Abstract
Foundational elements of lifelong health are formed during the preschool years. Child care attendance has nearly doubled in the past 5 years making child care centers an ideal setting to establish healthy habits that prevent pediatric obesity. Despite the promising evidence of efficacy of child care-based obesity prevention interventions, limited attention has been directed to criteria needed for implementation at scale. There is potential to improve children’s dietary and physical activity behaviors in diverse communities through theory-based, culturally appropriate, manualized interventions, delivered by child care staff. CHAMP (Creating Healthy Habits Among Maryland Preschoolers) is a 3-arm cluster randomized controlled childhood obesity prevention trial, aiming to improve motor skills, physical activity and willingness to try new foods among 864 preschoolers (age 3–5 years) enrolled in 54 child care centers in 10 Maryland counties. CHAMP is informed by social-cognitive and bioecological theories and based on an evidence-based program, The Food Friends®. The two intervention arms include: 1) child care-center based lessons (18-week gross motor and 12-week nutrition) administered by trained child care staff, and 2) a web-based intervention for caregivers in addition to center-based lessons. Evaluations are conducted among children, caregivers, and child care staff at fall enrollment, midline, and spring, following intervention completion. Analyses include linear mixed-models, accounting for clustering and repeated measures, incorporating center-arms as moderators. CHAMP will provide evidence-based information to inform wellness guidelines and policies that can be disseminated broadly, to ensure that child care centers provide opportunities for children to develop healthy eating, and physical activity habits.
Keywords: childhood obesity, child care-based intervention, willingness to try new foods, motor skills, cluster randomized controlled trial
Introduction
Pediatric obesity is a major public health problem that often begins early in life and increases the risk for chronic health conditions and health disparities. Excess weight gain by age five is often maintained into adulthood,1,2 increasing the risk of obesity-related co-morbidities later in life. To prevent obesity-related health disparities, interventions must start early in life, before poor dietary and physical activity patterns have been established and excess weight gain has occurred.3,4
A growing number of young children in the United States do not meet dietary guidelines.5–8 One possible explanation is that children are not exposed to healthy choices during early childhood. Children’s food preferences, formed during preschool years, tend to persist into adulthood.9 Children who are willing to try new foods have higher quality diets, compared to children who resist new foods. Food neophobia is a normal developmental phase where children reject unfamiliar foods.10,11 Repeated food exposures (8–12 interactions) are recommended to progress past food neophobia and promote children’s healthier food preferences. 12–15 However, repeated exposures may not be feasible for low-income families who are balancing mealtime efficiency (e.g., not waste time, food, or money) and the desire for their child to develop a preference for fruits and vegetables.16 Although promotion of fruit and vegetable consumption is an effective strategy to prevent obesity and chronic diseases17,18 there is limited evidence on strategies to improve fruit and vegetable intake among preschoolers.19
During the early years, physical activity and motor skills are interconnected,20 with both linked to obesity as well as current and future health indicators.21–23 Motor skill deficits may underlie preschoolers’ failure to meet physical activity guidelines, particularly in underserved low-income areas that have few safe places to be active and develop age appropriate gross motor skills.24 Thus, obesity prevention efforts aimed at altering developmental pathways by targeting food neophobia and gross motor development may improve healthy eating and increase children’s likelihood of being physically active throughout life, ultimately reducing obesity risk.
Child care centers are an ideal setting to prevent pediatric obesity.25 An estimated 5.9 million children (age 3–5) often spend a majority of waking time in child care.26 Wellness guidelines for child care centers are emerging through federal legislation including The Healthy Hunger Free Kids Act of 2010, and the United States Department of Agriculture (USDA) Child and Adult Care Food Program (CACFP), ensuring that children are exposed to healthy food options. Similarly, Healthy People 2020 calls for state regulations ensuring children in child care centers have opportunities to be physically active, along with the World Health Organization’s recently released guidelines for physical activity among children under age 5 years.27 Young children are also uniquely influenced by adults at home.28 Extending intervention strategies from child care centers to the home environment can simultaneously intervene across the different levels of the bioecological model that shape child behavior.
Building on existing studies promoting health in child care settings,29–31 CHAMP (Creating Healthy Habits among Maryland Preschoolers) is a multi-component child care-based intervention designed to improve both physical activity and healthy eating behaviors among preschoolers. CHAMP is comprised of interactive lessons delivered by child care staff and evaluates the impact of incorporating web-based strategies designed for caregivers. Ultimately, through improvements in nutrition and physical activity, CHAMP aims to prevent obesity among preschool children (age 3–5 years) in urban and semi-urban settings.
Methods/Design
Study Design
CHAMP is planned with the collaboration of four partners: the state Department of Health, the state Department of Education (including the Office of Child Care), a statewide network to provide training and support to child care centers, and the state School of Medicine, following a preliminary study conducted among child care centers in three counties.32 The aim of CHAMP is to evaluate strategies to prevent health disparities by building wellness-related habits of diet and physical activity into daily child care activities and extending the habits introduced in child care centers to caregivers. The impact of CHAMP is evaluated by recruiting 54 child care centers throughout Maryland and randomizing them through a 3-arm cluster randomized controlled trial. Centers randomized to the CHAMP group receive a wellness-related habits intervention delivered by child care staff; the centers in the CHAMP+ group receive the CHAMP intervention, plus a caregiver intervention delivered to primary caregivers through a website. Control centers receive intervention materials the following year, with no intervention during the study evaluation period. The hypothesis is that children in child care centers randomized to the CHAMP+ intervention group demonstrate more improvement across domains including gross motor competency, physical activity, food neophobia and maintenance of a healthy body weight from baseline to end line, compared to control centers, with the CHAMP group in an intermediate position (CHAMP+ > CHAMP > control).
Intervention
The CHAMP intervention is based on The Food Friends®, an evidence-based preschool program developed at Colorado State University in partnership with Head Start. The Food Friends curricula is delivered by child care staff and is designed to prevent childhood obesity by establishing healthful eating and physical activity habits early in life.33 The program curriculum is composed of two models: physical activity and eating behaviors. The physical activity component, Get Movin’ with Mighty Moves®, is an 18-week program that promotes gross motor skills implemented 4 days/week for 15–20 minutes per day (72 lessons) during the fall and winter months.34,35 The healthful eating component, Fun with New Foods®, is a 12-week program that provides 15–20 minute twice-weekly nutrition activities (story books, arts and crafts, and sensory activities) and twice-weekly opportunities to try new foods that takes place in the spring. The curricula are based on social cognitive theory and the bioecological model,36–38 utilize social marketing strategies,33,39 incorporate a superhero theme (Super Taster and Mighty Mover) to engage children, and include detailed implementation manuals on lesson plans and classroom activities.40,41 The CHAMP intervention modified Food Friends to make it culturally sensitive and appealing to a mid-Atlantic urban and semi-urban population by altering the vocabulary (i.e. replacing the term “junkie” with “enthusiast” and “sassy” with “friendly”), foods promoted (i.e., replacing, water chestnut for daikon radish, lychee for tangelo, hominy for tempeh) and replacing a puzzle activity with a Montessori based sensory activity (i.e. smelling jars). Alterations to the intervention were piloted in a local child care center the summer before the first cohort. CHAMP staff observed pilot lessons and gathered feedback from child care staff on clarity and acceptability of the lessons and associated materials. Alterations to the intervention were guided by feedback from focus groups and interviews with child care directors.
The CHAMP+ intervention arm extends the child care intervention to caregivers through a caregiver education website, hosted by the university. Each week caregivers in the CHAMP+ arm of the intervention are provided content on physical activity, nutrition, and wellness topics relevant to caregivers of preschoolers and coordinated with the activities conducted in the classrooms. For example, nutrition topics include appropriate serving sizes, strategies to support preschoolers trying new foods, and how to handle picky eating. Physical activity topics include ideas for games and activities for the family. General wellness topics include information on behavior management parenting strategies, toddler sleep, and stress management. Content is created by the interdisciplinary CHAMP research team, which includes registered dietitians, pediatric psychologists, public health professionals, exercise scientists and early childhood education specialists. Evidence-based content is used to create infographics and short videos (i.e. playing and learning strategies [PALS]42, Parent Child Interaction Therapy [PCIT]43). Caregiver intervention content and website usability were piloted in focus groups with caregivers from a local child care center the summer prior to the start of the first cohort. Photos of children participating in the CHAMP+ arm of the intervention are included weekly on the website to increase caregiver engagement. Additionally, quizzes and monthly challenges are available to increase caregiver interaction with the online content. Caregivers in the CHAMP+ arm are notified weekly (by email or text message) when new content is available on the website. Simple Texting is the short message service (SMS) platform used to communicate with caregivers. The platform provides analytics to track the number of users who click on the website link provided in the text message each week.
The CHAMP research team provides a tablet to each of the 54 child care centers. The child care staff use the tablet to take photos of children during the day. Photos are automatically uploaded to a center specific Google cloud. In the CHAMP+ arm, pictures are screened by the CHAMP research team and then uploaded to the CHAMP+ website along with new weekly content. Photos on the website are accessible only to caregivers in the CHAMP+ arm with a password unique to their child care center. For control and CHAMP arms, photos are compiled and returned in electronic form to the centers.
Timing, Recruitment and Randomization of Child Care Centers and Training
Timing
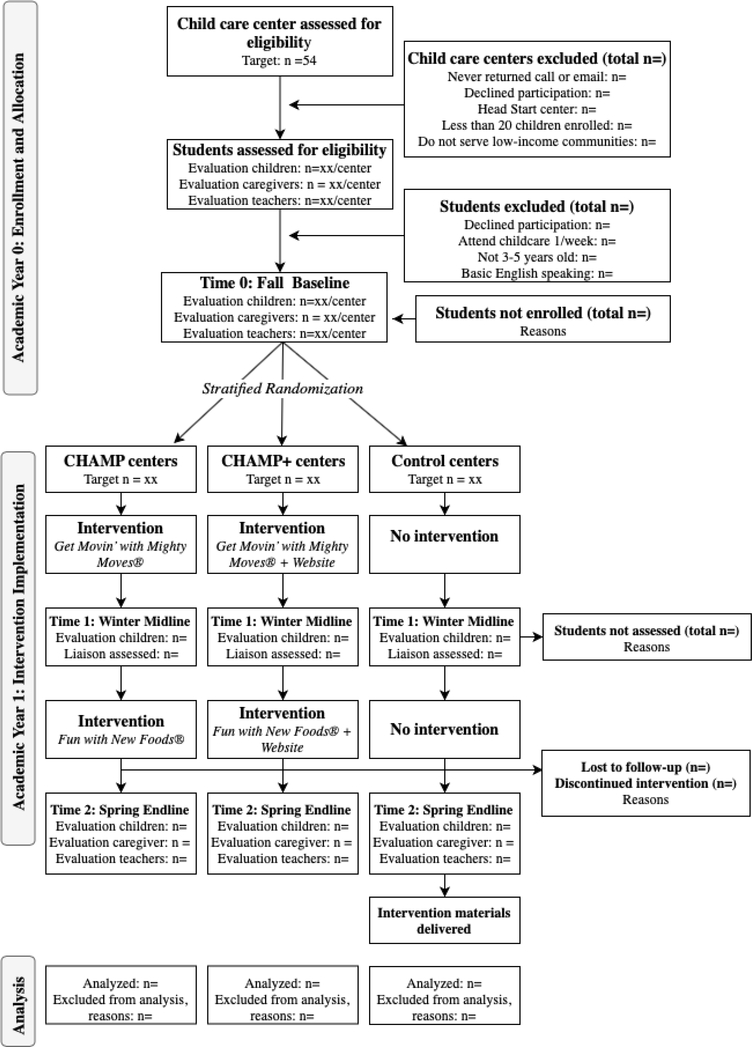
The CHAMP intervention and evaluation are designed to be implemented in one academic year (from August to June). Child care centers and staff are recruited in the summer before the academic year (June/July). Caregivers and children are recruited in August, followed by the baseline evaluation. Child care staff training to administer the physical activity curriculum Get Movin’ with Mighty Moves is conducted in August, and the 18-week Mighty Moves intervention begins following the baseline evaluation and extends through the fall and into the early winter. Staff training for Fun with New Foods (12-week intervention) is conducted at the conclusion of Mighty Moves, and prior to the start of the Fun with New Foods intervention. The Fun with New Foods portion of the intervention extends through the spring. The midline evaluation occurs following the Mighty Moves intervention and the end line evaluation occurs in the spring following the Fun with New Foods intervention (Figure 1).
Figure 1.
Study design and participation flow of CHAMP 3-arm intervention trial
The CHAMP intervention includes 54 child care centers and is implemented over two to three years across two to three different cohorts. Figure 1 describes the planned recruitment, enrollment and participant flow of the study.
Recruitment of Centers
A list of licensed centers is provided by the state Office of Child Care. Eligibility for centers includes: licensed, children age 3–5 years enrolled, and serving low-income communities. Low-income is defined by CACFP participation, acceptance of child care vouchers or a cost of less than $300/week for child care. Head Start centers are excluded due to existing infrastructure to support wellness policies.44 The remaining list of centers is filtered to include those that are within 50 miles of the university and have greater than 20 total children enrolled. The remaining eligible centers are contacted by phone by a CHAMP team member who describes the program, assesses initial eligibility and, in response to interest, sets up an appointment to visit the center and meet the director. Centers with at least 20 children enrolled between the ages of 3–5 are prioritized to allow for adequate sample size. Directors are shown an informational video about CHAMP. They are given information about the intervention, randomization, and evaluation processes. All eligible centers that express interest and complete the initial recruitment visit within the recruitment timeframe are invited to participate.
Randomization
Following recruitment of all centers within a cohort, centers are randomized using a stratified cluster randomization procedure. CHAMP staff match centers into stratified groups of three based on similarity of center size, location (urban/semi-urban), and racial/ethnic mix. Centers within the stratified group of three are then randomized (using a computer-generated random number with equal randomization allocation ratio) to one of the three intervention conditions (CHAMP, CHAMP+, and control), to maintain demographic balance across the three conditions. Randomization is conducted by a member of the research team not involved in data collection or intervention implementation.
Child Care Training
Trainings are conducted by the CHAMP research team in each child care facility. Child care staff receive two training sessions during the year which last approximately 1–2 hours each. During the trainings, child care staff are provided with general psychoeducation regarding childhood obesity, food neophobia and gross motor development. Child care staff are introduced to the intervention materials (including the provided materials and manualized lessons) and hands-on participatory activities are demonstrated and practiced. Child care staff are encouraged to discuss potential barriers and strategies to fit lessons into the existing curriculum at each center. Child care staff and directors receive a printed manual and have access to a staff website where they can access weekly lessons plans, handouts, additional resources and program content including music to accompany lessons. Each week, lesson plans are emailed or texted to child care staff. Child care staff in the CHAMP+ arm receive additional information about the caregiver website.
Liaisons, Eligibility and Recruitment of Children and Caregivers
A multi-step approach is used to recruit child care center directors, child care staff, and children and caregivers within centers. The center ‘liaison’ is a child care staff member whose job is to communicate with CHAMP research staff throughout the project. The eligibility and recruitment process for each role are described below.
Child Care Director
As described above, child care directors are initially contacted. They are given information about the intervention, randomization, and evaluation processes, and shown an informational video about CHAMP. After an initial in-person meeting with CHAMP research staff to verify center eligibility and answer any questions, child care directors can either agree or decline for their center to participate in the project.
Liaison
After participating centers are recruited, center directors identify a ‘liaison’ who serves as the contact person responsible for communication between CHAMP and the child care center. Eligible liaisons must be employed at the child care center, and be willing to communicate with the CHAMP staff on a regular basis and complete several center level questionnaires (listed below). Liaisons can include directors or child care staff.
Child Care Staff
Child care directors in participating centers identify potentially eligible staff members who are then contacted by the CHAMP research team. Classroom staff are eligible if they have direct contact with students (age 3–5) in their classroom, are willing to fill out questionnaire measures and if they agree to receive training and deliver the intervention.
Eligibility of Children and Caregivers
The intervention is delivered to all children in a classroom at participating centers. Children attending participating child care centers (at least 3 days per week) are eligible to be enrolled in the evaluation portion of the study if they are: between the ages of 3–5, are English speaking, their caregiver intends that the child will be enrolled in the center through the spring, and their caregiver signs the informed consent. Children with developmental delays that prevent assessment of key study outcomes (i.e. severe autism, Down syndrome) are excluded from participating in the evaluation. Children with physical disabilities that prevent them from participating in physical activities may be enrolled in the evaluation, though not assessed for gross motor skills. Siblings in the same center are eligible to participate in the evaluation. Siblings are flagged for sensitivity analyses during data analysis. Caregiver eligibility criteria include: being the child’s primary caregiver (living with the child for more than 3 days each week) and basic English literacy (per caregiver self-report).
Recruitment of Children and Caregivers
Liaisons assist with recruitment of children and caregivers in each center. CHAMP staff and center liaisons develop a child/caregiver recruitment plan for each center. Plans include flyers sent to caregivers, posters displayed in the center, and a short CHAMP video that outlines the program, presentations at back-to-school nights, and CHAMP staff attendance at drop-off/ pick-up times to talk directly with caregivers. Liaisons inform families about the program, collect consent forms and relay information between child care staff and the CHAMP research team. Liaisons are incentivized to recruit eligible participants (up to 20 children per center) with a gift card (maximum $50).
Ethical approval
The protocol is approved by the ethics committee of the university conducting the investigation. Caregivers provide written consent for their child to participate in the study, including consent to have child care center staff take photos of their child that are returned to the centers. Caregivers in the CHAMP+ centers provide additional consent to have their child’s picture uploaded to a secure website hosted by the university. Caregivers and child care staff provide consent for themselves through online explanations and consent forms. Child care staff are invited to participate in a direct assessment of physical activity by wearing an Actical accelerometer; written consent is provided separately for this portion of the study. Verbal child assent is obtained by research staff during data collection.
Sample Size Estimation
The proposed study design is a cluster-randomized trial, with individual preschoolers nested in child care centers (clusters). We anticipate enrolling 864 children across 54 centers (an average of 16 children per center). Power and sample size estimates are calculated with the GLIMMPSE 2.0 online tool designed for multilevel data.45 Based on previous literature, we assume an average ICC of 0.03. This is an average intraclass correlation coefficient (ICC) estimate across outcomes based on previous studies reporting ICCs of 0.06 for child body mass index (BMI),46 0.08 for child moderate-vigorous physical activity (MVPA),47 0.001 for willingness to try new foods,48 and 0.001 for fruit and vegetable consumption.49 We assume a correlation of (r = 0.5) between repeated measures of the same individual.
After accounting for a loss-to-follow-up rate of 20% (higher than anticipated) our proposed sample size will provide adequate power (> 0.8) to detect an effect as small as 0.27 standard deviations (SD) across outcomes (Cohen’s d=0.27). An effect of this size is roughly equivalent to about a 10-minute difference in MVPA, a 7% greater probability that a child will try a novel food (based on pilot data), a 6-point increase in gross motor skill percentile score,50 or a 0.3 difference in BMI z-score.51 An effect of this magnitude is plausible given results of our previous interventions where we detected an intervention effect size of 0.27 on toddler’s total fruit consumption, as part of a randomized trial of obesity prevention among toddlers.52
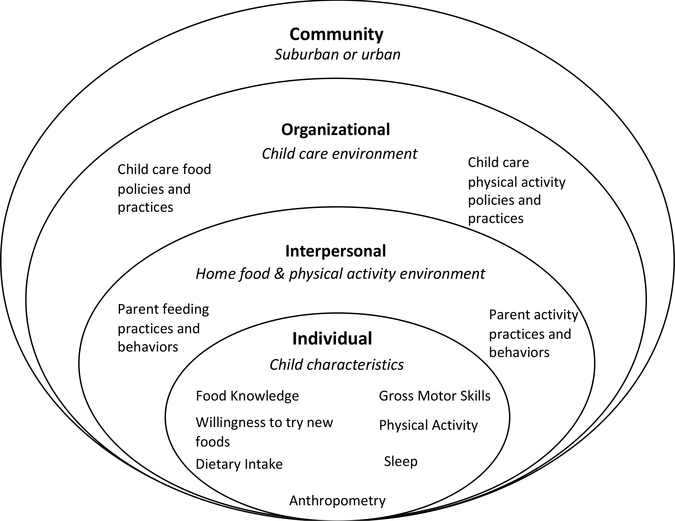
Measures
Assessments for CHAMP range across multiple levels of the bioecological model from the individual child to the interpersonal- and organizational-levels (caregivers and child care staff) and community-level (child care environment) with combined key constructs from the social cognitive theory (Figure 2). The individual level shows interactions between child characteristics in relation to eating and physical activity behaviors that ultimately influence healthy growth and development. The interpersonal level is characterized by the home food and physical activity environment that can concomitantly be shaped by and influence children’s behavior. At the organizational and community levels, CHAMP strengthens and expands collaborations with key players and policies governing state health and education systems that influence preschool eating and physical activity behaviors.
Figure 2.
Conceptual model for CHAMP intervention based on Bellows et al. (2013)53
Observational Child Measures
Child-related measures are described below and summarized in Table 1. The following measures are collected by trained CHAMP data collectors at the child care centers. CHAMP data collectors are unaware of the center’s randomization group. Data collectors receive at least two hours of initial training and one hour of booster training on each of the assessment measures below.
Table 1.
List of Child Measures
| Child Measures | Method | Baseline | Midline | End line |
|---|---|---|---|---|
| Anthropometry | ||||
| Weight, height, waist circumference | Direct | X | X | X |
| Gross Motor Skills | ||||
| Test of Gross Motor Development 2- Object Control | Direct | X | X | X |
| Test of Gross Motor Development 2- Locomotor | Direct | X | X | |
| Physical Activity/Sedentary Behavior/Sleep | ||||
| Actical Accelerometer | Direct | X | X | |
| Eating/Nutrition/ Dietary Habits | ||||
| Willingness to Try New Foods | Direct | X | X | |
| Fruit & Vegetable Knowledge | Direct | X | X | |
| Food Neophobia Scale – Child Version | Caregiver-proxy report | X | X | |
| Child Dietary Habits (Food Frequency Questionnaire) | Caregiver-proxy report | X | X | |
| Child Eating Behavior Questionnaire (CEBQ) | Caregiver-proxy report | X | X | |
| Child Behavior | ||||
| Child Screen Time Assessment | Caregiver-proxy report | X | X | |
| Child Strengths & Difficulties Questionnaire* | Caregiver-proxy report | X | ||
| Child Sleep Habits Questionnaire* | Caregiver-proxy report | X | ||
| Behavior Rating Inventory of Executive Function (BRIEF) – Inhibitory & emotional control subscales* | Caregiver-proxy report | X |
Measures with asterisks are considered auxiliary outcomes
Anthropometry (Primary Outcome)
Height, weight, and waist circumference are measured at baseline, midline, and end line, after removing children’s jackets, sweaters, and shoes. Height is measured with a portable stadiometer (Shorr Productions, Olney, Maryland) to the nearest 1 cm. Waist circumference is measured at the navel to the nearest 0.1 cm. Height and waist circumference measures are performed three times. Measures are repeated until difference between them is less than 2.0 cm. Weight is measured with TANITA BWB-800 (TANITA, Tokyo, Japan) digital scales to the nearest 0.1 kg. Weight measurement is performed twice and a third time if the two initial measures are not identical. BMI is calculated as weight in kg divided by height in meters squared; BMI-for-age z-scores (BMIz) are calculated based on the age- and sex-specific 2000 CDC Growth Charts.54
Gross Motor Skill
The Test of Gross Motor Development-2 (TGMD-2)55 is a norm-referenced instrument designed to assess gross motor development among children aged between three and 10 years and encompasses two sub-tests that evaluate locomotor and object control mastery. Skills such as throwing and catching a ball, running, hopping, and jumping are observed and rated as “1” (accurate completion) or “0” (non-completion). The TGMD-2 has been widely used in evaluating fundamental movement skills among typically developing children and shown to be a reliable and valid measure of gross motor development.56,57 Children are tested individually by two trained CHAMP data collectors. One data collector is responsible for demonstrating the 12 skills to the child while the second data collector records the scores on a tablet using the open source data collection software Epicollect (www.five.epicollect.net). Data collectors complete over 5 hours of training using a combination of videos and in-vivo assessments of preschoolers engaging in the 12 skills. Training includes group discussion, scoring consensus, and role-playing scenarios. Data collectors must achieve reliability above Kappa = 0.75 to score the TGMD-2.58 Follow-up training is conducted halfway through baseline data collection to prevent drift and preserve inter-rater reliability.
Objective Physical Activity
Actical accelerometers (Philips Respironics, Minimiter, Bend, OR) are secured on hospital bands and attached to the lateral malleolus of the non-dominant ankle of the children and worn continually for at least 7 days. The Actical is a small, light-weight, and waterproof device that can be worn throughout all activities—sleeping, swimming, and running.59 Actical protocols and data cleaning are based on previous studies which have used this device to measure physical activity and sleep among young children from low income families.59,60 Accelerometers are configured using Actical software (version 3.11) and data are collected in 15-sec intervals. At the child care centers, trained research assistants remove children’s accelerometers after seven consecutive days. Days with less than 20 activity counts per 15 seconds and 80 activity counts per minute are considered incomplete and are not included in analyses. Additionally, only data collected over a 24-hour period are included in analyses, meaning the first and last partial days are removed. If children wear the Actical longer than a week, the excess days are truncated.59 Age specific thresholds are applied to categorize MVPA, light and sedentary activity.59 Sleep is parsed from accelerometer data using the Sadeh sleep algorithm.61,62
Willingness to Try New Foods
To assess children’s willingness to try novel foods, children are presented with a flight of 9 foods; 6 novel and 3 familiar, following published methods.14,53 Such protocols have been shown to be sensitive to changes in children’s willingness to try new food and associated with parental reports of food neophobia.53 Novel foods are defined using pilot data indicating that the food is unknown to at least 75% of preschool children. The foods range from sweet to savory and include edamame (6g), papaya (6g), chick peas (6g), water chestnut (6g), olive (6g), kidney bean (6g), whole wheat cracker (4g), grapes (9g), and cheese (13g). Children are presented one food at a time and asked whether they know the food, what the name of food is, if they have eaten the food, and to rate the food as “Yummy”, “Yucky” or “Just Ok.” Children respond verbally or by pointing to visuals displaying faces that correspond to the descriptions. After answering the prompts, children are given 10 minutes to try the foods if they choose. A CHAMP data collector records the order and whether each food is tried or refused. Data collectors also note if a child discusses, smells, touches, or spits out each food. After 10 minutes, children are asked to rate each food a second time. Each food is weighed on a portable digital scale (Taylor 1020NFS) and subtracted from the initial food weight to determine consumption. All food assessments are conducted in the mornings prior to children’s lunchtime. Time of assessment is recorded and can be controlled for in analysis if needed.
Fruit & Vegetable Knowledge
The Fruit & Vegetable Knowledge assessment captures children’s knowledge of fruits and vegetables.63 Following two sample items to ensure children’s understanding of the task, each child is shown photographs of 9 fruits, 10 vegetables, and 1 common food (French fries). After each picture, a CHAMP data collector asks 3 questions: “What is this food?” “Have you eaten this food?” “Do you think it is “Yummy”, “Yucky”, or “Just OK”? CHAMP data collectors are trained to remain neutral. This measure has good internal consistency (α = .87), test-retest reliability (r = 0.73) and has been shown to be predictive of food consumption.63
Child-related Caregiver Report Measures
The following measures are completed by the child’s primary caregiver using the web-based questionnaire system Qualtrics. Caregivers are reimbursed with a gift card (between $20–40) for the completion of the questionnaires. All caregivers are asked to complete the primary measures. Secondary measures are offered to caregivers for an additional gift card incentive.
Child Food Neophobia
Caregivers complete the Food Neophobia Scale (child version) that assesses a child’s willingness to try new foods. The 10-item questionnaire uses a 7-point Likert scale ranging from “Strongly Agree” to “Strongly Disagree.” This measure has been shown to be reliable (α =0.88)64 and has been validated against behavioral observations of willingness to try new foods, and caregiver predictions of child’s willingness to try new foods.53
Child Dietary Habits (Food Frequency Questionnaire)
A 17-item short Food Frequency Questionnaire (sFFQ)65 is used to assess children’s dietary habits. The caregiver report questionnaire is designed to assess preschoolers’ usual eating habits for: daily servings of fruit, daily servings of vegetables, daily cups of beverages (e.g., milk, soft drinks, fruit juice, and water), and frequency of eating red meats, processed meats, take-out foods, snack foods, and desserts. The questionnaire also assesses behavioral habits including the regularity of consuming breakfast and eating in front of the television. The measure has been shown to be reliable66 and moderately valid to quickly assess dietary habits of 2–5 year-old children65 and has been used in similar obesity prevention cluster randomized trials.67
Child Eating Behavior
The Child Eating Behavior Questionnaire (CEBQ)68 is a caregiver-report measure designed to assess dimensions of a child’s eating style. It is comprised of 8 scales: Food Responsiveness (α = 0.80), Emotional Over-Eating (α = 0.79), Enjoyment of Food (α = 0.91), Desire to Drink (α = 0.89), Satiety Responsiveness (α = 0.74), Slowness in Eating (α = 0.74), Emotional Under-Eating (α = 0.74), and Food Fussiness (α = 0.91). The CEBQ is comprised of 35 items, each scored on a five-point Likert scale that ranges from 1= Never to 5= Always. It has been shown to have good internal consistency and test-retest reliability.68
Child Screen Time
Caregivers report on children’s screen time (smart phone, tablet, television, video game, and computer) during weekdays and weekends by responding to the prompt “How much screen time does your child have on an average weekend/weekday.” Similar single items measures have been used as part of the national Health and Nutrition Examination Survey (NHANES) to assess screen time among preschoolers and shown to be associated with obesity69 and active play.70
Auxiliary Child-related Caregiver Report Measures
To minimize participant burden, caregiver questionnaire measures are prioritized between primary and secondary. Caregivers are invited to complete the secondary questionnaires for additional compensation following the completion of the primary measures. Sensitivity analyses are conducted to examine predictors of those caregivers willing to complete the secondary measures. Measures selected as secondary focus on proposed mechanisms or moderators of treatment effectiveness. Exploration of potential moderators and mediators will inform future studies.
Child Strengths & Difficulties
The 25-item Child Strengths and Difficulties Questionnaire (SDQ) assesses child attributes (10 strengths, 14 difficulties, and 1 neutral) divided between 5 scales of 5 items each: Hyperactivity, Emotional Symptoms, Conduct Problems, Peer Problems, and Prosocial.71 The questionnaire uses a 3-point Likert scale ranging from “Not true”, “Somewhat true”, to “Definitely true”. The SDQ has shown to be reliable and has been validated against the well-established Rutter Child Behaviour Questionnaire which measures emotional and behavioral problems in young children.71
Child Sleep Habits
Caregivers report on children’s usual sleep quantity, and the previous week perceived quality and adequacy of children’s sleep using an abbreviated 18-item version of the Children’s Sleep Questionnaire.72 For each item, caregivers report the frequency of a sleep problem in the previous week on a scale from “rarely” (0–1 night/week), “sometimes” (2–4 nights/week), to “usually” (5–7 nights/week). This measure has shown adequate internal consistency (alpha = 0.68) and satisfactory test-retest reliability (alpha 0.62–0.79)73 and shown to be associated with children’s sleep measured via actigraphy and distinguish between children with and without clinical sleep difficulties.74
Child Inhibitory and Emotional Control
Children’s ability to modulate actions, responses, emotions, and behaviors is measured via the brief version of the caregiver-administered Inhibitory Self-Control Index on the Behavior Rating Inventory of Executive Function (BRIEF).75 The index is composed of the Inhibit and Emotional Control subscales. The BRIEF is normed among preschoolers in the United States, and has shown good internal consistency (α >.80), test-retest reliability and has been validated for use among preschool samples.76
Caregiver and Household Measures (Caregiver Report)
Demographics
Primary caregivers report on demographics including age, race/ethnicity, gender for themselves and the participating child. Additionally, caregivers report on the number of children and adults in the home, annual income, marital status, caregiver level of education and employment status. Caregiver weight and height are self-reported. A summary of caregiver and household measures, method of assessment, and timing of data collection is presented in Table 2.
Table 2.
Caregiver demographic, behavioral and household environment measures
| Method | Baseline | Endline | |
|---|---|---|---|
| Anthropometry/Demographics | |||
| Caregiver Weight & Height | Self-Report | X | X |
| Demographics | Self-Report | X | |
| Caregiver Health Behaviors | |||
| Food Behavior Checklist | Self-Report | X | X |
| International Physical Activity Questionnaire (IPAQ) | Self-Report | X | X |
| Caregiver Feeding/ Nutrition Environment | |||
| Comprehensive Feeding Practices Questionnaire | Self-Report | X | X |
| Screening Questionnaire for Food Insecurity (2 items) | Self-Report | X | X |
| Home Assessment for Physical Activity & Healthy Eating Environment | Self-Report | X | X |
| Caregiver Psychological Factors | |||
| Parenting Sense of Competence (PSOC)* | Self-Report | X | |
| Weight Related Eating Questionnaire (WREQ) * | Self-Report | X | |
| Contour Drawing Rating Scale* | Self-Report | X | |
| Preschooler Silhouettes [Perceived Child Body Size]* | Self-Report | X | |
| Spielberger State-Trait Anxiety Inventory (STAI)* | Self-Report | X | |
| Perceived Stress Scale (PSS)* | Self-Report | X | |
| Center for Epidemiologic Studies Depression Scale (CESD-R 10)* | Self-Report | X |
Measures with asterisks are considered auxiliary outcomes
Caregiver Dietary Intake
The Food Behavior Checklist questionnaire77 (16 items) is designed to be easy to administer and includes representative visuals to improve accuracy of the self-reported information. Items are separated into 5 topics to assess usual food-related behaviors: usual daily fruit and vegetable intake (α = 0.79), consumption of dairy items (α = 0.67), fat and cholesterol (α = 0.28), perceived diet quality (α = 0.61), and food security (α = 0.85)78. An additional question also assesses nutrition label understanding. Items have been shown to be correlated with biomarkers for food intake and 24-hour recall measurements.79 This measure has been used with caregivers in similar preschool obesity prevention studies.80
Self-reported Physical Activity
The International Physical Activity Questionnaire (IPAQ) is a 27-item seven-day recall of activity classified as either “vigorous” or “moderate”. This self-reported activity measure has been validated and demonstrated good reliability.81 The IPAQ consists of four different subscales: Job-Related Physical Activity, Transportation Physical Activity, Housework and Caring for Family, Sedentary Activities, and Recreation and Leisure-Time Physical Activity.
Caregiver Feeding Practices
The Comprehensive Feeding Practices Questionnaire (CFPQ)82 is a self-report measure to assess the feeding practices of caregivers of young children. It is comprised of 12 factors: Monitoring, Emotion Regulation, Food as a Reward, Child Control, Modeling, Restriction for Weight, Restriction for Health, Teaching Nutrition, Encourage Balance and Variety, Pressure, Healthy Environment, and Involvement. Internal consistency has been shown to be adequate to good (alpha = 0.58–0.81).82 The CFPQ has also demonstrated convergent validity with caregiver attitudes regarding child weight and responsibility for feeding.82
Household Food Security
A two item food insecurity screening questionnaire identifies families at risk for food insecurity. It contains 2 questions rated as ‘Often True’ to ‘Sometimes True’ to ‘Never True’. The 2-item measure has been found to demonstrate sensitivity (97%), specificity (83%), and convergent validity with the USDA Household Food Security Survey Module measure of food insecurity.83
Home Assessment for Physical Activity & Healthy Eating Environment
The Home Environment Inventory is used to assess accessibility/availability of foods and parenting behaviors. The inventory is comprised of the Fruit and Vegetable Availability subscale, Fats and Sweets Availability subscale, Physical Activity subscales for Parental Modeling and Policies 84 and the Beverage Availability subscale.85 Responses are rated on a 5-point scale: Never, Rarely, Sometimes, Frequently, Always.84 The Fruit and Vegetable Availability subscale has been shown to have high internal and test-retest reliability (α =0.84–0.82 respectively) and is associated with caregiver healthy role modeling and child nutrition.84 The Parental Modeling and Polices subscales have been shown to be moderately reliable (α =0.68–0.79) and associated with objective child physical activity and caregiver physical activity.84
Auxiliary Caregiver and Household Measures (Caregiver Report)
Parenting Sense of Competence
The Parenting Sense of Competence (PSOC) scale is used to measure parenting self-esteem.86 This questionnaire is comprised of 17 items measured on a 6-point scale ranging from “strongly agree” to “strongly disagree.” The questionnaire consists of two subscales; Satisfaction (α =.76) which measures liking the parenting role, and Efficacy (α =.88) defined as a caregivers’ perceived competence in the parenting role. The questionnaire has been validated for use among caregivers of infants up to elementary school-aged children.87,88
Weight Related Eating
Weight Related Eating Questionnaire (WREQ) is a 16-item, four-factor questionnaire which measures two constructs of dietary restraint (Routine and Compensatory Restraint), susceptibility to external cues (External Eating), and Emotional Eating. The questionnaire has shown to have good reliability (α = .76–.90) and has been validated against similar disordered eating inventories.89
Caregiver Body Size Perception/Dissatisfaction
The Contour Drawing Rating Scale consists of 9 gender specific contour drawings that are graduated in sizes. Participants are asked to select a body silhouette that most resembles their own body size. They are then asked to select the size they would like to be. The difference between current and ideal size is used to calculate body dissatisfaction. There is evidence to support strong test-retest reliability and validity to measure body size-perception and body size dissatisfaction.90
Perceived Child Body Size/Dissatisfaction
Caregivers’ perception of their child’s body size is assessed by figure silhouettes of 4-year-old children.91 These rating scales consist of line drawings of children’s bodies designed to be age and race appropriate. Caregivers are shown images containing seven figures which correspond to the gender and race of their child. They are prompted to view the images and indicate which of the seven figures most closely resembles the current size of their child and the ideal size or which child figure they would desire for their child. The difference between ideal and current size is used to define body size dissatisfaction. BMI for each child figure is determined by applying the volume to the CDC age-and gender-specific growth charts for 4 and 5 year-old children, and has been validated among mothers of preschool children91 and found to be reliable among parents of young children.92 Accuracy of child body size is determined by the response to the question, “Which picture looks most like your child?” with an allowance of 1 silhouette on either side of the child’s measured BMI.
Caregiver Anxiety
The 6-item short form of the State-Trait Anxiety Inventory (STAI) is one of the most frequently used measures of anxiety in applied research and has been shown to be a reliable (α = 0.82) and sensitive measure of anxiety.93 The six-item short-form of the STAI produces scores similar to those obtained using the full 20-item STAI across subject groups manifesting normal and raised levels of anxiety.94
Caregiver Perceived Stress
The 4-item Perceived Stress Scale (PSS)95,96 measures the degree to which situations in the previous month are appraised as stressful. The assessed items are general in nature rather than focused on specific events or experiences. Answers are rated on a 5-point scale. The PSS is designed for use in community samples and has been used to assess parenting stress. The measure has been shown to have acceptable psychometric properties.97
Caregiver Depressive Symptoms
The CESD-R (Center for Epidemiologic Studies – Depression Scale (Short Form)) is designed to measure depressive symptomatology in the general population. The scale is one of the most widely used instruments in the field of psychiatric epidemiology and has been shown to have good validity and reliability.98
Child Care Staff Measures
The following measures are assessed using the web-based questionnaire system Qualtrics. Child care staff are compensated with a gift card for the completion of all questionnaires. Table 3 provides an overview of the child care staff measures. Weight and height, and demographics are self-reported by child care staff.
Table 3.
Child care staff demographic and behavioral measures
| Child Care Staff Measures | Method | Baseline | End line |
|---|---|---|---|
| Anthropometry/Demographics | |||
| Child Care Staff Height & Weight | Self-Report | X | X |
| Demographics | Self-Report | X | |
| Child Care Staff Health Behaviors | |||
| Actical Accelerometer | Direct | X | X |
| International Physical Activity Questionnaire (IPAQ) | Self-Report | X | X |
| Food Behavior Checklist | Self-Report | X | X |
| The Pittsburg Sleep Quality Index (PSQI) | Self-Report | X | X |
| Child Care Staff Feeding/ Nutrition Environment | |||
| Child Care Staff Feeding Attitudes | Self-Report | X | X |
| Child Care Staff Child Feeding Knowledge | Self-Report | X | X |
| The Child Care Food and Activity Practices Questionnaire (CFAPQ) | Self-Report | X | X |
| Child Care Staff Psychological Factors | |||
| Spielberger State-Trait Anxiety Inventory (STAI) | Self-Report | X | X |
| Perceived Stress Scale (PSS) | Self-Report | X | X |
| Weight Related Eating Questionnaire (WREQ) | Self-Report | X | X |
| Screening Questionnaire for Food Insecurity (2 items) | Self-Report | X | X |
| Center for Epidemiologic Studies Depression Scale (CESD-R 10) | Self-Report | X | X |
| Contour Drawing Rating Scale | Self-Report | X | X |
Child Care Staff Demographics
Child care Staff report information including age, race/ethnicity, gender. Additionally, staff report on the number of children and adults in the home, annual income, marital status, level of education and employment status. Staff weight and height are self-reported. A summary of child care staff measures, method of assessment, and timing of data collection is presented in Table 3. Part of the survey given to caregivers is also applied to child care staff and teachers. Similar questionnaires include: Dietary Intake77, Objective and Self-Reported Physical Activity81, Body Size Perception/Dissatisfaction90, Food Security83, Anxiety93, Stress95,96, Depressive Symptoms98, and Weight Related Eating.89
Child Care Staff Sleep Quality
The Pittsburg Sleep Quality Index (PSQI) is used to assess child care staff sleep. The PSQI self-report measure of sleep quality, quantity and disturbance retrospectively over a 1-month period. The PSQI has been shown to distinguish between “good” and “poor” sleepers in clinical populations and shown to have acceptable internal consistency (α = .83).99
Child Care Staff Feeding Attitudes
The Child Care Provider Healthy Eating & Activity Survey (CCPHEA) is a 14-item questionnaire to assess child care providers’ beliefs and practices, regarding their role in child eating behaviors. Items are scored on a four point Likert scale from “strongly disagree” to “strongly agree” and “low priority” to “high priority.” The subscales of Efficacy, Misconceptions, Feeding Knowledge, and Priority have shown good internal consistency (α = .75, .70, .71, and .64 respectively)100 and demonstrated initial validity.4,101
Child Care Staff Food and Activity Practices
The Child Care Food and Activity Practices Questionnaire (CFAPQ) is comprised of items from the CFPQ (described above) and select items from the Preschooler Physical Activity Parting Practices (PPAPP) questionnaire. The questionnaire is adapted for child care settings show sufficient internal consistency (α = 0.53 to 0.96).102
Child Care Staff Child Feeding Knowledge
Child care staff feeding knowledge is assessed using a self-report measure consisting of 13 true or false questions, and been shown to have both face and construct validity. 103
Child Care Center Measures
Center-level measures are collected via staff-report or via observation by a trained CHAMP data collector (Table 4).
Table 4.
Child care center-level measures
| Child Care Center Measures | Method | Baseline |
|---|---|---|
| EPAO | Direct Audit | X |
| NAP-SACC Self-Assessment Instrument | Staff Report | X |
Nutrition and Physical Activity Self-Assessment for Child Care
NAP-SACC self-assessment instrument details the physical activity and nutrition policies and practices in child care settings, from the perspective of the director and staff.104 Previous studies indicate that this self-assessment is a stable and reasonably accurate instrument.104 The NAP-SACC self-assessment instrument is completed by all center liaisons prior to the intervention.
Environmental Policy Assessment and Observation
The EPAO measure is a comprehensive instrument that assesses the nutrition and physical environment of child care facilities. The EPAO has demonstrated good interobserver agreement (~80%)105 and has been shown to be associated with children’s physical activity.106 The measurement includes a one-day observation of a classroom for children age 3–5 years and review of center documents (food menus, guidelines, and policies) per child care center. CHAMP data collectors receive 4–5 hours of training on the EPAO to ensure reliability of information gathered. Data collection training and certification consists of video and in-person mock assessment compared to an experienced observer (gold standard). Data collectors must reach a reliability of Kappa > 0.7, prior to collecting data.
The EPAO and the NAP-SACC self-assessment instrument are similar measurements, however the EPAO is an observational non-biased collection of data from a researcher and the NAP-SACC self-assessment instrument is reported by a child care staff member (liaison).107 The NAP-SACC is conducted prior to randomization, and the EPAO is collected during the course of the intervention.
Process Evaluation
Monitoring of intervention implementation is assessed weekly by the CHAMP research team. Implementation indicators for Reach, Fidelity and Participant Responsiveness are based on existing literature.108–110 Process indicators are measured at the child and caregiver levels and differ conceptually to better capture the distinct nature of the intervention implemented at each level. For instance, process evaluation indicators for caregivers are based on the website intervention and include only caregivers in the evaluation sample assigned to CHAMP+ arm. Website process evaluation data are derived from Google analytics weekly reports generated online by two trained data collectors.
Process evaluation for children reflects the implementation of the child care-based CHAMP curriculum as delivered by child care staff. Trained data collectors conduct weekly phone calls with child care staff/center liaisons to gather information on implementation indicators. Each week child care staff report child care attendance, number of lessons implemented, and any challenges with implementing the CHAMP curricula. In addition, trained data collectors conduct in-person visits to the center to observe at least two lessons throughout the intervention. The in-person data collection informs data reported by child care staff over the phone using a paper instrument modified from previous childhood interventions.111–113 Only centers assigned to CHAMP and CHAMP+ arms are assessed for process evaluation and information gathered reflects the entire classroom, extending beyond the child evaluation sample.
Reach is defined for caregivers as the total number of individuals using the website per week (i.e. unique IP addresses). Reach for children is defined as the number of children (age 3–5 years) receiving CHAMP lessons in child care.
Fidelity measures the extent to which the intervention was delivered as planned.108 For children, fidelity is defined as the quality and integrity of intervention lessons delivered as described in the implementation protocol (e.g., lesson objectives met (assessed via direct observation by the CHAMP research team)). For caregivers, this is defined as the extent to which teachers upload photos of the lessons to the website, number of weekly content uploads to the website (e.g., number of recipes, infographics, videos, and challenges), and number of text messages and email reminders sent. Caregivers are sent one text message per week (n=28) through the Simple Texting SMS marketing service. They also receive weekly text messages containing the website link when content is uploaded to the website.
Participant Responsiveness measures the extent to which the target audience view, receive, or actively engage with CHAMP materials.108 For children, responsiveness is defined as the number of food sampling opportunities staff provided each week. For caregivers, this is defined as average amount of time per week caregivers spend on the CHAMP website, number of unique IP address log-ins to the website, and participation in CHAMP website quizzes and monthly challenges. This is calculated as the Website Engagement Index (see Table 5). An engagement index (EI)114 is used to characterize and quantify participant interaction with the CHAMP+ website and it is one of the domains of Dose Received. The Engagement Index includes five sub-indices (Table 5). Metrics needed to calculate the sub-indices are identified a priori and extracted from Google analytics. The Engagement Index formula is combined to assign an overall score as well as individual index scores. Data are collected at the unit of unique IP address.
Table 5.
Engagement index (EI) indices and metrics
| Indices | Definition | Analytic Equivalent |
|---|---|---|
|
Click Depth Index (Ci) |
The number of pages viewed in one session (session = 30 minutes) by a single internet connected device | pages/session |
|
Loyalty Index (Li) |
How many sessions per user | # of sessions per user |
|
Interaction Index (Ii) |
# of links clicked, # of interactive text, email message sent | links clicked from text/email messages |
|
Recency Index (Ri) |
How many days since last visit to the website | # of days since last session |
| Feedback Index (Fi) | Short website survey given at the final time point |
Sustainability
Following the intervention period, child care staff are asked about potential sustainability in exit interviews (see supplemental file 1). For centers in the intervention conditions (CHAMP and CHAMP+) child care staff are contacted following the intervention year and invited for in-depth interviews to assess barriers and facilitating factors for continuing to deliver the intervention with reduced CHAMP team technical support. The CHAMP team continues to monitor the CHAMP+ website engagement which remains available for the CHAMP+ centers. Child care staff are encouraged to send reminders to caregivers about the website.
Data Management and Analysis
Direct data entry systems (i.e. Qualtrics, EpiCollect) are used when possible to minimize data entry errors. Manually entered data are double entered by independent research assistants. Range and plausible value checks are conducted prior to any formal data analysis. Data are de-identified and stored on a password protected server. A Data and Safety Monitoring Board (DSMB) is assembled and meetings are held annually to review study progress and monitor for adverse events.
Intent-to-treat analyses are conducted for the primary outcomes. Initially descriptive analyses are conducted, including frequencies, means and standard deviations. Initial bivariate relationships between the sociodemographic variables and the outcome variables are examined to determine potential covariates. Analyses are adjusted for any significant relationships (covariates) in hypotheses testing. The initial hypothesized covariates are child age, race/ethnicity, sex, and family socioeconomic status (SES). Other candidate variables include household food security and caregiver age, sex, and education.
The primary outcomes are gross motor competence, physical activity, avoidance of food (neophobia), and maintenance of a healthy body weight. To assess the intervention effects, linear mixed models (LMM) are conducted for continuous outcomes variables (e.g., gross motor competence, physical activity, neophobia), and generalized linear mixed models (GLMM) are conducted for categorical outcome variables (e.g. child overweight or obesity). Models account for (1) repeated measures within each individual (e.g. child, caregiver, or staff), and (2) clustering of the individuals within each child care center. All analyses are conducted adjusting for location of child care centers (urban versus semi-urban) and other possible confounders (e.g. child’s age, race/ethnicity, sex and SES for caregiver or children’s outcomes). Nested model fit indices (AIC, BIC and −2LL) are used to determine if inclusion in the model improves model specification. Intervention is a three-category variable (control, CHAMP, CHAMP+). Two dummy variables are created (CHAMP, CHAMP+) with the control as a reference group. Time is also a three-categorical variables (baseline, midline and end line) and two dummy variables are created (midline and end line) with baseline as a reference group.
Discussion
Increases in child care enrollment make the child care setting ideal for childhood obesity prevention efforts. As enrollment in child care centers increases throughout the United States,26 CHAMP represents a timely investigation with the potential to inform policies and programs to advance children’s health and well-being. Not only do the majority of preschool-age children with working mothers attend a child care center for an average of 30 hours per week,115,116 but they often eat two meals and at least one snack and engage in both indoor and outdoor physical activities. During the preschool years, children are building daily habits that can last throughout childhood. Daily preschool activities provide opportunities to ensure that children’s habits are comprised of healthy dietary and physical activity patterns.
A growing number of child care-based interventions to prevent childhood obesity have reported positive impacts on healthy eating, physical activity, and weight gain.30,117,118 CHAMP adds to the current body of literature in five important ways: 1) tests the effect of a multi-component intervention to prevent obesity in child care; 2) tests the additive effect of a web-based caregiver intervention to augment the child care intervention; 3) builds capacity of child care staff to deliver intervention curricula; 4) adds to the science of scaled evidence-based interventions to promote nutrition and physical activity33 implemented in low-income urban and semi-urban settings; 5) evaluates the impact of the intervention on children, caregivers, and center-levels. CHAMP will provide evidence-based information to be included and reinforced in wellness guidelines and policies for child care centers, ensuring that children are exposed to healthy eating practices and opportunities for motor development and physical activity. Most of the CHAMP manualized intervention materials are available electronically, enabling the CHAMP intervention to be scaled and modified as needed to cultural-specific settings.
Key strengths of the current study protocol include cultural modifications, implementation, and expansion of an evidence-based intervention developed using social cognitive and bioecological theories, which span across multiple levels of the bioecological model (child, caregivers, child care staff, and center). Studies that are implemented and evaluated at multiple levels of the bioecological model and informed by theory have been shown to be most effective.117 Furthermore, CHAMP extends the evidence-based intervention developed by Bellows33 by testing the effectiveness across bioecological contexts.
CHAMP also examines the impact of a web-based intervention augmentation to increase caregiver engagement in the child care based intervention and promote behavior and environmental changes at the family-level. Web-based interventions offer a potential low-cost method to target families who may have limited time and resources to otherwise engage in an in-vivo intervention format. Novel caregiver communication strategies outside distribution of newsletters have been associated with greater intervention effects in school-based physical activity intervention.119 Website usage analytics provide direct assessment of caregiver engagement with the website and are used to test utilization of the intervention. Research that utilizes direct and engaging strategies is needed to establish the potential value of caregivers in maximizing the effectiveness of dietary and physical activity interventions in child care settings.120
The longitudinal design of the current protocol allows for examination of bi-directional interactions among caregivers, child care staff and children over the course of a school year, supporting a bi-directional view of caregiver-child interaction over time. Furthermore, the current study extends research by Bellows53 by examining the food and physical activity environments in urban and suburban child care centers in another state, both with validated subjective measures and objective audits.
Several limitations of the current study design should be acknowledged. The current study relies on child care staff and caregivers for self-reported measures of their attitudes and behavior, including height and weight. However, self-reported adult height and weight have been shown to be strongly related to objectively measured BMI.121 Although the current study utilizes novel website analytics methods to measure caregiver engagement, data are collected using device specific IP addresses, and therefore cannot be linked to specific caregiver data and may misattribute engagement data for caregivers who utilize multiple devices. Additionally, only a subset of child care staff are invited to wear the Actical accelerometer to measure objective physical activity due to limited device availability. Nevertheless, child care staff physical activity has been understudied and information from this study will provide valuable information on how child care staff physical activity relates to children’s physical activity. Furthermore, there is significant variability of preschool attendance over the course of a year, and the current study timeline is limited due to the transition of children in and out of child care centers. Unlike school attendance, which is mandatory, preschool attendance is influenced by factors, such as caregivers’ work schedules or the availability of alternative child care arrangements. Lastly, there is significant variability in competing activities in child care centers. Many have existing wellness policies and practices in place. However, using systematic interviews at recruitment, as well as center-level questionnaires and direct observations, we are able to measure existing wellness policies and practices and examine their potential impact on intervention outcomes.
Conclusion
Child care centers have the potential to be an effective point of intervention to help young children develop healthy dietary, motor, and physical activity habits that prevent childhood obesity and can be sustained throughout childhood. The current study allows for the longitudinal evaluation of an evidenced-based obesity prevention program implemented in urban and semi-urban areas throughout Maryland. The inclusion of the caregiver intervention through a web-based platform is innovative and may increase the impact and sustainability of the intervention. The long-term effects of early childhood wellness interventions are to reduce health disparities throughout life. The current study can inform wellness guidelines and policies that can be disseminated and implemented broadly, to ensure that child care centers provide opportunities for children to develop healthy eating, motor, and physical activity habits. Thus, CHAMP provides an important contribution to public health research and practice.
Supplementary Material
Acknowledgements
Authors acknowledge Halima Doka, Chukwudi Chidi Ezeonyebuchi, Paul Amsel, Sarah Kosterlitz, and Alison Hepworth for their contributions to CHAMP and for reviewing this manuscript.
Funding
This research was funded by the National Institute of Diabetes and Digestive and Kidney Diseases [Grant number R01 DK107761; PI: Black]. The funding body was not involved in the design of the study, collection, analysis, and interpretation of data, or in writing the manuscript.
List of abbreviations
- BMI
Body Mass Index
- BMIZ
Body Mass Index Z-score
- CACFP
Child and Adult Care Food Program
- CEBQ
The Child Eating Behavior Questionnaire
- CHAMP
Creating Healthy Habits Among Maryland Preschoolers
- EPAO
The Environment and Policy Assessment and Observation
- GLMM
Generalized linear mixed models
- LMM
Linear Mixed Models
- MVPA
Moderate-vigorous physical activity
- NAP-SACC
Nutrition and Physical Activity Self- Assessment for Child Care
- PA
Physical Activity
- PALS
Play and Learning Strategies
- PCIT
Parent Child Interaction Therapy
- SES
Socioeconomic Status
- SMS
Short Message Service
Footnotes
Trial Registration: ; https://clinicaltrials.gov/ct2/show/NCT03111264
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gardner DS, Hosking J, Metcalf BS, Jeffery AN, Voss LD, Wilkin TJ. Contribution of early weight gain to childhood overweight and metabolic health: a longitudinal study (EarlyBird 36). Pediatrics. 2009;123(1):e67–73. [DOI] [PubMed] [Google Scholar]
- 2.Nader PR, O’Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–601. [DOI] [PubMed] [Google Scholar]
- 3.Flynn MA, McNeil DA, Maloff B, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obesity Reviews. 2006;7 Suppl 1:7–66. [DOI] [PubMed] [Google Scholar]
- 4.Lanigan JD. The relationship between practices and child care providers’ beliefs related to child feeding and obesity prevention. J Nutr Educ Behav. 2012;44(6):521–529. [DOI] [PubMed] [Google Scholar]
- 5.Fox MK, Gearan E, Cannon J, et al. Usual food intakes of 2- and 3-year old U.S. children are not consistent with dietary guidelines. BMC Nutrition. 2016;2(1):67. [Google Scholar]
- 6.Bailey RL, Catellier DJ, Jun S, et al. Total usual nutrient intakes of US children (under 48 months): findings from the feeding infants and toddlers study (FITS) 2016. J Nutr. 2018;148(9S):1557S–1566S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Welker EB, Jacquier EF, Catellier DJ, Anater AS, Story MT. Room for improvement remains in food consumption patterns of young children aged 2–4 years. J Nutr. 2018;148(9S):1536S–1546S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomson JL, Tussing-Humphreys LM, Goodman MH, Landry AS. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am J Clin Nutr. 2018;109(1):127–138. [DOI] [PubMed] [Google Scholar]
- 9.Ventura AK, Worobey J. Early influences on the development of food preferences. Current Biology. 2013;23(9):R401–408. [DOI] [PubMed] [Google Scholar]
- 10.Dovey TM, Staples PA, Gibson EL, Halford JC. Food neophobia and ‘picky/fussy’eating in children: a review. Appetite. 2008;50(2–3):181–193. [DOI] [PubMed] [Google Scholar]
- 11.Galloway AT, Lee Y, Birch LL. Predictors and consequences of food neophobia and pickiness in young girls. J Am Diet Assoc. 2003;103(6):692–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birch LL, Marlin DW. I don’t like it; I never tried it: effects of exposure on two-year-old children’s food preferences. Appetite. 1982;3(4):353–360. [DOI] [PubMed] [Google Scholar]
- 13.Spill MK, Johns K, Callahan EH, et al. Repeated exposure to food and food acceptability in infants and toddlers: a systematic review. Am J Clin Nutr. 2019;109(Supplement_1):978S–989S. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan SA, Birch LL. Pass the sugar, pass the salt: Experience dictates preference. Developmental Psychology. 1990;26(4):546–551. [Google Scholar]
- 15.Wardle J, Cooke LJ, Gibson EL, Sapochnik M, Sheiham A, Lawson M. Increasing children’s acceptance of vegetables; a randomized trial of parent-led exposure. Appetite. 2003;40(2):155–162. [DOI] [PubMed] [Google Scholar]
- 16.Goodell LS, Johnson SL, Antono AC, Power TG, Hughes SO. Strategies low-income parents use to overcome their children’s food refusal. Maternal and Child Health Journal. 2017;21(1):68–76. [DOI] [PubMed] [Google Scholar]
- 17.Boeing H, Bechthold A, Bub A, et al. Critical review: vegetables and fruit in the prevention of chronic diseases. European Journal of Nutrition. 2012;51(6):637–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartley L, Igbinedion E, Holmes J, et al. Increased consumption of fruit and vegetables for the primary prevention of cardiovascular diseases. The Cochrane database of systematic reviews. 2013(6):Cd009874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hodder RK, O’Brien KM, Stacey FG, et al. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst Rev. 2018(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Global Recommendation on Physical Activity for Health. Geneva, Switzerland: 2010. [Google Scholar]
- 21.Goldfield GS, Harvey A, Grattan K, Adamo KB. Physical activity promotion in the preschool years: a critical period to intervene. Int J Environ Res Public Health. 2012;9(4):1326–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lubans DR, Morgan PJ, Cliff DP, Barnett LM, Okely AD. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40(12):1019–1035. [DOI] [PubMed] [Google Scholar]
- 23.Timmons BW, Leblanc AG, Carson V, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2012;37(4):773–792. [DOI] [PubMed] [Google Scholar]
- 24.Burdette HL, Whitaker RC. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics. 2005;116(3):657–662. [DOI] [PubMed] [Google Scholar]
- 25.Maher EJ, Li G, Carter L, Johnson DB. Preschool child care participation and obesity at the start of kindergarten. Pediatrics. 2008;122(2):322–330. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Department< of Education N. Early Childhood Program Participation Survey of the 2016 National Household Education Surveys Program (ECPP-NHES:2016).https://nces.ed.gov/pubs2017/2017101REV.pdf.
- 27.World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. World Health Organization; 2019; License: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/handle/10665/311664. [PubMed] [Google Scholar]
- 28.Addessi E, Galloway AT, Visalberghi E, Birch LL. Specific social influences on the acceptance of novel foods in 2–5-year-old children. Appetite. 2005;45(3):264–271. [DOI] [PubMed] [Google Scholar]
- 29.Craike M, Wiesner G, Hilland TA, Bengoechea EG. Interventions to improve physical activity among socioeconomically disadvantaged groups: an umbrella review. The international journal of behavioral nutrition and physical activity. 2018;15(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ling J, Robbins LB, Wen F. Interventions to prevent and manage overweight or obesity in preschool children: A systematic review. International Journal of Nursing Studies. 2016;53:270–289. [DOI] [PubMed] [Google Scholar]
- 31.Matwiejczyk L, Mehta K, Scott J, Tonkin E, Coveney J. Characteristics of effective interventions promoting healthy eating for pre-schoolers in childcare settings: an umbrella review. Nutrients. 2018;10(3):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schuler BR, Fowler B, Rubio D, et al. Building Blocks for Healthy Children: Evaluation of a Childcare Center-Based Obesity Prevention Pilot among Low-Income Children. Journal of Nutrition Education and Behavior. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bellows L, Anderson J, Gould SM, Auld G. Formative research and strategic development of a physical activity component to a social marketing campaign for obesity prevention in preschoolers. Journal of Community Health. 2008;33(3):169–178. [DOI] [PubMed] [Google Scholar]
- 34.Bellows L, Anderson J, Davies P, Kennedy C. Integration of social marketing elements in the design of a physical activity program for preschoolers. Social Marketing Quarterly. 2009;15(1):2–21. [Google Scholar]
- 35.Bellows LL, Davies PL, Anderson J, Kennedy C. Effectiveness of a physical activity intervention for Head Start preschoolers: a randomized intervention study. American Journal of Occupational Therapy. 2013;67(1):28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191. [DOI] [PubMed] [Google Scholar]
- 37.Bronfenbrenner U Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–531. [Google Scholar]
- 38.Bronfenbrenner UM PA The Bioecological Model of Human Development In: Damon W, Lerner RM, eds. Handbook of Child Psychology: Vol 1 Theoretical Models of Human Development. 6 ed. Hoboken NJ: Wiley; 2006:93–828. [Google Scholar]
- 39.Johnson SL, Bellows L, Beckstrom L, Anderson J. Evaluation of a social marketing campaign targeting preschool children. Am J Health Behav. 2007;31(1):44–55. [DOI] [PubMed] [Google Scholar]
- 40.Bellows L, Anderson J. The Food Friends: Encouraging Preschoolers to Try New Foods. Young Children. 2006;61(3):37. [Google Scholar]
- 41.Young L, Anderson J, Beckstrom L, Bellows L, Johnson SL. Making new foods fun for kids. J Nutr Educ Behav. 2003;35(6):337–338. [DOI] [PubMed] [Google Scholar]
- 42.Landry SH, Smith KE, Swank PR. Responsive parenting: establishing early foundations for social, communication, and independent problem-solving skills. Developmental Psychology. 2006;42(4):627. [DOI] [PubMed] [Google Scholar]
- 43.McNeil C, Hembree-Kigin TL. Parent-Child Interaction Therapy. New York, NY: Springer Science & Business Media; 2011. [Google Scholar]
- 44.Dev DA, McBride BA. Academy of nutrition and dietetics benchmarks for nutrition in child care 2011: Are child-care providers across contexts meeting recommendations? J Acad Nutr Diet. 2013;113(10):1346–1353. [DOI] [PubMed] [Google Scholar]
- 45.Kreidler SM, Muller KE, Grunwald GK, et al. GLIMMPSE: Online Power Computation for Linear Models with and without a Baseline Covariate. Journal of Statistical Software. 2013;54(10):i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Grieken A, Veldhuis L, Renders CM, et al. Population-based childhood overweight prevention: outcomes of the ‘Be active, eat right’ study. PLoS One. 2013;8(5):e65376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. Bmj. 2010;340:c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gibbs L, Staiger PK, Johnson B, et al. Expanding children’s food experiences: the impact of a school-based kitchen garden program. J Nutr Educ Behav. 2013;45(2):137–146. [DOI] [PubMed] [Google Scholar]
- 49.Haire-Joshu D, Elliott MB, Caito NM, et al. High 5 for Kids: the impact of a home visiting program on fruit and vegetable intake of parents and their preschool children. Preventive medicine. 2008;47(1):77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morano M, Colella D, Caroli M. Gross motor skill performance in a sample of overweight and non-overweight preschool children. Int J Pediatr Obes. 2011;6 Suppl 2:42–46. [DOI] [PubMed] [Google Scholar]
- 51.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity (Silver Spring). 2006;14(9):1616–1625. [DOI] [PubMed] [Google Scholar]
- 52.Black MM, Hager ER, Wang Y, et al. Toddler obesity prevention: A two-generation family-based randomized controlled trial. Under review. Under review. [Google Scholar]
- 53.Bellows LL, Johnson SL, Davies PL, Anderson J, Gavin WJ, Boles RE. The Colorado LEAP study: rationale and design of a study to assess the short term longitudinal effectiveness of a preschool nutrition and physical activity program. BMC Public Health. 2013;13:1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Advance Data. 2000(314):1–27. [PubMed] [Google Scholar]
- 55.Ulrich DA. TGMD 2 - Test of gross motor development examiner’s manual. Austin TX: Pro-ED, 2 2000. [Google Scholar]
- 56.Evaggelinou C, Tsigilis N, Papa A. Construct validity of the test of gross motor development: a cross-validation approach. Adapted Physical Activity Quarterly. 2002;19(4):483–495. [DOI] [PubMed] [Google Scholar]
- 57.Cools W, De Martelaer K, Samaey C, Andries C. Movement skill assessment of typically developing preschool children: A review of seven movement skill assessment tools. Journal of sports science & medicine. 2009;8(2):154. [PMC free article] [PubMed] [Google Scholar]
- 58.Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. American Journal of Mental Deficiency 1981. [PubMed] [Google Scholar]
- 59.Hager ER, Gormley CE, Latta LW, Treuth MS, Caulfield LE, Black MM. Toddler physical activity study: laboratory and community studies to evaluate accelerometer validity and correlates. BMC Public Health. 2016;16(1):936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Armstrong B, Covington LB, Hager ER, Black MM. Objective sleep and physical activity using 24-hour ankle-worn accelerometry among toddlers from low-income families. Sleep health. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meredith-Jones K, Williams S, Galland B, Kennedy G, Taylor R. 24 h Accelerometry: impact of sleep-screening methods on estimates of sedentary behaviour and physical activity while awake. J Sport Sci. 2016;34(7):679–685. [DOI] [PubMed] [Google Scholar]
- 62.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17(3):201–207. [DOI] [PubMed] [Google Scholar]
- 63.Jaramillo SJ, Yang SJ, Hughes SO, Fisher JO, Morales M, Nicklas TA. Interactive computerized fruit and vegetable preference measure for African-American and Hispanic preschoolers. J Nutr Educ Behav. 2006;38(6):352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pliner P, Hobden K. Development of a scale to measure the trait of food neophobia in humans. Appetite. 1992;19(2):105–120. [DOI] [PubMed] [Google Scholar]
- 65.Flood VM, Wen LM, Hardy LL, Rissel C, Simpson JM, Baur LA. Reliability and validity of a short FFQ for assessing the dietary habits of 2–5-year-old children, Sydney, Australia. Public Health Nutr. 2014;17(3):498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kunaratnam K, Halaki M, Wen LM, Baur LA, Flood VM. Reliability and comparative validity of a Diet Quality Index for assessing dietary patterns of preschool-aged children in Sydney, Australia. European Journal of Clinical Nutrition. 2018;72(3):464. [DOI] [PubMed] [Google Scholar]
- 67.Döring N, Hansson LM, Andersson ES, et al. Primary prevention of childhood obesity through counselling sessions at Swedish child health centres: design, methods and baseline sample characteristics of the PRIMROSE cluster-randomised trial. BMC Public Health. 2014;14(1):335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psychiatry. 2001;42(7):963–970. [DOI] [PubMed] [Google Scholar]
- 69.Mendoza JA, Zimmerman FJ, Christakis DA. Television viewing, computer use, obesity, and adiposity in US preschool children. The international journal of behavioral nutrition and physical activity. 2007;4(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Anderson SE, Economos CD, Must A. Active play and screen time in US children aged 4 to 11 years in relation to sociodemographic and weight status characteristics: a nationally representative cross-sectional analysis. BMC Public Health. 2008;8(1):366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goodman R The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40(5):791–799. [PubMed] [Google Scholar]
- 72.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. Journal of Developmental and Behavioral Pediatrics 2000;21(1):27–36. [DOI] [PubMed] [Google Scholar]
- 73.Sneddon P, Peacock GG, Crowley SL. Assessment of sleep problems in preschool aged children: An adaptation of the children’s sleep habits questionnaire. Behavioral sleep medicine. 2013;11(4):283–296. [DOI] [PubMed] [Google Scholar]
- 74.Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. Journal of Developmental & Behavioral Pediatrics. 2008;29(2):82–88. [DOI] [PubMed] [Google Scholar]
- 75.Gioia GA, Andrews K, Isquith PK. Behavior rating inventory of executive function-preschool version (BRIEF-P). Psychological Assessment Resources. 1996. [Google Scholar]
- 76.Sherman EMS, Brooks BL. Behavior Rating Inventory of Executive Function-Preschool Version (BRIEF-P): Test review and clinical guidelines for use. Child Neuropsychology. 2010;16(5):503–519. [Google Scholar]
- 77.Townsend MS, Kaiser LL, Allen LH, Joy AB, Murphy SP. Selecting items for a food behavior checklist for a limited-resource audience. J Nutr Educ Behav. 2003;35(2):69–77. [DOI] [PubMed] [Google Scholar]
- 78.Murphy SP, Kaiser LL, Townsend MS, Allen LH. Evaluation of validity of items for a food behavior checklist. J Am Diet Assoc. 2001;101(7):751–761. [DOI] [PubMed] [Google Scholar]
- 79.Natale RA, Lopez-Mitnik G, Uhlhorn SB, Asfour L, Messiah SE. Effect of a child care center-based obesity prevention program on body mass index and nutrition practices among preschool-aged children. Health Promot Pract. 2014;15(5):695–705. [DOI] [PubMed] [Google Scholar]
- 80.Natale RA, Messiah SE, Asfour L, Uhlhorn SB, Delamater A, Arheart KL. Role modeling as an early childhood obesity prevention strategy: effect of parents and teachers on preschool children’s healthy lifestyle habits. Journal of Developmental & Behavioral Pediatrics. 2014;35(6):378–387. [DOI] [PubMed] [Google Scholar]
- 81.Hagstromer M, Oja P, Sjostrom M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(6):755–762. [DOI] [PubMed] [Google Scholar]
- 82.Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. J Pediatr Psychol. 2007;32(8):960–972. [DOI] [PubMed] [Google Scholar]
- 83.Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 84.Gattshall ML, Shoup JA, Marshall JA, Crane LA, Estabrooks PA. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. The international journal of behavioral nutrition and physical activity. 2008;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Arcan C, Hannan PJ, Fulkerson JA, et al. Associations of home food availability, dietary intake, screen time and physical activity with BMI in young American-Indian children. Public Health Nutr. 2013;16(1):146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Johnston C, Mash EJ. A Measure of Parenting Satisfaction and Efficacy. Journal of Clinical Child & Adolescent Psychology. 1989;18(2):167–175. [Google Scholar]
- 87.Gilmore L, Cuskelly M. Factor structure of the Parenting Sense of Competence scale using a normative sample. Child Care Health Development. 2009;35(1):48–55. [DOI] [PubMed] [Google Scholar]
- 88.Ohan JL, Leung DW, Johnston C. The Parenting Sense of Competence scale: Evidence of a stable factor structure and validity. The Canadian Journal of Behavioural Science. 2000;32(4):251–261. [Google Scholar]
- 89.Schembre S, Greene G, Melanson K. Development and validation of a weight-related eating questionnaire. Eat Behav. 2009;10(2):119–124. [DOI] [PubMed] [Google Scholar]
- 90.Thompson MA, Gray JJ. Development and validation of a new body-image assessment scale. J Pers Assess. 1995;64(2):258–269. [DOI] [PubMed] [Google Scholar]
- 91.Killion L, Hughes SO, Wendt JC, Pease D, Nicklas TA. Minority mothers’ perceptions of children’s body size. Int J Pediatr Obes. 2006;1(2):96–102. [DOI] [PubMed] [Google Scholar]
- 92.Hager ER, McGill AE, Black MM. Development and validation of a toddler silhouette scale. Obesity (Silver Spring). 2010;18(2):397–401. [DOI] [PubMed] [Google Scholar]
- 93.Van Knippenberg F, Duivenvoorden H, Bonke B, Passchier J. Shortening the state-trait anxiety inventory. Journal of Clinical Epidemiology. 1990;43(9):995–1000. [DOI] [PubMed] [Google Scholar]
- 94.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). The British Journal Of Clinical Psychology. 1992;31 ( Pt 3):301–306. [DOI] [PubMed] [Google Scholar]
- 95.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 96.Cohen S, Williamson G. Perceived Stress in a Probability Sample of the United States In Spacapan S, & Oskamp S (Eds.), The Social Psychology of Health: Claremont Symposium on Applied Social Psychology (pp. 31–67). In: Newbury Park, CA: Sage Publications, Inc; 1988. [Google Scholar]
- 97.Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian nursing research. 2012;6(4):121–127. [DOI] [PubMed] [Google Scholar]
- 98.Van Dam NT, Earleywine M. Validation of the Center for Epidemiologic Studies Depression Scale--Revised (CESD-R): Pragmatic depression assessment in the general population. Psychiatry research. 2011;186(1):128–132. [DOI] [PubMed] [Google Scholar]
- 99.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 100.Esquivel MK, Nigg CR, Fialkowski MK, Braun KL, Li F, Novotny R. Influence of teachers’ personal health behaviors on operationalizing obesity prevention policy in head start preschools: a project of the Children’s Healthy Living Program (CHL). J Nutr Educ Behav. 2016;48(5):318–325. e311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Brann LS. Child-feeding practices and child overweight perceptions of family day care providers caring for preschool-aged children. J Pediatr Health Care. 2010;24(5):312–317. [DOI] [PubMed] [Google Scholar]
- 102.Gubbels JS, Sleddens EF, Raaijmakers L, Gies JM, Kremers SP. The Child-care Food and Activity Practices Questionnaire (CFAPQ): development and first validation steps. Public Health Nutr. 2016;19(11):1964–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Freedman MR, Alvarez KP. Early childhood feeding: assessing knowledge, attitude, and practices of multi-ethnic child-care providers. J Am Diet Assoc. 2010;110(3):447–451. [DOI] [PubMed] [Google Scholar]
- 104.Benjamin SE, Neelon B, Ball SC, Bangdiwala SI, Ammerman AS, Ward DS. Reliability and validity of a nutrition and physical activity environmental self-assessment for child care. The international journal of behavioral nutrition and physical activity. 2007;4:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ward D, Hales D, Haverly K, et al. An instrument to assess the obesogenic environment of child care centers. Am J Health Behav. 2008;32(4):380–386. [DOI] [PubMed] [Google Scholar]
- 106.Bower JK, Hales DP, Tate DF, Rubin DA, Benjamin SE, Ward DS. The childcare environment and children’s physical activity. Am J Prev Med. 2008;34(1):23–29. [DOI] [PubMed] [Google Scholar]
- 107.Henderson KE, Grode GM, Middleton AE, Kenney EL, Falbe J, Schwartz MB. Validity of a measure to assess the child-care nutrition and physical activity environment. J Am Diet Assoc. 2011;111(9):1306–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implementation science. 2007;2(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Linnan L, Steckler A. Process evaluation for public health interventions and research. Jossey-Bass San Francisco; 2002. [Google Scholar]
- 110.Loh IH, Schwendler T, Trude AC, et al. Implementation of text-messaging and social media strategies in a multilevel childhood obesity prevention intervention: Process evaluation results. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2018;55:0046958018779189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sato PM, Steeves EA, Carnell S, et al. A youth mentor-led nutritional intervention in urban recreation centers: A promising strategy for childhood obesity prevention in low-income neighborhoods. Health Educ Res. 2016;31(2):195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kennedy AB, Schenkelberg M, Moyer C, Pate R, Saunders RP. Process evaluation of a preschool physical activity intervention using web-based delivery. Evaluation and program planning. 2017;60:24–36. [DOI] [PubMed] [Google Scholar]
- 113.Lane HG, Deitch R, Wang Y, et al. “Wellness Champions for Change,” a multi-level intervention to improve school-level implementation of local wellness policies: Study protocol for a cluster randomized trial. Contemporary Clinical Trials. 2018;75:29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Taki S, Lymer S, Russell CG, et al. Assessing user engagement of an mHealth intervention: Development and implementation of the growing healthy app engagement index. JMIR mHealth and uHealth. 2017;5(6):e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Larson N, Ward DS, Neelon SB, Story M. What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J Am Diet Assoc. 2011;111(9):1343–1362. [DOI] [PubMed] [Google Scholar]
- 116.U.S. Department of Education N. National Household Education Survey Program, 2012 Early Childhood Program Participation Survey (ECPP-NHES:2012). 2012.
- 117.Sisson SB, Krampe M, Anundson K, Castle S. Obesity prevention and obesogenic behavior interventions in child care: A systematic review. Prev Med. 2016;87:57–69. [DOI] [PubMed] [Google Scholar]
- 118.Ward DS, Welker E, Choate A, et al. Strength of obesity prevention interventions in early care and education settings: A systematic review. Prev Med. 2017;95:S37–S52. [DOI] [PubMed] [Google Scholar]
- 119.Van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. British journal of sports medicine. 2008;42(8):653–657. [PubMed] [Google Scholar]
- 120.Finch M, Jones J, Yoong S, Wiggers J, Wolfenden L. Effectiveness of centre based childcare interventions in increasing child physical activity: a systematic review and meta analysis for policymakers and practitioners. Obesity Reviews. 2016;17(5):412–428. [DOI] [PubMed] [Google Scholar]
- 121.McAdams MA, Van Dam RM, Hu FB. Comparison of self reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring). 2007;15(1):188–188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.