Abstract
Background
Acute kidney injury (AKI) is common in neonatal encephalopathy (NE) and is associated with worse outcomes. Our objectives were to determine the incidence, risk factors, and outcomes of AKI in infants with NE.
Methods
We performed a retrospective analysis of infants ≥ 34 weeks’ gestational age with a diagnosis of NE from the AWAKEN (Analysis of Worldwide Acute Kidney injury Epidemiology in Neonates) database. AKI was defined using the modified Kidney Disease Improving Global Outcomes criteria. Perinatal and postnatal factors were evaluated. Multivariate logistic and linear regression were performed.
Results
113 patients with NE were included. 41.6% (47) developed AKI. Being born outside the admitting institution (OR 4.3; 95% CI:1.2 – 14.8; p = 0.02), intrauterine growth restriction (OR: 10.3, 95% CI:1.1 – 100.5; p = 0.04) and meconium at delivery (OR: 2.8, 95% CI:1.04 – 7.7; p = 0.04) conferred increased odds of AKI. After controlling for confounders, infants with AKI stayed in the hospital an average of 8.5 days longer than infants without AKI (95% CI: 0.79 – 16.2 days; p = 0.03).
Conclusions
In this multi-national analysis, several important perinatal factors were associated with AKI and infants with both NE and AKI had longer length of stay than NE alone. Future research aimed at early AKI detection, renoprotective management strategies, and understanding the long-term renal consequences are warranted in this high-risk group of patients.
Keywords: Neonate, Acute Kidney Injury, Neonatal Encephalopathy, Hypoxic-Ischemic Encephalopathy
Background
Neonatal encephalopathy (NE), as a consequence of perinatal asphyxia, occurs in 2–5 per 1000 live births and remains a major cause of morbidity and mortality in term infants (1). Neonatal acute kidney injury (AKI) occurs frequently in infants with NE (2), and is an independent risk factor for poor neurodevelopmental outcome and mortality (3, 4). Additionally, neonates who survive even a transient episode of AKI in infancy are at increased risk for long-term chronic kidney disease (5). Various therapies routinely used in the management of NE (including aggressive fluid restriction, reliance on parenteral nutrition, and antibiotic use) may pose additional risk to the kidneys. Thus, the primary episode of asphyxia and its subsequent treatment may exacerbate AKI in infants with NE, placing them at additional short and long-term risk to develop poor outcomes.
The modified Kidney Disease: Improving Global Outcomes (KDIGO) criteria classify neonatal AKI as Stage I, II, or III based on increases in serum creatinine (SCr) from baseline and/or decrease in urine output (6). To date, no multicenter studies have determined the incidence of AKI in asphyxiated infants using this definition. In certain high-risk neonatal populations (premature infants, very low birth weight (VLBW)/extremely low birth weight (ELBW) infants, and infants with sepsis), low Apgar scores, hypotension, non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotic exposure are among the factors known to increase the risk of AKI (6). However, antenatal risk factors that increase the likelihood of AKI among asphyxiated infants have not been well described.
We used the Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) database to : 1) determine the incidence of AKI (using the modified KDIGO definition) among infants with NE, 2) compare the maternal and infant risk factors associated with AKI among infants with and without neonatal encephalopathy, and 3) determine the independent association of AKI on length of stay, mortality, and respiratory support among infants with NE.
Methods
STUDY DESIGN AND DATA SOURCE
The AWAKEN study is the collaborative effort of 24 level III/IV neonatal intensive care units (NICUs) that comprise the Neonatal Kidney Collaborative (NKC)(6). The AWAKEN database was designed to describe the epidemiology, validate the definition, and identify risk factors for neonatal AKI. Infants admitted to the NICU between January 1- March 31, 2014 were included in AWAKEN if they met prespecified inclusion/exclusion criteria. The main inclusion criterion was receipt of intravenous fluids for at least 48 hours. Patients excluded from AWAKEN included infants > 14 days of age at admission, those with congenital heart disease requiring surgery within the first week of life, those with lethal chromosomal anomalies and infants who died within 48 hours of delivery. Details on the other criteria and specifics of the NKC and the database, which includes 325 unique variables including demographics, physiologic parameters, creatinine values and discharge characteristics, have been previously published (7). Additionally, our analysis excluded infants with severe congenital anomalies of the kidney and urinary tract (CAKUT) (including bilateral grade IV–V vesicoureteral reflux, bilateral moderate-severe hydronephrosis, bilateral hypoplasia/dysplasia, and either autosomal dominant or recessive polycystic kidney disease) and infants born <34 weeks GA. Institutional Review Board (IRB) approval was obtained at each participating site with a waiver of informed consent.
STUDY POPULATION
This retrospective cohort study included infants from the AWAKEN dataset ≥ 34 weeks’ gestational age (GA) who had an admission or discharge diagnosis of NE. Younger infants were excluded, as NE is not generally the primary admitting diagnosis for premature infants. Variables were predetermined based on their clinical relevance to neonatal AKI and/or NE.
VARIABLE DEFITIONS
AKI was defined by the KDIGO workgroup definition modified for neonates: any rise in SCr of 0.3mg/dl or 50% from the lowest previous value, and/or urine output of < 1 mL/kg/hour averaged over 24 hours on postnatal days 2–7 (8). Delivery room resuscitation data was captured by four variables describing respiratory support alone (mask or blow-by oxygen, continuous positive airway pressure, positive pressure ventilation breaths, or intubation), or respiratory support plus chest compressions, and/or epinephrine, and/or normal saline bolus. Deliveries occurring outside the AWAKEN institution (including home births, those occurring at a birth center, or those occurring at a lower-acuity referring hospital) were captured as “outborn.” Outcomes of interest included: NICU length of stay (in days), death during hospitalization, and duration of respiratory support.
Ventilation support was defined by receipt of noninvasive positive-pressure ventilation, invasive conventional ventilation, or high-frequency ventilation. Oxygen support was defined as the receipt of oxygen by hood or nasal cannula. Weekly evaluation of ventilation and oxygen support in the first 4 weeks of life was then calculated. We defined “oxygen-free weeks” as any week in which a subject was alive and not receiving supplemental oxygen or mechanical ventilation. We defined “ventilation-free weeks” as any week in which a subject was alive and either required supplemental oxygen only, or required no respiratory support.
STATISTICAL ANALYSIS
To assess the bivariate association between maternal and infant characteristics and AKI, categorical variables were analyzed by proportional differences with the Chi-square or Fisher Exact test (where appropriate). All continuous variables were tested for normality using the Shapiro-Wilk Test. For normally distributed continuous variables, the mean ± standard deviation (SD) were reported and analyzed using a Student t-test. For non-normally distributed variables, the median and interquartile ranges (IQR) were reported, and groups were compared using the Wilcoxon Rank-Sum test. To assess the independent associations, a forward selection logistic regression process was used with a standard of entry of p<0.2. Additionally, intrauterine growth restriction (IUGR), maternal diabetes, hypertensive gestational diseases (maternal hypertension, pre-eclampsia, or eclampsia) and intrapartum nuchal cord complications were prespecified and forced into the model due to the clinically relevant and biological mechanisms of NE and AKI. We also included nephrotoxic drug exposure and fluid overload in the first 7 days, as these are also known risk factors for AKI. Linear regression was used to determine the independent impact of AKI among those with NE on length of stay and was constructed using a backwards selection procedure with a significance level of < 0.2. All analyses were performed using SAS 9.4 software. (Copyright © 2012 SAS Institute Inc. Cary, NC, USA.)
Results
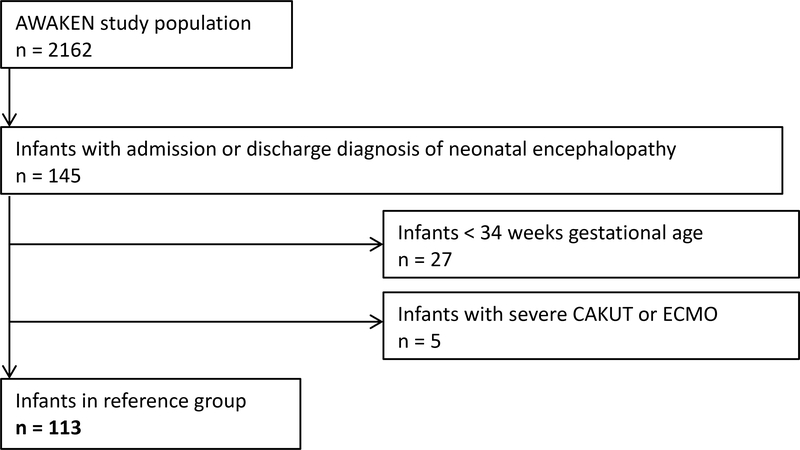
There were 2162 infants in the AWAKEN cohort. Figure 1 summarizes the breakdown of patients excluded and used in the final analysis. After excluding patients who did not meet inclusion criteria, 145 had an admission diagnosis of NE. An additional 32 infants were excluded based on pre-specified exclusion criteria (N=27 for < 34 weeks GA, and N=5 for CAKUT), leaving 113 patients in the final analysis. 70.3% of these infants were admitted to the ICU on day of life 0; 22.9% were admitted on day of life 1. Only 1 patient was admitted beyond 7 days of age.
Figure 1.
Description of study population and the reference group. AWAKEN = Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates. CAKUT = congenital anomalies of kidney or urinary tract. ECMO = Extracorporeal Membrane Oxygenation.
The incidence of AKI in the cohort was 41.6% (n = 47). Of the 47 infants with AKI, 13 (27.7%) had creatinine-defined AKI, 22 (46.8%) had urine output-defined AKI, and 12 (25.5%) met both creatinine and urine output criteria for AKI.
Patient demographics, maternal characteristics, and perinatal patient characteristics are summarized in Table 1. There were no significant differences in race/ethnicity, gestational age at delivery or birth weight among those with and without AKI. A greater proportion of infants who were outborn developed AKI (n = 43, 91.5%) compared to those who were born at the participating level III/IV NICU (n = 46, 69.7%) (p = 0.005). The NICU admission temperature was also significantly lower among patients with AKI (34.5 ± 2.2 ° Celsius) compared to patients without AKI (35.6 ± 1.8 ° Celsius) (p = 0.04.) Of the pregnancy characteristics, IUGR was more common in those with AKI, although not statistically significantly (p = 0.08). Of the intrapartum complications, the presence of meconium stained amniotic fluid (MSAF) was significantly more common among patients with AKI compared to those without AKI [17/47, 36.2% vs. 12/66, 18.2%; p = 0.03]. Need for advanced delivery room resuscitation (chest compressions, epinephrine, or volume expansion) and APGAR scores did not differ between those with and without AKI.
Table 1.
Patient demographics, maternal, perinatal and postnatal characteristics.
| NE; No AKI (n = 66) | NE + AKI (n = 47) | p-value | |
|---|---|---|---|
| Gender (Male) | 44 (66.7%) | 23 (48.9%) | 0.06 |
| Ethnicity | 1.00 | ||
| Hispanic | 4 (8.2%) | 3 (8.8%) | |
| Non-Hispanic | 45 (91.8%) | 31 (91.2%) | |
| Race | 0.50 | ||
| White | 33 (50%) | 26 (55.3%) | |
| Black | 11 (16.7%) | 10 (21.3%) | |
| Other | 22 (33.3%) | 11 (23.4%) | |
| Gestational Age (Weeks) | 0.64 | ||
| 34–37 | 14 (21.2%) | 8 (17%) | |
| 37 or Greater | 52 (78.8%) | 39 (83.0%) | |
| Birthweight (g) | 0.55 | ||
| 1501 – 2501 | 9 (13.6%) | 4(8.7%) | |
| ≥2501 | 57 (86.4%) | 42 (91.3%) | |
| Day of Life at Admission | 0 (0, 0) | 0 (0, 1) | 0.10 |
| Outborn* | 46 (69.7%) | 43 (91.5%) | 0.005 |
| Mode of Delivery | |||
| Caesarean Section | 34 (54.0%) | 18 (42.9%) | 0.26 |
| Vaginal Birth | 29 (46.0%) | 24 (57.1%) | |
| Delivery Room Resuscitation | |||
| Respiratory Support | 65 (98.5%) | 43 (91.5%) | 0.07 |
| Chest Compressions | 16 (24.2%) | 13 (27.7%) | 0.68 |
| Epinephrine | 8 (12.1%) | 9 (19.1%) | 0.30 |
| Normal Saline bolus | 12 (18.2%) | 13(27.7%) | 0.23 |
| Admission Temp. (°C) | 35.6 ± 1.8 | 34.5 ± 2.2 | 0.04 |
| Apgar Scores | |||
| 1 minute | 2.0 (1.0, 3.0) | 1.5 (1.0, 3.0) | 0.43 |
| 5 minute | 4.0 (3.0, 6.0) | 4.0 (2.0, 6.0) | 0.35 |
| Pregnancy Characteristics | |||
| Intrapartum infection | 9 (13.6%) | 5 (10.6%) | 0.77 |
| Diabetes | 8 (12.1%) | 6 (12.8 %) | 1.00 |
| Gestational Hypertension | 8 (12.1%) | 4 (8.5%) | 0.76 |
| IUGR | 1 (1.5%) | 5 (10.6%) | 0.08 |
| Prenatal Tobacco Use | 8 (12.1%) | 2 (4.3%) | 0.19 |
| Intrapartum Complications | |||
| Nuchal Cord | 11 (16.7%) | 12 (25.5%) | 0.34 |
| MSAF | 12 (18.2%) | 17 (36.2%) | 0.03 |
| Severe Bleeding | 6 (9.1%) | 3 (6.4%) | 0.73 |
| Shoulder Dystocia | 4 (6.1%) | 3 (6.4%) | 1.00 |
| Postpartum Factors | |||
| NT drug exposure** | 49 (74.2%) | 41 (87.2%) | 0.10 |
| Fluid overload ǂ | 22 (33.3%) | 23 (48.9%) | 0.12 |
| Bacteremia/meningitisǂǂ | 2 (3%) | 1 (2%) | 1.00 |
Data are n (%), mean (SD) or median (IQR 25, 75).
Outborn indicates infant born outside the admitting NICU (including home births, birth centers, and lower-acuity facilities).
NT drug exposure = nephrotoxic drug exposure within first 7 days (gentamicin, vancomycin, furosemide, indomethacin)
Fluid overload defined as weight > 5% above birth weight at any point in.first 7 days of life
Denotes culture-positive bacteremia or meningitis within the first 7 days of life.
AKI = acute kidney injury; wks = weeks; g = grams; cm = centimeters; °C degrees Celsius; IUGR = intrauterine growth restriction; MSAF = Meconium-Stained Amniotic Fluid
We also compared the demographics of all term and near-term infants with AKI, with and without neonatal encephalopathy (Table 2). There were no significant differences in gender, race, ethnicity, pregnancy-related conditions or mode of delivery. Infants with AKI and NE were more often 37 weeks’ or more gestation, born outside the admitting institution, required more advanced delivery room resuscitation, had lower Apgar scores, and had more intrapartum complications (nuchal cord, MSAF, or shoulder dystocia) than infants with AKI alone. Infants with AKI and NE were more frequently exposed to nephrotoxic drugs and fluid overload.
Table 2.
Comparison of patient demographics, maternal, perinatal and postnatal characteristics between infants with AKI with and without neonatal encephalopathy.
| AKI; no NE n = 364 | AKI + NE (n = 47) | p-value | |
|---|---|---|---|
| Gender (Male) | 220 (60.4) | 23 (48.9%) | 0.16 |
| Ethnicity | 0.76 | ||
| Hispanic | 31 (10.5%) | 3 (8.8%) | |
| Non-Hispanic | 264 (89.5%) | 31 (91.2%) | |
| Race | 0.27 | ||
| White | 239 (65.7%) | 26 (55.3%) | |
| Black | 49 (13.5%) | 10 (21.3%) | |
| Other | 76 (20.9%) | 11 (23.4%) | |
| Gestational Age (Weeks) | 0.047 | ||
| 34–37 | 113 (31.0%) | 8 (17%) | |
| 37 or Greater | 251 (69.0%) | 39 (83.0%) | |
| Birthweight (g) | 0.045 | ||
| 1501 – 2501 | 76 (20.9%) | 4(8.7%) | |
| ≥2501 | 283 (77.7%) | 42 (91.3%) | |
| Outborn* | 258 (70.9%) | 43 (91.5%) | 0.002 |
| Mode of Delivery | 0.97 | ||
| Caesarean Section | 144 (42.6%) | 18 (42.9%) | |
| Vaginal Birth | 194 (57.4%) | 24 (57.1%) | |
| Delivery Room Resuscitation | |||
| Respiratory Support | 185 (50.8%) | 43 (91.5%) | <0.0001 |
| Chest Compressions | 16 (4.4%) | 13 (27.7%) | <0.0001 |
| Epinephrine | 10 (2.7%) | 9 (19.1%) | <0.0001 |
| Normal Saline bolus | 25 (6.9%) | 13(27.7%) | <0.0001 |
| Admission Temp. (°C) | 36.6 ± 1.1 | 34.5 ± 2.2 | |
| Apgar Scores | |||
| 1 minute | 8 (4, 8) | 1.5 (1.0, 3.0) | <0.0001 |
| 5 minute | 8 (7, 9) | 4.0 (2.0, 6.0) | <0.0001 |
| Pregnancy Characteristics | |||
| Intrapartum infection | 37 (10.2%) | 5 (10.6%) | 0.92 |
| Diabetes | 42 (11.5%) | 6 (12.8 %) | 0.80 |
| Gestational Hypertension | 45 (12.4%) | 4 (8.5%) | 0.44 |
| IUGR | 31 (8.5%) | 5 (10.6%) | 0.63 |
| Prenatal Tobacco Use | 31 (8.5%) | 2 (4.3%) | 0.31 |
| Intrapartum Complications | |||
| Nuchal Cord | 31 (8.5%) | 12 (25.5%) | 0.0003 |
| MSAF | 63 (17.3%) | 17 (36.2%) | 0.002 |
| Severe Bleeding | 12 (3.3%) | 3 (6.4%) | 0.29 |
| Shoulder Dystocia | 6 (1.6%) | 3 (6.4%) | 0.04 |
| Postpartum Factors | |||
| NT drug exposure** | 266 (73.1%) | 41 (87.2%) | 0.03 |
| Fluid overload ǂ | 101 (27.7%) | 23 (48.9%) | 0.003 |
| Bacteremia/meningitisǂǂ | 15 (4.1%) | 1 (2%) | 0.51 |
Data are n (%), mean (SD), median (IQR).
Outborn indicates infant born outside the admitting NICU (including home births, birth centers, and lower-acuity facilities).
NT drug exposure = nephrotoxic drug exposure within first 7 days (gentamicin, vancomycin, furosemide, indomethacin)
Fluid overload defined as weight > 5% above birth weight at any point in.first 7 days of life
Denotes culture-positive bacteremia or meningitis within the first 7 days of life.
AKI = acute kidney injury; wks = weeks; g = grams; cm = centimeters; °C degrees Celsius; IUGR = intrauterine growth restriction; MSAF = Meconium-Stained Amniotic Fluid
In the multivariate logistic regression analysis (after adjusting for maternal diabetes, hypertensive diseases of pregnancy, intrapartum nuchal cord complications, nephrotoxic medications, and fluid overload), being outborn, having IUGR, and MSAF were independently associated with AKI. The logistic regression analysis is summarized in Table 3.
Table 3.
Multivariate logistic regression to determine associations between risk factors and acute kidney injury.
| Odds Ratio | 95% CI | p-value | |
|---|---|---|---|
| Outborn | 4.28 | 1.24 – 14.79 | 0.02 |
| Intrauterine Growth Restriction | 10.34 | 1.06 – 100.47 | 0.04 |
| Meconium-Stained Amniotic Fluid | 2.83 | 1.04 – 7.70 | 0.04 |
C statistic = 0.73. Logistic regression model includes Site of Delivery, IUGR, Exposure to Meconium, maternal diabetes, hypertensive gestational diseases (maternal hypertension, pre-eclampsia, or eclampsia) intrapartum nuchal cord complications, Nephrotoxic Medications, and Fluid Overload.
There was no difference in mortality rate in those with AKI (n = 3, 6.4%), compared to those without AKI (n = 5, 7.6%) (p = 1.0). When oxygen-free and ventilator-free weeks were compared, AKI was not associated with a statistically significant difference in degree or duration of respiratory support (Table 4). After controlling for IUGR, maternal diabetes, hypertensive gestational diseases, nuchal cord complications, nephrotoxic medications, and fluid overload, infants with AKI spent 8.5 days longer in the NICU than infants without AKI (95% CI 0.79 – 16.2, p = 0.03) (Table 5).
Table 4.
Unadjusted analysis for mortality, and length of stay and respiratory support among infants with NE.
| No AKI n = 66 | AKI n = 47 | p-value | |
|---|---|---|---|
| Mortality | 5 (7.6%) | 3 (6.4%) | 1.00 |
| Length of Stay (days) | 13.0 ± 9.7 | 24.2 ± 29.9 | 0.005 |
| Oxygen-Free Weeks | 0.33 | ||
| 0* | 6 (9.1%) | 8 (17.0%) | |
| 1–3 | 20 (30.3%) | 16 (34.0%) | |
| 4 | 40 (60.6%) | 23 (48.9%) | |
| Ventilator-Free Weeks | 0.22 | ||
| 0* | 5 (7.6%) | 7 (14.9%) | |
| 1–3 | 8 (12.1%) | 9 (19.1%) | |
| 4 | 53 (80.3%) | 31 (66.0%) | |
0 is the reference group
Table 5.
Adjusted Prediction Model for Length of Stay
| Crude | p-value | Adjusted | p-value | |
|---|---|---|---|---|
| Length of Stay (Days) | Parameter Estimate* | Parameter Estimate* | ||
| 11.05 (3.27–18.83) | 0.01 | 8.48 (0.79 – 16.2) | 0.03 | |
Linear model for LOS adjusted for IUGR, Maternal Diabetes, Hypertensive Gestational Diseases, Nuchal Cord complications, Nephrotoxic Medications, and Fluid Overload
Discussion
The incidence of AKI among term and near-term neonates with NE in the AWAKEN cohort was 41.6%. This is higher than the overall incidence of AKI (30%) in the entire AWAKEN cohort and higher than the incidence of AKI in the term infants (36.7%) (9). The diagnosis of AKI was made on the basis of oliguria alone in 48% of the NE cohort. This likely reflects that careful assessment of urine output is part of routine clinical practice in the management of encephalopathic term infants, while frequent serum creatinine monitoring is less common.
We found that being born outside the NKC-affiliated hospital had 4.3 times the odds of developing AKI. We hypothesize this relationship is multifactorial, and may be due at least in part to differences in care at large referral institutions, and differences in the disease severity for those transferred to a higher level of care. Having MSAF also increased odds of AKI. MSAF is thought to indicate a state of intrauterine stress and hypoxia, which could lead to increased vulnerability of the kidneys. Similarly, the finding that IUGR also increased an infant’s odds of developing AKI bespeaks the vulnerability of the kidneys in a state of chronic intrauterine hypoxia.
Within our subgroup of infants with neonatal encephalopathy, we did not find that those with AKI had worse mortality or more ventilator support. When assessing length of stay, we did find that even after controlling for multiple confounders, compared to infants without AKI, those with AKI had an increased adjusted length of stay of 8.5 days. Although there was a trend towards more oxygen-free and ventilation free weeks in the group without AKI, small sample size and lack of granularity of this data may have limited our statistical power.
Interestingly, we report for the first time that a lower admission temperature was associated with AKI (table 1). We speculate possible reasons for this association: first, it is possible that sicker infants (who are more likely to develop AKI) may have been passively or actively cooled at admission, as therapeutic hypothermia is standard of care for infants with moderate to severe neonatal encephalopathy (10). Second, it is possible that neonates that are transported to a referral NICU for hypothermia therapy may in fact be excessively cool at admission(11). Third, it is possible that outborn status may confound the association between admission temperature and AKI, and finally, it is possible that hypothermia is a marker for severity of illness in term neonates, similar to what has been seen in premature infants. This data is somewhat contrary to the data reported in a single-center study by Selewski et al which suggested that the incidence of AKI in NE was lower in the era since hypothermia has become standard of care (12). The specific impact of hypothermia on AKI in infants with NE needs to be further studied, with careful attention to NE severity and whether or not therapeutic hypothermia was offered.
The aforementioned study by Selewski et al found a similar incidence of AKI among asphyxiated neonates (38%) between 2003–2010 using a relative increase in SCr from baseline to define AKI (12). This study also found longer length of stay and duration of mechanical ventilation in the AKI group, as well as higher risk of mortality (though not statistically significant.) Our multicenter analysis did not find a mortality difference, likely because death during hospitalization was less common overall. This may be due to the fact that infants with mild neonatal encephalopathy are now routinely admitted for therapeutic hypothermia in many centers (13), and comprise a less critically ill patient population. Our study was also unable to demonstrate a difference in the duration or type of respiratory support between infants with and without AKI. This could be due to limitations of the data set with regard to respiratory support beyond the first week of admission, as the AWAKEN database collected continuous data for the first 7 days and then weekly data for each subsequent week of hospitalization (7).
Another single-center prospective study by Alaro et al in Nairobi examined infants who mostly had mild NE. They defined AKI as a SCr > 133 μmol/L (>1.5 mg/dL) on day 3 of life (3). Infants were not offered therapeutic hypothermia. They found a lower prevalence of AKI than in our study (11.7%) likely due to a high threshold value for SCr. Overall mortality in their cohort was nearly 17%. Using this higher threshold for AKI, the authors found a 24-fold increase in mortality (p = 0.001) compared to neonates with NE and no AKI (3). Our analysis failed to detect a mortality difference; perhaps because we applied a lower threshold to meet the AKI definition, or because this was a broader group of larger and more generalizable group of asphyxiated neonates. Alternatively, the lower mortality in our cohort may have been due to interval improvement in the care of asphyxiated infants, particularly in high-resource tertiary and quaternary centers. It is also possible that our cohort was too small to be powered to detect a mortality difference.
Recent data points to the importance of AKI as a truly independent contributor to morbidity and mortality rather than a marker of illness severity (14). Studies suggest that therapeutic strategies to mitigate AKI in this population may be warranted, such as the use of single-dose theophylline or aminophylline in patients with NE to prevent AKI (15). These therapeutic interventions are considered level C (16), and whether this intervention mitigates AKI in the context of therapeutic hypothermia has yet to be determined. Future studies investigating these drugs in context of current clinical practice (therapeutic hypothermia) and evaluating both short and long-term renal outcomes are necessary.
The strengths of our study include the use of contemporary definitions of AKI including urine output, and the multi-center nature of the study. We acknowledge several limitations, primarily those inherent to the retrospective nature of the data collection. The AWAKEN database was designed to capture data related to kidney risk specifically among neonates overall; thus some variables necessary to characterize a subgroup with NE (e.g., proportion of neonates receiving therapeutic hypothermia, severity of encephalopathy) were not collected. Although our study captured AKI risk in the largest cohort of NE to-date, the relatively small sample size limited the precision of our estimates, and we were unable to stratify odds ratios based on AKI severity. While causal inferences cannot be made from observational data, the emergence of IUGR, meconium, low admission temperature and being outborn as risk factors for AKI merit further exploration.
In conclusion, to our knowledge, this study is the first to report AKI incidence, explore risk factors and outcomes in a multi-national cohort of infants with NE. This study confirms that AKI occurs frequently in this group, is associated specifically with being outborn, IUGR, or having MSAF (a marker of antenatal stress), and low admission temperature. Infants with AKI have longer length of stay, even after adjusting for confounders. Survivors of NE merit inpatient monitoring for AKI and specific protocols for its management, as well as blood pressure screening by primary care pediatricians after discharge as recommended by the American Academy of Pediatrics (17). Future prospective research should be directed at improving diagnosis of AKI in the early neonatal period using biomarkers that account for unique neonatal physiology, and characterizing long-term renal outcomes in survivors of neonatal encephalopathy.
Acknowledgements
The authors would like to thank Krysta Smith for editing and assistance with the manuscript. The authors would also like to thank the outstanding work of the following clinical research personnel and colleagues for their involvement in AWAKEN:
Ariana Aimani, Ana Palijan, MD, Michael Pizzi — Montreal Children’s Hospital, McGill University Health Centre, Montreal, Quebec, Canada; Julia Wrona, BS — University of Colorado, Children’s Hospital Colorado, Aurora, Colorado, USA; Melissa Bowman, RN — University of Rochester, Rochester, New York, USA; Teresa Cano, RN, Marta G. Galarza, MD, Wendy Glaberson, MD, Denisse Cristina Pareja Valarezo, MD — Holtz Children’s Hospital, University of Miami, Miami, Florida, USA; Sarah Cashman, BS, Madeleine Stead, BS — University of Iowa Children’s Hospital, Iowa City, Iowa, USA; Jonathan Davis, MD, Julie Nicoletta, MD — Floating Hospital for Children at Tufts Medical Center, Tufts University School of Medicine, Boston, Massachusetts, USA; Alanna DeMello — British Columbia Children’s Hospital, Vancouver, British Columbia, Canada; Lynn Dill, RN — University of Alabama at Birmingham, Birmingham, Alabama, USA; Ellen Guthrie, RN — MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio, USA, Nicholas L. Harris, BS, Susan M. Hieber, MSQM — C.S. Mott Children’s Hospital, University of Michigan, Ann Arbor, Michigan, USA; Katherine Huang, Rosa Waters — University of Virginia Children’s Hospital, Charlottesville, Virginia, USA; Judd Jacobs, Tara Terrell — Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA; Nilima Jawale, MD — Maimonides Medical Center, Brooklyn, New York, USA; Emily Kane — Australian National University, Canberra, Australia; Patricia Mele, DNP — Stony Brook Children’s Hospital, Stony Brook, New York, USA; Charity Njoku, Tennille Paulsen, Sadia Zubair — Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas, USA; Emily Pao — University of Washington, Seattle Children’s Hospital, Seattle, Washington, USA; Becky Selman RN, Michele Spear, CCRC — University of New Mexico Health Sciences Center Albuquerque, New Mexico, USA; Melissa Vega, PA-C — The Children’s Hospital at Montefiore, Bronx, New York, USA); Leslie Walther RN — Washington University, St. Louis, Missouri, USA.
Funding sources
Cincinnati Children’s Hospital Center for Acute Care Nephrology provided funding to create and maintain the AWAKEN Medidata Rave electronic database. The Pediatric and Infant Center for Acute Nephrology (PICAN) provided support for web meetings, for the NKC steering committee annual meeting at the University of Alabama at Birmingham (UAB), as well as support for some of the AWAKEN investigators at UAB (LBJ, RJG). PICAN is part of the Department of Pediatrics at the University of Alabama at Birmingham (UAB), and is funded by Children’s of Alabama Hospital, the Department of Pediatrics, UAB School of Medicine, and UAB’s Center for Clinical and Translational Sciences (CCTS, NIH grant UL1TR001417). Finally, the AWAKEN study at the University of New Mexico was supported by the Clinical and Translational Science Center (CTSC, NIH grant UL1TR001449) and by the University of Iowa Institute for Clinical and Translational Science (U54TR001356). AWAKEN investigators at the Canberra Hospital were supported by the Canberra Hospital Private Practice fund, and investigators at University of Virginia Children’s Hospital were supported by a 100 Women Who Care Grant (100 Women Charitable Foundation, CA, USA).
Role of funding sources
Funding sources for this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Footnotes
Conflict of interest disclosures
All authors declare no real or perceived conflicts of interest that could affect the study design, collection, analysis and interpretation of data, writing of the report, or the decision to submit for publication.
For full disclosure, we provide here an additional list of other author’s commitments and funding sources that are not directly related to this study: David J Askenazi serves on the speaker board for Baxter (Baxter, USA), and the Acute Kidney Injury (AKI) Foundation (Cincinnati, OH, USA); he also receives grant funding for studies not related to this manuscript from National Institutes of Health — National Institutes of Diabetes and Digestive and Kidney Diseases (NIH-NIDDK, R01 DK103608 and NIH-FDA (R01 FD005092). Danielle E. Soranno also receives grant funding for studies not related to this manuscript from National Institutes of Health - National Institute of Diabetes and Digestive and Kidney Diseases, 1K08DK109226-01A1.
References
- 1.Pfister RH, Soll RF. Hypothermia for the treatment of infants with hypoxic-ischemic encephalopathy. J Perinatol. 2010;30 Suppl:S82–7. [DOI] [PubMed] [Google Scholar]
- 2.Karlowicz MG, Adelman RD. Nonoliguric and oliguric acute renal failure in asphyxiated term neonates. Pediatr Nephrol. 1995;9(6):718–22. [DOI] [PubMed] [Google Scholar]
- 3.Alaro D, Bashir A, Musoke R, Wanaiana L. Prevalence and outcomes of acute kidney injury in term neonates with perinatal asphyxia. Afr Health Sci. 2014;14(3):682–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta BD, Sharma P, Bagla J, Parakh M, Soni JP. Renal failure in asphyxiated neonates. Indian Pediatr. 2005;42(9):928–34. [PubMed] [Google Scholar]
- 5.Carmody JB, Charlton JR. Short-term gestation, long-term risk: prematurity and chronic kidney disease. Pediatrics. 2013;131(6):1168–79. [DOI] [PubMed] [Google Scholar]
- 6.Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, et al. Neonatal Acute Kidney Injury. Pediatrics. 2015;136(2):e463–73. [DOI] [PubMed] [Google Scholar]
- 7.Jetton JG, Guillet R, Askenazi DJ, Dill L, Jacobs J, Kent AL, et al. Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates: Design of a Retrospective Cohort Study. Front Pediatr. 2016;4:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chowdhary V, Vajpeyajula R, Jain M, Maqsood S, Raina R, Kumar D, et al. Comparison of different definitions of acute kidney injury in extremely low birth weight infants. Clin Exp Nephrol. 2018;22(1):117–25. [DOI] [PubMed] [Google Scholar]
- 9.Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. The Lancet Child & Adolescent Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013(1):Cd003311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bourque SL, Meier SA, Palmer C, Melara DL, Grover TR, Delaney CA. A Quality Initiative for Optimal Therapeutic Hypothermia during Transport for Neonates with Neonatal Encephalopathy. Pediatr Qual Saf. 2018;3(2):e056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr. 2013;162(4):725–9.e1. [DOI] [PubMed] [Google Scholar]
- 13.Kracer B, Hintz SR, Van Meurs KP, Lee HC. Hypothermia therapy for neonatal hypoxic ischemic encephalopathy in the state of California. J Pediatr. 2014;165(2):267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators A. Epidemiology of Acute Kidney Injury in Critically Ill Children and Young Adults. The New England journal of medicine. 2017;376(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhat MA, Shah ZA, Makhdoomi MS, Mufti MH. Theophylline for renal function in term neonates with perinatal asphyxia: a randomized, placebo-controlled trial. J Pediatr. 2006;149(2):180–4. [DOI] [PubMed] [Google Scholar]
- 16.Askenazi D Should neonates with perinatal asphyxia receive a single dose of IV theophylline to prevent acute kidney injury? Acta Paediatr. 2016;105(10):1125–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3). [DOI] [PubMed] [Google Scholar]