Abstract
Objective
Postoperative pain relief for total knee arthroplasty is an important concern for clinicians who seek to decrease pain, side effects associated with narcotics, increase mobility, and decrease hospital length of stay for total knee arthroplasty (TKA) patients. In today's day in age where patients and clinicians are looking to decrease length of stay and desire to take total knee replacement to the ambulatory surgery setting, appropriate and safe analgesia is paramount. The purpose of this study was to evaluate the analgesic efficacy of implementing a single shot adductor canal block (ACB) protocol in patients undergoing primary TKA by a single surgeon already using a multimodal analgesia protocol at a high volume community hospital.
Methods
75 patients who received a single shot ACB were compared to 75 patients that did not receive an ACB with respect to post-operative NRS pain scores and narcotic consumption.
Results
After addition of an ACB there was a 90% reduction in NRS pain scores in the PACU and a 38% reduction at 12 and 24-h post-operatively which were all statistically significant. Total post-operative morphine milligram equivalent (MME) decreased by 51%, after addition of an ACB, which was also statistically significant.
Conclusion
The administration of an ACB as an adjunct to a multimodal pain protocol for primary TKA patients is effective at minimizing post-operative pain and narcotic consumption, and plays a critical role in facilitating fast track and same day discharge in our practice.
Keywords: Total knee replacement, Adductor canal block, Rapid recovery, Multimodal pain control
1. Introduction
Osteoarthritis is estimated to affect one in four adults by 2040, and the predicted amount of total knee arthroplasty surgeries is set to increase to >3 million by 2030.1 Historically, post-operative pain relief following total knee arthroplasty is a challenge for the patient, surgeon, and the anesthesia provider and remains a contemporary concern.2 Optimal pain management is a national focus for the Joint Commission. The amount of postoperative pain following a TKA is the main determinant of early rehabilitation and recovery.3 Sub-optimal levels of postoperative pain are associated with an increased length of stay, decreased patient satisfaction, and decreased mobility.4
Health care institutions are focusing their attention on fast-track discharge programs to decrease patients’ length of stay, decrease cost, and improve patient outcomes and satisfaction.5 These multimodal protocols incorporate the use of improved surgical techniques, intraoperative anesthetic infiltration, as well as nerve blocks and a multimodal pharmacological approach to address pain post-operatively.6,7 These approaches have gained popularity recently in order to transition TKA to the ambulatory setting to improve patient satisfaction and outcomes. With the current opioid epidemic occurring in the United States, these practices also aim to decrease the amount of narcotic consumption post-operatively and have the potential to decrease subsequent issues with narcotic abuse.
Multiple studies have shown the administration of an adductor canal block (ACB) can assist in postoperative pain management and early ambulation.3,8, 9, 10, 11 The adductor canal block is a sensory block that spares motor fibers; as the saphenous nerve and part of the obturator nerve are blocked with local anesthetic as they travel through the adductor canal of the thigh.12 Koh et al. reported that the ACB provides comparable analgesia but facilitates earlier ambulation than the femoral nerve block, supporting the use of the ACB in a total joint protocol.13 Recent randomized controlled trails have called ACBs into question showing ACBs to be less effective for pain when given alone and equivocal when used in combination with peri-articular injection (PAI) compared to PAI alone.14 Ma et al. in their meta-analysis showed similar findings in regard to pain but had greater walking distances with ACB + PAI group.15 The purpose of our study was to determine if the addition of an ACB in conjunction with spinal anesthesia, a peri-articular infiltration, and a post-operative multimodal analgesia protocol would produce an improvement in post-operative pain and narcotic consumption. We hypothesize that implementing an ACB in this setting would decrease post-operative pain and narcotic consumption.
2. Methods and materials
The study group consisted of patients with symptomatic knee osteoarthritis presenting for definitive treatment with elective total knee arthroplasty. IRB approval was obtained and a total of 150 subjects between 2016 and 2017 from a single institution were enrolled in the study. A retrospective review of 75 gender-matched controls were randomly selected from the time period immediately prior to ACB protocol initiation. After initiation of the ACB protocol, a 3-month gap in time was provided as a learning period for the anesthesia team in administering the adductor canal block under ultrasound guidance. After this learning curve period, all patients at our institution received a single shot ACB.
The first 75 consecutive patients receiving an ACB were included in the treatment group. Inclusion criteria were male or female patients, patient age of 40–80, ASA Class II-III, and spinal anesthesia for the TKA procedure. Exclusion criteria included total knee arthroplasty revision surgery, prior knee surgery, ASA class > III, contraindication to spinal or regional anesthesia, and narcotic allergies specifically to tramadol, morphine, dilaudid, or roxicodone.
All TKAs were performed by a single, high volume, arthroplasty fellowship trained surgeon via mid-vastus approach. Prior to the start of the procedure in the pre-operative area, patients received celecoxib 200 mg oral, oxycodone 10 mg oral, and acetaminophen 1000 mg oral. All patients in the study received spinal anesthesia consisting of 1.8 mL 0.75% hyperbaric bupivacaine via 25 g spinal needle. A single shot ACB of 20 mL 0.5% ropivacaine via 21 g, 4-inch needle was administered to those in the ACB group pre-operatively. During the procedure and prior to closure, a peri-articular pain cocktail was administered consisting of 30 mL 0.5% bupivacaine, toradol 60 mg, and 20 mL 0.9% normal saline. Following the procedure, a post-operative multimodal pain protocol was utilized; patients were ordered standing doses of acetaminophen 500 mg every 6 h and toradol either 30 mg or 15 mg every 6 h for 3 doses or held depending on renal function. Patients had roxicodone 5 mg oral every 4 h, tramadol 50 mg oral every 4 h, and dilaudid 0.5 mg intravenous for breakthrough pain ordered on an as needed basis. All patients received a physical therapy session with a licensed physical therapist day of surgery and twice daily each day they stayed inpatient post-operatively with the majority of patients discharged by the afternoon on post-operative day number 1, followed by 6 weeks of outpatient physical therapy 3 times per week.
A retrospective chart review of prospectively collected data utilizing the electronic health-care record (EHR) was performed for patients who met the inclusion criteria. Specific data collected from the chart consisted of pain scores and narcotic use at three different time intervals: immediately in the PACU, 12 h post-operatively, and 24 h post-operatively as well as demographic data including age, sex, and ASA classification. The NRS pain scale was utilized to evaluate pain and was collected at each time point by the nursing staff. The NRS is a numerical scale that has been proven to be valid and reliable in assessing pain using a 0–10 point system, 0 = no pain and 10 = the worst pain.16 Narcotic requirements were measured by converting the 24-h narcotic consumption into a standardized morphine milligram equivalent (MME).1 Microsoft Excel statistical functions were used to calculate demographic data means and standard deviations and to perform independent two-sample t-tests to compare mean pain scores at the three different time intervals as well as the 24-h mean narcotic consumption after it was converted into the morphine milligram equivalents. A p-value of <0.05 was considered statistically significant.
3. Results
Table 1 summarizes the demographic information for patients in the ACB and no ACB groups.
Table 1.
Descriptive data.
| ACB | No ACB | |
|---|---|---|
| N | 75 | 75 |
| Age, mean±SD | 67.6 ± 7.8 | 67.2 ± 7.5 |
| Age, N (%) | ||
| Age group 1: 40 < age ≤ 50 | 2 (2.7) | 2 (2.7) |
| Age group 2: 50 < age ≤ 60 | 14 (18.7) | 12 (16.0) |
| Age group 3: 60 < age ≤ 70 | 31 (41.3) | 34 (45.3) |
| Age group 4: 70 < age ≤ 80 | 28 (37.3) | 27 (36.0) |
| Sex, N (%) | ||
| Male | 38 (50.7) | 38 (50.7) |
| Female | 37 (49.3) | 37 (49.3) |
| ASA, N (%) | ||
| 1 | 0 (0.0) | 0 (0.0) |
| 2 | 10 (13.3) | 18 (24.0) |
| 3 | 65 (86.7) | 57 (76.0) |
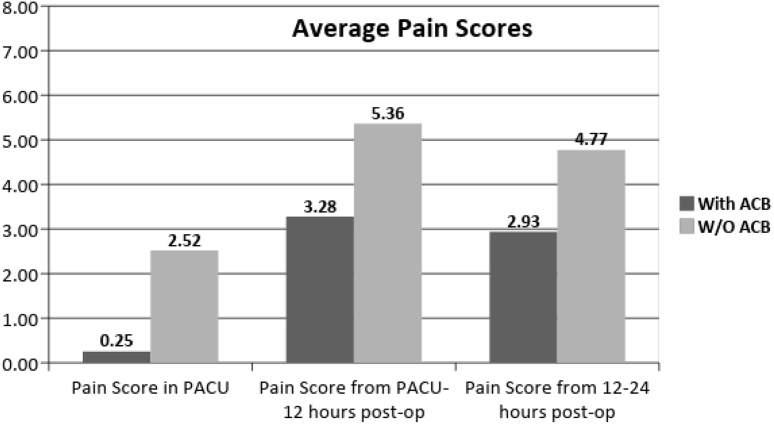
Mean pain scores measured and recorded at three different time intervals were determined and were compared between both groups. All three time intervals demonstrated significance in pain reduction between groups from 2.5 to 0.25 immediately in PACU (p = < 0.01), 5.36 to 3.28 at 12 h post-operatively (p = < 0.01), and 4.77 to 2.93 at 24-h post-operatively (p = < 0.01) (see Fig. 1).
Fig. 1.
Average pain scores.
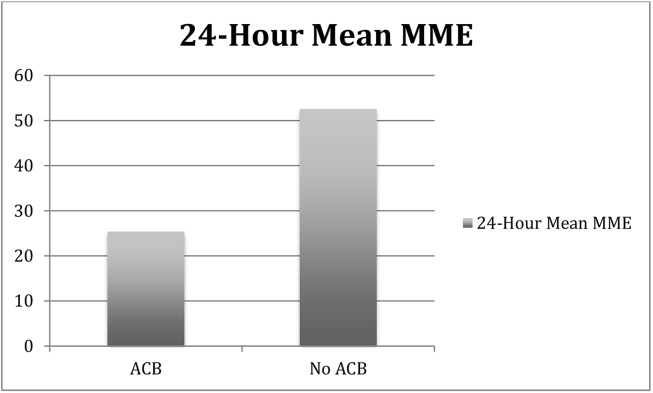
Narcotic requirements were extrapolated from the electronic chart mirroring the same time intervals. The mean 24-h MME was compared between the two groups (Fig. 2) and demonstrated a significant reduction of overall narcotic use from 52.56 mg to 25.39 mg (p = <0.01).
Fig. 2.
24-Hour mean MME
4. Discussion
This study demonstrates that ACB administration in addition to spinal anesthesia, a peri-articular infiltration, and a post-operative multimodal analgesia protocol can significantly decrease post-operative pain and minimize narcotic consumption for TKA patients. This is evidenced by a 90% reduction in pain scores in the PACU, a 38% reduction of the pain scores at 12 and 24-h post-operatively, and a 51% decrease in the MME in patients receiving an ACB versus those who did not.
There is a constant effort in the medical and orthopaedic community to reduce overall opioid consumption. The results of this study are consistent with other publications that the implementation of an ACB protocol in conjunction with multimodal pain control practices and peri-articular injection in TKA patients can significantly decrease post-operative pain throughout a 24-h period and minimize the narcotic requirement after surgery.2,4,8, 9, 10,17 This decrease in narcotic consumption has the potential to decrease narcotic abuse in this subset of patients. Jenstrup et al. noticed a similar decrease in morphine requirement of 40 ± 21 vs. 56 ± 26 mg (p = 0.006) with use of a ropivicaine ACB.9 However, our study differs in that of Grosso et al. in that we showed that even when using a peri-articular injection and a multimodal pharmacological protocol the inclusion of an ACB demonstrated a significant improvement in post-operative pain and narcotic requirements.18 Furthermore, the findings could be extrapolated to support the findings of other studies that ACB enhances recovery and helps to promote rapid discharge in TKA.19 This clinical practice can aid in minimizing post-operative pain, narcotic requirements and has potential implications in making same-day discharge TKA possible from a pain control perspective. In our practice same day discharge is becoming the norm, which was not possible prior to ACB protocol initiation due to inadequate pain control.
This study does carry the limitations inherent of a retrospective review. However, once the ACB protocol was initiated at our institution and the learning curve for the ACB by anesthesia was accounted for, all consecutive primary TKAs from that point on received an ACB and were included in the treatment group. In other words, a single surgeon performed all cases before and after addition of the ACB protocol and there were no changes in surgical technique or perioperative management other than the addition of the ACB. Although we recognize there was likely a learning curve within the anesthesia department to technically master the block under ultrasound, we adjusted for this limitation by allowing a 3-month learning curve period before patients were enrolled in the treatment arm of the study. Moreover, issues with the learning curve of administering the block, if anything, would reduce the magnitude of effect we noted in decreasing narcotic consumption and pain scores. Future areas of research include effect of ACB on early discharge and its effect on patient outcomes, function, and satisfaction.
5. Conclusion
Efforts aimed to decrease pain and overall opioid requirements will enhance fast track discharging of patients and act as a valuable tool when transitioning to ambulatory TKA. The compelling findings of this study demonstrate the effectiveness of addition of an adductor canal block and its ability to decrease post-operative pain scores and limit narcotic requirements following a TKA in patients receiving a peri-articular injection and a multimodal pain protocol.
Conflicts of interest
One author is a paid consultant for Stryker. One author is a paid consultant for Ethicon, Ortho Development and Depuy Synthes. One author is a paid consultant for Stryker and Smith & Nephew.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Jessica Deiter, Email: jessicajane1@comcast.net.
Danielle Ponzio, Email: Danielle.ponzio@rothmanortho.com.
Luis Grau, Email: luiscgrau@gmail.com.
Sean Griffiths, Email: griffithss@ihn.org.
Alvin Ong, Email: Alvin.ong@rothmanortho.com.
Zachary Post, Email: Zachary.post@rothmanortho.com.
David Doucette, Email: david.j.doucette@wilmu.edu.
Fabio Orozco, Email: Fabio.orozco@rothmanortho.com.
References
- 1.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion . 2016. Improving the Quality of Life for People with Arthritis: At a Glance.https://www.cdc.gov/chronicdisease/resources/publications/aag/arthritis.htm/ [Google Scholar]
- 2.Yuan S., Hanson N.A., Salinas F.V. Adductor canal block for total knee arthroplasty: a review of the current evidence. J Anesth Surg. 2016;3(6):1–9. https://doi:10.15436/2377-1364.16.053 [Google Scholar]
- 3.Rasouli M.R., Viscusi E.R. Adductor canal block for knee surgeries: an emerging analgesic technique. Arch Bone Jt Surg. 2017;5:131–132. [PMC free article] [PubMed] [Google Scholar]
- 4.Lamplot J., Wagner E., Manning D. Multimodal pain management in total knee arthroplasty: a prospective randomized controlled trial. J Arthroplast. 2014;29:329–334. doi: 10.1016/j.arth.2013.06.005. https://doi:10.1016/j.arth.2013.06.005 [DOI] [PubMed] [Google Scholar]
- 5.Prabhakar A., Cefalu J.N., Rowe J.S., Kaye A.D., Urman R.D. Techniques to optimize multimodal analgesia in ambulatory surgery. Curr Pain Headache Rep. 2017;21(5):24. doi: 10.1007/s11916-017-0622-z. https://doi:10.1007s/11916-017-0622-z [DOI] [PubMed] [Google Scholar]
- 6.Cullom C., Weed J.T. Anesthetic and analgesic management for outpatient knee arthroplasty. Curr Pain Headache Rep. 2017;21(5) doi: 10.1007/s11916-017-0623-y. https://doi:10.1007/s11916-017-0623-y [DOI] [PubMed] [Google Scholar]
- 7.Zhou M., Ding H., Ke J. Adductor canal block in combination with posterior capsular infiltration on the pain control after TKA. Ir J Med Sci. 2016;187:465–471. doi: 10.1007/s11845-017-1647-3. https://doi:10.1007/s11845-017-1647-3 [DOI] [PubMed] [Google Scholar]
- 8.Hanson N., Allen C., Hostetter L. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg. 2014;118:1370–1377. doi: 10.1213/ANE.0000000000000197. https://doi:10.1213/ANE.0000000000000197 [DOI] [PubMed] [Google Scholar]
- 9.Jenstrup M.T., Jæger P., Lund J. Effects of adductor-canal-block on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesilogica Scand. 2012;56:357–364. doi: 10.1111/j.1399-6576.2011.02621.x. https://doi:10.1111/j.1399-6576.2011.02621.x [DOI] [PubMed] [Google Scholar]
- 10.Nader A., Kendall M.C., Manning D.W. Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized double-blind placebo-controlled trial. Reg Anesth Pain Med. 2016;41:678–684. doi: 10.1097/AAP.0000000000000494. https://doi:10.1097/AAP.0000000000000494 [DOI] [PubMed] [Google Scholar]
- 11.Sawhney M., Mehdian H., Kasin B. Pain after unilateral total knee arthroplasty: a prospective randomized control trial examining the analgesic effectiveness of a combined adductor canal peripheral nerve block with periarticular infiltration versus adductor canal nerve bock alone, versus periarticular infiltration alone. Anesth Analg. 2016;122:2040–2046. doi: 10.1213/ANE.0000000000001210. https://doi:10.1213/ANE.0000000000001210 [DOI] [PubMed] [Google Scholar]
- 12.Sankineani S., Reddy A., Kumar K., Eachmapti K., Reddy A. Comparative analysis of influence of adductor canal block and multimodal periarticular infiltration versus adductor canal block alone on pain and knee range of movement after total knee arthroplasty: a prospective non-randomized study. Musculoskel Surg. 2017;102:173–177. doi: 10.1007/s12306-017-0519-3. https://doi:10.1007/s12306-017-0519-3 [DOI] [PubMed] [Google Scholar]
- 13.Koh I.J., Choi Y.J., Kim M.S., Koh H.J., Kang M.S., In Y. Femoral nerve block versus adductor canal nerve block for analgesia after total knee arthroplasty. Knee Surg Relat Res. 2016;29:87–95. doi: 10.5792/ksrr.16.039. https://doi:10.5792/ksrr.16.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grosu I., Lavand’homme P., Thienpont E. Pain after knee arthroplasty: an unresolved issue. Knee Surg Sport Traumatol Arthrosc. 2013;22:1744–1758. doi: 10.1007/s00167-013-2750-2. https://doi:10.1007/s00167-013-2750-2 [DOI] [PubMed] [Google Scholar]
- 15.Ma J., Gao F., Sun W., Guo W., Li Z., Wang W. Combined adductor canal block with periarticular infiltration versus periarticular infiltration for analgesia after total knee arthroplasty. Medicine. 2016;95(52):1–8. doi: 10.1097/MD.0000000000005701. https://doi:10.1097/MD0000000000005701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skovlund E., Breivik H. Analysis of pain-intensity measurements. Scand J Pain. 2016;13:123–124. doi: 10.1016/j.sjpain.2016.08.005. https://doi:10.1016/j.sjpain0.2016.08.005 [DOI] [PubMed] [Google Scholar]
- 17.Grevstad U., Mathiesen O., Valentiner L.S., Jaeger P., Hilsted L.K., Dahl J.B. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesth Pain Med. 2017;40(1):3–10. doi: 10.1097/AAP.0000000000000169. https://doi:10.1097/AAP.0000000000000169 [DOI] [PubMed] [Google Scholar]
- 18.Grosso M.J., Murtaugh T., Lakra A. Adductor canal block compared with periarticular bupivacaine injection for total knee arthroplasty. J Bone Jt. Surg. 2018;100(13):1141–1146. doi: 10.2106/jbjs.17.01177. [DOI] [PubMed] [Google Scholar]
- 19.Soffin E., YaDeau J.T. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anesth. 2016;117(3):62–72. doi: 10.1093/bja/aew362. https://doi:10.1093/bja/aew362 [DOI] [PubMed] [Google Scholar]