Abstract
The built environment (BE) has been viewed as an important determinant of health. Numerous studies have linked BE exposure, captured using a variety of methods, to diet quality and to area prevalence of obesity, diabetes, and cardiovascular disease. First-generation studies defined neighborhood BE as the area around the home. Second-generation studies turned from home-centric to person-centric BE measures, capturing an individual’s movements in space and time. Those studies made effective uses of global positioning system (GPS) tracking devices and mobile phones, sometimes coupled with accelerometers and remote sensors. Activity space (AS) metrics explored travel paths, modes and destinations to assess BE exposure that was both person and context specific. However, as measures of the contextual exposome have become ever more fine-grained and increasingly complex, connections to long-term chronic diseases with complex etiologies, such as obesity, are in danger of being lost. Further, few studies on obesity and BE have included intermediate energy-balance behaviors, such as diet and physical activity, or explored the potential roles of social interactions or psychosocial pathways. Emerging survey-based applications that identify habitual destinations and associated travel patterns may become the third generation of tools to capture health-relevant BE exposures in the long term.
Keywords: exposome, built environment, home-centered, activity space, mobile technologies, KARMA, obesity, diabetes
1. Introduction
The built environment (BE) has been defined as the human-modified space in which people conduct their daily lives.(1) Measuring and quantifying human exposure to the neighborhood BE has been accomplished in a variety of ways.(2–11) Current studies on obesity and the BE owe much to the development of geographic information systems (GIS)(2, 12, 13) and the widespread use of global positioning system (GPS) devices.(14–18) Elements of the neighborhood BE tend to be categorized into the food environment and the physical activity (PA) environment.(19) The food environment has been conceptualized in terms of physical access to local supermarkets, groceries, fast food restaurants, or convenience stores.(19) The PA environment refers to area walkability, greenness, blue water, land use mix, and access to recreational facilities.(19)
Much of the work on health and the BE, conducted over the past two decades, has focused on neighborhood-level BE features and their likely impact on poor diets, lack of exercise, and higher obesity prevalence.(19–23) Most studies were home-centric, meaning that the density of or distances to destinations of interest were measured in relation to the individuals’ homes.(2, 13) Whereas aspects of the neighborhood PA environment did predict walking and lower body weights,(23–28) there was little to link the food environment to diet or diet-related health outcomes, such as obesity, diabetes, and cardiovascular disease (CVD). Physical access to supermarkets around the home was unrelated to diet quality or obesity rates.(2, 20, 29–41) There is preliminary evidence that activity space (AS) metrics are also unrelated to diet, obesity, or diabetes.(17, 18) Indeed, there is a growing understanding, with respect to the evaluation of the food environment in particular, that the BE only comprises a small slice of the larger context of the food environment.
Capturing the full contextual exposome, the totality of BE exposures at the individual level, has been described as fundamental to a better understanding of diets, obesity, and diabetes.(42–46) The promise of evaluations of the BE was to show a causal link between elements of the BE, or changes in the BE over time, and obesity or other health outcomes.(42–46) To that end, evaluations of BE exposures have sought to develop methods to more accurately and completely capture elements of the BE. Accordingly, such BE measurement tools have become increasingly more sophisticated using wearable GPS devices, often augmented with travel diaries, travel logs, Google street views, or other mobile technologies.(9, 14, 15, 18, 23, 26, 28, 44, 45, 47–56) These approaches allow the capture of near instantaneous measures of exposure to the BE not only around the home location but also at work, school, and along travel routes.(14, 15, 18, 44, 45, 47–51, 56) Mobile technologies have become increasingly atomized, allowing researchers to capture the minutiae of daily activities in time and space, sometimes at time resolutions of 10 seconds or less. By contrast, measures of diet quality, PA, and health have not followed suit. Standard methods of dietary intake assessment, such as food recalls, or food frequency questionnaires were generally not used.(2, 4–6, 11, 19, 57–59) Instead, the frequency of consuming “healthy” and “unhealthy” foods per day was one proxy for diet quality.(11) Health outcomes, when included in BE studies, were limited to body weight, with only a few studies examining diabetes or cardiovascular outcomes.(60–62)
The almost exclusive focus on quantifying BE exposure, together with cross sectional study designs, (19) has limited the ability to draw causal inferences regarding potential links between BE exposure and obesity.(45, 56) Furthermore, there seems to be a conceptual disconnect between current measures of BE exposure and the long-term trajectories of body weight. Fine-grained mobile technologies capturing detailed movement in space and time of at time resolutions of 10 seconds or less may prove highly useful in predicting risk factors for positive or negative behavior change when paired with spatiotemporally synced ecological momentary assessment (EMA).(63) However, as the measures of BE exposome become instantaneous and increasingly time-specific, links to chronic diseases with long onset periods and complex etiologies, such as obesity and diabetes, is in danger of being lost. Describing the evolving concept of BE exposure in relation to obesity is the topic of this review.
2. Evolving measures of BE exposure
2.1. Home as the center for BE exposures
Interest in health geography began in the early 1990s as researchers sought to establish evidence for geographic disparities in health outcomes.(12, 64) Concurrently, there was a renewed interest in social determinants of health as well as in the socioeconomic and demographic factors that influence where people live.(12, 13) The earliest investigations into the BE and health often relied on neighborhood-level socioeconomic measures such as indexes of socioeconomic position derived from the Census Bureau in the United States, the Townsend index, Carstairs index, and Index of Multiple Deprivation in the United Kingdom and the Socio-Economic Indexes for Areas in Australia, among others.(65–70) These indexes were often composite indicators for area-level poverty or wealth, based on socio-demographic data on poverty, employment, education, incomes, among other metrics.(64–72) In these studies, an individual’s neighborhood was often defined by some administrative boundary (e.g. census tracts in the United States) in which the individual’s home was located.(64, 71, 72) Often, actual addresses were geocoded to the centroid of the geographic administrative unit.
Early studies combined individual addresses with area-based, socio-demographic data. The density of fast food restaurants or supermarkets, and structural environment features, such as land use mix or availability of parks and trails were calculated per administrative unit.(7, 13, 19, 58, 73) However, care was needed in choosing the most relevant level of aggregation as both the scale and shape of the defined geographic units could influence the observed association introducing a form of statistical bias known as the modifiable areal unit problem.(74) The mismatch in geographic scales was resolved through hierarchical modeling.(12, 64, 75)
Later studies used pre-specified buffer zones, such as 400- or 800-meter buffers around an individual’s home using GIS software packages. (7, 13, 19, 58, 73) Here the issue was between the nearest supermarket and the actual destination supermarket. While the location of the nearest supermarket could be readily obtained from GIS data, the location of the destination supermarket could only be ascertained through a survey.(19, 36, 76–78) Those studies undermined the main premise of density metrics by showing that people did not shop at the nearest supermarket and did not eat at the nearest fast food restaurant.(19, 36, 76–78) Those findings were instrumental in shifting attention to AS captured in space and time.
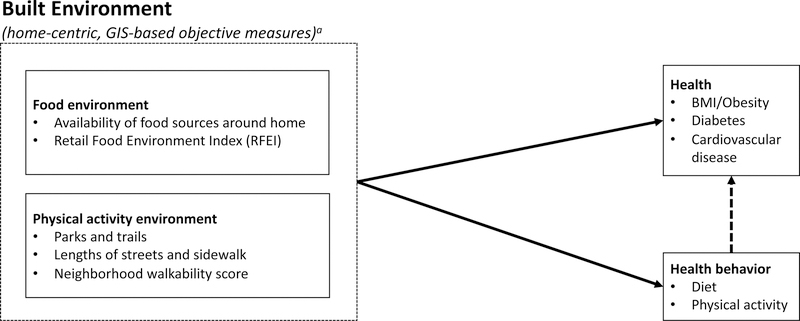
The postulated links between home BE and individual or neighborhood-level health are summarized in Figure 1. Elements of BE exposure were linked cross-sectionally to the prevalence of obesity, hypertension, diabetes, dyslipidemia, and metabolic syndrome.(2, 19, 34, 37, 61, 79, 80) With respect to the PA environment, studies have generally found that greater land use mix, higher residential density, higher walkability scores, and more green space were all associated with lower BMIs. Other measures of the BE such as road traffic and noise have been associated with a higher likelihood of having hypertension or dyslipidemia.(34) However, there was less evidence to link local PA resources, such as recreational facilities with body weight or hypertension.(34) Moreover the few examples of longitudinal evaluations of the PA environment and changes in body weight have produced null or inconsistent findings.(34, 81)
Figure 1.
Conceptual model of home-centric analyses linking the built environment to health
Note: Bulleted items are provided as examples and are not meant to represent an exhaustive list. Dashed arrow indicates the mediating role of health behaviors on the association between the built environment and health that was not directly evaluated by early studies.
a. Defined as fixed radius buffers around home address (e.g. 400 or 800-meter buffers)
The evidence on the association between the food environment and obesity was even less consistent.(2, 34) Studies suggested that a higher density of supermarkets or full-service restaurants was associated with lower body weight while higher densities of convenience stores or fast food restaurants were associated with higher body weight.(2, 20, 29–31, 34–41) However, other studies have not observed the same association between supermarket density and lower BMIs.(32, 33, 36, 39) Still more studies have been unable to replicate the findings between fast food restaurants or convenience stores and higher BMIs.(32, 39, 40)
Many early home-centric BE studies had several notable limitations with respect to their study design, measurement of the BE, and their consideration of BE-health pathways. First, the majority of early BE and health studies utilized a cross-sectional study design, which does not allow for a causal interpretation for observed associations between the BE and health.(81) Second, home-centric analyses can capture the BE features and resources within an individual’s neighborhood; however, proximity does not allow one to infer usage.(19, 36) For example, people do not shop for food in their immediate neighborhood but will instead travel great distances to the supermarket or fast food restaurant of choice.(36) Third, the choice of BE variables can influence the magnitude and direction of the observed association between BE and health – not all such metrics are predictive of health.(82) Relatedly, investigators should be more transparent regarding the variables and methods used to quantify the BE.(83) A recent systematic review examined 113 studies (encompassing 1937 tests of association) that sought to evaluate the relationship between the retail food environment and health.(83) The authors found that the reporting of methods was quite poor for more than half of the studies included in the review and that the wide diversity in methods led to an array of conclusions.(83) Fourth, some of the theoretical pathways through which features of the BE become internalized to influence health are not always readily apparent.(49) Additionally, as indicated in Figure 1, most early studies focused on the relationship between BE and health with few evaluating its effect on any energy balance behaviors. Few early studies had any actual measures of diet or physical activity and those that did usually evaluated these outcomes separately without consideration of the mediating role these energy balance behaviors might have on the BE-health relationship. Fifth, some studies do not adequately disentangle the physical attributes of the BE from the demographic and socioeconomic environments.(84) For example, studies have shown that the socioeconomic indicator, residential property values, is associated with both perceived proximity to neighbor PA environment features as well as health.(31, 36, 40, 41, 76, 84–86)
Some of these limitations can be overcome through the usage of person-centric analysis that incorporate individual-level behaviors (e.g. diet and physical activity), demographics (e.g. race and culture), socioeconomic status (e.g. property values and educational attainment), and psychosocial factors (e.g. attitudes and perceptions). Researchers should also move to directly examine the intermediary pathways through which BE features might operate to influence health via person-centric attributes. These methodological additions will aid researchers in understanding how individual-level characteristics influence a person’s exposure to BE elements in space and time and how the BE hinders or helps facilitate health-promoting behaviors.
2.2. Person as the center of BE exposure
Acknowledging that an individual’s home neighborhood cannot capture the full extent of health-related BE exposures, researchers turned to more advanced GPS technologies to track movements in space and time.(14, 15, 18, 44, 45, 47–51, 56) Cumulative mobility over a given time period is the basis for constructing AS areas.(18) These AS-derived areas are then supplemented with travel diary data to provide context for the GPS tracks, such as the reason for the trip, identified destination, and any participation in PA or foods consumed.(50)
Several different measures of AS have been used. The radius of gyration is defined as the average distance of a set of GPS points or tracks to the most frequented location.(87) The standard deviational ellipse of a set of GPS-recorded points is defined as the area which covers approximately 68 percent of GPS points and is centered on the average of the point pattern.(88) Convex hulls are defined as polygons that contain all GPS points or tracks and have no angles greater than 180 degrees.(89) Studies have also utilized a non-parametric method known as 2D kernel density estimation where a symmetrical kernel function is superimposed over a cluster of GPS points centered around its mean.(90) The set of overlapping kernel density functions are then superimposed to create a continuous density surface.(90) Other methods include mapping GPS points along street networks, buffered street networks, daily path areas, and more.(18)
The literature examining whether BE features captured in an individual’s AS are more predictive of health than home-centric defined features is relatively nascent.(14, 15, 18, 44, 45, 47–51, 56) In some cases AS-defined food and structural environment features have been shown to be more predictive of health behaviors than those captured in the home neighborhood. A study examining fast food outlet density and consumption of saturated fats, whole grains, as well as fruits and vegetables found that the density captured via the AS was positively associated with saturated fat intake and negatively associated with whole grains.(18) No such associations were observed using fast food outlet density captured in the 0.5 mile street network buffer.(18) However, two studies conducted in New York City produced counterintuitive results with one finding that higher noise density in AS-defined neighborhoods was associated with lower systolic and diastolic pressure and the other finding that home-centric food environments were more predictive of body mass index and blood pressure.(48, 49)
These disparate findings may be demonstrative of the utility of AS BE measures in various settings or highlight differences in the operationalization of the AS techniques. For example, Zenk (2011) found that AS defined by daily path areas were predictive of diet but standard deviational ellipse was not.(18) In addition, GPS monitoring and travel diaries place a heavy burden on participants and produce high volume data with thousands of data points. These data must then be cleaned and consolidated into useful metrics, for which there are many, with varying predictability based on setting and the health outcome(s) of interest. This varied predictability may also be due, in part, to the timing and duration of BE exposure covered by the AS measures. For example, a given GPS path may be predictive of physical activity or diet quality for that day or week but may be less predictive or long-term behavior or chronic diseases that are the result of the totality of behaviors over a protracted period of time (e.g. obesity, diabetes).
In order to overcome issues with the timing of BE exposures relative to the distal outcomes of interest, investigators have increasingly turned to exposure momentary assessment (EMA) to capture real-time, proximal dietary and physical activity decision-making as well as mood as they occur in a real-world setting.(63, 91–95) EMA is able to capture dynamic behaviors as they occur throughout the day and can allow investigators to observe the array of risk factors that precipitate a change in behavior that are spatiotemporally linked to the GPS-derived area measures.(63, 91–95)(63, 91–95) This method of data collection often uses short message services or applications via mobile devices and therefore can often be coupled with GPS and accelerometer data. EMA represents an exciting and rapidly growing field of exposure and outcome assessment which is readily applicable to the study of BE and health and complements new and evolving GPS-derived metrics.(63, 91–95)
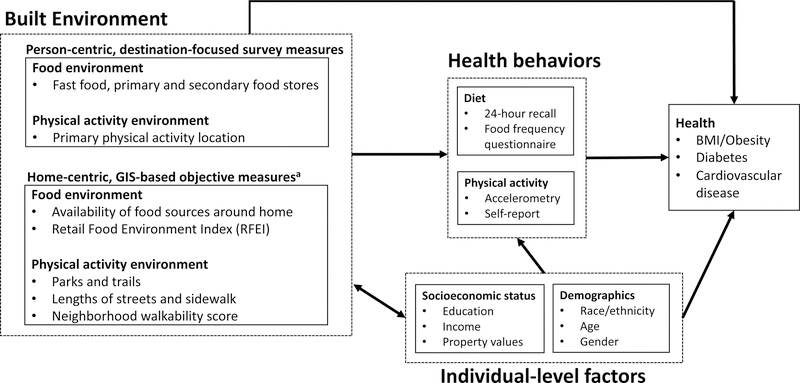
2.3. Energy balance pathways
Any observable relationship between the BE and obesity should first, logically, have some observable effect on upstream energy balance behaviors, such as diet and physical activity (Figure 2).(11) Several studies have examined the role that the PA environment plays on physical activity and use of active modes of transport to commute to work or school. One feature of the PA environment that has been consistently linked to increased PA, specifically, walking, is neighborhood walkability,(23–26) Walkability is typically defined by land use mix, residential density, retail floor area density, and street connectivity.(27, 28) With respect to the food environment, several studies have examined whether the composition of healthy and unhealthy food outlets, often referred to as the Retail Food Environment Index, in the home neighborhood was associated with diet quality. Several studies have observed that proximity to supermarkets, grocery stores, and sit-down restaurants was associated with high diet quality,(37, 38, 96–98) while proximity to convenience stores and fast food restaurants have been associated with poor quality diets.(2, 20, 99) However, as observed with obesity and diabetes, the relationship between the home food environment and diet quality has not always been consistent.(2)
Figure 2.
Conceptual model of SOS home- and person-centric analyses linking the built environment to health
Note: Bulleted items are provided as examples and are not meant to represent an exhaustive list.
a. Defined as fixed radius buffers around home address (e.g. 400 or 800-meter buffers)
While there are several studies that have evaluated the effect of BE exposures on health and health behavior separately, there are far fewer that have formally evaluated the potential mediating role of health behaviors in the BE-health relationship. International research examining the interplay amongst the BE, health behaviors, and health provide evidence that PA mediates the effect of the PA environment on health.(100–103) A study of Belgian adults examined the potential mediating effect of accelerometer-assessed PA and sedentary behavior on the relationship between walkability and adiposity.(100) They found that moderate-to-vigorous PA as well as walking and cycling for transport significantly mediated the relationship between walkability and both BMI as well as waist-to-height ratio; however, no such mediating relationship was found for sedentary behaviors.(100) A study of New Zealand adults found that PA and sedentary behaviors played a significant mediating role of the effect of street connectivity and neighborhood destination accessibility on BMI and waist circumference.(101) A third study found that light and moderate-to-vigorous PA mediated the relationship between elements of the urban walking environment and BMI among a group Japanese adults age 65–84 years.(102) With respect to cardio-metabolic outcomes, a study using a representative sample of adults in South Australia found that the effect of walkability and road network buffers on glycosylated hemoglobin (HbA1c) was significantly mediated by self-reported PA levels.(103) However, it is worth noting that since the walkability index has been derived from elements in the environment that relate to walking, it should be expected that, by design, walking and walkability will be correlated. Therefore, the observed associations between walkability and PA levels may represent a form of autocorrelation. To our knowledge there are few, if any, examples of formal mediational analyses of PA in the relationship between BE and obesity, diabetes, or metabolic syndrome in United States-based, adult populations. Moreover, there are no equivalent studies that have examined the mediating role of diet, food shopping, or cooking behaviors on the BE and health relationship either in the United States or internationally. However, such studies evaluating mediational effects of dietary behaviors may not prove fruitful if BE exposure assessment relies on home-centric measures alone.
Early evaluations of the neighborhood BE assumed that, much like the PA environment, the health-relevant food environment comprised the food stores and restaurants around the home.(2, 4, 8, 13, 19, 57) Yet, the current body of evidence evaluating the food environment and health shows that this was an overly simplistic model.(2, 4, 8, 13, 19, 36, 57) It is now understood that the built elements of the food environment only comprise a small slice of the wider context of the food environment. Other factors at the individual-level (e.g. socioeconomic status, cultural and religious norms, perceptions and attitudes), store and restaurant-level, (e.g. affordability, availability, convenience, and marketing), and even local, state, and federal levels (e.g. social, income, and food policies) are more predictive of where individuals shop.(19, 36, 104–108) Many studies fail to account for the diet cost at various food outlets as well as differences in individual purchasing power. Moreover, home-centric measurement fails to capture meals that may be consumed in the vicinity of the workplace or school leading to incomplete assessment of the food environment to which an individual is exposed. Therefore, more thorough investigations of the relationship between the food environment and health should include diet and diet cost in their analyses as well as extend capture of food environment exposures to wear people live, work, and spend their leisure time.
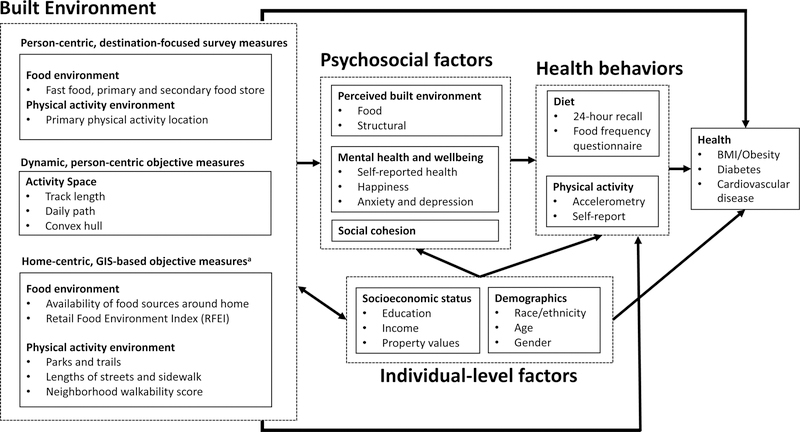
2.4. Psychosocial pathways
Individual-level psychosocial factors such as perceptions (e.g. neighborhood attractiveness or availability of fresh produce), attitudes, social cohesion, as well as self-rated health and wellness can aid researchers in elucidating how individuals interact with and internalize their environment (Figure 3).(2, 109–115) Indeed where objective, GIS-based assessments of the BE have failed to produce consistently significant associations with health outcomes, such as obesity and diabetes, perceived metrics such as the availability of supermarkets have been shown to be far more predictive.(2) Collection of survey-based psychosocial measures may also assist in accurately capturing individual-level utilization of BE resources better than objective, GIS-based measures alone.(2, 109)
Figure 3.
Conceptual model of home- and person-centric (dynamic and destination-focused) analyses linking the built environment to psychosocial factors and health
Note: Bulleted items are provided as examples and are not meant to represent an exhaustive list.
a. Defined as fixed radius buffers around home address (e.g. 400 or 800-meter buffers)
Individual perceptions of the built environment have been shown to be correlated with objective measures of the BE(109, 116) as well as measures of socioeconomic status(117) and are predictive of health.(2, 109–115, 118) One study found that a four-item food environment assessment tool, which measured an individual’s perceptions of healthy food access, matched very closely with actual access in a low-income population.(116) However, the degree to which perceived and objective measures of the BE match up may vary by population in a systematic way.(109) Caspi and colleagues found that mismatch between perceived and objective BE measures was high but also observed that perceived supermarket access was more predictive of fruit and vegetable consumption than objective measures such as supermarket proximity.(109) A similar relationship has been observed with perceived and objective measures of the structural environment and levels of PA with the perceived presence of facilities, sidewalks, shops, area traffic each showing a positive association with level of PA.(113) Likewise other self-rated measures of BE, such as attractiveness, noise, and crime, were associated individual property values, which in turn correlated highly to neighborhoods with a high prevalence of obesity.(117)
Positive attitudes, self-efficacy, and social supports have been demonstrated to be positively associated healthy eating and higher levels of PA.(55, 77, 119–126) One study found that participants who strongly agreed that a healthy diet was important to them had a healthier diet overall compared to those participants who disagreed or strongly disagreed.(127) This attitude-diet relationship was found to be present regardless of the average cost of a healthy diet at the supermarket.(127) Studies examining psychosocial factors predictive of PA levels have found that self-efficacy and social supports are associated with greater levels of activity.(55, 119, 125, 126) Interestingly, studies that have jointly examined both perceived or objective measures of the BE and psychosocial factors have found a synergistic relationship between the BE, self-efficacy, and social supports.(55, 119, 125, 126) Those individuals possessing positive psychosocial characteristics and living in environments conducive to physical activity showed the greatest levels of PA or participation in active transport to work or school.(55, 119, 125, 126)
While psychological factors have shown to be related to both BE features as well as health, more work is needed to understand how the perceived environment and positive attitudes mediate the effects of the BE on health. Furthermore, there is limited evidence evaluating the role that mental health and wellbeing play in mediating the effects of the BE on health. One study found that the presence of depressive symptoms changed both the strength and the direction of the association between the perceived structural environment and PA levels.(128) To our knowledge there are no studies that examine the how effect of the food environment on diet quality and health outcomes is mediated by individual perceptions, attitudes, and mental health. Such studies should use dynamic, person-centric measures of the food environment to capture the full extent of exposure at home, work, school, and during commutes as well additional contextual factors such as prices, policies, marketing, and cultural and religious norms.
EMA, now viewed as a new and promising behavioral outcome of BE exposure,(63) is concordant in space and time with spatiotemporally-driven GPS measures of the BE exposome such as AS metrics. EMA has helped to shift attention from dietary quality or body weight to momentary, place-driven impulses, behavioral triggers, or environmental cues. These triggers may be predictive of longer-term health outcomes, such as obesity and diabetes. While the EMA may provide answers to the relationship between BE and risk factors for behavior change, such methods may have less utility in providing insights into how the neighborhood BE or larger BE exposome influence chronic diseases with protracted onset periods. Such long-term chronic diseases have etiologies that are highly complex and result from the accumulation of exposures to the BE as well as socioeconomic status, behavior, and more.(129)
2.5. Residential selection bias
Underpinning many residential BE exposures are the socioeconomic and sociodemographic factors which determine where individuals are able to live and as well as whether and where they are able to relocate.(19, 74, 130) Historical patterns of residential segregation, a prominent manifestation of structural racism, have dramatically shaped the human geography of much of the world and have been linked to health disparities.(131, 132) Relatedly, inequities in educational and work opportunities as well as intergenerational accumulation of wealth also play a key role in where individuals locate as well as how they interact with the BE.(133) Two individuals may occupy the same physical residential space or AS but experience very different social or economic environments.(133) Therefore, careful confounding control is needed as there are a number of socioeconomic and sociodemographic factors that are associated with both where a person lives and their risk of obesity, which, in turn, may vary based on the shape and scale of the define area.(74, 130) Interestingly, the incongruence in area-level socioeconomic advantage or disadvantage between residential BE versus AS BE and its relationship to health is currently an active area of research that, to date, has produced mixed findings.(91, 134)
It is also worth noting that much of the extant research into the relationship between the BE and health has been conducted in the United States and other high income countries.(135) The investigation into whether such findings are applicable to low and middle income countries are still in their infancy.(135) As with high income countries, care must be taken in such evaluations to consider the larger social and political context behind where people live. Moreover, the development of new technologies to assess the BE should be flexible and adaptive enough for use in both settings.
3. Obesity and the BE: The third-generation studies
The shift from home-centric BE exposure measurement to a more flexible, person-centered approach was intended to provide better information on the extent of health-relevant BE exposures throughout the day. These GPS-driven approaches have demonstrated great utility in predicting PA, such as walking, as well as use of active transport.(23–26, 37, 38, 96–98) Moreover, the evaluation of GPS data and metrics continues to evolve and show great promise in predicting risk factors for behavior change when combined with spatiotemporally-linked outcome assessment methods such as EMA.(63) However, wearable GPS monitoring devices tend to produce big data that can be computationally intensive and difficult to operationalize into metrics predictive of health based on the outcome of interest, population, and setting. Such computational challenges are represented in Aiello and colleagues (2019) who evaluated the relationship between food purchase behavior and health outcomes using 1.6 billion geocoded food purchases.(136) Moreover, the cost of GPS monitoring is such that it cannot be readily scaled up to large longitudinal cohort studies. There is therefore a need for more efficient tools to assess the context of habitual interactions with the BE.(45, 56)
It is also worth considering the potential privacy concerns which arise with the use of continuous GPS monitoring techniques.(137) While there are several methods researchers have implemented to mask the exact location of their participants to prevent privacy breaches, each method comes with its own strengths and weaknesses as well as different associated reidentification risks.(137) There is currently no universally accepted geographic masking method for confidential locations.(137)
Chaix (2012) described the concept of “contextual expology” as a subdiscipline of BE research focusing on the spatiotemporal configuration of BE exposures and accurate mapping of spatial behavior.(56) With this in mind, the Residential Environment and CORonary Heart Disease (RECORD) study developed the Visualization and Evaluation of Route Itineraries, Travel Destinations, and Activity Spaces (VERITAS) as an interactive web mapping application that geolocates participant’s self-reported habitual destinations.(56) VERITAS has proven useful in identifying highly frequented locations which can then be operationalized in several ways such as creating convex AS polygons, buffered areas, or travel paths using street networks.(56) In addition, a validation study of VERITAS against continuous GPS monitoring data found that GPS data fell within 500 meters of a VERTIAS-identified location for approximately 86% of the RECORD study population.(45) While highly promising as an BE exposure assessment tool, to date, no study has used VERITAS-derived BE measures to examine health or health behavior. In addition, the VERITAS questionnaire does not ask participants to provide the path they travel to go to and from their key destinations.(45, 56)
A new tool, the Knowledge-based Activity Reporting and Mapping Application or KARMA, is a dynamic, cloud-based, interactive application which addresses some of the gaps identified in VERITAS. KARMA, like VERITAS, allows participants to self-report key destinations that they frequent most using an interactive, web-based tool with the in-person help of a trained interviewer. However, unlike VERITAS, KARMA uses the Google application programming interface (API) to then map the most logical travel path, based on travel mode, which is then able to be modified by the participant if necessary. This allows KARMA to evaluate flexible AS, buffered dwell points, as well as travel paths. In addition, KARMA allows participants to input the timing of travel and activities throughout a given day allowing researching to examine the duration of time spent at each dwell point or in transit.
KARMA was developed within the Seattle Obesity Study III (SOS III), which seeks to critically examine the interplay between the BE, diet quality, PA, and diet-related health outcomes. As such SOS collects both self-reported and objective measures of diet quality, PA, and BMI. Expanding beyond more traditional survey-based evaluations of diet, which usually only measure adequate fruit and vegetable intake, SOS III is able to collect detailed data on habitual dietary patterns using food frequencies questionnaires and assign objective diet quality scores using the Healthy Eating Index.(11, 138)PA was measured at baseline via Actigraph accelerometer (ActiGraph™ , Pensacola, CA) devices as well as was self-reported, allowing us to correct these self-reported metrics longitudinally.(139) Moreover, SOS III also collects information on an array of demographic, socioeconomic, and psychosocial factors (Figure 3). This puts the SOS III study in the unique position to address some of the existing gaps in the BE literature related to the mediating roles of health behaviors and psychosocial factors in the BE-health relationship.
4. Conclusion
As our understanding of how individuals interact with the BE, and how these interactions are internalized, becomes increasingly complex so too must our conceptual models of obesity and the BE. Studies examining the effects of the BE on obesity and diabetes must consider how these effects are enhanced or mitigated via health behaviors, socioeconomic status, and psychosocial factors. The assessment of the BE must expand beyond the immediate home environment to encompass a variety of other locations and destinations of travel. Streamlined, efficient, destination-focused, web-based tools such as VERITAS and KARMA may become the next generation of tools to assess habitual BE exposure in long-term studies of weight trajectories, obesity and diabetes.
Study Importance Questions.
What is already known about this subject?
Previous reviews of the built environment have provided comprehensive summaries of the state of knowledge regarding the relationship between the physical environment and food environment on their impact on poor diets, lack of exercise, and higher obesity prevalence.
What are the new findings in your manuscript?
The present review provides an in-depth examination of the evolution of our conceptual understanding of the built environment and obesity, a call for a closer examination of the role of energy balance pathways, technological advances in the capture of built environment exposures, and suggestions for promising new avenues of research.
Acknowledgments
Funding: The study was funded by NIH grants R01 DK 114196-01 and R01 DK076608-10.
Adam Drewnowski has received grants, honoraria, and consulting fees from numerous food, beverage, and ingredient companies and from other commercial and nonprofit entities with an interest in diet quality and nutrient density of foods. The University of Washington receives research funding from public and private sectors.
Abbreviations:
- API
application programming interface
- AS
activity space
- BE
built environment
- BMI
body mass index
- CVD
cardiovascular disease
- GPS
global positioning system
- PA
physical activity
- RECORD
Residential Environment and Coronary Heart Disease
- SOS III
Seattle Obesity Study III
- VERITAS
Visualization and Evaluation of Route Itineraries, Travel Destinations, and Activity Spaces
- KARMA
Knowledge-based Activity Reporting and Mapping Application
- RFE
retail food environment
Footnotes
Disclosure: All other authors have no conflicts of interest to declare.
5. References
- 1.Srinivasan S, O’Fallon LR, Dearry A. Creating healthy communities, healthy homes, healthy people: initiating a research agenda on the built environment and public health. Am J Public Health 2003;93:1446–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health Place 2012;18:1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: A systematic review of the epidemiologic evidence. Health Place 2010;16:175–190. [DOI] [PubMed] [Google Scholar]
- 4.Kelly B, Flood VM, Yeatman H. Measuring local food environments: An overview of available methods and measures. Heal Place 2011;17:1284–1293. [DOI] [PubMed] [Google Scholar]
- 5.Kirkpatrick S, Reedy J, Butler E, et al. Dietary Assessment in Food Environment Research: A Systematic Review. Am J Prev Med 2014;46:94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glanz K, Johnson L, Yaroch AL, Phillips M, Ayala GX, Davis EL. Measures of Retail Food Store Environments and Sales: Review and Implications for Healthy Eating Initiatives. J Nutr Educ Behav 2016;48:280–288.e1. [DOI] [PubMed] [Google Scholar]
- 7.Glanz K, Handy SL, Henderson KK, Slater SJ, Davis EL, Powell LM. Built environment assessment: Multidisciplinary perspectives. SSM - Popul Heal 2016;2:24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lytle LA, Sokol RL. Measures of the food environment: A systematic review of the field, 2007–2015. Health Place 2017;44:18–34. [DOI] [PubMed] [Google Scholar]
- 9.McKinnon RA, Reedy J, Handy SL, Brown RB. Measuring the Food and Physical Activity Environments: Shaping the Research Agenda. Am J Prev Med 2009;36:S81–S85. [DOI] [PubMed] [Google Scholar]
- 10.Berke EM, Vernez-Moudon A. Built environment change: a framework to support health-enhancing behaviour through environmental policy and health research. J Epidemiol Community Health 2014;68:586–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drewnowski A, Aggarwal A, Tang W, et al. Obesity, diet quality, physical activity, and the built environment: the need for behavioral pathways. BMC Public Health 2016;16:1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diez Roux AV Investigating neighborhood and area effects on health. Am J Public Health 2001;91:1783–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glanz K Measuring Food Environments: A Historical Perspective. Am J Prev Med 2009;36:S93–S98. [DOI] [PubMed] [Google Scholar]
- 14.Zenk SN, Kraft AN, Jones KK, Matthews SA. Convergent validity of an activity-space survey for use in health research. Health Place 2019;56:19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zenk SN, Matthews SA, Kraft AN, Jones KK. How many days of global positioning system (GPS) monitoring do you need to measure activity space environments in health research? Health Place 2018;51:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kestens Y, Lebel A, Chaix B, et al. Association between Activity Space Exposure to Food Establishments and Individual Risk of Overweight Miranda JJ (ed.). PLoS One 2012;7:e41418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drewnowski A, Aggarwal A, Rose CM, Gupta S, Delaney JA, Hurvitz PM. Activity space metrics not associated with sociodemographic variables, diet or health outcomes in the Seattle Obesity Study II. Spat Spatiotemporal Epidemiol 2019;30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zenk SN, Schulz AJ, Matthews SA, et al. Activity space environment and dietary and physical activity behaviors: A pilot study. Heal Place 2011;17:1150–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Drewnowski A, Arterburn D, Zane J, et al. The Moving to Health (M2H) approach to natural experiment research: A paradigm shift for studies on built environment and health. SSM - Popul Heal 2019;7:100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laska MN, Hearst MO, Forsyth A, Pasch KE, Lytle L. Neighbourhood food environments: are they associated with adolescent dietary intake, food purchases and weight status? Public Health Nutr 2010;13:1757–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR. Associations of the local food environment with diet quality - A comparison of assessments based on surveys and geographic information systems. Am J Epidemiol 2008;167:917–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health 2002;92:1761–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovasi GS, Moudon AV, Pearson AL, et al. Using built environment characteristics to predict walking for exercise. Int J Health Geogr 2008;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duncan GE, Cash SW, Horn EE, Turkheimer E. Quasi-causal associations of physical activity and neighborhood walkability with body mass index: A twin study. Prev Med (Baltim) 2015;70:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank LD, Sallis JF, Conway TL, Chapman JE, Saelens BE, Bachman W. Many Pathways from Land Use to Health: Associations between Neighborhood Walkability and Active Transportation, Body Mass Index, and Air Quality. J Am Plan Assoc 2006;72:75–87. [Google Scholar]
- 26.Moudon AV, Lee C, Cheadle AD, et al. Attributes of Environments Supporting Walking. Am J Heal Promot 2007;21:448–459. [DOI] [PubMed] [Google Scholar]
- 27.Moudon AV, Lee C, Cheadle AD, et al. Operational Definitions of Walkable Neighborhood: Theoretical and Empirical Insights. J Phys Act Heal 2006;3:S99–S117. [DOI] [PubMed] [Google Scholar]
- 28.Frank LD, Sallis JF, Saelens BE, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med 2010;44:924–33. [DOI] [PubMed] [Google Scholar]
- 29.Fraser LK, Edwards KL. The association between the geography of fast food outlets and childhood obesity rates in Leeds, UK. Health Place 2010;16:1124–1128. [DOI] [PubMed] [Google Scholar]
- 30.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: The Atherosclerosis Risk in Communities Study. Am J Prev Med 2006;30:333–339. [DOI] [PubMed] [Google Scholar]
- 31.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Heal Place 2009;15:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hattori A, An R, Sturm R. Neighborhood Food Outlets, Diet, and Obesity Among California Adults, 2007 and 2009. Prev Chronic Dis 2013;10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gase LN, DeFosset AR, Smith LV, Kuo T. The Association between Self-Reported Grocery Store Access, Fruit and Vegetable Intake, Sugar-Sweetened Beverage Consumption, and Obesity in a Racially Diverse, Low-Income Population. Front Public Heal 2014;2:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev 2011;12:217–230. [DOI] [PubMed] [Google Scholar]
- 35.Laska MN, Borradaile KE, Tester J, Foster GD, Gittelsohn J. Healthy food availability in small urban food stores: A comparison of four US cities. Public Health Nutr 2010;13:1031–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV Obesity and supermarket access: Proximity or price? Am J Public Health 2012;102:e74–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Black JL, Macinko J, Dixon LB, Fryer GE. Neighborhoods and obesity in New York City. Heal Place 2010;16:489–499. [DOI] [PubMed] [Google Scholar]
- 38.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J Urban Heal 2010;87:771–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fiechtner L, Block J, Duncan DT, et al. Proximity to supermarkets associated with higher body mass index among overweight and obese preschool-age children. Prev Med (Baltim) 2013;56:218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med (Baltim) 2004;38:57–63. [DOI] [PubMed] [Google Scholar]
- 41.Leung CW, Laraia BA, Kelly M, et al. The Influence of Neighborhood Food Stores on Change in Young Girls’ Body Mass Index. Am J Prev Med 2011;41:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Loh M, Sarigiannis D, Gotti A, et al. How Sensors Might Help Define the External Exposome. Int J Environ Res Public Health 2017;14:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chaix B Mobile Sensing in Environmental Health and Neighborhood Research. Annu Rev Public Health 2018;39:367–384. [DOI] [PubMed] [Google Scholar]
- 44.Perchoux C, Kestens Y, Brondeel R, Chaix B. Accounting for the daily locations visited in the study of the built environment correlates of recreational walking (the RECORD Cohort Study). Prev Med (Baltim) 2015;81:142–149. [DOI] [PubMed] [Google Scholar]
- 45.Kestens Y, Thierry B, Shareck M, Steinmetz-Wood M, Chaix B. Integrating activity spaces in health research: Comparing the VERITAS activity space questionnaire with 7-day GPS tracking and prompted recall. Spat Spatiotemporal Epidemiol 2018;25:1–9. [DOI] [PubMed] [Google Scholar]
- 46.Hajna S, Kestens Y, Daskalopoulou SS, et al. Neighbourhood walkability and home neighbourhood-based physical activity: an observational study of adults with type 2 diabetes. BMC Public Health 2016;16:957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perchoux C, Chaix B, Brondeel R, Kestens Y. Residential buffer, perceived neighborhood, and individual activity space: New refinements in the definition of exposure areas – The RECORD Cohort Study. Health Place 2016;40:116–122. [DOI] [PubMed] [Google Scholar]
- 48.Tamura K, Elbel B, Athens JK, et al. Assessments of residential and global positioning system activity space for food environments, body mass index and blood pressure among low-income housing residents in New York City. Geospat Health 2018;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tamura K, Elbel B, Chaix B, et al. Residential and GPS-Defined Activity Space Neighborhood Noise Complaints, Body Mass Index and Blood Pressure Among Low-Income Housing Residents in New York City. J Community Health 2017;42:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hurvitz PM, Moudon AV, Kang B, Saelens BE, Duncan GE. Emerging Technologies for Assessing Physical Activity Behaviors in Space and Time. Front Public Heal 2014;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu L, Yang B, Jing P. Travel Mode Detection Based on GPS Raw Data Collected by Smartphones: A Systematic Review of the Existing Methodologies. Information 2016;7:67. [Google Scholar]
- 52.Ulijaszek S Physical activity and the human body in the (increasingly smart) built environment. Obes Rev 2018;19:84–93. [DOI] [PubMed] [Google Scholar]
- 53.Ding D, Gebel K. Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health Place 2012;18:100–105. [DOI] [PubMed] [Google Scholar]
- 54.Koohsari MJ, Sugiyama T, Sahlqvist S, Mavoa S, Hadgraft N, Owen N. Neighborhood environmental attributes and adults’ sedentary behaviors: Review and research agenda. Prev Med (Baltim) 2015;77:141–149. [DOI] [PubMed] [Google Scholar]
- 55.Bauman AE, Reis Rodrigo S, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380:258–271. [DOI] [PubMed] [Google Scholar]
- 56.Chaix B, Kestens Y, Perchoux C, Karusisi N, Merlo J, Labadi K. An interactive mapping tool to assess individual mobility patterns in neighborhood studies. Am J Prev Med 2012;43:440–450. [DOI] [PubMed] [Google Scholar]
- 57.Ohri-Vachaspati P, Leviton LC. Measuring Food Environments: A Guide to Available Instruments. Am J Heal Promot 2010;24:410–426. [DOI] [PubMed] [Google Scholar]
- 58.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The Built Environment and Obesity. Epidemiol Rev 2007;29:129–143. [DOI] [PubMed] [Google Scholar]
- 59.Charreire H, Casey R, Salze P, et al. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutr 2010;13:1773–1785. [DOI] [PubMed] [Google Scholar]
- 60.Borrell LN, Diez Roux AV, Rose K, Catellier D, Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol 2004;33:398–407. [DOI] [PubMed] [Google Scholar]
- 61.Malambo P, Kengne AP, De Villiers A, Lambert EV, Puoane T. Built Environment, Selected Risk Factors and Major Cardiovascular Disease Outcomes: A Systematic Review Pizzi C (ed.). PLoS One 2016;11:e0166846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Anon. Environment, Obesity, and Cardiovascular Disease Risk in Low-Income Women. Am J Prev Med 2006;30:327–332.e1. [DOI] [PubMed] [Google Scholar]
- 63.Burke LE, Shiffman S, Music E, et al. Ecological Momentary Assessment in Behavioral Research: Addressing Technological and Human Participant Challenges. J Med Internet Res 2017;19:e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Diez Roux AV, Mair C Neighborhoods and health. Ann N Y Acad Sci 2010;1186:125–145. [DOI] [PubMed] [Google Scholar]
- 65.Krieger N, Zierler S, Hogan J, et al. Geocoding and measurement of neighborhood socioeconomic position: a US perspective. In: Kawachi I, Berkman LF (eds.). Neighbors and health. New York, New York: Oxford University Press, 2003, pp 147–178. [Google Scholar]
- 66.Krieger N, Waterman PD, Chen JT, Soobader M-J, Subramanian S. Monitoring Socioeconomic Inequalities in Sexually Transmitted Infections, Tuberculosis, and Violence: Geocoding and Choice of Area-Based Socioeconomic Measures—The Public Health Disparities Geocoding Project (US). Public Health Rep 2003;118:240–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health 2006;96:325–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Carstairs V Deprivation indices: their interpretation and use in relation to health. J Epidemiol Community Health 1995;49 Suppl 2:S3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the North. London: Croom Helm; 1988. [Google Scholar]
- 70.Australian Bureau of Statistics. Socio-economic Indexes for Areas. Canberra (Aust); 1998. [Google Scholar]
- 71.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: Does the choice of area-based measure and geographic level matter? The public health disparities geocoding project. Am J Epidemiol 2002;156:471–482. [DOI] [PubMed] [Google Scholar]
- 72.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health 2003;93:1655–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Promot Health 2006;126:262–267. [DOI] [PubMed] [Google Scholar]
- 74.Lovasi GS, Moudon AV, Smith NL, et al. Evaluating options for measurement of neighborhood socioeconomic context: Evidence from a myocardial infarction case–control study. Health Place 2008;14:453–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Diez Roux AV Neighborhoods and Health: What Do We Know? What Should We Do? Am J Public Health 2016;106:430–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jiao J, Drewnowski A, Moudon A, et al. The impact of area residential property values on self-rated health: A cross-sectional comparative study of Seattle and Paris. Prev Med Reports 2016;4:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aggarwal A, Cook AJ, Jiao J, et al. Access to supermarkets and fruit and vegetable consumption. Am J Public Health 2014;104:917–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Drewnowski A, Moudon AV, Jiao J, Aggarwal A, Charreire H, Chaix B. Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. Int J Obes 2014;38:306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cummins S, Macintyre S. Food environments and obesity—neighbourhood or nation? Int J Epidemiol 2006;35:100–104. [DOI] [PubMed] [Google Scholar]
- 80.Penney TL, Brown HE, Maguire ER, Kuhn I, Monsivais P. Local food environment interventions to improve healthy food choice in adults: a systematic review and realist synthesis protocol. BMJ Open 2015;5:e007161–e007161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Smith L, Foley L, Panter J. Activity spaces in studies of the environment and physical activity: A review and synthesis of implications for causality. Health Place 2019;58:102113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wilkins E, Morris M, Radley D, Griffiths C. Methods of measuring associations between the Retail Food Environment and weight status: Importance of classifications and metrics. SSM - Popul Heal 2019;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wilkins E, Radley D, Morris M, et al. A systematic review employing the GeoFERN framework to examine methods, reporting quality and associations between the retail food environment and obesity. Health Place 2019;57:186–199. [DOI] [PubMed] [Google Scholar]
- 84.An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med 2012;42:129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Does diet cost mediate the relation between socioeconomic position and diet quality? Eur J Clin Nutr 2011;65:1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Drewnowski A, Aggarwal A, Tang W, Moudon AV. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity 2015;23:671–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Giannotti F, Nanni M, Pedreschi D, et al. Unveiling the complexity of human mobility by querying and mining massive trajectory data. VLDB J 2011;20:695–719. [Google Scholar]
- 88.Cagney K, Cornwell E. Place, Aging, and Health. In: Directions for the Demography of Aging: Proceedings of a Workshop. National Academies Press, 2018. [PubMed] [Google Scholar]
- 89.Lee JH, Davis AW, Yoon SY, Goulias KG. Activity space estimation with longitudinal observations of social media data. Transportation (Amst) 2016;43:955–977. [Google Scholar]
- 90.Thierry B, Chaix B, Kestens Y. Detecting activity locations from raw GPS data: a novel kernel-based algorithm. Int J Health Geogr 2013;12:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tamura K, Langerman SD, Ceasar JN, Andrews MR, Agrawal M, Powell-Wiley TM. Neighborhood Social Environment and Cardiovascular Disease Risk. Curr Cardiovasc Risk Rep 2019;13:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Katapally TR, Bhawra J, Leatherdale ST, et al. The SMART Study, a Mobile Health and Citizen Science Methodological Platform for Active Living Surveillance, Integrated Knowledge Translation, and Policy Interventions: Longitudinal Study. JMIR public Heal Surveill 2018;4:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dunton GF, Kawabata K, Intille S, Wolch J, Pentz MA. Assessing the Social and Physical Contexts of Children’s Leisure-Time Physical Activity: An Ecological Momentary Assessment Study. Am J Heal Promot 2012;26:135–142. [DOI] [PubMed] [Google Scholar]
- 94.Dunton GF, Intille SS, Wolch J, Pentz MA. Investigating the impact of a smart growth community on the contexts of children’s physical activity using Ecological Momentary Assessment. Health Place 2012;18:76–84. [DOI] [PubMed] [Google Scholar]
- 95.Kirchner TR, Shiffman S. Spatio-temporal determinants of mental health and well-being: advances in geographically-explicit ecological momentary assessment (GEMA). Soc Psychiatry Psychiatr Epidemiol 2016;51:1211–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mellor JM, Dolan CB, Rapoport RB. Child body mass index, obesity, and proximity to fast food restaurants. Int J Pediatr Obes 2011;6:60–68. [DOI] [PubMed] [Google Scholar]
- 97.Li F, Harmer P, Cardinal BJ, et al. Obesity and the Built Environment: Does the Density of Neighborhood Fast-Food Outlets Matter? Am J Heal Promot 2010;23:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Spence JC, Cutumisu N, Edwards J, Raine KD, Smoyer-Tomic K. Relation between local food environments and obesity among adults. BMC Public Health 2009;9:6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jiao J, Moudon AV, Kim SY, Hurvitz PM, Drewnowski A. Health Implications of Adults’ Eating at and Living near Fast Food or Quick Service Restaurants. Nutr Diabetes 2015;5:e171–e171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Van Dyck D, Cerin E, Cardon G, et al. Physical activity as a mediator of the associations between neighborhood walkability and adiposity in Belgian adults. Health Place 2010;16:952–960. [DOI] [PubMed] [Google Scholar]
- 101.Oliver M, Witten K, Blakely T, et al. Neighbourhood built environment associations with body size in adults: mediating effects of activity and sedentariness in a cross-sectional study of New Zealand adults. BMC Public Health 2015;15:956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Koohsari MJ, Kaczynski AT, Nakaya T, et al. Walkable Urban Design Attributes and Japanese Older Adults’ Body Mass Index: Mediation Effects of Physical Activity and Sedentary Behavior. Am J Heal Promot 2019;33:764–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Carroll SJ, Niyonsenga T, Coffee NT, Taylor AW, Daniel M. Does Physical Activity Mediate the Associations Between Local-Area Descriptive Norms, Built Environment Walkability, and Glycosylated Hemoglobin? Int J Environ Res Public Health 2017;14:953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ball K, Timperio A, Crawford D. Neighbourhood socioeconomic inequalities in food access and affordability. Heal Place 2009;15:578–585. [DOI] [PubMed] [Google Scholar]
- 105.Chaloupka FJ, Powell LM. Price, availability, and youth obesity: evidence from Bridging the Gap. Prev Chronic Dis 2009;6:A93. [PMC free article] [PubMed] [Google Scholar]
- 106.Spoden AL, Buszkiewicz JH, Drewnowski A, Long MC, Otten JJ. Seattle’s minimum wage ordinance did not affect supermarket food prices by food processing category. Public Health Nutr 2018. [DOI] [PMC free article] [PubMed]
- 107.Otten J, Buszkiewicz J, Tang W, et al. The Impact of a City-Level Minimum-Wage Policy on Supermarket Food Prices in Seattle-King County. Int J Environ Res Public Health 2017;14:1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Buszkiewicz J, House C, Aggarwal A, Long M, Drewnowski A, Otten JJ. The Impact of a City-Level Minimum Wage Policy on Supermarket Food Prices by Food Quality Metrics: A Two-Year Follow Up Study. Int J Environ Res Public Health 2019;16:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Caspi CE, Kawachi I, Subramanian SV, Adamkiewicz G, Sorensen G. The relationship between diet and perceived and objective access to supermarkets among low-income housing residents. Soc Sci Med 2012;75:1254–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sallis JF, Slymen DJ, Conway TL, et al. Income disparities in perceived neighborhood built and social environment attributes. Health Place 2011;17:1274–1283. [DOI] [PubMed] [Google Scholar]
- 111.McCormack G, Giles-Corti B, Lange A, Smith T, Martin K, Pikora TJ. An update of recent evidence of the relationship between objective and self-report measures of the physical environment and physical activity behaviours. J Sci Med Sport 2004;7:81–92. [DOI] [PubMed] [Google Scholar]
- 112.Gustafson AA, Sharkey J, Samuel-Hodge CD, et al. Perceived and objective measures of the food store environment and the association with weight and diet among low-income women in North Carolina. Public Health Nutr 2011;14:1032–1038. [DOI] [PubMed] [Google Scholar]
- 113.Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: a meta-analysis of selected environmental characteristics. Int J Behav Nutr Phys Act 2005;2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.McGinn AP, Evenson KR, Herring AH, Huston SL, Rodriguez DA. Exploring Associations between Physical Activity and Perceived and Objective Measures of the Built Environment. J Urban Heal 2007;84:162–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chirinos DA, Garcini LM, Seiler A, et al. Psychological and Biological Pathways Linking Perceived Neighborhood Characteristics and Body Mass Index. Ann Behav Med 2018. [DOI] [PMC free article] [PubMed]
- 116.Freedman DA, Bell BA. Access to healthful foods among an urban food insecure population: Perceptions versus reality. J Urban Heal 2009;86:825–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Drewnowski A, Aggarwal A, Rehm CD, Cohen-Cline H, Hurvitz PM, Moudon AV. Environments Perceived as Obesogenic Have Lower Residential Property Values. Am J Prev Med 2014;47:260–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kim Y Impacts of the perception of physical environments and the actual physical environments on self-rated health. Int J Urban Sci 2016;20:73–87. [Google Scholar]
- 119.Wang X, Conway TL, Cain KL, et al. Interactions of psychosocial factors with built environments in explaining adolescents’ active transportation. Prev Med (Baltim) 2017;100:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Molina-García J, García-Massó X, Estevan I, Queralt A. Built Environment, Psychosocial Factors and Active Commuting to School in Adolescents: Clustering a Self-Organizing Map Analysis. Int J Environ Res Public Health 2018;16:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lê J, Dallongeville J, Wagner A, et al. Attitudes toward healthy eating: a mediator of the educational level–diet relationship. Eur J Clin Nutr 2013;67:808–814. [DOI] [PubMed] [Google Scholar]
- 122.Drewnowski A, Kawachi I. Diets and Health: How Food Decisions Are Shaped by Biology, Economics, Geography, and Social Interactions. Big Data 2015;3:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Aggarwal A, Rehm CD, Monsivais P, Drewnowski A. Importance of taste, nutrition, cost and convenience in relation to diet quality: Evidence of nutrition resilience among US adults using National Health and Nutrition Examination Survey (NHANES) 2007–2010. Prev Med (Baltim) 2016;90:184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Maddison R, Hoorn S, Jiang Y, et al. The environment and physical activity: The influence of psychosocial, perceived and built environmental factors. Int J Behav Nutr Phys Act 2009;6:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Saelens BE, Sallis JF, Frank LD, et al. Neighborhood environment and psychosocial correlates of adults’ physical activity. Med Sci Sports Exerc 2012;44:637–46. [DOI] [PubMed] [Google Scholar]
- 126.Carlson JA, Sallis JF, Conway TL, et al. Interactions between psychosocial and built environment factors in explaining older adults’ physical activity. Prev Med (Baltim) 2012;54:68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Positive Attitude toward Healthy Eating Predicts Higher Diet Quality at All Cost Levels of Supermarkets. J Acad Nutr Diet 2014;114:266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Orstad SL, McDonough MH, Klenosky DB, Mattson M, Troped PJ. The observed and perceived neighborhood environment and physical activity among urban-dwelling adults: The moderating role of depressive symptoms. Soc Sci Med 2017;190:57–66. [DOI] [PubMed] [Google Scholar]
- 129.Butland B, Jebb S, Kopelman P, et al. Tackling obesities: Future choices - project report 2nd edition. 2007. https://www.safefood.eu/SafeFood/media/SafeFoodLibrary/Documents/Professional/Allisland%20Obesity%20Action%20Forum/foresight-report-full_1.pdf. Accessed September, 30, 2019. [DOI] [PubMed]
- 130.Boone-Heinonen J, Guilkey DK, Evenson KR, Gordon-Larsen P. Residential self-selection bias in the estimation of built environment effects on physical activity between adolescence and young adulthood. Int J Behav Nutr Phys Act 2010;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Popescu I, Duffy E, Mendelsohn J, Escarce JJ. Racial residential segregation, socioeconomic disparities, and the White-Black survival gap Bowen M (ed.). PLoS One 2018;13:e0193222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Williams DR, Lawrence JA, Davis BA. Racism and Health: Evidence and Needed Research. Annu Rev Public Heal 2019;40:105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tung EL, Cagney KA, Peek ME, Chin MH. Spatial Context and Health Inequity: Reconfiguring Race, Place, and Poverty. J Urban Heal 2017;94:757–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kimbro RT, Sharp G, Denney JT. Home and away: Area socioeconomic disadvantage and obesity risk. Health Place 2017;44:94–102. [DOI] [PubMed] [Google Scholar]
- 135.Turner C, Aggarwal A, Walls H, et al. Concepts and critical perspectives for food environment research: A global framework with implications for action in low- and middle-income countries. Glob Food Sec 2018;18:93–101. [Google Scholar]
- 136.Aiello LM, Schifanella R, Quercia D, Del Prete L. Large-scale and high-resolution analysis of food purchases and health outcomes. EPJ Data Sci 2019;8:14. [Google Scholar]
- 137.Zandbergen PA. Ensuring Confidentiality of Geocoded Health Data: Assessing Geographic Masking Strategies for Individual-Level Data. Adv Med 2014;2014:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Drewnowski A, Aggarwal A, Cook A, Stewart O, Moudon AV. Geographic disparities in Healthy Eating Index scores (HEI–2005 and 2010) by residential property values: Findings from Seattle Obesity Study (SOS). Prev Med (Baltim) 2016;83:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Vanhelst J, Mikulovic J, Bui-Xuan G, et al. Comparison of two ActiGraph accelerometer generations in the assessment of physical activity in free living conditions. BMC Res Notes 2012;5:187. [DOI] [PMC free article] [PubMed] [Google Scholar]