Abstract
Proximal femoral fracture in an ankylosed hip is a challenging condition. There is no consensus on fixation method for these fractures. In addition, despite union the best outcome possible is the restoration of the pre morbid status. We report two different presentations of proximal femoral fracture in ankylosed hip that were successfully treated with primary total hip arthroplasty. We also discuss the surgical principles, technique and advantages of doing primary total hip arthroplasty in such cases.
1. Introduction
Proximal femoral fracture in an ankylosed hip is a challenging presentation for orthopedic surgeons. Selection of the appropriate treatment method is daunting, as the hip joint is immobile. Very few cases of proximal femoral fractures in ankylosed hip joints have been reported in the past. Furthermore, these reports have failed to recommend a consensus method of management.1, 2, 3, 4, 5, 6, 7 On the other hand, despite successful union with osteosynthesis by all the methods described, best outcome possible is the restoration of the pre morbid status with persistent disability. Hip ankylosis is a disabling entity, which also affects the adjacent joints by altering their biomechanics. This leads to backache and pain in ipsilateral knee as well as contralateral hip and knee.8, 9, 10
With advances in modern orthopedics and enhanced patient expectations, the goal of treatment has changed. There have been successful results of total hip arthroplasty in ankylosed hips that dramatically improve the quality of life with high patient satisfaction.11, 12, 13, 14, 15, 16 We herein present two rare cases with proximal femoral fractures in previously ankylosed hips, which were successfully treated with primary total hip arthroplasty. We also discuss the surgical principles, technique of dealing with the fracture as well as ankylosis of hip and the advantages of primary total hip arthroplasty in such presentation.
2. Case 1
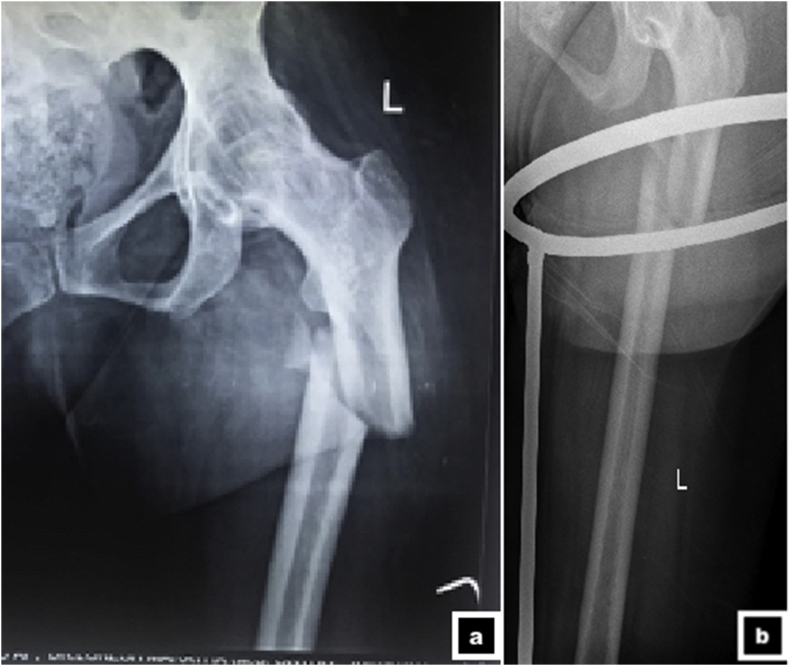
A 68 year old male patient with a history of fixation for proximal femur fracture done elsewhere in a surgically arthrodesed right hip presented to us with fixation failure, six months after the surgery (Fig. 1 A & B). The patient was counselled and planned for primary total hip arthroplasty with a long stem so as to simultaneously stabilize the fracture as well as give mobility to the joint. The surgery was performed via posterior approach. The distal end of the incision was extended to expose the implant in its whole length. The failed hardware (Dynamic Condylar Screw Plate and screws) were removed. Protecting the abductors, the femoral neck was carefully exposed. Femoral neck osteotomy was completed after removing a wedge (Napkin ring) of bone from the neck prior to osteotomy. The fracture was reduced and held in position with the help of reduction clamp. With the reduction held in position, the femoral stem preparation was done with the reamers provided for Wagner® stem (Zimmer-Biomet, Warsaw, IN). With femoral trial in situ, the femur was pushed anteriorly to expose the acetabulum. The gluteus minimus and reflected head of rectus femoris was incised to push the proximal femur further anteriorly. This gave the 360° view of the acetabulum. Acetabular preparation was done using the successive reamers after accessing the floor of the acetabulum with the smallest reamer. Regenerex cup® (Zimmer-Biomet, Warsaw, IN) was implanted. A trial reduction was done with trial stem in situ to check for the stability of the joint. Definitive stem was implanted and the stainless steel wires were passed around the trochanter to provide additional stability and securing the abductors to the construct.
Fig. 1.
a - b. Radiograph showing failed osteosynthesis for proximal femoral fracture in an arthrodesed hip in antero-posterior view (a) lateral view (b). Note the breakage of implant as well, which implies excessive stress over the fracture site due to ipsilateral fused hip. c - e. Serial radiographs after total hip arthroplasty at immediate post-operative period (a) at one month (b) at 6 months (c). Note the stable total hip prosthesis in situ showing total hip arthroplasty prosthesis in situ and healing of the fracture.
Patient was mobilized with toe touch weight bearing in an abduction brace for the first 6 weeks followed by full weight bearing. The patient was observed closely with bi-monthly follow up. The fracture showed good union on subsequent follow-up at 6 months (Fig. 1C to E). However, the patient developed cervical myelopathy due to cervical spondylosis with cervical cord comression for which he underwent posterior laminoplasty and decompression. He is currently walking full weight bearing with walker and has mostly recovered from the cervical myelopathy. The recent radiographs showed union of the fracture with stable implants in situ.
3. Case 2
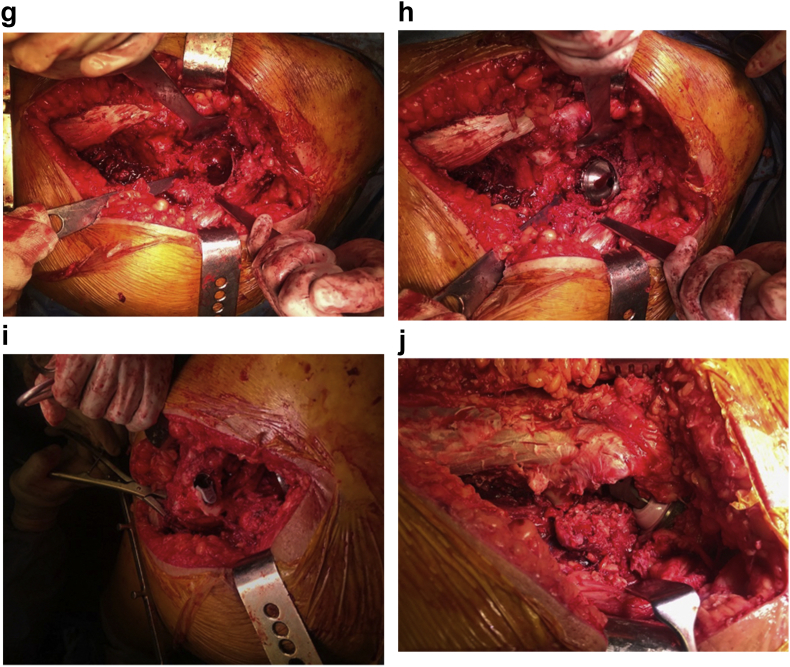
A 42-year-old diabetic and hypertensive female, known case of Ankylosing Spondylitis, sustained a fracture of the proximal femur in her ankylosed left hip following a road traffic accident (Fig. 2 A & B). The patient had a failed total hip prosthesis (failed femoral stem) in her right hip done seven years back. As the patient was crippled due to fracture, the treatment goal was to make the patient mobile as early as possible. With an experience of facing a failed osteosyntheis in an ankylosed hip, the patient was counselled for acute total hip arthroplasty. The patient was placed in lateral position and the femoral neck exposed via posterior approach (Fig. 2C). In-situ cut of the femoral neck was undertaken and the fracture site was temporarily reduced and held in that position (Fig. 2D). A modular stem was planned using S-ROM® (Depuy Synthes, Warsaw IN) system and the preparation were done for the sleeve and the stem accordingly (Fig. 2E). Acetabular preparation was done for the Gription coated pinnacle cup® (Depuy Synthes, Warsaw, IN) (Fig. 2 F, G, H). Trial stem was placed first to assess the fracture as well as hip joint stability followed by implantation of the definitive implants (Fig. 2 I &J).
Fig. 2.
a - b. Radiograph showing sub-trochanteric fracture in an ankylosed left hip in antero-posterior view (a) oblique view (b). 2 c. Intra-operative picture showing posterior approach to the hip joint with exposure of proximal femur and femoral neck. Note the narrow access to the neck due to ankylosed hip. d. Intra-operative picture showing insitu femoral neck osteotomy. e. Intra-operative picture showing femoral preparation. The fracture is being provisionally stabilized over the canal reamer. f. Intra-operative picture showing acetabular preparation. The first reamer should be the smallest reamer to identify the floor of the acetabulum. g. Intra-operative picture showing the finally prepared acetabular bed prior to final cup placement. h Intra-operative picture showing final placement of acetabular cup. I Intra-operative picture showing placement of the final sleeve of a modular prosthesis (SROM®, Depuy Orthopedics, Warsaw, IN). j Intra-operative picture showing final reduction of the joint prior to closure. k - m. Serial radiographs after acute total hip arthroplasty at 6 weeks (a) at 3 months (b), and at 6 months (c). Note the stable total hip prosthesis in situ and union of the fracture.
The patient was mobilized with full weight bearing on the next day of the surgery. Three months later, she underwent revision surgery for her right failed THA. At the latest follow up of one year, the fracture is united with stable implants in both hips (Fig. 2 K,L,M). The patient has good function with reasonable mobility at the hip joint to carry out her activities of daily living.
4. Discussion
Ankylosis of hip not only keeps the joint immobile but also alters the biomechanics of the adjacent joints, including ipsilateral knee, contralateral hip and knee, and the spine resulting in pain and decreased functional capacity in the later stages of life.1,2 These patients may present with a wide range of etiologies including inflammatory pathology, infection or surgically done arthrodesis.
Proximal femoral fractures in ankylosed hips are attributed to osteoporosis due to disuse atrophy and the primary inflammatory pathology when responsible. Abnormal stresses subjected to the femur, due the fixed hip joint with a higher lever arm than usual, may lead to an easy fracture in an already weak femur. Management of proximal femoral fracture in an ankylosed hip poses tremendous challenge to the orthopedic surgeons. An immobile hip may render the patient immobile due to the fracture. There is paucity of literature regarding the treatment options for such condition. Different treatment methods have been reported in the past including nails,1,2,5,7 plates,4 screws6 and historically even traction.3 However, despite union the best outcome was restoration of the pre morbid status. With high patient demand and successful results of total hip arthroplasty in ankylosed hips, our case presentation is one step ahead and advocates simultaneous solution to the dual problem by performing primary total hip arthroplasty which ultimately take cares of fracture as well as the ankylosis of hip.
The first patient had failed osteosynthesis as the joint was immobile and all the stresses concentrated at the fracture site. This led to non-union and eventual hardware breakage. Removal of the broken implants and total hip arthroplasty allowed early weight bearing, mobility to the patient and union of the fracture. This improved the quality of life as well.
We performed acute total hip arthroplasty in second patient to obviate the intermediate complications of fixation seen in the first case. Performing acute THA gives joint mobility, and reduces the morbidity and the recovery period, while taking care of both the fracture and ankylosis simultaneously. The outcome was excellent with high patient satisfaction. Hence, total hip arthroplasty not only provided early mobilization but also a mobile hip and better quality of life.10
A thorough literature search revealed 8 cases of femoral fractures with ipsilateral ankylosed/arthrodesed hip joints of which six of them were for proximal femur fractures. A brief description of the cases reported is summarized in Table 1. Retrograde nailing was described to fix shaft fracture as well as sub-trochanteric fractures, which provide a stable fixation with early mobilization of the patients, but the quality of life remained as it was before.1,2,7 Most authors, irrespective of the method used for fixation, have described difficulty in aligning the distal fragment with the immobile proximal fragment thus leading to difficult reduction. The outcomes of all authors have been satisfactory at best with high incidence of delayed union and prolonged use of walking aid following surgery. The patients, despite a long rehabilitation are hardly able to make it to their pre-injury state thus disabling them for life.2,5,7
Table 1.
A concise data review of all cases of proximal femoral fractures and their reported management.
| Author/Journal | Age/Gender of the patient | Site of fracture | Treatment | Outcome |
|---|---|---|---|---|
| Lonner et al. JOT 1995 |
NS | Sub-trochanteric | Retrograde nailing | Return to pre-injury status at 1 year |
| Wulke et al. JOT 2004 |
86/F | Fracture neck of femur | Retrograde nailing | Fracture union at 3 Months |
| Manzotti et al. JBJS 2007 |
74/F | Sub-trochanteric | Plating | Union but with 4 cm shortening |
| Font Vizcarra et al. Hip Int 2010 |
68/F | Intertrochanteric fracture | Cannulated Cancellous Screws | Good Function at 1 year |
| Ishimaru et al. Case Rep Orthop 2012 |
76/M | Intertrochanteric fracture | Gamma nail | Fracture union with walking with support at 1 year |
| Current study | Failed osteosynthesis for Intertrochanteric fracture | THA | Immediate mobilization, Fracture united at 3 months | |
| Sub-trochanteric fracture | THA | Immediate mobilization, Fracture united at 3 months |
M = Male, F= Female, NS= Not Specified, THA = Total Hip Arthroplasty.
Total Hip Arthroplasty for an ankylosed hip, however is also associated with a high risk of perioperative complications, including blood loss, nerve injuries and hip instability.15 Apart from the high risk of complications total hip arthroplasty in ankylosed hips is also technically demanding requiring special attention to hip abductor muscles, accurate identification of hip rotation center, achieving appropriate medialization and sizing of the component, optimizing cup placement with leg length equalization, and restoring ideal femoral offsets to avoid impingement and instability.12,17,18 The authors recommend a conical stem for intertrochanteric fractures and a modular stem for sub trochanteric fractures, which takes care of the femoral anteversion and also helps to adjust the combined anteversion in a fixed acetabular shell.
The option of total hip arthroplasty has not been explored well in such conditions and there is no description of the same in the literature. Following the in-situ neck cut in total hip arthroplasty, reduction of the fracture is also easier intra-operatively than conventional techniques of open or closed reduction where a long lever arm created by the fused hip makes reduction challenging.1,3 Total hip arthroplasty in ankylosed hip has been shown to provide improvement of pain in the adjacent joints and in the lower back and provide stable and mobile hip joint.10,11,14
5. Surgical tips
The authors’ recommend following surgical tips while dealing with proximal femoral fracture in ankylosed hip:
-
1.
Posterior approach used with most complex primary hip replacements/revisions would be a better approach. Extending the distal end of incision will help in exposing the fracture site.
-
2.
Protecting the abductor, expose the femoral neck and perform femoral neck osteotomy after removing a wedge (Napkin ring) of bone from the neck prior to osteotomy. Prior neck osteotomy helps in reducing the fracture easily with a short proximal fragment than the conventional techniques of open or closed reduction where a long lever arm created by the fused hip makes reduction challenging.
-
3.
The femoral preparation can be done separately for the proximal and distal fragments, or at a time depending on the choice of implant. For a modular prostheis, the preparation can be done separately, while for a conical long stem, the preparation can be done at a time just like in primary THA with the reduction of fracture held in position with reduction clamp. However, the authors recommend a modular stem in such cases.
-
4.
With trial stem in situ, the proximal femur can be pushed anteriorly. Protecting the gluteus medius, the gluteus minimus and refelcted head of rectus femoris can be incised to ease the mobilization of proximal femur anteriorly for better exposure of the acetabulum in its 360° view.
-
5.
Acetabular preparation should be started with smallest reamer first to access the floor of the acetabulum (soft tisue at the bed), and then with successive reamers to a planned size.
-
6.
A trial reduction with the trail stem should be done before final implantation to check for the stability of joint as well as the stability of fracture.
6. Summary
Mere osteosynthesis, even when successful, brings the patient to the previous morbid state of fused hip with persistent altered biomechanics. Moreover, there are several technical difficulties while fixing these fractures and the union is delayed leading to a prolonged rehabilitation of these patients. Even the future total hip arthroplasty may become difficult due to problem related to insitu hardware. Our experience with these cases shows that total hip arthroplasty provides a reliable fixation with early mobilization and better function.
7. Learning points
-
1.
Proximal femoral fracture in an ankylosed hip is a challenging condition
-
2.
Fixation is difficult and even if done only returns the patient back to the pre-injury status
-
3.
Total hip arthroplasty helps in fixing the fracture as well as make the hip simultaneously
-
4.
Use of modular stem helps to adjust the offsets, limb length and version intraoperatively
-
5.The authors strongly recommend acute total hip arthroplasty rather than mere fixation in cases of proximal femoral fractures in ankylosed hips due to several advantages
-
a.The patient can be mobilized early with full weight bearing
-
b.The patient will have a mobile hip
-
c.There is no need for a re-surgery either for implant removal or a future THA
-
d.The quality of life improves dramatically
-
a.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.06.014.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Wulke A.P., Mader K., Pennig D. Femoral neck fracture in an arthrodesed hip treated by a supracondylar intramedullary locked nail. J Orthop Trauma. 2004;18(2):116–118. doi: 10.1097/00005131-200402000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Wong T.C., Rikhraj I.S. Femoral shaft fracture in a hip arthrodesis: two cases of retrograde interlocking nailing. Singap Med J. 2004;45(2):85–87. [PubMed] [Google Scholar]
- 3.Aufranc O.E., Jones W.N., Stewart W.G. Femoral shaft fracture with ipsilateral ankylosed hip. J Am Med Assoc. 1965;192:1153–1155. doi: 10.1001/jama.1965.03080260041012. [DOI] [PubMed] [Google Scholar]
- 4.Manzotti A., Confalonieri N., Pullen C. Intertrochanteric fracture of an arthrodesed hip. J Bone Joint Surg Br. 2007;89(3):390–392. doi: 10.1302/0301-620X.89B3.18591. [DOI] [PubMed] [Google Scholar]
- 5.Ishimaru D., Nozawa S., Maeda M., Shimizu K. Intertrochanteric fracture of the ankylosed hip joint treated by a gamma nail: a case report. Case Rep Orthop. 2012;2012:278156. doi: 10.1155/2012/278156. http://www.hindawi.com/journals/crior/2012/278156/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Font-Vizcarra L., Carreño A.M., Prat S., Muñoz-Mahamud E., Camacho P., Casanova L. Less invasive fixation of an interthrocanteric fracture in an ankylosed hip with cannulated screws: a case report. Hip Int J Clin Exp Res Hip Pathol Ther. 2010;20(4):565–567. doi: 10.1177/112070001002000426. [DOI] [PubMed] [Google Scholar]
- 7.Lonner B.S., Lonner J.H., Sadler A.H. Retrograde femoral nailing between an ankylosed hip and a stiff knee. J Orthop Trauma. 1995;9(3):266–269. doi: 10.1097/00005131-199506000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Sponseller P.D., McBeath A.A., Perpich M. Hip arthrodesis in young patients. A long-term follow-up study. J Bone Joint Surg Am. 1984;66(6):853–859. doi: 10.2106/00004623-198466060-00005. [DOI] [PubMed] [Google Scholar]
- 9.Callaghan J.J., Brand R.A., Pedersen D.R. Hip arthrodesis. A long-term follow-up. J Bone Joint Surg Am. 1985;67(9):1328–1335. [PubMed] [Google Scholar]
- 10.Bhan S., Eachempati K.K., Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J Arthropl [Internet] 2008;23(6):859–866. doi: 10.1016/j.arth.2007.07.014. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0883540307004421. [DOI] [PubMed] [Google Scholar]
- 11.Hamadouche M., Kerboull L., Meunier A., Courpied J.P., Kerboull M. Total hip arthroplasty for the treatment of ankylosed hips : a five to twenty-one-year follow-up study. J Bone Joint Surg Am. 2001;83-A(7):992–998. doi: 10.2106/00004623-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y.-H., Oh S.-H., Kim J.-S., Lee S.-H. Total hip arthroplasty for the treatment of osseous ankylosed hips. Clin Orthop. 2003;414:136–148. doi: 10.1097/01.blo.0000081935.75404.7f. https://insights.ovid.com/crossref?an=00003086-200309000-00019 Available from: [DOI] [PubMed] [Google Scholar]
- 13.Idulhaq M., Park K.S., Diwanji S.R., Yoon T.R., Wie J.S. Total hip arthroplasty for treatment of fused hip with 90° flexion deformity. J Arthropl [Internet] 2010;25(3):498. doi: 10.1016/j.arth.2008.12.004. http://linkinghub.elsevier.com/retrieve/pii/S0883540308010000 e5-498.e9. Available from: [DOI] [PubMed] [Google Scholar]
- 14.Joshi A.B., Markovic L., Hardinge K., Murphy J.C.M. Total hip arthroplasty in ankylosing spondylitis: an analysis of 181 hips. J Arthropl [Internet] 2002;17(4):427–433. doi: 10.1054/arth.2002.32170. Available from: http://linkinghub.elsevier.com/retrieve/pii/S088354030245663X. [DOI] [PubMed] [Google Scholar]
- 15.Swanson M.A., Huo M.H. Total hip arthroplasty in the ankylosed hip. J Am Acad Orthop Surg. 2011;19(12):737–745. doi: 10.5435/00124635-201112000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Kerboull M., Bentley G., Kerboull L., Hamadouche M. Total hip replacement for ankylosed hips. In: Bentley G., editor. European Surgical Orthopaedics and Traumatology [Internet] Springer Berlin Heidelberg; Berlin, Heidelberg: 2014. http://link.springer.com/10.1007/978-3-642-34746-7_201 2453–60. Available from: [Google Scholar]
- 17.Kim Y.L., Shin S.I., Nam K.W., Yoo J.J., Kim Y.-M., Kim H.J. Total hip arthroplasty for bilaterally ankylosed hips. J Arthropl [Internet] 2007;22(7):1037–1041. doi: 10.1016/j.arth.2007.03.027. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0883540307001775. [DOI] [PubMed] [Google Scholar]
- 18.Bangjian H., Peijian T., Ju L. Bilateral synchronous total hip arthroplasty for ankylosed hips. Int Orthop. 2012;36(4):697–701. doi: 10.1007/s00264-011-1313-8. http://link.springer.com/10.1007/s00264-011-1313-8 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.