Abstract
Purpose
Our study compares the outcome and cost of distal femoral arthroplasty to that of Fixation (Plating/Retrograde Nailing) in the management of distal femur peri-prosthetic fractures.
Methods
We reviewed our database for patients admitted with peri-prosthetic distal femoral fractures between 2005 and 2013 (n = 61). The patients were stratified into 2 groups based on management method. The Distal Femoral Arthroplasty group (Group A) had 21 patients and the Fixation group (Group B) had 40 patients. Outcome & cost were compared. Minimum follow-up was 3 years.
Results
The mean length of stay in group A was 9 days whereas in group B was 32 days. All patients were fully weight bearing by day 3 in group A, compared to a mean of 11 weeks in group B. Mean OKS was 28 and KSS score was 70 in group A compared to 27 and 68 in group B. In group A, there were 2 deaths, 1 superficial infection, and 1 DVT. In group B, there were 6 deaths, 1 failure of fixation, 6 mal-unions, 1 non-union and 2 infections. Overall, the distal femoral arthroplasty procedure costs approximately £9600 and the fixation group costs were on average of £9800.
Conclusion
Distal femoral arthroplasty appears to provide good clinical results, with comparable overall costs to fixation.
Keywords: Peri-prosthetic, Distal femoral arthroplasty, Total knee arthroplasty, Outcome, Cost
1. Introduction
The management of periprosthetic distal femur fractures following TKA (Total Knee Arthroplasty) in elderly population remains a challenge with little or no consensus on the best treatment for these fractures.
Supracondylar periprosthetic femur fractures are those within 15 cm of the knee joint line or within 5 cm of the proximal end of the implant1 (Fig. 1). An incidence of 1.1% of patients after primary TKR and 2.5% of patients after revision TKR has been recently reported.2
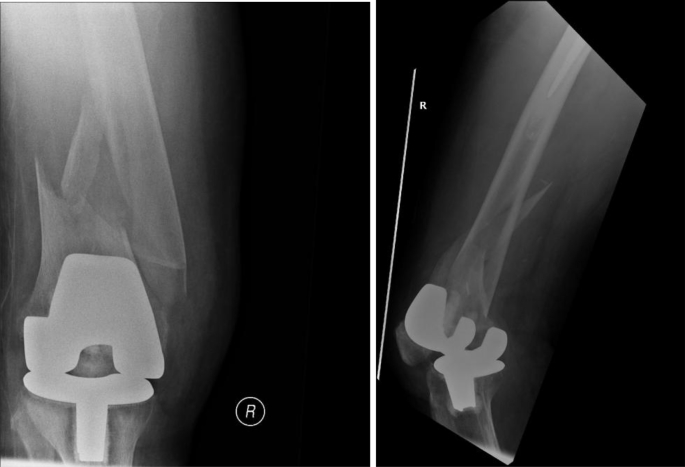
Fig. 1.
(Pre-operative X-ray).
Risk factors for periprosthetic fractures include poor bone stock, advancing age, female gender, chronic use of corticosteroids, inflammatory arthropathy, previous surgery, excessively stiff joints, various neurological conditions and stress risers.3, 4, 5, 6
A wide variety of treatment options have been described in the literature for this challenging and complex subgroup of fractures with complications as high as 25–75%, even when treated by experienced surgeons.7
Modern day treatment methods are superior to conventional treatment options in the management of distal femur fractures above TKAs.8 These range from open reduction and internal fixation using locked plates and retrograde nails to stemmed revision TKA and DFA (Distal Femoral Arthroplasty).9, 10, 11, 12, 13
DFA is perceived to be an extensive surgical procedure, technically demanding and has a high complication rate. It is also perceived to be expensive with no long-term results available in the literature.
We did this study to evaluate the results of DFA as an alternative to fixation and compare their clinical outcomes and cost in the management of distal femur periprosthetic fractures in the elderly patient.
2. Materials & methods
A retrospective review of our prospectively collected data between 2005 and 2013 was undertaken following institutional ethics review board approval.
The patients were stratified into 2 groups based on the management method. The Distal Femoral Arthroplasty group (Group A) (n = 21) and the Fixation group (Group B) (n = 40), 23 of those had plating of the fracture, while 17 had a retrograde nail inserted.
Choice of treatment method was made using the classification of Kim et al. (Table 1) for periprosthetic fractures.4 It takes into account the status of the prosthesis, quality of distal bone stock, and reducibility of the fracture.
Table 1.
Kim et al. Classification.
| Type | Fracture reducible | Bone quality in distal fragment | Component fixation & Component position | Treatment |
|---|---|---|---|---|
| I A | Yes | Good | Well fixed Satisfactory position |
Conservative |
| B | No | Good | Well fixed Satisfactory position |
Surgical fixation |
| II | Yes/No | Good | Loose or Unsatisfactory position | Revision/Long stem prosthesis |
| III | Yes/No | Poor | Loose or Unsatisfactory position | Distal Prosthetic replacement |
2.1. Demographics in group A (Fig. 2)
Fig. 2.
(Post-operative DFA).
In group A, we had 21 patients who underwent DFA for distal femur periprosthetic fractures. This group had a mean age of 78 years (range 68–90). Of these, there were 18 females and 3 males. The mechanism of injury was low velocity except for one patient who had a road traffic accident. All these patients were mobile and walking prior to the injury. 18 patients were Type 3 and 3 were Type 2 in the Kim classification.
All procedures were performed under tourniquet control through anterior midline approach and medial parapatellar arthrotomy.
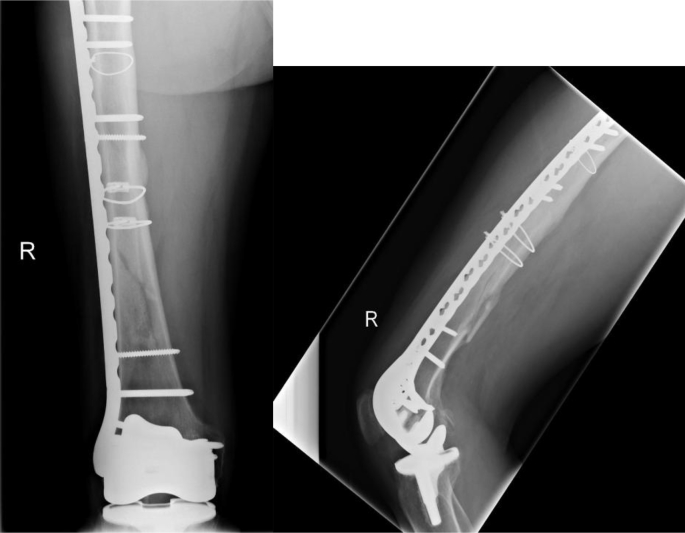
2.2. Demographics in group B (Fig. 3)
Fig. 3.
(Post-op locking plate).
In group B, we had 40 patients who underwent internal fixation for distal femur periprosthetic fractures. This group had a mean age of 74 years (range 65–83). Of these, there were 31 females and 9 males. 23 patients had plating (locking plates and standard non-locking peri articular plates) and 17 patients had retrograde nailing. There were 26 in Type 1B and 14 Type 2 fractures in the Kim classification. Most patients had a low velocity trauma and were independently mobile with or without walking aids.
2.3. Outcomes
Outcomes were analysed between the 2 groups using such parameters as length of hospital stay, day of full weight bearing mobilisation and fracture healing times. Functional outcomes were also assessed using Oxford knee scores, KSS scores, VAS pain assessment and knee ROM from last follow up appointment. The follow up was at 6 weeks, 3 months and then at 6 monthly basis in outpatient clinic with radiographic analysis at each visit.
2.4. Cost analysis
The cost analysis was done for management in both groups including implant costs, consumable costs (man power included), theatre utilisation time and length of hospital stay. The calculation was done based on the PbR(payment by results) system and “best practise tariffs -2010-11” utilised by the NHS (National Health Service) in England.
PbR is the payment system in England in which commissioners pay healthcare providers for each patient seen or treated, taking into account the complexity of the patient's healthcare needs.
The two fundamental features of PbR are nationally determined currencies and tariffs. Currencies are the unit of healthcare for which a payment is made. Tariffs are the set prices for a given currency.
The currencies for admitted patient care are set out in HRG4(Healthcare resource groups-latest version). HRGs are clinically meaningful groups of diagnoses and interventions that consume similar levels of NHS resources, covering a spell of care from admission to discharge.
Each intervention has been provided a unique OPCS code (Office of Population, Census and Surveys Classification of Surgical Operations and Procedures-OPCS 4.6). These clinical codes are grouped into HRGs followed by calculation of “best practise tariffs”.14
3. Results (Table- 2)
Results are summarized in Table 2. Blood loss was significantly higher in Group B (800 ml), but operative times were similar.
Table 2.
Comparison of outcomes.
| Group A | Group B | |
|---|---|---|
| Average Surgical Time | 116 min | 123 min |
| Average Blood Loss | 400 ml | 800 ml |
| Minimum Follow up | 72 months | 72 months |
| Length of Stay | 9 days | 32 days |
| Full Weight Bearing (days) | 1.5 days | 11 weeks |
| Oxford Knee Score | 28 | 27 |
| KSS Score | 70 | 68 |
| Pain VAS | 2 | 1.5 |
| Fracture Healing (Weeks) | - | 11.5 weeks |
| Range of Motion at last follow-up | 3.5–95° | 5-85° |
The mean length of hospital stay in group A was 9 days whereas in group B was 32 days. All patients were mobilising full weight bearing by day 1.5(range 1–3 days) in group A compared to a mean of 11 weeks in group B.
There was no real difference in functional outcomes or pain scores between the groups.
In group A, all patients returned to their own homes except for 5 patients who came from care homes and returned to the same facility.
Radiographic analysis in group A showed no progressive lucent lines suggestive of loosening and radiographic measurements confirmed that all knees were neutral to 6° of valgus.
3.1. Complications
We had 4 complications in group A. There were 2 deaths due to medical co-morbidities within 1 year of surgery, 1 superficial infection (treated with antibiotics) and 1 DVT.
In the fixation group, there were 6 deaths (medical co-morbidities), 1 failure of fixation, 6 malunions (>8 ° loss of sagittal or coronal alignment), 1 non-union (Fixation revised) and 2 infections. The failure of fixation and non-union involved periarticular plates. Both were revised to distal femoral replacements. Of the infections, 1 was a superficial infection and the other deep with the later patient opting for suppressive long term antibiotics.
3.2. Cost implications
Comparing the costs, the average implant of DFA (Distal segmental femoral replacement-Zimmer Plc) was £7500 and for Fixation group, the average implant costs for locking plates(NCB Plating system, Zimmer Plc) were £2300 and interlocking nailing system(Stryker Plc) was £1500. The average theatre time of 2 h was comparable and the same in either group. The length of stay in DFA group cost on an average, £2115(£235/day × 9days) whereas in the fixation group, it was £7520(£235 day × 32 days).
Taking into account of other consumables, investigations and rehabilitation, again there was no major cost differences in either group. Overall, the DFA procedure costs on average were approximately £9600 and fixation group costs were on average of £9800.
For NHS Payment by Results (PbR) system in the UK, DFA was coded using OPCS 4.6 coding system (W42·3/W 42.8) and HRG was coded as Major Reconstructive procedure category 4(HA03Z) with inpatient long stay trim point of 55 days with tariff payment of £9805. On the other hand, the fixation group was coded as OPCS W19.2/20.1/20.4/21.1/21.5, and HRG coding as Major Knee procedure (Category 2 Trauma HA21B) with inpatient long stay trim point of 21 days and tariff payment of £5679. As most patients in this group overstayed the trim point by at least 2 weeks, it resulted in an average additional cost of £3300 above the assigned best practice tariff making the ultimate cost comparable in the two groups.
4. Discussion
Kurtz et al. have estimated an increase in demand for primary TKA to grow by 673% in the United States from 2005-2030.15
Periprosthetic distal femur fractures are expected to rise in direct proportion to the number of primary TKAs.
Moreover, the ageing population with TKA in conjunction with increased activity levels following TKA may further amplify the incidence of this complex problem.
The demographics of our study identified that most injuries occurred in active elderly osteoporotic females following low velocity trauma.
Early-midterm results were favourable following DFA in our group. Most patients were discharged from hospital by 9 days and were mobilizing FWB by post-operative day 1. In the fixation group, average hospital stay was 32 days and mean time to FWB was 11 weeks following fracture fixation.
No significant difference was noted in functional outcome between the 2 groups using Oxford scores, KSS scores, Pain VAS assessment and final knee ROM. Fewer medical and surgical complications were noted in the Arthroplasty group compared to the fixation group.
On one hand, mixed results have been shown in literature following fixation of these fractures, whilst, on the other hand, there is a paucity of literature on treating these fractures with DFA.
In 1970s and 1980s, large numbers of periprosthetic distal femur fractures were treated conservatively with either plaster immobilisation or traction and cast bracing and were associated with high incidence of complications and less than desirable results.5
With the advent of modern methods of fixation such as locked plates, LISS plates and retrograde nails, increasing number of patients were treated with surgical fixation.
Osteosynthesis in these fractures in elderly patients with poor bone stock are fraught with high incidence of non-union, malunion and failure of surgical fixation.
Rorabeck et al.16 described the ultimate management goal in these injuries was to achieve a pain free knee ROM with fracture union in less than 6 months to allow ambulation and ROM to 90°. We feel that these timescales to return to function in the vulnerable elderly population are too long. Also, failure to mobilise FWB in elderly makes them more dependent resulting in need of more inpatient or rehabilitation beds adding to the economic burden.
McLaren et al., showed a return to pre-fracture function in 3 months using retrograde nails for fixation.17
Norrish AR et al. using LISS plates for fixation identified an average time to union of 3.7 months.18
Herrera et al., in their meta-analysis of 29 case series with a total of 415 fractures treated by retrograde nails, condylar locking and non-locking plates showed a non-union rate of 9%, fixation failure rate of 4%, revision surgery rate of 13% and infection rate of 3.1%.8
A recent study by Ebraheim et al.,19 using locked plates for fixation identified an average time to fracture healing and FWB was 4.5 months ± 2.7 months with union rate of 89% at 6 months. Up to 37% of patients experienced complications such as delayed union (7.4%), non-union (3.7%) and fixation failures (26%)
Only, a few reports in literature are available using DFA and long stem revision (hinged) knee prosthesis for treating these periprosthetic fractures.
Srinivasan K et al., in a small series of 8 patients with a mean age of 78 years highlighted the role of long stem revision (hinged) knee prosthesis in periprosthetic and some complex distal femur fractures in offering stability and early mobilisation.12 Appleton P et al., in their cohort of 54 periprosthetic distal femur fractures concluded that constrained knee prosthesis offers a useful alternative treatment to internal fixation in selected elderly patients and has a probability of surviving as long as the patient into whom it has been implanted.20
Mortazavi et al. reviewed 20 patients following DFA and considered it a viable option for complex periprosthetic femoral fractures after TKA. Their cohort had a mean age of 69.5 years with an average follow up of 58.6 months. Mean KSS score improved to 82.8 and mean SF-36 physical and mental score functional scores improved to 55.8 and 65.6 respectively.13
Lombardi et al. in their cohort of 39 rotating hinged distal femoral replacements, with 13 due to periprosthetic fractures identified excellent pain relief and function with a low short term re-operation rate and an implant survivorship rate of 87% at 46 months.21
More recently, Chen AF et al., supported the role of primary DFA to ORIF in osteopenic patients and those at high risk of non-union in these complex fractures.22
There is a perception that use of distal femoral replacement is cost prohibitive in revision knee settings.
Saidi K et al. compared allograft implant composites, standard revision components and distal femoral replacement prosthesis for treatment of supracondylar periprosthetic fractures of the knee in elderly.23 They mentioned the need for a thorough and formal cost benefit analysis between different management techniques in this complex injury.
To our best knowledge, our study is the first one to perform a detailed cost analysis between DFA and internal fixation in the management of distal femur periprosthetic fractures.
It appears that actual costs are comparable with no major differences between the 2 procedures.
The higher cost of implants in DFA is recouped in the much shorter hospital stay in this procedure. The lower cost of the implants added to the cost of prolonged hospital stay due to prolonged recovery and ambulatory dysfunction in the fixation group resulted in the actual costs between the 2 groups being comparable.
In fact, hospitals in the NHS (National Health Service) use payment by results (PbR) system and “best practise tariff” appear to lose on an average of £3300 per procedure in the fixation group.
5. Conclusion
Our study has a few limitations. It is a case-control study, with a small number of patients having an early-midterm follow up. Also, Group A (fixation group) has a less severe spectrum of fractures compared to Group B (DFA) based on the Kim et al. classification. However, Kim et al. classification (including radiological appearance, bone quality and stability/alignment of prosthesis) was not the sole criterion for choosing either treatment option. There were other confounding co-factors looked at in both groups of patients. These included medical co-morbidities, ASA grade, pre-injury mobility and social circumstances (living independently, home support etc). These confounding factors were essentially similar in fixation and DFA group.
The aim of our study was to evaluate the results of DFA as an alternative to fixation and compare their clinical outcomes and cost in the management of distal femur periprosthetic fractures in the elderly patient.
However, it has identified several interesting findings in the management of this complex and challenging subgroup of fractures.
DFA allowed early mobilisation avoiding prolonged hospital stay and preventing medical co morbidities. Complication rates were less than the fixation group and actual costs were comparable between the 2 groups.
DFA appears to be promising as an alternative treatment to internal fixation in elderly patients in these complex fractures. With appropriate patient selection, the prosthesis has a high probability of surviving as long as the patient into whom it is implanted.
In a scenario, with pre-existing loose total total knee replacement, this procedure itself can be a definitive treatment. One has to be aware that distal femoral arthroplasty does not match the function and longevity of the surface replacements in a primary situation; nevertheless, modern rotating hinged knee distal femoral replacements allowing increased freedom of rotation with decreased bone-prosthesis interface stresses, can be used in appropriate fractures and in low demand patients for good functional outcome.
Certainly, there is a need for randomised, multicentre trials and longer-term studies to assess the management of these complex and challenging group of fractures.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
References
- 1.Neer C.S., II, Grantham S.A., Shelton M.L. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am. 1967;49(4):591–613. [PubMed] [Google Scholar]
- 2.Singh Jasvinder A., Jensen Matthew, Lewallen David. Predictors of periprosthetic fracture after total knee replacement, an analysis of 21,723 cases. Acta Orthop. 2013 Apr;84(2):170–177. doi: 10.3109/17453674.2013.788436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ritter M.A., Faris P.M., Keating E.M. Anterior femoral notching and ipsilateral supracondylar femur fracture in total knee arthroplasty. J Arthroplast. 1988;3:185–187. doi: 10.1016/s0883-5403(88)80085-8. [DOI] [PubMed] [Google Scholar]
- 4.Kim K.I., Egol K.A., Hozack W.J. J. Parvizi Periprosthetic fractures after total knee arthroplasties Clin Orthop Relat Res. 2006;446:167–175. doi: 10.1097/01.blo.0000214417.29335.19. [DOI] [PubMed] [Google Scholar]
- 5.Chen F., Mont M.A., Bachner R.S. Management of ipsilateral supracondylar femur fractures following total knee arthroplasty. J Arthroplast. 1994;9(5):521–526. doi: 10.1016/0883-5403(94)90099-x. [DOI] [PubMed] [Google Scholar]
- 6.Engh G.A., Ammeen D.J. Periprosthetic fractures adjacent to total knee implants: treatment and clinical results. Instr Course Lect. 1998;47:437–448. [PubMed] [Google Scholar]
- 7.Herigou P., Poignard A., Manicom O., Chabane-Sari M.A. Treatment of fractures of the distal femur on total knee arthroplasty. Rev Chir Orthop Reparatrice Mot. 2006 Apr;92(2):148–157. doi: 10.1016/s0035-1040(06)75700-2. 18. [DOI] [PubMed] [Google Scholar]
- 8.Herrera D.A., Kregor P.J., Cole P.A., Levy B.A., Jonsson A., Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981–2006) Acta Orthop. 2008;79(1):22–27. doi: 10.1080/17453670710014716. [DOI] [PubMed] [Google Scholar]
- 9.Kolb W., Guhlmann H., Windisch C., Marx F., Koller H., Kolb K. Fixation of periprosthetic femur fractures above total knee arthroplasty with the less invasive stabilization system: a midterm follow-up study. J Trauma. 2010 Sep;69(3):670–676. doi: 10.1097/TA.0b013e3181c9ba3b. [DOI] [PubMed] [Google Scholar]
- 10.Dunlop D.G., Brenkel I.J. The Supracondylar intramedullary nail in elderly patients with distal femur fractures. Injury. 1999 Sep;30(7):475–484. doi: 10.1016/s0020-1383(99)00136-9. [DOI] [PubMed] [Google Scholar]
- 11.Hou Z., Bowen T.R., Irgit K. Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma. 2012 Feb 21;26(7):427–432. doi: 10.1097/BOT.0b013e31822c050b. [DOI] [PubMed] [Google Scholar]
- 12.Srinivasan Kuntrapaka, Macdonald David A., Tzioupis Christopher C., Giannoudis Peter V. Role of long stem revision knee prosthesis in periprosthetic and complex distal femoral fractures: a review of eight patients. Injury. 2005 Sep;36(9):1094–1102. doi: 10.1016/j.injury.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Javad Mortazavi S.M., Kurd Mark F., Bender Benjamin. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty - J Arthroplast. 2010 Aug;25(5):775–780. doi: 10.1016/j.arth.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 14.https://www.gov.uk/government/publications/simple-guide-to-payment-by-results
- 15.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg AM. 2007 Apr;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 16.Rorabeck C.H., Angliss R.D., Lewis P.L. Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instr Course Lect. 1998;47:449. [PubMed] [Google Scholar]
- 17.McLaren A.C., Dupont J.A., Schroeber D.C. Open reduction internal fixation of supracondylar fractures above total knee arthroplasties using the intramedullary supracondylar rod. Clin Orthop Relat Res. 1994 May;(302):194–198. [PubMed] [Google Scholar]
- 18.Norrish A.R., Jibri Z.A., Hopgood P. The LISS plate treatment of supracondylar fractures above a total knee replacement: a case-control study. Acta Orthop Belg. 2009 Oct;75(5):642–648. [PubMed] [Google Scholar]
- 19.Ebraheim Nabil A., Liu Jiayong, Hashmi Sohaib Z., Sochacki Kyle R., Moral Muhammad Z. High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties. J Arthroplast. 2012 May;27(5):809–813. doi: 10.1016/j.arth.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Appleton P., Moran M., Houshian S., Robinson C.M. Distal femoral fractures treated by hinged total knee replacement in elderly patients. J Bone Jt. Surg. 2006 Aug;88(8):1065–1070. doi: 10.1302/0301-620X.88B8.17878. [DOI] [PubMed] [Google Scholar]
- 21.Berend Keith R., Lombardi Adolph V., Jr. Distal femoral replacement in non tumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009;467:485–492. doi: 10.1007/s11999-008-0329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen A.F., Choi L.E., Colman M.W. Primary versus secondary distal femoral arthroplasty for treatment of total knee arthroplasty periprosthetic femur fractures. J Arthroplast. 2013 Oct;28(9):1580–1584. doi: 10.1016/j.arth.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 23.Saidi K., Ben-Lulu O., Tsuji M., Safir O., Gross A.E., Backstein D. Supracondylar periprosthetic fractures of the knee in the elderly patients: a comparison of treatment using allograft-implant composites, standard revision components, distal femoral replacement prosthesis. J Arthroplast. 2013 May 13;(13):00305–00307. doi: 10.1016/j.arth.2013.04.012. pii: S0883-5403. [DOI] [PubMed] [Google Scholar]