Abstract
The treatment of severe acetabular defects in revision total hip arthroplasty (Paprosky type IIIa and IIIb) is demanding and choosing the appropriate surgical technique remains controversial. The introduction of trabecular metal augments has led to a variety of new treatment options. The authors present a case of a Paprosky Type IIIb acetabular defect due to eight subsequent revisions of the left hip. The patient was treated with an alternative treatment option using multiple tantalum wedges. Anatomical reconstruction was achieved and at 12 months follow-up, the patient was pain free and was able to walk without walking aids.
Keywords: Revision hip arthroplasty, Tantalum wedges, Paprosky classification, Acetabular defect, Alternative treatment
1. Introduction
As estimated by Kurtz and colleagues, the number of hip revision procedures in the United States will double by the year 2026, increasing the demand for new and reliable techniques.1 Despite the rising number of revision total hip arthroplasty cases, there is still no clear consensus for the management of acetabular defects with severe bone loss. The appropriate surgical technique and implant choice mainly depends on the severity of bone loss and location of the defect.2,3
Contained defects allow the use of a morcellised allograft in combination with a conventional cemented or cementless acetabular component.4, 5, 6 Minor column defects with remaining vertical support can be treated by minor column allograft combined with a conventional component, an oblong implant or a jumbo cup.4 However, the reconstruction of Paprosky Type IIIa and IIIb defects with major acetabular column defects remains controversial in terms of implant choice and surgical technique.3,4,7,8
In recent years, the use of trabecular metal augments or trabecular metal cups has demonstrated satisfactory results.4,7,9, 10, 11 Other treatment options are the custom triflange cup or the use of a 3D-printed acetabular component.12
In this context, we report on a case of successful acetabular reconstruction with multiple tantalum wedges in a patient with severe acetabular bone loss.
2. Case presentation
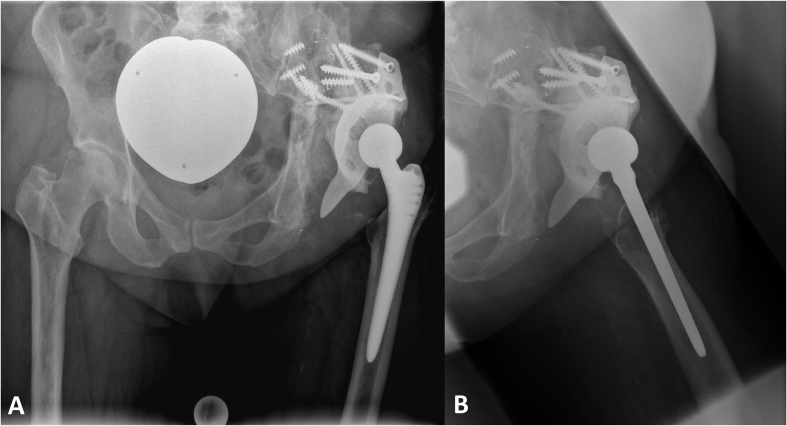
We report on a 60-year old female patient who had received a primary cementless THA of the left hip in 1995. A malposition of the cup during the index operation led to an early revision and in further consequence to recurrent cup dislocations of the left hip. Therefore, a total of 8 acetabular revision surgeries had been performed. The last previous surgery was performed 5 years prior to the current admission, and consisted of a reconstruction using a Burch-Schneider antiprotrusion cage in combination with impaction bone grafting (IBG) performed in the authors' clinic. The patient was readmitted 5 years later with pain of the left hip and a leg length discrepancy of 2 cm. On admission, the clinical examination showed a range of motion of the left hip with extension/flexion of 0-5-90°, abduction/adduction of 10-0-10° and internal/external rotation of 5-0-10°. Pelvis radiographs (Fig. 1a; 1b) showed a complete dislocation of the Burch-Schneider cage accompanied by a massive loss of acetabular bone formation. The patient's body mass index (BMI) was 34.5 kg/m2. Besides high blood pressure and nicotine abuse, no other systemic illnesses were noted. Preoperative blood samples showed only slightly elevated serum C-reactive protein (CRP) level of 12.8 mg/l (normal range < 5.0 mg/l) and a white blood cell count of 11.5 × 109/l (normal range 3.9–10.2 × 109/l). However, periprosthetic joint infection was ruled out using preoperative aspiration.
Fig. 1.
Admission radiographs of the pelvis (1a) and the left hip (axial view; 1b) shows a complete dislocation of the Burch-Schneider cage accompanied by a massive loss of acetabular bone formation.
2.1. Surgical technique
Revision surgery was performed under general anesthesia by an experienced attending orthopaedic surgeon. The patient was placed in a lateral position on the operating table and standard preparation and draping was performed. Exposure of the joint was achieved through a posterior approach. Due to scar tissue from previous revisions, dissection at the acetabulum was challenging and the gluteus medius muscle was only rudimentarily preserved. The stem indicated no signs of loosening or damage and was therefore retained. Several tissue samples were taken intraoperatively, however, histological and microbiological examinations did not reveal any evidence of infection.
In accordance to the preoperative CT scans, the Burch-Schneider antiprotrusion cage showed a complete dislocation and was removed along with the cemented cup and the structural bone graft. It revealed a massive bony column defect that presented as a flat plain merging continuously from the former acetabulum to the iliac wing (Paprosky Type IIIb) (14). No perforations or fractures were detected.
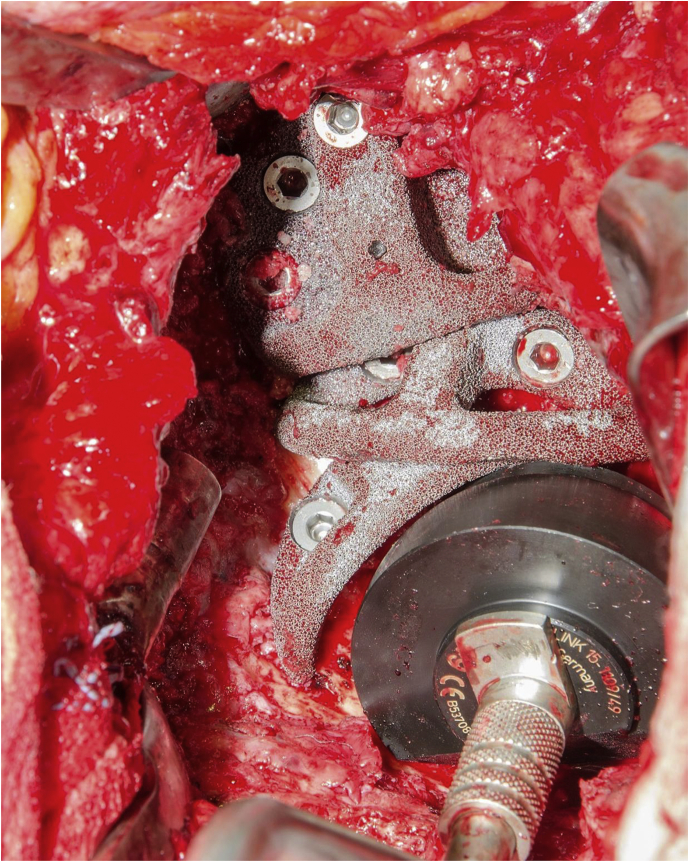
The lack of opportunities for sufficient vertical support led to the idea of an acetabular reconstruction with multiple tantalum wedges to ensure maximum joint stability. First, a large 30 mm cone (size 50/30 mm) (Zimmer; Warsaw, USA) was placed reversely at the distal part of the iliac ala, where bone quality was still satisfactory and five cortical screws where used for fixation. Subsequently, two more wedges (size 62/10 and 50/10 mm; Zimmer; Warsaw, USA) were attached caudally to distalize the center of rotation and to reconstruct the anatomical center of the hip. All wedges were placed in a reverse manner in order to mutually support each other (Fig. 2). Finally, a cemented dual mobility cup (Avantage® Dual Mobility, Biomet Orthopedics Inc., Warsaw, IN, USA) was implanted and cement was used to cover the tantalum wedges in order to prevent metal abrasion.
Fig. 2.
Intraoperative alignment of the used tantalum wedges to reconstruct the anatomical center of the hip.
Postoperatively, partial weight bearing limited to 10 kg was permitted for the first eight weeks. The patient was discharged 12 days after surgery. Full weight bearing was allowed after ten weeks.
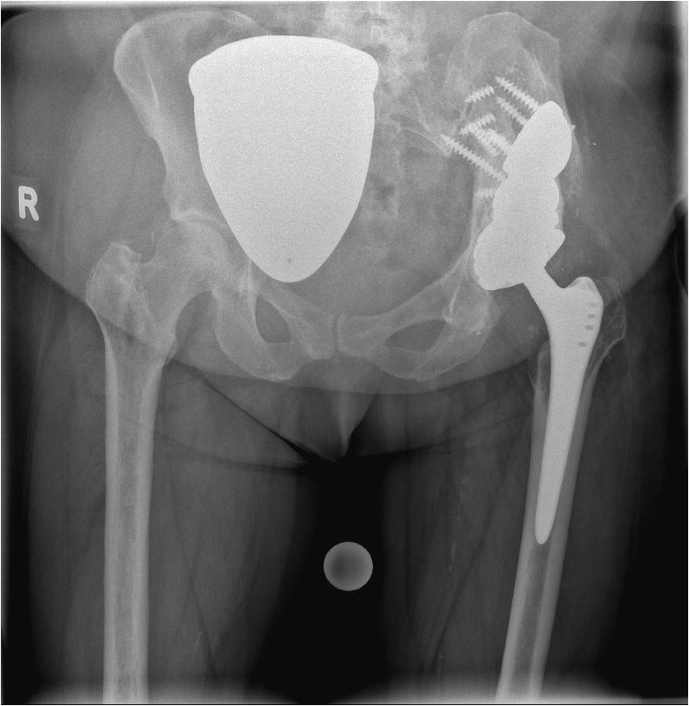
At 12 months of follow-up, the patient was pain free and was able to walk without walking aids. No leg length discrepancy was noted. The radiological control showed a good bony integration of the used implants without any signs of loosening (Fig. 3).
Fig. 3.
Radiological control at 12 months follow-up shows no signs of loosening and a good bony integration of the implants.
3. Discussion
The main purpose of reconstruction is to reestablish the center of rotation and to ensure a stable and durable fixation of the used implant.13 Intraoperative stability of the acetabular shell is crucial to achieve good long-term results.7
Commonly used procedures include acetabular reconstruction with impaction bone grafting and a cemented socket, structural allografts or metal cages.11,13, 14, 15 Although well-established, these traditional techniques have their limitations and different reports exist with mixed results, especially for the treatment of extensive acetabular column defects.11
As an attractive alternative, the use of highly porous metals for revision THA has evolved over the past decade, as it provides a range of new treatment options for acetabular reconstruction.4 Multiple studies have demonstrated good clinical and radiological results, as well as an improvement of quality-of-life parameters for the treatment of severe acetabular bone defects.2,4,7,11,13
Compared to other techniques, the use of trabecular metal augments (TMA) provides some biomechanical advantages, e.g., higher porosity than cobalt-chrome, a very high coefficient of friction and a similar modulus of elasticity to subchondral bone therefore allowing a better integration to the host bone.7 However, more studies are needed to investigate the long-term durability of the implants, as well as to fully understand the potential problems associated with trabecular metal reconstruction, such as debris generation at the augment-augment interface and the lack of ability to restore bone stock.7
As demonstrated in this case-report, a stable reconstruction of the former socket was possible due to the chain-like arrangement combined with a higher friction and a better bony integration of the TMA. It has yielded excellent radiological and clinical results at a 12month follow-up. The modular use of tantalum wedges allows an individual adaption to the presenting bone stock deficiency and therefore provides an effective tool for the reconstruction of extensive acetabular defects.
Conflicts of interest statement
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Declarations of interest
None.
Contributor Information
Markus Rossmann, Email: markus.rossmann@helios-gesundheit.de.
Eduardo M. Suero, Email: Eduardo.Suero@med.uni-muenchen.de.
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Dwivedi C., Gokhale S., Khim H.G., Oh J.K., Shon W.Y. Acetabular defect reconstruction with trabecular metal augments: study with minimum one-year follow-up. Hip Pelvis. 2017;29(3):168–175. doi: 10.5371/hp.2017.29.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong M., Kim H.J., Lim S.J., Moon Y.W., Park Y.S. Revision total hip arthroplasty using tantalum augment in patients with Paprosky III or IV acetabular bone defects: a minimum 2-year follow up study. Hip Pelvis. 2016;28(2):98–103. doi: 10.5371/hp.2016.28.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abolghasemian M., Tangsataporn S., Sternheim A., Backstein D., Safir O., Gross A.E. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint Lett. 2013;95-B(2):166–172. doi: 10.1302/0301-620X.95B2.30608. [DOI] [PubMed] [Google Scholar]
- 5.Della Valle C.J., Shuaipaj T., Berger R.A. Revision of the acetabular component without cement after total hip arthroplasty. A concise follow-up, at fifteen to nineteen years, of a previous report. J Bone Joint Surg Am. 2005;87(8):1795–1800. doi: 10.2106/JBJS.D.01818. [DOI] [PubMed] [Google Scholar]
- 6.Slooff T.J., Schimmel J.W., Buma P. Cemented fixation with bone grafts. Orthop Clin N Am. 1993;24(4):667–677. [PubMed] [Google Scholar]
- 7.Konan S., Duncan C.P., Masri B.A., Garbuz D.S. Porous tantalum uncemented acetabular components in revision total hip arthroplasty: a minimum ten-year clinical, radiological and quality of life outcome study. Bone Joint Lett J. 2016;98-B(6):767–771. doi: 10.1302/0301-620X.98B6.37183. [DOI] [PubMed] [Google Scholar]
- 8.Telleria J.J., Gee A.O. Classifications in brief: Paprosky classification of acetabular bone loss. Clin Orthop Relat Res. 2013;471(11):3725–3730. doi: 10.1007/s11999-013-3264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gehrke T., Bangert Y., Schwantes B., Gebauer M., Kendoff D. Acetabular revision in THA using tantalum augments combined with impaction bone grafting. Hip Int. 2013;23(4):359–365. doi: 10.5301/hipint.5000044. [DOI] [PubMed] [Google Scholar]
- 10.Grappiolo G., Loppini M., Longo U.G., Traverso F., Mazziotta G., Denaro V. Trabecular metal augments for the management of Paprosky type III defects without pelvic discontinuity. J Arthroplasty. 2015;30(6):1024–1029. doi: 10.1016/j.arth.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Siegmeth A., Duncan C.P., Masri B.A., Kim W.Y., Garbuz D.S. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467(1):199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Citak M., Kochsiek L., Gehrke T., Haasper C., Suero E.M., Mau H. Preliminary results of a 3D-printed acetabular component in the management of extensive defects. Hip Int. 2018 May;28(3):266–271. doi: 10.5301/hipint.5000561. [DOI] [PubMed] [Google Scholar]
- 13.Shon W.Y., Santhanam S.S., Choi J.W. Acetabular reconstruction in total hip arthroplasty. Hip Pelvis. 2016;28(1):1–14. doi: 10.5371/hp.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gross A.E., Goodman S. The role of cages and rings: when all else fails. Orthopedics. 2004;27(9):969–970. doi: 10.3928/0147-7447-20040901-32. [DOI] [PubMed] [Google Scholar]
- 15.Gross A.E., Goodman S. The current role of structural grafts and cages in revision arthroplasty of the hip. Clin Orthop Relat Res. 2004;429:193–200. doi: 10.1097/01.blo.0000149822.49890.5e. [DOI] [PubMed] [Google Scholar]