Abstract
The number of total hip arthroplasty (THA) procedures performed annually continues to rise. Specific challenges, including acetabular bone loss, are commonly encountered at the time of revision surgery, and orthopaedic surgeons must be prepared to address them. This review focuses on topics related to acetabular reconstruction, including pre-operative patient evaluation (clinical and radiographic), pre-operative planning, common causes of acetabular failure, classification of acetabular bone loss, methods of acetabular reconstruction, and clinical results based on reconstruction method. Pre-operative patient evaluation for revision THA begins with a thorough history and physical examination as well as laboratory workup to rule out infection. Detailed radiographic evaluation and pre-operative planning are also essential and will facilitate communication amongst all members of the operative team. Although there are several ways to describe acetabular bone loss, the Paprosky classification system – defined by anterosuperior and posteroinferior acetabular column integrity – is the system most commonly used today and will guide treatment strategy. Several treatment strategies have been developed and may be termed either “cemented” (e.g. impaction grafting, ring and cage construction, structural allograft) or “uncemented” (e.g. hemispheric shell ± porous metal augment, cup-cage, custom triflange acetabular component). Although each strategy has its advantages and disadvantages, the general principles remain the same. Successful treatment depends upon detailed pre-operative assessment, planning, and team-based plan execution. Uncemented techniques that allow for biologic fixation are preferred. In the special case of pelvic discontinuity, acetabular distraction is the authors’ preferred technique. Longer term studies are still needed to evaluate the longevity of each of the various reconstruction methods presented.
Keywords: Revision hip arthroplasty, Hip replacement, Acetabular bone loss, Pelvic discontinuity
1. Introduction
The number of total hip arthroplasty (THA) procedures performed annually is projected to rise 71% by the year 2030,1 and thus the revision burden is also predicted to grow. Specific challenges are commonly encountered at the time of revision surgery, and orthopaedic surgeons must be prepared to address them. One common challenge is acetabular bone loss, particularly when bone loss results in compromise of acetabular column support. In addition to comprehensively evaluating the patient and formulating a detailed pre-operative plan, properly classifying acetabular bone loss will identify the appropriate acetabular reconstruction treatment method.
This review focuses on topics related to acetabular reconstruction, including pre-operative patient evaluation (clinical and radiographic), pre-operative planning, common causes of acetabular failure, classification of acetabular bone loss, methods of acetabular reconstruction, and clinical results based on reconstruction method.
2. Patient evaluation
Pre-operative patient evaluation for revision THA begins with a thorough history and physical examination. The temporal nature of clinical symptoms is important. Patients reporting the absence of pain relief following the index procedure must be investigated for extra-articular etiologies of hip pain (e.g. lumbar spine)2 as well as for chronic peri-prosthetic infection. Components of the physical examination include range of motion, motor strength, neurovascular assessment, presence or absence of a sinus tract, leg length discrepancy (actual and apparent), lumbosacral spine pathology, and Trendelenburg gait.
Pre-operative laboratory workup includes measurement of serum inflammatory markers – erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Elevated inflammatory markers warrant a hip aspiration. Synovial fluid cell count, differential and culture are essential; infection is suspected with positive cultures or a white blood cell count greater than 3000 with a segmented neutrophil differential greater than 80%.3
Detailed radiographic evaluation is also essential, including an anteroposterior (AP) x-ray of the pelvis (with pubic symphysis centered over coccyx).4 Several radiographic landmarks on the AP pelvis have been defined for assessing bone loss, including: Köhler’s line (medial wall), the superior obturator line (acetabular dome), osteolysis of the acetabular teardrop (anteroinferior and medial wall), and/or osteolysis of the ischium (posteroinferior column) (Fig. 1).
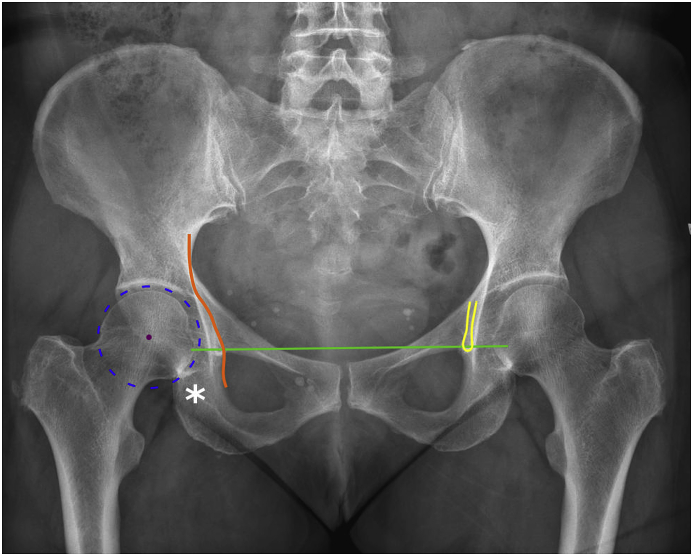
Fig. 1.
Anteroposterior X-ray of the pelvis demonstrating radiographic landmarks important for pre-operative evaluation. These include Köhler’s line (orange, left), the acetabular teardrop (yellow, right), the superior obturator line (green), and the ischium (asterisk).
Additional imaging should include AP, lateral, and cross-table views of the hip. Judet views further delineate anterior column (obturator oblique) and posterior column (iliac oblique) bone stock, and a computerized tomography (CT) will provide three-dimensional structural information. Intra-pelvic structures (e.g. pelvic vessels or ureter) are also at risk during acetabular revision, including either by inadvertent injury or by direct insult during removal of pre-existing implants.5,6 Contrast-enhanced CT can identify these at-risk structures pre-operatively and minimize iatrogenic injury.7
3. Pre-operative planning
Pre-operative planning ensures that all “thinking” has been done prior to surgery, so that plan execution is the main intra-operative focus. The pre-operative plan includes five essential elements: (1) what is the reason for acetabular failure/revision; (2) what implant(s) are currently in place; (3) what is the planned revision strategy; (4) what alternative strategies have been identified to address anticipated and unanticipated difficulties; and (5) what are the surgeon’s limitations?
Pre-operative planning is critical for less experienced revision surgeons. The plan facilitates communication amongst all members of the operative team. First, the surgeon must obtain operative reports to identify the current implants. Implant-specific tools may be needed for efficient implant removal. The remainder of the plan should focus on the revision strategy, having the necessary implants available, and developing plans “A”, “B” and “C” should unexpected issues arise.
4. Common causes and demographics of acetabular component failure
Despite the overall success of THA, there are several reasons why acetabular components may require revision. In a large database study of the national inpatient sample, Bozic et al. identified reasons for acetabular-only revision, including: instability (33.0%), mechanical loosening (24.2%), implant failure (10.8%), peri-prosthetic osteolysis (8.1%), bearing surface wear (8.0%), infection (4.7%), and peri-prosthetic fracture (1.8%).8 A single dislocation event usually is not an indication for revision; recurrent instability, however, more strongly suggests the presence of an underlying structural problem that cannot be solved without component repositioning.
All causes of acetabular failure may be further complicated by acetabular bone loss. Therefore, recognizing and being able to accurately describe the pattern of bone loss is a critical component of the pre-operative assessment that will help assist in selecting the most appropriate reconstruction strategy.
5. Classification of acetabular bone loss
Various classification systems have been developed to describe acetabular bone loss patterns and can be used to guide acetabular reconstruction.
One of the first classifications was proposed by the American Academy of Orthopaedic Surgeons (AAOS) Committee on the Hip in 1989.9 In this system, defects were described as either segmental (complete absence) or cavitary (volumetric loss) according to defect location (superior, anterior, posterior, medial wall). Segmental and peripheral defects can exist in combination, and pelvic discontinuity was defined as a “defect across the anterior and posterior columns with total separation of the superior from the inferior acetabulum.” A final category – termed “arthrodesis” – was characterized not by bone loss but by failure or difficulty in identifying the location of the true acetabulum.
In the early 1990’s, Paprosky et al. proposed an alternative method of acetabular defect classification based on a series of 147 patients undergoing acetabular component revision.10 The Paprosky classification system – defined on the basis of the anterosuperior and posteroinferior acetabular column integrity10 – is the system most commonly used today and has demonstrated acceptable validity.11 (Table 1).
Table 1.
Paprosky classification of acetabular bone loss.
| Type | Femoral head migration | Kohler’s line | Possible reconstruction strategy |
|---|---|---|---|
| 1 | None | Intact | Uncemented hemispheric shell |
| 2A | Superior (less than 3 cm) | Intact | Uncemented hemispheric shell |
| 2B | Superolateral (less than 3 cm) | Intact | Uncemented hemispheric shell |
| 2C | Medial | Disrupted | Uncemented hemispheric shell with medial bone grafting |
| 3A | “Up and out” (more than 3 cm) | Intact | Uncemented hemispheric shell with porous metal augment(s) or structural allograft |
| 3B | “Up and in” (more than 3 cm) | Disrupted | Uncemented shell with porous metal augment or structural allograft ± acetabular distraction; cup-cage reconstruction; or custom triflange |
The classification system can be simplified according to the following: type 1 defects have minimal bone loss; type 2 defects have supportive columns but a distorted acetabulum; and type 3 defects demonstrate significant bone loss and have inadequate column support. Key anatomic features include integrity of the superior acetabular dome, the extent of tear drop and ischial osteolysis, and violation of the medial wall (Fig. 2). In addition to providing a system for describing bone loss, the Paprosky classification also guides treatment strategy.
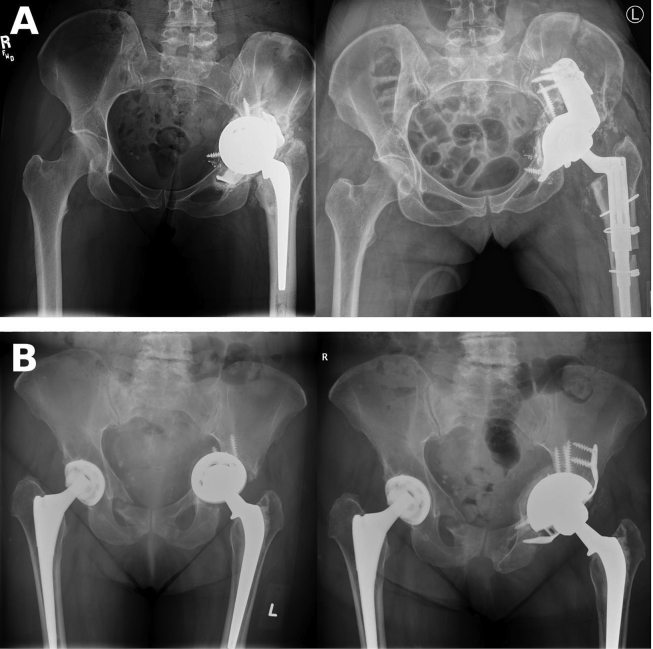
Fig. 2.
Pre-operative AP pelvis X-rays demonstrating Paprosky types 2A/2C, 3A, and 3B patterns of acetabular bone loss. A, anterosuperior migration (less than 3 cm) of the right hip is consistent with type 2A pattern, while concomitant medial migration and violation of Köhler’s line is also consistent with type 2C. B, Type 3A bone loss with “up and out” migration (greater than 3 cm) of the left hip following cup removal. C, type 3B bone loss with “up and in” migration and a possible chronic pelvic discontinuity.
Type 1 defects can be treated with a hemispherical acetabular shell with adjuvant screw fixation. Particulate bone graft often is not required, and more advanced techniques (e.g. porous metal augments, bulk allograft) are unnecessary.
Type 2 defects are further characterized by the direction of acetabular distortion. Type 2A defects demonstrate direct superior migration due to anterosuperior bone loss, whereas type 2B defects migrate superolaterally. Type 2C defects exhibit medial migration of the hip center and violate Köhler’s line. Type 2A and 2B defects can be revised with a hemispheric cup without additional allograft.12 2C defects are still amenable to treatment with a hemispheric cup but may require medial cancellous allograft to address the medial defect.12
Type 3 defects, by definition, exhibit insufficient anterosuperior and posteroinferior column support and require advanced reconstructive techniques. Type 3 defects are further sub-classified by the direction of bone loss and demonstrate more than 3 cm of superior hip migration with varying degrees of ischial and tear drop osteolysis. In type 3A defects, the hip center migrates in an “up and out” direction, while type 3B display an “up and in” migration. Type 3A defects have an intact medial wall, whereas type 3B defects violate Köhler’s line and have a higher association with a chronic pelvic discontinuity.
At the time of the original Paprosky classification description, structural allograft was commonly required for type 3 defects.10 Screw augmentation was also used to enhance cup fixation for type 3A and 3B defects. However, in addition to the structural allograft techniques mentioned above, a number of other reconstruction techniques have since been popularized and will be discussed in section 6.
6. Methods of acetabular reconstruction
Various cemented and uncemented methods of reconstruction are available for addressing acetabular bone loss. Each reconstructive method has its unique advantages and disadvantages which are delineated in the subsequent sections.
6.1. Impaction bone grafting & acetabular cementation
Impaction bone grafting and acetabular cementation has been described for treating segmental or combined acetabular defects. In this technique, the acetabulum is reamed to bleeding bone, and segmental defects are reconstructed using metal mesh or solid graft.13 Femoral head autograft or fresh-frozen allograft is morselized into <1 cm diameter cancellous pieces. The graft is impacted and bone cement is pressurized throughout the graft prior to implantation of an all-polyethylene cup.
Buttaro et al. reported on a cohort of 23 patients that underwent acetabular revision with metal mesh, impaction bone grafting, and a cemented cup and found 90.8% cup survival (using revision for any reason as an end-point) at an average follow-up of 36 months.14 Schreurs et al. reported on 62 acetabular revisions performed over a 7-year period from 1979 to 1986 with 96% cup survival (using aseptic loosening as an end-point) at 10 years and 84% survival at 15 year follow-up.15 In a subsequent study looking at 25-year follow-up that included only patients who had been younger than 50 years at time of revision surgery, cup survival decreased to 77%.13
Despite reasonable outcomes using cemented techniques, the authors do not recommend cemented reconstruction as first line treatment since these techniques are labor intensive and do not provide biologic fixation. Additionally, allograft reconstruction carries a risk of graft resorption and infection.
6.2. Ring and cage reconstruction
Rings and cages historically have been reserved for cases of acetabular revision with inadequate bone stock where a “bridge” is required to span the defect. Rings and cages are secured to the ilium and ischium with screws placed through small flanges, and a liner is then cemented into the appropriate version and abduction. Since the introduction of porous metal augments (see section 6.6) and custom triflange acetabular components (see section 6.8), the use of rings and cages has declined.
Rings and cages have shown favorable mid-term results. Zehntner and Ganz et al. studied 27 patients who underwent acetabular reconstruction using femoral head allograft with the Müeller acetabular reinforcement ring and reported 80% survivorship of the acetabular roof ring at 10 years.16 Similarly, Goodman et al. demonstrated 76% survivorship of Bursch-Schneider cages in 42 reconstructions with a mean follow-up of 4.6 years.17
Ring and cage reconstruction provides a relatively low cost method for bridging acetabular defects that cannot be achieved by a hemispheric cup alone. The major disadvantage of ring and cage reconstruction is the risk of subsequent implant failure, especially if used in “higher demand” patient populations. This technique also relies upon cementation rather than complete biologic fixation, which may compromise long-term component longevity.
6.3. Structural allograft with cement
In the case of significant acetabular bone loss or developmental hip dysplasia (where the superolateral acetabulum may be absent), reconstruction can be achieved using structural allograft alongside acetabular cementation. In this technique, allograft bone (e.g. femoral head) is shaped to fill the acetabular defect and fixed in place using cancellous screws, and the acetabular cup is cemented into place.
Sternheim et al. retrospectively studied 18 cemented acetabular cups and 27 uncemented acetabular cups with an average of 18-year follow-up.18 Ten and 20-year cup survival, respectively, was only 67% and 36% for cemented cups compared to 88% and 76% for uncemented cups, respectively. Therefore, structural allograft with cementation may be associated with greater loosening compared to use of structural allograft with a hemispheric implant alone and generally is not recommended by the authors given the availability of other more durable reconstruction methods.
6.4. Uncemented hemispheric acetabular reconstruction
Although the acetabular reconstruction techniques described in sections 1, 2, 3, 4, 5, 6 all involved cemented constructs, modern hip reconstruction commonly employs cementless, biologic fixation strategies. Cementless acetabular reconstruction with a hemispheric implant is the universally recommended treatment for Paprosky type 1 and 2 defects.12 Excellent mid-to long-term outcomes of uncemented hemispheric acetabular reconstruction have been shown in several studies, with reports of >90% survivorship when using aseptic loosening as an end-point.19, 20, 21, 22, 23 Della Valle et al. reported on 138 hips (131 patients) and demonstrated 96% cup survivorship at 15 years. Nineteen acetabular components required revision for recurrent instability, deep infection, or concomitant femoral component revision.
The main advantages of uncemented hemispheric acetabular reconstruction include a more familiar technique for surgeons and the potential for biologic fixation. However, uncemented hemispheric reconstruction techniques do require good pre-existing bone stock and at least 50% implant contact with host bone.
6.5. Uncemented structural allograft reconstruction
Hemispheric shells can also be used in the setting of inadequate column support with more extensive bone loss (e.g. Paprosky types 2 and 3) – in conjunction with bulk structural allograft – according to the severity of acetabular bone loss.10 Femoral head allograft (cut into a “Fig. 7” shape) was used in type 2B defects for reconstruction of the superolateral pillar. Distal femur and proximal tibia allograft (cut into a “Fig. 7” shape) may be needed for reconstruction of type 3A acetabular defects in which a larger graft with greater structural support is required.
For more severe type 3B defects, a proximal femoral allograft that has been transected in the coronal plane may be sufficient for restoring superomedial support. In their series of 147 acetabular revisions, Paprosky et al. reported a 4.0% rate of clinical and radiographic loosening (>3 mm).
Dewal et al. described a series of 13 patients who underwent revision THA with femoral head or distal femur structural allograft with an average follow-up of 6.8 years.24 That study reported acetabular loosening in 15% of patients. Lee et al. described a larger series of 85 hips that underwent acetabular revision utilizing minor column allografts for defects encompassing 30–50% of the acetabulum with a minimum follow-up of 5 years (mean 16 years).25 At 15- and 20-year follow-up, the authors reported cup survivorships of 67% and 61%, respectively, as well as graft survivorship of 81%.
Despite the favorable survivability of structural allografts in revision THA, porous metal augments have grown increasingly popular as an alternative reconstruction strategy for achieving biologic fixation and avoiding graft resorption over time. However, given that structural allografts may enhance future bone stock, younger patients (e.g. less than 40 years old) at greater risk of needing repeat revision surgery down the road may be better candidates for structural allograft rather than porous metal augments.26
6.6. Porous metal augments
Porous metal modular augments have revolutionized the treatment of severe acetabular bone loss over the past one and a half decades. Augments secured with screws and implanted prior to placement of the acetabular shell provide primary stability (e.g. anterosuperior, posteroinferior columns) for the overall acetabular construct and are more than just simple bone void “fillers.” Augments may also be placed posterosuperiorly following cup insertion (e.g. in the case of inadequate purchase of screws through the cup), thereby providing supplemental fixation. Augments should be thought of as extensions of the acetabular shell and are “unitized” to the cup using cement in order to minimize metal debris from micro-motion during the early post-operative period and extend the surface area of contact for the overall construct.
Mid-term reports of porous metal augments have shown excellent survivability. Sporer et al. reported on 18 acetabular revisions utilizing trabecular metal modular shell and trabecular metal augments and found 100% survivability (for acetabular loosening) with an average follow-up of 3.1 years.27 Similarly, Whitehouse et al. evaluated 53 acetabular revisions that used trabecular metal augments and found 92% survivability with a median follow-up of 9 years.28 Porous metal augments have so far performed well as useful adjuncts in the management of acetabular bone loss, but continued study is necessary to ensure long-term viability.
Porous metal augments have the advantage of allowing for intra-operative customization of the acetabular construct based on the bone loss defect. However, greater technical expertise and understanding of augment function is required for successful use of these devices for complex acetabular defects.
6.7. Cup-cage reconstruction
Cup-cage reconstruction has been recently popularized as a hybrid technique using a porous metal acetabular shell in conjunction with an acetabular cage (Fig. 3). This construct is reserved for treatment of severe type 3 acetabular defects with or without a chronic pelvic discontinuity. In this technique, a porous metal shell is implanted and secured with as many screws as possible; this may be supplemented by one or more modular porous metal augments.26 An acetabular cage is then implanted over the cup and spans the ilium and ischium. Screws are placed through the cage (and sequentially the cup, when possible) into host bone. Finally, a polyethylene liner is cemented into the acetabular cage. Bone wax is placed over all screw holes prior to cementation to facilitate subsequent implant removal. Cup-cage longevity requires successful biologic fixation by maximizing cup-host bone contact.
Fig. 3.
Pre- and postoperative AP pelvis X-rays showing examples of A, custom triflange acetabular component reconstruction and B, cup-cage reconstruction.
Outcomes after cup-cage reconstruction have been favorable with 80–90% survivability. In a study of 26 acetabular revisions with pelvic discontinuity that underwent cup-cage reconstruction, Kosashvilli et al. reported 88.5% without evidence of loosening and Harris hip scores that remained significantly improved at a mean follow-up of 3.7 years.29 Rogers et al. subsequently reported 86.3% survivorship at 8 years in 42 reconstructions with a mean follow-up of 3 years. Similarly, Abolghasemian et al. reported 85% survival in 26 reconstructions at 5.4 years – all in patients with pelvic discontinuity.30,31 Although good mid- and long-term data is not yet available, early results suggest that cup-cage reconstruction holds promise for treatment of significant acetabular bone loss, including pelvic discontinuity.
The major advantage of cup-cage constructs is that compared to traditional ring and cage reconstructions, they allow for biologic fixation. However, there is still a risk for cage fracture over time. There is also a tendency to place the cup too vertical in order to accommodate the cage, and placement of the ischial flange can prove difficult in the setting of severe ischial osteolysis. “Half-cage” techniques (without the inferior ischial flange) have also been described that utilize a “kick-stand” screw inferiorly in the ischium or the superior pubic ramus fracture to avoid abduction failure of the cup.
6.8. Custom triflange acetabular component reconstruction
Customized triflange acetabular components (CTACs) are customized implants that are created through detailed pre-operative planning [Fig. 3]. A three-dimensional CT scan is used to create a 3D-printed acrylic model of the affected hemipelvis. This model incorporates the planned hip center and designates screw placement, length and trajectory. Once the model structure is agreed upon between the manufacturer and surgeon, a custom porous or hydroxyapatite-coated tri-flanged titanium replica is created. The CTAC has the capacity to span acetabular defects in a more rigid fashion and therefore can be used to achieve bony union even in the setting of pelvic discontinuity. In order to maintain implant rigidity and solid fixation, Jennings et al. emphasize the importance of redundant ischial screw fixation as well as firm engagement of the superior edge of the CTAC with the inferior edge of the remaining ilium.32 CTACs and cup-cage constructs are both expensive, with costs estimated at ∼$11,250 to $12,500 in a 2012 review.33
One systematic review compared rates of revision and complication among three different types of revision hip techniques, including reinforcement devices (rings and cages), CTACs, jumbo cups, and tantalum metal.34 The study included 2480 hips and found that CTAC had overall higher rates of revision (15.9%) and complication (24.5%) compared to jumbo cup and tantalum systems (∼8% revision, ∼18% complication).
A more recent systematic review of CTAC survivorship in revision arthroplasty identified 579 CTACs from 17 different studies.35 Overall revision-free survivorship was found to be 87.2%, and the incidence of CTAC aseptic loosening was 1.7% with a mean follow-up of 4.8 years. However, nearly one third of patients experienced a complication, with instability (11%) and infection (6.2%) being the most common. Good mid- and long-term data is still lacking, though this review suggests that early survivorship following CTAC reconstruction is acceptable. Nevertheless, complications do occur, and patients must be counselled appropriately.
The major advantage of CTACs is the theoretical power to perfectly match distorted host anatomy with significant bone loss. However, CTACs require approximately 6 weeks of lead time, and they rarely fit perfectly according to the pre-operative plan due to additional bone loss encountered during component removal. CTACs also have a higher rate of post-operative instability, which the authors speculate may be related to superior gluteal nerve denervation that can occur when the abductors are elevated off the outer table during placement of the ilial flange.
6.9. Acetabular distraction
The acetabular distraction technique was first described in 2012 by Sporer and Paprosky for treatment of chronic pelvic discontinuity.36 Pelvic discontinuity can be diagnosed intra-operatively by applying an inferiorly directed force on the ischium (using a Cobb elevator). If the superior portion of the acetabulum does not move in concert with the ischium or if fluid egress is encountered in the central portion of the acetabulum, then pelvic discontinuity is confirmed. The acetabular distraction technique utilizes a large laminar spreader placed in an extra-acetabular position, which generates lateral or peripheral distraction and central or medial compression across the discontinuity (Fig. 4). It is imperative that the chronic discontinuity is not debrided too aggressively, as this may result in over-distraction and inadequate central compression.
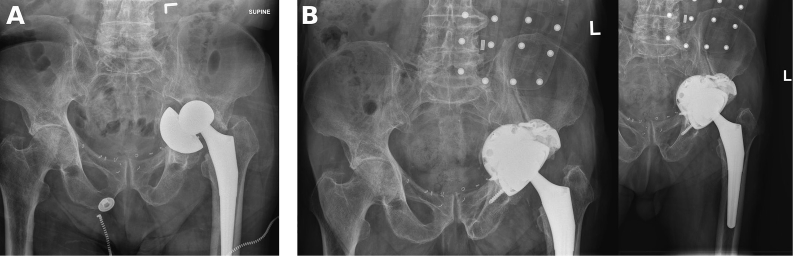
Fig. 4.
Pre-operative (A) and post-operative (B) X-rays of the pelvis and left hip demonstrating a chronic pelvic discontinuity of the left hemi-pelvis that required revision with an uncemented hemispherical shell supported by porous metal augments unitized to the shell. A Dome technique was used by placing augments into the massive anterosuperior acetabular defect. Acetabular distraction was utilized to ensure a large enough cup was implanted and to enhance compression across the discontinuity.
Mid- and long-term outcomes after acetabular distraction are not yet available, though early reports demonstrate its feasibility. Sporer et al. studied 20 pelvic discontinuities treated with pelvic distraction with a minimum follow-up of 2 years.36 One patient (5%) was revised for aseptic loosening, and four patients (20%) had early component migration that subsequently stabilized. Three patients (15%) experienced major complications including iatrogenic colonic perforation, intraoperative femoral artery injury, and superficial infection requiring subsequent irrigation and debridement.
Sheth et al. recently expanded on these results, identifying up to 32 patients with minimum 2 year follow-up and mean follow-up of 5.2 years.37 In that study, only one patient (3.1%) required revision for aseptic loosening, though two additional patients had radiographic loosening but were not revised. Radiographic healing of the pelvic discontinuity was observed in twenty-two (69%) patients, and overall survivorship (against aseptic loosening) was 83.3%.
The major advantage of acetabular distraction is that it provides greater stability of the revision construct by “pre-tensioning” the bone and soft tissues that support the acetabulum. Therefore, acetabular distraction may result in more reproducible healing of a chronic pelvic discontinuity with a theoretically decreased risk of subsequent implant loosening. Disadvantages of acetabular distraction are that it may be more technically demanding compared to other reconstruction methods, and the magnitude of distraction required for adequate fixation is not well defined.
7. Conclusions & future directions
As demonstrated in this review, there are multiple strategies for treatment of acetabular bone loss in revision THA. Each strategy has its advantages and disadvantages, but the general principles remain the same. Successful treatment depends upon thorough pre-operative assessment, planning, and team-based plan execution. When possible, we recommend using uncemented hemispherical shells with adjuvant screw fixation. If significant bone loss is expected, we recommend using the Paprosky classification to guide treatment and to focus on minimizing iatrogenic bone loss during implant removal and maximizing implant contact with host bone. Longer term studies are still needed to evaluate the longevity of these various reconstruction methods, but the authors’ preferred technique for severe acetabular bone loss with an associated chronic pelvic discontinuity is the acetabular distraction technique.
Author statements
George Fryhofer contributed to the conceptualization, investigation, data curation, writing (original draft and review/editing) and visualization of the work.
Sireesh Ramesh was involved in the writing (review/editing), project administration, and visualization of the work.
Neil Sheth contributed to the conceptualization, data curation, writing (original draft and review/editing), visualization, resources, and supervision of the work.
Declarations of competing interest
Two authors have nothing to disclose.
One author reports personal fees from Zimmer (consulting), personal fees from Smith and Nephew (consulting), personal fees from Medacta (consulting), and personal fees from Elsevier (royalites), all outside the submitted work.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am Vol. 2018;100(17):1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 2.Buckland A.J., Miyamoto R., Patel R.D., Slover J., Razi A.E. Differentiating hip pathology from lumbar spine pathology: key points of evaluation and management. J Am Acad Orthop Surg. 2017;25(2):e23–e34. doi: 10.5435/JAAOS-D-15-00740. [DOI] [PubMed] [Google Scholar]
- 3.Parvizi J., Tan T.L., Goswami K. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplast. 2018;33(5):1309–1314 e1302. doi: 10.1016/j.arth.2018.02.078. [DOI] [PubMed] [Google Scholar]
- 4.Sheth N.P., Nelson C.L., Springer B.D., Fehring T.K., Paprosky W.G. Acetabular bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2013;21(3):128–139. doi: 10.5435/JAAOS-21-03-128. [DOI] [PubMed] [Google Scholar]
- 5.Nachbur B., Meyer R.P., Verkkala K., Zurcher R. The mechanisms of severe arterial injury in surgery of the hip joint. Clin Orthop Relat Res. 1979;(141):122–133. [PubMed] [Google Scholar]
- 6.Reiley M.A., Bond D., Branick R.I., Wilson E.H. Vascular complications following total hip arthroplasty. A review of the literature and a report of two cases. Clin Orthop Relat Res. 1984;186:23–28. [PubMed] [Google Scholar]
- 7.Fehring T.K., Guilford W.B., Baron J. Assessment of intrapelvic cement and screws in revision total hip arthroplasty. J Arthroplast. 1992;7(4):509–518. doi: 10.1016/s0883-5403(06)80072-0. [DOI] [PubMed] [Google Scholar]
- 8.Bozic K.J., Kurtz S.M., Lau E., Ong K., Vail T.P., Berry D.J. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am Vol. 2009;91(1):128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 9.D’Antonio J.A., Capello W.N., Borden L.S. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;(243):126–137. [PubMed] [Google Scholar]
- 10.Paprosky W.G., Perona P.G., Lawrence J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplast. 1994;9(1):33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 11.Campbell D.G., Garbuz D.S., Masri B.A., Duncan C.P. Reliability of acetabular bone defect classification systems in revision total hip arthroplasty. J Arthroplast. 2001;16(1):83–86. doi: 10.1054/arth.2001.19157. [DOI] [PubMed] [Google Scholar]
- 12.Sporer S.M., Paprosky W.G., O’Rourke M.R. Managing bone loss in acetabular revision. Instr Course Lect. 2006;55:287–297. [PubMed] [Google Scholar]
- 13.Busch V.J., Gardeniers J.W., Verdonschot N., Slooff T.J., Schreurs B.W. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old: a concise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg Am Vol. 2011;93(4):367–371. doi: 10.2106/JBJS.I.01532. [DOI] [PubMed] [Google Scholar]
- 14.Buttaro M.A., Comba F., Pusso R., Piccaluga F. Acetabular revision with metal mesh, impaction bone grafting, and a cemented cup. Clin Orthop Relat Res. 2008;466(10):2482–2490. doi: 10.1007/s11999-008-0442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schreurs B.W., Bolder S.B., Gardeniers J.W., Verdonschot N., Slooff T.J., Veth R.P. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup. A 15- to 20-year follow-up. J Bone Joint Surg Br. 2004;86(4):492–497. [PubMed] [Google Scholar]
- 16.Zehntner M.K., Ganz R. Midterm results (5.5-10 years) of acetabular allograft reconstruction with the acetabular reinforcement ring during total hip revision. J Arthroplast. 1994;9(5):469–479. doi: 10.1016/0883-5403(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 17.Goodman S., Saastamoinen H., Shasha N., Gross A. Complications of ilioischial reconstruction rings in revision total hip arthroplasty. J Arthroplast. 2004;19(4):436–446. doi: 10.1016/j.arth.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 18.Sternheim A., Abolghasemian M., Safir O.A., Backstein D., Gross A.E., Kuzyk P.R. A long-term survivorship comparison between cemented and uncemented cups with shelf grafts in revision total hip arthroplasty after dysplasia. J Arthroplast. 2013;28(2):303–308. doi: 10.1016/j.arth.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Della Valle C.J., Berger R.A., Rosenberg A.G., Galante J.O. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;(420):96–100. doi: 10.1097/00003086-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Hallstrom B.R., Golladay G.J., Vittetoe D.A., Harris W.H. Cementless acetabular revision with the Harris-Galante porous prosthesis. Results after a minimum of ten years of follow-up. J Bone Joint Surg Am Vol. 2004;86(5):1007–1011. doi: 10.2106/00004623-200405000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Jamali A.A., Dungy D.S., Mark A., Schule S., Harris W.H. Isolated acetabular revision with use of the Harris-Galante Cementless Component. Study with intermediate-term follow-up. J Bone Joint Surg Am Vol. 2004;86(8):1690–1697. doi: 10.2106/00004623-200408000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Jones C.P., Lachiewicz P.F. Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J Bone Joint Surg Am Vol. 2004;86(2):342–347. doi: 10.2106/00004623-200402000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Templeton J.E., Callaghan J.J., Goetz D.D., Sullivan P.M., Johnston R.C. Revision of a cemented acetabular component to a cementless acetabular component. A ten to fourteen-year follow-up study. J Bone Joint Surg Am Vol. 2001;83(11):1706–1711. doi: 10.2106/00004623-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Dewal H., Chen F., Su E., Di Cesare P.E. Use of structural bone graft with cementless acetabular cups in total hip arthroplasty. J Arthroplast. 2003;18(1):23–28. doi: 10.1054/arth.2003.50013. [DOI] [PubMed] [Google Scholar]
- 25.Lee P.T., Raz G., Safir O.A., Backstein D.J., Gross A.E. Long-term results for minor column allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2010;468(12):3295–3303. doi: 10.1007/s11999-010-1591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Browne J.A., Lewallen D.G. Chapter 53: acetabular revision with cup-cage constructs. In: Lieberman J.R., Berry D.J., editors. Advanced Reconstruction Hip 2. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2017. pp. 523–528. [Google Scholar]
- 27.Sporer S.M., Paprosky W.G. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplast. 2006;21(6 Suppl 2):83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 28.Whitehouse M.R., Masri B.A., Duncan C.P., Garbuz D.S. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res. 2015;473(2):521–527. doi: 10.1007/s11999-014-3861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kosashvili Y., Backstein D., Safir O., Lakstein D., Gross A.E. Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br. 2009;91(7):870–876. doi: 10.1302/0301-620X.91B7.22181. [DOI] [PubMed] [Google Scholar]
- 30.Abolghasemian M., Tangsaraporn S., Drexler M. The challenge of pelvic discontinuity: cup-cage reconstruction does better than conventional cages in mid-term. Bone Jt J. 2014;96-B(2):195–200. doi: 10.1302/0301-620X.96B2.31907. [DOI] [PubMed] [Google Scholar]
- 31.Rogers B.A., Whittingham-Jones P.M., Mitchell P.A., Safir O.A., Bircher M.D., Gross A.E. The reconstruction of periprosthetic pelvic discontinuity. J Arthroplast. 2012;27(8):1499–1506. doi: 10.1016/j.arth.2011.12.017. e1491. [DOI] [PubMed] [Google Scholar]
- 32.Jennings J.M., Kim R.H., Dennis D.A. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2017. Chapter 52: Acetabular Revision with Triflange Cups. [Google Scholar]
- 33.Taunton M.J., Fehring T.K., Edwards P., Bernasek T., Holt G.E., Christie M.J. Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res. 2012;470(2):428–434. doi: 10.1007/s11999-011-2126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain S., Grogan R.J., Giannoudis P.V. Options for managing severe acetabular bone loss in revision hip arthroplasty. A systematic review. Hip Int. 2014;24(2):109–122. doi: 10.5301/hipint.5000101. [DOI] [PubMed] [Google Scholar]
- 35.De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK. Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplast. 2019;34(10):2511–2518. doi: 10.1016/j.arth.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 36.Sporer S.M., Bottros J.J., Hulst J.B., Kancherla V.K., Moric M., Paprosky W.G. Acetabular distraction: an alternative for severe defects with chronic pelvic discontinuity? Clin Orthop Relat Res. 2012;470(11):3156–3163. doi: 10.1007/s11999-012-2514-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sheth N.P., Melnic C.M., Brown N., Sporer S.M., Paprosky W.G. Two-centre radiological survivorship of acetabular distraction technique for treatment of chronic pelvic discontinuity: mean five-year follow-up. Bone Jt J. 2018;100-B(7):909–914. doi: 10.1302/0301-620X.100B7.BJJ-2017-1551.R1. [DOI] [PubMed] [Google Scholar]