of Internal Medicine Research 1993;21:81‐8. [DOI] [PubMed] [Google Scholar]
Siergiejko 1998 {published data only}
- Siergiejko Z, Zietkowsk1 Z, Rogalewska A, Chyrek‐Borowska S. Clinical evaluation of 12 week salmeterol therapy in allergic asthma patients. Pneumonologia i Alergololia Polski 1998;66:450‐5. [PubMed] [Google Scholar]
Simons 1992 {published data only}
- Simons F, Soni N, Watson W, Becker A. Bronchodilator and bronchoprotective effects of salmeterol in young patients with asthma. Journal of Allergy & Clinical Immunology 1992;90:840‐6. [DOI] [PubMed] [Google Scholar]
Simons 1997 {published data only}
- Simons FER, et al. A one year placebo controlled study of the efficacy and safety of beclomethasone DP versus salmeterol in glucocorticoid naive children with asthma. Journal of Allergy & Clinical Immunology 1997;99 Suppl:402. [Google Scholar]
Simons 2 1997 {published data only}
- Simons FER. A comparison of Beclomethasone, salmeterol and placebo in children with asthma. New England Journal of Medicine 1997;337(23):1659‐65. [DOI] [PubMed] [Google Scholar]
Simons Gerst 1997 {published data only}
- Simons FER, Gerstner TV, Cheang MS. Tolerance to the bronchoprotective effect of salmeterol in adolescents with exercise‐induced asthma using concurrent inhaled glucocorticoid treatment. Pediatrics 1997;99(5):655‐9. [DOI] [PubMed] [Google Scholar]
Smyth 1993 {published data only}
- Smyth ET, Pavord ID, Wong C, Wisniewiski ASZ, Williams J, Tattersfield AE. Interaction and dose equivalence of salbutamol and salmeterol in patients with asthma. British Medical Journal 1993;306:543‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Starke 1996 {published data only}
- Starke I, Luce P. The efficacy and safety of inhaled salmeterol 50 microg bd in older patients with reversible airflow obstruction. Age & Ageing 1996;25:67‐71. [DOI] [PubMed] [Google Scholar]
Sussman 1995 {published data only}
- Sussman HS. Continuous eformoterol and beta 2‐receptor responsiveness.. British Journal of Clinical Practice 1995;81(Symposium Supplement.):16‐7. [PubMed] [Google Scholar]
Tan 1997 {published data only}
- Tan KS, Grove A, McLean A, Gnosspelius Y, Hall IP, Lipworth BJ. Systemic corticosteroid rapidly reverses bronchodilator subsensitivity induced by formoterol in asthmatic patients. American Journal of Respiratory & Critical Care Medicine 1997;156:28‐35. [DOI] [PubMed] [Google Scholar]
Tattersfield 2001 {published data only}
- Tattersfield A, Lofdahl C‐G, Postma D, Eivindson A, Schreurs A, Rasidikis A, et al. Comparison of formoterol and terbutaline for as‐needed treatment of asthma: as randomised trial. The Lancet 2001;357:257‐61. [DOI] [PubMed] [Google Scholar]
Tattersfield 1999 {published data only}
- Tattersfield A, Postma D, Barnes P, Svensson K, Bauer C, O'Byrne P, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations. The FACET International Study Group. American Journal of Respiratory & Critical Care Medicine 1999;160(2):594‐9. [DOI] [PubMed] [Google Scholar]
Taylor 1992 {published data only}
- Taylor IK, O'Shaugnessy KM, Choudry NB, et al. A comparative study in atopic subjects with asthma of the effects of salmeterol and salbutamol on allergen induced bronchoconstriction, increase in AR ,increase in urinary leukotriene E4 excretion. Journal of Allergy & Clinical Immunology 1992;89:575‐83. [DOI] [PubMed] [Google Scholar]
Totterman 1998 {published data only}
- Totterman KJ, Huhti L, Sutinen E, Backman R, Pietinalho A, Falck M, et al. Tolerability to high doses of formoterol and terbutaline via Turbuhaler(TM) for 3 days in stable asthmatic patients. European Respiratory Journal 1998;12(3):573‐9. [DOI] [PubMed] [Google Scholar]
Turner 1998 {published data only}
- Turner M, Johnston P, Pizzichini E, et al. Anti‐inflammatory effects of salmeterol compared with beclomethasone in eosinophilic mild exacerbations of asthma: a randomized, placebo controlled trial. Canadian Respiratory Journal 1998;5:261‐8. [DOI] [PubMed] [Google Scholar]
Twentyman 1990 {published data only}
- Twentyman OP, Finnerty JP, Harris A, et al. Protection against allergen induced asthma by salmeterol. Lancet 1990;336:1338‐42. [DOI] [PubMed] [Google Scholar]
Ullman 1988 {published data only}
- Ullman A, Svedymr N. Salmeterol a new long acting inhaled beta agonist: comparison with salbutamol in adult asthmatic patients. Thorax 1988;43:674‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ullman 1990 {published data only}
- Ullman A, Hedner J, Svedmyr N. Inhaled salmeterol and salbutamol in asthmatic patients. An evaluation of asthma symptoms and the possible development of tachyphylaxis. American Review of Respiratory Disease 1990;142:571‐5. [DOI] [PubMed] [Google Scholar]
Van der Molen 1996 {published data only}
- Molen T, Postma DS, Turner MO, De‐Jong BM, Sears MR. Effects of the long acting beta agonist formoterol on asthma control in asthmatic patients using inhaled corticosteroids. Thorax 1996;52(6):535‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Molen 1998 {published data only}
- Molen T, Sears MR, Graaff CS, Postma DS, Meyboom‐de Jong B. Quality of life during formoterol treatment: comparison between asthma‐specific and generic questionnaires. European Respiratory Journal 1998;12(1):30‐4. [DOI] [PubMed] [Google Scholar]
Verberne 1991 {published data only}
- Verberne A, Lenney W, Kerribyjn K. A 3 way crossover study comparing twice daily dosing of salmeterol 25mcg and 50mcg with placebo in children with mild to moderate reversible airways disease[abstract]. American Review of Respiratory Disease 1991;143(suppl 2):20. [Google Scholar]
Verberne 1996 {published data only}
- Verberne AAPH, Hop WCJ, Creyghton FBM, et al. Airway responsiveness after a single dose of salmeterol and during four months of treatment in children with asthma. Journal of Allergy & Clinical Immunology 1996;97:938‐46. [DOI] [PubMed] [Google Scholar]
Verberne 1997 {published data only}
- Verberne A, Frost C, Roorda R, Laag H, Kerrebijn K. One year treatment with salmeterol compared with beclomethasone in children with asthma. The Dutch Paediatric Asthma Study Group. American Journal of Respiratory & Critical Care Medicine 1997;156:688‐95. [DOI] [PubMed] [Google Scholar]
Verberne 1998 {published data only}
- Verberne AA, Frost C, Duiverman EJea. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. The Dutch Asthma Study Group. American Journal of Respiratory & Critical Care Medicine 1998;158:213‐9. [DOI] [PubMed] [Google Scholar]
Verberne 2000 {published data only}
- Verberne A, Jongste J. Long‐acting beta2‐agonists in childhood asthma: Don't change a winning team (yet). Pediatric Pulmonology 2000;29(3):169‐171. [DOI] [PubMed] [Google Scholar]
Verini 1998 {published data only}
- Verini M, Verrotti A, Greco R, Chiarelli F. Comparison of the bronchodilator effect of inhaled short‐ and long‐acting beta2‐agonists in children with bronchial asthma. A randomised trial. Clinical Drug Investigation 1998;16(1):19‐24. [DOI] [PubMed] [Google Scholar]
Viskum 1990 {published data only}
- Viskum K. Inhaled salmeterol improves control in moderate to severe asthmatics: a 3mth study. European Respiratory Journal 1990;3 Suppl (10):235. [Google Scholar]
Von Berg 1996 {published data only}
- Berg A, Blic J, Rosa M, et al. Regular salbutamol xinafoate compared with salbutamol as required in children with moderate asthma [abstract]. American Journal of Respiratory & Critical Care Medicine 1996;4:A76. [Google Scholar]
Von Berg 1998 {published data only}
- Berg A, Blic J, Rosa M, et al. A comparison of regular salmeterol versus as required salbutamol in asthmatic children. Respiratory Medicine 1998;92:292‐9. [DOI] [PubMed] [Google Scholar]
Wallaert 1999 {published data only}
- Wallaert B, Brun P, Ostinelli J, Murciano D, Champel F, Blaive B, et al. A comparison of two long acting beta agonists, oral bambuterol and inhaled salmeterol, in the treatment of asthmatics with nocturnal symptoms. Respiratory Medicine 1999;93:33‐8. [DOI] [PubMed] [Google Scholar]
Wallin 1999 {published data only}
- Wallin A, Melander B, Rosenhall L, Sandstrom T, Wahlander L. Formoterol, a new long acting beta2 agonist for inhalation twice daily, compared with salbutamol in the treatment of asthma. Thorax 1990;45(4):259‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallin 1990 {published data only}
- Rosenhall L, Sandstrom T, Wallin A. Formoterol, a long acting inhaled beta‐2 agonist, twice daily for 1 year in asthmatic patients. American Review of Respiratory Disease 1990;141:A210. [Google Scholar]
- Wallin A, Melander B, Rosenhall L, Sandstrom T, Wahlander L. Formoterol, a new long acting beta2 agonist for inhalation twice daily, compared with salbutamol in the treatment of asthma. Thorax 1990;45(4):259‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walters 1992 {published data only}
- Walters H. Quality of life in long term studies. European Respiratory Journal 1992;5 Suppl:318. [Google Scholar]
Weinstein 1997 {published data only}
- Weinstein S, Chervinsky P, Pollard SJ, Bronsky EA, Nathan RA, Prenner B, et al. A one‐week dose‐ranging study of inhaled salmeterol in children with asthma. Journal of Asthma 1997;34(1):43‐52. [DOI] [PubMed] [Google Scholar]
Weinstein 1998 {published data only}
- Weinstein S, Pearlman D, Bronsky E, Byrne A, Arledge T, Liddle R, et al. Efficacy of salmeterol xinafoate powder in children with chronic persistent asthma. Annals of Allergy, Asthma, & Immunology 1998;81:51‐8. [DOI] [PubMed] [Google Scholar]
Wilding 1997 {published data only}
- Wilding P, Clark M, Thompson J, et al. The effect of long term treatment with salmeterol on asthma control: a double blind randomised crossover study. British Medical Journal 1997;314:1441‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolfe 2000 {published data only}
- Wolfe J, Kreitzer S, Chervinsky P, Lawrence M, Wang Y, Reilly D, et al. Comparison of powder and aerosol formulations of salmeterol in the treatment of asthma. Annals of Allergy 2000;84(3):334‐40. [DOI] [PubMed] [Google Scholar]
Wong 1997 {published data only}
- Wong AG, O'Shaughnessy AD, Walker CM, Sears MR. Effects of long‐acting and short‐acting beta‐agonists on methacholine dose‐response curves in asthmatics. European Respiratory Journal 1997;10:330‐6. [DOI] [PubMed] [Google Scholar]
Woolcock 1996 {published data only}
- Woolcock A, Lundback B, Ringdal N, et al. Comparison of the addition of salmeterol to inhaled steroids with the doubling of the dose of inhaled steroids. American Journal of Respiratory & Critical Care Medicine 1996;153:1481‐8. [DOI] [PubMed] [Google Scholar]
Wronska 1998 {published data only}
- Wronska J, Chazan R, Mazurek J, Droszcz W. Treatment with salmeterol and quality of life in patients with asthma. Pneumonologia i Alergologi Polski 1998;66:193‐7. [PubMed] [Google Scholar]
Yates 1995 {published data only}
- Yates DH, Sussman HS, Shaw MJ, Barnes PJ, Chung KF. Regular formoterol treatment in mild asthma. Effect on bronchial responsiveness during and after treatment. American Journal of Respiratory & Critical Care Medicine 1995;152:1170‐4. [DOI] [PubMed] [Google Scholar]
Yates 1997 {published data only}
- Yates DH, Worsdell M, Barnes PJ. Effect of regular salmeterol treatment on albuterol‐induced bronchoprotection in mild asthma. American Journal of Respiratory & Critical Care Medicine 1997;156(3):988‐91. [DOI] [PubMed] [Google Scholar]
Zarkovic 1998 {published data only}
- Zarkovic J, Gotz MH, Holgate ST, Taak NK. Effect of long‐term regular salmeterol treatment in children with moderate asthma. Clinical Drug Investigation 1998;15(3):169‐75. [Google Scholar]
Zellweger 1994 {published data only}
- Zellweger JP, Plenninger M, Ruff P. 24 hour protective effect of salmeterol 50mg v formoterol 24 mg against methacholine induced bronchoconstriction in mild to moderate asthmatic patients: a randomised double blind crossover single dose trial. European Respiratory Journal 1994 Suppl (18);suppl 18:422. [Google Scholar]
References to studies awaiting assessment
Cloosterman 2001 {published data only}
- Cloosterman SG, Bijl‐Hofland ID, Herwaarden CL, et al. A placebo‐controlled clinical trial of regular monotherapy with short‐acting and long‐acting beta(2)‐agonists in allergic asthmatic patients. Chest 2001;119:1306‐15. [DOI] [PubMed] [Google Scholar]
Rhee 1997 {published data only}
- Rhee YK. A comparison of salmeterol with salbutamol inhalation in treatment of mild to moderate asthma. Tuberculosis and Respiratory Diseases 1997;44(4):815‐21. [Google Scholar]
Sprogoe‐Jakobsen 92 {published data only}
- Sprogoe‐Jakobsen U, Viktrup L, Davidsen O, Viskum K. Bronchial asthma treated with long‐acting beta 2 agonist. Comparison between formoterol (12 mu/g) inhaled twice daily and salbutamol (200 mu/g) inhaled 4 times daily. Ugeskr‐Laeger 1992;154(3):325‐8. [PubMed] [Google Scholar]
Stalenheim 1994 {published data only}
- Stalenheim G, Wegener T, Grettve L, et al. Efficacy and tolerance of a 12‐week treatment with inhaled formoterol in patients with reversible obstructive lung disease. Respiration 1994;61:305‐9. [DOI] [PubMed] [Google Scholar]
Thomson 1998 {published data only}
- Thomson N, Angus R, Quebe‐Fehling E, Brambilla R. Efficacy and tolerability of formoterol in elderly patients with reversible obstructive airways disease. Respiratory Medicine 1992;92:562‐7. [DOI] [PubMed] [Google Scholar]
Additional references
AAACI 1993
- American Academy of Allergy and Clinical Immunology, Executive committee. Inhaled beta2 agonist in asthma. Journal of Allergy & Clinical Immunology 1993;91:1234‐7. [PubMed] [Google Scholar]
Abramson 2001
- Abramson M, Bailey M, Couper F, et al. Are asthma medications and management related to deaths from asthma?. American Journal of Respiratory & Critical Care Medicine 2001;163:12‐8. [DOI] [PubMed] [Google Scholar]
Adcock 1996
- Adcock I, Stevens D, Barnes P. Interactions of glucocorticoids and beta2 agonists. European Respiratory Journal 1996;9:160‐9. [DOI] [PubMed] [Google Scholar]
Adkins 1997
- Adkins JC, McTavish D. Salmeterol. A review of its pharmacological properties and clinical efficacy in the management of children with asthma. Drugs 1997;54(2):331‐54. [DOI] [PubMed] [Google Scholar]
Bartow 1998
- Bartow RA, Brogen RN. Formoterol. An update of its pharmacological properties and therapeutic efficacy in the management of asthma. Drugs 1998;55:303‐22. [DOI] [PubMed] [Google Scholar]
Beasley 1999
- Beasley R, Pearce N, Crane J, Burgess C. Beta‐agonists: What is the evidence that their use increases the risk of asthma morbidity and mortality?. Journal of Allergy & Clinical Immunology 1999;104 Suppl (2 ll):18‐30. [DOI] [PubMed] [Google Scholar]
Bisgard 2000
- Bisgaard H. Long‐acting beta(2)‐agonists in management of childhood asthma: A critical review of the literature. Pediatric Pulmonology 2000;29(3):221‐34. [DOI] [PubMed] [Google Scholar]
Boulet 1994
- Boulet LP. Long versus short acting beta agonists. Drugs 1994;47:207‐22. [DOI] [PubMed] [Google Scholar]
Bousquet 2000
- Bousquet J. Global initiative for asthma (GINA) and its objectives. Clinical & Experimental Allergy 2000;30 Supp (1):2‐5. [DOI] [PubMed] [Google Scholar]
BTS 1993
- British Thoracic Society, British Paediatric Association, et al. Guidelines on the management of asthma. Thorax 1993;48 Suppl:1‐24. [Google Scholar]
BTS 1997
- British Thoracic Society, NAtional Asthma Caompaign, Royal College of Pysicians, et al. The British guidelines on Asthma Management 1995 review and position statement. Thorax 1997;52 Suppl:1. [Google Scholar]
Campbell 1976
- Campbell A. Mortality from asthma and bronchodilator aerosols. Medical Journal of Australia 1976;1:386‐91. [PubMed] [Google Scholar]
Campbell 1999
- Campbell LM, Anderson TJ, Parashchak MR, Burke CM, Watson AS, Turbitt ML. [A comparison of the efficacy of long‐acting beta 2‐agonists: eformoterol via Turbohaler and salmeterol via pressurized metered dose inhaler or Accuhaler, in mild to moderate asthmatics. Respiratory Medicine]. Respiratory Medicine 1999;93(7):236‐44. [PubMed] [Google Scholar]
Cockcroft 1993
- Cockcroft DW, McParland CP, Britto SA. Regular inhaled salbutamol and airway responsiveness to allergen. Lancet 1993;342:833‐7. [DOI] [PubMed] [Google Scholar]
Cockcroft 1996
- Cockcroft DW, Swystun VA. Functional antagonism produced by inhaled beta agonists. Thorax 1996;51:1051‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crane 1989
- Crane J, Pearce N, Flatt A, et al. Prescribed fenoterol and death from asthma in New Zealand 1981‐1983. A case control study. Lancet 1989;1:917‐22. [DOI] [PubMed] [Google Scholar]
D'Urzo 1997
- D'Urzo D. Long acting beta agonists. Can Fam Physician 1997;43:1773‐7. [PMC free article] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Devoy 1995
- Devoy MAB, Fuller RW, Palmer JBD. Asthma mortality and beta agonists. Chest 1995;108:1768. [DOI] [PubMed] [Google Scholar]
Devoy Fuller 1995
- Devoy MAB, Fuller RW, Palmer JBD. Beta agonists in the treatment of asthma?. Chest 1995;107:1116‐24. [DOI] [PubMed] [Google Scholar]
Faurschou 1994
- Faurschou P, Engel AM, Haanaes OC. [Salmeterol in two different doses in the treatment of nocturnal bronchial asthma poorly controlled by other therapies]. Allergy 1994;10:827‐32. [DOI] [PubMed] [Google Scholar]
French 1994
- French DJ, Christie MJ, Sowden AJ. The reproducibility of the childhood asthma Questionnaires: measures of quality of life for children with asthma aged 4‐16 yrs. Quality of Life Research 1994;3:215‐24. [DOI] [PubMed] [Google Scholar]
Fuller 1995
- Fuller R. Safety of salmeterol in the treatment of asthma. European Respiratory Review 1995;5:133‐7. [Google Scholar]
Giannini 2000
- Giannini D, Franco A, Bacci E, Dente FL, Taccola M, Vagaggini B, et al. The protective effect of salbutamol inhaled using different devices on methacholine bronchoconstriction. Chest 2000;117(5):1319‐23. [DOI] [PubMed] [Google Scholar]
GINA 1995
- National heart Lung and Blood Institute/WHO. Global strategy for asthma management and prevention. Bethesda: National Institutes of Health, 1995. National heart Lung and Blood Institute/WHO Report. 1995. [Google Scholar]
Hasselblad 1995
- Hasselblad V, Mosteller F, Littenberg B, Chalmers TC, Hunink MG, Turner JA, et al. A survey of current problems in meta‐analysis. Discussion from the Agency for Health Care Policy and Research inter‐PORT Work Group on Literature Review/Meta‐Analysis. Med Care 1995;33(2):202‐20. [PubMed] [Google Scholar]
Howarth 2000
- Howarth PH, Beckett P, Dahl R. The effect of long‐acting beta2‐agonists on airway inflammation in asthmatic patients. Respiratory Medicine 2000;94 Supp (F):22‐25. [DOI] [PubMed] [Google Scholar]
Hyland 1991
- Hyland M. The living with asthma questionnaire. Respir Med 1991;85 Suppl:13‐6. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad A, Moore R, Carroll D, et al. [Assessing the quality of reports of randomised control trials: is blinding really neccesary?]. Controlled Clinical Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Janson 2001
- Janson C, Anto J, Burney P, et al. The European Community Respiratory Health Survey: what are the main results so far? European Community Respiratory Health Survey II. European Respiratory Journal 2001;18:598‐611. [DOI] [PubMed] [Google Scholar]
Juniper 1992
- Juniper EF, Guyatt GH. [Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials]. Thorax 1992;47:76‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juniper 1994
- Juniper EF, Guyatt GH, Willan A, Griffith L. [Determining a minimal important change in a disease‐specific quality of life questionnaire]. Journal of Clinical Epidemiology 1994;47:81‐7. [DOI] [PubMed] [Google Scholar]
Kips 2001
- Kips J, Pauwels R. Long‐acting inhaled best2agonist therapy in asthma. American Journal of Respiratory & Critical Care Medicine 2001;164:923‐32. [DOI] [PubMed] [Google Scholar]
Korosec 1999
- Korosec M, Novak D, Myers E, Skrowonski M, McFadden EJ. [Salmeterol does not compromise the bronchodilator response to albuterol during acute episodes of asthma]. American Journal of Medicine 1999;107:209‐13. [DOI] [PubMed] [Google Scholar]
Lai 1989
- Lai CKW, Twentyman OP, Holgate ST. The effect of an increase in inhaled allergen dose after rimiterol hydrobromide on the occurrence and magnitude of the late asthmatic response and the associated change in nonspecific bronchial hyperresponsiveness. American Review of Respiratory Disease 1989;140:917‐23. [DOI] [PubMed] [Google Scholar]
Lipworth 1999
- Lipworth B, Hall I, Tan S, Aziz I, Coutie W. Effects of genetic polymorphism on ex vivo and in vivo function of beta2‐adrenoceptors in asthmatic patients. Chest 1999;115:324‐8. [DOI] [PubMed] [Google Scholar]
Lipworth Demp 2000
- Lipworth BJ, Dempsey OJ, Aziz I. Functional antagonism with formoterol and salmeterol in asthmatic patients expressing the homozygous Glycine‐16 beta2 adrenoceptor polmorphism. Chest 2000;118(2):321‐8. [DOI] [PubMed] [Google Scholar]
Lipworth Hall 1999
- Lipworth BJ, Hall IP, Aziz I, Tan KS, Wheatley A. Beta2‐adrenoceptor polymorphism and bronchoprotective sensitivity with regular short and long‐acting beta2‐agonist therapy. Clin Sci (Colch) 1999;96:253‐9. [PubMed] [Google Scholar]
Moore 1996
- Moore RH, Khan A, Dickey B. long acting inhaled beta 2 agonists in asthma therapy. Chest 1996;113:1095‐108. [DOI] [PubMed] [Google Scholar]
NAC 1998
- National Asthma Campaign. Asthma Management Handbook. 1998. [Google Scholar]
Page 1993
- Page CP. An explanation of the asthma paradox. American Review of Respiratory Disease 1993;147 Suppl:29‐33. [DOI] [PubMed] [Google Scholar]
Palmquist 1997
- Palmquist M, Persson G, Lazer L, Rosenborg J, Larsson P, Lotvall J. Inhaled dry‐powder formoterol and slameterol in asthmatic patients: onset of action, duration of effect and potency. European Respiratory Journal 1997;10:2484‐9. [DOI] [PubMed] [Google Scholar]
Partridge 2000
- Partridge M, Fabbri L, Chung K. Delivering effective asthma care‐ how do we implement asthma guidelines?. European Respiratory Journal 2000;15:235‐7. [DOI] [PubMed] [Google Scholar]
Pearce 2000
- Pearce N, Sunyer J, Cheng S, et al. Comparison of asthma prevalence in the ISAAC and the ECRHS. ISAAC Steering Committee and the European Community Respiratory Health Survey. International Study of Asthma and Allergies in Childhood.. European Respiratory Journal 2000;16(3):420‐6. [DOI] [PubMed] [Google Scholar]
Sears 1998
- Sears MR. Asthma treatment: inhaled beta‐agonists [Review]. Canadian Respiratory Journal 1998;5:54‐9A. [PubMed] [Google Scholar]
Sears Rea 1986
- Sears M, Rea H, Rothwell R, et al. Asthma mortality: comparison between new Zealand and England. British Medical Journal 1986;293:1342‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Selroos 1998
- Selroos O. The pharmacologic and clinical properties of Oxis (formoterol) Turbuhaler. Allergy 1998;53(42 Suppl):14‐9. [DOI] [PubMed] [Google Scholar]
Shale 1994
- Shale DJ. Respiratory arrests in young asthmatics on salmeterol. Respiratory Medicine 1994;88:75‐6. [DOI] [PubMed] [Google Scholar]
Spitzer 1992
- Spitzer WO, Suissa S, Ernst P, Horwitz RI, Habbick B, et al. The use of beta agonists and the risk of death and near death from asthma. New England Journal of Medicine 1992;326:501‐6. [DOI] [PubMed] [Google Scholar]
Sullivan 1996
- Sullivan S, Elixhauser A, Buist A, Luce B, Eisenberg J, Weiss K. National Asthma Education and Prevention Program working group report on the cost effectiveness of asthma care Program working group report on the cost effectiveness of asthma care. American Journal of Respiratory & Critical Care Medicine 1996;154 Suppl:85‐95. [DOI] [PubMed] [Google Scholar]
Tan Hall 1997
- Tan KS, Hall IP, Dewar JC, Dow E, Lipworth BJ. Association between beta2‐adrenoceptor polymorphism and susceptibility to bronchodilator desensitisation in moderately severe stable asthmatics. Lancet 1997;350:995‐9. [DOI] [PubMed] [Google Scholar]
Tattersfield 1993
- Tattersfield AE. Clinical pharmacology of long‐acting beta‐receptor agonists. [review]. Life Sciences 1993;52(26):2151‐9. [DOI] [PubMed] [Google Scholar]
Taylor 1997
- Taylor D, Jensen M, Aikman S, Harris J, Barnes PJ, O'Connor B. Comparison of salmeterol and albuterol induced bronchoprotection against AMP and histamine in mild asthma. American Journal of Respiratory & Critical Care Medicine 1997;156:1731‐7. [DOI] [PubMed] [Google Scholar]
Taylor 2000
- Taylor DR, Hancox RJ. Interactions between corticosteroids and beta agonists. Thorax 2000;55:595‐602. [DOI] [PMC free article] [PubMed] [Google Scholar]
TSANZ 1989
- Thoracic Society Australia & NZ. Asthma management plan. Medical Journal of Australia 1989;15:650‐3. [PubMed] [Google Scholar]
Van der Molen 1997
- Molen T, Postma DS, Schreurs AJM, Bosveld HEP, Sears MR, Meyboom de Jong B. Discriminative aspects of two generic and two asthma‐specific instruments: Relation with symptoms, bronchodilator use and lung function in patients with mild asthma. Quality of Life Research 1997;6(4):353‐61. [DOI] [PubMed] [Google Scholar]
van Noord 1996
- Noord J, Smeets J, Raaijmakers J, Bommer a, Maesen F. Salmeterol versus formoterol in patients with moderately severe asthma: onset and duration of action. European Respiratory Journal 1996;9:1684‐8. [DOI] [PubMed] [Google Scholar]
Van Schayck 2000
- Schayck C. Do long‐acting beta2‐adrenergic agonists deserve a different place in guidelines for the treatment of asthma and COPD?. European Respiratory Journal 2000;15(4):631‐4. [DOI] [PubMed] [Google Scholar]
Verberne 1995
- Verberne AAPH, McCormack EM, Fuller R, et al. An overview of nine clinical trials of salmeterol in an asthmatic population. European Respiratory Journal 1995;8 Suppl (19)(suppl 19):156. [DOI] [PubMed] [Google Scholar]
Vervloet 1998
- Vervloet D, Ekstrom T, Pela R, Duce Gracia F, Kopp C, Silvert BD, et al. A 6‐month comparison between formoterol and salmeterol in patients with reversible obstructive airways disease. Respiratory Medicine 1998;92(6):836‐42. [DOI] [PubMed] [Google Scholar]
Walters 1999
- Walters EH, Walters J. Inhaled short acting beta‐2 agonist use in asthma: Regular versus as‐needed treatment. The Cochrane Library 1999, Issue 1. [DOI] [PubMed] [Google Scholar]
Weinberger 1995
- Weinberger M. Salmeterol for the treatment of asthma. Annals of Allergy, Asthma, & Immunology 1995;75:209‐11. [PubMed] [Google Scholar]
Woods 2001
- Woods R, Walters E, Wharton C, Watson N, M Abramson. The rising prevalence of asthma in young Melbourne adults is associated with improvement in treatment. Annals of Allergy, Asthma, & Immunology 2001;87:117‐23. [DOI] [PubMed] [Google Scholar]


