Abstract
Almost no research exists on the relationship between religion/spirituality (R/S) and health in the U.S. South Asian population. Using data from the joint Study on Stress, Spirituality, and Health and Mediators of Atherosclerosis Among South Asians Living in America Study (MASALA), this paper examined associations between self-rated R/S and self-rated health, emotional functioning, trait anxiety, and trait anger in a community-based sample (n = 933) from the Chicago and San Francisco Bay areas. OLS regression was used to analyze categorical differences in levels of R/S and ordinal trends for R/S, adjusting for potential confounders. Being slightly or moderately R/S was associated with lower levels of self-rated health compared to being very R/S, and being slightly or moderately R/S was associated with higher levels of anxiety. In both cases, there was no significant difference between very R/S individuals and non-R/S individuals, suggesting a curvilinear relationship. Self-rated R/S was not significantly associated with emotional functioning or anger. In sum, high-R/S and low-R/S individuals had positive associations with self-rated health and anxiety compared to individuals with slight/moderate levels of R/S. It is important for clinicians and policy makers to recognize the role R/S can play in the health status of South Asians living in the United States.
Keywords: Immigrants, US South Asians, Religion, Spirituality, Mental Health, Depression, Self-Rated Health, Anxiety, Anger
Introduction
South Asians are among the fastest growing ethnic groups in the United States (U.S.), yet epidemiological research among this group is scant (Kanaya et al., 2013; United States Census Bureau, 2010). Given higher rates of social discrimination and physical health problems experienced by South Asians, mental and physical health in this population are important spheres of study (Nadimpalli, Dulin-Keita, Salas, Kanaya, & Kandula, 2016). Within the psychosocial domain, religiosity and spirituality (R/S) are understudied constructs that may affect health outcomes.
In the general U.S. population, R/S have often, though not always, been linked to longevity and better mental and physical health (Zimmer et al., 2016). Research on R/S and health among South Asians is sparse, with prior work indicating that: (a) religious identity and organizational belonging are important in lives of U.S. South Asians; (b) Hindus, Muslims, and Sikhs are more likely to be overweight/obese compared to non-affiliates (Bharmal, McCarthy, Gadgil, Kandula, & Kanaya, 2018; Kandula et al., 2018); and (c) religious activities are inversely related to negative affect among Asian Indians (Diwan, Jonnalagadda, & Balaswamy, 2004). Extant research has not considered other R/S variables and health outcomes for the U.S. South Asian population. We extended previous work by investigating relationships between self-rated R/S, self-rated health, emotional functioning, anxiety, and anger in a large, community-based sample. Based on prior research on the general U.S. population we expected positive associations between R/S and health (Koenig, King, & Carson, 2012).
Methods
The MASALA study initially recruited participants from 2010–2013 in the San Francisco and greater Chicago areas. Participants were 40–84 years old, of South Asian descent, free of cardiovascular disease, and fluent in English, Hindi, or Urdu. The original cohort (Exam 1, n=906) was re-interviewed between 2015–2018 (Exam 2) where 733 returning cohort members completed an ancillary study, the Study on Stress, Spirituality, and Health. A new 2017–2018 recruitment wave (Exam 1A) added 258 participants. In all, 989 participants completed the R/S questionnaire. Individuals with missing data on key independent or dependent variables were excluded, with the exception of income (3.3% missing) and marital status (3.4% missing), where median and modal imputation were used. In all, 933 of 989 MASALA participants were included in these analyses. Further information on the MASALA study is available elsewhere (Kanaya et al., 2013).
Self-rated health ranged from 1 (poor) to 5 (excellent). Three variables from the Mental Health Inventory index (MHI-3), a depressive symptoms screen, comprised an index of emotional functioning (range=0–15; α=0.65). Trait anxiety (range 10–40; α=0.70) and trait anger (range=10–40; α=0.69) came from the Spielberger scales and each consisted of ten variables (Spielberger, 1980).
Self-rated R/S was measured with a question that asked, ‘To what extent do you consider yourself a religious or spiritual person?’ We focused on categories of self-rated R/S (not at all, slightly, moderately, and very) and also assessed ordinal p-trends.
Control variables included religious tradition (Hindu, Muslim, Jain, Sikh, other [Christian, Buddhist, etc.], multiple religions, and no affiliation); alcoholic drinks per week; depression/anxiety medication; language at home (1= South Asian language only, to 5=English only); and percent of life in the U.S. Demographic indicators included marital status (1=married), home ownership, full-time employment, education (less than college, college, and graduate degree), income (< $75,000, $75,000-$149,999, and $150,000+), sex, and age.
We reported descriptive statistics and estimated linear regressions (robust standard errors) using PROC GENMOD in SAS 9.4.
Results
Study variable descriptive statistics are shown in Table 1. Table 2 reports full models for self-rated health, emotional functioning, anxiety, and anger. Self-rated R/S was associated with self-rated health: being slightly (p=.001) or moderately R/S (p=.007) was associated with lower levels of health compared to being very R/S. The overall trend was significant (p=.006), indicating that higher levels of self-rated health were associated with higher categories of R/S, but no significant difference was observed between the very R/S and the non-R/S, indicating a U-shaped curvilinear relationship (see Figure 1). An inverse U-shaped pattern was seen with anxiety, such that those rating themselves as moderately (p=.024) and slightly R/S (p=.047) reported greater anxiety relative to the very R/S while no significant difference was observed between those rating themselves as very R/S and non-R/S individuals. Self-rated R/S was not significantly associated with emotional functioning or anger.
Table 1.
Descriptive statistics for study variables (MASALA, N=933)
| Mean | SD | Range | |
|---|---|---|---|
| Dependent Variables | |||
| Self-rated health | 3.57 | .82 | 1–5 |
| Mental Health Inventory-3 | 11.37 | 2.33 | 1–15 |
| Anxiety | 15.86 | 4.25 | 10–36 |
| Anger | 15.87 | 3.69 | 10–37 |
| Independent Variables | |||
| Religious or spiritual person | |||
| Not at all | .05 | 0–1 | |
| Slightly | .18 | 0–1 | |
| Moderately | .56 | 0–1 | |
| Very | .21 | 0–1 | |
| Religious tradition | |||
| Hindu | .61 | 0–1 | |
| Muslim | .08 | 0–1 | |
| Jain | .05 | 0–1 | |
| Sikh | .06 | 0–1 | |
| Other religion | .04 | 0–1 | |
| Multiple religions | .07 | 0–1 | |
| No affiliation | .09 | 0–1 | |
| Alcohol consumption/week | |||
| None | .68 | 0–1 | |
| 1–2 | .16 | 0–1 | |
| 3–5 | .09 | 0–1 | |
| 6–9 | .04 | 0–1 | |
| 10+ | .03 | 0–1 | |
| Depression/anxiety meds | .04 | 0–1 | |
| Language at home | 3.08 | 1.21 | 1–5 |
| % life lived in US | 49.04 | 18.78 | 1.63–100 |
| Married | .92 | 0–1 | |
| Own home | .89 | 0–1 | |
| Full time employment | .57 | 0–1 | |
| Education | |||
| <Bachelor’s | .12 | 0–1 | |
| Bachelor’s | .30 | 0–1 | |
| Graduate | .58 | 0–1 | |
| Income | |||
| <$75,000 | .38 | 0–1 | |
| $75,000-$149,999 | .35 | 0–1 | |
| $150,000+ | .27 | 0–1 | |
| Female | .47 | 0–1 | |
| Age | 61.02 | 8.88 | 44–89 |
Table 2.
Regression of self-rated health, MHI-3, anxiety, and anger on religiosity (MASALA, N=933)
| Self-rated health | MHI-3 | Anxiety | Anger | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | b | (SE) | b | (SE) | b | (SE) | b | (SE) | ||||
| Religious or Spiritual Person | ||||||||||||
| Very (Ref) | - | - | - | - | - | - | - | - | ||||
| Moderately | −0.183 | (.068) | ** | −0.329 | (.194) | 0.678 | (.340) | * | 0.261 | (.326) | ||
| Slightly | −0.272 | (.085) | ** | −0.287 | (.247) | 1.031 | (.456) | * | 0.210 | (.399) | ||
| Not at all | −0.187 | (.139) | −0.568 | (.418) | 0.282 | (.828) | 0.525 | (.691) | ||||
| p-trend | ** | |||||||||||
| Religious Tradition | ||||||||||||
| Hindu (Ref) | - | - | - | - | - | - | - | - | ||||
| Islam | −0.091 | (.105) | −0.301 | (.313) | −0.075 | (.585) | 0.249 | (.555) | ||||
| Jain | 0.223 | (.124) | 0.084 | (.372) | −0.323 | (.648) | 0.260 | (.731) | ||||
| Sikh | −0.060 | (.102) | −0.117 | (.310) | −0.005 | (.539) | 0.072 | (.444) | ||||
| Other religion | −0.077 | (.158) | −0.956 | (.417) | * | 1.407 | (.731) | 1.080 | (.608) | |||
| Multiple religions | −0.026 | (.102) | −0.281 | (.258) | 0.319 | (.583) | −0.182 | (.406) | ||||
| None | 0.108 | (.101) | 0.087 | (.256) | -0.106 | (.488) | −0.844 | (.395) | * | |||
| Alcoholic drinks/week | ||||||||||||
| None (Ref) | - | - | - | - | - | - | - | - | ||||
| 1–2 | 0.003 | (.075) | −0.193 | (.210) | −0.078 | (.380) | 0.370 | (.345) | ||||
| 3–5 | −0.061 | (.101) | −0.519 | (.285) | −0.077 | (.534) | −0.110 | (.457) | ||||
| 6–9 | 0.126 | (.138) | −0.107 | (.350) | −0.249 | (.655) | 0.570 | (.521) | ||||
| 10+ | 0.064 | (.113) | 0.214 | (.355) | −0.676 | (.746) | 1.827 | (.826) | * | |||
| Depression/anxiety meds | −0.245 | (.135) | −1.653 | (.465) | *** | 3.195 | (.996) | ** | 1.673 | (.766) | * | |
| Language at home | 0.006 | (.027) | −0.126 | (.078) | 0.065 | (.142) | −0.045 | (.114) | ||||
| % life lived in US | 0.004 | (.002) | * | −0.005 | (.005) | 0.014 | (.008) | −0.007 | (.008) | |||
| Married | 0.161 | (.102) | 0.482 | (.277) | −1.374 | (.574) | * | 0.003 | (.519) | * | ||
| Own home | −0.031 | (.095) | 0.257 | (.292) | −0.452 | (.553) | 0.873 | (.444) | * | |||
| Full time employment | 0.230 | (.062) | *** | 0.705 | (.177) | *** | −0.557 | (.323) | *** | −0.444 | (.288) | |
| Education | ||||||||||||
| Graduate degree (Ref) | - | - | - | - | - | - | - | - | ||||
| Bachelor’s degree | −0.197 | (.062) | ** | 0.014 | (.172) | 0.888 | (.320) | ** | 0.289 | (.284) | ||
| <Bachelor’s degree | −0.364 | (.093) | *** | −0.243 | (.282) | 0.759 | (.477) | −0.029 | (.450) | |||
| Income | ||||||||||||
| <$75,000 (Ref) | - | - | - | - | - | - | - | - | ||||
| $75,000-$149,999 | −0.027 | (.070) | 0.065 | (.203) | −0.620 | (.369) | −0.286 | (.313) | ||||
| $150,000+ | −0.005 | (.079) | 0.246 | (.235) | −0.704 | (.416) | −0.376 | (.351) | ||||
| Female | −0.007 | (.062) | −0.273 | (.170) | 0.105 | (.326) | −0.257 | (.283) | ||||
| Age | −0.001 | (.004) | 0.039 | (.010) | *** | −0.060 | (.017) | *** | −0.067 | (.015) | *** | |
| Intercept | 3.455 | (.309) | *** | 9.100 | (.870) | *** | 19.919 | (1.534) | *** | 19.773 | (1.290) | *** |
p<.05
p<.01
p<.001
Figure 1. Predicted values of self-rated health and anxiety by degree of religiosity/spirituality.
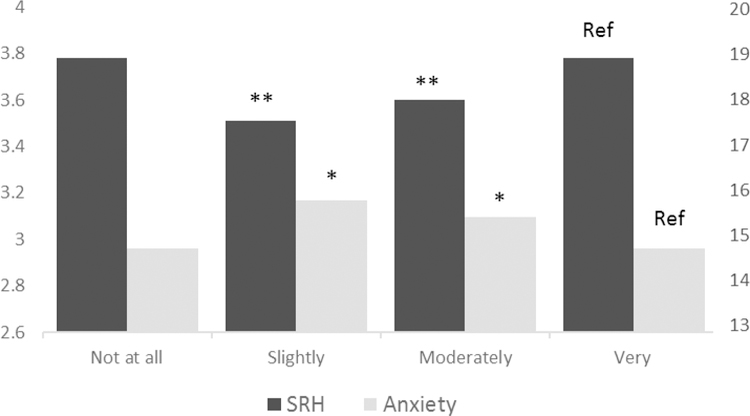
Notes: *p<.05, **p<.01
Based on Table 2. Significant covariates set to mean for predicted value calculations.
Discussion
We found that self-rated religiosity/spirituality had a curvilinear association with self-rated health and anxiety (a self-rated health trend was also significant). Those who reported being very R/S reported higher self-rated health and lower anxiety compared to somewhat and moderately R/S individuals, while non-R/S and very R/S individuals did not differ. There was no association with emotional functioning or anger. Several other cross-sectional studies have evaluated degree of religiosity or spirituality as a single item in non-South Asian populations. One study found that among U.S. Latinos, respondents who were 65+ and said religion was ‘not important at all’ were more likely to be anxious than those for whom religion was very important (Lerman et al., 2018); another found religiosity was associated with better self-rated health in Latin American and Caribbean elders (Reyes-Ortiz, Pelaez, Koenig, & Mulligan, 2007). Other research, using U.S. community and population-based samples, evaluated self-rated religiosity scaled with measures of religious participation and found mixed results when assessing anxiety and depressive symptoms (Deng, Lee, Lam, & Lee, 2016; Kasen, Wickramaratne, & Gameroff, 2014; Koenig et al., 2012).
In our data, persons indicating they were ‘not at all’ R/S did not significantly differ from those who were ‘very’ R/S. The curvilinear relationship between self-rated R/S and these outcomes resembled prior research that found a curvilinear relationship between other measures of religion (e.g., service attendance, belief in God) and mental well-being and depressive symptoms in U.S. community-based white and Black samples (Galen & Kloet, 2011; Taylor, Chatters, & Nguyen, 2013). However, to our knowledge, the current study is the first to show curvilinear associations for self-rated R/S on self-rated health and anxiety, and the first to examine these associations among U.S. South Asians.
An implication of these findings is that prior research measuring self-rated R/S as a continuous or binary variable possibly misspecified the relationship. Since previous research did not examine U.S. South Asians, it may also be that self-rated R/S operates differently among South Asians. One possibility is that persons who are somewhat religious, sometimes identified as R/S “liminals,” may experience stress due to their position on the periphery of faith communities—they are neither completely in nor out (Hastings, 2016; Lim, 2015; Mannheimer & Hill, 2014). Being slightly R/S may also suggest experiencing difficulty living out one’s faith in the U.S. context (e.g., dietary rules, religious practices, and religious holiday expectations). The highly R/S are likely to have a strong identity with which to reconcile their religiousness/spirituality with American society and see themselves as highly faithful. Conversely, secular South Asians may have a less pronounced faith dimension of life to reconcile with American society. While these explanations involve negative emotional effects of marginal R/S, reverse causation may also be an explanation. A pattern of resource mobilization may be operative whereby those experiencing poor health become somewhat R/S as they deal with health problems (Koenig et al., 2012).
Two main implications follow from our findings. First, high levels of self-rated R/S were linked to positive self-rated health among South Asians living in the U.S. It is important for clinicians and policy makers to recognize the role that R/S can play in positive health functioning. Second, this analysis has identified a vulnerable population—liminal South Asian religious adherents—a group potentially contributing a higher share of the illness burden among South Asians. Of the 690 liminal respondents in MASALA, 203 (29.4%) reported local religious congregation membership and 651 (94.3%) attended religious services at least once a month. Health programs might effectively collaborate with faith communities to help improve the health of this population.
Despite several strengths, our analysis also had several limitations. First, generalizability may be limited because MASALA targeted midlife and older South Asians in the Chicago and San Francisco areas, and high-income Asian Indians were overrepresented. Second, anxiety and anger measurement occurred concurrently with R/S variables among Exam 1A participants, but prior to R/S variables for Exam 1 participants, possibly resulting in a loss of power in analyses. Third, the data restricted this analysis to a cross-sectional design. Future longitudinal research is needed to better understand the relationship between self-rated R/S and health. Fourth, Asians with limited English proficiency may underreport self-rated health, though facility with English was controlled in all models (Kandula, Lauderdale, & Baker, 2007). Fifth, we used a measure that conflated religiosity and spirituality. The Study on Stress, Spirituality, and Health is now conducting analyses that will help differentiate between religion and spirituality, and these should be examined and utilized in the future.
Despite these limitations, this was the first examination of self-rated R/S and mental/self-rated health in a large community-based sample of U.S. South Asians. Our findings highlight the potential health vulnerability of religiously/spiritually liminal South Asians in America.
Acknowledgments
This analysis was supported by a grant from the John Templeton Foundation (grant #59607) and the Study on Stress, Spirituality, and Health. The MASALA Study was supported by NIH grants 1R01HL093009, 2R01HL093009, R01HL120725, UL1RR024131, UL1TR001872, and P30DK098722.
Abbreviations:
- R/S
Religiosity/spirituality
- U.S.
United States
- MASALA
Mediators of Atherosclerosis Among South Asians Living in America
Footnotes
Disclosures: The authors declare no conflicts of interest.
References
- Bharmal NH, McCarthy WJ, Gadgil MD, Kandula NR, & Kanaya AM (2018). The association of religious affiliation with overweight/obesity among South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. Journal of Religion and Health, 57(1), 33–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y, Lee K, Lam MHS, & Lee PH (2016). Understanding sociobehavioral mitigators of depressive symptoms among US young adults. Behavioral Medicine, 42(4), 217–226. [DOI] [PubMed] [Google Scholar]
- Diwan S, Jonnalagadda SS, & Balaswamy S (2004). Resources predicting positive and negative affect during the experience of stress: A study of older Asian Indian immigrants in the United States. The Gerontologist, 44(5), 605–614. [DOI] [PubMed] [Google Scholar]
- Galen LW, & Kloet JD (2011). Mental well-being in the religious and the non-religious: Evidence for a curvilinear relationship. Mental Health, Religion & Culture, 14(7), 673–689. [Google Scholar]
- Hastings OP (2016). Not a lonely crowd? Social connectedness, religious service attendance, and the spiritual but not religious. Social Science Research, 57, 63–79. [DOI] [PubMed] [Google Scholar]
- Kanaya AM, Kandula N, Herrington D, Budoff MJ, Hulley S, Vittinghoff E, & Liu K (2013). Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study: Objectives, Methods, and Cohort Description. Clinical Cardiology, 36(12), 713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula NR, Cooper AJ, Schneider JA, Fujimoto K, Kanaya AM, Van Horn L, … Siddique J (2018). Personal social networks and organizational affiliation of South Asians in the United States. BMC Public Health, 18(1), 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula NR, Lauderdale DS, & Baker DW (2007). Differences in self-reported health among Asians, Latinos, and non-Hispanic whites: the role of language and nativity. Annals of Epidemiology, 17(3), 191–198. [DOI] [PubMed] [Google Scholar]
- Kasen S, Wickramaratne P, & Gameroff MJ (2014). Religiosity and longitudinal change in psychosocial functioning in adult offspring of depressed parents at high risk for major depression. Depression and Anxiety, 31(1), 63–71. [DOI] [PubMed] [Google Scholar]
- Koenig HG, King DE, & Carson VB (2012). Handbook of religion and health (2nd ed.) New York, NY, US: Oxford University Press; (2012-25761-000). [Google Scholar]
- Lerman S, Jung M, Arredondo EM, Barnhart JM, Cai J, Castañeda SF, … Molina KM (2018). Religiosity prevalence and its association with depression and anxiety symptoms among Hispanic/Latino adults. PloS One, 13(2), e0185661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim C (2015). Religion and Subjective Well-Being Across Religious Traditions: Evidence from 1.3 Million Americans. Journal for the Scientific Study of Religion, 54(4), 684–701. [Google Scholar]
- Mannheimer AH, & Hill TD (2014). Deviating from Religious Norms and the Mental Health of Conservative Protestants. Journal of Religion and Health, 54(5), 1826–1838. [DOI] [PubMed] [Google Scholar]
- Nadimpalli SB, Dulin-Keita A, Salas C, Kanaya AM, & Kandula NR (2016). Associations Between Discrimination and Cardiovascular Health Among Asian Indians in the United States. Journal of Immigrant and Minority Health, 18(6), 1284–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes-Ortiz CA, Pelaez M, Koenig HG, & Mulligan T (2007). Religiosity and self-rated health among Latin American and Caribbean elders. The International Journal of Psychiatry in Medicine, 37(4), 425–443. [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1980). Preliminary Manual for the Sate-Trait Anger Scale (STAS) Palo Alto, CA: Consulting Psychology Press, Inc. [Google Scholar]
- Taylor RJ, Chatters LM, & Nguyen AW (2013). Religious Participation and DSM IV Major Depressive Disorder Among Black Caribbeans in the United States. Journal of Immigrant and Minority Health, 15(5), 903–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2010). Population groups summary file 1 Retrieved from https://www.census.gov/newsroom/releases/archives/2010_census/press-kits/summary-file-1.html
- Zimmer Z, Jagger C, Chiu C-T, Ofstedal MB, Rojo F, & Saito Y (2016). Spirituality, religiosity, aging and health in global perspective: A review. SSM-Population Health, 2, 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]


