Abstract
Background:
To date, there are few biomechanical studies comparing the strength between knot repair and knotless repair procedures for anterior talofibular ligament (ATFL) injury.
Purpose:
To perform a biomechanical comparison of the strength of the arthroscopic ATFL repair technique with knot or knotless suture anchors in a cadaveric model with partial or complete ATFL injuries.
Study Design:
Controlled laboratory study.
Methods:
A total of 24 fresh-frozen cadaveric ankles were used. Arthroscopy was used to identify, section, and repair the ATFL on the fibular insertion site. The specimens were then randomly placed into 1 of 4 groups: group A received complete ATFL section and 1–suture anchor repair with knot, group B received complete ATFL section and 1-anchor knotless repair, group C received partial ATFL section and 1–suture anchor repair with knot, and group D received partial ATFL section and 1-anchor knotless repair. After repair, the ATFL tension was measured first with a digitalized tensiometer. Specimens were then mounted on a materials testing system to determine the ultimate load to failure and stiffness.
Results:
The mean ± SD ligament tension measured during the arthroscopic procedure was 8.6 ± 0.6 N for group A, 9.2 ± 0.5 N for group B, 9.4 ± 1.1 N for group C, and 9.6 ± 0.9 N for group D. No significant difference in tension was detected among groups. In load-to-failure testing, the mean ultimate failure load was 27.9 ± 4.1 N for group A, 26.2 ± 9.3 N for group B, 81.9 ± 26.5 N for group C, and 88.1 ± 41.6 N for group D. The mean ultimate failure loads of the partial repair groups were significantly higher than those of the complete repair groups (C vs A, P = .008; D vs B, P = .002), while there was no significant difference between groups A and B (P > .05) or between groups C and D (P > .05).
Conclusion:
The results of the present study showed that there was no significant difference in biomechanical properties between knot repair and knotless repair techniques.
Clinical Relevance:
Biomechanically, the results showed that knot suture anchor and knotless suture repair provide similar biomechanical strength for ATFL injury. Unfortunately, these methods in the complete ATFL section models provided less than half the strength and stiffness in the partial ATFL section models at time zero after surgery. As a result, 1–suture anchor repair is not suitable for complete ATFL injury regardless of the repair method.
Keywords: knot, knotless, repair, ATFL, biomechanics, suture anchor
In the surgical management of chronic ankle disability, the anatomic lateral ankle ligament (mainly anterior talofibular ligament [ATFL]) repair technique with suture anchor is widely accepted as the reference standard, allowing immediate weightbearing and returning high-demand athletes to their preinjury sports level.12,17,19,23 Arthroscopic ATFL repair with a suture anchor is safe and effective, and excellent short- to midterm patient outcomes have been reported in the majority of cases.‡
Generally, the suture anchors for ankle ligament repair can be divided into knot and knotless. Previously, Takao et al25 described a simplified repair technique of the lateral ligament alone with a knot suture anchor, which avoids additionally tightening the inferior extensor retinaculum. Moreover, Li et al16 repaired the ATFL with a knot suture anchor technique and reported that arthroscopic repair of the ATFL produced favorable magnetic resonance imaging outcomes with excellent functional outcomes 2 years postoperatively. In 2013, Vega et al26 repaired the ATFL with a knotless suture anchor and found that all patients reported subjective improvement of their ankle instability, as indicated by the mean American Orthopaedic Foot and Ankle Society score increasing from 67 preoperatively to 97 at final follow-up. No major complications were reported. Pereira et al22 also described a knotless suture anchor repair technique. The knotless suture anchor has the following advantages: (1) it avoids the need for classic knot-tying methods, diminishing the chance of knot migration caused by pendulum movements; (2) it avoids some complications that have been related to the use of metallic anchors and some currently available biomaterials; (3) and it prevents prominent knots, which have been described as a possible cause of secondary complaints.
The arthroscopic ATFL repair technique with knotless suture anchor has become an increasingly popular option for the treatment for chronic ankle instability.21,22 However, there have been few biomechanical studies comparing the strength between knot repair and knotless repair procedures for chronic ankle instability. The purpose of our study was to perform a biomechanical comparison of the tension, ultimate load to failure, and stiffness between the knotless repair technique and a knot suture anchor repair of the ATFL. It was hypothesized that the knotless repair technique would produce similarly favorable outcomes when compared with the knot repair technique for the ATFL.
Methods
Study Design
Twenty-four fresh-frozen human cadaveric ankle specimens, donated to the Department of Anatomy of our university, were used and randomly divided into 4 groups of 6 specimens: group A received complete ATFL section and 1–suture anchor (SutureTak; Arthrex) repair with knot, group B received complete ATFL section and 1-anchor (PushLock; Arthrex) knotless repair, group C received partial ATFL section and 1–suture anchor (SutureTak) repair with knot, and group D received partial ATFL section and 1-anchor (PushLock) knotless repair. The mean ± SD age of the cadavers was 66 ± 7 years (range, 55-78 years), and the age distribution was similar among the 4 groups. The cadavers were stored at –20°C and were thawed at room temperature for 24 hours before use.
Surgical Procedure
All surgical procedures were performed by a senior sports medicine surgeon (Y.H.), who had considerable experience in arthroscopic ATFL repair surgery. The arthroscopic ATFL repair procedure was performed according to the following protocol. Two initial anterior arthroscopy portals were used. The arthroscope was introduced through a portal just medial to the tibialis anterior tendon, and this portal was used to identify the correct position for the lateral portal and accessory lateral portal. The ATFL was evaluated. In this study, all the specimens had ATFLs.
Then, the ATFL insertion at the distal fibula was determined with a shaver and ablator. The superior half of the ATFL was sectioned at the fibula insertion site in 12 ankles, creating partial ATFL injury models, while the other 12 ankles with complete ATFL section at the fibula insertion site were considered the complete ATFL injury models. Among the 12 ankles in each group, 6 ankles underwent knot suture anchor repair, and the others underwent knotless suture anchor repair.
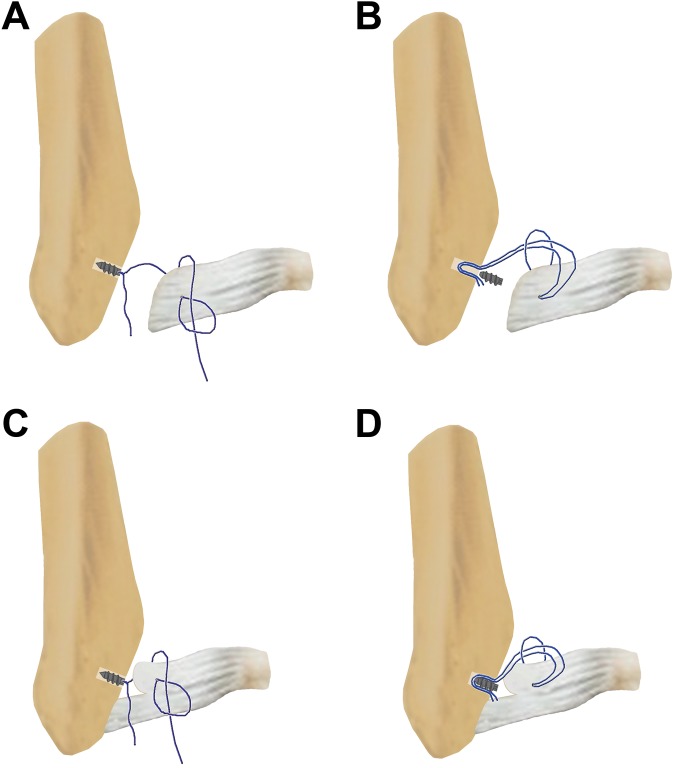
The knot suture anchor repair procedure was performed according to a previous report (Figure 1, A and C).25 After the ATFL insertion at the distal fibula was identified (a mean 10-11 mm proximal to the distal tip of the fibula), 1 suture anchor (3.0-mm SutureTak) was placed at the fibular ATFL footprint. The ATFL remnant was penetrated by a tissue-penetrating instrument. The midportion of the anchor suture was pulled through the ATFL such that a loop of suture was created in the ATFL. The free end of the suture was then passed through this loop and pulled tight, creating a self-cinching stitch. The other end of the anchor suture was used to draw the self-cinching stitch, tightening the ATFL. Afterward, a square knot and a granny knot were created 2 times with a knot pusher.
Figure 1.
(A) Group A received complete ATFL section and 1–suture anchor repair with knot. (B) Group B received complete ATFL section and 1-anchor knotless repair. (C) Group C received partial ATFL section and 1–suture anchor repair with knot. (D) Group D received partial ATFL section and 1-anchor knotless repair. ATFL, anterior talofibular ligament.
The knotless suture anchor repair procedure was performed according to another previous report (Figure 1, B and D).27 After preparation of the ATFL remnant, a No. 2 high-resistance nonabsorbable suture (FiberWire; Arthrex) penetrated the remnant, with 1 limb of the suture passing through a loop suture. After identification of the correct insertion site, a drill was introduced through the drill guide and directed anterior to posterior, parallel to the plantar plane as well as the plane of the talar lateral wall. The knotless anchor (2.9-mm PushLock; Arthrex) was loaded with the suture and passed with the sutures through the anterolateral portal. With the ankle in the dorsiflexion-valgus position, the sutures were tightened, and the anchor was introduced into the osseous tunnel by impaction.
Tension Measurement
After repair, a digitalized tensiometer (50FGN; Shimpo) was used to estimate ligament tension (Figure 2). The ATFL was inlaced with the hook at the middle site. When tension was measured, the direction of pull was perpendicular to the ligament direction. Manual traction was applied to the tensiometer until the ligament was pulled with a movement of 1 mm.
Figure 2.
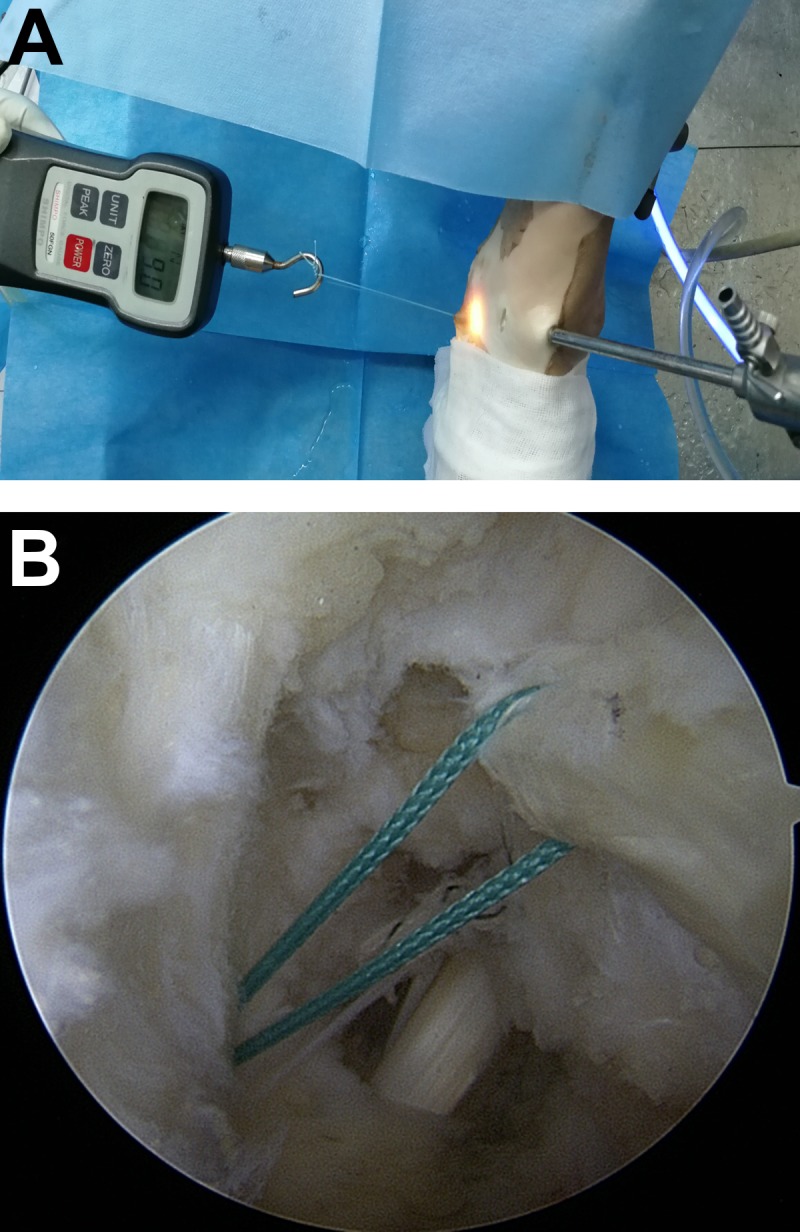
(A) The estimation of ligament tension with a digitalized tensiometer. (B) The direction of pull was perpendicular to the ligament direction when measuring tension.
Specimen Preparation
After ATFL repair, all the soft tissues were completely stripped from the tibia and fibula, and the foot was left completely intact with the skin present. The deltoid ligament, the anterior capsule, and the posterior capsule were incised, leaving only the ATFL intact. The syndesmosis ligaments, the posterior talofibular ligament, and the calcaneofibular ligament (CFL) were then cut and the tibia removed, leaving only the fibula and the ATFL isolated in all 24 specimens.
Biomechanical Testing
Biomechanical testing was performed with a CMT4204 Testing System (MTS) with a 20-kN load cell secured to the crosshead. A 5-mm Steinmann pin was placed medial to lateral through the proximal fibula to ensure that the fibula would be pulled in line with the load actuator applied by a dynamic tensile testing machine. The sample was further clamped to a custom jig secured to the test platform that placed the foot in 20° of inversion and 10° of plantarflexion.
A tensile load was applied with a preload of 10 N for 10 seconds. Then the load was held at 10 N for 5 seconds to remove potential creep. After loading, the actuator pulled the fibula at a rate of 10 mm/min until failure. The mechanism of failure was recorded (ligament-suture interface, ATFL midsubstance tear, or ATFL distal avulsion). Ultimate failure load (N) and pullout stiffness (N/mm) were determined. The ultimate load was defined as the maximum endured load during testing. Stiffness was calculated as the slope of the linear region of the load-elongation curve corresponding to the steepest straight-line tangent to the curve.
Statistical Analysis
Statistical analysis was performed with STATA v 10.0 (Stata Corp). The primary statistical analysis was done with 1-way analysis of variance (ANOVA). For results that demonstrated a statistically significant difference, a post hoc Tukey honestly significant difference test was conducted to assess the location of the means that were statistically significant between the groups. P values <.05 were considered significant.
Results
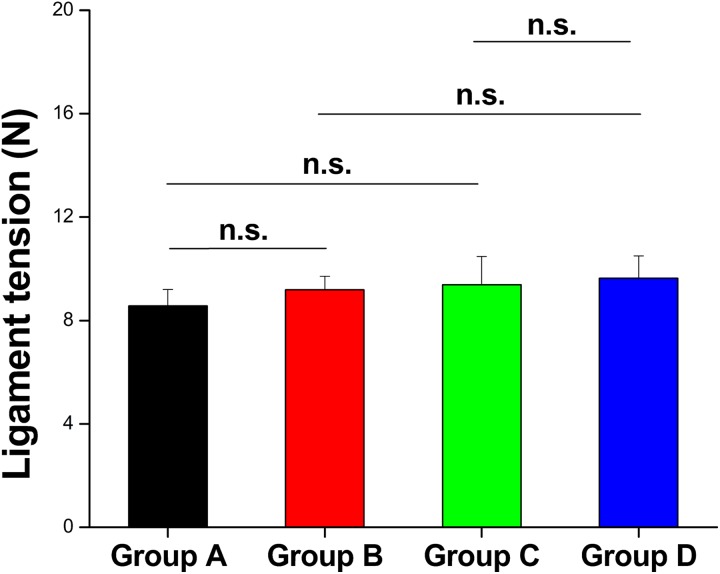
The mean ligament tension measured during the arthroscopic procedure was 8.6 ± 0.6 N for group A, 9.2 ± 0.5 N for group B, 9.4 ± 1.1 N for group C, and 9.6 ± 0.9 N for group D. No significant difference in tension was detected among groups (Figure 3).
Figure 3.
Comparison of ligament tension among groups. Values are presented as mean ± SD. n.s., no significant difference.
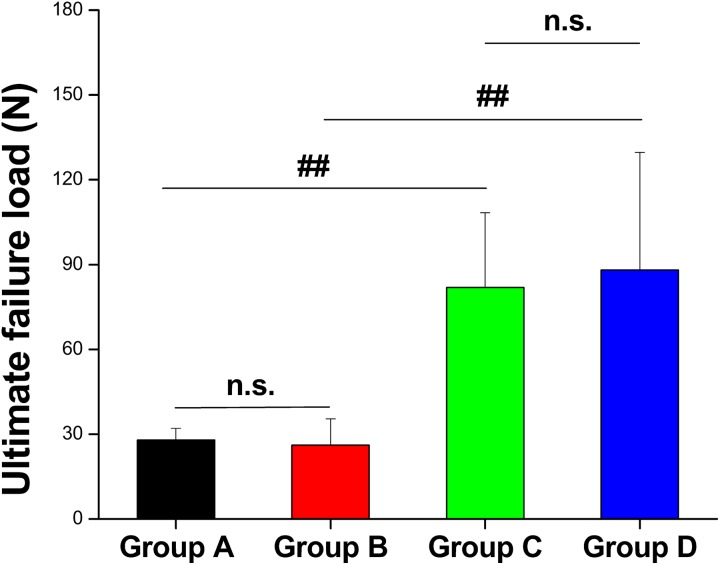
In load-to-failure testing, the mean ultimate failure load was 27.9 ± 4.1 N for group A, 26.2 ± 9.3 N for group B, 81.9 ± 26.5 N for group C, and 88.1 ± 41.6 N for group D. The mean ultimate failure loads of the partial repair groups were significantly higher than those of the complete repair groups (group C vs group A, P = .008; group D vs group B, P = .002), while there was no significant difference between groups A and B (P > .05) or between groups C and D (P > .05) (Figure 4).
Figure 4.
Comparison of ultimate failure load among groups. Values are presented as mean ± SD. ##Significant difference. n.s., no significant difference.
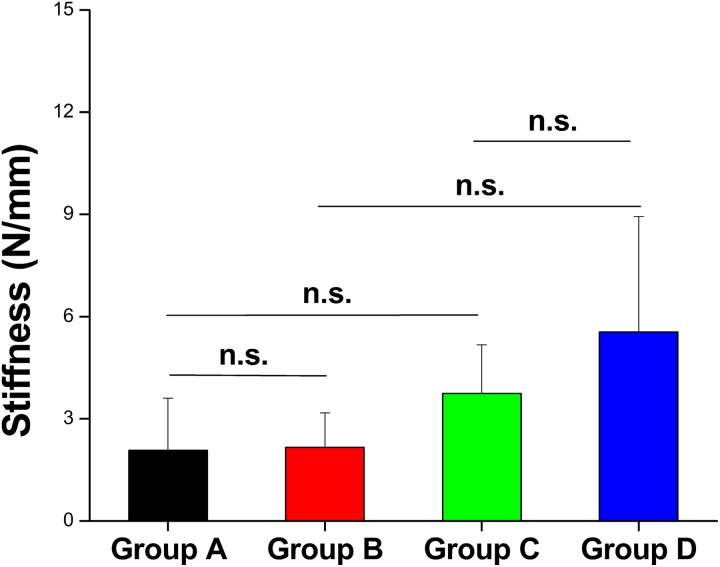
The mean stiffness was 2.1 ± 1.5 N for group A, 2.2 ± 1.0 N for group B, 3.7 ± 1.4 N for group C, and 5.6 ± 3.4 N for group D. There was no significant difference in stiffness between groups A and B (P > .05) or between groups C and D (P > .05) (Figure 5).
Figure 5.
Comparison of stiffness among groups. Values are presented as mean ± SD. n.s., no significant difference.
The mechanism of failure was at the ligament-suture interface for all specimens in group A and group B. However, in group C, the mechanism of failure was predominantly at the midsubstance (3 specimens), while 2 failed at the distal attachment site and the 1 remaining specimen failed at the ligament-suture interface. The mechanism of failure for group D was predominantly at the midsubstance (4 specimens), with distal attachment site failure for the remaining 2 specimens.
Discussion
In the present study, we performed a biomechanical comparison of the strength of the arthroscopic ATFL repair technique with knot or knotless suture anchors in partial and complete ATFL injury cadaveric models. Generally, our study has 3 unique points: (1) the ATFL repair was performed under arthroscopy; (2) a partial ATFL injury mode was used; and (3) the knot suture–relay technique and the knotless repair technique were compared. It was demonstrated that there was no significant difference in biomechanical properties between knot repair and knotless repair, regardless of partial or complete ATFL injury.
To the best of our knowledge, there has been no biomechanical analysis of the ultimate load to failure or stiffness regarding knot or knotless repair for ATFL injury. Previous biomechanical studies that compared PushLock and SutureTak anchors in shoulder glenoid and hip acetabula rim revealed no statistical difference in the ultimate failure load for the 2 types of anchors.3,24 Jarrett et al14 compared the biomechanical strength of the PushLock suture anchor with a traditional Bio-SutureTak suture anchor in the repair of ulnar collateral ligament injuries and demonstrated no statistical difference in the ultimate load to failure between the PushLock group (28.0 N) and the Bio-SutureTak group (18.8 N) under cyclic loading. A controlled laboratory study from 2018 showed that a knotless fixation construct with suture tape improved biomechanical performance as compared with knots or a knotless fixation construct with No. 2 suture, while there was still no difference in load to failure between the group with knotless fixation with No. 2 suture and the knotted group.8
In the present study, the mean ultimate failure load was 27.9 ± 4.1 N with knot suture anchor repair and 26.2 ± 9.3 N with knotless anchor suture repair for the complete ATFL injury. Waldrop et al29 performed a biomechanical study of ATFL repair with knot suture anchor, and they found that the ultimate failure load of the knot suture anchor repair group (79.2 ± 34.3 N) was significantly lower than that of the intact ATFL group (160.9 ± 72.2 N) at time zero after surgery. The failure loads in our study were much lower than that of Waldrop et al. This discrepancy might be because of the following reasons: (1) Our study was performed under arthroscopy with only the ATFL sutured, and (2) Waldrop et al performed ATFL repair using an open manner with one 3.0-mm suture anchor loaded with 2 No. 0 nonabsorbable continuous braided sutures, and 4 suture limbs were passed through the ligament and tied over the top with 2 knots. More soft tissues might have been sutured together.
Moreover, Cottom et al6 repaired a complete ATFL injury with a single-row 2–suture anchor construct in an open manner and with the suture limbs passed through the ATFL and inferior extensor retinaculum, and the failure load was 156.43 ± 30.39 N. Similarly, Giza et al11 repaired the lateral ankle ligament with two 3.0-mm suture anchors via arthroscopy, and suture limbs were passed percutaneously through the ATFL and CFL incorporating the inferior extensor retinaculum. Their test results showed a mean maximum load of 154.4 ± 60.3 N in the standard Broström repair group. Based on the previously published studies by Viens et al28 and Waldrop et al,29 the load to failure of the intact ATFL was approximately 154.0 N to 160.9 N. These findings indicate that ATFL repair with 2 anchors might be enough for complete ATFL injuries.
Generally, surgeons use a probe to feel the tension of the repaired ATFL. In the present study, no significant difference in tension was detected between groups, while the mean ultimate failure loads of the partial repair groups were significantly higher than those of the complete repair groups. These data have drawn our attention to the possibility that an optimal tension level of the repaired ATFL may not be equal to good biomechanical properties. Furthermore, the mean ultimate failure load for the partial ATFL injury groups was 81.9 ± 26.5 N with knot suture anchor and 88.1 ± 41.6 N with knotless anchor suture repair. Since our results presented the strength of the repaired ligament at approximately half of an intact one or even weaker, it illustrates the importance of protection from excessive stress for these repairs during the early postoperative rehabilitation phase, even for a partial ATFL injury.
In the present study, the mechanism of failure was at the ligament-suture interface for all specimens in the complete ATFL tear groups (groups A and B), while the mechanism of failure for the partial tear groups (groups C and D) was predominantly at the midsubstance and the distal attachment site. In their complete ATFL tear model, Waldrop et al29 similarly found that the mechanism of failure was at the ligament-suture interface for all specimens with or without 1-anchor repair. Previously, Cottom et al6 repaired a complete ATFL injury with a single-row 2–suture anchor construct in an open manner, and the final failure mechanism was 33.3% with anchor pullout, 33.3% with ligament-suture interface failure, and 33.3% with the tissues tearing from the talus. Brown et al4 compared biomechanical properties between specimens repaired with two 1.4-mm JuggerKnot all-soft suture anchors and the modified Brostrom-Gould technique with 2-0 FiberWire sutures only and found that the major mode of failure was a gradual manner of AFTL tissue failure rather than suture breakage or anchor pullout. All these findings indicate that 1 anchor, whether knot or knotless, is not enough for a complete ATFL tear at time zero after surgery, and 2-anchor repair may be a better option for complete ATFL injuries.
Commonly, we may find that a superior band of the ATFL is loose while an inferior band of the ATFL is tight, particularly in chronic ankle instability cases. Clinically, we would use 1 anchor to repair the superior band of the ATFL. Here, we wanted to make a model of a partial ATFL tear and analyze the biomechanical capacity of this construct. We acknowledge that partial tears would be expected to be inherently stronger than a complete tear that was repaired, which was also demonstrated in this study. We did not test the load to failure of the partial tears, as we did not have so many specimens. Moreover, the main purpose of this study was to perform a biomechanical comparison of the strength of the arthroscopic ATFL repair technique with knot or knotless suture anchors.
There were several limitations to this study. First, only the ATFL was investigated in this cohort. It is unclear whether there is any difference in terms of functional outcomes with or without CFL repair. Additional studies with larger sample sizes of CFL repair may be necessary to determine differences in patient-reported outcomes between groups. Second, the mean age of the cadavers was 66 ± 7 years, which is relatively old. The diminished bone density and poor ATFL tissue quality might have affected the biomechanical results. The final results appeared much lower than those of the study by Waldrop et al29; however, as far as our study purpose was concerned, there was no significant difference in biomechanical properties between the knot repair and knotless repair techniques.
Another limitation was that we did not have an intact ATFL group. However, the previously published studies by Viens et al28 and Waldrop et al indicated that the load to failure of the intact ATFL was approximately 154.0 to 160.9 N. Moreover, all the ATFL repairs were performed under arthroscopy in the present study. It is unclear if there would be a different result with an open ATFL repair. However, previous biomechanical studies have reported no statistical difference in strength or stiffness between traditional open repair and arthroscopic anatomic repair of the lateral ligaments of the ankle.9,10 Finally, this was an in vitro biomechanical study, which did not take into consideration the biological healing of the ATFL after repair. It is possible that the biomechanical properties of the different constructs increase after some time.
Conclusion
The results of the present study showed no significant difference in biomechanical properties between the knot repair and knotless repair techniques. However, the strength of the suture anchor repair in the complete ATFL injury models was much weaker than that in the partial ATFL injury models, indicating that 1–suture anchor repair is not suitable for complete ATFL injury.
Footnotes
Final revision submitted September 13, 2019; accepted October 4, 2019.
One or more of the authors declared the following potential conflict of interest or source of funding: This study was supported by the National Natural Science Foundation of China (81572209), Shanghai Excellent Talents Program (201609), and Shanghai Sports Science and Technology “Comprehensive Plan” Project (18Z004). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Huashan Hospital Fudan University Ethics Committee.
References
- 1. Acevedo JI, Mangone P. Arthroscopic Brostrom technique. Foot Ankle Int. 2015;36:465–473. [DOI] [PubMed] [Google Scholar]
- 2. Acevedo JI, Ortiz C, Golano P, Nery C. ArthroBrostrom lateral ankle stabilization technique: an anatomic study. Am J Sports Med. 2015;43:2564–2571. [DOI] [PubMed] [Google Scholar]
- 3. Barber FA, Coons DA, Ruiz-Suarez M. Cyclic load testing and ultimate failure strength of biodegradable glenoid anchors. Arthroscopy. 2008;24:224–228. [DOI] [PubMed] [Google Scholar]
- 4. Brown CA, Hurwit D, Behn A, Hunt KJ. Biomechanical comparison of an all-soft suture anchor with a modified Brostrom-Gould suture repair for lateral ligament reconstruction. Am J Sports Med. 2014;42:417–422. [DOI] [PubMed] [Google Scholar]
- 5. Corte-Real NM, Moreira RM. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213–217. [DOI] [PubMed] [Google Scholar]
- 6. Cottom JM, Baker JS, Richardson PE, Maker JM. A biomechanical comparison of 3 different arthroscopic lateral ankle stabilization techniques in 36 cadaveric ankles. J Foot Ankle Surg. 2016;55:1229–1233. [DOI] [PubMed] [Google Scholar]
- 7. Cottom JM, Rigby RB. The “all inside” arthroscopic Brostrom procedure: a prospective study of 40 consecutive patients. J Foot Ankle Surg. 2013;52:568–574. [DOI] [PubMed] [Google Scholar]
- 8. Denard PJ, Adams CR, Fischer NC, Piepenbrink M, Wijdicks CA. Knotless fixation is stronger and less variable than knotted constructs in securing a suture loop. Orthop J Sports Med. 2018;6:2325967118774000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Drakos MC, Behrens SB, Paller D, Murphy C, DiGiovanni CW. Biomechanical comparison of an open vs arthroscopic approach for lateral ankle instability. Foot Ankle Int. 2014;35:809–815. [DOI] [PubMed] [Google Scholar]
- 10. Giza E, Shin EC, Wong SE, et al. Arthroscopic suture anchor repair of the lateral ligament ankle complex: a cadaveric study. Am J Sports Med. 2013;41:2567–2572. [DOI] [PubMed] [Google Scholar]
- 11. Giza E, Whitlow SR, Williams BT, et al. Biomechanical analysis of an arthroscopic brostrom ankle ligament repair and a suture anchor-augmented repair. Foot Ankle Int. 2015;36:836–841. [DOI] [PubMed] [Google Scholar]
- 12. Guillo S, Bauer T, Lee JW, et al. Consensus in chronic ankle instability: aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res. 2013;99:S411–S419. [DOI] [PubMed] [Google Scholar]
- 13. Hua Y. Editorial commentary: repair of lateral ankle ligament. Is arthroscopic technique the next station? Arthroscopy. 2018;34:2504–2505. [DOI] [PubMed] [Google Scholar]
- 14. Jarrett CD, McGillivary GR, Hutton WC. The 2.5 mm PushLock suture anchor system versus a traditional suture anchor for ulnar collateral ligament injuries of the thumb: a biomechanical study. J Hand Surg Eur Vol. 2010;35:139–143. [DOI] [PubMed] [Google Scholar]
- 15. Kim ES, Lee KT, Park JS, Lee YK. Arthroscopic anterior talofibular ligament repair for chronic ankle instability with a suture anchor technique. Orthopedics. 2011;34:273. [DOI] [PubMed] [Google Scholar]
- 16. Li H, Hua Y, Li H, Ma K, Li S, Chen S. Activity level and function 2 years after anterior talofibular ligament repair: a comparison between arthroscopic repair and open repair procedures. Am J Sports Med. 2017;45:2044–2051. [DOI] [PubMed] [Google Scholar]
- 17. Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Brostrom repair using suture anchors. Am J Sports Med. 2009;37:488–494. [DOI] [PubMed] [Google Scholar]
- 18. Lui TH. Modified arthroscopic Brostrom procedure. Foot Ankle Surg. 2015;21:216–219. [DOI] [PubMed] [Google Scholar]
- 19. Matheny LM, Johnson NS, Liechti DJ, Clanton TO. Activity level and function after lateral ankle ligament repair versus reconstruction. Am J Sports Med. 2016;44:1301–1308. [DOI] [PubMed] [Google Scholar]
- 20. Matsui K, Takao M, Miyamoto W, Innami K, Matsushita T. Arthroscopic Brostrom repair with Gould augmentation via an accessory anterolateral port for lateral instability of the ankle. Arch Orthop Trauma Surg. 2014;134:1461–1467. [DOI] [PubMed] [Google Scholar]
- 21. Pellegrini MJ, Sevillano J, Ortiz C, Giza E, Carcuro G. Knotless modified arthroscopic-Brostrom technique for ankle instability. Foot Ankle Int. 2019;40(4):475–483. [DOI] [PubMed] [Google Scholar]
- 22. Pereira H, Vuurberg G, Gomes N, et al. Arthroscopic repair of ankle instability with all-soft knotless anchors. Arthrosc Tech. 2016;5:e99–e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Petrera M, Dwyer T, Theodoropoulos JS, Ogilvie-Harris DJ. Short- to medium-term outcomes after a modified Brostrom repair for lateral ankle instability with immediate postoperative weightbearing. Am J Sports Med. 2014;42:1542–1548. [DOI] [PubMed] [Google Scholar]
- 24. Ruiz-Suarez M, Aziz-Jacobo J, Barber FA. Cyclic load testing and ultimate failure strength of suture anchors in the acetabular rim. Arthroscopy. 2010;26:762–768. [DOI] [PubMed] [Google Scholar]
- 25. Takao M, Matsui K, Stone JW, et al. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sports Traumatol Arthrosc. 2016;24:1003–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vega J, Golano P, Pellegrino A, Rabat E, Pena F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34:1701–1709. [DOI] [PubMed] [Google Scholar]
- 27. Vega J, Guelfi M, Malagelada F, Pena F, Dalmau-Pastor M. Arthroscopic all-inside anterior talofibular ligament repair through a three-portal and no-ankle-distraction technique. JBJS Essent Surg Tech. 2018;8:e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Viens NA, Wijdicks CA, Campbell KJ, Laprade RF, Clanton TO. Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Brostrom repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405–411. [DOI] [PubMed] [Google Scholar]
- 29. Waldrop NE, 3rd, Wijdicks CA, Jansson KS, LaPrade RF, Clanton TO. Anatomic suture anchor versus the Brostrom technique for anterior talofibular ligament repair: a biomechanical comparison. Am J Sports Med. 2012;40:2590–2596. [DOI] [PubMed] [Google Scholar]