Abstract
Background
Metallosis is a syndrome of metal-induced synovitis caused by friction between two metal surfaces. In contrast to the hip joint after resurfacing arthroplasty or metal-on-metal (MoM) total hip replacement, metallosis of the knee is extremely rare.
Materials
We describe 4 patients who underwent revision total knee replacement because of disabling pain and implant loosening after a mean time of 21 (range: 13–30) years of knee replacement surgery. They were all females with a mean age of 79 (range: 75–82) years. Septic loosening was excluded through microbiological examination and synovial fluid analysis.
Results
Direct metal-on-metal contact at the tibiofemoral interface was confirmed intraoperatively in all cases. All knees showed severe metallosis with advanced osteolysis and pseudotumor formation. In one knee there was a complete fracture of the tibial tray. All patients had a one-stage revision surgery with implant removal, profound synovectomy and implantation of a constrained modular revision knee system. Long modular stems with offset adapters, wedges and/or blocks were used in all cases.
Conclusion
Metallosis-associated osteolysis should be suspected in cases with radiologically evident polyethylene wear after knee replacement. Recognizing that revision arthroplasty is very technically demanding in such cases, surgeons should have a back-up with modular revision components and a ready access to reconstructive options at this revision setting.
Keywords: Metallosis, Arthroplasty, Polyethylene wear, Metal on metal, Revision total knee replacement
1. Introduction
Metallosis is a syndrome of metal-induced synovitis, commonly associated with osteolysis, soft tissue necrosis and formation of pseudotumours.1 It is caused by friction between two metal surfaces that releases metal debris into the periprosthetic soft tissues thus triggering an inflammatory response in the synovium and adjacent bone.1, 2, 3
In contrast to the hip joint where failure of resurfacing arthroplasty and large-head metal on metal (MoM) total hip replacement has been frequently associated with this problem leading to a wide-spread recall for most of these implants, metallosis of the knee joint is extremely rare after total knee replacement because of the standard use of polyethylene (PE) as a bearing surface. Thus its occurrence here almost always indicates abnormal metal-on-metal contact following advanced full-thickness PE wear at the tibiofemoral or the patellofemoral joint (in metal-backed patellar components).4, 5, 6, 7, 8, 9, 10, 11, 12
Metallosis induces a foreign-body inflammatory reaction with lymphocytic, histiocytic and giant cell infiltration and massive release of cytokines including Interleukin I, interleukin 6, interleukin 8 and tumor necrosis factor (TNF), leading to chronic synovitis and osteoclastic bone resorption causing progressive peri-prosthetic osteolysis with pain and implant loosening making revision surgery necessary to prevent further bone loss.4,5
Only a few reports in the literature have dealt with this problem in the knee joint. This study describes the presentation, diagnostic features and management of late total knee replacement failure because of metallosis and reviews the available literature in this regard.
2. Materials and methods
We describe four patients who underwent revision total knee replacement because of persistent knee pain and progressive swelling years after primary knee replacement surgery. Three patients had a total knee arthroplasty (TKA) and one was treated using a unicondylar knee arthroplasty (UKA). They were all females above 75 years old with a mean age of 79 years (range: 75–82). The Body Mass Index (BMI) was 30 in three patients and 20.5 in the fourth (mean: 27.6 kg/m2).
Preoperatively, all patients were evaluated radiographically using anteroposterior and lateral x-rays of the knee as well as long standing views to assess lower limb alignment and allow computer-based implant planning. Radiologically, advanced PE wear was suspected in the plain x-rays and bubbly radiopaque densities (cloud or bubble sign) were seen with fine linear radio-opacities (metal lines) outlining the joint cavity and the suprapatellar pouch in addition to gross metal debris (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 1.
A case of severe metallosis of the knee joint following fracture of the tibial tray and MoM contact showing the typical radiographic signs (bubble and cloud sign, metal lines and gross metal debris) 20 years after TKA. Revision was done using an RT-Plus system (Smith & Nephew, Memphis, TN).
Fig. 2.
A case of metallosis due to complete wear of the posteromedial part of the inlay with joint subluxation 13 years after TKA. Revision was done using an RT-Plus system with 10 mm tibial augmentation block (Smith & Nephew, Memphis, TN).
Fig. 3.
A case of advanced metallosis with bone loss and metal debris due to MoM contact with aseptic loosening of a unicondylar knee replacement. Revision was done using an RT-Plus system (Smith & Nephew, Memphis, TN).
Fig. 4.
A case of metallosis due to MoM contact at the tibiofemoral and patellofemoral articulation 30 years after TKA. Revision was done using a Legion Revision Knee system (Smith & Nephew, Memphis, TN).
Septic loosening was excluded preoperatively through laboratory work-up (total leucocytic count, ESR and CRP) and microbiological examination after knee joint puncture and synovial fluid analysis. Joints were considered aseptic if the synovial leucocytic count was below 2000 and cultures remained negative for pathogens after 10 days. None of the patients had signs of systemic metal toxicity like skin rash, tinnitus, deafness or confusion.
Revision surgery was done after a mean time of 21 (range: 13–30) years of the primary joint replacement procedure. Surgery was done under general anaesthesia in a standard operating room with laminar flow with a single-shot antibiotic prophylaxis using a second-generation cephalosporin (Cefuroxime 1.5 gm i. v.). A tourniquet was used in all patients.
3. Results
Direct metal-on-metal (MoM) contact at the tibiofemoral interface at sites of radiologically apparent polyethylene wear was confirmed intraoperatively in all cases. In one knee, there was also MoM contact at the patellofemoral interface. All knees showed a severe metallosis of the joint with extreme black staining of the synovial tissues (Fig. 5). Furthermore, some knees showed cystic cavities extending from the joint capsule into the popliteal fossa with metal-debris pseudotumor formation. In one knee there was even a complete fracture of the medial part of the tibial tray after the medial part of the PE inlay has totally worn away. A profound synovectomy was done in all cases and biopsy specimens were sent for pathological examination using haematoxylin and eosin staining and polarised light microscopy. Samples for culture and sensitivity testing were also taken. The implants were removed using a combination of small oscillating saws and narrow osteotomes. Advanced osteolysis with holes filled with black metal debris was seen underneath the prosthetic components. Local debridement was done until all macroscopic evidence of metallosis were removed and bone cysts were curetted. This was followed by extensive jet lavage of all bony and soft tissue surfaces using at least 3 L of normal saline.
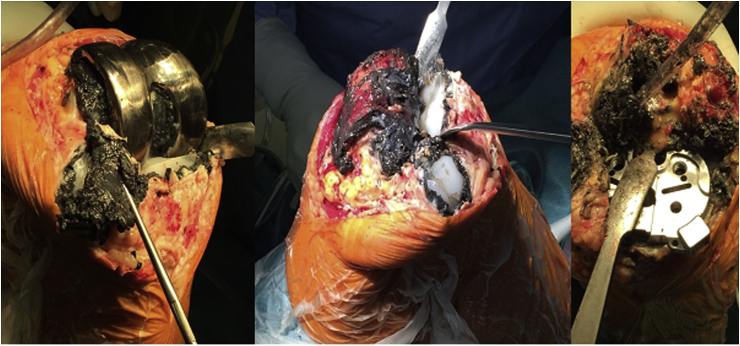
Fig. 5.
Intraoperative photographs of the last case showing dark black staining of the synovial tissues and advanced osteolysis with holes filled with metal debris underneath all prosthetic components.
All cases were revised using a cemented constrained modular revision knee system (Smith & Nephew, Memphis, TN): the RT-Plus system in three knees and the Legion Revision Knee System in one. Long modular stems with offset adapters, wedges and/or blocks were needed in all revisions. No cases required the implantation of tumor prostheses. Cultures from intraoperative samples remained negative for bacterial pathogens. The retrieved implants showed deep linear scratching visible to the naked eye coinciding with the axis of frictional motion (Fig. 6). Histological examination of the synovial tissue samples obtained revealed the picture of chronic inflammation with hyperplasia and extensive fine black metal particles partially engulfed by macrophages with no or few particles of PE wear (Fig. 7).
Fig. 6.
Retrieved implants showing linear scratches on the femoral component and PE-wear of the metal-backed tibial and patellar components.
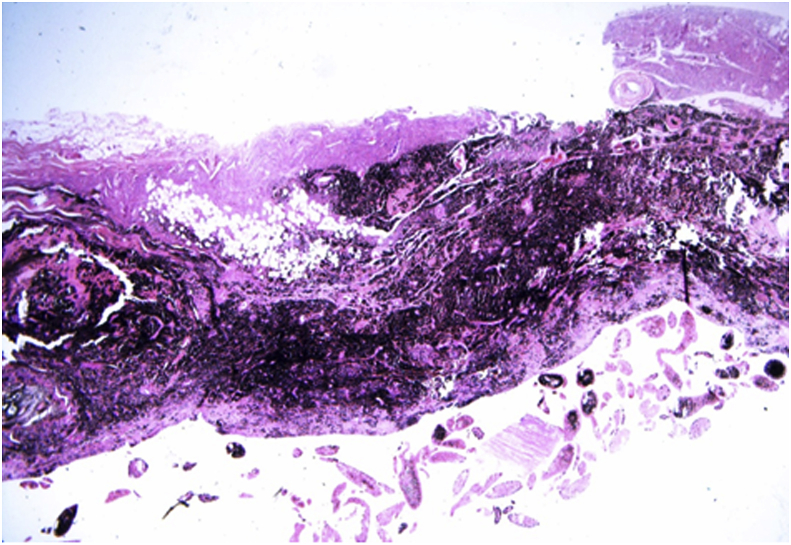
Fig. 7.
Microscopic picture of metallosis-associated synovitis from the last case.
Postoperatively, patients were mobilized on crutches with weight bearing according to the pain tolerance. Range of motion exercises were done on a CPM machine in addition to physiotherapy before discharging the patients into a multimodal rehabilitation program on an in-patient basis. There was an immediate pain relief in all cases after surgery. All patients were satisfied with the treatment outcome at their last visit. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC score) improved by a minimum of 20 in all cases. The average follow-up of the study cases was 25 (range: 10–54) months.
4. Discussion
Metallosis was first seen in the setting of fracture fixation with metallic implants.13 Basically every metal implant (e.g. screws, plates, spinal instrumentations) has a potential local or systemic effect due to metal ions.14 The real incidence of metallosis after joint replacement surgery is still unknown.5 It has been extensively reported after metal-on-metal (MoM) hip replacement with associated osteolysis and early failure.15, 16, 17 Chang et al. reported an overall 5.3% incidence of metallosis in total hip replacement.16 Ollivere et al. reported a 3.1% rate of metallosis-related failure at five years in hip resurfacing.17 Metallosis was also described after shoulder,18 elbow19 and wrist arthroplasty.20 Titanium (Ti) components appear to cause more metallosis as compared to cobalt-chrome (CoCr) implants.4,6
Metallosis after total knee replacement is extremely rare because direct MoM contact is avoided.7 However, if the PE inlay have worn away, unintended MoM contact at the tibiofemoral8,9 or the patello-femoral interface (with metal-backed patellar components)10,11 or with constrained implants using metallic bushes21 can take place. Rarely, MoM contact may occur because of breakage of the PE inlay or its dislodgmenet from the metal backing without advanced wear. Klontz et al. even reported a case of metallosis due to metallic debris from the oscillating saw blades used during surgery in a sclerotic bone.22 Currently, metal-backed patellar components are replaced by all-PE patellar buttons in order to avoid the problem of backside wear but patients having these implants are still being seen.23
The pathogenesis of metallosis-related joint changes is complex and involves direct cytotoxic effects, a delayed hypersensitivity (type IV) response to metal debris and particle-induced synovitis.4,8,24,25 The local adverse reactions include a pleomorphic clinical spectrum from small asymptomatic soft tissue lesions to dramatic osteolysis, bone necrosis, effusion and growing masses that can cause secondary pathological effects.14 Furthermore, the phagocyted metal particles could also be transported to the inguinal lymph nodes as well as to distant reticuloendothelial tissues such as the liver and spleen inducing necrosis and fibrosis of these regions or to the blood stream causing systemic toxicity. The association between metallic debris and development of tumors remains controversial.5
Only few case reports and even fewer case series described early or late-onset metallosis after total knee arthroplasty. Early-onset metallosis was described by Willis-Owen and colleagues in a series of 14 patients (15 knees) within two years of total knee replacement using a cementless rotating-platform prosthesis because of two-body abrasive wear caused by femoral component modification with a beaded porous coating without direct MoM contact.7 Similarly, Vivegananthan et al. reported a case of early onset metallosis six months after TKA with the distinctive radiological signs.3 Klontz et al. reported a case of acute metallosis-related synovitis nine months after TKA.22 On the other hand, Weissman et al. reviewed the radiographs of 18 patients with metal-induced synovitis subsequent to wear of titanium (11 cases) or cobalt-chrome (5 cases) metal backed components or cobalt-chrome hinges (2 cases), years after knee arthroplasty.6 Schiavone Panni et al. also reported on four patients who underwent revision surgery because of severe metallosis after full thickness PE wear causing friction between the metal-back patellar component and the femoral shield in one case or between the femoral and tibial prosthetic metal surfaces in the remaining three cases after a mean time of 12.5 years after knee arthroplasty.5 Late-onset metallosis after 26 years of primary TKA was also described by Sharareh et al.2
Metallosis after unicondylar knee replacement is extremely rare. One case was described by Hart et al. eight years after surgery because of a break of the femoral component and was treated by a posterior stabilized TKA.26 Another case was reported by Sanchis-Alfonso 11 years after surgery because of a massive wear of the tibial PE.27 La Verde et al. described a case of catastrophic metallosis 17 years after modular prosthetic replacement of the distal femur using a tumor prosthesis after resection of a chondroblastic osteosarcoma.1
The differential diagnosis of patients presenting with painful enlarging masses of the knee joint include primary soft tissue or bone sarcomas, metastatic disease, popliteal artery aneurysms, popliteal cysts, infection, deep vein thrombosis or cellulitis.8 Imaging studies, ultrasonography and biopsy can readily differentiate these cases from wear-debris associated cysts.8 The metal-line sign helps the preoperative diagnosis of metal-induced synovitis.6 Romesburg et al. payed attention to the radiological findings indicating metal within the synovium after TKA like the “bubble sign”, the “cloud sign” and the “metal-line sign”.4 They recommended CT examination to evaluate the degree of osteolysis preoperatively. MRI is not routinely used in the metallosis workup, however, if done, it would show susceptibility artifact confirming the presence of metal within the soft tissues.28 Outpatient knee joint aspiration can exclude infection and help in the diagnosis of metallosis if dense black fluid is obtained. Scintigraphy has been shown to be sensitive for identifying a problematic joint but unhelpful in distinguishing between metallosis and infection.29
Intraoperatively, the macroscopic appearance of the knee joint with extensive black metal staining of the synovium and marked linear scratching of the femoral component is striking and unmistakable. Synovial biopsies consistently showed the typical histological features of metallosis-related synovitis. Although the real degree of associated bone loss is variable, it always exceeded what we expected to encounter when reviewing the preoperative radiographs. This may limit reconstructive options in this technically demanding revision setting. It is therefore essential for the surgeon to obtain a preoperative CT-scan of the affected joint and to have a wide armamentarium of modular revision components available during the operation in these cases that may sometimes require the implantation of a tumor prosthesis in case of advanced bone loss.
We conclude that metallosis-associated osteolysis should be suspected in cases with radiologically evident polyethylene wear after knee replacement that may allow metal-on-metal contact. Bone destruction is usually more severe than radiologically apparent. Recognizing that revision arthroplasty is very technically demanding in such cases, we recommend that surgeons should be generous in doing CT preoperatively if this complication is suspected and have a back-up with modular revision components and a ready access to reconstructive options at this revision setting.
Conflicts of interest
Nil.
References
- 1.La Verde L., Fenga D., Spinelli M.S., Campo F.R., Florio M., Rosa M.A. Catastrophic metallosis after tumoral knee prosthesis failure: a case report. Int J Surg Case Rep. 2017;30:9–12. doi: 10.1016/j.ijscr.2016.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharareh B., Phan D.L., Goreal W., Schwarzkopf R. Metallosis presenting as knee pain 26 years after primary total knee arthroplasty. J Orthop Case Rep. 2015;5(2):62–65. doi: 10.13107/jocr.2250-0685.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vivegananthan B., Shah R., Karuppiah A.S., Karuppiah S.V. Metallosis in a total knee arthroplasty. BMJ Case Rep. Mar. 2014;18 doi: 10.1136/bcr-2013-202801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Romesburg J.W., Wasserman P.L., Schoppe C.H. Metallosis and metal-induced synovitis following total knee arthroplasty: review of radiographic and CT findings. J Radiol Case Rep. 2010;4(9):7–17. doi: 10.3941/jrcr.v4i9.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schiavone Panni A., Vasso M., Cerciello S., Maccauro G. Metallosis following knee arthroplasty: histological and immunohistochemical study. Int J Immunopathol Pharmacol. 2011;24(3):711–719. doi: 10.1177/039463201102400317. [DOI] [PubMed] [Google Scholar]
- 6.Weissman B.N., Scott R.D., Brick G.W., Corson J.M. Radiographic detection of metal-induced synovitis as a complication of arthroplasty of the knee. J Bone Joint Surg Am. 1991;73(7):1002–1007. [PubMed] [Google Scholar]
- 7.Willis-Owen C.A., Keene G.C., Oakeshott R.D. Early metallosis-related failure after total knee replacement: a report of 15 cases. J Bone Joint Surg Br. 2011;93(2):205–209. doi: 10.1302/0301-620X.93B2.25150. [DOI] [PubMed] [Google Scholar]
- 8.Mavrogenis A.F., Nomikos G.N., Sakellarious V.I., Karaliotas G.I., Kontovazenitis P., Papagelopoulos P.J. Wear debris pseudotumor following total knee arthroplasty: a case report. J Med Case Rep. 2009;3:9304. doi: 10.1186/1752-1947-3-9304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huo M.H., Romness D.W., Huo S.M. Metallosis mimicking infection in a cemented total knee replacement. Orthopedics. 1997;20:466–470. doi: 10.3928/0147-7447-19970501-17. [DOI] [PubMed] [Google Scholar]
- 10.Arredondo J., Worland R.L., Jessup D.E., Angles F. Midterm results in metal-backed patella revisions for metallosis. Am J Orthop (Belle Mead NJ) 1997;26:598–600. [PubMed] [Google Scholar]
- 11.Rader C.P., Lohr H., Whittmann R., Eulert J. Results of total knee arthroplasty with a metal-backed patellar component: a 6 year follow-up study. J Arthroplast. 1996;11:923–930. doi: 10.1016/s0883-5403(96)80133-1. [DOI] [PubMed] [Google Scholar]
- 12.Matsushita I., Morita Y., Gejo R., Kimura T. Severe bone defects and reduced mineralization caused by massive metallosis after total knee arthroplasty: histopathologic and bone morphometric findings. Mod Rheumatol. 2007;17:507–510. doi: 10.1007/s10165-007-0618-3. [DOI] [PubMed] [Google Scholar]
- 13.von Ludinghausen M., Meister P., Probst J. Metallosis after osteosynthesis. Pathol Eur. 1970;5:307–314. [PubMed] [Google Scholar]
- 14.Pisanu F., Doria C., Andreozzi M. Pleomorphic clinical spectrum of metallosis in total hip arthroplasty. Int Orthop. 2019;43(1):85–96. doi: 10.1007/s00264-018-4176-4. [DOI] [PubMed] [Google Scholar]
- 15.Korovessis P., Petsinis G., Repanti M., Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty: five- to nine-year follow-up. J Bone Joint Surg Am. 2006;88(6):1183–1191. doi: 10.2106/JBJS.D.02916. [DOI] [PubMed] [Google Scholar]
- 16.Chang J.D., Lee S.S., Hur M., Seo E.M., Chung Y.K., Lee C.J. Revision total hip arthroplasty in hip joints with metallosis: a single-center experience with 31 cases. J Arthroplast. 2005;20(5):568–573. doi: 10.1016/j.arth.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Ollivere B., Darrah C., Barker T., Nolan J., Porteous M.J. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br. 2009;91(8):1025–1030. doi: 10.1302/0301-620X.91B8.21701. [DOI] [PubMed] [Google Scholar]
- 18.Khan W.S., Agarwal M., Malik A.A., Cox A.G., Denton J., Holt E.M. Chromium, cobalt and titanium metallosis involving a Nottingham shoulder replacement. J Bone Joint Surg Br. 2008;90(4):502–505. doi: 10.1302/0301-620X.90B4.20302. [DOI] [PubMed] [Google Scholar]
- 19.Degreef I., Sciot R., De Smet L. Metallosis in revision total elbow arthroplasty. Complications and staging method. Acta Orthop Belg. 2008;74:753–760. [PubMed] [Google Scholar]
- 20.Groot D., Gosens T., van Leeuwen N.C.M., Rhee M.V., Teepen H.J. Wear induced osteolysis and synovial swelling in a patient with a metal-polyethylene wrist prosthesis. J Hand Surg Am. 2006;31(10):1615–1618. doi: 10.1016/j.jhsa.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Papagelopoulos P.J., Mavrogenis A.F., Karamitros A.E., Zahos K.A., Nomikos G., Soucacos P.N. Distal leg wear debris mass from a rotating hinged knee prosthesis. J Arthroplast. 2007;22:909–915. doi: 10.1016/j.arth.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 22.Klontz K.C., Smith W.I., Jonathan C.K. Acute metallosis following total knee replacement - a case report. J Orthop Case Rep. 2014;4(1):21–23. doi: 10.13107/jocr.2250-0685.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chew F.S., Ramsdell M.G., Keel S.B. Metallosis after total knee replacement. AJR Am J Roentgenol. 1998;170(6):1556. doi: 10.2214/ajr.170.6.9609173. [DOI] [PubMed] [Google Scholar]
- 24.Mahendra G., Pandit H., Kliskey K., Murray D., Gill H.S., Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties. Acta Orthop. 2009;80(6):653–659. doi: 10.3109/17453670903473016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Niki Y., Matsumoto H., Otani T., Tomatsu T., Toyama Y. Five types of inflammatory arthritis following total knee arthroplasty. J Biomed Mater Res A. 2007;81A:1005–1010. doi: 10.1002/jbm.a.31152. [DOI] [PubMed] [Google Scholar]
- 26.Hart R., Janecek M., Bucek B. [Case report of extensive metallosis in extra-articular tissues after unicompartmental knee joint replacement] Acta Chir Orthop Traumatol Cech. 2003;70(1):47–50. (Czech) [PubMed] [Google Scholar]
- 27.Sanchis-Alfonso V. Severe metallosis after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):361–364. doi: 10.1007/s00167-006-0207-6. Epub 2006 Oct 7. [DOI] [PubMed] [Google Scholar]
- 28.Heffernan E.J., Alkubaidan F.O., Nielsen T.O., Munk P.L. The imaging appearances of metallosis. Skeletal Radiol. 2008;37:59–62. doi: 10.1007/s00256-007-0362-y. [DOI] [PubMed] [Google Scholar]
- 29.Worland R.L., Arredondo J., Angles F., Jessup D.E. Scintigraphic evaluation in total knee failure secondary to severe metallosis. J Arthroplast. 1998;13:116–119. doi: 10.1016/s0883-5403(98)90087-0. [DOI] [PubMed] [Google Scholar]