Abstract
Background
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by elevated interferon (IFN) signature genes. Galectin-9 (Gal-9) is a β-galactoside-binding lectin that is reportedly useful as a biomarker for IFN gene signatures. In a cross-sectional study of Japanese patients with recent-onset SLE, we aimed to determine whether raised serum Gal-9 levels were associated with the disease activity or organ damage seen in SLE patients.
Methods
The current study included 58 Japanese patients with SLE and 31 age-matched healthy individuals. Disease activity and organ damage were assessed using SLE Disease Activity 2000 (SLEDAI-2K) and Systemic Lupus International Collaborating Clinics (SLICC) damage index. Serum and cerebrospinal fluid (CSF) Gal-9 concentrations were quantified using ELISA. Correlation analyses between Gal-9 and clinical parameters including disease activity were performed.
Results
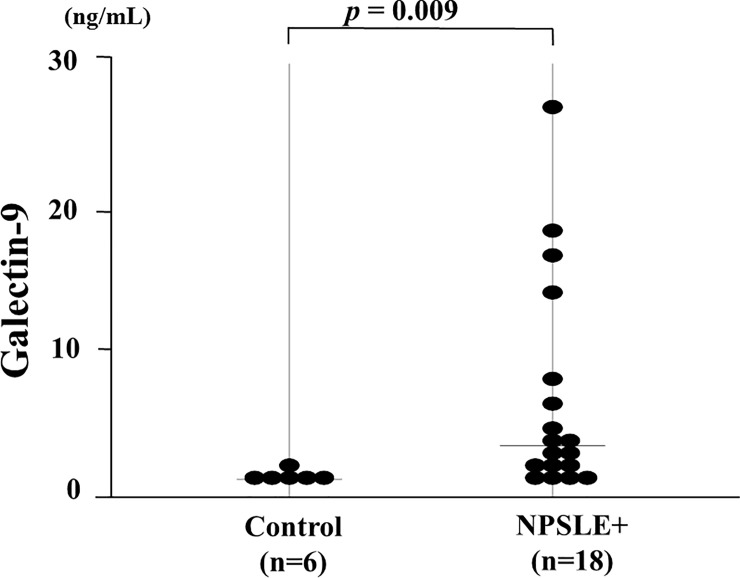
Serum levels of Gal-9 were significantly increased in patients with SLE compared with the control group (16.6 ng/ml, [interquartile range (IQR); 3.6–59.7] versus 4.74 ng/ml, [IQR; 3.0–9.5], p<0.0001). Gal-9 was significantly correlated with disease activity measures in the SLEDAI-2K. Serum Gal-9 levels were significantly greater in patients with SLE-related organ involvement (23.1 ng/ml, [IQR; 5.1–59.7] versus 12.5ng/ml, [IQR; 3.6–39.0], p = 0.013). Whereas there was no difference in serum levels of CXCL10 or M2BPGi between patients with and without SLE-related organ involvement. Serum levels of Gal-9 were significantly higher in SLE patients with active renal involvement determined by BILAG renal score (A-B) compared to those without active renal involvement (C-E). Whereas there was no significant difference in serum levels of Gal-9 between SLE patients with or without active other organ involvements (neurological or hematological) determined by BILAG score. SLE patients with detectable circulating IFN-α had raised serum Gal-9 levels. Levels of Gal-9 were significantly higher in the CSF from patients with recent-onset neuropsychiatric SLE (NPSLE) than in those from non-SLE controls (3.5 ng/ml, [IQR; 1.0–27.2] versus 1.2 ng/ml, [IQR; 0.9–2.1], p = 0.009).
Conclusions
Gal-9 could be a serologic marker of disease activity and organ involvement in SLE patients. Future studies evaluating the role of Gal-9 in the SLE phenotype may provide insights into SLE pathogenesis.
Background
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease characterized by the loss of immunological tolerance against nuclear antigens [1]. The clinical and paraclinical tools to assess disease activity and predict the disease course are inadequate, and identification of easily accessible biomarkers is required for SLE [2]. Activation of the type I interferon (IFN) system is involved in the pathogenesis of SLE [3]. Therefore, type I IFN signatures, such as raised circulating levels of IFN-α or IFN-inducible genes could be linked with the disease activity and disease flares in SLE patients [4]. Surrogate markers for the IFN signature, such as CXCL 10, have been evaluated in SLE patients [5]; however, easy and accurate methods to measure IFN signatures have not been generally established [6]. More recently, Hoogenet et al. demonstrated that galactin-9 (Gal-9) is a novel, easy to measure biomarker for type1 IFN signatures and Gal-9 could aid in clinical decision marking in SLE [7]. Gal-9, one of the β-galactoside binding lectins, plays important regulatory roles in autoimmune diseases [8]. T cell immunoglobulin and mucin domain containing molecule-3 (Tim-3) expressed on T cells is involved in the regulation of Th1 cell-mediated immunity and has been identified as the ligand of Gal-9 [9]. Recent studies also suggest that Gal-9 can suppress the differentiation of Th17 cells in Tim-3-dependent or independent manners [10]. Due to the heterogeneity of the SLE disease phenotype, reliable biomarkers that reflect SLE disease activity and/or organ damage are required. Complement proteins or autoantibodies, such as anti-ds-DNA antibody, are used to monitor global disease activity [11]. However, these parameters could be associated with disease activity and may not reflect the SLE disease phenotype or associated organ damage [12]. Gal-9, which is a type1 IFN signature, should be further evaluated in SLE patients with various disease phenotypes. Mac-2 Binding Protein Gylcan Isomer (M2BPGi), which interacts with galectins, is a reliable marker for assessing liver fibrosis in autoimmune liver diseases [13]. The impact of M2BPGi on outcome was also demonstrated in SLE in addition to autoimmune liver diseases [14]. In this study we sought to determine the role of these circulating soluble proteins related to IFN signatures, including Gal-9, in patients with SLE with different levels of disease activity and disease phenotypes. We also examined the relationship of Gal-9 with disease activity and whether it is a useful biomarker for predicting disease activity including organ involvement in patients with SLE.
Methods
Patients and clinical evaluations
A total of 58 Japanese patients with recent-onset SLE were included in the study. SLE patients were enrolled within 32 months (mean 18 month, range 0–32) of SLE diagnosis, which was based on the fulfillment the American College of Rheumatology (ACR) 1997 criteria [15]. All patients were treated in Department of Rheumatology, Fukushima Medical School from June 2009 to March 2019. All patients with SLE underwent a structured interview, physical examination, laboratory tests, and a review of medical records. In patients with SLE, disease activity and organ damage were ascertained with the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) [16] and the Systemic Lupus International Collaborating Clinics (SLICC) damage index [17], respectively. SLEDAI scores were recorded at the time of follow-up for SLE patients. SLE disease activity was also determined using the British Isles lupus assessment Group (BILAG) score which consisted of evaluation of 8 domains, general, musculocutaneous, neurological, musculoskeletal, cardio-respiratory, renal manifestations, vasculitis and hematological findings [18]. It was designed to reflect physicians’ intention-to-treat with five categories (A, B, C, D and E). As a control group, 31 age- and sex-matched healthy controls (HCs; 5 males and 26 females, median age 39 years [26–52]) were enrolled. This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval for this study (No. 30285) was provided by the Ethics Committee of Fukushima Medical University and written informed consent was obtained from each individual.
Serological analysis
Serum levels of complement 3 (C3) and serum complement 4 (C4), the presence of double strand (ds)-DNA and anti-nuclear antibodies (ANA), and the total number of white blood cells (WBCs) were measured in the clinical laboratory of Fukushima Medical University. Serum samples were obtained from 58 patients with SLE (50 women and 8 men; mean ± SD age 35.8 ± 1.8 years). Among these 58 patients, 5 patients were selected for consecutive analysis with serial serum samples drawn. These patients were chosen due to fluctuations in disease activity during the treatments.
Cerebrospinal fluid (CSF)
CSF samples were obtained in all 18 patients with NPSLE (3 males and 15 females). Among these, 7 patients with NPSLE were included outside of the enrolled 58 SLE paints in whom serum samples were not collected. Their average age at the onset of CNS manifestations was 34.6 years (range 16–63 years). According to the ACR nomenclature [19], the symptoms of NPSLE exhibited by our patients were follows: aseptic meningitis (8), seizures (3), cognitive dysfunction (3), headache (1), cerebrovascular disease (1), myelopathy (1), cranial neuropathy (1).
For ethical reasons, CSF samples were not collected from SLE patients without any neuropsychiatric involvement or from healthy volunteers. Because of the difficulty in confirming neurologic diagnoses and of assigning cause to SLE, we defined NPSLE as the presence of at least 1 clinical feature of neuropsychiatric syndromes and at least 1 of the following: abnormal findings on brain magnetic resonance imaging, diffuse abnormal signal of brain single-photon-emission computerized tomography, severely abnormal results on a neuropsychiatric test, and elevated CSF IgG index or increased interleukin-6 (IL-6) activity in their CSF [20]. We also tested CSF samples from 6 patients with a history of headache who did not have SLE or any other autoimmune diseases, as non-SLE controls. Serum and CSF samples were prepared and stored at -70°C until analyzed. All assays were performed without information of the diagnosis and clinical manifestations.
Enzyme-linked immunosorbent assay for CXCL-10 and Galectin-9
Serum concentrations of Galectin-9 and CXCL10 were measured using human enzyme-linked immunosorbent assay kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instruction. The measurement of IFN- α was performed with the VeriKine ™ Human IFN- α ELISA Kit (Product #41100), following the manufacturer’s instructions.
Measurement of M2BPGi
Serum M2BPGi level was directly measured with the HISCL™ M2BPGi™ reagent kit (Sysmex, Kobe, Japan) using an automatic immunoanalyzer HISCL‐5000 (Sysmex, Hyogo, Japan). M2BPGi levels were indexed using the following equation: Cut‐off Index (C.O.I.) = ([M2BPGi]sample‐[M2BPGi]NC)/([M2BPGi]PC)‐[M2BPGi]NC), where [M2BPGi]sample represents the M2BPGi count of the serum sample (PC: positive control, NC: negative control) [21].
Statistical analysis
Results were non-normally distributed and are presented throughout the manuscript with median and 25–75th centiles [median, IQR] and were compared by the Mann-Whitney U test. Correlations between continuous variables were analyzed by the Spearman’s rank correlation test. Paired data were analyzed by non-parametric tests using the Wilcoxon signed-rank test for the comparison of paired data.
Results
Demographic and clinical characteristics in patients with SLE
We studied 58 patients with SLE and 31 healthy control subjects and the demographics and clinical characteristics of SLE patients are presented in Table 1. Patients were predominantly female (86%), and all patients were of Japanese ethnicity. Approximately 95% of patients had active disease (SLEDAI-2K > 4) and approximately 57% had any organ damage (SDI ≥ 1). Patients and HCs showed no significant differences in age or sex distribution.
Table 1. Baseline characteristics of 58 Japanese patients with SLE.
| Characteristics | n = 58 |
|---|---|
| Gender | |
| Female, n (%) | 50 (86) |
| Male, n (%) | 8 (14) |
| Age, median (range), years | 36 (16–79) |
| Duration of SLE, median (range), month | 18 (0–32) |
| Untreated patients (%) | 52(90) |
| Components of SLE diagnostic criteria, n (%) | |
| Skin rash | 30 (52) |
| Oral ulcers | 4 (7) |
| Alopecia | 1 (2) |
| Arthritis | 20 (34) |
| Serositis | 15 (26) |
| Renal disease | 29(50) |
| CNS disease | 11(19) |
| Hemolytic anemia | 9 (15) |
| Laboratory findings | |
| Leukocytopenia | 21 (36) |
| Thrombocytopenia | 15 (26) |
| Anti-ds-DNA Ab positive | 46 (79) |
| Anti-smith Ab positive | 28 (48) |
| Anti-phospholipid Ab positive | 27 (47) |
| SLEDAI, median(range) | 13(0–50) |
| SDI, median(range) | 1(0–4) |
CNS = central nervous system, Ab = antibody, SLEDAI = SLE Disease Activity, SDI = Systemic Lupus International Collaborating Clinics (SLICC) damage index
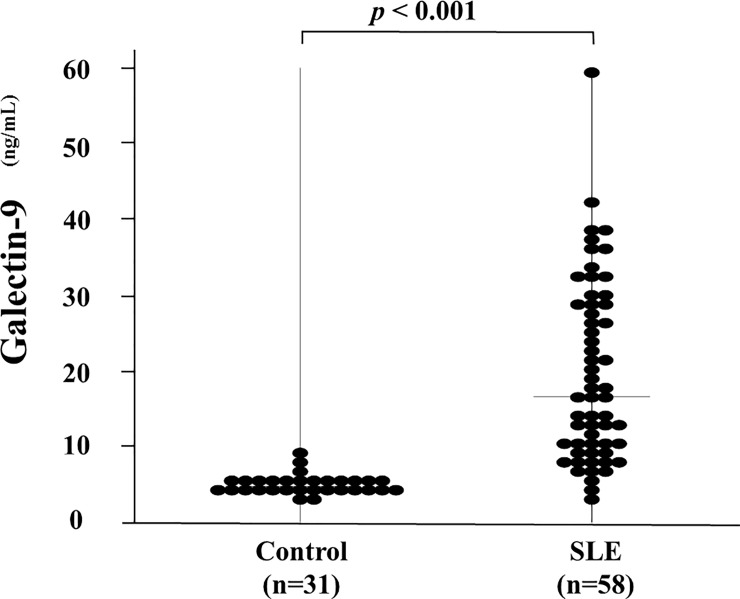
Correlation between circulating levels of Gal-9 and SLE disease activity
We measured serum levels of Gal-9 using specific ELISA assays. As shown in Fig 1, the serum levels of Gal-9 were significantly higher in patients with SLE compared with the healthy controls (16.6 ng/ml [IQR; 3.6–59.7] versus 4.74 ng/ml [IQR; 3.0–9.5], p<0.0001).
Fig 1. Serum levels of Gal-9 in SLE patients (n = 58) and healthy subjects (n = 31).
Higher Gal-9 levels were found in patients with SLE compared with those in healthy subjects. Median Gal-9 levels (bar) are depicted and statistical analysis was performed using the Mann-Whitney U test.
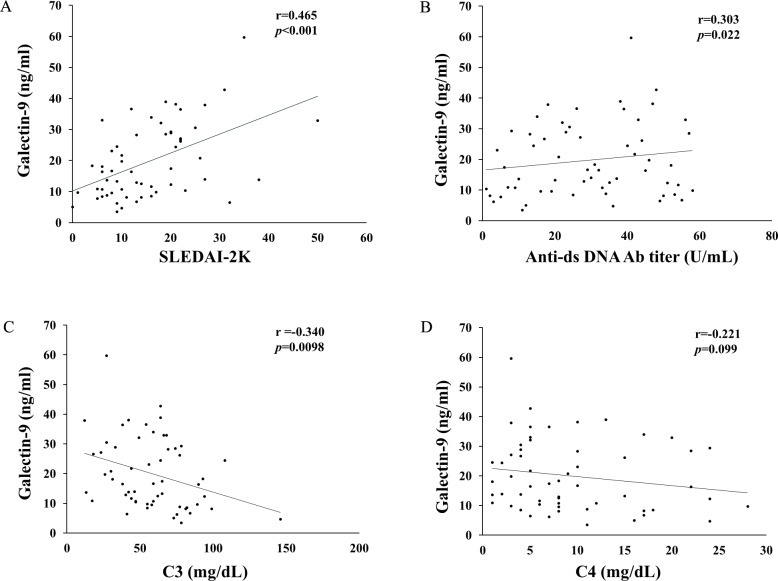
Correlations between Gal-9 levels and disease activity and clinical serological parameters were examined. As sown in Fig 2A–2D, the serum levels of Gal-9 in SLE patients showed a moderate positive correlation with SLE disease activity as measured by the SLEDAI-2K (Fig 2A, p<0.001, r = 0.47 [95%CI; 0.27–0.67]). Additionally, serum levels of Gal-9 showed a weak correlation with serum ds-DNA antibody titer (Fig 2B, p = 0.02, r = 0.30 [95%CI; 0.15–0.42]) and a negative correlation with serum levels of C3 (Fig 2C p = 0.01, r = −0.34 [95%CI; -0.54- -0.11]). There was no significant correlation between serum levels of Gal-9 and C4 (Fig 2D, p = 0.19, r = -0.18 [95%CI; -0.32- -0.02]).
Fig 2.
Correlations between serum levels of Gal-9 and clinical parameters (A: SLEDAI-2K, B: anti-ds-DNA Ab, C: C3 and D: C4) in SLE patients. Serum levels of Gal-9 significantly positively correlated with SLEDAI-2K (A) or anti-ds-DNA Ab (B) and negatively correlated with C3 levels (C). There was no significant correlation between serum levels of Gal-9 and C4 levels (D). Statistics and regression line are represented by the solid line.
Relationships between serum levels of biomarkers and organ involvements
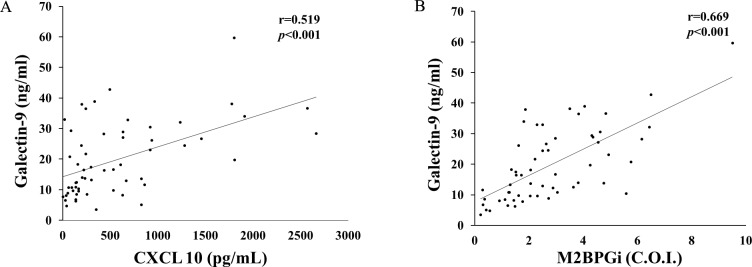
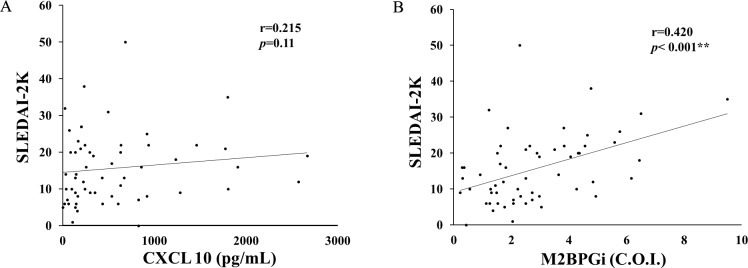
CXCL-10 has been found to be elevated in SLE patients with high type I IFN gene signatures [5]. Therefore, we measured CXCL 10 and M2BPGi using the same sera and tested their correlations with Gal-9. Serum Gal-9 levels were significantly correlated with serum CXCL 10 levels as well as M2BPGi (Fig 3).
Fig 3.
Correlations between serum levels of Gal-9 and CXCL 10 (A) or M2BPGi (B) in patients with SLE. Serum levels of Gal-9 significantly correlated with serum levels of CXCL 10 (A) or M2BPGi (B) in patients with SLE. Statistics and regression line are represented by the solid line. Gal-9 = galetin-9, I CXCL10 = C-X-C motif chemokine 10, M2BPGi = Mac-2 binding protein glycosylation isomer.
We then examined the relationship between serum levels of CXCL 10 or M2BPGi and the SLE disease activity (Fig 4A and Fig 4B). A significant correlation was found between SLEDAI-2K score and circulating levels of M2BPGi (Fig 4A). Whereas there was no significant correlation between SLEDAI-2K score and circulating levels of CXCL 10 (Fig 4B).
Fig 4.
10 (A) or M2BPGi (B) and SLEDAI-2K in patients with SLE. There was no significant correlation between serum levels of Gal-9 and CXCL 10 (A). Serum levels of M2BPGi (B) significantly correlated with SLEDAI-2K in SLE patients. Statistics and regression line are represented by the solid line. Gal-9 = galetin-9, CXCL10 = C-X-C motif chemokine 10, M2BPGi = Mac-2 binding protein glycosylation isomer.
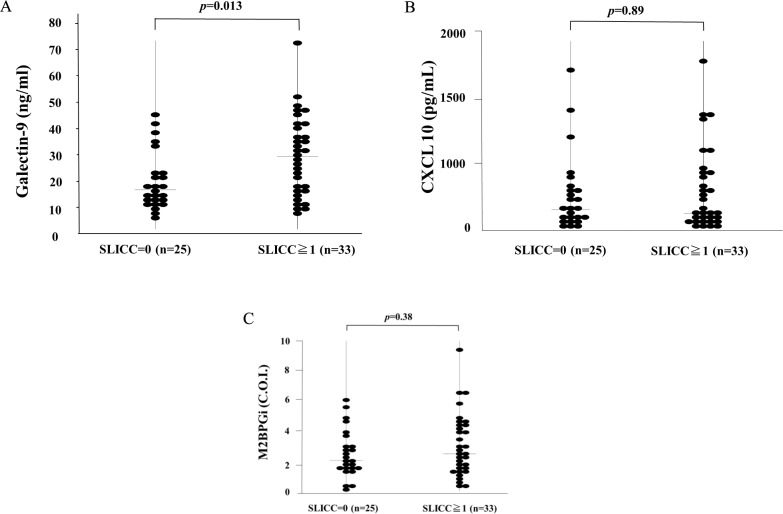
We then divided the patients into groups with or without organ damage measured by the SLICC/ACR Damage Index (SDI) and compared them with the circulating levels of Gal-9 (A), CXCL10 (B) or M2BPGi (C). As shown in Fig 5A, serum levels of Gal-9 were significantly higher in SLE patients with at least one organ damage (SDI ≥ 1) compared with those without organ involvement (23.1 ng/ml [IQR: 4.8–59.7] versus 12.5 ng/ml [IQR: 3.6–36.6], p = 0.013). Conversely, there was no significant difference in serum levels of CXCL 10 (240.2 ng/ml [IQR: 20.9–2664.8] versus 299.6 ng/ml [IQR: 0.4–2570.4], p = 0.89) or M2BPGi (2.5 ng/ml [IQR: 0.6–9.5] versus 2.1ng/ml [IQR: 0.2–6.2], p = 0.38) between SLE patients with and those without organ damage (Fig 5B and Fig 5C).
Fig 5. Serum biomarkers in SLE patients with or without organ damage.
We compared serum levels of biomarkers (A: Gal-9, B: CXCL 10, C: M2BPGi) between SLE patients with any organ damage (i.e., SDI ≥ 1) and those without organ damage (i.e., SDI = 0). Raised serum Gal-9 levels were found in SLE patients with any organ damage compared with those without organ damage (A). No significant difference in CXCL 10 (B) or M2BPGi (C) levels was observed between SLE patients with and without any organ damage. SDI: Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index.
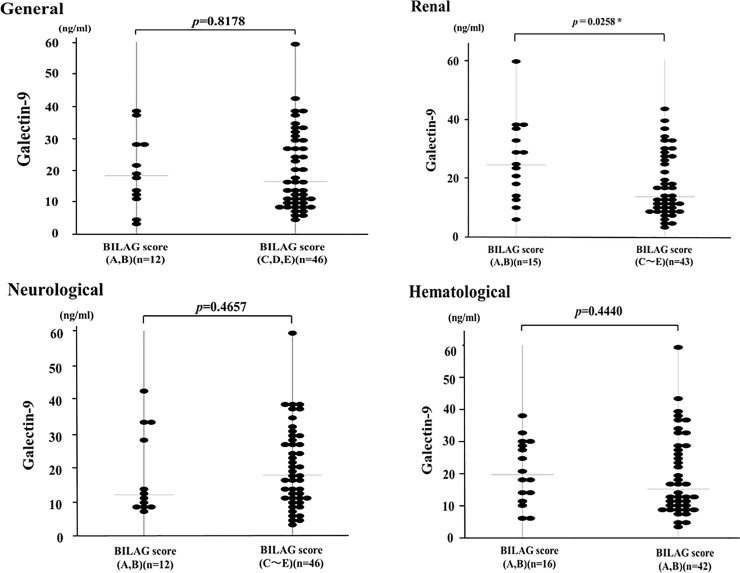
The SDI scores irreversible organ damage that occurred since the onset of SLE regardless of cause. The British Isles lupus assessment Group (BILAG) is used to evaluate the specific manifestations over the previous 4 weeks in a total 8 organ systems. BILAG was found to be useful tool in monitoring disease activity in SLE patients, which was developed to report disease activity in eight organ systems including renal or neurological manifestations [18]. Details of patient’s distribution according to the results of BILAG scores are shown in Table 2. Among 8 domains of BILAG grading, active organ involvements were detected mainly in neurological, renal and hematological domains. As shown in Fig 6, in SLE patients with active renal involvement (BILAG renal A-B), the serum levels of Gal-9 were significantly higher compared to those without active renal involvement (BILAG renal C-E). Whereas there was no significant difference in serum levels of Gal-9 between SLE patients with (BILAG A-B) or without active neurological or hematological involvements (BILAG C-E).
Table 2. Disease activity as assessed by the British Isles Lupus Assessment Group (BILAG) grading.
| BILAG | BILAG grade | ||||
|---|---|---|---|---|---|
| Manifestations | A | B | C | D | E |
| General | 0 | 12 | 14 | 4 | 28 |
| Mucocutaneous | 1 | 4 | 19 | 2 | 32 |
| Neurological | 2 | 10 | 1 | 0 | 45 |
| Musculoskeletal | 1 | 4 | 14 | 2 | 37 |
| Cardiorespiratory | 0 | 6 | 9 | 3 | 40 |
| Gastrointestinal | 0 | 7 | 0 | 0 | 51 |
| Renal | 10 | 5 | 6 | 3 | 34 |
| Hematological | 1 | 15 | 32 | 1 | 9 |
| Opthalmic | 1 | 4 | 6 | 1 | 46 |
BILAG: British Isles Lupus Assessment Group. BILAG grades: A:severe, B: intermediate, C: mild, D: inactive, E: no activity.
Fig 6. Serum levels of Gal-9 in SLE patients with or without active organ involvements.
We compared serum levels of Gal-9 between SLE patients with active organ involvements (BILAG general, renal, neurological, hematological domains; A-B) and without active organ involvement (BILAG; C-E).
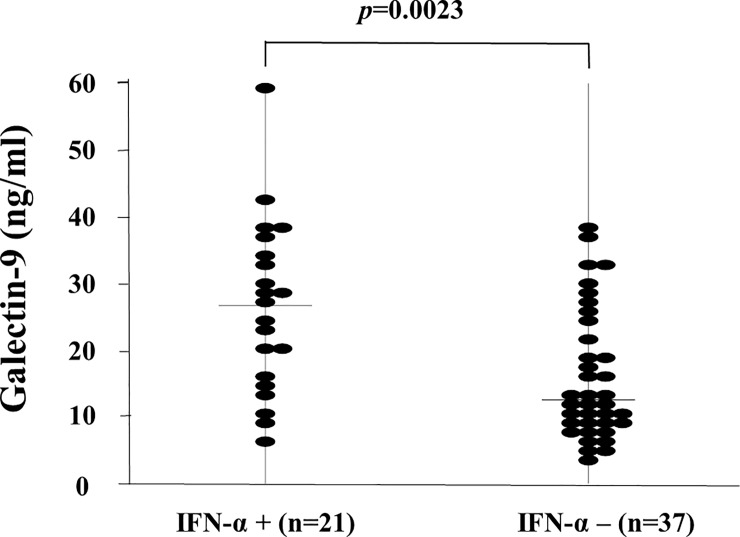
Relationships between serum levels of IFN-α and organ involvements
To examine whether serum IFN-α concentrations were relevant to SLE disease activity, we measured IFN-α using the same sera isolated from SLE patients. IFN-α was detectable in the sera of only a subset of SLE patients (21/58, 36.2%, 70.0pg/ml [IQR: 1.4–601.0]). We compared the circulating levels of Gal-9 between SLE patients with detectable serum IFN-α (cut-off value = 1.0pg/ml, n = 21) and those without detectable serum IFN-α (n = 37). As shown in Fig 7, serum levels of Gal-9 were significantly higher in SLE patients with detectable IFN-α compared with those without detectable IFN-α (26.7 ng/ml [IQR: 6.5–59.7] versus 12.5 ng/ml [IQR: 3.6–39.0], p<0.002).
Fig 7. Serum Galectin-9 (Gal-9) levels in SLE patients with detectable circulating IFN-α.
We compared serum levels of Gal-9 between SLE patients with and those without detectable circulating IFN-α. Raised serum Gal-9 levels were found in SLE patients with detectable circulating IFN-α compared with those without detectable circulating IFN-α. Median Gal-9 levels (bar) are depicted and statistical analysis was performed using the Mann-Whitney U test.
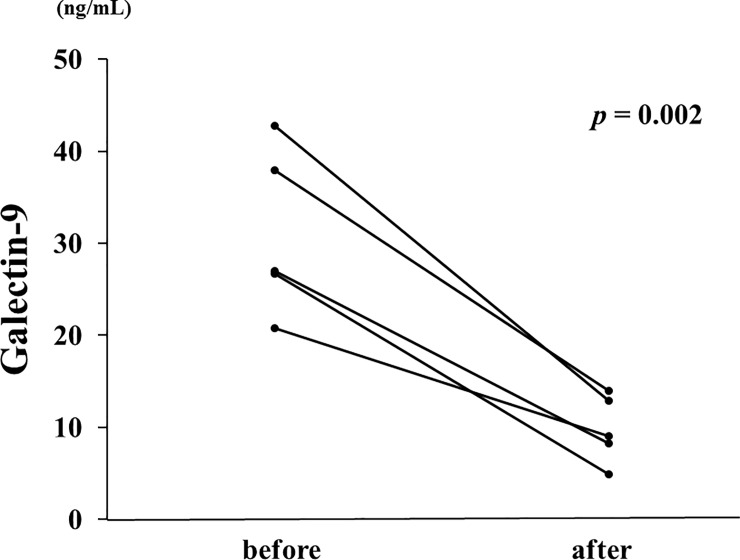
Longitudinal changes in Gal-9 serum concentrations
To explore the longitudinal changes in Gal-9 and associations with disease activity, we included 5 patients with two longitudinal samples (at least 1 month apart) and with high disease activity. In the longitudinal study, 5 active SLE patients were followed until they became inactive and then resampled (SLEDAI-2K before 23.4± 7.6, after 6.0 ± 5.1). The median duration of follow-up was 2 months (1–12 months). The levels of serum Gal-9 decreased significantly after treatment with glucocorticoids and immunosuppressive drugs (Fig 8). Therefore, serum Gal-9 levels in patients with active SLE were diminished following successful treatment with clinical improvement.
Fig 8. Longitudinal changes in serum Gal-9 concentrations in 5 patients with active SLE before and after immunosuppressive treatments.
Paired samples from the same subjects were compared by Wilcoxon signed-rank test. Gal-9 = galetin-9.
Neuropsychiatric manifestations and CSF levels of Gal-9
Although there was no differences in serum levels of Gal-9 between SLE patients with and without active neurological involvement (BILAG neurological A-B), we determined whether Gal-9 in CSF could be influenced by the presence of NPSLE. To test this hypothesis, we assayed the Gal-9 levels in CSF isolated from 18 patients with NPSLE. As shown in Fig 9, levels of Gal-9 in CSF samples from patients with neuropsychiatric involvement (NPSLE) were significantly higher (6.7 ±7 .4 ng/ml, media [IQR: 1.0–27.2]), p = 0.0093) compared to non-SLE controls (1.3 ± 0.4 ng/ml, media [IQR: 0.9–2.1]).
Fig 9. Levels of Galectin-9 (Gal-9) in cerebrospinal fluid (CSF).
Samples of CSF were obtained from patients with neuropsychiatric systemic lupus erythematosus (NPSLE, n = 18) and non-SLE controls (n = 6). Each point represents an individual patient. Median Gal-9 levels (bar) are depicted and statistical analysis was performed using the Mann-Whitney U test.
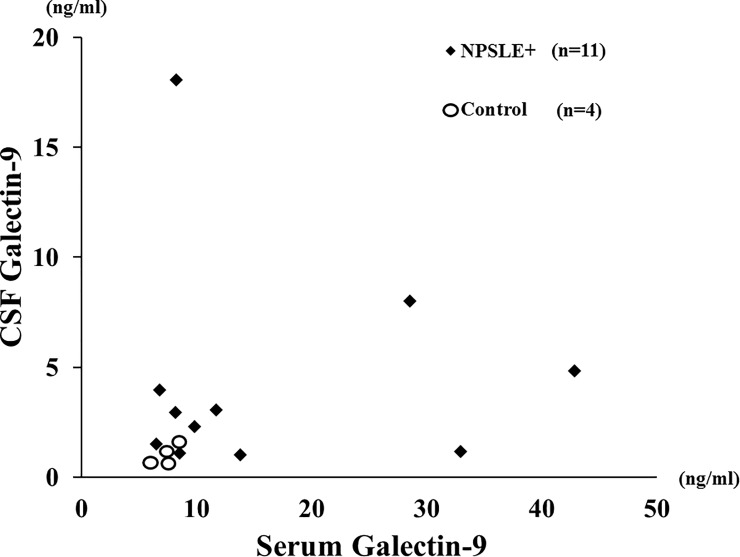
Although the paired samples (CSF plus serum) were available in a limited number of subjects, we compared CSF Gal-9 with serum Gal-9 levels in patients with NPSLE (n = 11) or controls (n = 4). The relationships between CSF Gal-9 and serum Gal-9 were shown in Fig 10. It is likely that CSF Gal-9 levels seem to be elevated regardless of the values of serum Gal-9 levels in a subset of NPSLE patients.
Fig 10. Relationship between cerebrospinal fluid (CSF) Gal-9 and serum Gal-9 in NPSLE patients and controls.
Relationship between cerebrospinal fluid (CSF) Gal-9 and serum Gal-9 were evaluated in patients with NPSLE and non-SLE controls. NPSLE: neuropsychiatric systemic lupus erythematosus.
Discussion
SLE is an autoimmune disease characterized by systemic vasculitis and inflammation of connective tissues leading to multiple organ damage [3]. Many studies have been performed to identify reliable biomarkers for SLE including non-invasive and easily measurable surrogates which are able to assess disease activity or treatment response [22]. Several cytokines, particularly type I IFNs, are implicated in the pathogenesis of SLE [4]. Despite an important role of type 1 IFNs, the direct quantification of type 1 IFNs has been challenging. We focused on Galectin-9, which was shown to be a potential biomarker for the interferon signature [7], with regard to SLE disease activity. The major finding in this study is that circulating levels of Gal-9 are elevated in patients with SLE and are correlated with SLE disease activity and could be a discriminator between SLE patients with and without organ damage distinguished by SLCC damage score. Our results suggest that Gal-9 could be a predictor for SLE disease phenotype and deserves attention as a clinically useful biomarker.
Tim-3 has been implicated in the pathogenesis of autoimmune diseases [23]. Gal-9 is one of the β-galactosidase binding lectins that suppresses Th1 cell or Th17 cells in a Tim-3-dependent or independent manner [24]. SLE patients had been demonstrated to contain high proportions of CD3+CD4+Tim-3+ T cell subsets compared with healthy subjects and Tim-3 expression on T cells correlates with SLE disease activity [25]. Galectin-9 is ubiquitously expressed in a variety of tissues, whereas, Galectin-9 expressed mainly in the immune system [26]. Galectin-9 expression is induced by IFN-γ suggesting a feedback mechanism whereby the IFN-γ induces tissue inflammation also induces an inhibitory ligand, Galectin-9 [27], which suppresses the differentiation of Th1/Th17 cells in Tim-3-dependent manner [28]. These close associations between Tim-3 expression and SLE disease activity could be linked with elevated levels of circulating Gal-9, a specific ligand of Tim-3. Our findings suggest that the circulating levels of Gal-9 may be useful to evaluate the SLE disease activity and highlight Gal-9 as a potential biomarker for SLE.
In this study we also demonstrated that Gal-9 is elevated in CSF isolated from patients with NPSLE. NPSLE involving the central nervous system is a life-treating manifestation of SLE [29]. Although the pathophysiology of NPSLE is not completely determined, research into the underlying mechanisms has focused on autoantibodies or cytokines [30]. It has been reported that certain autoantibodies or cytokines are relevant to NPSLE [31]. CSF studies have been instrumental in evaluating immunobiomarkers related to the immune dysfunction in NPSLE [32]. NPSLE is often associated with the presence of neuropathic cytokines such as IL-6 and IFN-α in CSF [33]. Additionally, the passage of autoantibodies across the blood-brain barrier (BBB) had been suggested in NPSLE [34]. To our knowledge, CSF levels of Gal-9 in NPSLE had never been described and no study has shown involvement of Gal-9 in NPSLE. The present study showed that elevated levels of Gal-9 in CSF were observed in patients with NPSLE and is the first to show the clinical significance of CSF Gal-9. These findings suggest that Gal-9 might also play a pathogenic role in NPSLE.
Our study demonstrated that Gal-9 levels are correlated with serum levels of CXCL-10 or M2BPGi. Furthermore, M2BPGi is correlated with SLE disease activity. We suggest that M2BPGi could be used in clinics as a noninvasive and useful biomarkers for SLE activity as described previously [14]. Serum Gal-9 levels were significantly higher in patients with SLE-related organ involvement than in SLE patients without organ involvement. Conversely, there was no significant difference in circulating CXCL10 and M2BPGi between SLE patients with and without organ damage. These findings suggest that only Gal-9 could be useful biomarker that reflects SLE organ involvements among these biomarkers. Analysis using longitudinal samples from active SLE patients also demonstrated that serum levels of Gal-9 are useful to assess the therapeutic changes of SLE disease activity. It has been generally accepted that high disease activity increase the risk of subsequent organ damage in SLE [35]. Indeed, the link between SLE disease activity and organ damage has been demonstrated in recent studies. Lopez et al demonstrated that SLE disease activity measured by BILAG score predicts the risk of subsequent organ damage and mortality [36]. Although serum levels of Gal-9 were demonstrated to be a promising marker to assess the IFN signature, our data suggest that Gal-9 could be a biomarker for SLE disease activity or particular SLE-related organ involvement. Elevated levels of Gal-9 were demonstrated in patients with primary Sjögren's syndrome, and to be correlated with disease activity assessed by EULAR Sjögren's syndrome Disease Activity Index (ESSDAI) [37]. Additionally, Gal-9 was validated as reliable biomarker for disease activity in juvenile dermatomyositis (DM) [38]. In accordance with these reports, our data suggest that Gal-9 could be a biomarker that reflects the particular SLE-related organ involvement in addition to SLE disease activity.
This study has some limitations. First, the sample size is relatively small and the design is cross-sectional. Second the CSF samples were not obtained from SLE patients without NPSLE. Third, the methods for identifying type I IFN signatures such as the global gene expression analysis were not performed in this study. Finally, our sample is mainly composed of patients with recent-onset SLE, we recognize that this aspect might have impact on the organ damage due to the short follow-up periods in contrast to other cohorts with different characteristics. A more detailed association of Gal-9 with lupus-related organ damage should be elucidated in a large-scale study.
Conclusions
In conclusion, our study demonstrates that serum Gal-9 has clinical association in SLE, in particular highlighting the associations between Gal-9 and SLE disease activity and organ involvement. These data suggest that Gal-9 may be linked with SLE-mediated organ involvements. Further research is required to elucidate the importance of Gal-9 in SLE, including NPSLE to determine how Gal-9 might be modulated by SLE phenotype.
Acknowledgments
We are grateful to Ms Kanno Sayaka for her technical assistance in this study.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The study was supported by the Practical Research Project for Rare / Intractable Diseases from Japan Agency for Medical Research and Development, AMED.
References
- 1.Zharkova O, Celhar T, Cravens PD, Satterthwaite AB, Fairhurst AM, Davis LS. Pathways leading to an immunological disease: systemic lupus erythematosus. Rheumatology. 2017;56(suppl_1):i55–i66. 10.1093/rheumatology/kew427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Griffiths B, Mosca M, Gordon C. Assessment of patients with systemic lupus erythematosus and the use of lupus disease activity indices. Best Pract Res Clin Rheumatol. 2005;19(5):685–708. 10.1016/j.berh.2005.03.010 [DOI] [PubMed] [Google Scholar]
- 3.Crow MK. Advances in understanding the role of type I interferons in systemic lupus erythematosus. Curr Opin Rheumatol. 2014;26(5):467–74. 10.1097/BOR.0000000000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elkon KB, Wiedeman A. Type I IFN system in the development and manifestations of SLE. Curr Opin Rheumatol. 2012;24(5):499–505. 10.1097/BOR.0b013e3283562c3e [DOI] [PubMed] [Google Scholar]
- 5.Bauer JW, Petri M, Batliwalla FM, et al. Interferon-regulated chemokines as biomarkers of systemic lupus erythematosus disease activity: a validation study. Arthritis Rheum. 2009;60(10):3098–107. 10.1002/art.24803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagberg N, Rönnblom L. Systemic Lupus Erythematosus—A Disease with A Dysregulated Type I Interferon System. Scand J Immunol. 2015;82(3):199–207. 10.1111/sji.12330 [DOI] [PubMed] [Google Scholar]
- 7.van den Hoogen LL, van Roon JAG, Mertens JS, et al. Galectin-9 is an easy to measure biomarker for the interferon signature in systemic lupus erythematosus and antiphospholipid syndrome. Ann Rheum Dis. 2018;77(12):1810–1814. 10.1136/annrheumdis-2018-213497 [DOI] [PubMed] [Google Scholar]
- 8.Bianco GA, Toscano MA, Ilarregui JM, Rabinovich GA. Impact of protein-glycan interactions in the regulation of autoimmunity and chronic inflammation. Autoimmun Rev. 2006;5(5):349–56. 10.1016/j.autrev.2006.02.003 [DOI] [PubMed] [Google Scholar]
- 9.Zhu C, Anderson AC, Kuchroo VK. TIM-3 and its regulatory role in immune responses. Curr Top Microbiol Immunol. 2011;350:1–15 10.1007/82_2010_84 [DOI] [PubMed] [Google Scholar]
- 10.Rodriguez-Manzanet R, DeKruyff R, Kuchroo VK, Umetsu DT. The costimulatory role of TIM molecules. Immunol Rev. 2009;229(1):259–70. 10.1111/j.1600-065X.2009.00772.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bengtsson A, Nezlin R, Shoenfeld Y, Sturfelt G. DNA levels in circulating immune complexes decrease at severe SLE flares-correlation with complement component C1q. J Autoimmun. 1999;13(1):111–9. 10.1006/jaut.1999.0300 [DOI] [PubMed] [Google Scholar]
- 12.Wu H, Zeng J, Yin J, Peng Q, Zhao M, Lu Q. Organ-specific biomarkers in lupus. Autoimmun Rev. 2017;16(4):391–397. 10.1016/j.autrev.2017.02.011 [DOI] [PubMed] [Google Scholar]
- 13.Nishikawa H, Enomoto H, Iwata Y, Hasegawa K, Nakano C, Takata R, et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level and high-sensitivity C-reactive protein concentration in autoimmune hepatitis. Hepatol Res. 2016;46:613–21. 10.1111/hepr.12596 [DOI] [PubMed] [Google Scholar]
- 14.Ahn SS, Park Y, Lee DD, Bothwell ALM, Jung SM, Song JJ, et al. Serum Wisteria floribunda agglutinin-positive Mac-2-binding protein can reflect systemic lupus erythematosus activity. Lupus. 2018;27(5):771–779. 10.1177/0961203317747719 [DOI] [PubMed] [Google Scholar]
- 15.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40(9):1725. [DOI] [PubMed] [Google Scholar]
- 16.Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29(2):288–91. [PubMed] [Google Scholar]
- 17.Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39(3):363–9. 10.1002/art.1780390303 [DOI] [PubMed] [Google Scholar]
- 18.Stoll T, Stucki G, Malik J, Pyke S, Isenberg DA. Further validation of the BILAG disease activity index in patients with systemic lupus erythematosus. Ann Rheum Dis. 1996. 55(10):756–60. 10.1136/ard.55.10.756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ACR Ad Hoc Committee on Neuropsychiatric Lupus Nomenclature. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999;42(4):599–608. [DOI] [PubMed] [Google Scholar]
- 20.Hanly JG. Diagnosis and management of neuropsychiatric SLE. Nat Rev Rheumatol. 2014;10(6):338–47. 10.1038/nrrheum.2014.15 [DOI] [PubMed] [Google Scholar]
- 21.Yamasaki K, Tateyama M, Abiru S, Komori A, Nagaoka S, Saeki A et al. Elevated serum levels of Wisteria floribunda agglutinin-positive human Mac-2 binding protein predict the development of hepatocellular carcinoma in hepatitis C patients. Hepatology. 2014;60(5):1563–1570. 10.1002/hep.27305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Merrill JT, Buyon JP. The role of biomarkers in the assessment of lupus. Best Pract Res Clin Rheumatol. 2005;19(5):709–26. 10.1016/j.berh.2005.05.004 [DOI] [PubMed] [Google Scholar]
- 23.Anderson AC, Anderson DE. TIM-3 in autoimmunity. Curr Opin Immunol. 2006;18(6):665–9. 10.1016/j.coi.2006.09.009 [DOI] [PubMed] [Google Scholar]
- 24.Zhu C, Anderson AC, Kuchroo VK. TIM-3 and its regulatory role in immune responses. Curr Top Microbiol Immunol. 2011;350:1–15. 10.1007/82_2010_84 [DOI] [PubMed] [Google Scholar]
- 25.Jiao Q, Qian Q, Zhao Z, Fang F, Hu X, An J, et al. Expression of human T cell immunoglobulin domain and mucin-3 (TIM-3) and TIM-3 ligands in peripheral blood from patients with systemic lupus erythematosus. Arch Dermatol Res. 2016;308(8):553–61. 10.1007/s00403-016-1665-4 [DOI] [PubMed] [Google Scholar]
- 26.Wada J, Kanwar YS. Identification and characterization of galectin-9, a novel beta-galactoside-binding mammalian lectin. J Biol Chem. 1997;272(9):6078–86. 10.1074/jbc.272.9.6078 [DOI] [PubMed] [Google Scholar]
- 27.Imaizumi T, Kumagai M, Sasaki N, Kurotaki H, Mori F, Seki M, et al. Interferon-gamma stimulates the expression of galectin-9 in cultured human endothelial cells. J Leukoc Biol. 2002;72(3):486–91. [PubMed] [Google Scholar]
- 28.Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, et al. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat Immunol. 2005;6(12):1245–52. 10.1038/ni1271 [DOI] [PubMed] [Google Scholar]
- 29.Hanly JG, Kozora E, Beyea SD, Birnbaum J. Review: Nervous System Disease in Systemic Lupus Erythematosus: Current Status and Future Directions. Arthritis Rheumatol. 2019;71(1):33–42. 10.1002/art.40591 [DOI] [PubMed] [Google Scholar]
- 30.Schwartz N, Stock AD, Putterman C. Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol. 2019;15(3):137–152. 10.1038/s41584-018-0156-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jeltsch-David H, Muller S. Neuropsychiatric systemic lupus erythematosus: pathogenesis and biomarkers. Nat Rev Neurol. 2014;10(10):579–96. 10.1038/nrneurol.2014.148 [DOI] [PubMed] [Google Scholar]
- 32.Fragoso-Loyo H, Atisha-Fregoso Y, Llorente L, Sánchez-Guerrero J. Inflammatory profile in cerebrospinal fluid of patients with headache as a manifestation of neuropsychiatric systemic lupus erythematosus. Rheumatology. 2013;52(12):2218–22. 10.1093/rheumatology/ket294 [DOI] [PubMed] [Google Scholar]
- 33.Fragoso-Loyo H, Richaud-Patin Y, Orozco-Narváez A, Dávila-Maldonado L, Atisha-Fregoso Y, Llorente L, et al. Interleukin-6 and chemokines in the neuropsychiatric manifestations of systemic lupus erythematosus. Arthritis Rheum. 2007;56(4):1242–50. 10.1002/art.22451 [DOI] [PubMed] [Google Scholar]
- 34.Duarte-Delgado NP, Vásquez G, Ortiz-Reyes BL. Blood-brain barrier disruption and neuroinflammation as pathophysiological mechanisms of the diffuse manifestations of neuropsychiatric systemic lupus erythematosus. Autoimmun Rev. 2019;18(4):426–432. 10.1016/j.autrev.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 35.Stoll T, Sutcliffe N, Mach J, Klaghofer R, Isenberg DA. Analysis of the relationship between disease activity and damage in patients with systemic lupus erythematosus—a 5-yr prospective study. Rheumatology. 2004;43(8):1039–44. 10.1093/rheumatology/keh238 [DOI] [PubMed] [Google Scholar]
- 36.Lopez R, Davidson JE, Beeby MD, Egger PJ, Isenberg DA. Lupus disease activity and the risk of subsequent organ damage and mortality in a large lupus cohort. Rheumatology. 2012;51(3):491–8. 10.1093/rheumatology/ker368 [DOI] [PubMed] [Google Scholar]
- 37.van den Hoogen LL, van der Heijden EHM, Hillen MR, Mertens JS, Fritsch-Stork RDE, Radstake TRDJ, et al. Galectin-9 reflects the interferon signature and correlates with disease activity in systemic autoimmune diseases. Ann Rheum Dis. 2018. December 8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Wienke J, Bellutti Enders F, Lim J, Mertens JS, van den Hoogen LL, et al. Galectin-9 and CXCL10 as Biomarkers for Disease Activity in Juvenile Dermatomyositis: A Longitudinal Cohort Study and Multicohort Validation. Arthritis Rheumatol. 2019;71(8):1377–1390. 10.1002/art.40881 [DOI] [PMC free article] [PubMed] [Google Scholar]