Abstract
Background
Tele-monitoring (TM) is remote monitoring of individuals via info-communication technology, enabling them and their relatives or care-providers to recognize their health status conveniently. TM will be successful only if the individuals, often patients with medical conditions, are willing to accept and adopt it in their daily lives. This study aimed to determine the prevalence of willingness of patients with type 2 diabetes mellitus (T2DM) and/or hypertension towards the use of TM, and the factors influencing their uptake.
Methods
A cross-sectional survey was conducted at two public primary care clinics (polyclinics) in north-eastern Singapore, where TM had not been implemented. After the patients with T2DM and/or hypertension consented after fulfilling the eligibility criteria, they were first introduced to the concept of TM using pictogram and explanation by the investigators. Data on their demography, clinical parameters, technological literacy and acceptance of TM based on the Health Information Technology Acceptance Model (HITAM) were subsequently collected, computed, analyzed, followed by regression analyses to identify the factors associated with their willingness to use TM.
Results
Among 1125 eligible multi-ethnic Asian patients approached, 899 of them completed the assisted questionnaire survey, yielding a response rate of 79.9%. Their mean age was 58 ± 8 years, females 51.3% and Chinese 69.3%. Overall, 53.0% of the patients were willing to use TM. Personal beliefs on technology (OR = 3.54, 95%CI = 2.50–4.50, p < 0.001), prior technology utility (OR = 3.18, 95%CI = 1.57–6.42, p = 0.001), Patient’s requirements to be accompanied (OR = 1.48, 95% CI = 1.054–2.082, P = 0.03) Cost considerations (OR = 2.96, 95% CI = 2.257–3.388, P < 0.01) and technological literacy (OR = 2.77, 95%CI = 2.05–3.38, p < 0.001) were associated with willingness to use TM.
Conclusion
Slightly over half of the patients were willing to use TM. Factors such as age, ethnicity, technological literacy, beliefs and previous utility of technology of the patients have to be addressed before implementing TM in primary care.
Keywords: Tele-monitoring, Health information technology, Model, Type-2 diabetes mellitus, Hypertension
Background
Telemedicine or Telehealth is the delivery of healthcare services remotely by means of telecommunications technology [1, 2]. Tele-monitoring (TM is a method of remote monitoring of vital parameters by persons outside of healthcare setting (such as from their residences), which are transmitted electronically via blue tooth technology to the healthcare provider [3–8]. Leveraging on TM to check on the clinical status of patients with non-communicable diseases (NCD) such as Type 2 Diabetes mellitus (T2DM) and hypertension in the community is of particular significance and relevance to their optimal long term management. The global prevalence of NCD is increasing rapidly. T2DM was estimated to be 9% in 2014, contributing to 1.5 million deaths and 89 million disability-adjusted life-years (DALYS) [9]. Global prevalence for hypertension was even higher at over 22%, leading to 9.4 million deaths [1, 9].
There is thus an urgent need to curb the rising morbidity and mortality from these NCD. Traditional model of care for NCD is episodic. Physicians review patients during face-to-face consultations but do not have access to their clinical status in between consultations. Patients may develop complications as a result of events or occurrences that go unnoticed or unattended to during this interval, resulting in missed opportunities for early intervention to prevent adverse outcomes.
Optimal glycaemic and blood pressure (BP) control are critical in preventing vascular complications and mortality. Regular monitoring of these vital parameters via TM allows patients to gain better insights into their real-time diabetes and hypertension control in relation to their treatment. TM has shown to be beneficial for chronic disease management [3–8] such as in Diabetes mellitus management in children, outcomes in women with gestational Diabetes Mellitus, in management of uncontrolled hypertension and paired with self-monitoring of blood pressure. In addition, any abnormal health status trend detected via TM can alert the patients and their care providers, enabling them to take remedial measures to prevent complications. Thus, TM extends the scope of patient monitoring beyond the clinical setting, which is important for surveillance of NCD such as diabetes mellitus and hypertension.
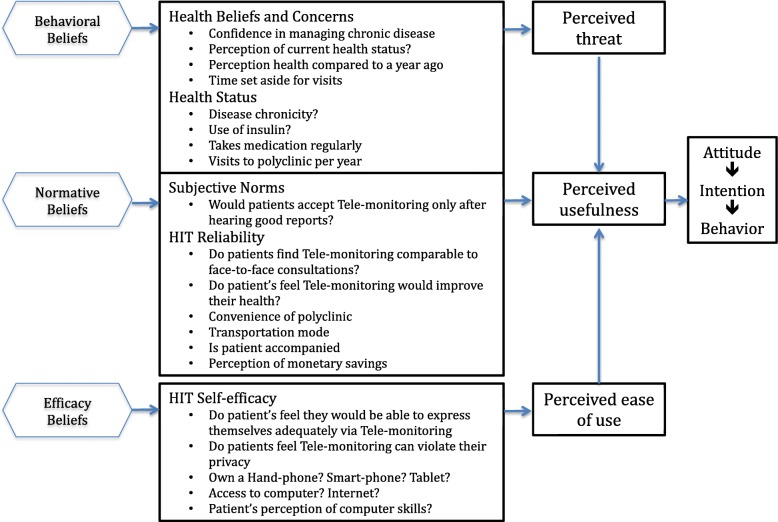
Acceptance and adoption of TM is pivotal in achieving its objectives. Despite its potential to complement traditional model of care, the benefits of TM can only be reaped if there is sufficient uptake by patients themselves. Theoretical frameworks have been developed to assess the acceptance of technology implementation in healthcare, one of which is the Health Information Technology Acceptance Model (HITAM) [10]. This framework takes into account behavioural beliefs, normative beliefs and efficacy belief, leading to the concepts of perceived threat, usefulness and ease of use respectively.
Understanding and addressing the barriers towards the use of TM is necessary for its successful implementation. Known deterrents of TM include older age, lower education, patients’ beliefs, concerns about the costs and privacy, and preferences for face-to-face consultations [11–16].
These factors are influenced by the socioeconomic, psychological and cultural context of the local population. Located at the centre of Southeast Asia, Singapore has an urbanised, Western-educated multi-ethnic Asian population with one of the highest penetrance of info-communication technology in the world [17, 18]. Nonetheless, a local study in 2008 reported that only 40.3% of patients, who were managed in public primary care centres (polyclinics), were willing to use communication technologies in healthcare services, namely Short Message Service (SMS) and internet [19]. Patients’ personal beliefs and technological literacy were the main factors which influenced their acceptance of a technology-based healthcare system. However, we postulated that the level of acceptance of TM would have risen since 2008, as info-communication technology has advanced significantly over the last decade to mitigate some of the barriers.
The need to re-evaluate the acceptability and perceptions of TM in Singapore is imminent, in view of rising prevalence of NCD such as T2DM and hypertension, and a shrinking workforce to support its rapidly aging population [20]. In the last 10 years, complexity of technology, access to technology, health behaviors and the medico-legal landscape have significantly evolved [21]. .Population demographics and healthcare needs in Singapore have also evolved in the past decade, with an aging population increasingly consisting of more educated and self-reliant middle-aged population, and a shift in focus from tertiary and acute care to preventive and primary care in the community. Since 2008, there have been greater integration of technology and healthcare such as through E-appointments, E-payment, Teleradiology at the institution where the study was executed. However, technology can be expensive. With rising number of people living with chronic diseases, increasing healthcare cost and increasing evidence to support the use of tele-monitoring in patients with non-communicable diseases, a re-evaluation of the acceptability and perceptions of Tele-monitoring in Singapore is timely to support its implementation successfully in the community, so as to maximize the use of scarce healthcare manpower and resources.. TM is a potential tool to maximise the healthcare manpower to manage these NCD and to engage the respective patients in self-management to optimise disease control and alleviate the rising disease burden. Thus the study aimed to determine the prevalence of willingness and associated factors in the use of TM by patients who consulted the polyclinics for their T2DM and/or hypertension management. It takes into consideration that patients have varying levels of understanding of tele-monitoring, and that tele-monitoring interventions, with the potential to be wide-ranging, are grounded by similar concepts.
Method
Study design
A cross-sectional observational study was conducted using interviewer-administered questionnaires. The questionnaires consists of 3 segments. First, information was collected on patients’ biodata, perceptions towards medical conditions, self-monitoring behaviours, accessibility to technology and technological literacy, underpinned by the Health Information Technology Acceptance Model (HITAM) [10, 22–33]. (Additional file 1: Questionnaire and Fig. 1).
Fig. 1.
HITAM Model with the relevant questions used in this study, adapted from: Kim J et al. [4]
Next, concepts and current TM services were introduced to each patient via a scripted explanation and information pamphlet to ensure a standardised understanding of TM across the study. (Figure 2 in Appendix): education segment. The information were standardized and scripted after close discussion with SingHealth Polyclinics, a major public primary healthcare provider.
In the final segment, the willingness to use TM and associated factors were assessed based on the question “Would you be willing to use tele-monitoring as part of managing your diabetes/ hypertension now?” Response options to this question were “Yes”, “Sometimes”, “No”, and “Unsure”. As TM will require a certain level of commitment to work as intended, a “yes” response was taken to mean that the patient was willing, while the remaining options were regarded as unwilling.
A pilot study was conducted at a clinic to assess the content of the questionnaire as well as the feasibility of its administration. Amendments were made based on the feedbacks and issues identified during the pilot study. The final questionnaire was also translated to mandarin language for ease of administration to the predominant Chinese patient pool in the polyclinics.
Study site and population
Multi-ethnic Asian patients were recruited from two public primary care clinics (polyclinics) located in Pasir Ris and Sengkang in north-eastern Singapore [34]. In 2015, the former manages daily attendances of 600–700 patients in an estate with a population of 139,890 residents. The latter attended to 1000–1100 patients daily in an estate populated by 206,690 residents.
The eligibility criteria for study participants were: aged 21–70 years old; had Type 2 DM and/or hypertension with ≥2 follow-up consultations within the past year and were able to converse in English or Mandarin. We excluded patients with prior exposure to TM and/or could not respond to the survey due to language, cognitive, hearing or visual barriers.
Recruitment
This study used consecutive sampling to recruit suitable patients. Study team members were stationed at the Health Monitoring Station (HMS) in each study site, where all patients on follow-up visits for diabetes and/or hypertension had measurements of their blood pressure and body mass index by trained healthcare workers. Every patient at the HMS from 7 to 15 February 2017 were approached and screened for their eligibility for this study.
After queries on the study were addressed, verbal consent was obtained from each patient in a private room where the questionnaire survey was conducted. A participant information sheet was provided for all participants. A total of 37 interviewers, comprising final year medical students, underwent rigorous pre-implementation training prior to the study initiation. Every interviewer used the standardized script to administer the questionnaire to ensure consistency.
Sample size estimation and statistical analysis
Assuming a 3% error margin and a prevalence of willingness of 66.8% derived from studies done overseas, it was estimated that a total of 944 respondents would be required [35–37]. All statistical analyses were performed using IBM SPSS Statistics software Version 23.0 (IBM Co., Armonk, New York, US). Descriptive data is presented as counts and in percentages. Bivariate analyses were conducted using the Pearson Chi-Squared Test for categorical variables. To adjust for confounding variables, a logistic regression model was performed on all factors that were significant in the univariate analysis. A p-value of < 0.05 was used to determine statistical significance.
Ethics approval and funding
This study was approved by SingHealth Centralised Institutional Review Board (CIRB Ref: 2016/3162). Funding for printing of questionnaires and materials was provided by the Yong Loo Lin School of Medicine at the National University of Singapore. The investigators declared no conflict of interest in this study.
Results
Among the 1125 eligible patients who were approached, 899 of them consented and completed the survey, yielding a response rate of 79.9%. The demographic characteristics of the study population are presented in Table 1.
Table 1.
Socio-demographic characteristics of patients and their willingness to use TM
| Total, n (%) | Willinga, n (%) | Odds ratio and confidence Interval | p value | |
|---|---|---|---|---|
| All participants | 899 (100) | 472 (52.5) | NA | NA |
| Gender | ||||
| Female | 460 (51.2) | 224 (48.7) | Reference | 0.02 |
| Male | 439 (48.8) | 248 (56.5) | 1.367 (1.051–1.779) | |
| Age | ||||
| ≤ 59 | 465 (51.7) | 278 (59.8) | 1.838 (1.410–2.398) | < 0.01 |
| 60 and older | 434 (48.3) | 194 (44.7) | Reference | |
| Age (10 year intervals) | ||||
| ≤ 40 | 22 (2.4) | 17 (77.3) | < 0.01 | |
| 41–50 | 115 (12.8) | 78 (67.8) | ||
| 51–60 | 382 (42.5) | 209 (54.7) | ||
| 61–70 | 380 (42.3) | 168 (44.2) | ||
| Ethnicity | ||||
| Chinese | 626 (69.6) | 305 (48.7) | Reference | |
| Non-Chinese | 273 (30.4) | 167 (61.2) | 1.658 (1.240–2.212) | < 0.01 |
| Spoken language | ||||
| Chinese | 329 (36.6) | 130 (39.5) | Reference | |
| English | 570 (63.4) | 342 (60.0) | 2.293 (1.739–3.030) | < 0.01 |
| Marital statusa | 895 (100) | 471 (52.6) | ||
| Single | 171 (19.1) | 77 (45.0) | Reference | |
| Married | 724 (80.9) | 394 (54.4) | 1.458 (1.043–2.037) | 0.03 |
| Employment statusa | 892 (100) | 469 (52.6) | ||
| Working | 538 (60.3) | 306 (56.9) | 1.546 (1.180–2.024) | < 0.01 |
| Not working | 354 (39.7) | 163 (46.0) | Reference | |
| Highest education level | ||||
| None/ PSLE | 231 (25.7) | 92 (39.8) | Reference | |
| O-Level and higher | 668 (74.3) | 380 (56.9) | 1.994 (1.470–2.704) | < 0.01 |
| Total household incomea (S$) | 668 (100) | 378 (56.6) | ||
| < 3400 | 317 (47.5) | 162 (51.1) | Reference | |
| ≥ 3400 | 351 (52.5) | 216 (61.5) | 1.531 (1.125–2.083) | < 0.01 |
| Financial assistancea | 895 (100) | 470 (52.5) | ||
| Yes | 392 (43.8) | 182 (46.4) | Reference | |
| No | 503 (56.2) | 288 (57.3) | 1.545 (1.184–2.016) | < 0.01 |
an for these factors are < 899 instead of the total n = 889 participants as some individuals deemed these questions sensitive and declined to answer.
Primary study objective: willingness to take-up Tele-monitoring
A total of 472 patients (52.5%) were willing to take up TM to manage their condition, regardless of their medical conditions. Among the 427 participants who reported unwillingness to use TM, 52.2% of them felt that they would be willing after hearing positive reports.
Factors associated with willingness to take up Tele-monitoring
All socio-demographic characteristics investigated were significantly associated with willingness to take up TM based on univariate analysis. Younger, males, married, minority ethnicity, English speaking, working patients, those with higher education, those with higher income and those without any need for financial assistance were more willing to use TM (Table 1).
Table 2 shows the HITAM related factors which were associated with willingness to use TM. Hand-phone and smartphone ownerships, and self-reported computer skills were associated with increased willingness to use TM. In contrast, patients who set aside more time for polyclinic visits, and those who had concerns about privacy violations were less willing to use TM.
Table 2.
HITAM-related factors influencing willingness to use TM (Univariate analysis)
| Total, n(%) | Willinga, n(%) | Odds ratio and confidence Interval | P Value | |
|---|---|---|---|---|
| Behavioural Beliefs (Health Status) | ||||
| No. of Years since diagnosis of diabetes mellitusa | ||||
| 5 or less | 210 (49.5) | 123 (58.6) | 1.672 (1.139–2.457) | < 0.01 |
| More than 5 years | 214 (50.5% | 98 (45.8) | Reference | |
| No. of Years since diagnosis of hypertensiona | ||||
| 5 or less | 298 (40.7) | 167 (56.0) | 1.298 (1.020–1.745) | 0.10 |
| More than 5 years | 434 (59.3) | 215 (49.5) | Reference | |
| Is patient on insulin injectiona | ||||
| On insulin | 49 (11.3) | 27 (55.1) | 1.165 (0.641–2.117) | 0.65 |
| Not on insulin | 384 (88.7) | 197 (51.3) | Reference | |
| T2DM and Hypertension medicationa | ||||
| Takes regularly | 849 (94.6) | 449 (52.9) | 1.220 (0.682–2.184) | 0.55 |
| Does not take regularly | 48 (5.4) | 23 (47.9) | Reference | |
| Visits to Polyclinic per yeara | ||||
| 4 or less visits | 587 (65.5) | 296 (62.7) | 1.301 (0.986–1.717) | 0.07 |
| More than 4 visits | 309 (34.5) | 176 (57.0) | Reference | |
| Behavioural beliefs (health beliefs and concerns) | ||||
| In general, would you say your health is (i.e. perception of health): | ||||
| Good | 504 (56.1) | 293 (58.1) | 1.676 (1.285–2.185) | < 0.01 |
| Poor | 395 (43.9) | 179 (45.3) | Reference | |
| How much time did the patient set aside for the appointment todaya | ||||
| < 3 h | 705 (78.5) | 385 (54.6) | 1.427 (1.036–1.964) | 0.03 |
| > 3 Hours | 193 (21.5) | 88 (45.6) | Reference | |
| Confidence managing T2DM/Hypertension | ||||
| Confident | 630 (70.1) | 350 (74.2) | 1.506 (1.130–2.007) | 0.06 |
| Not confident | 269 (29.9) | 122 (45.4) | Reference | |
| Perception of health compared to 1 year agoa | ||||
| Worse health | 197 (21.9) | 87 (44.2) | Reference | |
| Same or better | 701 (78.1) | 384 (54.7) | 1.532 (1.114–2.105) | 0.01 |
| Normative beliefs (hit reliability) | ||||
| TM would be satisfactory compared to seeing the doctor in persona | ||||
| Agree | 316 (35.1) | 225 (71.2) | 3.535 (2.5–4.449) | < 0.01 |
| Disagree | 582 (64.9) | 247 (42.4) | Reference | |
| Convenience of visit to polyclinic | ||||
| Convenient | 825 (91.8) | 435 (52.7) | 1.115 (0.693–1.795) | 0.72 |
| Not convenient | 74 (8.2) | 37 (50.0) | Reference | |
| Transport Mode† | ||||
| Public or personal transport | 626 (72.2) | 334 (53.4) | 1.116 (0.829–1.502) | 0.50 |
| Walk | 241 (27.8) | 122 (50.6) | Reference | |
| Is patient accompanied | ||||
| Accompanied | 169 (18.8) | 102 (60.4) | 1.481 (1.054–2.082) | 0.03 |
| Not accompanied | 730 (81.2) | 370 (50.7) | Reference | |
| Perceptions on monetary savings from telemedicinea | ||||
| Saves money | 470 (52.4) | 306 (65.1) | 2.963 (2.257–3.388) | < 0.01 |
| Does not save money | 427 (47.6) | 165 (38.6) | Reference | |
| Normative beliefs (Subjective Norms) | ||||
| Patient would be more convinced after seeing benefits from reports | ||||
| More willing | 532 (59.2) | 309 (58.1) | 1.734 (1.326–2.268) | < 0.01 |
| Not more willing | 367 (40.8) | 163 (44.4) | Reference | |
| Efficacy beliefs (hit self efficacy) | ||||
| Patients feel they would not be able to explain their problems adequately via tele-monitoring.a | ||||
| Disagree | 465 (51.8) | 203 (43.7) | Reference | |
| Agree | 433 (48.2) | 268 (61.9) | 2.096 (1.605–2.740) | < 0.01 |
| Tele-monitoring can violate patients’ privacy | ||||
| Agree | 204 (22.7) | 90 (44.1) | Reference | |
| Disagree | 695 (77.3) | 382 (55.0) | 1.546 (1.129–2.119) | < 0.01 |
| Handphonea | ||||
| Owns | 857 (95.4) | 461 (53.8) | 3.175 (1.571–6.418) | < 0.01 |
| Does not own | 41 (4.6) | 11 (26.8) | Reference | |
| Smartphonea | ||||
| Owns | 778 (86.6) | 433 (55.7) | 2.607 (1.735–3.917) | < 0.01 |
| Does not own | 120 (13.4) | 39 (32.5) | Reference | |
| Access to computera | ||||
| Has access to computer | 666 (74.2) | 384 (57.7) | 2.228 (1.640–3.027) | < 0.01 |
| No access to computer | 232 (25.8) | 88 (37.9) | Reference | |
| Access to internet | ||||
| Yes | 792 (88.4) | 435 (54.9) | 2.206 (1.442–3.375) | < 0.01 |
| No | 232 (11.6) | 37 (15.9) | Reference | |
| Computer skillsa | ||||
| Yes | 635 (70.6) | 380 (59.8) | 2.77 (2.054–3.375) | < 0.01 |
| No | 262 (29.4) | 93 (35.5) | Reference | |
| Use Smartphone appsa | ||||
| Uses apps | 609 (78) | 366 (60.1) | 2.36 (1.669–3.339) | < 0.01 |
| Does not use apps | 172 (22) | 67 (39.0) | Reference | |
| Tablets | ||||
| Owns | 407 (45.5) | 252 (61.9) | 2.023 (1.547–2.645) | < 0.01 |
| Does not own | 487 (54.5) | 217 (44.6) | Reference | |
| Patient feels communication devices too challenging | ||||
| Challenging | 397 (44.2) | 160 (40.3) | Reference | |
| Not Challenging | 502 (55.8) | 312 (62.2) | 2.227 (1.859–3.185) | < 0.01 |
an for these factors are < 899 instead of the total n = 889 participants as the question was not applicable to the participant or they declined to answer
Results of the multi-variate analysis are presented in Table 3. Patients who perceived comparable satisfaction between TM and face-to face physician consultation, no privacy violation, cost savings with TM, need accompaniment for physician visit, were convinced of positive results of TM, and did not face challenges in using communication devices, were associated with willingness to take up TM.
Table 3.
Factors associated with willingness to use TM
| Factors associated with willingness | p-value | Odds ratio |
|---|---|---|
| Gender | 0.44 | 0.875 (0.622–1.231) |
| Age | 0.29 | 0.826 (0.579–1.178) |
| Ethnicity | 0.13 | 0.743 (0.507–1.087) |
| Highest Education | 0.30 | 1.271 (0.806–2.004) |
| Employment | 0.41 | 1.164 (0.811–1.671) |
| Marital Status | 0.94 | 1.018 (0.669–1.548) |
| Financial Assistance | 0.18 | 0.794 (0.567–1.112) |
| (Perception of Health) In general, would you say your health is: | 0.21 | 1.240 (0.886–1.736) |
| How much time did the patient set aside for the appointment today | 0.32 | 0.821 (0.556–1.214) |
| Perception of health compared to 1 year agoa | 0.70 | 1.082 (0.723–1.620) |
| Tele-monitoring would be satisfactory compared to seeing the doctor in person. | < 0.01 | 2.790 (1.961–3.970) |
| Is patient accompanied | 0.04 | 1.595 (1.029–2.473) |
| Perceptions on monetary savings from telemedicinea | 0.01 | 1.777 (1.279–2.469) |
| Patient would be more convinced after seeing benefits from reports | 0.04 | 1.425 (1.019–1.994) |
| Tele-monitoring can violate patients’ privacy | 0.02 | 0.635 (0.432–0.934) |
| Handphonea | 0.67 | 0.483 (0.017–13.359) |
| Access to computera | 0.22 | 1.323 (0.841–2.082) |
| Access to internet | 0.41 | 0.748 (0.375–1.493) |
| Computer skillsa | 0.11 | 1.480 (0.913–2.401) |
| Use Smartphone appsa | 0.34 | 1.235 (0.798–1.911) |
| Tablet | 0.08 | 1.352 (0.968–1.890) |
| Patient feels communication devices too challenging | 0.02 | 1.546 (1.088–2.192) |
| Patient is concerned they are unable to express their problems over telemonitoring | 0.06 | 1.585 (1.139–2.203) |
an for these factors are < 899 instead of the total n = 889 participants as the question was not applicable to the participant or they declined to answer.
Discussion
Our study revealed a slim majority of our study population (52.5%) were willing to use TM to manage their NCD. Nonetheless, the willingness to use TM has increased compared to 40.3% in the earlier survey [19]. In this study 95.1 and 88.5% of patients owned a hand-phone and had access to the internet respectively, versus 71.2 and 49.4% in the earlier study.
Greater access to mobile technology is postulated to be associated with the rising willingness to use TM. Based on HITAM, ownership of hand-phone(s), usage of smartphone apps and having at least basic computer skills were important ‘technological’ factors influencing the use of TM (Table 2). Those who found “using communication devices challenging” were less willing to use TM (Table 3). Nevertheless, over these years, government agencies have launched programmes, such as the Smart Nation Singapore initiative, to improve the technology literacy of the local population [38]. Specific efforts are directed to equip the elderly with the relevant technological skills through various free or heavily subsidized courses and workshops in the community [39]. The prevalence of willingness to use TM in disease surveillance is expected to escalate in the immediate future with these measures to lower the barriers [19].
Patients who required caregivers to accompany them for their physician consultation were more willing to use TM. Convenience is likely the major attributing factor. For stable patients who are diligently monitoring their clinical parameters, TM could potentially replace a physician visit but safety has to be evaluated more stringently with appropriately designed trial. The healthcare infrastructure must also be able to document their health status via linkage to the electronic health records and support the continuity and timely supply of their medications. However, TM should not be confused with tele-consultation. It should remain as an adjunct tool to support patients in their chronic disease management.
Individual beliefs and perceptions of TM in healthcare also influence a patient’s willingness to use TM. Patients were more willing to use TM if they were shown reported evidences of its effectiveness. However, the results showed that patients had other concerns.
The fee-for-service healthcare system in Singapore also has implications for the introduction of TM to patients. Patients who consult primary care physicians have to pay for the services and medications. The technology involved in TM can be expensive and cost will eventually be passed over to these primary care users. What mattered to them seemed to be their perceived cost-savings of using the TM system, as alluded in this study. Cost consideration for adding on TM to a polyclinic consultation is inevitable. It is imperative to assess if the population is ready to pay for the new technology in monitoring their health. Substitution for a face-to-face consultation when clinical parameters from the TM system are stable and economy of scale when the pool of users expands can potentially lead to cost-savings. Thus, aside from patients, the results of the study will interest the health finance and policy makers to evaluate the feasibility and cost-effectiveness of scaling up a TM system to support chronic disease management nation-wide.
These factors are potentially modifiable but will require time and intervention to gain public trust. TM has been implemented in isolated private healthcare system in Singapore but the results are not published [40]. A well-designed randomised controlled trial on TM is being planned in a public primary care institution, which will be able to provide proof of values in terms of satisfaction of TM to the users, its cost-effectiveness and scalability in its implementation.
Perception of non-intrusion to personal privacy in using TM is also a key influencing factor. A TM system with secured data encryption, data repository and restricted access when transmitting patient data to healthcare providers [41] is essential for its implementation [42]. .Privacy protection is especially critical where multiple incidences of data breaches in local healthcare systems were recently reported [43, 44]. Local healthcare providers have to work closely with the official IT governing agencies to ensure strict adherence to measures which have since been implemented for personal data protection.
The strength of this study lies in the systematic sampling of the potential patients, notwithstanding the large daily volumes of patients at the study sites. The results showed that perceptions and beliefs of TM influenced the willingness of its adoption. They are modifiable and can be mitigated with appropriate measures to optimise the successful implementation of TM in primary care.
Nonetheless, we acknowledged that self-reported willingness to adopt TM might not correspond to actual utility by the patients. The forthcoming trial will provide more objective evidences of TM utilization.
Conclusion
Our study showed that 52.5% of patients with T2DM and/or hypertension reported willingness to adopt TM. They were influenced by perceived effectiveness ease of use, cost savings, privacy protection, and satisfaction of care using TM compared to face-to-face physician consultation. It is heartening to recognise from the results that the awareness of telemonitoring among patients has increased with the growth and expanding use of technology in our society. A randomised controlled study (RCT) is to be implemented soon, to prove effectiveness in health outcomes of the patients recruited into the telemonitoring system compared with usual care. Beyond the RCT, there are plans to scale up the telemonitoring system to cater to those who are currently unwilling to use it using implementation science approaches.
Supplementary information
Acknowledgements
The authors would like to thank the two teams of medical students from the Yong Loo Lin School of Medicine, who recruited the patients and the polyclinic staff at the study sites who supported the study implementation. They are also grateful to Patricia Kin and Caris Tan for helping in the submission of the study protocol to the ethics committee and Eileen Koh for reviewing the statistical analysis and tutors from the School of Public Health at the National University of Singapore.
Abbreviations
- BP
Blood pressure
- DALYS
Disability-adjusted life-years
- HITAM
Health Information Technology Acceptance Model
- HMS
Health Monitoring Station
- NCD
Non-communicable diseases
- SMS
Short Message Service
- T2DM
Type 2 Diabetes mellitus
- TM
Tele-monitoring
Appendix
Fig. 2.
Infographic on Tele-monitoring to educate participants
Authors’ contributions
DYES, DWWY and TYQ designed the study; M-RF, XG, PKSM, NCT reviewed and approved the study; DYES, DWWY and TYQ led the study team, recruited the patients, collated and analysed the data, reported the results; DYES drafted the manuscript; XG, PKSM, NCT reviewed and revised the manuscript; all authors reviewed and approved the final draft.
Funding
No funding.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by Singhealth Centralised Institutional Review Board (CIRB Ref: 2016/3162). After queries on the study were addressed, verbal consent was obtained from each patient (including consent for findings of the study to be published) in a private room where the questionnaire survey was conducted. A participant information sheet was provided for all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12911-020-1024-4.
References
- 1.Organisation, W.H . Telemedicine, opportunities and developments in Memeber states. 2010. p. 2. [Google Scholar]
- 2.Coiera E. Essentials of telemedicine and Telecare. Brit Med J. 2002;324(7345):1104. doi: 10.1136/bmj.324.7345.1104. [DOI] [Google Scholar]
- 3.Losiouk E, et al. Parental evaluation of a telemonitoring service for children with type 1 diabetes. J Telemed Telecare. 2018;24(3):230–237. doi: 10.1177/1357633X17695172. [DOI] [PubMed] [Google Scholar]
- 4.Al-Ofi EA, et al. Management of postprandial hyperglycaemia and weight gain in women with gestational diabetes mellitus using a novel telemonitoring system. J Int Med Res. 2019;47(2):754–764. doi: 10.1177/0300060518809872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Margolis KL, et al. Long-term outcomes of the effects of home blood pressure Telemonitoring and pharmacist management on blood pressure among adults with uncontrolled hypertension: follow-up of a cluster randomized clinical trial. JAMA Netw Open. 2018;1(5):e181617. doi: 10.1001/jamanetworkopen.2018.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wild SH, et al. Supported Telemonitoring and glycemic control in people with type 2 diabetes: the Telescot diabetes pragmatic multicenter randomized controlled trial. PLoS Med. 2016;13(7):e1002098. doi: 10.1371/journal.pmed.1002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKinstry B, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013;346:f3030. doi: 10.1136/bmj.f3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tucker KL, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. doi: 10.1371/journal.pmed.1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Organisation, W.H . Global status report on noncommunicable diseases 2014. 2014. [Google Scholar]
- 10.Kim J, Park HA. Development of a health information technology acceptance model using consumers' health behavior intention. J Med Internet Res. 2012;14(5):e133. doi: 10.2196/jmir.2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorst SL, et al. Home telehealth uptake and continued use among heart failure and chronic obstructive pulmonary disease patients: a systematic review. Ann Behav Med. 2014;48(3):323–336. doi: 10.1007/s12160-014-9607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albert NM, et al. Factors associated with telemonitoring use among patients with chronic heart failure. J Telemed Telecare. 2017;23(2):283–291. doi: 10.1177/1357633X16630444. [DOI] [PubMed] [Google Scholar]
- 13.Jung SG, et al. Preference and awareness of telemedicine in primary care patients. Korean J Fam Med. 2012;33(1):25–33. doi: 10.4082/kjfm.2012.33.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asche SE, et al. Patient characteristics associated with greater blood pressure control in a randomized trial of home blood pressure telemonitoring and pharmacist management. J Am Soc Hypertens. 2016;10(11):873–880. doi: 10.1016/j.jash.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Currell R, et al. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;2:CD002098. doi: 10.1002/14651858.CD002098. [DOI] [PubMed] [Google Scholar]
- 16.Heinzelmann PJ, Lugn NE, Kvedar JC. Telemedicine in the future. J Telemed Telecare. 2005;11(8):384–390. doi: 10.1177/1357633X0501100802. [DOI] [PubMed] [Google Scholar]
- 17.Division, U.N.S . Percentage of individuals using the internet. 2014. [Google Scholar]
- 18.Fund, U.N.C.s . Internet Users. 2011. [Google Scholar]
- 19.Luo N, et al. Acceptance of information and communication technologies for healthcare delivery: a SingHealth polyclinics study. Ann Acad Med Singapore. 2009;38(6):529–528. [PubMed] [Google Scholar]
- 20.Phan TP, et al. Forecasting the burden of type 2 diabetes in Singapore using a demographic epidemiological model of Singapore. BMJ Open Diabetes Res Care. 2014;2(1):e000012. doi: 10.1136/bmjdrc-2013-000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao G, Wei D. Mobile health: new technologies, new modes and new era. J Biomed Res. 2016;30(4):251–252. doi: 10.7555/JBR.30.20160002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health, S . National Health Survey 2010. Singapore: Ministry of Health: Ministry of Health; 2010. [Google Scholar]
- 23.Bradford NK, Caffery LJ, Smith AC. Awareness, experiences and perceptions of telehealth in a rural Queensland community. BMC Health Serv Res. 2015;15:427. doi: 10.1186/s12913-015-1094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gwee KA, Setia S. Demographics and health care seeking behavior of Singaporean women with chronic constipation: implications for therapeutic management. Int J Gen Med. 2012;5:287–302. doi: 10.2147/IJGM.S29011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singapore, G.o . General Household Survey 2015. 2016. [Google Scholar]
- 26.Ayatollahi A, et al. Computer and internet use among undergraduate medical students in Iran. Pak J Med Sci. 2014;30(5):1054–1058. doi: 10.12669/pjms.305.5355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forman LJ, Pomerantz SC. Computer-assisted instruction: a survey on the attitudes of osteopathic medical students. J Am Osteopath Assoc. 2006;106(9):571–578. [PubMed] [Google Scholar]
- 28.Wiseman JT, et al. Conceptualizing smartphone use in outpatient wound assessment: patients' and caregivers' willingness to use technology. J Surg Res. 2015;198(1):245–251. doi: 10.1016/j.jss.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim MY, et al. Feasibility of a smartphone application based action plan and monitoring in asthma. Asia Pac Allergy. 2016;6(3):174–180. doi: 10.5415/apallergy.2016.6.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmed SN, et al. Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient's perspective. Epilepsia. 2008;49(4):573–585. doi: 10.1111/j.1528-1167.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 31.Center, S.P.E.R . Sample Questionnaire Diabetes. 2007. [Google Scholar]
- 32.Nolte E, Knai C, Saltman RB. Assessing chronic disease management in European health systems, Concepts and approaches. 2014. [PubMed] [Google Scholar]
- 33.Chow WL, et al. Factors that influence the choice of seeking treatment at polyclinics. Singapore Med J. 2012;53(2):109–115. [PubMed] [Google Scholar]
- 34.Singapore, D.o.S . Population trends 2017, D.o.S. Singapore: Department of Statistics Singapore website; 2017. [Google Scholar]
- 35.Shaw RJ, et al. Organizational factors associated with readiness to implement and translate a primary care based telemedicine behavioral program to improve blood pressure control: the HTN-IMPROVE study. Implement Sci. 2013;8:106. doi: 10.1186/1748-5908-8-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Watson AJ, et al. Reevaluating the digital divide: current lack of internet use is not a barrier to adoption of novel health information technology. Diabetes Care. 2008;31(3):433–435. doi: 10.2337/dc07-1667. [DOI] [PubMed] [Google Scholar]
- 37.Watson AJ, et al. Diabetes connected health: a pilot study of a patient- and provider-shared glucose monitoring web application. J Diabetes Sci Technol. 2009;3(2):345–352. doi: 10.1177/193229680900300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Office, P.M.s . About Smart Nation. 2017. [Google Scholar]
- 39.Cheng Wei A. Use SkillsFuture Credits for classes, seniors urged, in The Straits Times. Singapore: Press Holdings The Sunday Times; 2016. [Google Scholar]
- 40.Lee RM. Tele-health for NTUC Income policyholders tested. In: Today: Mediacorp Press Ltd; 2016. http://www.Todayonline.com.
- 41.Hall JL, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff (Millwood) 2014;33(2):216–221. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 42.Maglogiannis I, et al. Enabling location privacy and medical data encryption in patient telemonitoring systems. IEEE Trans Inf Technol Biomed. 2009;13(6):946–954. doi: 10.1109/TITB.2008.2011155. [DOI] [PubMed] [Google Scholar]
- 43.Kwang, K. Singapore health system hit by ‘most serious breach of personal data’ in cyberattack; PM Lee's data targeted. Channel News Asia 2018 18 October 2018; Available from: https://www.channelnewsasia.com/news/singapore/singhealth-health-system-hit-serious-cyberattack-pm-lee-target-10548318.
- 44.Leyi S. Singapore HIV data leak shakes a vulnerable community. 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.