Abstract
Background:
Chronic strain and/or tendinopathy of the adductor longus tendon can be a cause of long-standing groin pain in the elite athlete, resulting in significant time lost from competition. Accurate diagnosis and treatment can expedite return to play.
Purpose/Hypothesis:
To evaluate return to sport and performance in National Collegiate Athletic Association (NCAA) Division I football players and National Football League (NFL) players following adductor longus release with or without sports hernia repair. We hypothesized that adductor release will be an effective method of treatment for recalcitrant groin/adductor pain in these athletes.
Study Design:
Case series; Level of evidence, 4.
Methods:
A cohort study was performed of all NFL players and NCAA Division I college athletes who had undergone an adductor longus tendon release with or without sports hernia repair by 1 of 2 fellowship-trained orthopaedic surgeons between May 1999 and January 2013. All patients reported groin pain below the inguinal ligament and localized to their adductor longus. Symptoms lasted longer than 10 weeks and limited their ability to effectively perform during sport, as assessed by their coach and self-assessment. Questionnaires were given to all 26 patients to assess long-term surgical outcomes. A subgroup analysis was performed for NFL players, in which “performance scores” were calculated according to individual player statistics while playing. Scores obtained before the diagnosis of chronic adductor longus tendinopathy or strain were compared with those after surgery. Patients with prior abdominal or pelvic surgery, radiographic evidence of degenerative joint disease of the hip, labral tears or femoral acetabular impingement, prostatic or urinary tract disease, or nerve entrapment of the ilioinguinal, genitofemoral, or lateral femoral cutaneous nerves were excluded from the study.
Results:
A total of 32 athletes underwent an adductor longus tenotomy during the study period. Of these patients, 28 were college- or professional-level athletes who underwent an adductor longus tenotomy, with a mean ± SD follow-up time of 6.2 ± 4.2 years (range, 12-178 months). Of the 32 patients, 20 had a concomitant sports hernia repair in addition to an adductor longus tenotomy. Thirty-one patients (97%) were able to return to their previous sport, and 30 (94%) were able to return at their previous level of play. Thirty patients (94%) reported that they were satisfied with their decision to have surgery. No player complained of weakness or a decrease in running speed or power. Mean return to play was 12 weeks from date of surgery. In the subgroup analysis of 16 NFL players, there were no statistically significant differences for the pre- versus postoperative comparisons of the athlete performance scores (P = .74) and the percentage of the games started versus played (P = .46). After separation of players who had a concomitant hernia repair from players who did not, there was no statistically significant difference in performance scores or percentages of games started.
Conclusion:
In this study of elite athletes, adductor longus tenotomy with or without a concomitant sports hernia repair provided overall acceptable and excellent results. Athletes were able to return to their previous level of athletic competition and performance with consistent relief of groin pain. Return to play in an NFL game averaged 12 weeks following surgery.
Keywords: sports hernia, adductor longus, tenotomy, treatment
Groin pain is a common problem for athletes. Diagnosis and management can be challenging. Studies have reported that injuries to the hip region can account for 5% to 9% of all injuries faced by high school athletes,1,3,10 and the incidence of groin pain has been reported as 10% to 18% in male soccer players.4,7,12,16 Time lost from sport owing to injury can be significant in these patients.9
Adductor tendinopathy is a well-established cause of groin pain in the athlete. In professional soccer players, it has been shown to account for 23% of the muscle injuries commonly affecting those between 22 and 30 years of age.5,17 While active physical therapy can be helpful in certain cases, for patients with recalcitrant adductor tendinopathy and pain, operative treatment can be effective.12,17 The results of surgical treatment, while promising, are limited. A common technique for treatment of recalcitrant adductor longus tendinopathy with release off its pubic attachment site has been described.8 The purpose of this study was to evaluate the outcome of adductor longus release for chronic recalcitrant tendinopathy on performance and return to sport for the elite athlete. The coexistence of sports hernias in many athletes with adductor longus tendinopathy is highlighted as well.
Methods
Institutional review board approval was obtained to identify and contact National Football League (NFL) players as well as college (National Collegiate Athletic Association Division I) and high school athletes who had undergone an adductor tendon release by 1 of 2 orthopaedic surgeons (T.J.G. and B.Z.) between May 1999 and January 2013. All patients older than 18 years were considered for this study. A total of 44 patients were identified, and 12 were lost to follow-up and excluded from the study. The remaining 32 patients agreed to participate in the study. These included 20 professional football players, 3 college football players, 3 college hockey players, 1 semiprofessional soccer player, 1 college soccer player, 1 recreational basketball player, 1 recreational volleyball player, 1 recreational runner, and 1 high school lacrosse player.
Patients were included if they had at least 12 months of follow-up. Patients with prior abdominal or pelvic surgery, radiographic evidence of degenerative joint disease of the hip, labral tears or femoral acetabular impingement, prostatic or urinary tract disease, or nerve entrapment of the ilioinguinal, genitofemoral, or lateral femoral cutaneous nerves were excluded from the study.
Each player initially presented with groin pain below the inguinal ligament localized to the adductor longus and had symptoms that lasted longer than 10 weeks and limited their ability to compete. During the initial physical examination, a complete examination of the hip joint was performed. Patients were screened for evidence of pain with internal rotation of the hip at 90° of flexion to rule out intra-articular sources of pain, such as labral tears and femoral acetabular impingement. The most reproducible finding was tenderness along the adductor longus tendon with resisted hip adduction in extension. An injection test with anesthetic in the proximal adductor longus tendon was used to confirm the adductor longus as the source of pain and exclude an intra-articular etiology. Plain radiographs of the pelvis and hip joint did not reveal significant degenerative changes or bony abnormalities. Patients with radiographic evidence of femoral acetabular impingement were excluded. Patients were diagnosed with chronic pain of the adductor origin if (1) all of their pain emanated from below the inguinal ligament, (2) pain was re-created with resisted hip adduction, (3) point tenderness was present over the proximal muscle tendon junction of the adductor longus, and (4) there was no tenderness over the pubic symphysis. All patients had failed a trial of nonoperative management, specifically activity modification and strengthening by a physical therapist.
Patients who consented to participate were asked to complete a questionnaire to assess the outcome of the procedure. Questions were asked about their ability to actively compete in sports, their level of function and range of motion in the area of the surgery, any current symptoms, and their current level of pain.
Performance-Based Outcome Measures
A subgroup analysis was performed for NFL players who underwent an adductor longus tenotomy by 1 of the 2 senior orthopedic surgeons. Their performance scores were calculated from publically available game statistics collected during regular season. Information used to calculate the performance scores consisted of games played, games started, seasons played, interceptions, sacks, touchdowns, and yards gained. This information was compared between pre- and postoperative athletic seasons.
A standardized, previously published player performance scoring system was used to evaluate the athletes.13 Relevant statistics related to the position played by the player were scored and then normalized by the amount of games played. Offensive line players were excluded from this scoring system because of a lack of measured game statistics available. The ratio of number of games played versus number of games started was also calculated as an additional measure of on-field performance. Each player served as his own control before and after treatment of the adductor longus tendinopathy.
Statistical Analysis
The Wilcoxon test was used to compare pre- and postoperative player performance scores and percentages of games started of those played. Statistical significance was accepted with P < .05.
Results
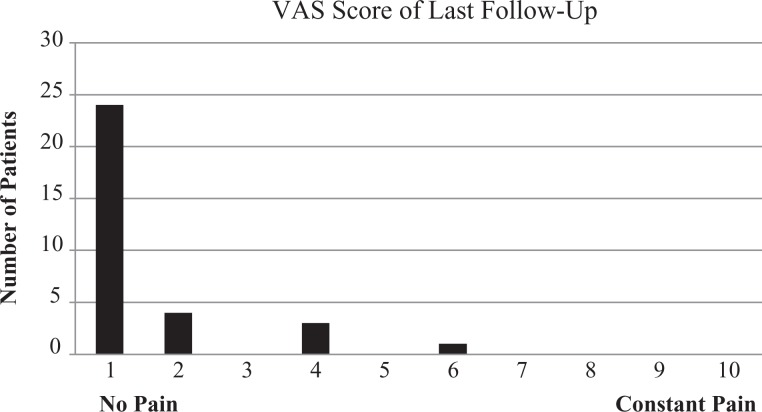
A total of 32 patients were able to participate in the study. Demographic information is highlighted in Table 1. All patients were male, and the mean age was 24.5 years at the time of the surgery (range, 18.1-34.5 years). The mean follow-up time was 68.3 months (range, 12-178 months); 20 patients were professional football players; and 20 players had a concomitant sports hernia repair in addition to adductor longus tenotomy performed by a fellowship-trained general surgeon based on preoperative diagnosis (see Table 2). There were no reported complications from the procedure, and each patient tolerated the procedure well. Overall, 31 (97%) patients reported a significant improvement in their symptoms; 30 (94%) reported an increase in their ability to participate in activities and sports; and 24 (75%) were asymptomatic at the time of follow-up (Figure 1). Furthermore, 22 (69%) patients felt that they had full hip range of motion at time of follow-up; 31 (97%) were able to return to their previous sport; and 30 (94%) were able to return at their previous level of play. Thirty patients (94%) also reported that they were satisfied with their decision to have surgery (Table 3). No player complained of weakness or decrease in running speed or power. Mean return to play was 12 weeks from date of surgery.
TABLE 1.
Demographic Informationa
| Sex, n | |
| Male | 32 |
| Female | 0 |
| Age at time of, y | |
| Adductor longus tendon release | 24.5 ± 4.0 (18.1-34.5) |
| Follow-up | 30.4 ± 6.1 (19.7-42.6) |
| Follow-up time from adductor longus tendon release, mo | 68.3 ± 49.3 (12-178) |
aData are reported as mean ± SD (range) unless otherwise indicated.
TABLE 2.
Patients by Sport Played and Surgical Procedure
| Athletes, n | |||
|---|---|---|---|
| Sport | Total | With an Isolated Adductor Release | With an Adductor Release and Concomitant Sports Hernia Repair |
| Professional football | 20 | 6 | 14 |
| Semiprofessional soccer | 1 | 1 | 0 |
| College | |||
| Football | 3 | 1 | 2 |
| Hockey | 3 | 2 | 1 |
| Soccer | 1 | 0 | 1 |
| Recreational | |||
| Basketball | 1 | 1 | 0 |
| Volleyball | 1 | 0 | 1 |
| Running | 1 | 1 | 0 |
| High school lacrosse | 1 | 0 | 1 |
Figure 1.
Visual analog scale (VAS) of pain level at most recent patient follow-up.
TABLE 3.
Patient Questionnaire (Yes/No)
| Patients Marking “Yes,” % | |
|---|---|
| Is the hip better now compared with preoperation? | 96.8 |
| Is your ability to participate in activities better now compared with preoperation? | 93.7 |
| Is your ability to participate and compete in sports better now compared with preoperation? | 93.7 |
| Were you able to return to the sport that you participated in preinjury? | 96.8 |
| Were you able to return to the same level of competition and ability compared with preinjury? | 93.7 |
| Are you able to compete without symptoms resulting from injury? | 75 |
| Would you undergo this surgery again? | 93.7 |
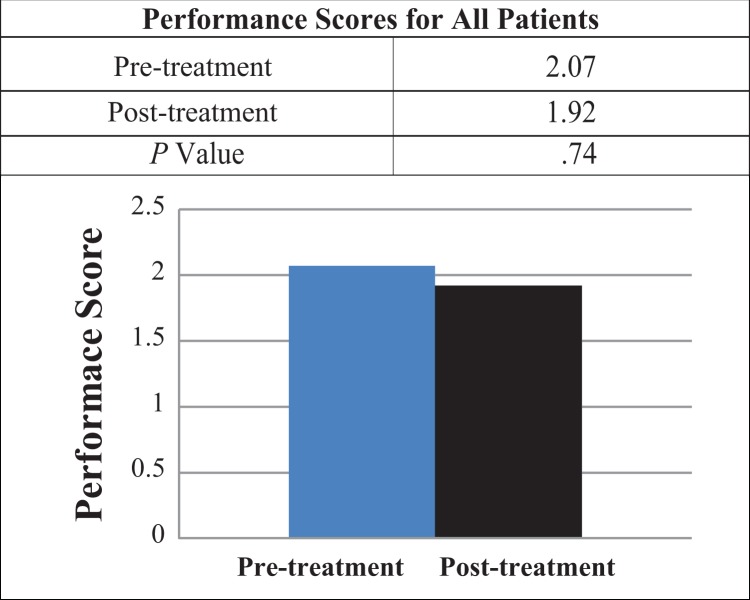
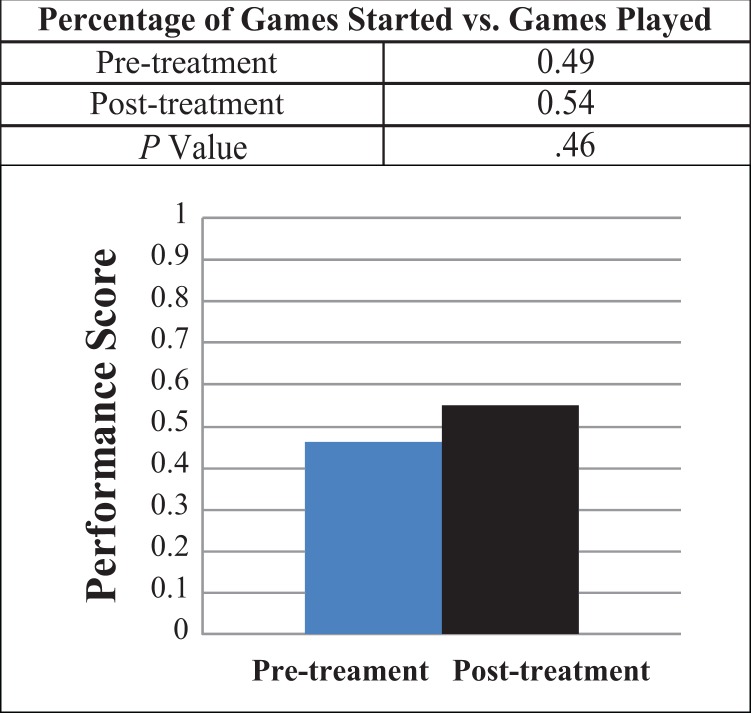
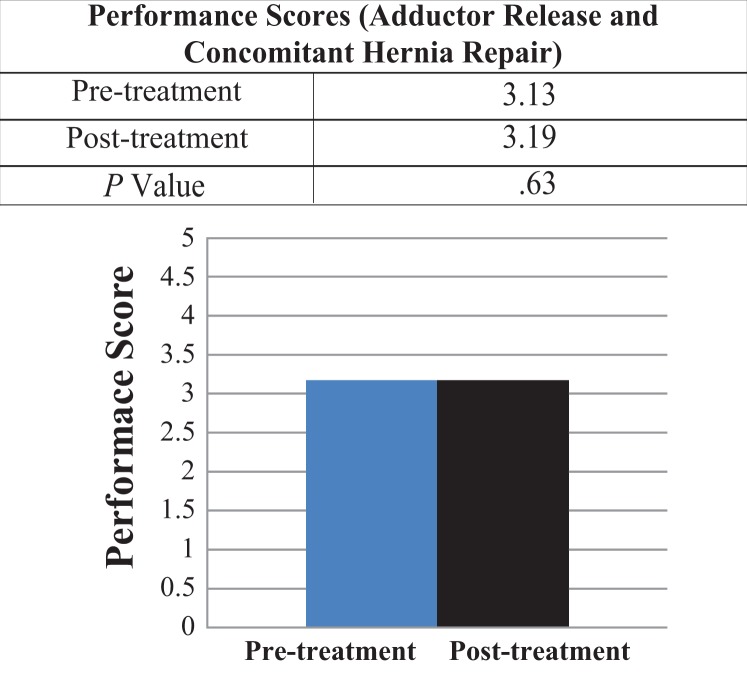
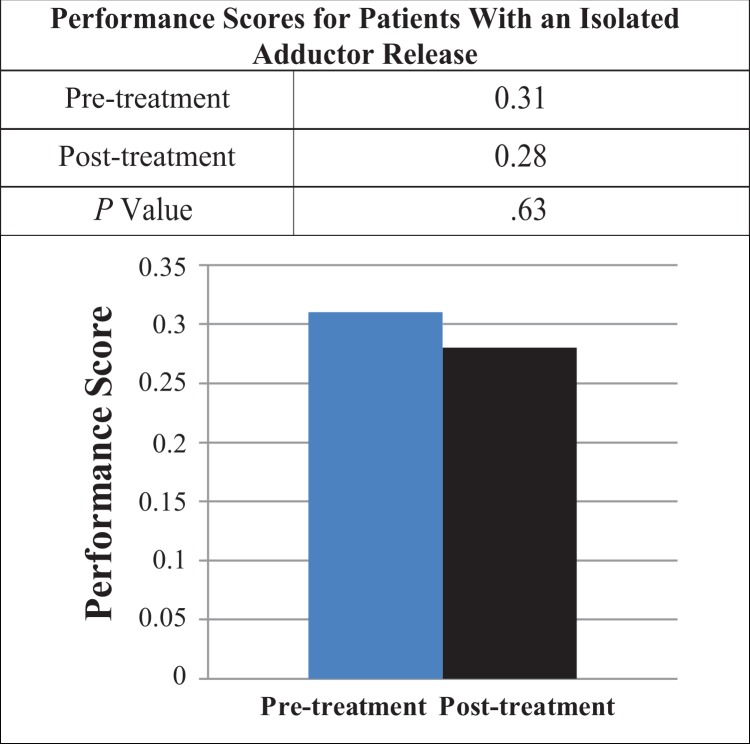
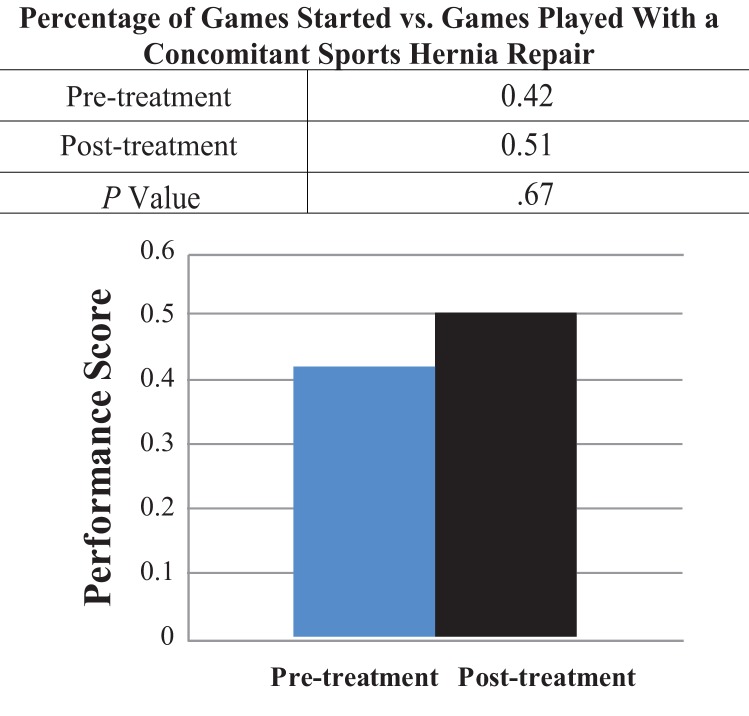
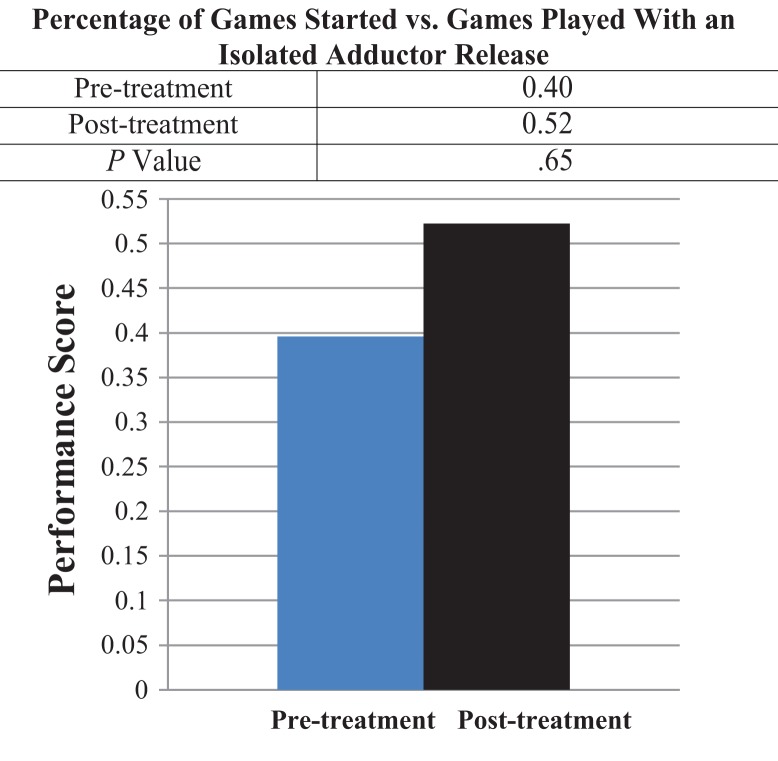
In the subgroup analysis of 16 NFL players, there were no statistically significant differences for the pre- versus postoperative comparison of the athlete performance scores (P = .74) (Figure 2) and the percentage of games started versus games played (P = .46) (Figure 3). After separation of players who had a concomitant hernia repair from players who did not, there was no statistically significant difference in performance scores or percentages of games started (Figures 4 -7).
Figure 2.
Performance scores for National Football League athletes.
Figure 3.
Percentage of games started versus games played for National Football League athletes.
Figure 4.
Performance scores for National Football League athletes who underwent an adductor release with a concomitant sports hernia repair.
Figure 5.
Performance scores for National Football League athletes who underwent an isolated adductor release.
Figure 6.
Percentage of games started versus games played for National Football League athletes who underwent an adductor release with a concomitant sports hernia repair.
Figure 7.
Percentage of games started versus games played for National Football League athletes who underwent an isolated adductor release.
Discussion
Tendinopathies can account for 10% of sports-related pathology.16,18 Adductor tendinopathy is a common cause of pain and has been associated with lower abdominal and inguinal pain in the high-performance athlete.6,15 As stated in our inclusion/exclusion criteria, players with any objective evidence of intra-articular hip pathology, such as femoral acetabular impingement, labral tear, or degenerative changes, were specifically excluded from this cohort to minimize bias of the results.
In a study by Brophy et al,2 NFL kickers were more likely to have injuries in the pelvis and hip than any other anatomic location, and muscle-tendon injuries were the most common type. Many patients can be treated effectively with an active training program.12 For patients with persistent recalcitrant pain, adductor longus release can provide an effective treatment option.8,11 The literature in professional athletes is limited, and findings are most commonly reported in soccer players. To our knowledge, there are no outcome studies of adductor longus release in professional football athletes. Maffulli et al14 showed a high return to sport at the preinjury level following bilateral adductor release for unilateral tendinopathy. In our study, 96% of all patients were able to return to their sport, and 93% were able to return at their previous level. All NFL athletes returned to sport at their previous level. There was a slight trend toward a greater percentage of games started posttreatment, but this did not reach statistical significance.
In total, 94% of patients reported that they would undergo the surgery again. There was a high percentage of patients who were diagnosed with concomitant sports hernia and had repair performed by a fellowship-trained general surgeon. Between the group undergoing isolated adductor release and the group with concomitant hernia repair, there were no significant differences in percentage of games started or performance scores.
We used a previously published scoring system13 for NFL players that allowed each player to serve as his own control. Scoring was based on the position and publically available performance statistics. This allowed us to evaluate performance in sport and compare the pre- and posttreatment states. There was no significant difference in these metrics after surgery. However, as mentioned, there was a trend toward a slightly higher percentage of games started.
We acknowledge some limitations of this study, including its retrospective design. We obtained subjective outcomes for nonprofessional athletes, and future directions are aimed at evaluating objective outcomes for these patients, including strength measurements. While the NFL players studied were evaluated with a performance score metric, offensive linemen could not be analyzed given the limits of the game statistics used in the calculation. However, surgery did not adversely affect the percentage of games started in this group.
Footnotes
Final revision submitted July 7, 2017; accepted July 18, 2017.
One or more of the authors has declared the following potential conflict of interest or source of funding: T.J.G. has received consulting fees from ConMed Linvatec and Mitek and royalties from SLACK Inc and has stock/stock options in Visionscope Technologies. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was approved by the Partners Healthcare Human Research Committee (protocol No. 2010P002275/MGH).
References
- 1. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521–533. [DOI] [PubMed] [Google Scholar]
- 2. Brophy RH, Wright RW, Powell JW, Matava MJ. Injuries to kickers in American football: the National Football League experience. Am J Sports Med. 2010;38(6):1166–1173. [DOI] [PubMed] [Google Scholar]
- 3. DeLee JC, Farney WC. Incidence of injury in Texas high school football. Am J Sports Med. 1992;20(5):575–580. [DOI] [PubMed] [Google Scholar]
- 4. Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15(3):267–270. [DOI] [PubMed] [Google Scholar]
- 5. Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–1232. [DOI] [PubMed] [Google Scholar]
- 6. Emblom BA, Mathis T, Aune K. Athletic pubalgia secondary to rectus abdominis-adductor longus aponeurotic plate injury: diagnosis, management, and operative treatment of 100 competitive athletes. Orthop J Sports Med. 2018;6(9):2325967118798333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Engstrom B, Forssblad M, Johansson C, Tornkvist H. Does a major knee injury definitely sideline an elite soccer player? Am J Sports Med. 1990;18(1):101–105. [DOI] [PubMed] [Google Scholar]
- 8. Gill TJ, Carroll KM, Makani A, Wall AJ, Dumont GD, Cohn RM. Surgical technique for treatment of recalcitrant adductor longus tendinopathy. Arthrosc Tech. 2014;3(2):e293–e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gilmore J. Groin pain in the soccer athlete: fact, fiction, and treatment. Clin Sports Med. 1998;17(4):787–793. [DOI] [PubMed] [Google Scholar]
- 10. Gomez E, DeLee JC, Farney WC. Incidence of injury in Texas girls’ high school basketball. Am J Sports Med. 1996;24(5):684–687. [DOI] [PubMed] [Google Scholar]
- 11. Harr JN, Brody F. Sports hernia repair with adductor tenotomy. Hernia. 2017;21(1):139–147. [DOI] [PubMed] [Google Scholar]
- 12. Holmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet. 1999;353(9151):439–443. [DOI] [PubMed] [Google Scholar]
- 13. Hsu WK. Outcomes following nonoperative and operative treatment for cervical disc herniations in National Football League athletes. Spine. 2011;36(10):800–805. [DOI] [PubMed] [Google Scholar]
- 14. Maffulli N, Loppini M, Longo UG, Denaro V. Bilateral mini-invasive adductor tenotomy for the management of chronic unilateral adductor longus tendinopathy in athletes. Am J Sports Med. 2012;40(8):1880–1886. [DOI] [PubMed] [Google Scholar]
- 15. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2–8. [DOI] [PubMed] [Google Scholar]
- 16. Nielsen AB, Yde J. Epidemiology and traumatology of injuries in soccer. Am J Sports Med. 1989;17(6):803–807. [DOI] [PubMed] [Google Scholar]
- 17. Schilders E, Dimitrakopoulou A, Cooke M, Bismil Q, Cooke C. Effectiveness of a selective partial adductor release for chronic adductor-related groin pain in professional athletes. Am J Sports Med. 2013;41(3):603–607. [DOI] [PubMed] [Google Scholar]
- 18. Valent A, Frizziero A, Bressan S, Zanella E, Giannotti E, Masiero S. Insertional tendinopathy of the adductors and rectus abdominis in athletes: a review. Muscles Ligaments Tendons J. 2012;2(2):142–148. [PMC free article] [PubMed] [Google Scholar]