Abstract
Prostate cancer is the most commonly diagnosed cancer among men in the United States as well as most Western countries. A significant proportion of men report having a positive family history of prostate cancer in a first-degree relative (father, brother, son), which is important in that family history is one of the only established risk factors for the disease and plays a role in decision-making for prostate cancer screening. Familial aggregation of prostate cancer is considered a surrogate marker of genetic susceptibility to developing the disease, but shared environment cannot be excluded as an explanation for clustering of cases among family members. Prostate cancer is both a clinically and genetically heterogeneous disease with inherited factors predicted to account for 40%–50% of cases, comprised of both rare highly to moderately penetrant gene variants, as well as common genetic variants of low penetrance. Most notably, HOXB13 and BRCA2 mutations have been consistently shown to increase prostate cancer risk, and are more commonly observed among patients diagnosed with early-onset disease. A recurrent mutation in HOXB13 has been shown to predispose to hereditary prostate cancer (HPC), and BRCA2 mutations to hereditary breast and ovarian cancer (HBOC). Genome-wide association studies (GWAS) have also identified approximately 100 loci that associate with modest (odds ratios < 2.0) increases in prostate cancer risk, only some of which have been replicated in subsequent studies. Despite these efforts, genetic testing in prostate cancer lags behind other common tumors like breast and colorectal cancer. To date, National Comprehensive Cancer Network (NCCN) guidelines have highly selective criteria for BRCA1/2 testing for men with prostate cancer based on personal history and/or specific family cancer history. Tumor sequencing is also leading to the identification of germline mutations in prostate cancer patients, informing the scope of inheritance. Advances in genetic testing for inherited and familial prostate cancer (FPC) are needed to inform personalized cancer risk screening and treatment approaches.
Keywords: Genetics, Epidemiology, Hereditary prostate cancer, Genome-wide association, HOXB13, BRCA1/2
1. Introduction
Familial clustering of prostate cancer has been a long-standing observation [1–3], with concentrated clustering or young-onset of disease indicating a strong predisposition to hereditary prostate cancer [2,4]. Over time, the link of prostate cancer to other cancers in families has also been observed [5–9], potentially expanding the scope of family cancer history when considering the diagnosis of hereditary prostate cancer (HPC). Several factors have been associated with familial prostate cancer (FPC), including genetic variants, family cancer history, race/ethnicity, and diet/environmental factors. This brief review will discuss the risk factors for prostate cancer, current knowledge of the genetic basis for inherited predisposition to prostate cancer, and emerging developments in clinical translation relevant to FPC.
2. The epidemiology of familial prostate cancer
Prostate cancer is the most common cancer diagnosed among men in the United States and most of the Western world [10,11]. In the United States, an estimated 220,800 new cases of prostate cancer were diagnosed in 2015, representing over one quarter of all new invasive cancers among men [11]. Prostate cancer is also the second leading cause of cancer death with an estimated 27,500 deaths in the United States attributed to the disease in 2015 [11]. Prostate cancer is a heterogeneous disease, with a wide spectrum of age of onset and clinical severity, which complicates the study of epidemiologic risk factors. Established risk factors include older age, African American race, and a positive family history of prostate cancer [12]. Other factors with inconsistent associations include energy intake, diet, obesity and metabolic syndrome, physical inactivity, and environmental exposure to heavy metals such as cadmium [13,14] and herbicides such as Agent Orange [15].
A positive family history of prostate cancer, particularly when diagnosed in a first-degree relative, has been associated with an approximate two- to threefold increase in the risk of prostate cancer [16]. Risk generally increases with the number of affected relatives and the specific relatives (affected brothers as opposed to father and sons), and it is inversely related to the age at diagnosis among affected relatives [3]. FPC has been defined as families with either: (1) two first-degree relatives diagnosed with prostate cancer at any age, or (2) one first-degree relative and two or more second-degree relatives diagnosed at any age [17]. A more stringent definition of HPC has been used to characterize families with a particularly strong history of prostate cancer and includes those families with either: (1) three or more affected first-degree relatives, (2) prostate cancer diagnosed in three successive generations of the same lineage (paternal or maternal), or (3) two first-degree relatives both diagnosed with early-onset disease (age ≤ 55 years) [4]. It has been estimated that 5%–10% of prostate cancer cases may be considered hereditary.
Study results have been mixed with respect to the clinicopathologic characteristics and short-term and long-term outcomes of patients diagnosed with FPC or HPC. These studies are also likely confounded by enhanced prostate-specific antigen (PSA) screening among those with a family history of disease. Among 16,472 radical prostatectomy patients treated at the Mayo Clinic, patients with a family history were more likely to be diagnosed with organ-confined disease, lower pathologic Gleason score, and higher 10-year cancer-specific and overall survival compared with sporadic cases [18]. These findings are inconsistent with those of an earlier study by Kupelian et al, which observed a greater risk of biochemical recurrence after surgery among patients with a family history of prostate cancer where the period of study (1987–1996) was less likely influenced by screening history and intensity [19]. Findings from the prostate arm of the Prostate, Lung, Colorectal and Ovarian (PLCO) trial also indicate the prostate cancer death rate was significantly higher among men with a positive family history of prostate cancer; however, age and PSA at diagnosis and Gleason score were similar between those with and without a family history. Notably, comparison of the usual care versus screening arms of the PLCO trial among patients with a positive family history indicate the potential benefit of screening on cancer-specific mortality (hazard ratio [HR] = 0.49; 95% confidence interval [CI] 0.22–1.1) that was not observed in men with no family history [20]. It should be noted that the vast majority of studies have been conducted among patients almost, if not entirely, exclusively European descent and further investigation is required among minorities diagnosed with prostate cancer.
Though family history is often considered an indicator of genetic susceptibility, one cannot exclude the possibility of shared environmental exposures, particularly exposures in the environment occurring early in life, as well as the interaction between gene(s) and environment in explaining aggregation of prostate cancer within families. A recently published study of more than 80,000 adoptees and their adoptive parents identified from the Swedish Register and linked to the Swedish Cancer Registry suggested that 5% of prostate cancers diagnosed among family members are attributed to shared environmental factors and not genetics [21].
3. Genetic contribution to inherited prostate cancer
Prostate cancer has a substantial inherited component estimated at 40%–50% [22]. This genetic contribution is made up of a combination of rare variants in genes of high- to moderate-penetrance and common, low-penetrance genes. However, the identification of susceptibility genes in prostate cancer has been challenging due to both the clinical and genetic heterogeneity of the disease.
3.1. Rare gene mutations of high- to moderate-penetrance
Genetic mutations that impact cancer risk management typically have been rare (< 5% of the population) and highly penetrant (80%–100% likelihood of expressing the phenotype), and have usually been associated with hereditary cancer syndrome phenotypes. Numerous studies have focused specifically on identifying these variants in HPC, while others have observed prostate cancers diagnosed in hereditary cancer syndromes notably linked to other solid tumors including hereditary breast and ovarian cancer (HBOC) and Lynch syndrome. Table 1 shows the range of risk for prostate cancer, aggressive prostate cancer, risk for early-onset prostate cancer, and outcomes from selected studies by genes associated with hereditary cancer syndromes. HBOC syndrome is a hereditary cancer syndrome associated with a significantly increased lifetime risk for breast and ovarian cancers in families, most commonly caused by mutations in BRCA1 or BRCA2 [23–25]. Other cancers implicated in HBOC caused by BRCA mutations include prostate cancer [5,26], pancreatic cancer, and melanoma [26–28]. BRCA2 mutation carriers have been reported to have more aggressive prostate cancer and decreased cause-specific survival [29–31]. Lynch syndrome, also referred to as hereditary non-polyposis colorectal cancer (HNPCC), is an autosomal dominant disorder caused by germline mutations in DNA mismatch repair (MMR) genes and is associated with increased risks for cancers of the colon, uterus, ovaries, upper urologic tract, stomach, small bowel, biliary tract, and brain in addition to predisposing to sebaceous adenomas [32]. Germline mutations/alterations in DNA MMR genes accounting for Lynch syndrome include MLH1, MSH2, MSH6, and PMS2 [33–35]. Furthermore, deletions in EPCAM have also been implicated in Lynch syndrome [36,37]. Prostate cancer incidence has been reported at higher rates in Lynch syndrome families and in male carriers of mutations in the DNA MMR genes [9,38]. Prostate tumor testing among male MMR gene mutation carriers displayed microsatellite instability and loss of MMR gene expression in one study implicating this pathway in prostate cancer formation in those with germline MMR mutations [39].
Table 1.
Risk estimates for prostate cancer (PCA) by genes associated with hereditary cancer syndromes.
| Gene | Risk for PCA* | Risk for aggressive PCA features*,‡ | *+Risk for early-onset PCA (age at diagnosis < 65)*,§ | PCA-specific outcomes† |
|---|---|---|---|---|
| BRCA1 | 1.07–3.81 [26,53,89–92] | -- | 1.82 [90] | 5.16 [56] |
| BRCA2 | 3.18–8.6 [26,56,57,89,93–95] | 3.18–4.38 [30,55,96] | 7.33 [89] | HR for death 2.4–5.48 [56,96–98], decreased survival [31] |
| Mismatch repair genes | 1.99–3.67 [38,99] | -- | 2.48 [38] | -- |
| HOXB13 | 2.8–8.47 [41,44,47,50] | -- | 2.7–10.11 [41,44,47,50,100] | -- |
Risks are a combination of odds ratios, relative risks, hazard ratios, or standardized incidence ratios depending on the study. Risks vary based on strength of family history reported.
Outcomes are a combination of survival estimates or mortality depending on the study.
Definition of aggressive prostate cancer features include Gleason score ≥ 7, depending on the study. Additional studies have described an association of BRCA1 and BRCA2 in particular to features of aggressiveness. The table highlights those studies with reported risk estimates.
While definitions for early-onset prostate cancer can vary, risks are reported for age at diagnosis < 65 years to encompass the majority of studies with an age-related focus.
Next-generation sequencing (NGS) technology has ushered in an era of new genetic testing approaches, such as germline multigene panel testing and somatic multigene/genomic testing, which have led to the identification of rare variants in genes of moderate penetrance [40]. These moderately penetrant gene mutations typically lead to a 35%–60% lifetime risk of manifesting the disease phenotype, and several of these genes have been identified in prostate cancer populations. Most notably, in 2012, a rare, recurrent mutation in the homeobox transcription factor HOXB13 gene was identified in a subset of HPC and early-onset cases and has been consistently replicated in numerous independent populations (Table 1) [41–50]. The reported penetrance estimates of prostate cancer associated with the HOXB13 G84E mutation have ranged from 33%–60%. [51,52]
Overall, studies have consistently demonstrated the role of BRCA2 and HOXB13 mutations in prostate cancer risk. However, these genes account for a small fraction of inherited predisposition to prostate cancer. The reported frequency of BRCA2 mutations ranges from 1.3%–3.2% depending on the study design and population [53–57], with some smaller studies reporting frequencies of < 1% among cases. The carrier frequency of HOXB13 mutations has been reported at 0.66%–6.25% from studies of cases and controls encompassing a variety of geographic regions [45]. A large pooled analysis including 9,016 prostate cancer cases reported a carrier frequency of 1.34% among cases [47]. Mutations in CHEK2, PALB2, and NBS1 have also been reported in prostate cancer with less consistency in replicative studies. Mutations in CHEK2 (checkpoint kinase 2) have been reported to confer an approximate 2.0- to 2.7-fold increased risk for prostate cancer in a Polish population [58]. This study also reported an odds ratio (OR) of 2.3 (95% CI 1.8–3.1) for prostate cancer diagnosis at age < 60 years. In a Finnish study, a truncating mutation in PALB2 was observed among multiple family members affected with prostate cancer [59]. This gene is of particular interest due to its reported association with breast cancer and the encoded protein’s ability to bind with BRCA2. Findings from a subsequent study of 95 University of Michigan HPC families did not support a role for this mutation in HPC [60]. Mutations in NBS1 (Nijmegen breakage syndrome 1) have also been reported to associate with prostate cancer risk (OR 2.5, 95% CI 1.5–4.0), age at diagnosis < 60 (OR 3.1, 95% CI 1.5–6.4), and FPC (OR 4.3, 95% CI 2.0–9.0) [58,61]. Additional germline mutations in moderately penetrant genes are being reported from studies of somatic sequencing of prostate tumors aimed at identifying treatment targets [62,63].
3.2. Common variants
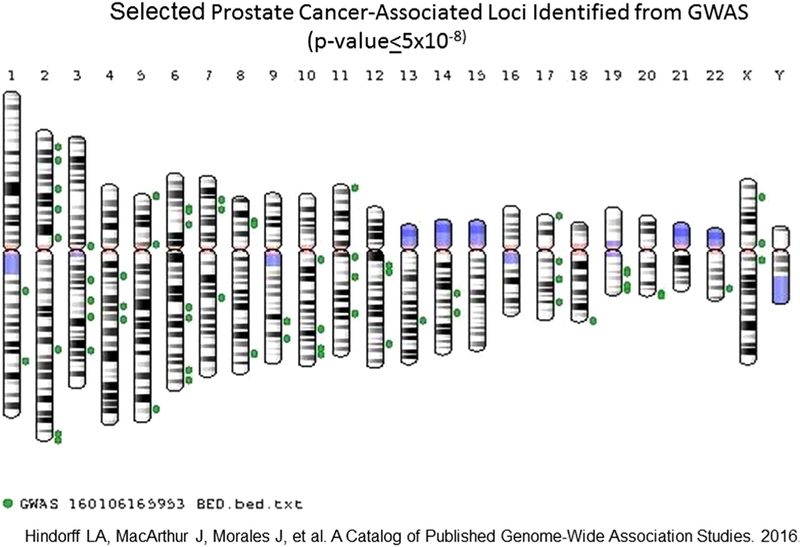
With the growing knowledge of the human genome, common genetic variation has been able to be exploited to identify new loci associated with a multitude of diseases, including prostate cancer risk. Genome-wide association studies (GWAS) have identified multiple loci that explain an estimated 33% of FPC risk [64,65]. Figure 1 depicts a subset of those loci identified for association to prostate cancer achieving variant-trait associations with P ≤ 5.0 × 10−8 [66]. Overall, approximately 100 loci have been reported to associate with prostate cancer with validation in independent cohorts [67]. While these loci have associations to prostate cancer with a high level of statistical significance, the magnitude of risk remains modest with typical ORs of < 2.0 [68]. Furthermore, the functional significance of identified variants remains unclear, with ongoing efforts at functional annotation of variants identified from GWAS [69]. Finally, no common variants have been consistently associated with prostate cancer-specific survival [70], which is an important factor regarding the clinical utility of germline variants in informing management. While studies are reporting the cumulative risk for prostate cancer associated with carrying multiple GWAS-identified variants [71,72], the clinical utility remains uncertain. Taken together, while multiple genetic variants have been identified from GWAS with strong statistical associations to prostate cancer, the discriminative ability to identify individuals at risk for developing prostate cancer remains modest and therefore these variants are not advocated for clinical use at the present time [73,74].
Fig. 1.
Selected prostate cancer associated loci identified from GWAS (P ≤ 5 × 10−8).
4. Clinical translation
4.1. Genetic testing for inherited prostate cancer
Genetic counseling and genetic testing for inherited prostate cancer has been a more slowly evolving field when compared to other common cancers such as breast cancer or colon cancer. Of all of the genetic determinants of prostate cancer identified so far, genetic testing for BRCA1 and BRCA2 mutations in the context of prostate cancer is now emerging from national organizations [75]. The National Comprehensive Cancer Network (2015) guidelines incorporate prostate cancer for genetic counseling and potential genetic testing for the following: personal history of breast cancer and two or more close blood relatives with pancreatic cancer and/or prostate cancer (Gleason score ≥ 7) at any age. “Close blood relatives” include first-degree, second-degree, or third-degree relatives on the same side of the family per the guideline. An additional criterion for genetic counseling/testing includes personal history of prostate cancer (Gleason score ≥ 7) at any age with one or more close blood relatives with breast cancer (age ≤ 50 years) and/or invasive ovarian and/or pancreatic or prostate cancer (Gleason score ≥ 7) at any age [76]. These criteria highlight the importance of obtaining a detailed and thorough family cancer history on the maternal and paternal sides of the family for an individual presenting for prostate cancer risk evaluation. Furthermore, genetic counseling remains vital in order to provide patients with pre-test information regarding potential additional cancer risks for the proband and their blood relatives that could be identified from genetic testing for BRCA1/2 gene mutations, such as risk for breast and ovarian cancers, male breast cancer, pancreatic cancer, and melanoma.
Histopathologic features can also be indicative of underlying germline predisposition to prostate cancer [77]. Approximately 42% of BRCA2 mutation carriers with prostate cancer have been reported to have intraductal carcinoma on pathology, while approximately 45% of prostate cancer patients harboring a HOXB13 mutation have been reported to have “pseudohyperplastic” features [77]. Furthermore, prostate cancers of these individuals with the HOXB13 G84E mutation have been reported to have lower prevalence of ERG expression compared to unselected cases, pointing to a potential underlying molecular phenotype of HOXB13-associated prostate cancer [78]. Unique histopathologic and molecular features of prostate cancer tissues may prove useful in identifying individuals for referral to genetic counseling.
4.2. Prostate cancer screening
The use of PSA in screening for prostate cancer in the general population remains controversial. Current US Preventive Services Task Force recommends against the use of PSA screening in asymptomatic men [79]. However, both the American Urologic Association (AUA) and the American Cancer Society (ACS) suggest that clinicians consider patient age, life expectancy, family history and race in making decisions about recommendations for screening [80,81]. Family history of prostate cancer is factored into ACS guidelines for recommendation of when to begin the discussion of PSA-based prostate cancer screening. The ACS recommends that men with a first-degree relative diagnosed with prostate cancer younger than age 65 should have a discussion of PSA screening starting at age 45. Those with an even stronger family history, such as more than one first-degree relative with prostate cancer at a young age, should have this screening discussion at age 40 [82]. Current NCCN guidelines support discussion of baseline PSA testing for all men beginning at age 45 with the frequency of testing post-baseline dependent on the baseline PSA concentration. Despite the fact that African Americans and men with a positive family history have a greater risk of being diagnosed, NCCN guidelines do not suggest separate screening guidelines for these high-risk groups. NCCN does recommend that BRCA2 mutation carriers begin prostate cancer screening at age 40 and suggest the same for BRCA1 cancers [83]. These recommendations are partly in response to early findings from the IMPACT screening trial, which reported a significantly higher positive predictive value (PPV) for prostate cancer detected upon subsequent biopsy among BRCA2 carriers compared with related non-carriers (48.0% v 33.3%) [84]. Current NCCN guidelines do not comment on prostate cancer screening for men with Lynch syndrome [83].
4.3. Prostate cancer treatment
One important goal of genetic information is to provide individualized estimates of disease prognosis and severity in order to tailor management. An example of this approach for germline genetic testing is in relapsed/refractory ovarian cancer, where women are tested for BRCA mutations, and if positive, can be treated with a poly(ADP-ribose) polymerase (PARP) inhibitor where there has been demonstrated improvement in progression-free survival [85,86]. In prostate cancer treatment, data regarding BRCA mutations is informing expert opinion about potential individualized management. Prostate cancer patients with BRCA mutations have been reported to have higher rates of metastatic disease and prostate cancer-specific death after localized treatment with radical prostatectomy or radiotherapy [31]. Prostate cancer-specific survival has also been reported to be lower among screen-detected prostate cancer for individuals carrying a BRCA2 mutation compared to non-carriers (61.8% v 94.3%, P < 10−4) [30]. Another study reported no significant difference in response of castrate-resistant prostate cancer to taxane-based therapy between BRCA mutation carriers versus non-carriers in an Ashkenazi Jewish population [87], providing further insight into potential systemic treatment for prostate cancer patients carrying BRCA mutations. While genetically-based treatment guidelines do not currently exist for prostate cancer, expert opinion is emerging regarding how to consider individualizing management [88]. Suggestions include combining local therapy with systemic approaches in BRCA mutation carriers, particularly for BRCA2 carriers, due to the poorer prognosis in these patients. Furthermore, PARP inhibition may play more of a role in the metastatic, castrate-resistant setting based on emerging data [62,63,88].
As precision medicine efforts launch forward, somatic sequencing of prostate tumor tissues is also identifying potential targets for treatment. The goal of somatic sequencing is to identify tumor-specific genetic alterations in specific genes for which there are treatments available or clinical trial options for patients. A recent study reported that patients with metastatic, castrate-resistant prostate cancer with DNA repair defects (as defined by a homozygous deletion or deleterious mutation in the tumor in a gene reported to be involved either in DNA damage repair or sensitivity to PARP inhibition) had significantly improved radiologic progression-free survival and overall survival compared to those without evidence of DNA repair defects [62]. This study also reported a prevalence of BRCA2 germline mutations of 6% in the cohort. Another report of precision oncology that integrated somatic sequencing with multidisciplinary management recommendations for patients reported a rate of 8% clinically actionable germline pathogenic mutations in metastatic castrate-resistant individuals [63]. Furthermore, another study assessing germline inherited DNA-repair mutations in men with metastatic, castrate-resistant prostate cancer reported 11.2% rate of mutations in DNA-repair genes, and 5.3% were in BRCA2 [100]. Thus sequencing efforts will likely expand the knowledge of prevalence and scope of germline mutations identified in prostate cancer patient populations, and inform treatment options for these patients.
5. Conclusion
FPC remains an important clinical entity, with a spectrum of epidemiologic and genetic risk factors. Advances in DNA sequencing technologies will lead to new discoveries of the genetic predisposition to this disease, and potential gene-environment contribution to FPC. Insight into the predisposition to FPC is expected to further inform individualized prostate cancer screening and treatment.
References
- [1].Steinberg GD, Carter BS, Beaty TH, Childs B, Walsh PC. Family history and the risk of prostate cancer. Prostate 1990;17:337–47. [DOI] [PubMed] [Google Scholar]
- [2].Carter BS, Beaty TH, Steinberg GD, Childs B, Walsh PC. Mendelian inheritance of familial prostate cancer. Proc Natl Acad Sci USA 1992;89:3367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Stanford JL, Ostrander EA. Familial prostate cancer. Epidemiol Rev 2001;23:19–23. [DOI] [PubMed] [Google Scholar]
- [4].Carter BS, Bova GS, Beaty TH, et al. Hereditary prostate cancer: epidemiologic and clinical features. J Urol 1993;150:797–802. [DOI] [PubMed] [Google Scholar]
- [5].Liede A, Karlan BY, Narod SA. Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol 2004;22:735–42. [DOI] [PubMed] [Google Scholar]
- [6].Beebe-Dimmer JL, Yee C, Cote ML, et al. Familial clustering of breast and prostate cancer and risk of postmenopausal breast cancer in the Women’s Health Initiative Study. Cancer 2015;121:1265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Brandt A, Sundquist J, Hemminki K. Risk for incident and fatal prostate cancer in men with a family history of any incident and fatal cancer. Ann Oncol 2012;23:251–6. [DOI] [PubMed] [Google Scholar]
- [8].Soravia C, van der KH, Brundler MA, et al. Prostate cancer is part of the hereditary non-polyposis colorectal cancer (HNPCC) tumor spectrum. Am J Med Genet 2003;121A:159–62. [DOI] [PubMed] [Google Scholar]
- [9].Haraldsdottir S, Hampel H, Wei L, et al. Prostate cancer incidence in males with Lynch syndrome. Genet Med 2014;16:553–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].ACS Global Facts and Figures. 3rd ed. Atlanta, GA, American Cancer Society; 2012. [Google Scholar]
- [11].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5–29. [DOI] [PubMed] [Google Scholar]
- [12].Hsing AW, Chokkalingam AP. Prostate cancer epidemiology. Front Biosci 2006;11:1388–413. [DOI] [PubMed] [Google Scholar]
- [13].Platz E, Giovannucci E. Prostate cancer In: Schottenfeld D, Fraumeni JF, editors. Cancer epidemiology and prevention. 3rd edition New York: Oxford University Press; 2006. p. 1128–50. [Google Scholar]
- [14].Hsing AW, Sakoda LC, Chua S Jr. Obesity, metabolic syndrome, and prostate cancer. Am J Clin Nutr 2007;86:s843–57. [DOI] [PubMed] [Google Scholar]
- [15].Giri VN, Cassidy AE, Beebe-Dimmer J, et al. Association between Agent Orange and prostate cancer: a pilot case-control study. Urology 2004;63: 757–760. [DOI] [PubMed] [Google Scholar]
- [16].Kiciński M, Vangronsveld J, Nawrot TS. An epidemiological reappraisal of the familial aggregation of prostate cancer: a meta-analysis. PLoS ONE 2011;6 (10):e27130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ostrander EA, Markianos K, StanfordJL. Finding prostate cancer susceptibility genes. Annu Rev Genomics Hum Genet 2004;5:151–75. [DOI] [PubMed] [Google Scholar]
- [18].Westerman ME, Gershman B, Karnes RJ, Thompson RH, Rangel L, Boorjian SA. Impact of a family history of prostate cancer on clinicopathologic outcomes and survival following radical prostatectomy. World J Urol 2015;8:1115–22. [DOI] [PubMed] [Google Scholar]
- [19].Kupelian P, Klein E, Witte J, Kuppelian V, Suh J. Familial prostate cancer: a different disease? J Urol 1997;158:2197–201. [DOI] [PubMed] [Google Scholar]
- [20].Liss MA, Chen H, Hemal S, et al. Impact of family history on prostate cancer mortality in white men undergoing prostate specific antigen based screening. J Urol 2015;193:75–9. [DOI] [PubMed] [Google Scholar]
- [21].Sundquist K, Sundquist J, Ji J. Contribution of shared environmental factors to familial aggregation of common cancers: an adoption study in Sweden. Eur J Cancer Prev 2015;24:162–4. [DOI] [PubMed] [Google Scholar]
- [22].Hjelmborg JB, Scheike T, Holst K, et al. The heritability of prostate cancer in the Nordic Twin Study of Cancer. Cancer Epidemiol Biomarkers Prev 2014;23 (11):2303–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Whittemore AS. Risk of breast cancer in carriers of BRCA gene mutations. N Engl J Med 1997;337:788–9. [PubMed] [Google Scholar]
- [24].Blackwood MA, Weber BL. BRCA1 and BRCA2: from molecular genetics to clinical medicine. J Clin Oncol 1998;16:1969–77. [DOI] [PubMed] [Google Scholar]
- [25].Venkitaraman AR. Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 2002;108:171–82. [DOI] [PubMed] [Google Scholar]
- [26].Mersch J, Jackson MA, Park M, et al. Cancers associated with BRCA1 and BRCA2 mutations other than breast and ovarian. Cancer 2015;121: 269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ferrone CR, Levine DA, Tang LH, et al. BRCA germline mutations in Jewish patients with pancreatic adenocarcinoma. J Clin Oncol 2009;27:433–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hahn SA, Greenhalf B, Ellis I, et al. BRCA2 germline mutations in familial pancreatic carcinoma. J Natl Cancer Inst 2003;95:214–21. [DOI] [PubMed] [Google Scholar]
- [29].Narod SA, Neuhausen S, Vichodez G, et al. Rapid progression of prostate cancer in men with a BRCA2 mutation. Br J Cancer 2008;99:371–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Akbari MR, Wallis CJ, Toi A, et al. The impact of a BRCA2 mutation on mortality from screen-detected prostate cancer. Br J Cancer 2014;111:1238–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Castro E, Goh C, Leongamornlert D, et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol 2015;68:186–93. [DOI] [PubMed] [Google Scholar]
- [32].Lynch HT, Lynch PM, Lanspa SJ, Snyder CL, Lynch JF, Boland CR. Review of the Lynch syndrome: history, molecular genetics, screening, differential diagnosis, and medicolegal ramifications. Clin Genet 2009;76:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Pino MS, Mino-Kenudson M, Wildemore BM, et al. Deficient DNA mismatch repair is common in Lynch syndrome-associated colorectal adenomas. J Mol Diagn 2009;11:238–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Balmana J, Stockwell DH, Steyerberg EW, et al. Prediction of MLH1 and MSH2 mutations in Lynch syndrome. JAMA 2006;296:1469–78. [DOI] [PubMed] [Google Scholar]
- [35].Barrow E, Robinson L, Alduaij W, et al. Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. Clin Genet 2009;75:141–9. [DOI] [PubMed] [Google Scholar]
- [36].Kempers MJ, Kuiper RP, Ockeloen CW, et al. Risk of colorectal and endometrial cancers in EPCAM deletion-positive Lynch syndrome: a cohort study. Lancet Oncol 2011;12:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Ligtenberg MJ, Kuiper RP, Geurts van KA, Hoogerbrugge N. EPCAM deletion carriers constitute a unique subgroup of Lynch syndrome patients. Fam Cancer 2013;12:169–74. [DOI] [PubMed] [Google Scholar]
- [38].Raymond VM, Mukherjee B, Wang F, et al. Elevated risk of prostate cancer among men with Lynch syndrome. J Clin Oncol 2013;31:1713–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Bauer CM, Ray AM, Halstead-Nussloch BA, et al. Hereditary prostate cancer as a feature of Lynch syndrome. Fam Cancer 2011;10:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Domchek SM, Bradbury A, Garber JE, Offit K, Robson ME. Multiplex genetic testing for cancer susceptibility: out on the high wire without a net? J Clin Oncol 2013;31:1267–70. [DOI] [PubMed] [Google Scholar]
- [41].Ewing CM, Ray AM, Lange EM, et al. Germline mutations in HOXB13 and prostate-cancer risk. N Engl J Med 2012;366:141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Xu J, Lange EM, Lu L, et al. HOXB13 is a susceptibility gene for prostate cancer: results from the International Consortium for Prostate Cancer Genetics (ICPCG). Hum Genet 2013;132(1):5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Chen Z, Greenwood C, Isaacs WB, et al. The G84E mutation of HOXB13 is associated with increased risk for prostate cancer: results from the REDUCE trial. Carcinogenesis 2013;34:1260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Shang Z, Zhu S, Zhang H, Li L, Niu Y. Germline homeobox B13 (HOXB13) G84E mutation and prostate cancer risk in European descendats: a meta-analysis of 24 213 cases and 73 631 controls. Eur Urol 2013;640:173–6. [DOI] [PubMed] [Google Scholar]
- [45].Handorf E, Crumpler N, Gross L, Giri VN. Prevalence of the HOXB13 G84E mutation among unaffected men with a family history of prostate cancer. J Genet Couns 2014;23:371–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Laitinen VH, Wahlfors T, Saaristo L, et al. HOXB13 G84E mutation in Finland; population-based analysis of prostate, breast and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 2013;22(3):452–60. [DOI] [PubMed] [Google Scholar]
- [47].Witte JS, Mefford J, Plummer SJ, et al. HOXB13 mutation and prostate cancer: studies of siblings and aggressive disease. Cancer Epidemiol Biomarkers Prev 2013;22(4):675–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Stott-Miller M, Karyadi DM, Smith T, et al. HOXB13 mutations in a population-based, case-control study of prostate cancer. Prostate 2013;73 (6):634–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Alanee S, Shah S, Vijai J, et al. Prevalence of HOXB13 mutation in a population of Ashkenazi Jewish men treated for prostate cancer. Fam Cancer 2013;12:597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kote-Jarai Z, Mikropoulos C, Leongamornlert DA, et al. Prevalence of the HOXB13 G84E germline mutation in British men and correlation with prostate cancer risk, tumour characteristics and clinical outcomes. Ann Oncol 2015;26:756–61. [DOI] [PubMed] [Google Scholar]
- [51].Macinnis RJ, Severi G, Baglietto L, et al. Population-based estimate of prostate cancer risk for carriers of the HOXB13 missense mutation G84E. PLoS One 2013;8:e54727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Karlsson R, Aly M, Clements M, et al. A population-based assessment of germline HOXB13 G84E mutation and prostate cancer risk. Eur Urol 2014;65:169–76. [DOI] [PubMed] [Google Scholar]
- [53].Giusti RM, Rutter JL, Duray PH, et al. A two-fold increase in BRCA mutation-related prostate cancer among Ashkenazi Israelis is not associated with distinctive histopathology. J Med Genet 2003;40:787–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Kirchhoff T, Satagopan JM, Kauff ND, et al. Frequency of BRCA1 and BRCA2 mutations in unselected Ashkenazi Jewish patients with colorectal cancer. J Natl Cancer Inst 2004;96:68–70. [DOI] [PubMed] [Google Scholar]
- [55].Agalliu I, Gern R, Leanza S, Burk RD. Associations of high-grade prostate cancer with BRCA1 and BRCA2 founder mutations. Clin.Cancer Res 2009;15:1112–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Gallagher DJ, Gaudet MM, Pal P, et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin Cancer Res 2010;16:2115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Kote-Jarai Z, Leongamornlert D, Saunders E, et al. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer 2011;105:1230–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Cybulski C, Wokolorczyk D, Kluzniak W, et al. An inherited NBN mutation is associated with poor prognosis prostate cancer. Br J Cancer 2013;108:461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Erkko H, Xia B, Nikkila J, et al. A recurrent mutation in PALB2 in Finnish cancer families. Nature 2007;446:316–9. [DOI] [PubMed] [Google Scholar]
- [60].Tischkowitz M, Sabbaghian N, Ray AM, Lange EM, Foulkes WD, Cooney KA. Analysis of the gene coding for the BRCA2-interacting protein PALB2 in hereditary prostate cancer. Prostate 2008;68:675–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Cybulski C, Gorski B, Debniak T, et al. NBS1 is a prostate cancer susceptibility gene. Cancer Res 2004;64:1215–9. [DOI] [PubMed] [Google Scholar]
- [62].Mateo J, Carreira S, Sandhu S, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med 2015;373:1697–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Robinson D, Van Allen EM, Wu YM, et al. Integrative clinical genomics of advanced prostate cancer. Cell 2015;161:1215–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Bambury RM, Gallagher DJ. Prostate cancer: germline prediction for a commonly variable malignancy. BJU Int 2012;110:E809–18. [DOI] [PubMed] [Google Scholar]
- [65].Al Olama AA, Kote-Jarai Z, Berndt SI, et al. A meta-analysis of 87,040 individuals identifies 23 new susceptibility loci for prostate cancer. Nat Genet 2014;46:1103–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Hindorff LA, MacArthur J, (European Bioinformatics Institute), Morales J (European Bioinformatics Institute), et al. A catalog of published genome-wide association studies. Available at: www.genome.gov/gwastudies. Accessed December 27, 2016.
- [67].Eeles R, Goh C, Castro E, et al. The genetic epidemiology of prostate cancer and its clinical implications. Nat Rev Urol 2014;11:18–31. [DOI] [PubMed] [Google Scholar]
- [68].National Cancer Institute PDQ Cancer Information Summaries: Genetics. Available at: https://www.cancer.gov/publicaitons/pdq/information-summaries/genetics.
- [69].Hazelett DJ, Rhie SK, Gaddis M, et al. Comprehensive functional annotation of 77 prostate cancer risk loci. PLoS Genet 2014;10:e1004102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Szulkin R, Karlsson R, Whitington T, et al. Genome-wide association study of prostate cancer-specific survival. Cancer Epidemiol Biomarkers Prev 2015;24:1796–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Lindstrom S, Schumacher FR, Cox D, et al. Common genetic variants in prostate cancer risk prediction—results from the NCI Breast and Prostate Cancer Cohort Consortium (BPC3). Cancer Epidemiol.Biomarkers Prev 2012;21:437–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Nordstrom T, Aly M, Eklund M, Egevad L, Gronberg H. A genetic score can identify men at high risk for prostate cancer among men with prostate-specific antigen of 1–3 ng/ml. Eur Urol 2014;65:1184–90. [DOI] [PubMed] [Google Scholar]
- [73].Little J, Wilson B, Carter R, et al. Multigene panels in prostate cancer risk assessment. Evid Rep Technol Assess 2012:1–166. [PMC free article] [PubMed] [Google Scholar]
- [74].Park JH, Gail MH, Greene MH, Chatterjee N. Potential usefulness of single nucleotide polymorphisms to identify persons at high cancer risk: an evaluation of seven common cancers. J Clin Oncol 2012;30:2157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines), Genetic/familial high-risk assessment: breast and ovarian (version 2.2016). 2012. Available at: www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf [December 27, 2015].
- [76].Hussein S, Satturwar S, Van der Kwast T. Young-age prostate cancer. J Clin Pathol 2015;68:511–5. [DOI] [PubMed] [Google Scholar]
- [77].Smith SC, Palanisamy N, Zuhlke KA, et al. HOXB13 G84E-related familial prostate cancers: a clinical, histologic, and molecular survey. Am J Surg Pathol 2014;38:615–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Moyer VA. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2012;157:120–34. [DOI] [PubMed] [Google Scholar]
- [79].Wolf AM, Wender RC, Etzioni RB, et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin 2010;60:70–98. [DOI] [PubMed] [Google Scholar]
- [80].Carter HB, Albertsen PC, Barry MJ, et al. Early detection of prostate cancer: AUA Guideline. J Urol 2013;190:419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Prostate Cancer Prevention and Early Detection. American Cancer Society; Available at: www.cancer.org/cancer/prostatecancer. Accessed December 15, 2015. [Google Scholar]
- [82].Carroll PR, Parsons JK, Andriole G, et al. Prostate cancer early detection, version 2.2015. J Natl Compr Cancer Netw 2015;13:1534–61. [DOI] [PubMed] [Google Scholar]
- [83].Bancroft EK, Page EC, Castro E, et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol 2014;66:489–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Wiggans AJ, Cass GK, Bryant A, Lawrie TA, Morrison J. Poly(ADP-ribose) polymerase (PARP) inhibitors for the treatment of ovarian cancer. Cochrane Database Syst Rev 2015:5CD007929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Oza AM, Cibula D, Benzaquen AO, et al. Olaparib combined with chemotherapy for recurrent platinum-sensitive ovarian cancer: a randomised phase 2 trial. Lancet Oncol 2015;16:87–97. [DOI] [PubMed] [Google Scholar]
- [86].Gallagher DJ, Cronin AM, Milowsky MI, et al. Germline BRCA mutation does not prevent response to taxane-based therapy for the treatment of castration-resistant prostate cancer. BJU Int 2012;109:713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Bratt O, Loman N. Clinical management of prostate cancer in men with BRCA mutations. Eur Urol 2015;68:194–5. [DOI] [PubMed] [Google Scholar]
- [88].Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst 1999;91:1310–6. [DOI] [PubMed] [Google Scholar]
- [89].Thompson D, Easton D. Variation in cancer risks, by mutation position, in BRCA2 mutation carriers. Am J Hum Genet 2001;68:410–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Thompson D, Easton DF. Cancer Incidence in BRCA1 mutation carriers. J Natl Cancer Inst 2002;94:1358–65. [DOI] [PubMed] [Google Scholar]
- [91].Leongamornlert D, Mahmud N, Tymrakiewicz M, et al. Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer 2012;106:1697–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Eerola H, Pukkala E, Pyrhonen S, Blomqvist C, Sankila R, Nevanlinna H. Risk of cancer in BRCA1 and BRCA2 mutation-positive and -negative breast cancer families (Finland). Cancer Causes Control 2001;12:739–46. [DOI] [PubMed] [Google Scholar]
- [93].Kirchhoff T, Kauff ND, Mitra N, et al. BRCA mutations and risk of prostate cancer in Ashkenazi Jews. Clin Cancer Res 2004;10:2918–21. [DOI] [PubMed] [Google Scholar]
- [94].Agalliu I, Karlins E, Kwon EM, et al. Rare germline mutations in the BRCA2 gene are associated with early-onset prostate cancer. Br J Cancer 2007;97:826–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Edwards SM, Evans DG, Hope Q, et al. Prostate cancer in BRCA2 germline mutation carriers is associated with poorer prognosis. Br J Cancer 2010;103:918–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Tryggvadottir L, Vidarsdottir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst 2007;99:929–35. [DOI] [PubMed] [Google Scholar]
- [97].Thorne H, Willems AJ, Niedermayr E, et al. Decreased prostate cancer-specific survival of men with BRCA2 mutations from multiple breast cancer families. Cancer Prev Res (Phila) 2011;4:1002–10. [DOI] [PubMed] [Google Scholar]
- [98].Ryan S, Jenkins MA, Win AK. Risk of prostate cancer in Lynch syndrome: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 2014;23:437–49. [DOI] [PubMed] [Google Scholar]
- [99].Beebe-Dimmer JL, Isaacs WB, Zuhlke KA, et al. Prevalence of the HOXB13 G84E prostate cancer risk allele in men treated with radical prostatectomy. BJU Int 2014;113:830–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-repair gene mutations in ment with metstatic prostate cancer. N Engl KJ Med 2016;375 (5):443–53. [DOI] [PMC free article] [PubMed] [Google Scholar]