In vitro synergy between an antimicrobial protein lysin (cell wall hydrolase) called exebacase and each of 12 different antibiotics was examined against Staphylococcus aureus isolates using a nonstandard medium approved for exebacase susceptibility testing by the Clinical and Laboratory Standards Institute. In the checkerboard assay format, fractional inhibitory concentration index values of ≤0.5, consistent with synergy, were observed for the majority of interactions tested.
KEYWORDS: Staphylococcus aureus, MRSA, exebacase, CF-301, lysin, synergy, direct lytic agent
ABSTRACT
In vitro synergy between an antimicrobial protein lysin (cell wall hydrolase) called exebacase and each of 12 different antibiotics was examined against Staphylococcus aureus isolates using a nonstandard medium approved for exebacase susceptibility testing by the Clinical and Laboratory Standards Institute. In the checkerboard assay format, fractional inhibitory concentration index values of ≤0.5, consistent with synergy, were observed for the majority of interactions tested. Synergy was further confirmed in time-kill assays.
INTRODUCTION
Direct lytic agents, including lysins, represent a new modality to address the unmet need arising from antibiotic resistance (1). Lysins are recombinantly produced cell wall hydrolase enzymes that rapidly kill target bacteria via cell wall hydrolysis and concomitant osmotic lysis. Notable features of the lysin class, in particular that of the antistaphylococcal lysin exebacase, include rapid and species-specific bactericidal effects, potent antibiofilm activity, a low propensity for resistance, and synergy with antibiotics (1–5). Importantly, exebacase recently became the first lysin to have results reported from a phase 2 clinical trial, which demonstrated 42.8% higher clinical responder rates with a single dose of exebacase used in addition to standard-of-care antibiotics compared with standard of care alone for the treatment of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia, including endocarditis (6).
The synergistic capacity of lysins is particularly compelling and holds prospects for extending the antimicrobial activities of coadministered agents to below their single-agent MICs and, thereby, potentiating bactericidal effects (1, 2, 7). Previous in vitro demonstrations of synergy with exebacase were limited to daptomycin and vancomycin using antimicrobial susceptibility testing (AST) media approved for use with these antibiotics, including cation-adjusted Mueller-Hinton broth (CAMHB) with and without supplementation with Ca2+ to a final concentration of 50 μg/ml, respectively (2, 8, 9). The effectiveness of exebacase added to daptomycin or vancomycin was further confirmed in vivo in the neutropenic mouse thigh infection and rabbit infective endocarditis models (2, 5). In the current work, analysis of in vitro synergy was extended to a group of 12 antistaphylococcal antibiotics in both checkerboard and time-kill assay formats, using a nonstandard AST medium-developed exebacase and comprised of CAMHB supplemented with horse serum (Sigma-Aldrich) and dl-dithiothreitol (Sigma-Aldrich) to final concentrations of 25% and 0.5 mM, respectively (4, 10). The medium, referred to as CAMHB-HSD, was previously validated in a Clinical Laboratory and Standards Institute (CLSI) M23-A3 quality control (QC) study, which demonstrated the reproducibility of exebacase MICs and established QC ranges that were accepted by CLSI in January 2017 (11; https://clsi.org/education/microbiology/ast/ast-meeting-files-resources/).
To inform concentration selection in synergy assays, MICs of each agent were first determined by broth microdilution against each of 10 methicillin-susceptible S. aureus (MSSA) and 10 MRSA strains. Exebacase MICs in CAMHB-HSD ranged from 0.25 to 1 μg/ml for all strains tested (see Table S1 in the supplemental material), including the S. aureus QC strain ATCC 29213, for which a QC range of 0.25 to 2 μg/ml was previously determined in the CLSI M23-A4 studies (11). For the antibiotics, MICs were determined in both CAMHB-HSD and the standard AST medium described in CLSI documents M100-A28 and M07-A11 (8, 9). Each antibiotic was active in CAMHB-HSD (see Fig. S1 in the supplemental material); and, for all strains tested, the MICs of daptomycin, vancomycin, nafcillin, oxacillin, cefazolin, gentamicin, linezolid, levofloxacin, and sulfamethoxazole-trimethoprim were identical to or within one 2-fold dilution of values determined in the standard media (Table S1). Importantly, all antibiotic MICs against QC strain ATCC 29213 were within CLSI-acceptable QC ranges (9). For telavancin and clindamycin, activity was diminished in CAMHB-HSD compared with standard media (by greater than two 2-fold dilutions); azithromycin, on the other hand, was more active in CAMHB-HSD than in standard media (by less than two 2-fold dilutions).
Based on the single-agent MIC values determined in CAMHB-HSD, exebacase was tested in addition to each of 12 antibiotics against the 10 MSSA and 10 MRSA strains using a standard checkerboard assay format (2, 12). Mean fractional inhibitory concentration index (FICI) values were calculated based on the individual FICI values observed by row over at least three consecutive rows on each checkerboard panel examined. The activity inferred from the resulting FICI values was assessed according to the following criteria: synergy, ≤0.5; additivity, >0.5 to ≤1; no interaction (indifference), >1 to ≤4; antagonism, >4. Synergy was the primary interaction observed for exebacase in addition to daptomycin, vancomycin, nafcillin, oxacillin, cefazolin, telavancin, linezolid, azithromycin, or clindamycin (Table 1). For this group, 87% (154/177) of the interactions tested were synergistic, 11.3% were additive (20/177), and 1.7% (3/177) were indifferent. For exebacase in addition to gentamicin, levofloxacin, or sulfamethoxazole-trimethoprim, the primary interaction observed was additivity. For this group, 6.7% (4/60) of the interactions were synergistic, 60% (36/60) were additive, and 33.3% (20/60) were indifferent. Importantly, no antagonism was observed. Furthermore, we observed no overall differences in activities against the MSSA and MRSA isolate sets. For the 10 MSSA isolates, 66.6% (80/120) of the interactions tested were synergistic, 24.2% (29/120) were additive, and 9.2% (11/120) were indifferent. For the 10 MRSA isolates, 66.6% (78/117) of the interactions were synergistic, 23.1% (27/117) were additive, and 10.3% (12/117) were indifferent.
TABLE 1.
Mean FICI values of exebacase used in addition to antibiotics in CAMHB-HSD
| Designationb | Resistance | FICA scores with:a
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DAP | VAN | NAF | OXA | CFZ | TLV | AZM | CLI | GEN | LNZ | LVX | SXT | ||
| ATCC BAA-1718 | MSSA | 0.500 | 0.250 | 0.375 | 0.500 | 0.250 | 0.500 | 0.375 | 0.500 | 1.031 | 0.500 | 1.000 | 0.508 |
| NRS 107 | MSSA | 0.500 | 0.500 | 0.500 | 0.375 | 0.500 | 0.500 | 0.312 | 0.375 | 0.508 | 0.750 | 0.516 | 1.031 |
| NRS 143 | MSSA | 0.500 | 0.500 | 0.500 | 0.500 | 0.750 | 0.500 | 0.312 | 0.500 | 1.031 | 0.503 | 1.000 | 1.031 |
| NRS 112 | MSSA | 0.750 | 0.250 | 0.500 | 0.312 | 0.500 | 0.250 | 0.500 | 0.375 | 1.031 | 0.625 | 1.031 | 0.625 |
| NRS161 | MSSA | 0.500 | 0.500 | 0.500 | 0.500 | 0.500 | 0.500 | 0.500 | 0.500 | 0.750 | 0.500 | 0.625 | 0.750 |
| NRS111 | MSSA | 0.500 | 0.625 | 0.250 | 0.375 | 0.500 | 0.500 | 0.375 | 0.500 | 0.625 | 0.375 | 1.000 | 0.750 |
| ATCC 29213 | MSSA | 0.375 | 0.500 | 0.312 | 0.312 | 0.500 | 0.750 | 0.500 | 0.375 | 1.031 | 0.625 | 0.750 | 0.516 |
| ATCC 49521 | MSSA | 0.500 | 0.500 | 0.375 | 0.500 | 0.500 | 0.500 | 0.500 | 0.375 | 0.563 | 0.500 | 0.750 | 1.031 |
| JMI 2559 | MSSA | 0.375 | 0.500 | 0.250 | 0.315 | 0.500 | 0.500 | 0.500 | 0.500 | 0.500 | 0.625 | 0.563 | 1.031 |
| JMI 3126 | MSSA | 0.500 | 0.625 | 0.250 | 0.375 | 0.500 | 0.625 | 0.375 | 0.500 | 0.500 | 0.625 | 1.031 | 1.031 |
| NRS 271 | MRSA | 0.254 | 0.500 | 0.250 | 0.563 | 0.500 | 0.500 | 0.313 | 0.375 | 1.063 | 0.531 | 0.625 | 1.031 |
| NRS 100 | MRSA | 0.375 | 0.500 | 0.313 | 0.500 | 0.500 | 0.500 | 0.313 | 0.375 | 0.375 | 0.500 | 1.031 | 0.750 |
| ATCC 43300 | MRSA | 0.500 | 0.375 | 0.375 | 0.375 | 0.313 | 0.500 | ND | 1.031 | 1.031 | 0.750 | 1.031 | 0.531 |
| ATCC BAA-44 | MRSA | 0.500 | 0.500 | 0.375 | 0.375 | 0.375 | 1.031 | 0.375 | 0.500 | 1.031 | 0.750 | 0.500 | 0.750 |
| CAIRD 456 | MRSA | 0.500 | 0.500 | 0.375 | 0.313 | 0.313 | 0.500 | 0.500 | 0.250 | 0.500 | 0.500 | 0.563 | 0.750 |
| JMI 227 | MRSA | 0.500 | 0.281 | 0.375 | 0.375 | 0.500 | 0.500 | 0.500 | 0.375 | 0.508 | 0.625 | 1.000 | 0.750 |
| JMI 1280 | MRSA | 0.375 | 0.313 | 0.500 | 0.156 | 0.188 | 0.750 | ND | 0.500 | 1.000 | 0.500 | 1.000 | 1.000 |
| JMI 4789 | MRSA | 0.375 | 0.281 | 0.375 | 0.375 | 0.500 | 0.500 | 0.375 | 0.375 | 0.508 | 0.500 | 0.750 | 0.504 |
| MW2 | MRSA | 0.500 | 0.515 | 0.250 | 0.375 | 0.500 | 1.031 | 0.375 | 0.500 | 0.750 | 0.625 | 1.000 | 1.031 |
| ATCC 33591 | MRSA | 0.500 | 0.500 | 0.500 | 0.500 | 0.250 | 0.504 | ND | 0.500 | 1.000 | 0.375 | 1.000 | 0.508 |
Mean FICI values were calculated based on the individual FICI values observed by row over at least 3 consecutive rows on each checkerboard panel. The FICI values are consistent with the following interactions: synergy, ≤0.5 (bold); additivity, >0.5 to ≤1 (italic); no interaction (indifference) >1 to ≤4 (shaded); antagonism, >4. ND, not determined; DAP, daptomycin; VAN, vancomycin; NAF, nafcillin; OXA, oxacillin; CFZ, cefazolin; TLV, telavancin; AZM, azithromycin; CLI, clindamycin; GEN, gentamicin; LNZ, linezolid; LVX, levofloxacin; SXT, sulfamethoxazole-trimethoprim.
The bacterial strains are described in Table S2 in the supplemental material.
Checkerboard assays were performed using 100% human serum as the AST medium against 5 MRSA and 5 MSSA strains. Human serum (from pooled male type AB plasma, U.S. origin, sterile filtered; Sigma-Aldrich) was used to confirm synergy in a physiologically relevant medium, considering the intended clinical use of exebacase as an intravenously administered antimicrobial agent (5). We have previously shown that S. aureus AST can be performed in human serum, providing MIC determinations by broth microdilution with clear endpoints (4, 5; https://clsi.org/education/microbiology/ast/ast-meeting-files-resources/). MICs determined in human serum are, furthermore, equivalent to those determined in CAMHB-HSD (5, 13). The mean FICI values for exebacase plus each of 12 antibiotics, determined in human serum, are described in Table 2 and are consistent with synergy in 92.6% (88/95) of checkerboards (92.6%) with daptomycin, vancomycin, nafcillin, oxacillin, cefazolin, telavancin, azithromycin, clindamycin, linezolid, and levofloxacin. Exebacase used with gentamicin and sulfamethoxazole-trimethoprim were additive in 100% (20/20) of checkerboards tested, with FICI values of 0.508 to 1.031. Synergy was detected for 78.3% (47/60) of the assays tested against MSSA and 74.5% (41/55) of the assays tested against MRSA. No antagonism was observed.
TABLE 2.
FICI values of exebacase used in addition to antibiotics in human serum
| Designation | Resistance | FICI scores with:a
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DAP | VAN | NAF | OXA | CFZ | TLV | AZM | CLI | GEN | LNZ | LVX | SXT | ||
| NRS111 | MSSA | 0.375 | 0.500 | 0.563 | 0.625 | 0.375 | 0.500 | 0.500 | 0.500 | 0.625 | 0.500 | 0.500 | 1.031 |
| ATCC 29213 | MSSA | 0.375 | 0.500 | 0.500 | 0.313 | 0.500 | 0.500 | 0.375 | 0.250 | 1.000 | 0.500 | 0.375 | 1.000 |
| ATCC 49521 | MSSA | 0.375 | 0.375 | 0.500 | 0.507 | 0.500 | 0.500 | 0.375 | 0.250 | 0.508 | 0.375 | 0.500 | 0.750 |
| JMI 2559 | MSSA | 0.375 | 0.375 | 0.500 | 0.500 | 0.313 | 0.375 | 0.375 | 0.250 | 1.000 | 0.375 | 0.500 | 1.031 |
| JMI 3126 | MSSA | 0.500 | 0.375 | 0.500 | 0.500 | 0.500 | 0.375 | 0.375 | 0.313 | 1.000 | 0.375 | 0.500 | 1.031 |
| ATCC 43300 | MRSA | 0.250 | 0.500 | 0.625 | 0.500 | 0.375 | 0.500 | 0.500 | ND | 0.750 | 0.500 | 0.500 | 1.031 |
| JMI 227 | MRSA | 0.375 | 0.500 | 0.563 | 0.250 | 0.500 | 0.500 | 0.500 | 0.375 | 1.000 | 0.500 | 0.500 | 1.000 |
| JMI 1280 | MRSA | 0.313 | 0.375 | ND | ND | ND | 0.375 | 0.500 | ND | 0.750 | 0.500 | 0.500 | 0.625 |
| JMI 4789 | MRSA | 0.250 | 0.375 | 0.375 | 0.375 | 0.313 | 0.375 | 0.375 | 0.313 | 0.625 | 0.375 | 0.563 | 1.000 |
| MW2 | MRSA | 0.375 | 0.500 | 0.313 | 0.250 | 0.313 | 0.5 | 0.375 | 0.500 | 1.000 | 0.5 | 0.563 | 1.000 |
Mean FICI values were calculated based on the individual FICI values observed by row over at least 3 consecutive rows on each checkerboard panel. The FICI values are consistent with the following interactions: synergy, ≤0.5 (bold); additivity, >0.5 to ≤1 (italic); no interaction (indifference) >1 to ≤4 (shaded); antagonism, >4.
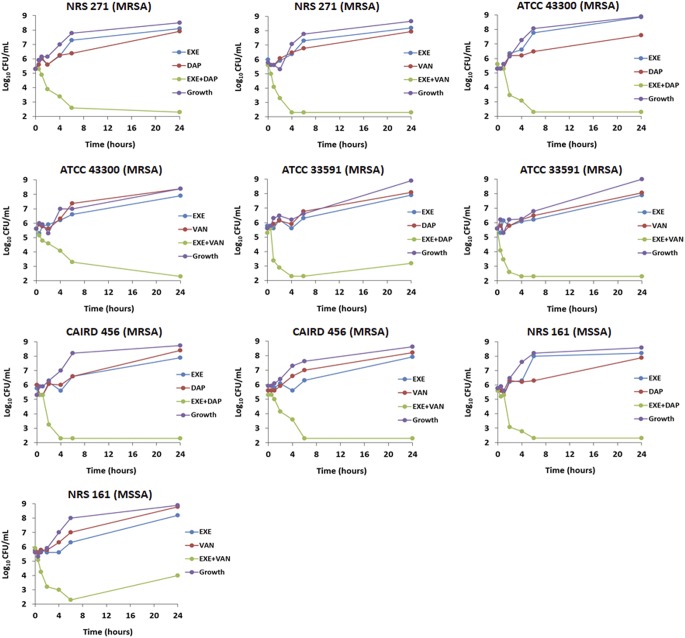
As an independent confirmation of synergy, we examined the activity of exebacase added to two of the antibiotics, daptomycin and vancomycin, against a set of five S. aureus isolates following the time-kill assay format described by CLSI (10), with the exception of using CAMHB-HSD as the testing medium. The addition of 0.25× MIC exebacase to 0.25× MIC of either daptomycin or vancomycin resulted in a ≥2-log10 decrease in CFU/ml compared with combined single-agent values for all strains tested (Fig. 1). The findings were consistent with synergy in each case and consistent with results from the checkerboard titrations.
FIG 1.
Time-kill curves for S. aureus strains NRS 271, ATCC 43300, ATCC 33591, CAIRD 456, and NRS 161 using exebacase (EXE) plus daptomycin (DAP) or vancomycin (VAN), as indicated. Each agent was tested alone and in combination at 0.25× the MIC value determined in CAMHB-HSD. In each experiment, the threshold of detection was 2.2 log10 CFU/ml. All data points were an average of duplicate time points within an experiment, and the assay was repeated at least twice independently.
Overall, this study provides the first description of the notable breadth of synergy for exebacase with a wide range of antibiotics. Our results support the concept of using direct lytic agents, such as exebacase, in addition to antibiotics as a novel treatment paradigm to address the unmet need for more effective antimicrobial strategies in an environment of increasing antibiotic resistance. The clinical effectiveness of exebacase added to standard-of-care antibiotics (primarily vancomycin and daptomycin) may certainly be attributable to the notable synergy observed in the current report. Although the exact mechanisms of synergy remain to be identified, it is notable that the strongest synergy was observed for exebacase plus antibiotics targeting the cell envelope, including daptomycin, vancomycin, nafcillin, oxacillin, cefazolin, and telavancin. Based on the cell wall hydrolytic activity of exebacase and our previous observations of enhanced labeling of staphylococci with BODIPY-daptomycin in the presence (but not absence) of exebacase (2), synergy may be the result of lysin-mediated destabilization of the cell wall and concomitant improvement of antibiotic access to and/or activity at cell wall targets.
Importantly, no differences were noted in the synergy observed with MSSA or MRSA isolate groups. Of particular note was the synergy between exebacase and the β-lactam antibiotics (i.e., nafcillin, oxacillin, and cefazolin) against MRSA strains, which are resistant to these antibiotics. Such synergy may reflect a potential “resensitizing effect,” i.e., lowering of the MRSA β-lactam MICs into the CLSI susceptible range. Such a resensitizing effect against MRSA will be examined in future in vitro and in vivo experiments.
Supplementary Material
ACKNOWLEDGMENTS
We thank Patricia Bradford for critical review of the manuscript and Temima Yellin for assistance in MIC testing.
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Wittekind M, Schuch R. 2016. Cell wall hydrolases and antibiotics: exploiting synergy to create efficacious new antimicrobial treatments. Curr Opin Microbiol 33:18–24. doi: 10.1016/j.mib.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Schuch R, Lee HM, Schneider BC, Sauve KL, Law C, Khan BK, Rotolo JA, Horiuchi Y, Couto DE, Raz A, Fischetti VA, Huang DB, Nowinski RC, Wittekind M. 2014. Combination therapy with lysin CF-301 and antibiotic is superior to antibiotic alone for treating methicillin-resistant Staphylococcus aureus-induced murine bacteremia. J Infect Dis 209:1469–1478. doi: 10.1093/infdis/jit637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuch R, Khan BK, Raz A, Rotolo JA, Wittekind M. 2017. Bacteriophage lysin CF-301, a potent antistaphylococcal biofilm agent. Antimicrob Agents Chemother 61:e02666-16. doi: 10.1128/AAC.02666-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oh JT, Cassino C, Schuch R. 2019. Postantibiotic and sub-MIC effects of exebacase (lysin CF-301) enhance antimicrobial activity against Staphylococcus aureus. Antimicrob Agents Chemother 63:e02616-18. doi: 10.1128/AAC.02616-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Indiani C, Sauve K, Raz A, Abdelhady W, Xiong YQ, Cassino C, Bayer AS, Schuch R. 2019. The antistaphylococcal lysin, CF-301, activates key host factors in human blood to potentiate methicillin-resistant Staphylococcus aureus bacteriolysis. Antimicrob Agents Chemother 63:e02291-18. doi: 10.1128/AAC.02291-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fowler VG, Das A, Lipka J, Schuch R, Cassino C. 2019. Exebacase (lysin CF-301) improved clinical responder rates in methicillin-resistant Staphylococcus aureus bacteremia and endocarditis compared to standard of care antibiotics alone in a first-in-patient phase 2 study, abstr L0012. Abstr Eur Congr Clin Microbiol Infect Dis (ECCMID), Amsterdam, Netherlands.
- 7.Letrado P, Corsini B, Díez-Martínez R, Bustamante N, Yuste JE, García P. 2018. Bactericidal synergism between antibiotics and phage endolysin Cpl-711 to kill multidrug-resistant pneumococcus. Future Microbiol 13:1215–1223. doi: 10.2217/fmb-2018-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clinical and Laboratory Standards Institute. 2018. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically—11th ed. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 9.Clinical and Laboratory Standards Institute. 2019. Performance standards for antimicrobial susceptibility testing—29th ed. Clinical and Laboratory Standards Institute, Wayne, PA. [Google Scholar]
- 10.Watson A, Oh JT, Sauve K, Bradford PA, Cassino C, Schuch R. 2019. Antimicrobial activity of exebacase (lysin CF-301) against the most common causes of infective endocarditis. Antimicrob Agents Chemother 63:e01078-19. doi: 10.1128/AAC.01078-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Traczewski MM, Oh J, Schuch R. 2017. Quality control studies of CF-301 versus Staphylococcus aureus ATCC 29213 and Enterococcus faecalis ATCC 29212, abstr Friday-961. Abstr ASM Microbe, New Orleans, LA.
- 12.Moody J. 2010. Synergy testing: broth microdilution checkerboard and broth macrodilution methods, p 5.12.1–5.12.23. In Garcia LS. (ed), Clinical microbiology procedures handbook, vol 2 ASM Press, Washington, DC. [Google Scholar]
- 13.Oh J, Sauve K, Wittekind M, Ambler J, Schuch R. 2017. Development of an antimicrobial susceptibility test (AST) for the antistaphylococcal lysin CF-301, abstr 6193. Abstr 27th European Congress of Clinical Microbiology and Infectious Diseases, Vienna, Austria.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.