Abstract
BACKGROUND:
Smoking is associated with various systemic conditions and contributes to a huge financial burden to economies around the world.
AIM:
The study aimed to evaluate global data about the prevalence of tobacco use among male and female adolescents and to discuss smoking-related oral complications.
METHODS:
The prevalence data of tobacco use among adolescents (13-15 years) was retrieved from the World Health Organization (Global Health Observatory). The World Bank’s statistics about gross national income (GNI) per capita were used to categorise low-income, lower-middle-income, upper-middle-income, and high-income countries. PubMed, Web of Science, Scopus, and Embase databases were searched to gather updated evidence about the adverse consequences of smoking on oral health among adolescents.
RESULTS:
The prevalence of tobacco use was 19.33%, and there were 23.29% of male and 15.35% female smoker adolescents in 133 countries (p < 0.001). The highest prevalence of tobacco use in male (24.76%) and female (19.4) adolescents was found in high-income countries. Significantly higher proportions of male adolescents were smokers than female counterparts in low-income, lower-middle-income, and upper-middle-income (p < 0.001). However, there were no statistically significant differences in tobacco use between male and female adolescents in high-income countries. Low-income countries had the lowest prevalence (14.95%) of tobacco use, while high-income countries had the highest prevalence estimates (22.08). Gingivitis (72.8%), gingival bleeding (51.2%), oral malodor or halitosis (39.6%) is common oral conditions among smoker adolescents. Smoking habit is significantly associated with dental caries, periodontal disease, hairy tongue, smoking-related melanosis, and hyperkeratosis among adolescents.
CONCLUSION:
There was a high prevalence of tobacco use among male and female adolescents around the globe. Available evidence suggests a strong association between smoking and compromised oral health among adolescents. Globally, measures should be taken to prevent and control the menace of tobacco use to reduce systemic and oral complications.
Keywords: Tobacco use, Oral health conditions, Adolescence, Global prevalence, Cigarette smoking
Introduction
Exposure to tobacco is associated with increased morbidity and mortality among children around the world [1]. Smoking contributes to increased risk of asthma, bronchitis, tuberculosis, inflammatory bowel disease, and leukaemia in children [1]. Moreover, children exposed to second-hand smoke may demonstrate structural and functional impairment in arteries that can lead to premature atherosclerosis and adverse long-term effects on the cardiovascular system [2]. Economic burden of smoking is enormous on individuals and healthcare systems. A recent study found that the economic cost of smoking was US$ 1436 billion around the globe in 2012 (equal to 1.8% of the annual gross domestic product of the world) which accounted for both direct health care expenditures and loss of productivity [3].
Cigarettes contain about 600 ingredients, they produce 7000 chemicals on combustion, and 69 of these chemicals can cause carcinomas. Nicotine is one of the toxic chemicals found in tobacco smoke [4]. It is documented that nicotine exposure among adolescents can affect the central nervous system and can cause cognitive functional and developmental impairment which can be of great concern considering the long-term use of tobacco [5]. Besides, adolescents may develop symptoms of dependence sooner and at lower levels of tobacco consumption [6]. There is a reciprocal relationship between diminished autonomy and frequency of smoking, and even the consumption of one cigarette can prompt the loss of autonomy in adolescents [7].
The initiation and establishment of smoking behaviour frequently occur during adolescence, and 9 of 10 children start smoking by the age of 18 years [8]. Globally, about 80,000 to 100,000 children use tobacco per day [9]. Several factors are associated with smoking which includes the influence of smoker peers and smoker parents, genetic factors, and low socioeconomic status [10]. Moreover, there is sufficient evidence about the role of tobacco advertisement in causing the onset and continuation of smoking among adolescents [8]. Smoking initiation in the early age is associated with regular smoking in adulthood [11]. This underscores the importance of controlling the habit of smoking during adolescence so that immediate and long-term complications can be prevented in adolescents and adults, respectively.
Oral conditions pose significant public health problems and can negatively affect systemic health and quality of life of individuals [12]. Globally, untreated oral conditions affected 2.5 billion people in 1990 which rose to 3.5 in 2015 [13]. According to the Global Burden of Disease Study (2017), oral conditions accounted for 1.83 million disability-adjusted life-years, an increase of 21.4 % during the past decade (2007-2017) [14]. It was estimated that the cost of dental treatment was $102 billion and 1.6 million school days were missed because of acute dental conditions in 2009 in the U.S. [8].
There is widespread use of tobacco among adolescents which enormously contributes to a high burden of oral and systemic diseases. Therefore, the present review aimed to evaluate global data about the prevalence of tobacco use during adolescence and to discuss oral complications commonly seen among smoker adolescents. The review utilised most updated evidence about the adverse effects of smoking on oral health among adolescents. The information presented in the review is expected to benefit healthcare professionals and other stakeholders so that they familiarise with the global smoking trends and its negative impacts on oral health. Their contribution in raising awareness is critical to preventing smoking-related oral and systemic complications during adolescence and long-term adverse effects in adulthood.
Methods
Data about the prevalence of tobacco use (including smoking cigarettes, oral tobacco, and snuff) among adolescents (13-15 years) were retrieved from the Global Health Observatory, the World Health Organization [15]. Data were collected from 133 countries since 2007. Many of these countries have data collected in multiple years (more than one data), however latest data were used. The countries with data collected in 2006 and beyond were excluded from the study. To evaluate the ecological impact of the income of countries (Gross national income (GNI) per capita) on the prevalence of tobacco use, we compared data among low-income, lower-middle-income, upper-middle-income, and high-income countries. According to the World Bank (2017), the countries with a GNI per capita of ≤ $1,025 are defined as low-income countries; those with a GNI per capita between $1,026 and $4,035 as lower-middle-income countries, those with a GNI per capita between $4,036 and $12,475 as upper-middle-income countries, and those with a GNI per capita of ≥ $12,476 as high-income countries.
For this review, PubMed (Medline) was searched to retrieve studies about tobacco use and its impact on oral tissues. Using the library resources of Imam Abdulrahman Bin Faisal University, Scopus and Web of Science databases were searched. Search through Embase was also carried out to ensure a comprehensive search of related studies. Further, the reference lists of retrieved studies were searched to obtain more information regarding the topic of the review. The literature review gathered recent studies, mostly published during the last ten years, to provide updated information. Data from animal studies, case series, and case reports were excluded. Medical Subject Headings (MeSH)/keywords such as “smoking”, “tobacco”, “nicotine”, “caries”, “decay”, “cavities”, “gingival”, “periodontal”, “halitosis”, “oral malodor”, “cancers”, “carcinoma”, “oral health”, and “oral conditions,” were used to retrieve relevant studies.
Statistical analyses of the data were performed using SPSS Version 22.0 (IBM Corp. Armonk, NY, USA). Mann Whitney U test was conducted to make comparisons between the prevalence of tobacco use in male and female adolescents. Kruskal Wallis test compared the prevalence data among low-income, lower-middle-income, upper-middle-income, and high-income-countries. A significance level of p < 0.05 was used.
Results
There were 28 low-income, 76 lower-middle-income, 48 upper-middle-income, and 33 high-income countries included in the present review. The prevalence of tobacco use in adolescents in low-income countries is presented in Figure 1.
Figure 1.
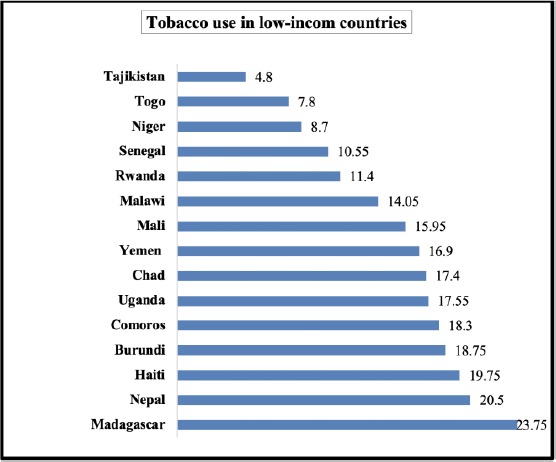
The prevalence of tobacco use in adolescents in low-income countries
Among low-income countries, tobacco use was most frequent in Madagascar (23.75%), followed by Nepal (20.5%), and Haiti (19.75%) whereas 4.8% of adolescents in Tajikistan used tobacco. About half the adolescents (47.85%) in Papua New Guinea consumed tobacco which was highest among lower-middle-income countries. On the other hand, tobacco use was the least common in Vietnam (4%), Bangladesh (6%) and Cambodia (6.45%) (Figure 2).
Figure 2.

The prevalence of tobacco use in adolescents in lower-middle-income countries
Approximately one-quarter of adolescents in Tuvalu (37.15%), Lebanon (36.65%), and Tonga (36.45%) consumed tobacco in upper-middle-income countries. Montenegro (6.25), China (6.7%), and Azerbaijan (6.75%) had the lowest consumption of tobacco in upper-middle-income countries (Figure 3).
Figure 3.
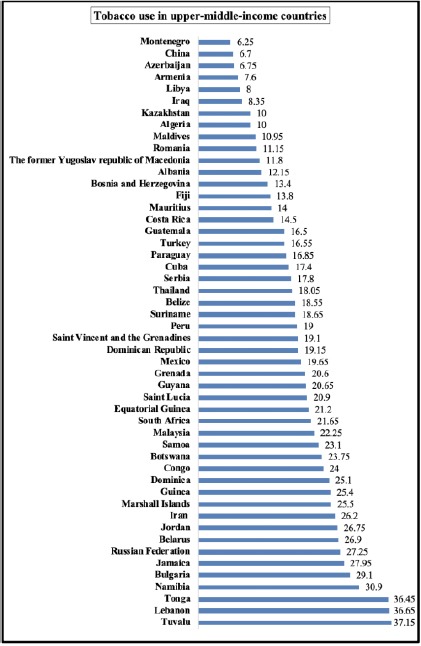
The prevalence of tobacco use in adolescents in upper-middle-income countries
Oman had the lowest prevalence of tobacco use (3.3%), whereas Palau demonstrated the highest distribution of tobacco use in adolescents in high-income countries (Figure 4).
Figure 4.
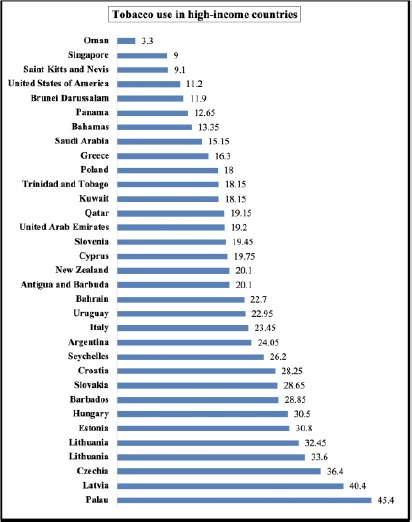
The prevalence of tobacco use in adolescents in high-income countries
The prevalence of tobacco use in adolescents in 133 countries was 19.33%, and it ranged from 1.5% to 65.5%. There were 23.29% male and 15.35% female smoker adolescents in these countries (p < 0.001). In low-income countries, 18.48% of male and 11.41% of female adolescents consumed tobacco (p 0.006). The prevalence of tobacco use was higher in males (24.18%) than females (13.37%) in lower-middle-income countries (p < 0.001). Upper-middle-income countries had prevalence estimates tobacco use in 22.97% of male and 15.29% of female adolescents (p < 0.001). Adolescents in high-income countries showed no statistically significant differences in the prevalence of tobacco use (p 0.052) (Table 1).
Table 1.
Tobacco use among male and female adolescents (13-15 years) in 133 countries
| Countries based on GNI | Number of countries | Prevalence of tobacco use in male adolescents (Percentages) | Prevalence of tobacco use in female adolescents (Percentages) | p-value |
|---|---|---|---|---|
| Low-Income Countries | 28 | 18.48 Min = 6.8 Max = 33.2 | 11.41 Min = 2.8 Max = 19.2 | 0.006 |
| Lower-Middle-Income Countries | 76 | 24.18 Min = 6.5 Max = 65.5 | 13.37 Min = 1.5 Max = 40.3 | < 0.001 |
| Upper-Middle-Income Countries | 48 | 22.97 Min = 6.6 Max = 44.9 | 15.29 Min = 2.1 Max = 32.7 | < 0.001 |
| High-Income Countries | 33 | 24.76 Min = 4.9 Max = 54.1 | 19.4 Min = 1.7 Max = 41.4 | 0.052 |
| Total | 133 | 23.29 | 15.35 | < 0.001 |
Table 2.
Description of 5 A’s Model
| 5 A’s | Description |
|---|---|
| Ask | Health care providers should “ASK” their patients about using tobacco and identify and document tobacco users in each visit. |
| Advise | They should strongly “ADVISE” tobacco users to quit smoking. |
| Assess | Smoker’s readiness to quitting should be “ASSESSED” health care professionals. |
| Assist | The tobacco users should be “ASSISTED” by providing them with a smoking quit plan. |
| Arrange | A follow-up visit or a referral to a specialist should be “ARRANGED” to identify problems and challenges and provide support. |
Table 3.
Description of 5 R’s Model
| 5 R’s | Description |
|---|---|
| Relevance | When using “RELEVANCE”, health care providers should describe that quitting smoking is personally relevant to tobacco users concerning diseases, health risks, and family or social concerns. |
| Risks | Health care providers should help individuals identify negative consequences (RISKS) associated with the use of tobacco, such as acute risks, long-term risks, and environmental risks. |
| Rewards | The “REWARDS” are potentially relevant advantages of quitting, such as better health outcomes, improved social interactions, and economic benefits. Health care providers should encourage tobacco users to recognize the benefits of quitting. |
| Road Blocks | They should explain barriers (ROADBLOCKS) to quitting to their patients which may include dependence, fear of failure, and lack of support. |
| Repetition | “REPETITION” involves repeating motivational counselling intervention if the patient does not demonstrate readiness to quit smoking. |
Discussion
The comparison of tobacco use among different countries is shown in Figure 5. Low-income countries had the lowest prevalence (14.95%) of tobacco use, while high-income countries had the highest prevalence estimates (22.08). There were statistically significant differences in the prevalence of tobacco use among low-income, lower-middle-income, upper-middle-income, and high-income countries (p 0.008).
Figure 5.
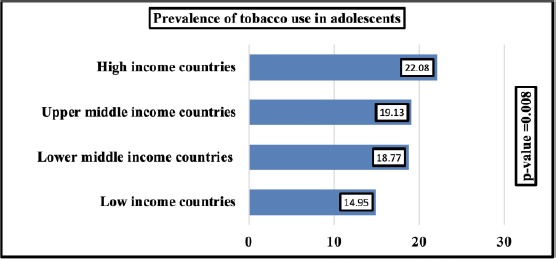
Differences in the prevalence of tobacco use in 133 countries according to their income
Mechanisms of Adverse Effects of Tobacco Use on Oral Health
Several mechanisms are responsible for the adverse effects of tobacco use on oral health. Tobacco smoke is a mixture of thousands of complex chemicals, many of which are poisonous and are responsible for the chemically mediated disease, including cancers [16]. Cigarette smoking is associated with alterations in oral microbial profile. A recent study showed that oral microbiome was significantly different in smokers compared with non-smokers. The smokers demonstrated the depletion of Actinobacillus, Neisseria, Aggregatibacter, Eikenella, Haemophilus, Lautropia, Fusobacterium, Leptotrichia, and Cyanobacteria and abundance of Treponema, and Mycoplasma [17]. Oral microorganisms accumulate to form biofilm on the tooth surface and subgingival sulcus, and smokers have been shown to demonstrate diverse microbial colonisation of biofilms than non-smokers, thus suggesting the role of smoking in promoting bacterial acquisition and colonisation in the biofilm [18].
Compared with non-smokers, smokers exhibit increased pathogenic species in marginal and subgingival biofilms and greater pro-inflammatory response [19]. It is well recognised that increased susceptibility of smokers to oral infections is because smoking promotes virulence of microorganisms and increases antibiotic resistance [20]. Besides, the adverse health effects of smoking can be related to potential microbial pathogens present in cigarettes. A variety of cigarette brands contain microorganisms which include Acinetobacter, Bacillus, Staphylococcus species, Clostridium, Serratia, and Pseudomonas [20].
Health consequences of tobacco consumption are related to its suppressive effects on the immune system. Exposure to tobacco smoke plays an important role in the production of immune and inflammatory mediators [21]. Similarly, provocation of oxidative stress because of smoke can result in dysregulation of the immune system to cause autoimmunity. Smoke can also produce autoantibodies and contribute to autoreactivity in some autoimmune diseases [22]. Smoking is also known to cause temperature variations and alterations in the pH in the oral cavity, which can be attributed to increased incidence of oral cancers. High intraoral temperature variations are associated with certain oral conditions and act as co-carcinogens. Also, chemicals present in tobacco are responsible for high alkaline pH which promotes the absorption of nicotine in the oral mucosal membrane [23]. Tobacco use compromises wound healing by inducing changes in connective and vascular tissues, reducing the supply of oxygen and nutrient to tissues, and decreasing collagen synthesis [24].
Common Oral Conditions among Smoker Adolescents
Smoker adolescents are predisposed to increased risk of oral conditions which include gingivitis and gingival bleeding, oral malodor, staining, dental caries, oral mucosal lesions, periodontal disease, dryness of mouth, and sensitivity.
Gingivitis and bleeding gums
Common adverse oral health consequences among adolescents include gingivitis, including bleeding gums and tooth staining [25]. Gingivitis is dental plaque-induced inflammation of gingiva without periodontal attachment loss or alveolar bone loss. However, persistent gingivitis is a risk factor for attachment loss and tooth loss later in life [26]. A recent study showed a high prevalence rate of gingivitis (72.8%) among adolescents, and male gender, poor oral hygiene, and smoking were significantly associated with gingivitis. It was also found that the smokers were 2.26 times more likely to have gingivitis than non-smokers [27]. A previous study also showed that 51.2% of adolescent smokers exhibited gingival bleeding than 33.1% of non-smokers (p < 0.02) [25]. It is documented that poor oral hygiene results in plaque accumulation which causes gingival inflammation and bleeding gums [27].
Oral Malodor
Oral malodor, also known as halitosis has negative effects on self-confidence, self-esteem, professional life, and social interaction. There is a high prevalence of oral malodor among school children. Yokoyama et al. detected oral malodor in 39.6% of senior high school children [28]. Oral malodor prevalence of 23.6% in adolescents was observed by Kim et al., [29]. Tobacco use is considered an extrinsic cause of oral malodor and smoking habit is known to correlate with the presence of oral malodor in youth [30]. Nevertheless, some studies did not find a significant association between smoking and oral malodor in adolescents and youth [29], [31].
Dental caries
The literature consistently shows an association between smoking and increased risk of caries during adolescence [32], [33], [34]. Tobacco consumption (tobacco and smokeless tobacco) is a significant risk factor for caries development. A population-based longitudinal study of 10,068 adolescents (2006-2012) found that tobacco users had significantly higher mean value of decay, missing, and filled surface (DMFS = 1.8) than never tobacco users (mean DMFS = 1.2), and tobacco use was significantly associated with increased caries incidence [32]. Another epidemiological study of 20,703 schoolchildren reported an association between household smoking and increased risk of dental caries. The study also demonstrated a significant dose-response relationship between household smoking and prevalence of decayed and or filled teeth [33]. Passive tobacco exposure also contributes to the development of caries in adolescents. A recent meta-analysis of 21 studies found a moderate association between passive smoking and dental caries in children and adolescents [34].
Periodontal Disease
According to the American Academy of Periodontology, several periodontal diseases affect adolescents, although their prevalence is higher in adults than adolescents [35]. Smoking negatively affects periodontal health by causing degradation of periodontal tissues. A study of adolescents found that smoker participants had significantly more periodontal pockets of ≥ 4 mm than non-smokers. Also, the study identified significantly higher root calculus in smokers than non-smoker adolescents [36]. Available evidence suggests that tobacco consumption can affect inflammatory biomarkers in saliva which have been successfully used as an alternative to evaluating periodontal health. It was reported that smoking increased the risk of periodontal disease among adolescents by lowering salivary biomarkers like matrix metalloproteinase (MMP)-8 and male adolescents demonstrated more susceptibility to periodontitis than female teenagers [37].
Oral Mucosal Lesions
The studies documented high prevalence (26.2%-28%) of oral mucosal lesions in adolescents [38], [39]. Male adolescents were found to have a high prevalence of oral mucosal lesions than females [39]. Aphthous ulcers, traumatic ulcerations, herpes stomatitis, angular cheilitis, geographic tongue, and candidiasis are the most common types of oral mucosal lesions during adolescence [38], [40]. A recent study of adolescents observed a significant association between smoking habit and hairy tongue, smoking-related melanosis, and hyperkeratosis. The authors suggested that smoking can induce alterations in oral microbial profile, thickening of oral mucous membrane, and extravasation of melanocytic pigment which may lead to oral mucosal lesions [41]. A study of 17,027 schoolchildren showed that about 1.5% had smokeless tobacco lesions which were more common in male than female students. The study also demonstrated a dose-response relationship between tobacco use and smokeless tobacco lesions, and snuff was strongly associated with increased odds (odds ratio 18.4) of these lesions [42].
Dryness and hypersensitivity
A significantly higher proportion of smokers were shown to have tooth sensitivity and dryness of the mouth than non-smokers [43]. Evidence suggests that smoking reduces salivary flow which predisposes individuals to dryness of the mouth or xerostomia [44]. A previous study also showed a significant difference in the prevalence of xerostomia among smokers (39%) and non-smokers (12%) [45]. Similarly, it was reported that 37% of smokers had xerostomia compared with 13% of non-smokers [44]. It is well-known that dryness of the mouth can cause inflammation of oral tissues including salivary glands, and can promote caries development, oral malodor, calculus formation, and fungal infection [45], [46].
Oral pre-cancerous lesions and cancers
Tobacco smoking contributes to the formation of oral pre-cancerous lesions, such as leukoplakia and erythroplakia [24]. Oral cancers involve carcinomas of lip, tongue, mouth, and pharynx, and are considered the sixth most prevalent cancers around the world [47]. Globally, 128,000 patients with oral cancer die annually [48]. Men have a higher incidence of oral cancer than women, and tobacco use is a major contributor to oral cancer [49]. The incidence of lip, oral cavity, and pharyngeal cancers was 3.8% (529,500 cases) of all cancers in 2012, and it was predicted that the number of these cancers would increase to 856,000 cases in 2035 representing 62% increase in 23 years [48].
Although childhood cancers are rare, however, there is a rise in the number of new cancer cases of oral cavity and pharynx in adolescents which are associated with human papillomavirus (HPV) infection in addition to tobacco use [50]. Since smoking is widely prevalent among adolescents, and adverse health consequences of oral cancers are huge and far-reaching. Therefore, health professionals should be aware of the signs and symptoms of oral cancers so that early detection and treatment should be started as early as possible to reduce morbidity and mortality later in life. It is the responsibility of healthcare providers to provide counselling to adolescents and their patients about the hazardous consequences of smoking on oral and systemic health in daily practice. A previous study found that the adolescents who were aware of the adverse effects of smoking on oral health had 22% – 47% lesser chances of smoking than those who were unaware of negative smoking consequences [51].
Prevention of smoking
The WHO suggested the 5 A’s model that helps individuals avoid exposure to secondhand smoke and prepares individuals to quit smoking, and the 5R’s model that increases the motivation of quitting [52]. More than 80% of smokers approach primary health care providers each year, which place them in a central position to advise smokers to quit tobacco use. The 5 A’s model (Ask, Advise, Assess, Assist, Arrange) involves using actions and strategies to provide advice to tobacco users [52].
The 5 R’s model (Relevance, Risks, Rewards, Roadblocks, and Repetition) provides strategies that can be used in motivational counselling for those individuals who are not ready to quit tobacco use.[52]
Conclusion and recommendations
The study found a high prevalence of tobacco use among male and female adolescents in 133 countries. High-income countries had the highest prevalence of smoker adolescents, while low-income countries had the lowest prevalence of tobacco use. A significantly higher proportion of male than female adolescents used tobacco in low-income, lower-middle-income, and upper-middle-income countries. However, male and female smoker adolescents in high-income countries showed no significant differences, suggesting that both male and female adolescents were almost equally exposed to tobacco in high-income countries.
The smoker adolescents exhibit a high burden of gingivitis, gingival bleeding, malodor (halitosis), and tooth staining. There is a significant association between smoking and increased incidence of caries, calculus, periodontal pockets, oral mucosal lesions among adolescents. Healthcare professionals, decision-makers in healthcare agencies, and other stakeholders should be aware of the epidemic of smoking and associated systemic and oral health complications among adolescents. They should play their roles at the individual level and through collaborations in the prevention and control of smoking.
Medical and dental curricula should include strategies on smoking cessation in addition to the epidemiology of tobacco use and pathology of tobacco-related conditions. The health care professionals should use 5A’s and 5R’s models in their clinical practice to encourage quitting, and they should act as clinicians, educators, opinion makers, role models, researchers, and collaborators to help control tobacco epidemic and to improve the quality of life of adolescents.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.M Wilson K, Weis E. The epidemiology and health effects of tobacco smoke exposure. Current Pediatric Reviews. 2011;7(2):76–80. https://doi.org/10.2174/157339611795735594. [Google Scholar]
- 2.Raghuveer G, White DA, Hayman LL, et al. Cardiovascular consequences of childhood secondhand tobacco smoke exposure:prevailing evidence, burden, and racial and socioeconomic disparities:a scientific statement from the American Heart Association. Circulation. 2016;134(16):e336–e59. doi: 10.1161/CIR.0000000000000443. https://doi.org/10.1161/CIR.0000000000000443 PMid:27619923 PMCid:PMC5207215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodchild M, Nargis N, Tursan d'Espaignet E. Global economic cost of smoking-attributable diseases. Tob Control. 2018;27(1):58–64. doi: 10.1136/tobaccocontrol-2016-053305. https://doi.org/10.1136/tobaccocontrol-2016-053305 PMid:28138063 PMCid:PMC5801657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Lung Association Stop smoking. Smoking Facts. 2018. [accessed on 13 November 2018]. Available from: https://www.lung.org/stop-smoking/smoking-facts/whats-in-a-cigarette.html .
- 5.Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb Perspect Med. 2012;2(12):a012120. doi: 10.1101/cshperspect.a012120. https://doi.org/10.1101/cshperspect.a012120 PMid:22983224 PMCid:PMC3543069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiFranza JR, Savageau JA, Fletcher K, et al. Symptoms of tobacco dependence after brief intermittent use:the Development and Assessment of Nicotine Dependence in Youth-2 study. Arch Pediatr Adolesc Med. 2007;161(7):704–10. doi: 10.1001/archpedi.161.7.704. https://doi.org/10.1001/archpedi.161.7.704 PMid:17606835. [DOI] [PubMed] [Google Scholar]
- 7.Scragg R, Wellman RJ, Laugesen M, DiFranza JR. Diminished autonomy over tobacco can appear with the first cigarettes. Addict Behav. 2008;33(5):689–98. doi: 10.1016/j.addbeh.2007.12.002. https://doi.org/10.1016/j.addbeh.2007.12.002 PMid:18207651. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health and Human Services. The health consequences of smoking-50 years of progress:a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. p. 17. [Google Scholar]
- 9.Xi B, Liang Y, Liu Y, et al. Tobacco use and second-hand smoke exposure in young adolescents aged 12-15 years:data from 68 low-income and middle-income countries. Lancet Global Health. 2016;4(11):e795–e805. doi: 10.1016/S2214-109X(16)30187-5. https://doi.org/10.1016/S2214-109X(16)30187-5. [DOI] [PubMed] [Google Scholar]
- 10.Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General: US Surgeon General's Office Washington, DC. 2012 [Google Scholar]
- 11.Reidpath DD, Davey TM, Kadirvelu A, Soyiri IN, Allotey P. Does one cigarette make an adolescent smoker, and is it influenced by age and age of smoking initiation?Evidence of association from the U.S. Youth Risk Behavior Surveillance System (2011) Prev Med. 2014;59:37–41. doi: 10.1016/j.ypmed.2013.11.011. https://doi.org/10.1016/j.ypmed.2013.11.011 PMid:24270054. [DOI] [PubMed] [Google Scholar]
- 12.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Kassebaum NJ, Smith AGC, Bernabe E, et al. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries 1990-2015:A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J Dent Res. 2017;96(4):380–87. doi: 10.1177/0022034517693566. https://doi.org/10.1177/0022034517693566 PMid:28792274 PMCid:PMC5912207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–922. doi: 10.1016/S0140-6736(18)32335-3. https://doi.org/10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The World Health Organization. Global Health Observatory data repository. Tobacco use. 2018. [accessed on 16 November 2018]. Available from: http://apps.who.int/gho/data/node.main.65 .
- 16.Behera SN, Xian H, Balasubramanian R. Human health risk associated with exposure to toxic elements in mainstream and sidestream cigarette smoke. Sci Total Environ. 2014;472:947–56. doi: 10.1016/j.scitotenv.2013.11.063. https://doi.org/10.1016/j.scitotenv.2013.11.063 PMid:24342102. [DOI] [PubMed] [Google Scholar]
- 17.Valles Y, Inman CK, Peters BA, et al. Types of tobacco consumption and the oral microbiome in the United Arab Emirates Healthy Future (UAEHFS) Pilot Study. Sci Rep. 2018;8(1):11327. doi: 10.1038/s41598-018-29730-x. https://doi.org/10.1038/s41598-018-29730-x PMid:30054546 PMCid:PMC6063860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar PS, Matthews CR, Joshi V, de Jager M, Aspiras M. Tobacco smoking affects bacterial acquisition and colonization in oral biofilms. Infect Immun. 2011;79(11):4730–8. doi: 10.1128/IAI.05371-11. https://doi.org/10.1128/IAI.05371-11 PMid:21859855 PMCid:PMC3257914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joshi V, Matthews C, Aspiras M, et al. Smoking decreases structural and functional resilience in the subgingival ecosystem. J Clin Periodontol. 2014;41(11):1037–47. doi: 10.1111/jcpe.12300. https://doi.org/10.1111/jcpe.12300 PMid:25139209. [DOI] [PubMed] [Google Scholar]
- 20.Feldman C, Anderson R. Cigarette smoking and mechanisms of susceptibility to infections of the respiratory tract and other organ systems. J Infect. 2013;67(3):169–84. doi: 10.1016/j.jinf.2013.05.004. https://doi.org/10.1016/j.jinf.2013.05.004 PMid:23707875. [DOI] [PubMed] [Google Scholar]
- 21.Qiu F, Liang CL, Liu H, et al. Impacts of cigarette smoking on immune responsiveness:Up and down or upside down? Oncotarget. 2017;8(1):268–84. doi: 10.18632/oncotarget.13613. https://doi.org/10.18632/oncotarget.13613 PMid:27902485 PMCid:PMC5352117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perricone C, Versini M, Ben-Ami D, et al. Smoke and autoimmunity:The fire behind the disease. Autoimmun Rev. 2016;15(4):354–74. doi: 10.1016/j.autrev.2016.01.001. https://doi.org/10.1016/j.autrev.2016.01.001 PMid:26772647. [DOI] [PubMed] [Google Scholar]
- 23.Naveen-Kumar B, Tatapudi R, Sudhakara-Reddy R, et al. Various forms of tobacco usage and its associated oral mucosal lesions. J Clin Exp Dent. 2016;8(2):e172–7. doi: 10.4317/jced.52654. https://doi.org/10.4317/jced.52654 PMid:27034758 PMCid:PMC4808313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sham AS, Cheung LK, Jin LJ, Corbet EF. The effects of tobacco use on oral health. Hong Kong Med J. 2003;9(4):271–7. [PubMed] [Google Scholar]
- 25.Ayo-Yusuf OA, Van Den Borne B, Reddy PS, Van Wyk PJ, Severson HH. Longitudinal Association of Smoking-Related Attitude to Oral Health with Adolescents'Smoking Onset. J Public Health Dent. 2009;69(1):29–33. doi: 10.1111/j.1752-7325.2008.00090.x. https://doi.org/10.1111/j.1752-7325.2008.00090.x PMid:18662254. [DOI] [PubMed] [Google Scholar]
- 26.Lang NP, Schatzle MA, Loe H. Gingivitis as a risk factor in periodontal disease. J Clin Periodontol. 2009;36(10):3–8. doi: 10.1111/j.1600-051X.2009.01415.x. https://doi.org/10.1111/j.1600-051X.2009.01415.x PMid:19432625. [DOI] [PubMed] [Google Scholar]
- 27.Chrysanthakopoulos NA. Prevalence of gingivitis and associated factors in 13-16-year-old adolescents in Greece. European Journal of General Dentistry. 2016;5(2):58. https://doi.org/10.4103/2278-9626.179536. [Google Scholar]
- 28.Yokoyama S, Ohnuki M, Shinada K, et al. Oral malodor and related factors in Japanese senior high school students. J Sch Health. 2010;80(7):346–52. doi: 10.1111/j.1746-1561.2010.00512.x. https://doi.org/10.1111/j.1746-1561.2010.00512.x PMid:20591100. [DOI] [PubMed] [Google Scholar]
- 29.Kim SY, Sim S, Kim SG, Park B, Choi HG. Prevalence and Associated Factors of Subjective Halitosis in Korean Adolescents. PLoS One. 2015;10(10):e0140214. doi: 10.1371/journal.pone.0140214. https://doi.org/10.1371/journal.pone.0140214 PMid:26461837 PMCid:PMC4603949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Setia S, Pannu P, Gambhir RS, et al. Correlation of oral hygiene practices, smoking and oral health conditions with self perceived halitosis amongst undergraduate dental students. J Nat Sci Biol Med. 2014;5(1):67–72. doi: 10.4103/0976-9668.127291. https://doi.org/10.4103/0976-9668.127291 PMid:24678201 PMCid:PMC3961956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nazir MA, Almas K, Majeed MI. The prevalence of halitosis (oral malodor) and associated factors among dental students and interns, Lahore, Pakistan. Eur J Dent. 2017;11(4):480–85. doi: 10.4103/ejd.ejd_142_17. https://doi.org/10.4103/ejd.ejd_142_17 PMid:29279674 PMCid:PMC5727733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holmen A, Stromberg U, Magnusson K, Twetman S. Tobacco use and caries risk among adolescents--a longitudinal study in Sweden. BMC Oral Health. 2013;13:31. doi: 10.1186/1472-6831-13-31. https://doi.org/10.1186/1472-6831-13-31 PMid:23855639 PMCid:PMC3723799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanaka K, Miyake Y, Arakawa M, Sasaki S, Ohya Y. Household smoking and dental caries in schoolchildren:the Ryukyus Child Health Study. BMC Public Health. 2010;10:335. doi: 10.1186/1471-2458-10-335. https://doi.org/10.1186/1471-2458-10-335 PMid:20540808 PMCid:PMC2893097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzalez-Valero L, Montiel-Company JM, Bellot-Arcis C, et al. Association between passive tobacco exposure and caries in children and adolescents. A systematic review and meta-analysis. PLoS One. 2018;13(8):e0202497. doi: 10.1371/journal.pone.0202497. https://doi.org/10.1371/journal.pone.0202497 PMid:30114212 PMCid:PMC6095572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Academy of Periodontology-Research, Scicence and therapy Committee. Periodontal diseases of children and adolescents. Pediatr Dent. 2008;30(7):240–7. [PubMed] [Google Scholar]
- 36.Heikkinen AM, Pajukanta R, Pitkaniemi J, et al. The effect of smoking on periodontal health of 15- to 16-year-old adolescents. J Periodontol. 2008;79(11):2042–7. doi: 10.1902/jop.2008.080205. https://doi.org/10.1902/jop.2008.080205 PMid:18980511. [DOI] [PubMed] [Google Scholar]
- 37.Heikkinen AM, Sorsa T, Pitkaniemi J, et al. Smoking affects diagnostic salivary periodontal disease biomarker levels in adolescents. J Periodontol. 2010;81(9):1299–307. doi: 10.1902/jop.2010.090608. https://doi.org/10.1902/jop.2010.090608 PMid:20450405. [DOI] [PubMed] [Google Scholar]
- 38.Parlak AH, Koybasi S, Yavuz T, et al. Prevalence of oral lesions in 13- to 16-year-old students in Duzce, Turkey. Oral Dis. 2006;12(6):553–8. doi: 10.1111/j.1601-0825.2006.01235.x. https://doi.org/10.1111/j.1601-0825.2006.01235.x PMid:17054767. [DOI] [PubMed] [Google Scholar]
- 39.Jahanbani J, Morse DE, Alinejad H. Prevalence of oral lesions and normal variants of the oral mucosa in 12 to 15-year-old students in Tehran, Iran. Arch Iran Med. 2012;15(3):142–5. [PubMed] [Google Scholar]
- 40.Furlanetto DL, Crighton A, Topping GV. Differences in methodologies of measuring the prevalence of oral mucosal lesions in children and adolescents. Int J Paediatr Dent. 2006;16(1):31–9. doi: 10.1111/j.1365-263X.2006.00674.x. https://doi.org/10.1111/j.1365-263X.2006.00674.x PMid:16364090. [DOI] [PubMed] [Google Scholar]
- 41.Amadori F, Bardellini E, Conti G, Majorana A. Oral mucosal lesions in teenagers:a cross-sectional study. Ital J Pediatr. 2017;43(1):50. doi: 10.1186/s13052-017-0367-7. https://doi.org/10.1186/s13052-017-0367-7 PMid:28569171 PMCid:PMC5452358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomar SL, Winn DM, Swango PA, Giovino GA, Kleinman DV. Oral mucosal smokeless tobacco lesions among adolescents in the United States. J Dent Res. 1997;76(6):1277–86. doi: 10.1177/00220345970760060701. https://doi.org/10.1177/00220345970760060701 PMid:9168861. [DOI] [PubMed] [Google Scholar]
- 43.Al-Qurashi H, Al-Farea M, Al-Qurai T, et al. Comparison of oral hygiene practices and oral health problems among smoker and non-smoker male adolescents in the Eastern Province of Saudi Arabia. The Saudi Journal for Dental Research. 2016;7(2):106–11. https://doi.org/10.1016/j.sjdr.2016.04.002. [Google Scholar]
- 44.Dyasanoor S, Saddu SC. Association of Xerostomia and Assessment of Salivary Flow Using Modified Schirmer Test among Smokers and Healthy Individuals:A Preliminutesary Study. J Clin Diagn Res. 2014;8(1):211–3. doi: 10.7860/JCDR/2014/6650.3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rad M, Kakoie S, Niliye Brojeni F, Pourdamghan N. Effect of Long-term Smoking on Whole-mouth Salivary Flow Rate and Oral Health. J Dent Res Dent Clin Dent Prospects. 2010;4(4):110–4. doi: 10.5681/joddd.2010.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Petrusic N, Posavac M, Sabol I, Mravak-Stipetic M. The Effect of Tobacco Smoking on Salivation. Acta Stomatol Croat. 2015;49(4):309–15. doi: 10.15644/asc49/4/6. https://doi.org/10.15644/asc49/4/6 PMid:27688415 PMCid:PMC4945334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lopez E, Tudela R. Prevalence of Oral Cancer in Adolescents Related to Areca (Betel) Nut Chewing, Using Tobacco and Other Additives in Saipan, Northern Marianas Islands:A Review of Literature. Journal of Health Disparities Research & Practice. 2016:9. [Google Scholar]
- 48.Shield KD, Ferlay J, Jemal A, et al. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J Clin. 2017;67(1):51–64. doi: 10.3322/caac.21384. https://doi.org/10.3322/caac.21384 PMid:28076666. [DOI] [PubMed] [Google Scholar]
- 49.Tandon P, Dadhich A, Saluja H, Bawane S, Sachdeva S. The prevalence of squamous cell carcinoma in different sites of oral cavity at our Rural Health Care Centre in Loni, Maharashtra - a retrospective 10-year study. Contemp Oncol (Pozn) 2017;21(2):178–83. doi: 10.5114/wo.2017.68628. https://doi.org/10.5114/wo.2017.68628 PMid:28947890 PMCid:PMC5611509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bleyer A. Cancer of the oral cavity and pharynx in young females:increasing incidence, role of human papilloma virus, and lack of survival improvement. Semin Oncol. 2009;36(5):451–9. doi: 10.1053/j.seminoncol.2009.07.005. https://doi.org/10.1053/j.seminoncol.2009.07.005 PMid:19835740. [DOI] [PubMed] [Google Scholar]
- 51.Nazir MA, Almas K. Awareness about the effects of tobacco consumption on oral health and the possibility of smoking behavior among male Saudi schoolchildren. Eur J Dent. 2017;11(1):29–35. doi: 10.4103/ejd.ejd_300_16. https://doi.org/10.4103/ejd.ejd_300_16 PMid:28435362 PMCid:PMC5379831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The World Health Organization. Toolkit for delivering the 5A's and 5R's brief tobacco interventions in primary care. 2014. [accessed on 27 January 2019]. Available from: https://www.who.int/tobacco/publications/smoking_cessation/9789241506953/en/


