Abstract
Background
Total knee arthroplasty (TKA) with fixed-bearing (FB) implants have demonstrated impressive functional results and survival rates. Meanwhile, rotating-platform (RP) constructs have biomechanically shown to reduce polyethylene wear, lower the risk of component loosening, and better replicate anatomic knee motion. There is growing question of the clinical impact these design changes have long-term.
Questions/purposes: The aim of this double-blinded prospective randomized trial was to compare function and implant survival in patients who received either FB or RP press-fit condylar Sigma (PFC Sigma, DePuy, Warsaw, IN) total knee replacements at a minimum follow-up of twelve years.
Patients and methods
Patient reported outcome measures used included the functional Knee Society Score, Western Ontario and McMaster University Osteoarthritis Index (WOMAC) scores, Medical Outcomes Short Form-36 (SF-36) score, and satisfaction assessment on a four-point Likert scale. The data was collected from times preoperative, two-years, and final encounter (mean 13.95 years). A total of 28 RP and 19 FB knees (58.8%) were analyzed at the final follow-up.
Results
Among all patients, KSS and WOMAC scores statistically improved from pre-op to 2-year, while KSS statistically worsened from 2-year to final follow-up. The RP group averaged better follow-up scores in all assessments at the final follow-up with exception of overall satisfaction. There was no statistically significant difference in the functional Knee Society Score, Short Form-36, WOMAC scores, patient satisfaction or implant survival between the two groups at any measured period.
Conclusions
The use of a fixed-bearing or rotating-platform design does not convey significant superiority in terms of function or implant longevity at a minimum twelve years after total knee arthroplasty.
Level of evidence
Level I, Experimental study, randomized controlled trial (RCT).
Keywords: Knee arthroplasty, Total knee replacement, Mobile bearing, Fixed bearing
1. Introduction
Total knee arthroplasty (TKA) is a successful surgical treatment for knee osteoarthritis, with cemented fixed-bearing implants demonstrating impressive functional results and survival rates.1 However, there is persistent concern for polyethylene wear, patellar maltracking, and osteolysis around these implants; especially in younger patients. Mobile-bearing implants allow the polyethylene insert to rotate short distances inside the tibial tray, granting a few degrees of greater rotational freedom.2 This design element can theoretically correct rotational mismatch between femoral and tibial components, in addition to decreasing contact stresses at the bone-prosthesis interface.3,4 These features are estimated to reduce polyethylene wear, lower the risk of component loosening, decrease anterior knee pain, and better replicate anatomic knee motion.2,5
There exists growing consensus that the theoretical advantages of mobile-bearing constructs do not translate to long-term clinical outcomes.6, 7, 8, 9, 10, 11, 12, 13, 14 Mobile-bearing knees require greater support from ligamentous and soft tissue structures surrounding the knee, and as a result, are more likely to dissociate from the tibial tray.15,16 Furthermore, in vivo biomechanical and fluoroscopic studies have found minimal kinematic differences between fixed bearing and mobile bearing groups.17,18 Thus, surgeons have argued whether the additional cost of mobile-bearing implants is valuable to the patient when fixed-bearing implants have an already excellent track record.
A relative paucity of studies exists comparing the long-term function and survival of the mobile-bearing prostheses.7,17, 18, 19 Long-term analyses have been conducted mainly for the New Jersey Low Contact Stress (LCS) knee (DePuy Orthopedics, Warsaw, IN), showing excellent survivorship, but notable significant incidences of polyethylene spin-out.20,21 The Press Fit Condylar (PFC) Sigma rotating-platform (RP) (DePuy Orthopedics, Warsaw, IN) was introduced in 2000 with a design meant to reduce spin-out, reduce polyethylene wear, and increase knee range of motion compared to the LCS implant.22,23 There are few long-term studies looking at the function and longevity of the PFC Sigma RP and even fewer studies comparing the long-term outcomes of this RP knee design to the standard FB implant.24, 25, 26, 27, 28, 29
We previously reported the two-year results comparing this patient population with regards to clinical, functional and radiographic outcomes.30 In that sample of data, there was no statistically significant difference between the implants in terms of functional or radiographic outcomes. Several short and mid-term studies have echoed those results.24, 25, 26, 27, 28, 29 The aim of this double-blinded prospective randomized controlled trial was to present the longest follow-up to date (mean 13.95 years) comparing the PFC Sigma fixed-bearing (FB) and rotating platform (RP) implants.
2. Materials and methods
All patients were randomized intra-operatively to either a PFC Sigma fixed- or rotating-platform prosthesis (PFC Sigma, DePuy, Warsaw, Indiana), and the decision to sacrifice the posterior cruciate ligament was at the surgeon's discretion. The patients and the assessor (C.K.) were blinded to the type of implant received.
The present study was approved by our institutional review board, and all patients were consented over the phone to participate in a phone-based series of surveys. The surveys employed were the Knee Society Functional Score (KSS),31 the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) scores,32 the Medical Outcomes Short Form-36 score33 and a satisfaction scale on a on a four-point Likert scale.34
The data collected at the patients’ preoperative and two-year follow-up visit was used to compare the changes in the Knee Society Functional scores, the WOMAC scores. The original preoperative SF-36 data was de-identified and could not be specifically attributed to our newly refined patient population; leaving the two-year data available for comparison. At the time of original publication, this cohort had one revision documented for the fixed-bearing group and no revisions or failures in the rotating-platform arm.30
2.1. Statistical analysis
Generalized estimating equations (GEE models) were used to compare KSS, WOMAC, and SF-36 scores between knees assigned to Fixed-Bearing versus Rotating-Platform by time. In these models, a normal distribution with identity link was specified for each sub-score. Further, each model used an interaction term to test whether the association between treatment assignment and sub-scores depended on time. When the interaction was not significant, it was removed from the model to estimate the overall change in KSS, WOMAC, and SF-36 scores by time while controlling for participants’ treatment assignment. Participants could contribute multiple surgeries to the analysis and, for this reason, an exchangeable correlation structure was used to account for their within-subject correlation. Model assumptions were assessed using QQ plots (for normality), residual plots (for linearity), and box plots (for outliers).
Finally, a frailty model was used to compare the risk of failure for knees assigned to Fixed-Bearing versus Rotating-Platform. In this model, a lognormal distribution was specified for the frailty effect allowing patients to contribute multiple surgeries to the analysis. Time was measured in years from the date of surgery to date of knee failure, and knees free from failure were censored at the last date the implant was known to remain successful. Regarding model assumptions, the proportional hazards assumption was assessed graphically using Martingale residuals as described by Lin, Wei, and Ying (1993), and a Kaplan-Meier plot was used to display the cumulative probability of success for each treatment group by time.35 Additionally, due to the sparse number of expected knee failures, a Fisher's exact test was also used to compare the rate of knee failures between the two treatments; conclusions from this sensitivity analysis were similar. All analyses were completed using SAS version 9.4 (Cary, NC).
3. Results
The demographic data and surgical technique employed for this study have been previously described.30 In the original report, there were 132 patients contributing 140 surgeries (72 FB and 68 RP procedures) to the analysis. Of these patients, 28 patients expired prior to the 12 year minimum follow-up, and an additional 28 patients requested removal prior to this report, leaving 76 patients (80 surgeries) remaining. Of these, 40 patients (52.6%) and 47 procedures (58.8%) had valid KSS, WOMAC, and SF-36 scores available for analysis.
The mean age for participants was 76.66 years (76.79 and 76.57 years for fixed bearing and rotating platform, respectively). See Table 1. There was no significant difference in KSS, WOMAC, and SF-36 sub-scores between knees assigned to a Fixed-Bearing (FB) treatment versus Rotating-Platform (RP) treatment at any time (all p > .05). See Table 2, Table 3. However, a subsequent analysis that modeled change in these sub-scores for the entire cohort revealed that WOMAC pain, stiffness, and function scores declined from the preoperative assessment to the final follow-up visit. See Table 4A. For WOMAC pain, participants’ scores improved by an average of −4.84 (95% CI: −6.15 to −3.54) points from the pre-operative assessment to two year follow-up (p < .001) and improved by an average of −5.72 (95% CI: −7.22 to −4.22) points from the pre-operative assessment to final follow-up visit (p < .001); there was no significant change from the 2-year to final follow-up visits (p = .13). Further analysis modeled the change for the entire cohort revealed the SF-36 physical function (p = .61), role emotion (p = .064) and mental health (p = .30) increased meanwhile there was a general decline in the role physical (p = .87), pain (p = .11), vitality (p = .46), and social function (p = .74) sub-scores. See Table 4B.
Table 1.
Patient demographics.
| Fixed Bearing | Rotating Platform | Total | |
|---|---|---|---|
| Mean Age (SD) | 76.79 (10.54) | 76.57 (9.70) | 76.66 (9.94) |
| Years from Surgery | 13.94 (.70) | 13.95 (0.67) | 13.95 (0.67) |
| Females | 16 (76%) | 18 (60%) | 34 (67%) |
| Males | 5 (24%) | 12 (40%) | 17 (33%) |
Note: Valid N = 104. SD = Standard deviation of the mean.
Table 2.
Difference in KSS and WOMAC scores between Fixed Bearing and Rotating Platform by time.
| Mean Difference (FB vs RP) | 95% Confidence Interval |
p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| KNEESOC Score | .34 | |||
| Pre-Op | 0.30 | −6.58 | 7.18 | – |
| 2-year | −7.86 | −20.80 | 5.08 | .23 |
| Final | −7.96 | −23.18 | 7.27 | .31 |
| WOMAC Pain | .94 | |||
| Pre-Op | 0.09 | −2.32 | 2.50 | – |
| 2-year | 0.31 | −1.66 | 2.27 | .76 |
| Final | 0.63 | −0.81 | 2.06 | .39 |
| WOMAC Stiffness | .80 | |||
| Pre-Op | 0.04 | −1.04 | 1.11 | – |
| 2-year | 0.08 | −0.65 | 0.81 | .83 |
| Final | 0.37 | −0.36 | 1.10 | .32 |
| WOMAC Function | .51 | |||
| Pre-Op | −0.94 | −7.81 | 5.93 | – |
| 2-year | 2.43 | −2.82 | 7.67 | .36 |
| Final | 4.18 | −0.27 | 8.63 | .066 |
Note: Valid N = 40 for all estimates. Pre-operative comparisons are assumed to be comparable due to the use of randomization.
Table 3.
Difference in SF-36 scores between Fixed Bearing and Rotating Platform by time.
| Mean Difference (FB vs RP) | 95% Confidence Interval |
p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Physical Function | .15 | |||
| 2-year | 3.48 | −8.71 | 15.67 | .58 |
| Final | −10.35 | −22.96 | 2.27 | .11 |
| Role Physical | .96 | |||
| 2-year | −9.08 | −31.55 | 13.38 | .43 |
| Final | −9.98 | −28.00 | 8.04 | .28 |
| Pain | .22 | |||
| 2-year | 1.86 | −6.66 | 10.38 | .67 |
| Final | −5.45 | −12.82 | 1.91 | .15 |
| Vitality | .91 | |||
| 2-year | −2.12 | −11.74 | 7.51 | .67 |
| Final | −2.81 | −10.73 | 5.10 | .49 |
| Social Function | .41 | |||
| 2-year | −3.23 | −15.17 | 8.72 | .60 |
| Final | −10.79 | −23.66 | 2.08 | .10 |
| Role Emotion | .69 | |||
| 2-year | −4.96 | −18.64 | 8.72 | .48 |
| Final | −1.77 | −10.34 | 6.81 | .69 |
| Mental Health | .69 | |||
| 2-year | −2.35 | −13.26 | 8.57 | .67 |
| Final | −4.81 | −11.01 | 1.40 | .13 |
Note: Valid N = 40 for all estimates.
Table 4A.
Change in KSS and WOMAC scores by time.
| Mean Difference | 95% Confidence Interval |
p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| KNEESOC | <.001 | |||
| 2-Year vs Pre-op | 41.70 | 34.40 | 49.00 | <.001 |
| Final vs Pre-op | 17.02 | 9.22 | 24.82 | <.001 |
| Final vs 2-Year | −24.68 | −34.63 | −14.73 | <.001 |
| WOMAC Pain | <.001 | |||
| 2-Year vs Pre-op | −4.84 | −6.15 | −3.54 | <.001 |
| Final vs Pre-op | −5.72 | −7.22 | −4.22 | <.001 |
| Final vs 2-Year | −0.87 | −2.01 | 0.27 | .13 |
| WOMAC Stiffness | <.001 | |||
| 2-Year vs Pre-op | −1.84 | −2.51 | −1.18 | <.001 |
| Final vs Pre-op | −2.33 | −3.02 | −1.64 | <.001 |
| Final vs 2-Year | −0.49 | −1.01 | 0.03 | .067 |
| WOMAC Function | <.001 | |||
| 2-Year vs Pre-op | −13.40 | −17.39 | −9.41 | <.001 |
| Final vs Pre-op | −16.76 | −21.05 | −12.47 | <.001 |
| Final vs 2-Year | −3.36 | −7.66 | 0.94 | .13 |
Note: Valid N = 40 patients for all estimates. Estimates are adjusted for treatment assignment.
Table 4B.
Change in SF-36 sub-scores from the 2-year visit to final visit.
| Mean Difference (Final vs 2-year) | 95% Confidence Interval |
p | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Physical Function | 2.45 | −6.91 | 11.81 | .61 |
| Role Physical | −1.26 | −16.50 | 13.98 | .87 |
| Pain | −5.28 | −11.79 | 1.23 | .11 |
| Vitality | −2.53 | −9.21 | 4.14 | .46 |
| Social Function | −1.52 | −10.48 | 7.44 | .74 |
| Role Emotion | 11.15 | −0.64 | 22.94 | .064 |
| Mental Health | 3.15 | −2.84 | 9.14 | .30 |
Note: Valid N = 40 patients for all estimates. Estimates are adjusted for treatment assignment.
Trends were similar for the WOMAC stiffness and function sub-scores. Regarding stiffness, scores improved by an average of −1.84 (95% CI: −2.51 to −1.18) points from the pre-operative assessment to 2-year follow-up assessment (p < .001) and by an average of −2.33 (95% CI: −3.02 to −1.64) points from the pre-operative assessment to final follow-up visit (p < .001). Like the WOMAC pain score, there was no significant change in WOMAC stiffness from the 2-year to final follow-up visits (p = .067). Regarding WOMAC functioning, there was also a significant improvement from the pre-operative visit to 2-year follow-up visit (Mdiff = −13.40, 95% CI: −17.39 to −9.41; p < .001) and from the pre-operative visit to final follow-up (Mdiff = −16.76, 95% CI: −21.05 to −12.47; p < .001) but, as before, there was no significant change from the 2-year follow-up visit to final follow-up visit (Mdiff = −3.36, 95% CI: −7.66 to 0.94; p = .13). The KSS functional scores showed a curvilinear relationship with an average improvement of 41.70 (95% CI: 34.40–49.00) points from the pre-operative assessment to the 2-year follow-up visit (p < .001) followed by a worsening of an average −24.68 (95% CI: −34.63 to −14.73) points from the 2-year visit to final follow-up visit (p < .001).
The Self-Administered Patient Satisfaction Scale is a valid instrument for measuring patient satisfaction following primary hip and knee arthroplasty.34 A portion of this scale was used to assess patient satisfaction. Overall, 82.1% of mobile bearing subjects and 84.2% of fixed-bearing were very satisfied with their knee. Subjects further reported being somewhat satisfied at 10.7% and 10.5%, somewhat dissatisfied at 3.6% and 0.0%, and very dissatisfied at 3.6% and 5.3% for the mobile bearing and fixed-bearing groups, respectively. See Table 5.
Table 5.
Patient satisfaction.
| Fixed Bearing | Rotating Platform | Total | |
|---|---|---|---|
| Very Satisfied | 16 (84.2%) | 23 (82.1%) | 39 (83.0%) |
| Somewhat Satisfied | 2 (10.5%) | 3 (10.7%) | 5 (10.6%) |
| Somewhat Dissatisfied | 0 (0.0%) | 1 (3.6%) | 1 (2.1%) |
| Very Dissatisfied | 1 (5.3%) | 1 (3.6%) | 2 (4.3%) |
Note: Valid N = 47. SD = Standard deviation of the mean.
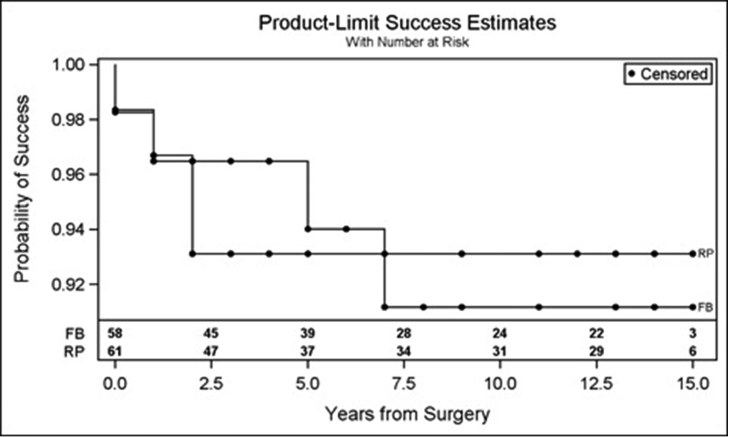
In terms of implant survival and success, there were exactly four failures in the fixed-bearing group and four failures in the rotating platform group. In this sample of data, there was no significant difference in the risk of knee failure between the FB versus RP groups (HR = 1.05, 95% CI: 0.26–4.20; p = .95). The probability of success for the RP implant at 15 years was 93% compared with 91% in the FB group. See Fig. 1.
Fig. 1.
Cumulative probability of success.
4. Reoperations and complications
Four failures were seen in each group, with two revisions in each group. Of note, seven of the eight (87.5%) failures were in posterior stabilized (PS) knee implants; the single cruciate-retaining (CR) failure was due to patella dislocation at almost eight years post-op. The FB groups’ reoperations were at an average of 49.5 months post-op. One FB revision was for persistent pain with an oversized femoral component at 10 months. One FB was found to have a loose tibial baseplate on radiographs at 7 years. The other two failure were due to patella fracture and patellar dislocation (CR) and involved patellar augmentation only. In the RP group, the reoperations were at an average of 15.3 months post-op. Two revisions were performed for deep infections at six weeks and 11 months. The other two reoperations for patellar component loosening and patella fracture involved only patellar augmentation. There were no cases of spin-out in the RP group. The rate of complications was similar for each group. There were four diagnosed DVTs in the RP and three in the FB groups. One non-lethal pulmonary embolism was diagnosed in each group during the acute postoperative hospital stay. Two FB knees required manipulation under anesthesia for persistent stiffness at six weeks post-op.
5. Discussion
Carothers et al. performed a meta-analysis comparing various mobile-bearing designs and found that the 15-year survivorship of rotating-platform designs (96.4%) was excellent.36 Recent meta-analyses comparing all MB and FB TKA designs indicated there were no clinically relevant or significant differences among revision rates, range of motion, KSS, or SF-36 scores21 Van Der Voort et al. performed a meta-analysis specifically assessing differences between rotating-platform and fixed-bearing implants, and also found no statistically significant differences in function, alignment, revisions or complications.37 Despite the theoretical benefits and laboratory testing, there exists a discrepancy between biomechanical and clinical studies that have attempted to compare the two implant types.
To date, there has been only one long-term (>10 year, mean 11.1 years) study directly comparing the PFC Sigma RP to the FB implant.28 Comparing PFC Sigma RP to FB implants uses an identical femoral component, thus allows statistical differences between implants to be largely attributed to the RP or FB portion. Our study represents the longest follow-up comparing these two implant types.
Riaz et al. recently published a prospective comparative study of the PFC Sigma cruciate-retaining RP and FB implants range of motion, Oxford Knee Scores, complications, and radiographic wear at a minimum of 10 years (mean 11.1 years, range 10.0–12 years). Comparing 113 RP and 89 FB knees, they were unable to elicit a statistically significant difference among functional capacity, wear, or complications rates between implant groups. Our study similarly reported no statistically significant difference among KSS, WOMAC, SF-36, and satisfaction recordings. Riaz et al. further reported both implant groups experienced functional improvement and pain relief at final follow-up compared to preoperative testing, similar to our study. Finally, they found no statistical difference in survivorship between implant groups with 98% survival probability at 10 years in the RP arm. Our study supports this finding with a similar survival probability at 15 years found to be 93% in our RP arm, and no statistical difference between implant groups.28
Meftah et al. published a long-term follow-up involving 117 consecutive patients (138 knees) who received PFC Sigma rotating-platform (RP) posterior-stabilized (PS) cemented implants by a single surgeon at an average of 10 years (range: 9.5–11 years) follow-up. They found the mean KSS function and WOMAC scores improved from 39.4 to 90.2 (p < .001) and 32.2 to 6.6 points (p < .001), respectively. Our RP KSS functional score also improved from pre-op with a mean difference of 17.02 (p < .001), but the final KSS averaged less at 65.36. We suspect this lower reporting may, in part, be due to an average 3 year later follow-up and that our surveys were not conducted in person, potentially reducing Hawthorne effect. They also found that 94% of patients were satisfied with their knee(s) overall. The group reported 3 revisions with Kaplan-Meier survival analysis at ten years with 100% survival due to mechanical failure revisions, 97.7% survival with revision for any reason, and 95% survival with reoperation for any reason.26 Our RP group closely matched this with a 93% survival probability at 15 years, 100% survival due to mechanical failures, and a total of two revisions.
Another recent publication by Ulivi et al. reported on a minimum 10-year survivorship (range: 11.5±1.4 years) of the PFC Sigma RP posterior-stabilized implant in 160 consecutive patients (166 knees). They reported a 3% revision rate for all knees, with no cases of polyethylene spin-out. The final data on 88 knees showed a 96.6% chance of implant survival at 11.5 years and no mechanical failures, similar to our data at 15 years.29 This group further noted worse orthopaedic knee scores in terms of knee function than Mefta et al., closer to our reported values.26 The researchers also collected data on major and minor medical comorbidities at 11.5 year follow-up and found 21.5% were free of any coexisting conditions, meanwhile those with severe diseases negatively impacted the functional scoring. They found functional KSS to be nearly the same at final follow-up when compared to the preoperative measure, but when controlled for the concomitant pathologies, was significantly improved.29
We also noted that, while both the RP and FB groups showed significant improvement at the final encounter compared to preop scores, both groups also had equal and significantly lower KSS scores at the final encounter compared to the 2-year follow-up (Table 3). Meanwhile, the WOMAC function was not significantly different at the final follow-up. We suspect the KSS statistically identified a decreased knee function after 10 years of post-op follow-up due to its more objective nature, while the WOMAC scores are reportedly influenced by factors outside the lower extremity.38 Hofstede et al. also showed a trend, though insignificant, for the RP groups to have improved scores on several patient reported outcome measures.19
The patients who reported being very satisfied overall with the results of their knee replacement were not statistically significant between the two groups at the final encounter. 93% of the RP knees and 95% of the FB knees were at least somewhat satisfied with the outcome of their knee at an average of 13.7 years. This data is in line with a study by Wylde et al. who employed the same satisfaction scale and found 88.2% satisfaction with the RP and 87% with the FB implant at 2 year follow-up.39 Similarly, Mefta et al. found that 94% (eighty-four patients) of their RP knees were satisfied with the end result at an average 10-years postoperative.26 In the age of quality improvement and patient reported outcome measures, patient satisfaction is a vital component of overall result.
There exist several shortcomings with the present study. The retention rate from the initial study was significantly diminished due to the fact that many of the original cohort could not be reached by phone or given contact information and were subsequently lost to follow-up. Due to the majority of patients responding that they were either infirm or unable to secure transportation to a physician appointment, all contact with the patient was conducted via phone call. As such, we were unable to obtain any radiographs of the implants to observe signs of aseptic loosening or osteolysis. Zeng et al. recently reviewed 34 studies, 6861 knees, to conclude no statistical difference in the incidence of radiolucent lines, osteolysis, aseptic loosening or survival between fixed bearing and mobile bearing constructs.40 In a direct comparison study, Ulivi et al. found no difference between the PFC Sigma RP and FB groups in terms of radiolucencies, osteolysis and other mid-to long-term reports have elicited only subclinical radiolucent lines in the mobile-bearing groups.26,29
6. Conclusion
In this sample of data, the PFC Sigma rotating-platform demonstrated nearly equivalent survivorship and functional outcomes when compared to the fixed-bearing implant with an average of 13.95 years and a cumulative probability of success at 15 years being 93%. We found no statistically significant difference between the implant types in terms of functional KSS scores, WOMAC scores, SF-36 scores, satisfaction, or implant survival.
Conflicts of interest
This research does not have any funding or financial support to disclose. No authors have any potential sources of conflict of interest to disclose.
Contributor Information
Cameron J. Killen, Email: cameron.killen@lumc.edu.
Michael P. Murphy, Email: mmurphy12@luc.edu.
William J. Hopkinson, Email: whopkin@lumc.edu.
Melvyn A. Harrington, Email: melvynh@bcm.edu.
William H. Adams, Email: wadams@luc.edu.
Harold W. Rees, Email: harees@lumc.edu.
References
- 1.Callaghan J.J., O'rourke M.R., Iossi M.F. Cemented rotating-platform total knee replacement: a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am. 2005;87:1995–1998. doi: 10.2106/JBJS.D.03039. [DOI] [PubMed] [Google Scholar]
- 2.Dennis D., Komistek R. Mobile-bearing total knee arthroplasty: design factors in minimizing wear. Clin Orthop Relat Res. 2006;452:70–77. doi: 10.1097/01.blo.0000238776.27316.d6. [DOI] [PubMed] [Google Scholar]
- 3.Buechel F.F., Pappas M.J. Long-term survivorship analysis of cruciate-sparing versus cruciate-sacrificing knee prostheses using meniscal bearings. Clin Orthop Relat Res. 1990;260:162–169. [PubMed] [Google Scholar]
- 4.Hooper G., Rothwell A., Frampton C. The low contact stress mobile-bearing total knee replacement: a prospective study with a minimum follow-up of ten years. J Bone Joint Surg Br. 2009;91:58–63. doi: 10.1302/0301-620X.91B1.20484. [DOI] [PubMed] [Google Scholar]
- 5.D'Lima D., Netter J., D'Alessio J., Keste M., Colwell C. Prediction of wear in mobile and fixed bearing, cross-linked and non-cross-linked, unicompartmental and tricompartmental knee arthroplasty. Bone Joint J. 2016;98:102. [Google Scholar]
- 6.Aggarwal A.K., Agrawal A. Mobile vs fixed-bearing total knee arthroplasty performed by a single surgeon: a 4-to 6.5-year randomized, prospective, controlled, double-blinded study. J Arthroplast. 2013;28:1712–1716. doi: 10.1016/j.arth.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Bailey O., Ferguson K., Crawfurd E. No clinical difference between fixed-and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1653–1659. doi: 10.1007/s00167-014-2877-9. [DOI] [PubMed] [Google Scholar]
- 8.Cheng T., Pan X., Liu T., Zhang X. Tibial component designs in primary total knee arthroplasty: should we reconsider all-polyethylene component? Knee Surg Sports Traumatol Arthrosc. 2012;20:1438–1449. doi: 10.1007/s00167-011-1682-y. [DOI] [PubMed] [Google Scholar]
- 9.Cheng T., Zhang G., Zhang X. Metal-backed versus all-polyethylene tibial components in primary total knee arthroplasty: a meta-analysis and systematic review of randomized controlled trials. Acta Orthop. 2011;82(5):589–595. doi: 10.3109/17453674.2011.618913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y.H., Park J.W., Kim J.S., Kulkarni S.S., Kim Y.H. Long-term clinical outcomes and survivorship of press-fit condylar sigma fixed-bearing and mobile-bearing total knee prostheses in the same patients. J Bone Joint Surg Am. 2014;96:e168. doi: 10.2106/JBJS.M.01130. [DOI] [PubMed] [Google Scholar]
- 11.Kremers H.M., Sierra R.J., Schleck C.D. Comparative survivorship of different tibial designs in primary total knee arthroplasty. J Bone Joint Surg Am. 2014;96:e121. doi: 10.2106/JBJS.M.00820. [DOI] [PubMed] [Google Scholar]
- 12.Heesterbeek P.J.C., van Houten A.H., Klenk J.S. Superior long-term survival for fixed bearing compared with mobile bearing in ligament-balanced total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2018;26:1524–1531. doi: 10.1007/s00167-017-4542-6. [DOI] [PubMed] [Google Scholar]
- 13.Nouta K.A., Verra W.C., Pijls B.G., Schoones J.W., Nelissen R.G. All-polyethylene tibial components are equal to metal-backed components: systematic review and meta-regression. Clin Orthop Relat Res. 2012;470:3549–3559. doi: 10.1007/s11999-012-2582-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Voigt J., Mosier M. Cemented all-polyethylene and metal-backed polyethylene tibial components used for primary total knee arthroplasty: a systematic review of the literature and meta-analysis of randomized controlled trials involving 1798 primary total knee implants. J Bone Joint Surg Am. 2011;93:1790–1798. doi: 10.2106/JBJS.J.01303. [DOI] [PubMed] [Google Scholar]
- 15.Pandit H., Jenkins C., Beard D.J. Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee. 2010;17:392–397. doi: 10.1016/j.knee.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Streit M.R., Walker T., Bruckner T. Mobile-bearing lateral unicompartmental knee replacement with the Oxford domed tibial component: an independent series. J Bone Joint Surg Br. 2010;94:1356–1361. doi: 10.1302/0301-620X.94B10.29119. [DOI] [PubMed] [Google Scholar]
- 17.Kim T.W., Lee S.M., Seong S.C., Lee S., Jang J., Lee M.C. Different intraoperative kinematics with comparable clinical outcomes of ultracongruent and posterior stabilized mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24:3036–3043. doi: 10.1007/s00167-014-3489-0. [DOI] [PubMed] [Google Scholar]
- 18.Okamoto N., Nakamura E., Nishioka H., Karasugi T., Okada T., Mizuta H. In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplast. 2014;29:2393–2396. doi: 10.1016/j.arth.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Hofstede S.N., Nouta K.A., Jacobs W. Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. 2015;4:CD003130. doi: 10.1002/14651858.CD003130.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Callaghan J.J., Wells C.W., Liu S.S., Goetz D.D., Johnston R.C. Cemented rotating-platform total knee replacement: a concise follow-up, at a minimum of twenty years, of a previous report. J Bone Joint Surg Am. 2010;92:1635–1639. doi: 10.2106/JBJS.I.01012. [DOI] [PubMed] [Google Scholar]
- 21.Hopley C.D., Crossett L.S., Chen A.F. Long-term clinical outcomes and survivorship after total knee arthroplasty using a rotating platform knee prosthesis: a meta-analysis. J Arthroplast. 2013;28:68–77. doi: 10.1016/j.arth.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 22.Buechel F.F. Mobile-bearing knee arthroplasty: rotation is our salvation! J Arthroplast. 2004;19:27–30. doi: 10.1016/j.arth.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Callaghan J.J., Insall J.N., Greenwald A.S. Mobile-bearing knee replacement: concepts and results. Instr Course Lect. 2001;50:431–449. [PubMed] [Google Scholar]
- 24.Bhatt H., Rambani R., White W., Chakrabarty G. Primary total knee arthroplasty using the PFC Sigma®-rotating platform cruciate retaining endoprosthesis—a 6 year follow up. Knee. 2012;19:856–859. doi: 10.1016/j.knee.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Hanusch B., Lou T.N., Warriner G., Hui A., Gregg Z. Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomised controlled trial. Int Orthop. 2010;34:349–354. doi: 10.1007/s00264-009-0901-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meftah M., Ranawat A.S., Ranawat C.S. Ten-year follow-up of a rotating-platform, posterior-stabilized total knee arthroplasty. J Bone Joint Surg Am. 2012;94:426–432. doi: 10.2106/JBJS.K.00152. [DOI] [PubMed] [Google Scholar]
- 27.Moskal J.T., Capps S.G. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res. 2014;472:2185–2193. doi: 10.1007/s11999-014-3539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riaz O., Aqil A., Sisodia G., Chakrabarty G. PFC Sigma® cruciate retaining fixed-bearing versus mobile-bearing knee arthroplasty: a prospective comparative study with minimum 10-year follow-up. Uer J Orthop Surg Traumatol. 2017;27:1145–1149. doi: 10.1007/s00590-017-1920-1. [DOI] [PubMed] [Google Scholar]
- 29.Ulivi M., Orlandini L., Meroni V., Consonni O., Sansone V. Survivorship at minimum 10-year follow-up of a rotating-platform, mobile-bearing, posterior-stabilised total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015:231669–231675. doi: 10.1007/s00167-014-3118-y. [DOI] [PubMed] [Google Scholar]
- 30.Harrington M.A., Hopkinson W.J., Hsu P., Manion L. Fixed-vs mobile-bearing total knee arthroplasty: does it make a difference?—a prospective randomized study. J Arthroplast. 2009;24:24–27. doi: 10.1016/j.arth.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 31.Ewald F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 32.Bellamy N., Buchanan W.W., Goldsmith C.H., Campbell J., Stitt L.W. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 33.Ware J.E., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 34.Mahomed N.N., Sledge C.B., Daltroy L., Fossel A.H., Katz J.N. Self-administered patient satisfaction scale for joint replacement arthroplasty. J Bone Joint Surg Br. 1998;80:9. [Google Scholar]
- 35.Lin D.Y., Wei L.J., Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80:557–572. [Google Scholar]
- 36.Carothers J.T., Kim R.H., Dennis D.A., Southworth C. Mobile-bearing total knee arthroplasty: a meta-analysis. J Arthroplast. 2011;26:537–542. doi: 10.1016/j.arth.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 37.Van der Voort P., Pijls B.G., Nouta K.A., Valstar E.R., Jacobs W.C.H., Nelissen R.G.H.H. A systematic review and meta-regression of mobile-bearing versus fixed-bearing total knee replacement in 41 studies. Bone Joint J. 2013;95:1209–1216. doi: 10.1302/0301-620X.95B9.30386. [DOI] [PubMed] [Google Scholar]
- 38.Senden R., Grimm B., Meijer K., Savelberg H., Heyligers I.C. The importance to including objective functional outcomes in the clinical follow up of total knee arthroplasty patients. Knee. 2011;18:306–311. doi: 10.1016/j.knee.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 39.Wylde V., Learmonth I., Potter A., Bettinson K., Lingard E. Patient-reported outcomes after fixed-versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br. 2008;90:1172–1179. doi: 10.1302/0301-620X.90B9.21031. [DOI] [PubMed] [Google Scholar]
- 40.Zeng Y., Shen B., Yang J., Zhou Z.K., Kang P.D., Pei F.X. Is there reduced polyethylene wear and longer survival when using a mobile-bearing design in total knee replacement? Bone Joint J. 2013;95:1057–1063. doi: 10.1302/0301-620X.95B8.31310. [DOI] [PubMed] [Google Scholar]