Sir,
The co-occurrence of neurofibromatosis type 1 (NF-1), Becker's nevus (BN), and nevus of Ota is expected to be very rare. No such cases were found in MEDLINE and EMBASE.
A 22-year-old woman, who had a 5-year history of underlying slowly growing painless soft masses involving her trunk, presented to us with an asymptomatic congenital brownish patch on her right cheek [Figure 1a and b]. There had been multiple cafe′-au-lait macules (CALMs) of different size all over the body [Figure 1c]) since her birth and bilateral axillary freckles appeared when she was 5 year old. The soft skin-colored nodules which were found initially during adolescence increased both in number and size gradually, and also the brownish patch of her right face became heterogeneous and presented excess hair partly. There was no history of musculoskeletal or neurological disorder. Systematic examinations (skeletal survey, ophthalmological and ENT evaluation, etc.) were done and no other defect was found. Both her mother and maternal grandfather suffered from NF-1.
Figure 1.

A 22-year-old female with NF-1, BN, and nevus of Ota. (a) CALMs (the black arrow), nevus of Ota (the red arrow) and excess hair of BN (the yellow arrow). (b) The left face. (c) Multiple CALMs and soft skin-colored nodules of different size on the back
Histological examination of one of the nodules on her abdomen revealed a tumor consisting of wavy cells arranged in a haphazard manner in fibrous and myxoid stroma [Figure 2] which indicated neurofibroma. So she was diagnosed as NF-1 associated with BN and nevus of Ota. We recommended Q-switched laser treatments, but she refused.
Figure 2.
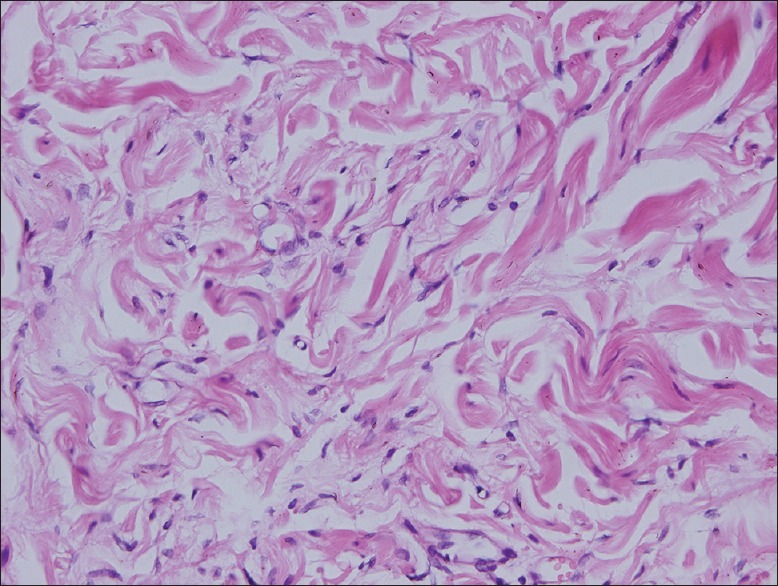
Tumor in the lower dermis consisted of wavy cells arranged in a haphazard manner in fibrous and myxoid stroma.(H and E, ×200)
NF-1, caused by mutation of the gene neurofibromin 1 (located at chromosome 17q11.2), is a multisystem disorder affecting around one in 3,500 individuals. Various kinds of hyperpigmentation skin disorders are related to NF-1, including CALMs, hyperpigmentation overlying plexiform neurofibromas and axillary freckles, nevus spilus, congenital giant melanocytic nevus, and segmental unilateral melanosis, etc.[1,2]
BN is a unilateral, hyperpigmented, hairy cutaneous disorder which is usually associated with various pigmented lesions, malignant melanoma, and leiomyoma too. It is characterized by lesions located over the upper trunk and displayes a corresponding regional relationship to the nevus.[3] Many cutaneous complications, including lymphangioma, intradermal or connective tissue nevi, and perforating folliculitis have been reported in association with this disorder.[3]
Nevus of Ota is a congenital or acquired pigmentary disease of the skin and mucous membranes, both of which are innervated by the trigeminal nerve. It is rare that NF-1, BN, and nevus of Ota occurred simultaneously[1,2,4] and the pathogenesis of hyperpigmentation related to NF-1 is still unclear.
There had been intimate relationships between the above three disorders from the perspective of developmental biology. In fact, NF-1 is a multisystem disorder caused by abnormal development of neural crest cells from which melanocytes and Schwann cell precursors (SCPs) are derived. In addition to contributing primarily to glia, SCPs adjacent to nerves were a cellular source of melanocytes and postnatal mature pigmented melanocytes in the cutis.[5] SCPs losing contact with the peripheral nerves during development acquired a melanoblast fate.[5] Consequently, BN and nevus of Ota might just be different manifestations of hamartoma arising from the differentiation of neural crest cells in NF-1. More studies are needed to focus on the coexistence of lesions especially in terms of malignancy in the future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kar S, Preetha K, Yadav N, Madke B, Gangane N. Becker's nevus with neurofibromatosis type 1. Ann Indian Acad Neurol. 2015;18:90–2. doi: 10.4103/0972-2327.144281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim SY, Kim MY, Kang H, Kim HO, Park YM. Becker's naevus in a patient with neurofibromatosis. J Eur Acad Detmatol Vencreol. 2008;22:394–5. doi: 10.1111/j.1468-3083.2007.02346.x. [DOI] [PubMed] [Google Scholar]
- 3.Danarti R, Konig A, Salhi A. Becker's nevus syndrome revisited. J Am Acad Dermatol. 2004;51:965–9. doi: 10.1016/j.jaad.2004.06.036. [DOI] [PubMed] [Google Scholar]
- 4.Connolly S, DiCaudo D, Speetzen L. A subtle nevus of Ota in a neurofibromatosis type 1 patient. J Am Acad Dermatol. 2011;64:AB87. [Google Scholar]
- 5.Adameyko I, Lallemend F. Glial versus melanocyte cell fate choice: Schwann cell precursors as a cellular origin of melanocytes. Cell Mol Life Sci. 2010;67:3037–55. doi: 10.1007/s00018-010-0390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


