Abstract
BACKGROUND:
The first methodologic step needed to compare pediatric health outcomes at children’s hospitals (CHs) and non–children’s hospitals (NCHs) is to classify hospitals into CH and NCH categories. However, there are currently no standardized or validated methods for classifying hospitals. The purpose of this study was to describe a novel and reproducible hospital classification methodology.
METHODS:
By using data from the 2015 American Hospital Association survey, 4464 hospitals were classified into 4 categories (tiers A–D) on the basis of self-reported presence of pediatric services. Tier A included hospitals that only provided care to children. Tier B included hospitals that had key pediatric services, including pediatric emergency departments, PICUs, and NICUs. Tier C included hospitals that provided limited pediatric services. Tier D hospitals provided no key pediatric services. Classifications were then validated by using publicly available data on hospital membership in various pediatric programs as well as Health Care Cost Institute claims data.
RESULTS:
Fifty-one hospitals were classified as tier A, 228 as tier B, 1721 as tier C, and 1728 as tier D. The majority of tier A hospitals were members of the Children’s Hospital Association, Children’s Oncology Group, and National Surgical Quality Improvement Program–Pediatric. By using claims data, the percentage of admissions that were pediatric was highest in tier A (88.9%), followed by tiers B (10.9%), C (3.9%), and D (3.9%).
CONCLUSIONS:
Using American Hospital Association survey data is a feasible and valid method for classifying hospitals into CH and NCH categories by using a reproducible multitiered system.
Children’s hospitals (CHs) provide high-volume, specialized, and resource-intensive care to children who are the sickest and often require highly trained care providers and cutting-edge technology. Although CHs comprise <5% of all hospitals in the United States, they account for 40% of pediatric inpatient days and 50% of national pediatric health care costs.1 Because these hospitals represent a disproportionate amount of pediatric health care costs, it is important to determine if the high-cost, resource-intensive care provided by CHs is justified by improved health outcomes. To compare health outcomes at CHs and non–children’s hospitals (NCHs), the first step is to classify hospitals into CH and NCH categories. However, the lack of a systematic and standardized process for classifying hospitals poses methodological challenges for these studies.
In this study, we present a novel and reproducible method for distinguishing CHs from NCHs that addresses the limitations with existing classification strategies. By using the 2015 American Hospital Association (AHA) survey, 4464 hospitals were classified into 4 categories on the basis of the level of pediatric services offered. The classifications were then verified by using publicly available data on hospital membership in various pediatric programs as well as commercial insurance claims data.
Methods
Data Sources
The AHA survey is an ongoing comprehensive census of US hospitals. The purpose of the survey is to collect facility-level demographics and characteristics, including service offerings, beds, use, and staffing. The survey profiles a universe of >6400 hospitals, and historically, response rates have been >75% each year.2
For this analysis, we used the 2015 AHA survey, which contains responses from 6251 hospitals in the United States. Non–community hospitals, or hospitals not accessible to the public, were excluded from the data set. Specialty hospitals (such as cancer, orthopedics, rehabitlitation, behavioral, surgical, psychiatric, and cardiac facilities, or other individually described specialty centers) were excluded from the data set as well. After exclusion of noncommunity and specialty centers, the sample included 4464 hospitals.
Once the hospitals were classified into CH and NCH categories by using AHA data (described below), Health Care Cost Institute (HCCI) claims data were used to validate the classifications. The HCCI data consist of the universe of hospital inpatient claims to 3 large national insurers.3 This database uses AHA hospital identification numbers, which allows for merging of the 2 data sources. This study was deemed exempt from full institutional board review because of the patient-level de-identified nature of the data sets.
Defining CHs Versus NCHs
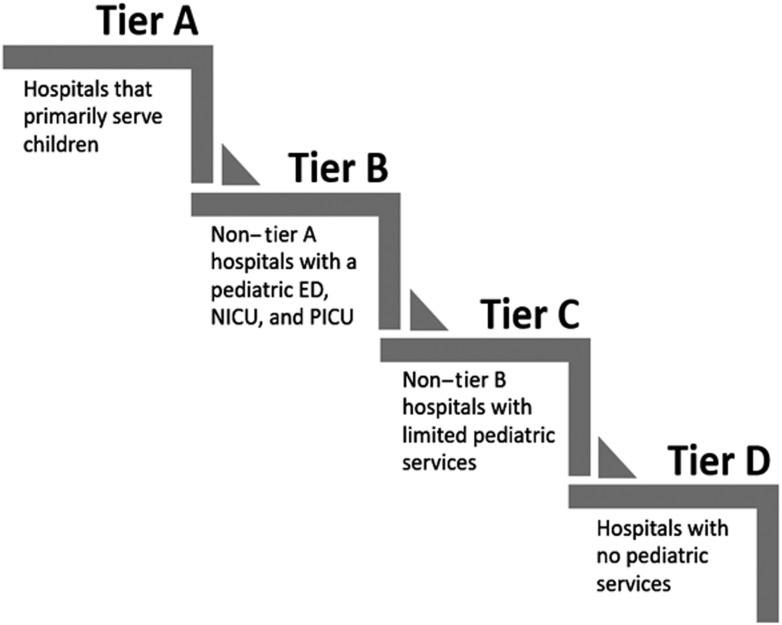
Using the sample of 4464 hospitals from the 2015 AHA survey, we categorized the hospitals into 4 different tiers (tiers A–D) on the basis of self-reported presence of pediatric-specific structural elements and service lines. All hospitals that answered yes to the question “Does the hospital restrict admissions primarily to children?” were classified as tier A. Tier B hospitals were defined as all non–tier A hospitals that had all of the following: a pediatric emergency department, NICU, and PICU. Tier C hospitals were defined as all non–tier B hospitals that had any pediatric services (ie, hospitals that had at least 1 of the following: pediatric beds, a NICU, a PICU, or a pediatric emergency department). The remaining hospitals were placed into tier D (Fig 1).
FIGURE 1.
Strategy for classifying hospitals into tiers A to D. ED, emergency department.
Characteristics of Hospitals in Each Tier
To characterize the hospitals within each tier, cross tabulations were performed between the 4 tiers and other pediatric-related variables in the AHA data set. Variables from the AHA data set used to describe the tiers included presence of general pediatric medical and surgical care, presence of full-time neonatal intensivists, presence of full-time pediatric intensivists, Council of Teaching Hospitals membership, presence of pediatric cardiac services, and hospital location (metropolitan, micropolitan, or rural). Hospitals were categorized as having pediatric cardiac services if they had at least 1 of the following: general pediatric cardiac services, pediatric cardiac surgery, pediatric diagnostic catheterization, pediatric interventional catheterization, or pediatric cardiac electrophysiology. In addition to these variables, we also calculated the mean number of pediatric hospital beds and the mean percentage of hospital beds devoted to pediatric patients in each tier. The percentage of hospital beds devoted to pediatric patients was calculated by summing the total number of pediatric beds (sum of general pediatric beds, NICU beds, neonatal intermediate care beds, and PICU beds), dividing it by the total number of hospital beds, and converting it to a percentage. χ2 tests and 1-way analysis of variance tests were used to assess between-tier differences in each of these characteristics. All analyses were conducted in SPSS version 24.4
Validating Classifications by Using Publicly Available Data
The tiers were then validated against publicly available data, which included Children’s Hospital Association (CHA) membership5; Children’s Oncology Group membership6; presence of an American College of Surgeons–verified pediatric trauma center (level I or II),7 availability of pediatric heart, liver, or kidney transplants8; presence of a NICU (level 3 or 4)9; availability of congenital heart surgery10; and participation in the American College of Surgeons National Surgical Quality Improvement Program–Pediatric (ACS NSQIP-P).11 Cross tabulations were performed between the tiers and each of these variables, and χ2 tests were used to assess significance.
Validating Classifications by Using Health Care Claims Data
The AHA hospital identification number was used to link the 2015 AHA data set to the 2015 HCCI data set. Approximately, 40% (n = 1769) of the AHA hospitals were represented in the HCCI claims data. Once merged, the percentage of hospital admissions that were pediatric was calculated for each tier and for the unclassified hospitals (ie, hospitals that did not receive a tier designation because of missing AHA data). This percentage was calculated by dividing the number of pediatric admissions (patients aged 0–18, excluding newborns) by the total number of admissions observed within each tier (including newborns). Newborns were purposefully excluded to avoid capture of delivery or birthing hospitals.
Results
Characteristics of Hospitals Within Each Tier
On the basis of the 2015 AHA data, 51 hospitals were classified as tier A, 228 as tier B, 1721 as tier C, and 1728 as tier D, and 736 hospitals could not be classified because of missing data. Almost all hospitals in tier A (98.0%) and tier B (99.6%) had general pediatric medical and surgical care, whereas fewer tier C (71.8%) and tier D (16.7%) hospitals had these services (P < .001). The proportion of hospitals that had pediatric cardiac services was greatest in tiers A and B (86.3% and 77.6%, respectively) and lowest in tiers C and D (11.1% and 2.5%, respectively; P < .001). Similarly, the proportion of hospitals that had full-time neonatal intensivists and full-time pediatric intensivists, were members of the Council of Teaching Hospitals, and were located in a metropolitan area was highest in tiers A and B. Furthermore, the average percentage of hospital beds devoted to pediatric patients was greatest in tier A (mean 84.5: SD ±19.2), followed by tier B (mean 15.8; SD ±7.9), tier C (mean 6.7; SD ±6.6), and tier D (mean 0) (P < .001). See Table 1 for more specific descriptive statistics.
TABLE 1.
Characteristics of Hospitals in Each Tier, Based on the 2015 AHA Survey
| Tier A (n = 51) | Tier B (n = 228) | Tier C (n = 1721) | Tier D (n = 1728) | Pa | |
|---|---|---|---|---|---|
| Restricts admissions to children, n (%)b | 51 (100) | 0 (0) | 0 (0) | 0 (0) | <.001 |
| NICU, n (%)b | 44 (86.3) | 228 (100) | 710 (41.3) | 0 (0) | <.001 |
| PICU, n (%)b | 43 (84.3) | 228 (100) | 134 (7.8) | 0 (0) | <.001 |
| Pediatric emergency department, n (%)b | 42 (82.4) | 228 (100) | 557 (32.4) | 0 (0) | <.001 |
| General pediatric medical and surgical care, n (%) | 50 (98.0) | 227 (99.6) | 1236 (71.8) | 289 (16.7) | <.001 |
| Pediatric cardiac services, n (%)c | 44 (86.3) | 177 (77.6) | 191 (11.1) | 44 (2.5) | <.001 |
| Full-time neonatal intensivists, n (%) | 29 (56.7) | 163 (71.5) | 360 (20.9) | 14 (0.8) | <.001 |
| Full-time pediatric intensivists, n (%) | 34 (66.7) | 167 (73.2) | 72 (4.2) | 2 (0.1) | <.001 |
| Member of the Council of Teaching Hospitals, n (%) | 16 (29.6) | 114 (50.0) | 97 (5.6) | 20 (1.2) | <.001 |
| No pediatric beds, mean (SD)d | 224.8 (130.7) | 95.4 (58.8) | 15.5 (18.5) | 0 (0) | <.001 |
| Percentage of pediatric beds, mean (SD)e | 84.5 (19.2) | 15.8 (7.9) | 6.7 (6.6) | 0 (0) | <.001 |
| Location, n (%)f | <.001 | ||||
| Metropolitan | 51 (100) | 223 (97.8) | 1220 (70.9) | 734 (42.5) | |
| Micropolitan | 0 (0) | 3 (1.3) | 287 (16.7) | 358 (20.7) | |
| Rural | 0 (0) | 2 (0.9) | 214 (12.4) | 636 (36.8) |
P values are based on χ2 and 1-way analysis of variance tests.
The variable was used to categorize hospitals into tiers.
Includes hospitals with any of the following services: pediatric cardiac services, cardiac surgery, pediatric diagnostic catheterization, pediatric interventional catheterization, pediatric cardiac electrophysiology.
Includes NICU beds, PICU beds, neonatal intermediate care beds, and general pediatric medical and surgical beds.
Percentage of total hospital beds devoted to pediatric patients ((NICU beds + PICU beds + neonatal intermediate care beds + general pediatric medical and surgical beds)/the total number of hospital beds.
Metropolitan areas contain at least 50 000 people, micropolitan areas contain at least 10 000 but <50 000 people, and rural areas contain <10 000 people.
Validating Classifications by Using Publicly Available Data
The tier classifications were then validated by using publicly available hospital data (Table 2). The majority of tier A hospitals were members of the CHA (90.2%), approximately half of tier B hospitals were members (52.6%), and few tier C, tier D, and unclassified hospitals were members (1.2%, 0.1%, and 1.4%, respectively; P < .001). Similar trends were seen for Children’s Oncology Group membership, in which 80.2% of tier A, 40.8% of tier B, 0.8% of tier C, 0.1% of tier D, and 1.0% of unclassified hospitals were members (P < .001). Also, 47.3% of hospitals in tier A, 24.1% of hospitals in tier B, 0.7% of hospitals in tier C, 0.1% of hospitals in tier D, and 0.4% of unclassified hospitals were pediatric trauma level 1 or 2 centers (P < .001). Furthermore, pediatric transplants (heart, liver, and kidney) and congenital heart surgery were most common among tier A hospitals. The proportion of hospitals with level 3 or 4 NICUs was highest in tiers A and B (84.3% and 86.8%, respectively) and lowest in tier C, tier D, and unclassified hospitals (26.1%, 0.9%, and 7.9%, respectively; P < .001). ACS NSQIP-P membership also varied by tier, with 76.1% of the hospitals in tier A, 23.7% of the hospitals in tier B, 0.1% of the hospitals in tier C, none of the hospitals in tier D, and 0.4% of unclassified hospitals having this designation (P < .001).
TABLE 2.
Characteristics of Hospitals in Each Tier, Based on Publicly Available Data Sources
| Tier A (n = 51) | Tier B (n = 228) | Tier C (n = 1721) | Tier D (n = 1728) | Unclassified (n = 736) | Pa | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| CHA5 | 46 (90.2) | 120 (52.6) | 20 (1.2) | 1 (0.1) | 10 (1.4) | <.001 |
| Children’s Oncology Group6 | 41 (80.2) | 93 (40.8) | 14 (0.8) | 1 (0.1) | 7 (1.0) | <.001 |
| Trauma level7 | ||||||
| 1 | 19 (37.3) | 27 (11.8) | 5 (0.3) | 1 (0.1) | 0 (0) | <.001 |
| 2 | 5 (10.0) | 28 (12.3) | 7 (0.4) | 0 (0) | 3 (0.4) | <.001 |
| Transplants8 | ||||||
| Heart | 27 (53.0) | 26 (11.4) | 5 (0.3) | 1 (0.1) | 1 (0.1) | <.001 |
| Liver | 21 (41.2) | 25 (11.1) | 3 (0.2) | 1 (0.1) | 1 (0.1) | <.001 |
| Kidney | 29 (56.9) | 60 (26.3) | 7 (0.4) | 4 (0.2) | 2 (0.3) | <.001 |
| Congenital heart surgery10 | 34 (66.7) | 33 (14.5) | 2 (0.1) | 0 (0) | 1 (0.1) | <.001 |
| NICU level 3 or 49 | 43 (84.3) | 198 (86.8) | 450 (26.1) | 15 (0.9) | 58 (7.9) | <.001 |
| ACS NSQIP-P11 | 35 (76.1) | 54 (23.7) | 2 (0.1) | 0 (0) | 3 (0.4) | <.001 |
P values are based on χ2 tests.
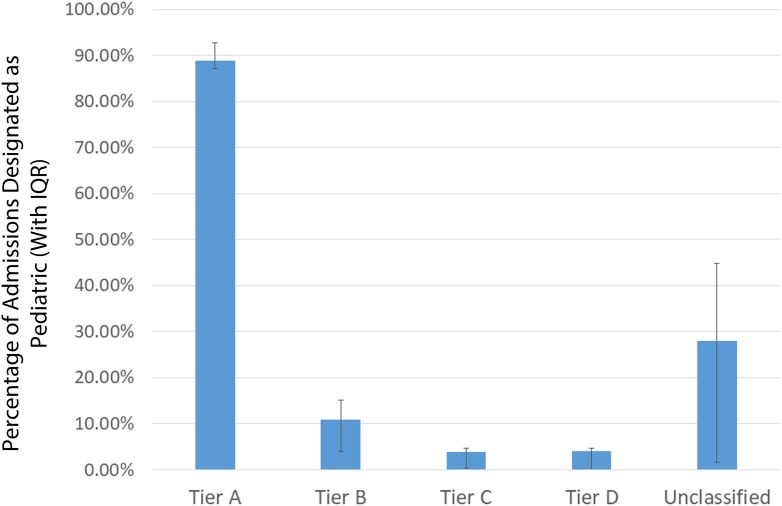
Validating Classifications by Using Health Care Claims Data
The tier classifications were then validated by using 2015 HCCI claims data. Of the hospitals that were in the HCCI data set, 36 were tier A, 215 were tier B, 1011 were tier C, 344 were tier D, and 163 were unclassified hospitals. These figures were stable when assessing HCCI data from 2010 to 2014. The percentage of admissions that were pediatric was highest in tier A (88.95% with an interquartile range (IQR) of 87.1%–92.8%). Pediatric admissions were substantially lower in tier B (10.96%; IQR 4.0%–15.1%), tier C (3.92%; IQR 0.4%–4.7%), and tier D (3.98%; IQR 0%–4.7%). Additionally, 28.06% (IQR 1.6%–44.8%) of admissions at unclassified hospitals were pediatric (Fig 2).
FIGURE 2.
Percentage of admissions that are designated pediatric, by tier.
Discussion
In this study, we developed a reproducible method to classify hospitals using AHA survey data. This methodology was then validated by using publicly available hospital data as well as health care claims data. Our validations reveal that hospitals in tier A have the most comprehensive pediatric services and have substantially higher pediatric admissions than hospitals in the other tiers, suggesting that these 51 hospitals are CHs. Tier A hospitals are most likely to have level I pediatric trauma centers, conduct organ transplants, and conduct congenital heart surgery and are most likely to have memberships in the CHA, Children’s Oncology Group, and ACS NSQIP-P. Many of the tier B hospitals have similar pediatric services and memberships, but they have a lower proportion of admissions that are pediatric (10.96% in tier B versus 88.95% in tier A). The provision of comprehensive pediatric services and low pediatric admissions suggests that tier B hospitals are general hospitals with children’s units. Therefore, for specific studies and research questions, investigators may elect to consider both Tier A and Tier B hospitals as CHs rather than only considering tier A hospitals as CHs. Although stand-alone children’s hospitals may be directly of interest in some studies, our analysis reveals that limiting the definition of CHs only to those with CHA membership will exclude a significant number of hospitals for which comparable pediatric services are available. tier C and D hospitals have minimal pediatric services, and virtually none of these hospitals are members of the CHA, Children’s Oncology Group, or ACS NSQIP-P. Therefore, we would categorize tier C and D hospitals as NCHs.
We were able to conduct these analyses because the claims data provider that we used, HCCI, provided hospital-level matching on features abstracted from the AHA survey data and from our manual designations of publicly available pediatric services. This level of collaboration with administrative and claims data providers is rare, and health services researchers are left to use proportions of pediatric admissions to reliably differentiate CHs from NCHs. Our study suggests that this practical application of the proportion of pediatric admissions (or discharges) is valid. For example, our study revealed that nearly 90% of admissions at tier A hospitals were pediatric admissions, compared with ∼≤11% at tier B, C, and D hospitals. Thus, distinguishing between hospital types is possible even when hospital-level identifiers are not available. Although possible, we would advise caution of additional stratifications of hospital types, such as tier B versus tier C, by using discharge proportions alone.
Authors of previous studies investigating differences between CHs and NCHs used a variety of strategies to classify hospitals. One commonly used method for determining CH status is participation in the Pediatric Health Information System, which is a pediatric database that includes clinical and resource use data for 49 freestanding CHs that are members of the CHA.12–16 CHA membership is also commonly used as a method to determine CH status, with >200 US hospitals currently having this membership.17,18 Another commonly used database is the Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID).19,20 This database includes pediatric hospital discharge abstracts from 46 states, with all freestanding CHs being classified as CHs and all other hospitals being classified as NCHs. The KID is typically released in 3-year intervals, but the definition used to classify hospitals in the 2012 version dramatically changed compared with the definition used in previous versions, making multiyear comparisons challenging.21 Other methods to identify CHs include the availability of pediatric services such as pediatric trauma centers.17,22
Although commonly used, these previous classification strategies have several limitations. First, the Pediatric Health Information System and KID data sets only include a subset of US hospitals. Furthermore, these strategies are often focused on freestanding CHs and do not granularly account for varying types of pediatric hospitals, such as children’s units within general hospitals. In most studies, children’s units are placed in the NCH category, which may not accurately represent the level of pediatric care provided at these facilities. Furthermore, the lack of a standardized classification method limits cross-study comparisons.
The classification methodology proposed in this study addresses many of the limitations with previous strategies to distinguish CHs from NCHs. First, the AHA survey profiles a universe of >6400 hospitals each year, allowing investigators to easily classify all hospitals in the United States using a single data source. This method may be replicated for all years of the AHA survey. Additionally, the use of a standardized classification strategy will allow for cross-study comparisons. Granular comparisons of care delivery at CHs versus NCHs are needed to inform health care delivery system structure and resource deployment. Trends toward regionalization of care and increasing care complexity at CHs must be critically appraised, with hospitals categorized in a reproducible and validated fashion.23 Furthermore, the use of up to 4 tiers gives investigators the opportunity to consider varying types of pediatric hospitals, such as freestanding children’s centers and children’s units within general hospitals. Investigators can consider tiers separately or combine them on the basis of specific research questions and analyses.
Although we present a validated strategy to classify hospitals, there are some limitations to this method. Because the tier classifications rely on self-reported data collected by the AHA survey, there is the potential for hospitals to be misclassified. Additionally, there were many hospitals (n = 736) in the AHA survey that had missing data, making it impossible to classify these hospitals into tiers. Although the response rate for the AHA survey is high, the response rate for individual questions is frequently low (<50%).24 To combat the high amounts of missing data in the AHA survey, survey administrators conduct imputation and estimation of some variables on the basis of previous years, but they do not estimate variables related to service offerings, beds, and facilities (ie, variables used to categorize hospitals in this study).24 Despite this limitation, we were able to classify the vast majority of non–specialty hospitals in the United States (n = 3728) and validate the tiers using health care claims data. The percentages and interquartile ranges of pediatric discharges obtained from the HCCI also suggest that the bulk of the unclassified hospitals are NCHs. A final limitation of our proposed methodology is that many administrative and claims data providers strip hospital-level identifiers that facilitate linkage to AHA data. Under ideal circumstances, data custodians will provide linkages with key data elements before providing investigators with fully stripped data for further analyses. If this is not feasible, using proportions of pediatric admissions and discharges and searching for critical services of interest, as proposed in this study, may be possible.
Conclusions
On the basis of validations with publicly available hospital information and health care claims data, using the AHA survey is a feasible and valid method for classifying hospitals into CH and NCH categories by using a reproducible multitiered system. For specific studies and research questions, investigators may elect to consider both Tier A and Tier B hospitals as CHs. When hospital-level linkages are not available, using proportions of pediatric admissions and discharges may reliably distinguish CHs from NCHs. This study addresses many of the limitations with previous classification strategies by allowing investigators to classify virtually all hospitals in the United States into CH and NCH categories using a single data source. The multitiered system also gives researchers the flexibility to investigate between-tier differences or combine tiers on the basis of specific research questions.
Footnotes
Ms Piper assisted with conceptualizing the study, conducted analyses, and drafted the initial manuscript; Dr McCarthy conceptualized and designed the study, conducted analyses, and reviewed and revised the manuscript; Drs Baxter and Raval conceptualized and designed the study, coordinated data analysis, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant R01HS024712 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.National Association of Children’s Hospitals and Related Institutions. All Children Need Children’s Hospitals. Alexandria, VA: National Association of Children’s Hospitals and Related Institutions; 2007 [Google Scholar]
- 2.American Hospital Association. AHA Annual Survey. Chicago, IL: American Hospital Association; 2015 [Google Scholar]
- 3.Health Care Cost Institute. Health Care Cost and Utilization Dataset. Washington, DC: Health Care Cost Institute; 2015 [Google Scholar]
- 4.IBM Corporation. IBM SPSS Statistics for Windows [computer program]. Version 24. Armonk, NY: IBM Corporation; 2016 [Google Scholar]
- 5.Children’s Hospital Association. Children’s hospital directory. 2017. Available at: https://www.childrenshospitals.org/Directories/Hospital-Directory. Accessed April 10, 2019
- 6.Children’s Oncology Group. Locations. 2017. Available at: https://childrensoncologygroup.org/index.php/locations/. Accessed April 10, 2019
- 7.American College of Surgeons. Searching for verified trauma centers. 2017. Available at: https://www.facs.org/search/trauma-centers. Accessed April 10, 2019
- 8.Scientific Registry of Transplant Recipients. Transplant center search results. Available at: https://www.srtr.org/transplant-centers/. Accessed April 10, 2019
- 9.American Academy of Pediatrics. NICU search.2017. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/nicuverification/Pages/NICUSearch.aspx. Accessed April 10, 2019
- 10.The Society of Thoracic Surgeons.Congenital heart surgery public reporting. 2017. Available at: http://publicreporting.sts.org/chsd?title=&field_state_value=All&page=0. Accessed April 10, 2019
- 11.American College of Surgeons. Searching for NSQIP participating hospitals. 2017. Available at: https://www.facs.org/search/nsqip-participants. Accessed April 10, 2019
- 12.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children’s hospitals in the United States. Clin Infect Dis. 2009;49(1):65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feudtner C, Pati S, Goodman DM, et al. State-level child health system performance and the likelihood of readmission to children's hospitals. J Pediatr. 2010;157(1):98–102.e1 [DOI] [PubMed] [Google Scholar]
- 15.Morse RB, Hall M, Fieldston ES, et al. Hospital-level compliance with asthma care quality measures at children’s hospitals and subsequent asthma-related outcomes. JAMA. 2011;306(13):1454–1460 [DOI] [PubMed] [Google Scholar]
- 16.Pasquali SK, He X, Mohamad Z, et al. Trends in endocarditis hospitalizations at US children’s hospitals: impact of the 2007 American Heart Association Antibiotic Prophylaxis Guidelines. Am Heart J. 2012;163(5):894–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spinella PC, Dressler A, Tucci M, et al. ; Pediatric Acute Lung Injury and Sepsis Investigators Network. Survey of transfusion policies at US and Canadian children’s hospitals in 2008 and 2009. Transfusion. 2010;50(11):2328–2335 [DOI] [PubMed] [Google Scholar]
- 18.Feudtner C, Womer J, Augustin R, et al. Pediatric palliative care programs in children’s hospitals: a cross-sectional national survey. Pediatrics. 2013;132(6):1063–1070 [DOI] [PubMed] [Google Scholar]
- 19.Merenstein D, Egleston B, Diener-West M. Lengths of stay and costs associated with children’s hospitals. Pediatrics. 2005;115(4):839–844 [DOI] [PubMed] [Google Scholar]
- 20.Tian Y, Heiss KF, Wulkan ML, Raval MV. Assessment of variation in care and outcomes for pediatric appendicitis at children’s and non-children’s hospitals. J Pediatr Surg. 2015;50(11):1885–1892 [DOI] [PubMed] [Google Scholar]
- 21.Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP KIDS’ Inpatient Database (KID). Rockville, MD: Agency for Healthcare Research and Quality; 2015 [Google Scholar]
- 22.Ochoa C, Chokshi N, Upperman JS, Jurkovich GJ, Ford HR. Prior studies comparing outcomes from trauma care at children’s hospitals versus adult hospitals. J Trauma. 2007;63(suppl 6):S87–S91; discussion S92–S95 [DOI] [PubMed] [Google Scholar]
- 23.Short HL, Sarda S, Travers C, Hockenberry JM, McCarthy I, Raval MV. Trends in common surgical procedures at children’s and nonchildren’s hospitals between 2000 and 2009. J Pediatr Surg. 2018;53(8):1472–1477 [DOI] [PubMed] [Google Scholar]
- 24.Mullner R, Chung K. The American Hospital Association’s Annual Survey of Hospitals: a critical appraisal. J Consum Mark. 2002;19(7):614–618 [Google Scholar]