Abstract
OBJECTIVES:
Pediatric discharge from the inpatient setting is a complex, error-prone process. In this study, we evaluated the outcomes of using a standardized process for hospital discharge of pediatric patients.
METHODS:
A 1-year pre- and postintervention pilot study was designed to improve discharge transition of care. The bundle intervention, facilitated by advanced practice providers, included risk identification and intervention. Process and outcome metrics included patient satisfaction measures on the discharge domain (overall discharge, speed of discharge process, whether they felt ready for discharge), use of handouts, scheduling of follow-up appointments, and postdischarge phone call.
RESULTS:
Significant improvements were found in all aspects of patient satisfaction, including speed of the discharge process and instructions for discharge, discharge readiness, and the overall discharge process. Length of stay decreased significantly after intervention. The checklist identified ∼4% of discharges without a correct primary care physician. Significant differences were found for scheduled primary care appointment before discharge and patients receiving handouts. The bundle identified risks that may complicate transition of care in approximately half of the patients. Phone communication occurred with almost half of the patients after discharge.
CONCLUSIONS:
Integration of an evidence-based discharge checklist can improve processes, increase delivery of patient education, and improve patient and family perceptions of the discharge process. Involvement of key stakeholders, use of evidence-based interventions with local adaptation, and use of a consistent provider responsible for implementation can improve transitions of care.
Facilitating inpatient pediatric discharges from the inpatient to home setting is a multifaceted and complex process.1 Approximately 1 in 5 patients has an adverse event in the discharge process; more than half of these adverse events are preventable.2,3 Miscommunication continues to be a concern in many of the preventable adverse effects.4 Patients’ incomplete understanding of their clinical diagnosis and treatment plan on discharge can also contribute to adverse events after discharge.5 In 2015, local needs assessment, gap analysis, and group consensus on the need for improvement in discharge processes inspired the design of a project at our center. Varied discharge planning tool kits have been promoted as helpful in addressing discharge efficiency,6 reducing readmissions,7 or addressing transitions of care gaps.8,9 Our hospital medicine focus led us to choose to model our interventions after the Society of Hospital Medicine’s pediatric discharge tool kit because it was pediatric specific and included interventions to assess and reduce transition of care risks.10 In this study, we evaluated the outcomes of using a standardized process for hospital discharge of pediatric patients.
Methods
Context
This study was performed from July 2014 to June 2017 on the general inpatient pediatric wards of a children’s hospital within a general hospital. Our children’s hospital is a rural academic center that serves a geographic area that includes West Virginia, western Maryland, southern Pennsylvania, and eastern Ohio, with ∼1500 annual admissions to the pediatric ward (non-ICUs). The primary language spoken is English (98%), and the payor mix is divided as 50% Medicaid and 50% all other payors. The average daily census on the pediatric ward is 15, with an average of 5 daily discharges. The ward patient care team is a traditional model that consists of a trainee or nurse practitioner, attending pediatric hospitalist, and bedside nurse. Multidisciplinary team members, including the pharmacist, care manager, and social worker, are involved in discharge. Existing admission processes included health literacy screening completed by the nursing staff using the Pediatric Caregiver Health Literacy Screening tool.11 Existing discharge processes include securing follow-up postdischarge appointments with the primary care physician (PCP) before discharge and giving disease-specific information to patients’ families via handouts.
Planning the Intervention
A 1-year preintervention (July 2014–June 2015) and a 1-year postintervention (July 2016–June 2017) pilot study was designed to assess rates for readmission, caregiver satisfaction, primary care appointments (scheduled before discharge), and caregiver education before and after implementation of a discharge bundle that included tools (Supplemental Tables 5 and 6) used by advanced practice providers (APPs). The planning phase (July 2015–June 2016) included local self-assessment, background data review, stakeholder buy-in and engagement, multidisciplinary team involvement, process mapping, and shared norming. An interdisciplinary team reviewed evidence-based literature and local processes and created the intervention for the study. Members of the local center for quality outcomes were involved in the initial conceptualization of this project and received results intermittently throughout the project. Local and external mentors, both nurses and physicians with expertise in process improvement and study design, facilitated the implementation. External mentors facilitated phone calls to address barriers and approaches toward team roles and implementation of interventions. This study included all patients admitted to our children’s hospital pediatric ward across all ages (0–21 years).
Improvement Activities
The interventions were focused on the 2 key drivers: (1) use of evidence-based interventions with local adaptation and (2) key stakeholder buy-in, shared norming, and use of a consistent provider responsible for implementation.
Evidence-Based Interventions With Local Adaptation
We adapted core elements of the discharge intervention bundle from the Society of Hospital Medicine PediBOOST tool kit.10 This tool kit contains a set of comprehensive expert-consensus and evidence-based interventions to improve the transition of care of children from the inpatient to outpatient setting. Our bundle included 2 tools that were used to address known gaps in both the process and quality of discharge: a risk assessment and an intervention. These tools incorporated the PediBOOST tool kit with other existing published tools and recommended best practices.8,10,12 The format and acronyms chosen were locally determined by the team to promote engagement in the new process steps. The risk assessment was used to address items such as high-risk medication, socioeconomic barriers, chronic conditions, lack of a PCP, and lack of transportation and was given the acronym DISCHARGE (drugs, individual, socioeconomic, chronic disease, health literacy, acute disease, readmission, general, and equipment) (Table 1). The intervention included tasks completed by APPs and was given the acronym IMPACT (interdisciplinary family meeting; medication review, enhanced; patient education [handouts and videos]; appointments [scheduled before discharge with PCP]; communication [patient call after discharge]; and teach-back, focused) (Table 2). This tool also included a space for PCP identification and documentation in the electronic medical record (EMR) during family-centered rounds (FCRs). In addition to the DISCHARGE risk assessment checklist and the IMPACT intervention, the full discharge bundle also included an intent-to-discharge order set. This order set was created with nursing input and included instructions to schedule appointment and instructions for the nurse to complete relevant teaching. APPs received patient sign-out early in the morning from the overnight staff. Before safety walkrounds and the daily team huddle, APPs reviewed patient data in the EMR. APPs were empowered to expedite the discharge process by entering orders that were in keeping with care plans agreed on in previous rounds, such as changing medications from an intravenous to oral route, stopping or decreasing intravenous fluids, or ordering discharge medication teaching. They performed a quick screening for DISCHARGE risk factors by reviewing the medication list, the literacy screening result, recent admissions and the chronic medical history or problem list, intake questions related to access and insurance, existing or new equipment needs, and the current clinical condition. Items were then reviewed with the team on rounds and modified if needed by team consensus. A given category was noted as having a risk if any 1 of the items was identified in that category. Any risk factor triggered the IMPACT intervention.
TABLE 1.
DISCHARGE Risk Assessment Checklist by Category
| Risk | Criteria |
|---|---|
| Drugs | High-risk medicationsa |
| >5 medications concurrently in use | |
| Compounded medications | |
| Individual | Newborn (0–28 d of age) |
| Infant (28 d to 1 y of age) | |
| Adolescent (13–18 y of age) | |
| Socioeconomic | No insurance |
| No transportation | |
| Child Protective Services involvement | |
| Not discharged to a family home | |
| Chronic diseaseb | Asthma |
| Cystic fibrosis | |
| Bronchopulmonary dysplasia or chronic lung disease of infancy | |
| Diabetes mellitus | |
| Inflammatory bowel disease | |
| Neuromuscular disorders | |
| Seizure disorders | |
| Health literacyc | Low health literacy |
| Acute disease | Conditions not yet resolved (patient is improved but not at baseline at discharge) |
| Readmissiond | 30-d readmission |
| General | Lack of PCP |
| Equipment | Durable medical equipment or outpatient infusion required |
One or more criteria met in 1 category would equal risk in that category.
Per the Institute for Safe Medication Practices.31
The chronic conditions list is adapted from Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655. The most common conditions seen at our institution are noted above as examples.
Low health literacy was determined by using our Pediatric Caregiver Health Literacy Screening tool.11
This hospitalization occurred within 30 d of a previous hospitalization.
TABLE 2.
IMPACT Intervention Elements
| I for interdisciplinary family meeting |
| I for interdisciplinary family meeting |
| M for medication review, enhanced |
| P for patient education (handouts and videos) |
| A for appointments (scheduled before discharge with PCP) |
| C for communication (patient call after discharge) |
| T for teach-back, focused |
Key Stakeholder Buy-in, Shared Norming, and Use of a Consistent Provider Responsible for Implementation
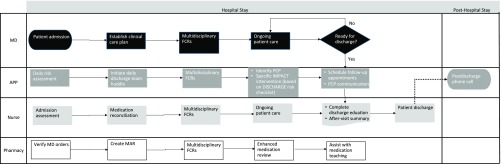
Two APPs who were already an integral part of our team were selected to perform this process because of their consistent schedule and familiarity and continuity with our patient care team. APPs had been hired to perform clinical work and had existing quality goals and acted as liaisons between different rotating members of the team. Because of this expectation for involvement in quality projects, the APPs were a natural fit for this initiative. Team members (including hospitalists, APPs, and residents) were trained via webinars and conference calls (every other month) with an external mentor. The training also included a site visit conducted by the external mentor. The tool was used in paper form during and after FCRs. Existing disease-specific handouts were given out by the discharge nurse. The APPs communicated with the PCP to schedule follow-up appointments, review the hospitalization, and discuss transition of care needs. The APPs also completed the postdischarge phone call 24 to 48 hours after discharge for every patient who was discharged. Phone call scripts included clarification of the diagnosis, medications, follow-up care coordination, and warning signs. The Agency for Healthcare Research and Quality postdischarge phone call script was used (available at https://www.ahrq.gov/professionals/systems/hospital/red/toolkit/redtool5.html). A process map of the APP workflow is noted in Fig 1.
FIGURE 1.
Workflow process map. MAR, medication administration record.
Study of the Interventions
Demographic, readmission, and DISCHARGE risk assessment checklist data were entered into a spreadsheet by a research coordinator on a weekly basis. Patient satisfaction measures (readiness for discharge, speed of the discharge process, instructions for the discharge process, and the overall discharge process) were obtained from a selection of Press Ganey survey results.
Measures
Data collected included basic demographic information and process and outcome metrics, including patient satisfaction measures on the discharge domain (the overall discharge process, speed of the discharge process, and readiness for discharge), readmissions, use of handouts, scheduling of follow-up appointments, and the postdischarge phone call. An additional process metric was adherence to our DISCHARGE risk assessment checklist. A balancing measure chosen was length of stay (LOS). Definition of measures and collection methods are noted in Table 3.
TABLE 3.
Key Project Measures
| Measurement Category | Measure | Description | Data Collection (Source) |
|---|---|---|---|
| Process measures | Percentage of discharged patients with postdischarge phone calls | A measure of process compliance for operations calculated as No. patients with a postdischarge phone call divided by No. discharges | Chart review (research assistant) |
| Use of electronic handouts | A measure of process compliance for discharge education calculated as No. patients with electronic handouts divided by No. discharges | EMR data extraction (quality outcomes department) | |
| Percentage of discharged patients with a follow-up appointment scheduled before discharge | A measure of process compliance for successful after-hospital planning calculated as No. patients with a scheduled follow-up appointment before discharge divided by No. discharges | EMR data extraction (research assistant) | |
| DISCHARGE risk assessment checklist adherence | A measure of process compliance for discharge risk assessment checklist completion calculated as No. discharges with completion of the discharge risk assessment checklist divided by No. discharges | Chart review (research assistant) | |
| Outcome measures | Patient satisfaction | A measure of patient satisfaction for the inpatient pediatric unit measured by using the discharge domain of the Press Ganey inpatient survey | Press Ganey survey data (quality outcomes department) |
| Readmission rate | A measure of the percentage of discharged patients who are readmitted to the hospital with the same diagnosis-specific grouping within 7 d of discharge | EMR data extraction (quality outcomes department) | |
| Balancing measures | LOS | A measure of duration (in d) of the hospital stay | EMR data extraction (quality outcomes department) |
Analysis
Data were analyzed via SAS version 9.4 (SAS Institute, Inc, Cary, NC). Basic descriptive statistics were presented. Seven-day readmissions, primary care follow-up appointments, and use of handouts were analyzed with the χ2 test. Patient satisfaction data were analyzed by using the t test. P < .05 was considered statistically significant.
Ethical Considerations
Local institutional review board approval was obtained with a full waiver of consent before the start of the study (8256491). There were no conflicts of interest. The project was supported by the center for quality outcomes at our institution.
Results
There were 1321 patients in the preintervention group and 1413 patients in the postintervention group. There were no significant differences in demographics for sex (female sex preintervention: 45.9%; female sex postintervention: 47.5%; P = .29), case-mix index (preintervention: 1.293; postintervention: 1.283; P = .34), or insurance type (Medicaid preintervention: 50.9%; Medicaid postintervention: 52.2%; P = .4) between pre- and postintervention groups. However, LOS decreased significantly after the intervention (preintervention: 4.08 days; postintervention: 3.43 days; P = .005).
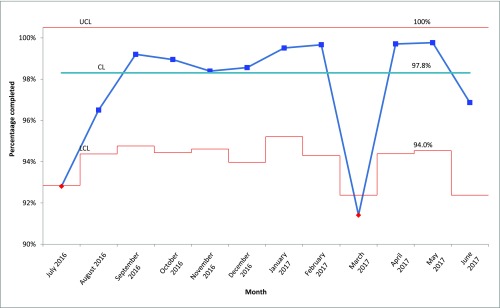
The adherence rate for using the DISCHARGE risk assessment checklist was 97.8% (1381 of 1413 discharges). We noted special cause in March 2017 because of APP staffing issues (Fig 2). Of the risk categories, individual (26.3%), chronic illness (15.9%), drugs (13.2%), and healthy literacy and acute illness (each 8%) were most commonly noted, with socioeconomic (6%), readmission (3.5%), equipment (2.8%), and general (1.3%) risk categories reported less often. Two or more risk factors were noted in 25% (355) of discharges. The individual elements of the IMPACT intervention to be completed for all discharges and for those with specific risks noted are in Table 4. Significant differences were found, with improvement for both scheduled primary care appointment before discharge and patients receiving handouts (both P < .0001). Preintervention data were not tracked for other IMPACT interventions; thus, no comparisons can be made for these items. Of those with specific risks, completion of targeted IMPACT interventions is shown in Supplemental Table 7. Patient follow-up calls and appointments were more often completed in those with literacy and equipment risks, but rates were high (>70% for appointment scheduled in 8 of 9 categories; >40% for postdischarge calls in 7 of 9 categories. Interdisciplinary meetings were not often completed but were most frequently performed for patients with history of readmission. Teach-back also was most commonly performed for this population.
FIGURE 2.
Adherence to DISCHARGE risk assessment checklist completed (p-chart). CL, center line; LCL, lower control limit; UCL, upper control limit.
TABLE 4.
Percentage of Interventions Performed
| Intervention | Percentage of All Discharges With Intervention Performed, % | P | |
|---|---|---|---|
| Preintervention | Postintervention | ||
| All discharges | |||
| Patient handouts | 17.9 | 77.1 | <.0001 |
| Appointments (scheduled before discharge with PCP) | 33 | 71.6 | <.0001 |
| Communication (with patient after discharge) | Not tracked | 42.8 | — |
| Triggered by risk | |||
| Teach-back, focused | Not tracked | 24.9 | — |
| Medication review, enhanced | Not tracked | 16.2 | — |
| Interdisciplinary meeting | Not tracked | 3.1 | — |
—, not applicable.
Significant differences were found in aspects of patient satisfaction, including speed of the discharge process (preintervention: 78.9 [SD 29.9]; postintervention: 82.6 [SD 27.6]; P = .008), instructions for discharge (preintervention: 79.7 [SD 29.4]; postintervention: 88.6 [SD 21.7]; P < .0001), discharge readiness (preintervention: 79.7 [SD 27.3]; postintervention: 88.6 [SD 21.3]; P < .0001), and the overall discharge process (preintervention: 79.4 [SD 23.1]; postintervention: 86.1 [SD 17.8]; P < .0001). There was no statistically significant decrease in 7-day readmissions (preintervention: 2.7%; postintervention: 2.1%; P = .305).
One unexpected outcome was that many patients without PCPs were identified and care was reestablished. The checklist helped us identify 53 patients from 1413 discharges (3.75%) with an incorrect or no PCP in the EMR.
Discussion
In this study of discharge process changes, a simple checklist and interventions embedded into consistent workflows were associated with significant increases in scheduled follow-up visits before discharge (operations) and the number of patients given handouts (education) as well as improved patient and family perceptions of and readiness for discharge (satisfaction) and the identification of risk factors amenable to targeted interventions. We achieved this and documented an unanticipated shorter LOS. We identified risks that may complicate transition of care in approximately half of our patients, and we were able to address these risks in ∼40% of them. Approximately one-quarter of patients had ≥2 risk factors. We reached almost half of our patients by phone after discharge who had specific risks related to health literacy, acute illness resolution, and equipment. Although standardizing and realigning processes alone might have impacted our LOS, we believe the addition of risk assessment and other changes in what and how the processes were performed might have led to the changes observed in patient and family satisfaction.
The discharge process may vary from provider to provider and may result in patient and family anxiety, uncertainty, and a lack of overall health education.13 Using a standardized teaching tool on discharge has been shown to improve patient satisfaction.13 It prevents the loss of information with handovers. Communication and education have the biggest impact on patient satisfaction.14–18 In our study, we used APPs to standardize the discharge process. The use of a team member with a consistent role in various health care processes is not new. Dunn and Rogers1 described a role of a pediatric nurse practitioner as a liaison between nursing and medicine to facilitate and expedite the discharge process to safely, efficiently, and effectively discharge pediatric patients. Tran et al18 reported that the repeated supplying of clinically based information by a medical student significantly improved a range of satisfaction measures. Taylor et al14 demonstrated that a patient liaison nurse provided education, increased communication, and improved Press Ganey scores in the emergency department. Local contextual factors influence health care quality.19 In our teaching facility, residents and attending hospitalists rotate on and off the ward every few weeks. Thus, the APP is uniquely positioned to provide continuity and consistency in the discharge processes. We were unable to assess whether our positive process and patient satisfaction outcomes were due specifically to APPs or to having few and consistent team members responsible for discharge actions. Although our tools provided standardization, it is likely that having a team member with advanced skills allowed for more effective risk assessments. Institutions may wish to formalize the expectation for APPs or other team members to integrate quality initiative work into their job expectation. This, and the whole team approach toward addressing risks and implementing actions, led to our improvements in patient education and discharge processes, which may affect patient and family perceptions of discharge readiness.
In quality improvement, checklists provide a lower level of process reliability compared with true forcing functions, such as lockout drawers that require a code to open them. However, done in a microsystem in which each team member has the expectation to ask and address checklist items, these tools can be highly effective. Checklists may affect provider workflow and should be carefully designed with a concise list of judiciously selected elements that are aimed at reducing errors of omission and improving throughput.20 High-reliability organizations in different industries have used checklists as memory aids and to assist with decision-making.21 Checklists can improve adherence to following various procedures in different specialties of medicine.21 In pediatrics, checklist use in FCRs can increase performance of individual elements of FCRs, which has been shown to increase family engagement and families’ perceptions of patient safety.22 With our study, we suggest that a comprehensive discharge intervention can help improve the discharge process as well as patient satisfaction, patient education, and primary care follow-up appointments. Although we did not obtain data on PCP follow-up appointment completion, scheduling a postdischarge follow-up appointment before discharge has been shown to increase the attendance rate by 25%.23 These phone calls to PCPs also served as an opportunity to communicate with the PCP about the reason for hospitalization, pending laboratory tests, and a follow-up plan. Our study was designed to use the same APPs to ensure a standardized process. We believe that using APPs for this process and engaging the team in the creation of the checklist worked well and were major strengths in ensuring a smooth process at our site. Starting discharge planning early, engaging the patient in the discharge education process, and creating a forum for multidisciplinary review of patient’s discharge planning needs can reduce the LOS.24,25
Reducing readmissions has become a focal point for hospital systems nationwide, but there is a lack of high-quality evidence throughout the literature on how to improve the discharge process. Evidence suggests that if more needs are addressed during discharge transition of care, the discharge will be more effective.26–28 Although we were not able to decrease our readmission rate, it is not clear whether this rate would further improve if we increased the percentage of successful interventions completed before discharge. Our hospital is the only “complete” tertiary care pediatric facility in the rural state. Some of these readmissions may be preventable. However, even readmissions related to discharge failures deemed to be under health care system control may be unavoidable because of the paucity of local resources. As shown in other studies, readmissions may not be a good surrogate for quality or adequacy of pediatric discharge transitions of care.29
Limitations
Our study was limited to a pediatric patient population of a single institution in West Virginia and may not be reproducible in other institutions across the nation. Our assessment tools were based on published works, existing tool kits, and commonly used surveys but were modified for local context with team agreement. Although Press Ganey is the largest vendor of patient satisfaction surveys and is used in ∼40% hospitals in the United States, it is not the only survey tool or method used in hospital settings. It is used to measure and compare hospitals and providers in 10 domains of patient care.30 Our site’s response rate has been consistent at 25%, which is similar to national rates for this tool. Despite its inherent limitations, complexities, and potential response biases, it can be helpful to identify domains for improvement.13
Not all IMPACT intervention items were completed for all patients. Availability of APPs for night discharges and discharges during weekends may have limited our ability to complete interventions, particularly making follow-up appointments. In addition, the sustainability of the process is dependent on APPs being present, as we noted with our March 2017 special cause variation in the DISCHARGE checklist completion rate. We did not have baseline data for all metrics we assessed in the postintervention period, so we were unable to determine if our interventions resulted in the outcomes for these metrics. We did not have access to completed PCP follow-up visit information and therefore cannot assess whether having these appointments scheduled before discharge made any impact. Finally, we are not aware of any competing initiatives at our site during this time that addressed discharge or patient education based on input from the hospital’s center for quality outcomes.
Implications for Practice
Integration of an evidence-based discharge risk assessment checklist and risk-related interventions can improve processes, increase delivery of patient education, and improve patient and family perceptions of the discharge process. Involvement of key stakeholders, use of evidence-based interventions with local adaptation, and use of a consistent provider responsible for implementation can improve transitions of care.
Acknowledgments
This project was done under the mentorship of the Society of Hospital Medicine PediBOOST program and the Academic Pediatric Association Research Scholars Program. We thank the nursing staff; the residents; the staff; our pediatric hospitalists at West Virginia University Medicine Children’s Hospital; Dr Samir S. Shah, MD, MSCE, MHM (Cincinnati Children’s Hospital); and Jennifer Ball, MPH, CPHQ (Center for Quality Outcomes, West Virginia University Medicine), for their help in the project.
Footnotes
Dr Patra conceptualized and designed the study, designed the data collection instruments, coordinated and supervised data collection at the sites, and drafted the initial manuscript; Dr Mains assisted with the write-up and critically reviewed and revised the manuscript; Ms Dalton and Ms Welsh designed the data collection instruments, coordinated and supervised data collection at the sites, conducted the initial analyses, and critically reviewed and revised the manuscript; Ms Iheonunekwu assisted with data collection and the write-up and critically reviewed and revised the manuscript; Mr Dai conducted the statistical analysis and critically reviewed and revised the manuscript; Dr Murray provided mentorship, conducted the initial analyses, and critically reviewed and revised the manuscript; Dr Fisher provided mentorship, assisted with design of the study, conducted the initial analyses, and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by a grant from the West Virginia Clinical and Translational Science Institute. Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funded by by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Dunn K, Rogers J. Discharge facilitation: an Innovative PNP role. J Pediatr Health Care. 2016;30(5):499–505 [DOI] [PubMed] [Google Scholar]
- 2.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167 [DOI] [PubMed] [Google Scholar]
- 3.Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital [published correction appears in CMAJ. 2004;170(5):771]. CMAJ. 2004;170(3):345–349 [PMC free article] [PubMed] [Google Scholar]
- 4.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841 [DOI] [PubMed] [Google Scholar]
- 5.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991–994 [DOI] [PubMed] [Google Scholar]
- 6.Advisory Board. The on-time discharge toolkit. Available at: https://www.advisory.com/research/clinical-best-practice-collaborative/tools/2018/on-time-discharge. Accessed October 23, 2019
- 7.Centers for Medicare and Medicaid Services. Guide to reducing disparities in readmissions. Available at: https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/OMH_Readmissions_Guide.pdf. Accessed October 23, 2019
- 8.Institute for Healthcare Improvement. SMART discharge protocol. Available at: www.ihi.org/resources/Pages/Tools/SMARTDischargeProtocol.aspx. Accessed October 23, 2019
- 9.Agency for Healthcare Research and Quality. Tool 3: How to Deliver the Re-Engineered Discharge at Your Hospital. Rockville, MD: Agency for Healthcare Research and Quality; 2013. Available at: https://www.ahrq.gov/hai/red/toolkit/redtool3.html. Accessed October 23, 2019 [Google Scholar]
- 10.Society of Hospital Medicine. PediBOOST toolkit. Available at: https://www.hospitalmedicine.org/clinical-topics/care-transitions/. Accessed February 14, 2019
- 11.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594 [PubMed] [Google Scholar]
- 12.Polster D. Patient discharge information: tools for success. Nursing. 2015;45(5):42–49; quiz 49–50 [DOI] [PubMed] [Google Scholar]
- 13.Waniga HM, Gerke T, Shoemaker A, Bourgoine D, Eamranond P. The impact of revised discharge instructions on patient satisfaction. J Patient Exp. 2016;3(3):64–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor D, Kennedy MP, Virtue E, McDonald G. A multifaceted intervention improves patient satisfaction and perceptions of emergency department care. Int J Qual Health Care. 2006;18(3):238–245 [DOI] [PubMed] [Google Scholar]
- 15.Krishel S, Baraff LJ. Effect of emergency department information on patient satisfaction. Ann Emerg Med. 1993;22(3):568–572 [DOI] [PubMed] [Google Scholar]
- 16.Sun BC, Adams J, Orav EJ, Rucker DW, Brennan TA, Burstin HR. Determinants of patient satisfaction and willingness to return with emergency care. Ann Emerg Med. 2000;35(5):426–434 [PubMed] [Google Scholar]
- 17.Stuart PJ, Parker S, Rogers M. Giving a voice to the community: a qualitative study of consumer expectations for the emergency department. Emerg Med (Fremantle). 2003;15(4):369–375 [DOI] [PubMed] [Google Scholar]
- 18.Tran TP, Schutte WP, Muelleman RL, Wadman MC. Provision of clinically based information improves patients’ perceived length of stay and satisfaction with EP. Am J Emerg Med. 2002;20(6):506–509 [DOI] [PubMed] [Google Scholar]
- 19.Coles E, Wells M, Maxwell M, et al. The influence of contextual factors on healthcare quality improvement initiatives: what works, for whom and in what setting? Protocol for a realist review. Syst Rev. 2017;6(1):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JC, Horst M, Rogers A, et al. Checklist-styled daily sign-out rounds improve hospital throughput in a major trauma center. Am Surg. 2014;80(5):434–440 [PubMed] [Google Scholar]
- 21.Kramer HS, Drews FA. Checking the lists: a systematic review of electronic checklist use in health care. J Biomed Inform. 2017;71(suppl):S6–S12 [DOI] [PubMed] [Google Scholar]
- 22.Cox ED, Jacobsohn GC, Rajamanickam VP, et al. A family-centered rounds checklist, family engagement, and patient safety: a randomized trial. Pediatrics. 2017;139(5):e20161688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang R, Spahlinger D, Kim CS. Re-engineering the post-discharge appointment process for general medicine patients. Patient. 2012;5(1):27–32 [DOI] [PubMed] [Google Scholar]
- 24.Khalifa M. Reducing length of stay by enhancing patients’ discharge: a practical approach to improve hospital efficiency. Stud Health Technol Inform. 2017;238:157–160 [PubMed] [Google Scholar]
- 25.Lackman A. Reducing hospital length of stay through a patient centered discharge pathway [abstract]. J Hosp Med. 2015;10(suppl 1) [Google Scholar]
- 26.Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hansen LO, Greenwald JL, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421–427 [DOI] [PubMed] [Google Scholar]
- 28.Burke R, Guo R, Misky GJ. Identifying keys to success for reducing readmissions: using the Ideal Transition in Care framework [abstract]. J Gen Intern Med. 2013;28(suppl 1):S94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auger KA, Simmons JM, Tubbs-Cooley HL, et al. ; H2O Trial Study Group. Postdischarge nurse home visits and reuse: the Hospital to Home Outcomes (H2O) trial [published correction appears in Pediatrics. 2019;143(4):e20190092]. Pediatrics. 2018;142(1):e20173919. [DOI] [PubMed] [Google Scholar]
- 30. Press Ganey Scoring Quick Guide for Quick Reports. 2013. Available at: https://helpandtraining.pressganey.com/lib-docs/default-source/ip-training-resources/Scoring_Quick_Guide_for_Quick_Reports.pdf?sfvrsn=0 Accessed December 2, 2019.
- 31.Institute for Safe Medication Practices. High-alert medications in acute care settings. 2014. Available at: www.ismp.org/tools/institutionalhighAlert.asp. Accessed February 14, 2018