Abstract
Objective:
To study social and demographic differentiation of assisted reproduction technology (ART) use at the population level in the United States.
Design:
Population-based study.
Setting:
Not applicable.
Patient(s):
Women 15–49 years old in the American Community Survey and National Vital Statistics Birth Certificate data from 2010–2017.
Interventions:
Not applicable.
Main Outcome Measure(s):
Birth rate after ART by major sociodemographic categories and likelihood of having an ART birth.
Result(s):
Net of education, age, period, and marital status, the incidence rates of ART births are lower for black women (0.57 times; 95% CI, 0.52–0.62) and Hispanic women (0.67 times; 95% CI, 0.57–0.62) relative to white women’s rates; for Asian women, the incidence rates are 1.21 times that of white women’s rates. Further, the incidence rates of ART births are higher for women with more than a 4-year degree (2.08 times; 95% CI, 1.90–2.27) relative to women with a 4-year degree, and are lower for women with less education. Women who are married have an incidence rate of ART that is 5.72 times (95% CI, 5.37–6.09) that of unmarried women. The incidence rates for 2013–2016 are statistically significantly higher than for 2010 by a factor of 1.16 (95% CI, 1.02–1.31), 1.16 (95% CI, 1.03–1.31), 1.27 (95% CI, 1.12–1.43), and 1.51 (95% CI, 1.43–1.82), respectively. The educational differences in ART exist across all age groups from 20 to 49, but are the largest among the 35–39 and 40–44 age groups.
Conclusion(s):
Large differences in the risk of an ART birth and the proportion of births and the total fertility rate due to ART exist across period, age, race, education, and marital status groups in the United States. Current measures of ART births may disguise an unmet need for ART.
Keywords: ART utilization, birth certificate data, social disparities
Abstract
Objetivo:
Estudiar las diferencias sociales y demográficas del uso de la tecnología de reproducción asistida (ART) a nivel poblacional en Estados Unidos.
Diseño:
estudio poblacional
Establecimiento:
no aplica.
Paciente (s):
Mujeres de 15 a 49 años en la Encuesta de la Comunidad Estadounidense y en los Datos del Certificado Nacional de Nacimiento de Estadisticas Vitales de 2010–2017.
Intervenciones:
no aplica.
Principales medidas de resultado:
tasa de natalidad después de ART por categorías sociodemográfícas principales y por probabilidad de tener un nacimiento por ART.
Resultado (s):
para el nivel de Educación, edad, período y estado civil, las tasas de incidencia de nacimientos con ART son más bajas para las mujeres negras (0,57 veces; IC 95%, 0.52-0.62) y mujeres hispanas (0.67 veces; IC 95%, 0.57-0.62) en relación con las tasas de mujeres blancas; para las mujeres asiáticas, las tasas de incidencia son 1.21 veces mayores que las tasas de las mujeres blancas. Además, las tasas de incidencia de nacimientos con ART son más altas para las mujeres con grado de educación mayor a 4 años (2.08 veces; IC del 95%, 1.90–2.27) en relacion con las mujeres con un grado de 4 anos, y son más bajas para las mujeres con menos educación. Las mujeres casadas tienen una tasa de incidencia de ART que es 5,72 veces (IC 95%, 5,37–6,09) que la de las mujeres solteras. La tasa de incidencia para 2013–2016 son estadísticamente significativamente más altas que para 2010 en un factor de 1.16 (IC del 95%, 1.02–1.31), 1.16 (IC del 95%, 1.03–1.31), 1.27 (IC 95%, 1.12–1.43) y 1.51 (IC 95%, 1.43–1.82), respectivamente. Las diferencias educativas en ART existen en todos los grupos de edad desde 20 a 49, pero son más grandes entre los grupos de edad 35-39 y 40-44.
Conclusión (es):
Existen grandes diferencias en el riesgo de un nacimiento con ART y la proportión de nacimientos y la tasa de fertilidad total debido a ART existe a través del período, edad, raza, educación y estado civil en los Estados Unidos. Las medidas actuales de nacimientos con ART pueden ocultar una necesidad no satisfecha con el ART.
Ever since the first “test-tube baby” was born in the United Kingdom in 1978 and the first success of in vitro fertilization in the United States in 1981, assisted reproductive technology (ART) has helped millions of families worldwide to achieve their reproductive desires. Today, with the continued delay in marriage and childbearing, the importance of ART is becoming ever more apparent; it is a resource for many to achieve a balance between work and family, and for others to overcome biological obstacles in conceiving.
The use of ART and ART births have increased over time. The use of ART documented in the National Survey of Family Growth (NSFG) increased from 0.1% of women aged 22–44 years in 1995 to 0.6% in the 2006–2010 survey (1). Further, when limiting the analyzes to women aged 22–44years who had sought any medical help to become pregnant, Stephen et al. (1) found an increasing portion of women received ART: 5.2% in 2006–2010 compared with 3.1% in 2002 and 1.0% in 1995. According to the most recent report, ART births comprised 1.8% of all U.S. births (2).
Along with observed growth in ART cycles and births, scholars have noted ART usage and outcomes vary considerably among racial/ethnic and socioeconomic groups (3–11), and access is unequal due to economic, social, and structural barriers (12). Despite the identification of these disparities, our knowledge about the social and demographic differentiation in ART use in the United States is still limited due the lack of suitable data.
On the one hand, sample data from nationally representative surveys like the NSFG do not have sufficient statistical power to detect differences observed in rare events like ART because of small cell counts, and the data from individual clinics are not nationally representative. On the other hand, population-level data on ART collected from clinics by the Centers for Disease Control and Prevention (CDC) and the Society for Assisted Reproductive Technology (SART) are not available for public use. As a result, researchers are limited to the reported statistics from the CDC and SART, which include a highly general ART rate (the number of ART procedures per 1 million women aged 15 to 44 years) (2). This metric includes a broad age group of women, many of whom are likely not at risk for an ART birth. In addition, the data reported by SART and the CDC are often truncated for ages under 35 and are not disaggregated by race/ethnic groups nor by education, marital status, or other sociodemographic characteristics.
As a result, ART measures from sample data and those reported from population-level data may disguise potential disparities and make it difficult to assess inequalities in ART use and births. A more detailed assessment of ART use with proper adjustments for exposure to risk (e.g., age) and disaggregation by group social groups within the U.S. population is critical for understanding how U.S. fertility and the fertility of subgroups within the United States are impacted by these new and growing technologies and assessing the real demand. Thus, we have quantified the proportion of births attributable to ART across age, race, educational, and marital groups in a population-based study.
MATERIALS AND METHODS
National Vital Statistics System (NVSS) Birth Certificate Data
Birth certificate data from the National Vital Statistics System (NVSS) are collected by U.S. states and are compiled by the National Center for Health Statistics. Our study uses publicly available data from 2010–2017. The 2003 revised standard birth certificate collects a variety of health and demographic data about biological parents and infants born, including indicators of infertility treatment and use of ART.
American Community Survey (ACS)
The American Community Survey (ACS) is a publically available, nationally representative, continuous cross-sectional survey administered by the U.S. Census Bureau. About 3.5 million households are surveyed per year (13). The survey asks about a number of topics including education, housing, and occupation, and it is used to estimate the size of the population between Census years. These data will be used to derive the size of the population of women by age, race, marital status, and education.
Methods
This study calculated single and 5-year interval age-specific fertility rates (ASFR) for ART and all births. The ASFR is calculated using a demographic formula:
The number of ART births was determined using NVSS data, excluding states that did not report ART. The number of person-years lived by women was estimated using a midyear population estimate from the ACS data, matching states that reported ART in the NVSS data. We stratified the ASFR by race/ethnicity, educational attainment, and marital status.
Total ART Fertility Rate and Truncated Total ART Fertility Rates
A total fertility rate (TFR) is a synthetic cohort measure that estimates the number of births a woman could anticipate having if the ASFR of the current period applied to her entire reproductive lifetime (14). The truncated TFR was calculated for women over 30 years using the following formula:
We completed these calculations across the aforementioned groups using the data sources previously described. A truncated TFR was used because ART births were less common among women aged younger than 30.
Multivariate Analyses
We employ multivariate negative binomial regression to estimate the effect of age, year, and sociodemographic group membership on the number of ART births at the population level. Exposure to risk is accounted via the size of the population at risk for a birth derived from the ACS data set.
Sensitivity Analyses
Evidence from Moaddab et al. (15) and Thoma et al. (16) show ART births are underreported in the NVSS birth certificate data. As a result, we conducted sensitivity analyses to assess the robustness of our results. First, we compared the counts of ART births from the NVSS and the National ART Surveillance System (NASS) using the published reports from the CDC. The next three sensitivity analyses restricted the NVSS data based on the findings from Thoma et al. (16), which show that ART births are more accurately reported among births that were [1] triplets or higher order, [2] under 1,499 grams, and/or [3] at or before 32 weeks’ gestation.
Data Restrictions and Missing Data
Missing data are removed via casewise deletion for both the descriptive analyses and the multivariate analyses. The NVSS data were restricted to [1] women aged 15–49 years, [2] states that reported ART births, and [3] cases with no missing data. In total, 826,016 births, or 3.2% of total births between 2010–2017, were excluded due to missing data. Births with missing data account for 12,019 ART births, or 5.3% of all ART births, from 2010 to 2017. Of the missing data, 2.89% were missing both education and marital status, and 42.93% were missing only education; the remaining were missing only marital status.
All California births in 2017 were excluded from the analyses for 2017 due to new reporting restrictions on marital status. To address potential selection effects due to missing data from California in 2017, we conducted analyses using a missing category for marital status with the appropriate matched denominator from the ACS data. No substantive differences between these analyses and those presented were found (analyses available upon request).
The use of listwise deletion for the descriptive analyses does not substantively change the descriptive results (analyses available upon request). The ACS data were restricted to include women aged 15–49 years in states with reporting of ART births in the NVSS data set. The Census Bureau uses allocation methods to fill in missing in the ACS data. We used the public-use micro sample provided by IPUMS-USA (17). This study was deemed exempt from institutional review board review by the University of North Carolina at Chapel Hill’s institutional review board.
RESULTS
Age-specific Fertility Rates
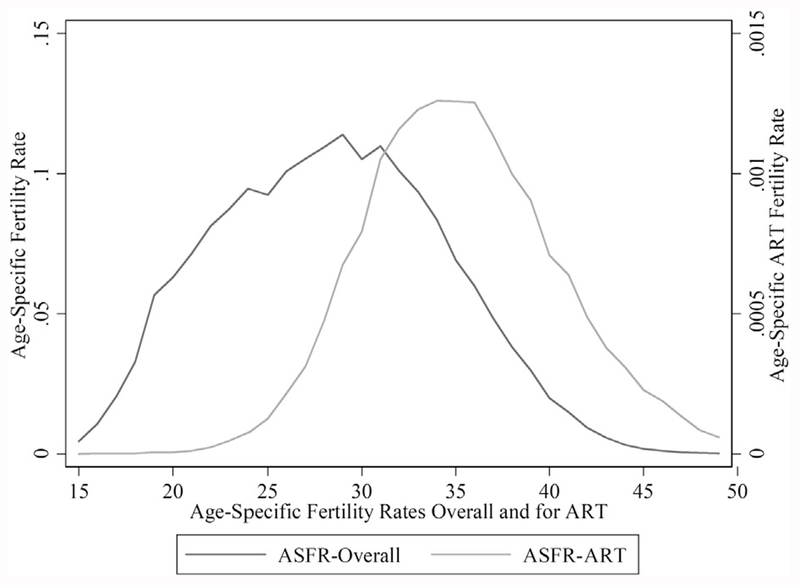
Figure 1 shows the ASFR by single year of age for ART and all births for the entire study period (2010–2017). Note that the two lines are shown in difference scales. The age patterns of fertility for all births and ART births are substantively different from one another. In the overall ASFR curve, we observed a peak of births between 25 and 30 years of age and lower ASFR rates past age 35 (e.g., skewed to the right). By contrast, for ART births, the ASFR peaks in the mid-30s with a narrower spread and a slight skew to the left. We found that ART births are almost as common before age 35 as after age 35: 46.7% of ART births were to mothers younger than 35 years, with 34.2% between ages 30 and 34; 12.5% of births were to mothers younger than 30 years.
FIGURE 1.
Comparison of age-specific fertility rates overall and for ART totaled across years 2010–2017. Note: The scale for the ART age-specific fertility rates (ASFR) rates are 100 times the ASFR overall rates.
Tierney. ART use: a population assessment. Fertil Steril 2019.
Confirming the growing trend of ART use over time, the proportion of births attributable to ART increases over time and across ages, but the increases are much more prominent among older age groups (Supplemental Table 1, available online). Across all years, the percentage of births to women younger than 29 due to ART is below 1%. By contrast, births among women 30 and over have increased across the study period, from 1.54% in 2010 to 2.19% in 2017. The increase is observed across all 5-year age groups over 30: from 0.95% in 2010 to 1.37% in 2017 for women aged 30–34, from 1.92% to 2.82% for women aged 35–39, from 4.02% to 5.83% for women aged 40–44, and from 17.29% to 23.20% for women aged 45–49.
Truncated Total Fertility Rates
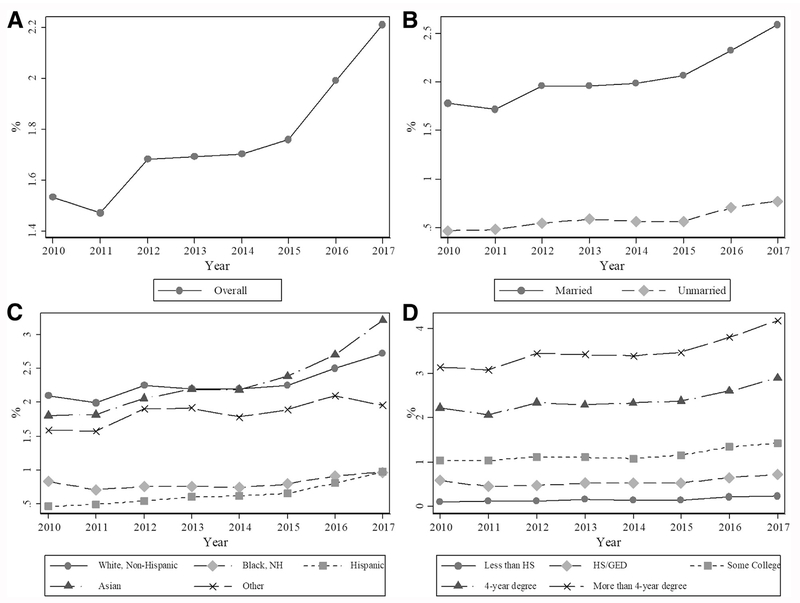
Stratified analyses of truncated total fertility rates (TFR) reveal variation in the contribution of ART to fertility by race, education, and marital status. We found the percentage of the TFR for women older than 30 years due to ART increased over time, from 1.56% in 2010 to 2.21% in 2017 (Fig. 2A). Across all years, the percentage of the TFR of women over 30 due to ART is about three times higher among married women compared with unmarried women (see Fig. 2B). As expected from prior research, the percentage of the TFR for white women over 30 attributable to ART was higher than observed for black or Hispanic women; meanwhile, the proportion of the TFR due to ART was similar among white and Asian women (see Fig. 2C). The percentage of the TFR to women over 30 due to ART increases with educational attainment across all years under study, with a clear gradient (Fig. 2D). The patterns observed in the TFR of women over 30 years of age are similar as those observed across all ages (analyses available upon request).
FIGURE 2.
Percentage of after age 30 fertility for women due to ART by year and group: (A) overall rates, (B) marital status, (C) race, and (D) educational attainment. After age 30 fertility is defined as truncated total fertility after age 30. The y-axis scales vary to best show patterns in the data.
Tierney. ART use: a population assessment. Fertil Steril 2019.
Multivariate Analyses
Multivariate negative binomial regression analysis further showed differences in the risk of ART births by age, period, race, educational, and marital status. The multivariate model presented includes women of all ages because parallel analyses only on women over 30 showed no considerable differences. Table 1 shows the main effects of race, education, age, marital status, and period (year), and Figure 3 and Supplemental Table 3 (available online) show the interaction between age and education status after controlling for other factors. The findings are consistent with the bivariate analyses in Figure 2 and Supplemental Table 1. Stepwise entry models are provided in Supplemental Table 2 (available online) to demonstrate how different factors affect the risk of ART births.
TABLE 1.
Negative binomial analysis of incidence rate ratios for ART births adjusted for age, race, education, marital status, and period (N = 2,079).
| Parameter | Incidence risk ratios | Standard error | 95% Confidence interval |
|---|---|---|---|
| Age | |||
| 15–19 | 0.08a | 0.01 | 0.06–0.10 |
| 20–24 | 0.23a | 0.01 | 0.20–0.26 |
| 25–29 | 0.58a | 0.03 | 0.52–0.63 |
| 30–34 | 1.00 | — | 1.00–1.00 |
| 35–39 | 1.12b | 0.05 | 1.02–1.22 |
| 40–44 | 0.70a | 0.03 | 0.64–0.78 |
| 45–49 | 0.28a | 0.01 | 0.25–0.31 |
| Race | |||
| White | 1.00 | — | 1.00–1.00 |
| Black | 0.57a | 0.03 | 0.52–0.62 |
| Hispanic | 0.62a | 0.03 | 0.57–0.68 |
| Asian/NHOPI | 1.21a | 0.06 | 1.10–1.33 |
| Other | 0.91 | 0.05 | 0.82–1.01 |
| Education | |||
| Less than high school | 0.21a | 0.01 | 0.19–0.24 |
| High school | 0.22a | 0.01 | 0.20–0.24 |
| Some college | 0.53a | 0.02 | 0.48–0.58 |
| 4-year degree | 1.00 | — | 1.00–1.00 |
| More than 4-year degree | 2.08a | 0.09 | 1.90–2.27 |
| Marital status | |||
| Married | 5.72a | 0.18 | 5.37–6.09 |
| Unmarried | 1.00 | — | 1.00–1.00 |
| Year | |||
| 2010 | 1.00 | — | 1.00–1.00 |
| 2011 | 0.99 | 0.06 | 0.87–1.12 |
| 2012 | 1.06 | 0.07 | 0.94–1.21 |
| 2013 | 1.16b | 0.07 | 1.02–1.31 |
| 2014 | 1.16b | 0.07 | 1.03–1.31 |
| 2015 | 1.27a | 0.08 | 1.12 −1.43 |
| 2016 | 1.51a | 0.09 | 1.34–1.70 |
| 2017 | 1.61a | 0.10 | 1.43–1.82 |
| Constant | 0.00a | 0.00 | 0.00–0.00 |
| Ln dispersion parameter (alpha) | 0.34a | 0.01 | 0.32–0.37 |
Note: Incidence risk ratios are calculated by exponentiating the log-transformed rate ratios.
Note: NHOPI ¼ Native Hawaiian and Other Pacific Islanders.
P < .001.
P < .01.
Tierney. ART use: a population assessment. Fertil Steril 2019.
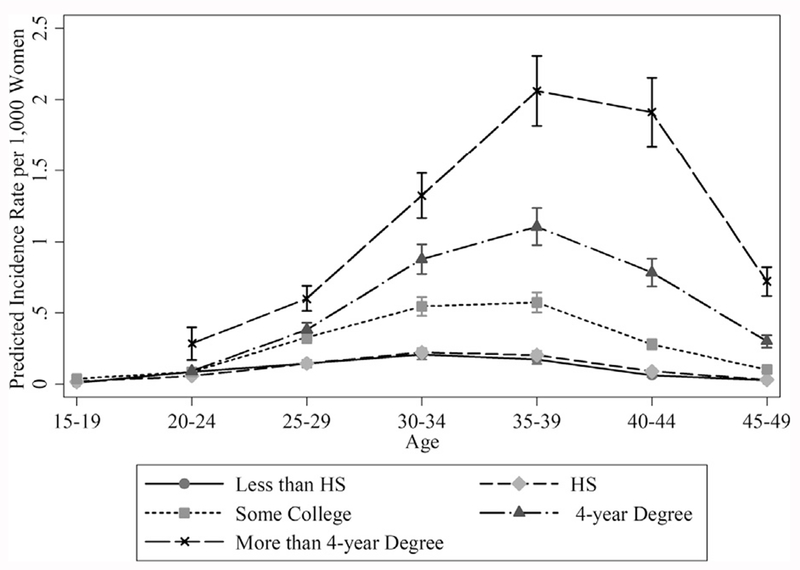
FIGURE 3.
Predicted incidence rates of ART births per 1,000 women with 95% confidence intervals by age and educational groups net of covariates in the full negative binomial regression model.
Tierney. ART use: a population assessment. Fertil Steril 2019.
Based on multivariate regression analysis, we make six observations on the sociodemographic differentiation in the risk of ART births. First, consistent with Figure 2, we find statistically significant differences in the rates of ART across periods (see Table 1). Net of the other covariates, in 2017 the incidence rate of ART births was 1.61 times the incidence rate of ART births of 2010. Similarly, the incidence rates for 2016, 2015, 2014, and 2013 are statistically significantly higher than the 2010 rates by a factor of 1.51, 1.27, 1.16, and 1.16, respectively. There were no statistically significant differences between 2010 and 2011 or 2012. A linear term for year was also statistically significant.
Second, net of the covariates, the incidence rate of ART births for women aged 35–39 is 1.12 times that of women aged 30–34. By contrast, all other age groups have statistically significantly lower incidence rates of an ART birth than women aged 30–34. This multivariate finding differs from the bivariate model (see Supplemental Table 2, model 1) where the risk of ART birth for women aged 30–34 and women aged 35–39 do not differ, indicating the importance of marital status and other covariates in understanding the risk of an ART birth.
Third, net of the covariates, black women’s ART incidence rates are 0.57 and Hispanic women’s ART incidence rates are 0.67 times the incidence rates for white women; Asian women’s ART incidence rates are 21% higher than that of white women. By contrast, we observed no statistically significant differences in the incidence rate of ART births between white women and women of “other” races net of the covariates.
Fourth, with regard to the role of educational attainment, net of the covariates, women with more than a 4-year degree have an incidence rate 2.08 times that of women with a 4-year degree. Women with less than a 4-year degree all have statistically significantly lower incidence rates than women with a 4-year degree.
Fifth, consistent with the descriptive analyses, the effects of marital status are strong. Table 1 shows that net of age, race, education, and year, women who are married have an incident rate that is 5.72 times that of unmarried women.
Finally, based on the model shown in Supplemental Table 3, Figure 3 demonstrates the interaction between education and age. This analysis clarifies the extent to which the observed age effects are moderated by educational attainment (or vice versa). Both the Bayesian information criterion and likelihood-ratio test show that the model with interaction terms between age and education provides a better fit with the data than the model in Table 1. Statistically significant interaction terms indicate the influence of age varies by education (and vice versa). Figure 3 presents the predicted incidence rates of ART per 1,000 by age and education group net of the covariates of period, race, and marital status. The predicted incidence rates assume all other factors are held at their sample mean.
There are distinct age-education patterns in the predicted ART incidence rates. Among women with less than a high-school degree and women with a high-school degree, ART use is low across all age groups. Across all applicable age groups, women with more than 4 years of education have a statistically significantly higher predicted incidence rate of ART than women with other educational attainment, with the predicted rates for women who have more than 4 years of education at 0.29, 0.60, 1.32, 2.05, 1.91, and 0.72 ART births per 1,000 women for ages 20–24, 25–29, 30–34, 3539, 40–44, and 45–49, respectively.
The differences in the risk of ART births between women with a 4-year degree and some college vary by age. At ages 20–24 and 25–29, there are no statistically significant differences in the predicted incidence rates of ART births for women with a 4-year degree and those with some college. However, among women aged 30–34, the predicted incidence rate for women with some college is 0.54 ART births per 1,000 women compared with 0.87 among women who have a 4-year degree. Similarly, among women aged 35–39, the predicted incidence rate for women with a 4-year degree is 1.10 per 1,000 compared with 0.57 for women with some college. For women aged 40–44, the predicted incidence rate for women with a 4-year degree is 0.78 per 1,000 women compared with 0.28 for women with some college, and for women aged 45–49, the incidence rate for women with a 4-year degree is 0.30 per 1,000 compared with 0.10 for women with some college.
Sensitivity Analyses
The sensitivity analyses revealed several important issues. First, in comparing the age-specific counts from the publicly available reports of NASS data to the counts from the NVSS data, we found discrepancies that were consistent with prior work (15, 16). Overall, NVSS captures between 41.2% (in 2010) and 50.0% (in 2016) of expected ART births (see Supplemental Table 2). The analyses exclude 2017 as the NASS report was not available for this analysis. Despite the underreporting of ART use in the NVSS data, the age patterns observed in Figure 1 are mirrored in the NASS data (Supplemental Fig. 1, available online).
Second, there was general agreement between the differences across groups reported in Figure 2 and the parallel analyses done on births more likely to be reported as ART births (Supplemental Figs. 2–4, available online). Notably, however, the proportion of the TFR due to ART among multiple births declines over time, rather than increases. This finding, however, is consistent with the efforts since the 1990s to reduce the occurrence of multiple births via in vitro fertilization (18–22). In addition, although all three subpopulation sensitivity analyses follow the same general stratification by marital status, education, and race, they have more volatility and less clear time-trends as observed in the full analyses. However, this is likely due to the small cell sizes rather than substantive differences in trends.
DISCUSSION
Our analyses make four contributions, which have implications for researchers, providers, and policy makers. First, our work provides new insights into the age distribution of ART births. Specifically, our analyses suggest a sizeable proportion of ART births occur before age 35. However, much of the population level data released about ART births is truncated for women under 35. For example, the majority of age than 35 together. The evidence presented, especially in light of underreporting in the NVSS data, suggests there is both utility and need for single-year of age data especially for women 30 and older to be released from the CDC’s surveillance program of ART. More detailed age-specific data will help researchers assess risk and likelihood of success with greater accuracy as well as to conduct methodologically robust analyses of the contribution of ART births to fertility in the United States.
Second, the demographic rates and analysis of total fertility across groups demonstrate that ART has an important and substantial impact on the fertility of some groups using risk-adjusted population-level data. Our findings are consistent with the available analyses of the SART and CDC data and clinic-based studies regarding race (4, 6, 7, 9, 23) as well as the clinic and sample-based findings showing disparities in ART use and infertility treatment by socioeconomic status (3, 7, 10, 24–27). We also provide new findings documenting how ART impacts total fertility differently for married and unmarried women.
Third, these demographic analyses provide a new lens with which to consider ART. The ART surveillance reports from the CDC have reported a generalized ART rate (ART procedures per 1 million women aged 15–44 years) (2), whereas the analyses presented assess the age-specific contribution of ART to total fertility across groups and ages. This approach more accurately captures both risk and the impact of ART at a population level, which is important for understanding and contextualizing disparities in ART births.
Fourth, the multivariate analyses constitute a unique contribution to the field as they assess the degree to which ART births vary across sociodemographic groups net of other factors using population-level data. Our work adjusts for risk and incorporates covariates such as education, marital status, and interaction terms to show the occurrence of an ART birth is unequal using population-level data. Prior multivariate analyses of the SART data set have focused on the likelihood of live birth but are limited due to the lack of data on socioeconomic status and marital status, and none have explored interactive relationships. For a review and for detailed discussions of race analyses in the SART data, see Wellons et al. (23), Fujimoto et al. (28), Seifer et al. (29), and the Ethics Committee of the American Society for Reproductive Medicine (30).
In our model, both socioeconomic status and marital status are statistically significant predictors, and the stepwise models demonstrate how socioeconomic status may mediate the relationship between race and ART births. Thus, our work improves our understanding of ART by demonstrating observed racial disparities cannot be solely attributed to socioeconomic status, while also showing the importance of marital status and education independently on ART incidence rates. As a result, our work clarifies the nature of the relationship between ART births and sociodemographic features that have been previously identified.
Limitations
We acknowledge the NVSS data has known underreporting issues. Our sensitivity analyses suggest the trends we document are reliable. However, because ART births are underreported rather than overreported, our results could be construed as a lower bound to the contribution of ART births in the population. Additionally, the trends we document with regard to race and socioeconomic status are consistent with prior research, suggesting the trends are likely in the right direction. At this time, however, there are limited options for evaluation of these findings as the more accurate NVSS or SART data are not available in their entirety for public use or do not include characteristics like education or marital status.
Another limitation of this analysis is that it does not allow us to determine either the proximate causes or the social causes of the observed differences in ART births. Social differences in ART births could be because medical factors or social factors, such as differences in incidence of infertility, in access to or use of infertility services, in treatment success rates, and in acceptance of technology. It will require specially designed perspective studies to answer this important issue.
CONCLUSION
These analyses confirm that there are differences in the concentrations and rates of ART births by period as well as by age, racial/ethnic, marital, and educational groups. Thus, the usual reporting of the percentage of births attributable to ART among all women of reproductive age obscures the large differences across groups. Uneven ART birth patterns further suggest that estimates and assumptions about the demand for ART services may be underestimated. For example, if barriers to access and use were diminished among racial and ethnic minority women or women with lower socioeconomic status, we might observe more ART births in the population.
Our analyses also find ART births are influenced by both main effects of period, age, race, marital status, and education as well interactive effects of age and educational attainment. Despite the overall low birth rates due to ART, ART use may be related information in the 2016 Assisted Reproductive Technology National Summary Report groups patients younger the difference in having children or being involuntarily childless for some women. Thus, quantifying unmet need and differential ART birth patterns is an important first step in addressing access to these services. Future research should replicate these analyses with NASS or SART data and explore the impact of differential health care coverage for infertility treatment on these relationships.
The demographic and multivariate analyses not only document the sociodemographic differences in the incidence of an ART birth but also provide a foundation for assessing unmet needs in ART and projecting the potential effect of ART on fertility under varied policy and access conditions and environments. Although the data presented in this paper cannot pinpoint the causes in the sociodemographic difference in ART use, nor the relevant contribution of each, our findings could be used to design future studies and interventions to address concerns voiced by the Ethics Committee of the American Society for Reproductive Medicine (30) about unequal access to and utilization of ART.
Supplementary Material
Acknowledgments:
Any opinion, findings, and conclusions or recommendations expressed in this material are those of the author and do not necessarily reflect the National Science Foundation. This paper uses data from NCHS. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the author and do not necessarily reflect the NCHS, which is responsible for only the initial data.
Supported by National Science Foundation Graduate Research Fellowship under Grant No. DGE-1650116, and the Carolina Population Center and its NIH/NICHD center grant (P2C HD050924).
Footnotes
K.T. has nothing to disclose. Y.C. has nothing to disclose.
REFERENCES
- 1.Stephen EH, Chandra A, King RB. Supply of and demand for assisted reproductive technologies in the United States: clinic- and population-based data, 1995–2010. Fertil Steril 2016;105:451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sunderam S, Kissin DM, Zhang Y, Folger SG, Boulet SL, Warner L, et al. Assisted reproductive technology surveillance—United States, 2016. MMWR Surveill Summ 2019;68:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dayal MB. The impact of sociocultural and economic factors in seeking fertility services In: Sharara FI, editor. Ethnic differences in fertility and assisted reproduction. New York: Springer; New York; 2013:27–38. [Google Scholar]
- 4.Feinberg EC, Larsen FW, Catherino WH, Zhang J, Armstrong AY. Comparison of assisted reproductive technology utilization and outcomes between Caucasian and African American patients in an equal-access-to-care setting. Fertil Steril 2006;85:888–94. [DOI] [PubMed] [Google Scholar]
- 5.Greil AL, McQuillan J, Shreffler KM, Johnson KM, Slauson-Blevins KS. Race-ethnicity and medical services for infertility: stratified reproduction in a population-based sample of U.S. women. J Health Soc Behav 2011;52: 493–509. [DOI] [PubMed] [Google Scholar]
- 6.Humphries LA, Chang O, Humm K, Sakkas D, Hacker MR. Influence of race and ethnicity on in vitro fertilization outcomes: systematic review. Am J Obstet Gynecol 2016;214:212.e1–17. [DOI] [PubMed] [Google Scholar]
- 7.Jain T. Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril 2006;85:876–81. [DOI] [PubMed] [Google Scholar]
- 8.Kissin DM, Boulet SL, Jamieson DJ. Fertility treatments in the United States: improving access and outcomes. Obstet Gynecol 2016;128:387–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McQueen DB, Schufreider A, Lee SM, Feinberg EC, Uhler ML. Racial disparities in in vitro fertilization outcomes. Fertil Steril 2015;104:398–402.e1. [DOI] [PubMed] [Google Scholar]
- 10.Smith JF, Eisenberg ML, Glidden D, Millstein SG, Cedars M, Walsh TJ, et al. Socioeconomic disparities in the use and success of fertility treatments: analysis of data from a prospective cohort in the United States. Fertil Steril 2011; 96:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weedin EA, Janitz A, Peck JD, Craig LB. Racial/ethnic differences in the utilization of infertility services: a focus on American Indian/Alaska Natives. Fertil Steril 2017;107:e45. [Google Scholar]
- 12.Adashi EY, Dean LA. Access to and use of infertility services in the United States: framing the challenges. Fertil Steril 2016;105:1113–8. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Census Bureau. American Community Survey Information Guide [Internet] 2017. Available at: https://www.census.gov/content/dam/Census/programs-surveys/acs/about/ACS_Information_Guide.pdf.
- 14.Preston S, Heuveline P, Michel M. Demography—measuring and modelling population processes. Malden, MA: Blackwell; 2001. [Google Scholar]
- 15.Moaddab A, Bateni ZH, Dildy GA, Clark SL. Poor compliance and lack of improvement in birth certificate reporting of assisted reproductive technology pregnancies in the United States. Am J Obstet Gynecol 2016;215: 528–30. [DOI] [PubMed] [Google Scholar]
- 16.Thoma ME, Boulet S, Martin JA, Kissin D. Births resulting from assisted reproductive technology: comparing birth certificate and National ART Surveillance System data, 2011. Hyattsville, MD: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 17.Ruggles S, Genadek K, Goeken R, Grover J, Sobek M. Integrated public use microdata series: version 7.0 [dataset]. Minneapolis: University of Minnesota; 2017. Available at: 10.18128/D010.V7.0. [DOI] [Google Scholar]
- 18.Practice Committee of the Society for Assisted Reproductive Technology, Practice Committee of the American Society for Reproductive Medicine. Guidelines on number of embryos transferred. Fertil Steril 2006;86(Suppl 1):S51–2. [DOI] [PubMed] [Google Scholar]
- 19.Kulkarni AD, Jamieson DJ, Jones HW, Kissin DM, Gallo MF, Macaluso M, et al. Fertility treatments and multiple births in the United States. N Engl J Med 2013;369:2218–25. [DOI] [PubMed] [Google Scholar]
- 20.Martin JA, Osterman MJK, Thoma ME. Declines in triplet and higher-order multiple births in the United States, 1998–2014. NCHS Data Brief 2016:1–8. [PubMed] [Google Scholar]
- 21.Penzias A, Bendikson K, Butts S, Coutifaris C, Fossum G, Falcone T, et al. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril 2017;107:901–3. [DOI] [PubMed] [Google Scholar]
- 22.Reynolds MA, Schieve LA, Martin JA,Jeng G, Macaluso M.Trends in multiple births conceived using assisted reproductive technology, United States, 1997–2000. Pediatrics 2003;111:1159–62. [PubMed] [Google Scholar]
- 23.Wellons MF, Fujimoto VY, Baker VL, Barrington DS, Broomfield D, Catherino WH, et al. Race matters: a systematic review of racial/ethnic disparity in Society for Assisted Reproductive Technology reported outcomes. Fertil Steril 2012;98:406–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chambers GM, Hoang VP, Illingworth PJ. Socioeconomic disparities in access to ART treatment and the differential impact of a policy that increased consumer costs. Hum Reprod 2013;28:3111–7. [DOI] [PubMed] [Google Scholar]
- 25.Eisenberg ML, Smith JF, Millstein SG, Nachtigall RD, Adler NE, Pasch LA, et al. Predictors of not pursuing infertility treatment after an infertility diagnosis: examination of a prospective U.S. cohort. Fertil Steril 2010; 94:2369–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farland LV, Collier AY, Correia KF, Grodstein F, Chavarro JE, Rich-Edwards J, et al. Who receives a medical evaluation for infertility in the United States? Fertil Steril 2016;105:1274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler LM, Craig BM, Plosker SM, Reed DR, Quinn GP. Infertility evaluation and treatment among women in the United States. Fertil Steril 2013;100: 1025–32.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fujimoto VY, Luke B, Brown MB, Jain T, Armstrong A, Grainger DA, et al. Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril 2010;93:382–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seifer DB, Frazier LM, Grainger DA. Disparity in assisted reproductive technologies outcomes in black women compared with white women. Fertil Steril 2008;90:1701–10. [DOI] [PubMed] [Google Scholar]
- 30.Ethics Committee of the American Society for Reproductive Medicine. Disparities in access to effective treatment for infertility in the United States: an Ethics Committee opinion. Fertil Steril 2015;104:1104–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.