Abstract
Background
Revision of failed total hip arthroplasty (THA) presents great challenge to any orthopaedic surgeon especially in the presence of acetabular defects where the main goal is to achieve durable fixation of prosthetic components to bone which is the key to successful revision surgery.
Methods
Seventeen patients (17 hips) with mean age of 52 (40–61) years had revision surgery for aseptic failure of Furlong hydroxyapatite-ceramic-coated (HAC) prosthesis using cementless jumbo cups. Patients were reviewed clinically and radiographically with mean follow-up of 3.5 years (2–6). No patient was lost to follow up.
Results
All revised acetabular components showed polyethylene wear, severe metallosis, with acetabular defects IIB (4/17), and IIIA (13/17) according to Paprosky classification. The femoral component was well fixed in all cases but one patient had stem revision for femoral fracture mal-union. There was one early post-operative infection; there was no postoperative dislocation, sciatic nerve injury, periprosthetic fracture or deep venous thrombosis. At last follow-up, no progressive radiolucencies or acetabular migration was identified. The mean Harris hip score improved from 42 (24–59) pre-operatively to 85 (72–92).
Conclusion
Good clinical results and radiographic stability were obtained at short term follow up after acetabular revision using cementless jumbo cups, which justify its use in revision surgery even in the face of major acetabular defects. Furlong HAC femoral component gives excellent long-term survival in young and active patients with a survival rate of 94% at 18.6 years.
Keywords: Jumbo cup, Furlong, Acetabular revision, Arthroplasty
1. Introduction
Total hip arthroplasty (THA) remains the gold standard of treatment when end-stage arthritis leads to significant pain and loss of function. The aim of a hydroxyapatite-ceramic (HAC) coating, first introduced in 1985, is to facilitate the formation of a biological bond between the host bone and the implant, creating a firm cementless fixation, and the cementless Furlong prosthesis (JRI, London, UK) has produced encouraging results in primary arthroplasty.1, 2, 3, 4
Acetabular defects in failed THA cases add to the difficulties in revision surgery. Despite improvements in cementing techniques and component design, results have shown high rates of radiological loosening, especially for the acetabulum after a relatively short follow-up.5,6 Cementless revision has become more popular,7,8 as it allows direct biological contact between the implant and bone and the ability to remodel over time in order to maintain mechanical stability.9 In this prospective case series study we report on clinical and radiological results of acetabular revision for aseptic failure with acetabular deficiency using cementless jumbo cups in a consecutive series of patients who had been followed up for between two and six years. The primary prosthesis in all revised cases was cementless Furlong HAC-coated prosthesis.
2. Patients and methods
Between 2009 and 2013, seventeen hips in 17 patients (nine males, eight females), had been operated upon for a cementless revision hip arthroplasty because of failure of cementless Furlong HAC cups, the inclusion criterion followed in this study. The mean age of patients at primary arthroplasty was 38.3 years (26–48) and at revision 52 years (40–61), and the mean time to revision was 13.8 years (11–16). A prospective analysis was conducted where the Furlong acetabular component was revised in all cases (100%) using fibre metal coated cementless jumbo cup (Trilogy acetabular system, Zimmer, Warsaw, IN, USA), and the femoral component was revised in only one case (5.8%) using cementless long stem (Revitan stem, Zimmer, Warsaw, IN, USA).
Patients were reviewed in the outpatient clinic at two weeks, six weeks, three months, six months and 12 months, then on annual basis. Harris Hip Score (HHS)10 was recorded pre-operatively then at six and 12 months postoperatively, and at every year with mean follow up 3.5 years (2–6 years).
The pre-operative radiographs were evaluated for bony deficiencies of the acetabulum using Paprosky classification11 which may be modified according to operative findings. Radiological evaluation included anteroposterior (AP) and lateral radiographs taken immediately post-operatively, at six weeks, 3 months, 6 months, 12 months, then on annual basis. Final post-operative radiographs were analysed for bony ingrowth and cup-bone radiolucencies in the zones of DeLee and Charnley.12 Acetabular inclination was measured on the AP radiograph as well as vertical and horizontal cup position in relation to the inter teardrop line and Kohler line to detect any change during the follow up. Definite loosening of the acetabular component was diagnosed if there was a change in its position (>2 mm vertically and/or horizontally) or a continuous radiolucent line wider than 2 mm on the AP radiograph.13,14 To adjust all the measurements for magnification, the ratio of the actual and measured widths of the femoral head was calculated for each radiograph, and used as a co-efficient. The fixation and stability of the femoral component were assessed using the criteria described by Engh.15,16 Definite loosening of the femoral component was defined as a progressive axial subsidence of >3 mm.14
2.1. Operative technique
A posterolateral approach was used in all cases. After removing the loose acetabular components, meticulous debridement was performed to remove the lining membrane and the black coloured tissues of metallosis from the socket aided by pulsatile lavage to expose healthy bone. We used Paprosky classification11 based on the pre-operative X-ray appearance but later modified this in the light of the operative findings, where four patients had type IIB, and thirteen patients had type IIIA acetabular defects. Careful reaming was used to expand, freshen, and shape the peripheral rim and the dome of the socket. Particulate bone grafting from the iliac crest was used to fill remaining cavitary defects after reaming of the socket. The trial prosthesis was inserted to assess the appropriate size, ability of the acetabular rim to take load, aiming for covering at least half of the circumference of the acetabulum, & at least 50% of host bone contact. The Trilogy multi-hole cups (coated with commercially pure titanium fibre metal) were impacted into the reamed bed and screws were used to complete the fixation. Highly Cross linked Polyethylene liners (Longevity, Zimmer, Warsaw, IN, USA) were used in all the acetabular components. The femoral component was revised in only one hip due to mal-united femoral fracture at the tip of the stem. An oblique femoral osteotomy was performed just below the tip of the stem, and the stem was extracted by back hammering using stem extractor. To facilitate extraction, the bone bridges resulted from osseointegration between the Furlong stem & femur were broken using osteotomes through the osteotomy performed. The mal-union was corrected and the femur was prepared for insertion of cementless long stem (Revitan stem, Zimmer, Warsaw, IN, USA) to bypass the osteotomy level. A 28 mm cobalt-chrome head was used in 5 cases, and 32 mm head in 12 cases.
Patients received low molecular weight heparin for 5 weeks for prophylaxis against deep venous thrombosis, and toe touch weight bearing was allowed with the aid of a walking frame for the first 6 weeks then increase progressively over the next 6 weeks. The mean follow-up period was 3.5 years (2–6) and no patient was lost to follow-up.
3. Results
Seventeen hips in 17 patients, with mean age 52 years (40–61), were operated upon. The mean follow-up period was 3.5 years (2–6). No patient was lost to follow-up. The indication for revision surgery was symptomatic aseptic loosening of the acetabular component in all cases. Intra-operative assessment of acetabular deficiency confirmed the preoperative radiological assessment, with 4 patients (23.5%) had type IIB, and 13 patients (76.5%) had IIIA acetabular defects according to Paprosky classification. Cementless jumbo cups with an outer diameter larger than 60 mm were used in all cases. Intra-operatively, all femoral stems were found to be rigidly fixed and stable. Only one case (5.8%) had revision of the femoral component, combined with femoral osteotomy to correct mal-united fracture femur, which progressed to union within 6 months. There was one postoperative infection (5.9%). (Table 1).
Table 1.
Complications.
| Complication | Total |
|---|---|
| Infection | 1 |
| Dislocation | 0 |
| Sciatic nerve palsy | 0 |
| Aseptic loosening | 0 |
| Deep venous thrombosis | 0 |
| Periprosthetic fracture | 0 |
| Re-revision | 0 |
Mean leg length discrepancy (LLD) improved from 2.6 cm (2–3) preoperatively to 0.1 cm (0–0.5) postoperatively. Fourteen patients (82%) had a good or excellent result with a Harris hip score of >79 points. Mean HHS improved from 42 (24–59) pre-operatively to 85 (72–92) at last follow-up (Table 2).
Table 2.
Demography, LLD, and HHS of the study group.
| No | Sex | Age at revision | Time since index operation (Y) | Preop LLD (cm) | Postop LLD (cm) | FU in Y after revision | Preop HHS | HHS at last FU | Acetabular defect (Paprosky class) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 43 | 12 | 2 | 0 | 6 | 57 | 92 | IIIA |
| 2 | M | 40 | 14 | 3 | 0 | 2 | 31 | 72 | IIIA |
| 3 | M | 46 | 12 | 3 | 0 | 5 | 24 | 72 | IIIA |
| 4 | F | 59 | 15 | 3 | 0 | 3.5 | 33 | 87 | IIIA |
| 5 | F | 47 | 12 | 2 | 0 | 4 | 54 | 90 | IIIA |
| 6 | F | 55 | 14 | 3 | 0 | 3.2 | 56 | 86 | IIIA |
| 7 | M | 47 | 15 | 2 | 0 | 2 | 29 | 76 | IIB |
| 8 | F | 57 | 14 | 3 | 0.5 | 4 | 33 | 83 | IIIA |
| 9 | M | 51 | 13 | 3 | 0 | 3 | 35 | 87 | IIIA |
| 10 | F | 53 | 16 | 3 | 0 | 3 | 53 | 90 | IIB |
| 11 | F | 46 | 11 | 2 | 0.5 | 4 | 31 | 87 | IIIA |
| 12 | M | 56 | 14 | 2 | 0 | 3.5 | 35 | 88 | IIIA |
| 13 | M | 55 | 13 | 2.5 | 0 | 3.25 | 57 | 90 | IIB |
| 14 | M | 60 | 15 | 3 | 0 | 3 | 59 | 90 | IIIA |
| 15 | M | 52 | 15 | 3 | 0 | 3.5 | 35 | 86 | IIIA |
| 16 | F | 57 | 16 | 2 | 0 | 2 | 57 | 87 | IIB |
| 17 | M | 61 | 13 | 2.5 | 0 | 4 | 33 | 81 | IIIA |
No case in this study required re-revision of either component for any cause, and none were considered loose radiographically at last follow-up.
4. Discussion
The revision of failed acetabular components in the presence of acetabular deficiency presents a formidable problem and challenging scenario encountered by the arthroplasty surgeon because it is often accompanied by varying degrees of osteolysis, bone loss, and sclerosis of the remaining bone. Flugsrud showed that patients who undertake intermediate to intense activity are four times more likely than the less-active to develop acetabular prosthesis loosening.17
Different treatment strategies have been described to deal with acetabular defects. These include cemented components with impacted bone graft,18,19 porous-coated cementless implants,20,21 anti-protrusio rings and cages,22,23 custom implants,24,25 and porous tantalum (trabecular metal) acetabular system.26,27
Successful acetabular revision with cementless cups is achieved by gaining sufficient cup contact against biologically active and mechanically supportive acetabular bone to provide initial stability till osseointegration takes place aiming for long-term biologic fixation. When little bone loss is present (Paprosky types I, IIA and IIB), these goals can be achieved by conventional hemispherical cup at the normal hip centre. However, with severe bone loss (Paprosky IIIA, IIIB), conventional cups cannot satisfy these goals, and other methods must be employed to position the cup against sufficient host bone if cementless cups are to be used for revision. The two main options to achieve these goals are either to place the cup in a superior position (high hip centre),28,29 or to use a larger cup (Jumbo cup).30, 31, 32, 33
Jumbo cup, a cup with an extra-large diameter, following bone grafting for focal defects can be used to gain increased cup surface area of contact with host bone in acetabular revision surgery which plays an important role in determining the success of cementless acetabular fixation.34,35 There is no universally-accepted definition of what diameter defined the jumbo cup. Whaley et al. used a diameter of 66 mm in males and 62 in females in recognition of the inherent differences in average pelvic dimensions between the sexes.36 Jumbo cups are loosely defined by the ratio of component size to the pelvis and the hip joint, as compared to the size of the original implant.37
Favourable results for jumbo cups have been reported. Patel et al. reported on 43 jumbo cups followed a minimum of 5 years, only two hips were re-revised for acetabular loosening, and shell survival at 14 years was 92%, with only 2 hips (4.6%) dislocated.38 Lachiewicz & Soileau reported low rates of loosening and infection after revision THA using jumbo cups and high survival at fifteen years.39 In a more recent publication Von Roth et al. found the twenty-year results of revision with uncemented jumbo acetabular components demonstrated acceptable clinical outcomes and radiographic stability.40
Jumbo cups also have some disadvantages: more host bone is sacrificed in shaping the acetabulum to accept a large cup, which may compromise bone stock for further revision, large cups can impinge against nearby soft tissue structures, particularly the iliopsoas tendon. A large mismatch between a large shell and a small femoral head may increase the rate of impingement and reduce the soft tissue constraints, making dislocation one of the most common complications reported in some studies.36,39
The aim of this study was to report the short to midterm results of Jumbo cup for revision of acetabular defects in a consecutive series of patients with aseptic failure of cementless prosthesis. A common feature among patients in this study that the primary THA which was revised in all cases was Furlong HAC prosthesis, and the revision implant used was fibre metal coated cementless acetabular component, with an outer diameter larger than 60 mm.
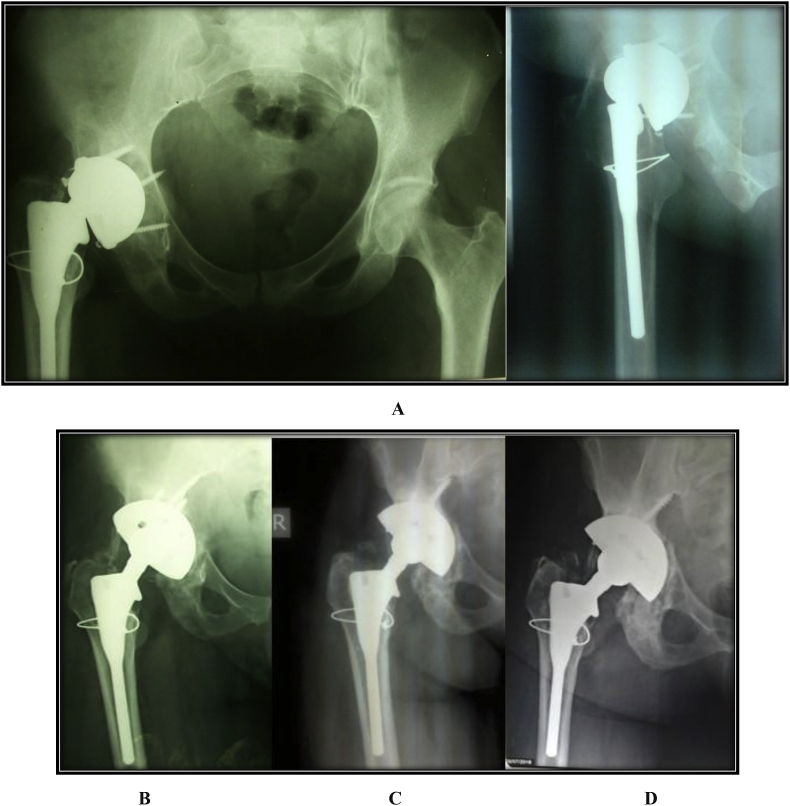
In this series, all patients had acetabular defects ranging from Type IIB and Type IIIA according to Paprosky classification. The acetabular components were found to be loose with broken screws in 11 hips, severe metallosis and polyethylene wear were common features in all cases (Fig. 1).
Fig. 1.
A Severe metallosis and B. severe polyethylene wear were common features encountered in all cases.
No patient was lost to follow-up in this series. Although high rate of dislocation was reported in revision THA with the use of jumbo cups36,39 there was no dislocation in our series, which may be attributed to the use of 32 mm head in most cases (12/17, 71%). One case (5.9%) had early postoperative infection, and was managed by early debridement, antibiotics, and retention of the prosthesis. No case showed radiological signs of loosening or cup migration, and no case required re-revision of the cup for any reason at last follow-up. The final mean Harris hip score was 85 with 82% had a good or excellent result. In this study, we found the survival free of revision for any reason of Jumbo cups, used for acetabular revision in presence of major bone defects, at 3.5 years was 100% (Fig. 2).
Fig. 2.
A. Pre-operative radiographs of a 43-years-old female patient with failed Furlong acetabular component with type IIIA acetabular defect; B. Postoperative radiographs after 3 months C. after 3 years; D. last follow-up after 6 years with no signs of loosening or cup migration, with HHS improved to 92.
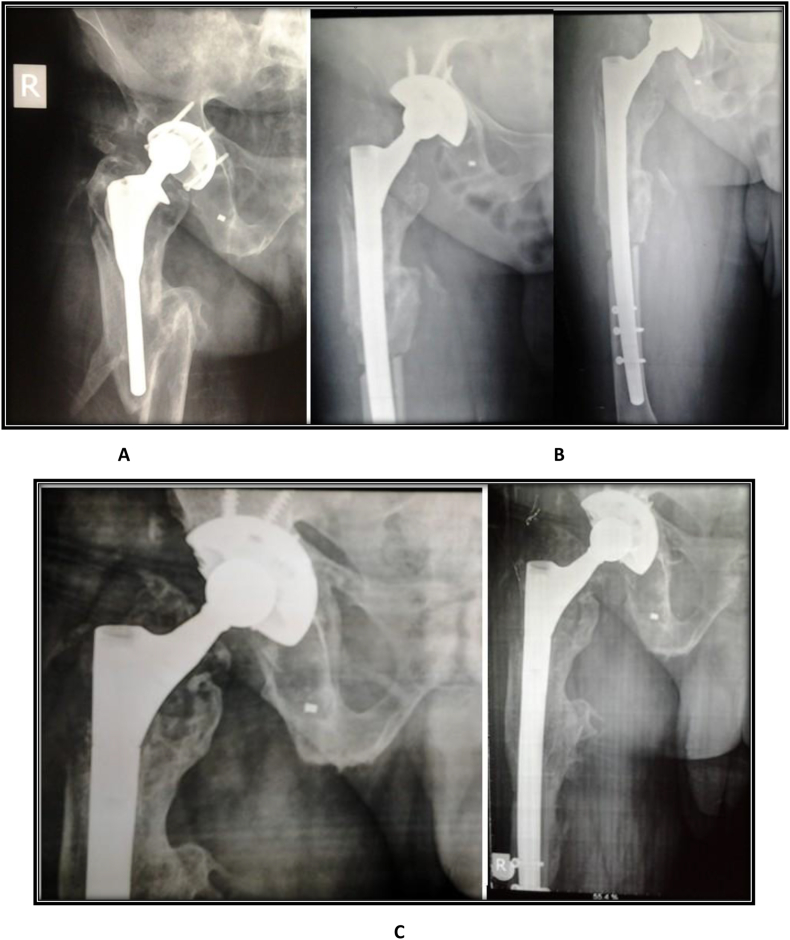
Furlong HAC femoral stem that was used in the index operation was rigidly fixed in all patients at time of revision, and none needed revision for aseptic loosening. Only one case required revision of the femoral stem because of mal-union of femoral fracture that necessitated femoral osteotomy and revision with cementless long stem, with complete union of the osteotomy 6 months postoperatively (Fig. 3).
Fig. 3.
A. Pre-operative anteroposterior (AP) radiograph of hip in 47-year-old man with Ankylosing Spondylitis had failed Furlong cup and mal-union fracture shaft femur; B. immediate post-operative radiographs; C. last follow-up after 2.5 years with stable cup, no signs of loosening, and fully united femur at the corrective osteotomy site, with HHS improved from 29 to 76.
All non-revised stems met radiological stability criteria of biologic fixation of cementless femoral components as described by Engh et al.15 at last follow up. In this study, the survival of the Furlong femoral stem at 18.6 years with revision for any reason as the endpoint was 94%, and survival with aseptic loosening of the stem as the endpoint was 100%. Many studies reported excellent results of using Furlong HAC femoral component in young and active patients with long-term survival ranging from 94.29% to 100%2,4
Our study has some limitations; the number of patients was relatively small due to the inclusion criterion selected for the patients in the study, and longer-term follow-up is required.
5. Conclusion
In this series, we reported satisfactory short to midterm results with use of jumbo cups in revision arthroplasty with acetabular defects of types IIB & IIIA according to Paprosky's classification. These results support the use of jumbo cups even in the face of major acetabular defects, and presents the method as one of armamentarium to be considered by surgeons dealing with such challenging cases. The Furlong HAC femoral component provides excellent clinical and radiologic results at long term follow up.
Contributor Information
Ahmed Salem Eid, Email: ahmedsalem5474@yahoo.com.
Ahmed Kotb, Email: drakotb@live.com.
Waleed Elshabrawy, Email: waleedortho@gmail.com.
References
- 1.Rajaratnam S.S.1, Jack C., Tavakkolizadeh A. Long-term results of a hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-year follow-up study. J Bone Joint Surg Br. 2008;90(1):27–30. doi: 10.1302/0301-620X.90B1.19731. [DOI] [PubMed] [Google Scholar]
- 2.Shah N.N.1, Edge A.J., Clark D.W. Hydroxyapatite-ceramic-coated femoral components in young patients followed-up for 16 to 19 years: an update of a previous report. J Bone Joint Surg Br. 2009;91(7):865–869. doi: 10.1302/0301-620X.91B7.22311. [DOI] [PubMed] [Google Scholar]
- 3.Sandiford N.1, Doctor C., Rajaratnam S.S. Primary total hip replacement with a Furlong fully hydroxyapatite-coated titanium alloy femoral component: results at a minimum follow-up of 20 years. Bone Joint Lett J. 2013;95(4):467–471. doi: 10.1302/0301-620X.95B4.30445. [DOI] [PubMed] [Google Scholar]
- 4.Gabbar O.A.1, Rajan R.A., Londhe S., Hyde I.D. Ten- to twelve-year follow-up of the furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in patients younger than 65 years. J Arthroplasty. 2008;23(3):413–417. doi: 10.1016/j.arth.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 5.Katz R.P., Callaghan J.J., Sullivan P.M., Johnston R.C. Results of cemented femoral revision total hip arthroplasty using improved cementing techniques. Clin Orthop Relat Res. 1995;319:178–183. [PubMed] [Google Scholar]
- 6.Elting J.J., Mikhail W.E., Zicat B.A. Preliminary report of impaction grafting for exchange femoral arthroplasty. Clin Orthop Relat Res. 1995;319:159–167. [PubMed] [Google Scholar]
- 7.Emerson R.H., Jr., Head W.C., Higgins L.L. Clinical and radiographic analysis of the Mallory-Head femoral component in revision total hip arthroplasty: a minimum 8.8- year and average eleven-year follow-up study. J Bone Joint Surg [Am] 2003;85-A:1921–1926. doi: 10.2106/00004623-200310000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Templeton J.E., Callaghan J.J., Goetz D.D., Sullivan P.M., Johnston R.C. Revision of a cemented acetabular component to a cementless acetabular component: a ten to fourteen-year follow-up study. J Bone Joint Surg [Am] 2001;83-A:1706–1711. doi: 10.2106/00004623-200111000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Soballe K., Hansen E.S., Brockstedt-Rasmussen H., Bunger C. Hydroxyapatite coating converts fibrous tissue to bone around loaded implants. J Bone Joint Surg [Br] 1993;75-B:270–278. doi: 10.1302/0301-620X.75B2.8444949. [DOI] [PubMed] [Google Scholar]
- 10.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. J Bone Joint Surg [Am] 1969;51-A:737–755. [PubMed] [Google Scholar]
- 11.Paprosky W.G., Perona P.G., Lawrence J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9(1):33–44. doi: 10.1016/0883-5403(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 12.DeLee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 13.Massin P., Schmidt L., Engh C.A. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/s0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 14.Kim Y.H., Kim V.E. Uncemented porous-coated anatomic total hip replacement: results at six years in a consecutive series. J Bone Joint Surg [Br] 1993;75-B:6–13. doi: 10.1302/0301-620X.75B1.8421036. [DOI] [PubMed] [Google Scholar]
- 15.Engh C.A., Massin P., Suthers K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 16.Engh C.A., Bobyn J.D., Glassman A.H. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg [Br] 1987;69-B:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 17.Flugsrud G.B., Nrdsletten L., Espenhaug B., Havelin L.I., Meyer H.E. The effect of middle-age body weight and physical activity on the risk of early revision hip arthroplasty: a cohort study of 1,535 individuals. Acta Orthop. 2007;78(1):99–107. doi: 10.1080/17453670610013493. [DOI] [PubMed] [Google Scholar]
- 18.Boldt J.G., Dilawari P., Agarwal S. Revision total hip arthroplasty using impaction bone grafting with cemented non-polished stems and Charnley cups. J Arthroplasty. 1997;12:403–415. doi: 10.1054/arth.2001.25559. [DOI] [PubMed] [Google Scholar]
- 19.Sporer S.M., O'Rourke, Chong P. The use of structural distal femoral allografts for acetabular reconstruction: average 10-year follow-up. J Bone Joint Surg. 2005;87A:760–765. doi: 10.2106/JBJS.D.02099. [DOI] [PubMed] [Google Scholar]
- 20.Hallstrom B.R., Golladay G.J., Vittetoe D.A. Cementless acetabular revision with the Harris- Gallante porous prosthesis: results after a minimum of ten years of follow-up. J Bone Joint Surg. 2004;86A:1007–1011. doi: 10.2106/00004623-200405000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Park D.K., Della Valle C.J., Quigley L., Moric M., Rosenberg A.G., Galante J.O. Revision of the acetabular component without cement. A concise follow-up, at twenty to twenty-four years, of a previous report. J Bone Joint Surg [Am] 2009;91(2):350–355. doi: 10.2106/JBJS.H.00302. Erratum in: J Bone Joint Surg Am. 2009 Dec; 91(12):2931. [DOI] [PubMed] [Google Scholar]
- 22.Gill T.J., Sledge J.B., Muller M.E. The Burch-Schneider anti-protrusio cages in revision total hip arthroplasty. J Bone Joint Surg. 1998;80B:946–953. doi: 10.1302/0301-620x.80b6.8658. [DOI] [PubMed] [Google Scholar]
- 23.Berry D.J. Antiprotrusio cages for acetabular revision. Clin Orthop Relat Res. 2004;420:106–112. doi: 10.1097/00003086-200403000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Dennis D.A. Management of massive acetabular defects in revision total hip arthroplasty. J Arthroplasty. 2003;18(3 Suppl 1):121–125. doi: 10.1054/arth.2003.50105. [DOI] [PubMed] [Google Scholar]
- 25.DeBoer D.K., Christie M.J., Brinson M.F., Morrison J.C. Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg [Am] 2007;89(4):835–840. doi: 10.2106/JBJS.F.00313. [DOI] [PubMed] [Google Scholar]
- 26.Skyttä E.T., Eskelinen A., Paavolainen P.O., Remes V.M. Early results of 827 trabecular metal revision shells in acetabular revision. J Arthroplasty. 2011;26:342–345. doi: 10.1016/j.arth.2010.01.106. [DOI] [PubMed] [Google Scholar]
- 27.Davies J.H., Laflamme G.Y., Delisle J., Fernandes J. Trabecular metal used for major bone loss in acetabular hip revision. J Arthroplasty. 2011;26(8):1245–1250. doi: 10.1016/j.arth.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 28.Harris W.H. Reconstruction at a high hip centre in acetabular revision surgery using a cementless acetabular component. Orthopaedics. 1998;21:991–992. doi: 10.3928/0147-7447-19980901-17. [DOI] [PubMed] [Google Scholar]
- 29.Hendricks K.J., Harris W.H. High placement of noncemented acetabular components in revision total hip arthroplasty. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg [Am] 2006;88:2231–2236. doi: 10.2106/JBJS.E.00247. [DOI] [PubMed] [Google Scholar]
- 30.Emerson R.H., Head W.C. Dealing with the deficient acetabulum in revision hip arthroplasty: the importance of implant migration and use of the jumbo cup. Semin Arthroplasty. 1993;4:2–8. [PubMed] [Google Scholar]
- 31.Jasty M. Jumbo cups and morselized graft. Orthop Clin N Am. 1998;29:249–254. doi: 10.1016/s0030-5898(05)70323-0. [DOI] [PubMed] [Google Scholar]
- 32.Dearborn J.T., Harris W.H. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow up study. J Arthroplasty. 2000;15:8–15. doi: 10.1016/s0883-5403(00)90999-9. [DOI] [PubMed] [Google Scholar]
- 33.Wedemeyer C., Neuerburg C., Heep H. Jumbo cups for revision of acetabular defects after total hip arthroplasty: a retrospective review of a case series. Arch Orthop Trauma Surg. 2008;128:545–550. doi: 10.1007/s00402-007-0501-x. [DOI] [PubMed] [Google Scholar]
- 34.Dearborn J.T., Harris W.H. High placement of an acetabular component inserted without cement in a revision total hip arthroplasty: results after a mean of ten years. J Bone Joint Surg. 1999;81A:469–480. doi: 10.2106/00004623-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Kwong L.M., O'Conner D.O., Sedlacek R.C., Krushell R.J., Maloney W.J., Harris W.H. A quantitative in vitro assessment of fit and screw fixation on the stability of the cementless hemispherical acetabular component. J Arthroplasty. 1994;9:163–170. doi: 10.1016/0883-5403(94)90065-5. [DOI] [PubMed] [Google Scholar]
- 36.Whaley A.L., Berry D.J., Harmsen W.S. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg. 2001;83A:1352–1357. doi: 10.2106/00004623-200109000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Ito H., Matsuno T., Aoki Y., Minami A. Acetabular components without bulk bone graft in revision surgery: a 5- to 13-year follow-up study. J Arthroplasty. 2003;18:134–139. doi: 10.1054/arth.2003.50029. [DOI] [PubMed] [Google Scholar]
- 38.Patel J.V., Masonis J.L., Bourne R.B. The fate of cementless jumbo cups in revision hip arthroplasty. J Arthroplasty. 2003;18:129–133. doi: 10.1054/arth.2003.50038. [DOI] [PubMed] [Google Scholar]
- 39.Lachiewicz P.F.1, Soileau E.S. Fixation, survival, and dislocation of jumbo acetabular components in revision hip arthroplasty. J Bone Joint Surg [Am] 2013;95(6):543–548. doi: 10.2106/JBJS.L.00758. [DOI] [PubMed] [Google Scholar]
- 40.Von Roth P., Abdel M.P., Harmsen W.S., Berry D.J. Uncemented jumbo cups for revision total hip arthroplasty: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg [Am] 2015;97(4):284–287. doi: 10.2106/JBJS.N.00798. [DOI] [PubMed] [Google Scholar]