Abstract
Objective.
In 1987, the Omnibus Reconciliation Act (OBRA) called for a dramatic overhaul of the nursing home (NH) quality assurance system. This study examines trends in facility, resident, and quality characteristics since passage of that legislation.
Methods.
We conducted univariate analyses of national data on U.S. NHs from three sources: (1) the 1985 National Nursing Home Survey (NNHS), (2) the 1992–2015 Online Survey Certification and Reporting (OSCAR) Data, and (3) LTCfocUS data for 2000–2015. We examined changes in NH characteristics, resident composition, and quality.
Setting and Participants.
US NH facilities and residents between 1985 and 2015.
Results.
The proportion of NHs that are Medicare and Medicaid certified, members of chains, and operating not-for-profit has increased over the past 30 years. There have also been reductions in occupancy and increases in the share of residents who are: racial/ethnic minorities, admitted for post-acute care, in need of physical assistance with daily activities, primarily supported by Medicare, and diagnosed with a psychiatric condition such as schizophrenia. With regards to NH quality, direct care staffing levels have increased. The proportion of residents physically restrained has decreased dramatically, coupled with changes in inappropriate antipsychotic (chemical restraint) use.
Conclusions and Implications.
Together with changes in the long-term care market, the NHs of today look very different from NHs 30 years ago. The 30th anniversary of OBRA provides a unique opportunity to reflect, consider what we have learned, and think about the future of this and other sectors of long-term care.
Keywords: Quality, Nursing Home Reform Act, OBRA 1987, Nursing Home Characteristics
Brief Summary:
Since 1985 there have been several improvements in quality and changes in demographics. Coupled with changes in the long-term care market, the NHs of today look very different from NHs 30 years ago.
Introduction
For more than 30 years, the quality of nursing home (NH) care has been a continuous concern.1 In 1984, following published reports and concerns about resident abuse, neglect, and a lack of regulation and oversight, Congress asked the Institute of Medicine (IOM) to investigate the quality of NHs and make recommendations for improvement. The resulting report proposed radical NH reforms,2 many of which were codified by Congress as part of the Nursing Home Reform Act of the Omnibus Budget Reconciliation Act of 1987 (OBRA 1987).
OBRA 1987 created regulations for NHs in an effort to improve the quality of care delivered to residents. OBRA included a minimum set of care standards and rights for people residing in Medicare and Medicaid certified NHs. OBRA 1987 had a focus on residents’ quality of life and care, expectations for improved or maintained resident health, as well as residents’ rights to banking, organized family councils, and freedom from unnecessary physical and chemical restraints. The Act also standardized certification standards and enforcement strategies. As such, OBRA 1987 was an overhaul of the NH industry and marked a new beginning for NH care and regulation.
In the 30+ years since OBRA 1987, there have been a number of other changes that have directly impacted the NH industry. In response to consumer preferences to remain in the community, “age-in-place”, and efforts to rebalance states’ long-term care budgets,3–5 there has been a considerable increase in home- and community-based services (HCBS). HCBS were seen as mechanisms to divert or delay expensive, and often undesired NH placement. Over the last several decades, states have begun funding more HCBS, primarily through Medicaid waiver programs; and, for the first time in 2013, states spent more on HCBS than care provided in NHs.6 Accompanying these care delivery, market, and financing changes, has been growth of an aging and diversifying population, as well as a number of laws and regulations directly impacting the NH industry (e.g., the Balanced Budget Act of 1997 and the introduction of case-mix reimbursement).
The purpose of this study was to summarize changes in the NH industry in the 30 years since the seminal regulatory change affecting NHs. Specifically, we use historical data from three national sources and describe changes in NH facility characteristics, resident characteristics, and quality of care from 1985 through 2015. The 30th Anniversary of OBRA provides a unique opportunity to examine the changes within this vitally important industry. This paper can aid in understanding long-term trends, as well as provide insight into what changes we might expect in the future.
Methods
Data
We analyzed data from three sources to examine resident and facility characteristics, longitudinally: (a) National Nursing Home Survey, (b) Online Survey Certification and Reporting Data/Certification and Survey Provider Enhanced Reporting, and (c) LTCFocUS data.
National Nursing Home Survey (NNHS)
The National Center for Health Statistics conducted the NNHS. The NNHS consists of a nationally representative sample of over 1,000 NHs and their residents. NHs included in the surveys had at least three or more beds and were Medicare or Medicaid certified or had a state license to operate as a NH. The facilities and residents were selected by a stratified two-stage probability design. In the first stage, NHs were selected, and in the second stage, residents were sampled from the selected NHs. NNHS data were used to describe facility and aggregated resident characteristics. Data for these analyses came from the University of Michigan ICPSR public use NNHS data files for 1985.7
Online Survey Certification and Reporting Data (OSCAR) /Certification and Survey Provider Enhanced Reporting (CASPER)
CMS’ OSCAR/CASPER database is a national database of all NH data elements collected by state survey agencies during the required annual onsite Medicare and Medicaid Certification inspection. The inspections occur at least once during a 15-month period. OSCAR/CASPER data are used to determine facility characteristics, deficiencies in care noted during the survey, and aggregated resident data. Data included all certified NHs between the years 1992 and 2015. Variables in OSCAR/CASPER have been validated for research purposes.8
Long-Term Care FocUS (LTCFocUS)
We used LTCFocUS.org, a product of the Shaping Long-Term Care in America Project at the Brown University Center for Gerontology and Healthcare Research and supported, in part, by the National Institute on Aging (www.ltcfocus.org). This dataset included information for years 2000–2015 and combined variables from the OSCAR data; the Minimum Data Set (MDS), resident-level data related to resident clinical and functional status; the Area Resource File (ARF), a national county-level health resources database maintained by the Health Resources and Services Administration that contains data about the health professionals and facilities in each county; and the Residential History File, a data resource built using Medicare Enrollment data, Medicare claims data, and assessment data to track individuals as they move through the long-term care system.9 For these analyses, we used the LTCFocUS data to describe the aggregated characteristics of residents served in NHs between 2000 and 2015.
Variables
We included the following facility characteristics to describe changes in the NH market over time: dual certification for Medicare and Medicaid, multi-facility chain membership, for-profit status (versus non-profit or government), presence of an Alzheimer’s special care unit, facility size (i.e., total number of beds), and occupancy rate.
To describe the resident composition, we included demographic characteristics, length of stay, admission source, physical function, mental health diagnoses, and medication use measures. Demographic variables from LTCfocUS included the percent of female residents in each facility; the percent of blacks, whites, and Hispanics in each facility; and the average age for residents residing in each facility. Also from the LTCfocUS, we included the percent of long-stay residents, defined as the percent of residents in the NH at least 90 of the last 100 days. We also include the percent of residents admitted to the NH directly from the hospital versus the community or other LTC setting. From the OSCAR/CASPER, we included information about residents’ primary payer, as the percent of residents whose primary support was Medicaid or Medicare. Measures of resident physical and cognitive function included the facility’s average Activities of Daily Living (ADL) scale score, bed/chair bound measures, individual early-, middle-, and late-loss ADLs, and the percent of residents with dementia. The ADL scale score comes from LTCFocUS, ranges from 0–28, and is created by summing seven ADL items on a scale from 0–4 (with 0=complete independence and 4=total dependence for each item). The facility average represents the average across all residents in the facility. Chairbound and bedbound measures come from the NNHS and OSCAR/CASPER data and refer to the percent of residents unable to leave their chair or bed, respectively, at the time of the survey. The individual ADLs of interest from the NNHS and OSCAR/CASPER data include dressing, bathing, transferring, toileting, and eating and represent the percentage of residents who were not completely independent in each of these activities at the time of the survey. From the NNHS and OSCAR/CASPER data we also included a measure for the percent of residents with dementia within the facility. Measures of resident mental health and medication use included the percent of residents with a psychiatric diagnosis (excluding dementia and depression), a schizophrenia diagnosis, receiving antianxiety medications, receiving antidepressants, and receiving antipsychotics.
Information on facility quality consisted of structure, process, and outcome measures.10 As a measure of structure, we included the number of certified nursing aides, licensed professional nurses, and registered nurse hours per resident per day from the OSCAR/CASPER data. We obtained information about facilities’ quality process measures including the percent of residents in a facility who: were physically restrained, received tube feeding, had a catheter, received antipsychotic medications without a diagnosis of schizophrenia or bipolar disorder at the time of the survey, and the percent of facilities experiencing medication errors. Medication error refers to the percentage of facilities cited for drug error rates over 5% reported during the annual survey. Quality outcome measures included the percent of residents within a facility with pressure ulcers, and the percent of residents within a facility experiencing incontinence. Values for pressure ulcers/bedsores indicate the percentage of residents during the annual survey with pressure sores. The incontinence measures indicate the percent of residents with bladder or bowel incontinence at the time of the survey.
Analyses
Univariate analyses of the above variables were completed using STATA 14.11 Data from the NNHS were weighted using the facility, bed, and current resident weights provided. OSCAR/CASPER and LTCFocUS data are available at the facility-level. Facility-level variables are averaged for each study year. We do not include inferential statistics in this paper because we are presenting data for the entire population of NHs in the US for the majority of years.
Results
Facility Characteristics
In the past 30 years, the NH industry has decreased in size, from 19,068 facilities in 1985 to 15,686 in 2016 (Table 1). There has also been an increase in the percent of facilities that are non-profit (25% in 1985 and 31% in 2015) and that are dually certified by both Medicare and Medicaid (33% in 1985 and up to 97% 2015). Between 1995 and 2015, chain membership increased from 51% to 57%, the percent of facilities with an Alzheimer’s special care unit increased from 11% to 15%, and the overall NH occupancy rates declined from 87% to 81%.
Table 1.
Changes over Time in Facility Characteristics (1985–2015)
| Year | 1985 | 1995 | 2005 | 2015 |
|---|---|---|---|---|
| Mean (CI) | % or Mean (SD) | % or Mean (SD) | % or Mean (SD) | |
| Number of Nursing Homes, N | 19,068* | 16,824 | 16,091 | 15,686 |
| Percent Dual (Medicare+Medicaid) Certified | 33.34 (28.85, 37.82) | 78.55 | 93.39 | 97.08 |
| Percent Member of a Chain | 51.24 | 52.43 | 56.81 | |
| Percent For-Profit | 74.98 (70.85, 79.12) | 66.38 | 66.01 | 69.13 |
| Percent with Alzheimer’s Unit | 11.22 | 18.23 | 15.15 | |
| Average Number of Beds | 100.84 (67.93) | 104.97 (65.37) | 106.13 (61.31) | |
| Percent with 3–49 Beds | 33.67 (26.83, 40.5) | 18.76 | 14.89 | 12.89 |
| Percent with 50–99 Beds | 32.39 (28, 36.78) | 35.97 | 36.34 | 37.14 |
| Percent with 100–199 Beds | 27.84 (24.23, 31.45) | 38.53 | 42.23 | 43.99 |
| Percent with 200+ Beds | 6.11 (5.05, 7.16) | 6.75 | 6.54 | 5.98 |
| Average Occupancy Rate | 87.14 (16.41) | 84.43 (15.14) | 81.19 (15.79) |
Source: The 1985 National Nursing Home Survey and the 1995, 2005, and 2015 Online Survey Certification and Reporting/Certification and Survey Provider Enhanced Reporting Data
Notes.
=Weighted number of facilities.
SD = Standard Deviation.
CI = Confidence Interval.
Resident Composition
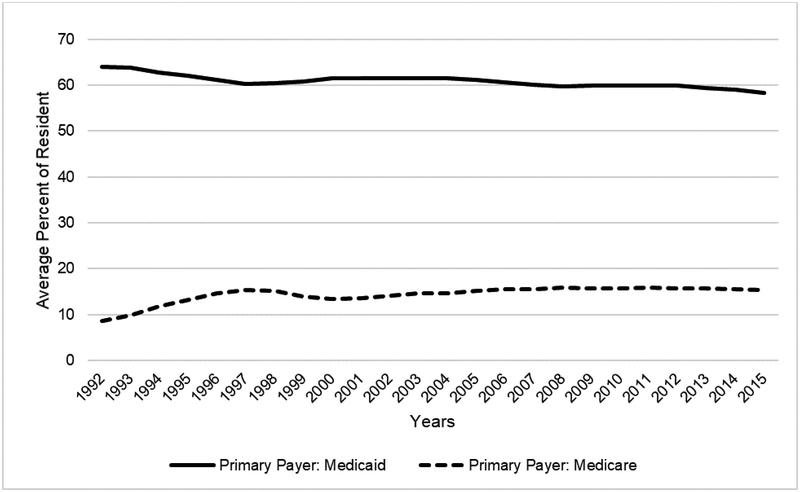
The population that NHs serve has changed over the last 30 years (Table 2). Data from the NNHS and LTCFocUS suggest that while the average age of residents has remained constant, the percent of residents who are racial and ethnic minorities have increased from 7.8% in 1985 to 20.7% in 2015. The average percent of females decreased from 72% of residents in 1985 to 67% in 2015. The prevalence of long-stay residents within NHs has remained stable at 69% of all residents over this time period. However, the percent of residents admitted from the hospital increased from 67% in 2000 to 85% in 2015. There has also been a shift of payer types over time (Figure 1). Between 1992 and 2015 the average percent of residents with Medicaid as a primary payer decreased from 64% to 58%; while the average percent of residents with Medicare as the primary payer rose from 9% to 15%.
Table 2.
Changes over Time in Resident Demographics, Length of Stay, and Admission Source (1985–2015)
| Year | 1985 | 2000 | 2005 | 2015 |
|---|---|---|---|---|
| Mean (CI) N=l,489,508* | Mean (SD) N=16,824 | Mean (SD) N=16,091 | Mean (SD) N=15,686 | |
| Percent Female | 71.63 (70.3, 72.97) |
72.12 (13.81) | 70.94 (13.97) | 66.67 (13.04) |
| Percent Black | 6.98 (6.2, 7.76) |
9.94 (17.84) | 10.91 (18.51) | 11.55 (17.99) |
| Percent Hispanic | 2.75 (2.3,3.21) |
2.87 (9.08) |
3.42 (9.82) |
4.54 (11.25) |
| Percent White | 92.18 (91.36,93) |
85.63 (21.31) | 83.66 (22.56) | 79.31 (23.97) |
| Average Age | 79.61 (79.21, 80) |
80.95 (7.11) | 80.15 (7.68) | 79.71 (7.34) |
| Percent Long Stay | 69.28 (22.62) | 70.61 (19.25) | 68.56 (16.97) | |
| Percent Admitted from the Hospital | 66.52 (22.88) | 72.83 (21.46) | 84.68 (17.16) |
Source: The 1985 National Nursing Home Survey(NNHS) and Brown University’s LTCFocUS Data for 2000, 2005, and 2015
Notes.
NNHS data represent the weighted national averages whereas LTCFocUS data represent the average of facility averages.
=Weighted number of residents. SD = Standard Deviation. CI = Confidence Interval.
Figure 1:
Primary Payment Source Using OSCAR/CASPER Data (1992–2015)
Resident physical and cognitive function has decreased over the years (Table 3). According to LTCFocUS data, the average ADL dependency score amongst NH residents increased slightly from 15 to 17 between 2000 and 2015. According to NNHS and OSCAR/CASPER data, residents who required assistance in bathing increased from a national average of 89% in 1985 to an average facility average of 96% in 2015. The same trend is demonstrated in the increased share of residents who need assistance with the other ADLs from 1985 to 2015: assistance with dressing rose from 74% to 92%; assistance with transferring from 60% to 85%; assistance with toileting from 49% to 88%; and assisting with eating increased from 38% to 56%. However, there was a decrease in the percent of residents who were bedbound from 6% in 1985 to 4% in 2015, while being chair bound rose from 39% to 64%. The percent of residents with dementia increased from an average of 39% in 1995 to an average of 45% across the facilities in 2015.
Table 3.
Changes over Time in Resident Function, Mental Health, and Medication Use (1985–2015)
| Year | 1985 | 1995/2000+ | 2005 | 2015 |
|---|---|---|---|---|
| % (CI) N=l,489,508* | Mean (SD) N=16,824 | Mean (SD) N=16,091 | Mean (SD) N=15,686 | |
| Physical & Cognitive Function | ||||
| Average Activities of Daily Living (ADL) Scale Score+ | 15.26 (3.47) | 15.60 (3.32) | 16.87 (2.62) | |
| Percent of Residents Bed Bound | 6.46 (5.77, 7.16) | 6.56 (9.85) | 4.33 (7.41) | 3.74 (6.92) |
| Percent of Residents Chair Bound | 39.48 (38.05, 40.91) | 48.13 (21.28) | 55.08 (21.21) | 64.32 (21.37) |
| Percent of Residents Needing Assistance with Early-Loss ADLs | ||||
| Dressing | 74.18 (72.83, 75.52) | 86.62 (12.44) | 88.20 (11.66) | 91.82 (10.85) |
| Bathing | 89.16 (88.14, 90.18) | 94.18 (10.11) | 95.40 (9.24) | 96.46 (8.46) |
| Percent of Residents Needing Assistance with Middle Loss ADLs | ||||
| Transfer | 60.21 (58.75,61.67) | 72.71 (16.49) | 77.26 (15.39) | 85.49 (14.65) |
| Toileting | 49.16 (47.68, 50.63) | 76.57 (15.03) | 81.50 (13.89) | 88.11 (13.02) |
| Percent of Residents Needing Assistance with Late Loss ADLs | ||||
| Eating | 37.73 (36.32, 39.14) | 52.95 (22.23) | 49.39 (21.86) | 56.45 (28.85) |
| Percent of Residents with Dementia | 43.34 (41.89, 44.79) | 38.98 (19.95) | 45.19 (19.35) | 45.27 (18.4) |
| Mental Health & Medication Use | ||||
| Percent of Residents with Psychiatric Diagnosis | 11.2 (13.91) | 19.78 (17.19) | 31.37 (19.5) | |
| Percent of Residents with Schizophrenia+ | 5.72 (5.02, 6.41) | 6.05 (9.92) | 7.66 (11.01) | 10.43 (13.04) |
| Percent of Residents Receiving Antianxiety Medications | 14.62 (10.15) | 17.64 (10.27) | 22.98 (11.64) | |
| Percent of Residents Receiving Antidepressant Medications | 19.51 (10.93) | 45.77 (14.28) | 48.74 (14.52) | |
| Percent of Residents Receiving Antipsychotic Medication | 15.96 (13.08) | 25.95 (14.73) | 20.07 (14.50) | |
Source: The 1985 National Nursing Home Survey (NNHS), the 1995, 2005, and 2015 Online Survey Certification and Reporting/Certification and Survey Provider Enhanced Reporting Data(OSCAR/CASPER), and the Brown University’s LTCFocUS Data for 2000, 2005, and 2015.
Notes. NNHS data represents the national averages whereas OSCAR data represent the average of facility averages. ADLs= Activities of Daily Living. The average ADL score is based on 7 ADLs ranges from 0–28 scale where 0=total independence and 28=total dependence.
Weighted number of residents.
These data are from the 2000, 2005, and 2015 LTCFocUs instead of the OSCAR/CASPER Data.
SD = Standard Deviation.
CI = Confidence Interval.
Average Acuity Index = Includes ADL and special treatment measures.9
The share of residents with psychiatric diagnoses has increased over the years, as has the use of psychotropic medications. According to the OSCAR/CASPER data, there was an almost three-fold increase in the share of residents with a psychiatric diagnosis, from 11% in 1995 to 31% by 2015. Between 1985 and 2015, the average percent of residents with schizophrenia increased from 6% to 11%. The percent of residents receiving antianxiety, antidepressant, and antipsychotic medications in 1995 were 15%, 20%, and 16%, respectively and by 2015, increased to 23%, 49%, and 20%, respectively.
Quality of Care
The average direct care staffing hours have increased over time, with the greatest increases observed among CNAs (see Table 4). Overall, quality process measures have also improved since the passage of OBRA 1987. Notably, the average proportion of residents being physically restrained decreased dramatically from 19% to 1%, and the percent of residents receiving antipsychotic medications inappropriately, as a chemical restraint, decreased from 16% in 2000 to 12% in 2015, although there was a peak of 22% in 2005. However, there was not much change in the proportion of facilities cited for medication errors over this time period.
Table 4:
Changes over Time in Quality Indicators (1995–2015)
| Year | 1995/2000+ | 2005 | 2015 |
|---|---|---|---|
| Mean (SD) N=16,824 | Mean (SD) N=16,091 | Mean (SD) N=15,686 | |
| Structure (Staffing) | |||
| CNA Hours Per Resident Day | 2.26 (1.73) | 2.30 (1.15) | 2.42 (1.05) |
| LPN Hours Per Resident Day | 0.87 (1.49) | 0.84 (0.81) | 0.88 (0.73) |
| RN Hours Per Resident Day | 0.66 (1.64) | 0.45 (0.86) | 0.58 (0.87) |
| Direct Care Hours Per Resident Day | 3.39 (2.08) | 3.48 (1.56) | 3.79 (1.42) |
| Process | |||
| Percent of Residents Restrained | 18.55 (17.22) | 6.86 (8.74) | 1.40 (4.91) |
| Percent of Residents Receiving Tube Feeding | 6.33 (8.49) | 6.02 (8.36) | 4.73 (8.23) |
| Percent of Residents with a Catheter | 8.29 (9.49) | 6.96 (7.04) | 5.90 (5.34) |
| Percent of Residents Receiving Inappropriate Antipsychotic Medication+ | 16.43 (9.44) | 21.88 (10.19) | 12.44 (7.63) |
| Percent of Facilities Cited for Medication Errors over 5% | 1.48 | 1.79 | 1.71 |
| Outcome | |||
| Percent of Residents with Pressure Ulcers | 7.56 (7.95) | 7.38 (5.97) | 6.22 (5.07) |
| Percent of Residents with Bowel Incontinence | 41.76 (19.10) | 42.90 (18.00) | 43.86 (18.37) |
| Percent of Residents with Bladder Incontinence | 49.25 (18.45) | 53.48 (17.36) | 62.10 (18.17) |
Source: The 1995, 2005, and 2015 Online Survey Certification and Reporting/Certification and Survey Provider Enhanced Reporting Data (OSCAR/CASPER), and the 2000, 2005, and 2015 Brown University LTCFocUS Data.
Note.
These data are from the 2000, 2005, and 2015 LTCFocUs instead of the OSCAR/CASPER Data. SD = Standard Deviation. CNA= Certified Nursing Aide. LPN=Licensed Professional Nurse. RN= Registered Nurse.
Quality outcome measures also improved over time. The proportion of residents with pressure ulcers decreased from 8% to 6%. Lastly, congruent with increased need for assistance, bowel and bladder incontinence increased from 42% to 44% and 49% to 62%, respectively.
Discussion
Within this 30-year period, there were facility, resident, and quality of care changes that can be linked to regulations adopted through the OBRA 1987 and other policy shifts in the long-term care sector.
Certification
Over the last 30 years, we witnessed a change in NH certification. This change is consistent with the OBRA 1987 requirement for NHs to be certified and meet the federal participation requirements in order to receive Medicaid and Medicare payments.12 Previously, Medicare-certified facilities had more stringent requirements but seeing that the majority of government spending came from Medicaid, OBRA 1987 stipulated that all Medicaid-certified facilities met a set of standards that were similar to that of Medicare.1 Additionally, noting Medicare’s generous reimbursement for skilled care, many Medicaid-only NHs became dually certified in both Medicare and Medicaid.13 These policy and financing incentives likely contributed to the increase in the proportion of facilities that were dually certified during this time period.
Changing Demand and Supply, and Lower Occupancy
Concurrent with shifting U.S. demographics (e.g., an aging and increasingly diverse population), NHs in the last 30 years have witnessed increases in the proportion of minorities and decreases in the proportion of white residents. Recognizing the aging population, the long-term care market began to appear more lucrative and attracted a greater number of investors to NH operations.14 This is evidenced by the percent of NHs that were owned and operated by a chain. Stevenson, Grabowski, and Coots (2006) posit that chain facilities increased due to the interplay of certificate of need laws and resulting acquisitions.
Despite the aging of the population, there was a decrease in the number of NHs and facility occupancy rates during this time period. This decrease in NH supply and occupancy is likely attributable to the rise of community options such as assisted living and other HCBS.15,16 In 2000, Medicaid spent about 27% of its total Medicaid long-term services and supports (LTSS) expenditures on HCBS and 73% on institutional care; by 2016, 57% of the expenditures were for HCBS and 43% for NH care.6 It can be difficult to quantify the increase in community-based services due to data challenges, however the National Survey of Resident Care Facilities identified approximately 31,100 residential facilities in 2010 and researchers have suggested a continued growth in the market.17–19 The growth of long-term care alternatives allows individuals to remain in their homes and communities longer, in many cases delaying NH placement or diverting it all together.20–24 These trends may also explain some of the reason behind the increase in functional impairment among NH residents over this time period.
Another potential explanation for the increase in functional impairment witnessed over this 30-year period may be the increase in post-acute, rehabilitative care provided in NHs. Recognizing the profitability associated with providing Medicare-reimbursed services,25 NHs began to accept more post-acute care patients, with a large number of NHs choosing to specialize in the care of post-acute patients.13,26 This shift in the orientation of NHs over this time period, from providing typically long-term custodial care to post-acute, rehabilitative care, may contribute to the increase in resident acuity witnessed in this study. It is evident from our findings that there is an increase percentage of residents being admitted directly from the hospital, presumably for post-acute care, and may contribute to higher levels of functional impairment as residents may be leaving hospitals “quicker and sicker”.27,28
Quality Improvement
Despite higher resident levels of need, NH quality appears to have improved over time. Our data show modest gains in quality indicators between 1995 and 2015. The literature around drivers of quality improvement in NHs is vast and includes mechanisms such as NH ownership, nurse staffing, public reporting and quality improvement initiatives. The quality improvement that we witnessed during this time period could have been attributable to the increase in non-profit NHs, which have consistently shown to have higher quality ratings.14 Quality improvement could also be directly related to the increase in nursing hours witnessed over this time period. OBRA 1987 improved the standards for nursing hours, and we observed these increases over time. While it is possible that the increase in nursing hours may be in direct response to increasing need among residents, prior research has concluded that increasing nursing hours improves patient outcomes.29–31 It is also plausible that new inspection, survey, enforcement efforts, and public reporting prompted improvements in quality measures.1,32 While it can be argued that NHs still have room to improve in their quality indicators, it is important to note that despite an increasingly vulnerable and higher need population, we still observe quality gains among NHs during this time period.
One of the direct effects of OBRA 1987 was a substantial decrease in the use of physical restraints. Physical restraints were initially used on residents with serious mental illness to manage behaviors, but began to be used more widely on residents with behavioral symptoms, including residents with dementia.33 Prior research indicates that physical restraints are associated with worse outcomes for residents, such as increased depression, less social engagement among NH residents,34–36 reduced muscle strength34 and pressure ulcers.34,35,37 Parts of OBRA 1987 focused directly on the residents’ rights to be free from all restraints. Unfortunately, decreases in physical restraints were coupled with initial increases in chemical restraint use, such as inappropriate antipsychotic use. Antipsychotic medications increase the risk of falls38 and death.39,40 In 2005, the FDA released a Black Box warning to decrease the use of antipsychotics among older adults.41 This warning is consistent with the 2005 peak in antipsychotic use that is present in our data. In 2011, CMS launched a national partnership to further reduce inappropriate antipsychotic use, which has been largely successful.42 With the increase in dementia residents and initiatives to improve dementia care in NHs, there was a simultaneous increase in Alzheimer’s SCUs, with a peak in the percent of facilities with an Alzheimer’s SCU in 2005. Literature suggests that residents within facilities with SCUs have significantly more challenging behaviors and have increased risk for chemical restraint use.43,44 The presence of these units may also account for the increased resident impairment.
It is also important to note the dramatic increase in residents with serious mental illnesses (SMI), as this could be a direct result of state psychiatric facilities closures in the 1960s and 1970s. The increase in the SMI population creates a new and increased burden for NHs and their staff that may negatively affect the quality of care that NHs are able to provide.45,46
Despite the success of several prompted voiding interventions,47,48 we observed increases into the share of NH residents experiencing incontinence over the past 30 years, potentially reflective of the increasing needs of the NH population. Prompting toileting interventions can be labor intensive, and it is often more convenient to diaper a resident than toilet.49 More work is needed in this important quality of life area.
Limitations
This work provides a high-level look at national trends in NH characteristics, resident composition, and quality measures. Data are averaged across all facilities for the available study years. We do not have access to annual data available between 1986–1994, and because of the facility-level nature of our data we are unable to summarize resident-level changes over time. For example, it would be interesting to examine changes in acuity, separately for long-stay vs. short-stay residents, or changes in residents’ lengths of stay. This would help us understand if the increase in acuity over time is due to an increased focus on post-acute care, or attributable to higher levels of acuity among long-term residents who may delay entry into NHs through home and community-based alternatives. Future work in this area would be beneficial to understanding additional impacts of OBRA on the long-term care industry, as a whole.
Conclusions and Implications
Overall, OBRA 1987 is positively associated with the quality of care improvements in NHs despite increasing impairment of NH residents. OBRA 1987 was also successful in implementing/enforcing the MDS resident assessment survey, and without that this research would not be possible. Due to the aging-in-place movement, we are seeing lower occupancy rates in NHs. Older adults without financial resources, disproportionality minority older adults, are becoming an increasing proportion of NH residents, as they may not be able to as readily access these care alternatives. Current and future policies should focus on expanding equitable access to the remaining long-term care services and supports in the continuum of care, particularly given the policies and initiatives focused on decreasing NH utilization through support of home and community based alternatives.50 While NHs continue to focus more on short-stay post-acute care residents and long-stay residents with dementia, more work will need to be done in community-based settings to ensure the highest quality care and life. Improving quality is also about improving equity, and it is important for future work to examine access to quality care for our most vulnerable elders who are sometimes triply and doubly vulnerable because of their cognitive status, race, and/or socioeconomic position. As our work shows, much of the quality progress made in NHs has been because of regulation and oversight over the years. The same level of oversight does not exist for all community alternatives, but the evidence presented here is indicative of effective practices.
Future research is also needed to understand whether these improvements in quality over the past 30 years have been equitable on the basis of race, socioeconomic status, gender, and geography. In sum, our findings document the 30-year history of NHs since the passage of the seminal legislation: OBRA ‘87. As we look toward the future of long-term care, it is important that we reflect on the past.
Funding:
This work was supported by the National Institute on Aging [P01 AG027296]; the Agency for Healthcare Research and Quality [4T32 HS000011]; and the Veterans Affairs Health Services Research and Development Service [CDA 14–422].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
- HCR Manor Care - Chair, Independent Quality Committee
- NaviHealth, Inc. - Chair of Scientic Advisory Board, consultant
- PointRight, Inc. - former Director. Holds less than I% equity.
References
- 1.Wiener JM, Freiman MP, Brown D. Nursing Home Care Quality Twenty Years After The Omnibus Budget Reconciliation Act of 1987 Nursing Home Quality Twenty Years After The Omnibus Budget Reconciliation Act of 1987.; 2007. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7717.pdf. Accessed November 30, 2018. [Google Scholar]
- 2.Institute of Medicine. Improving the Quality of Care in Nursing Homes. Washington, D.C.: National Academy Press.; 1986. doi: 10.17226/646 [DOI] [Google Scholar]
- 3.Konetzka RT. The Hidden Costs of Rebalancing Long- Term Care Health Services Research. 2014. doi: 10.1111/1475-6773.12190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grabowski DC, Cadigan RO, Miller EA, Stevenson DG, Clark M, Mor V. Supporting Home- and Community-Based Care: Views of Long-Term Care Specialists. Med Care Res Rev Suppl to. 2010;67(4):82–101. doi: 10.1177/1077558710366863 [DOI] [PubMed] [Google Scholar]
- 5.Harrington C, Ng T, Kaye SH, Newcomer R. HOME AND COMMUNITY-BASED SERVICES: PUBLIC POLICIES TO IMPROVE ACCESS, COSTS, AND QUALITY. 2009. http://nasuad.org/sites/nasuad/files/hcbs/files/153/7617/PASCenter_HCBS_policy_brief.pdf. Accessed November 14, 2016. [Google Scholar]
- 6.Eiken S, Sredl K, Burwell B, Saucier P. Medicaid Expenditures for Long-Term Services and Supports (LTSS) in FY 2013: Home and Community-Based Services Were a Majority of LTSS Spending.; 2015. https://www.medicaid.gov/medicaid/ltss/downloads/ltss-expenditures-fy2013.pdf. Accessed October 3, 2018. [Google Scholar]
- 7.Services USD of H and H National Center for Health Statistics. National Nursing Home Survey, 1985. Ann Arbor, MI; 2006. [Google Scholar]
- 8.Feng Z, Katz PR, Intrator O, Karuza J, Mor V. Physician and nurse staffing in nursing homes: The role and limitations of the Online Survey Certification and Reporting (OSCAR) system. J Am Med Dir Assoc. 2005;6(1):27–33. doi: 10.1016/j.jamda.2004.12.008 [DOI] [PubMed] [Google Scholar]
- 9.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46(1 Pt 1):120–137. doi: 10.1111/j.1475-6773.2010.01194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donabedian A The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. http://www.ncbi.nlm.nih.gov/pubmed/3045356. Accessed May 11, 2018. [DOI] [PubMed] [Google Scholar]
- 11.StataCorp Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; https://www.stata.com/support/faqs/resources/citing-software-documentation-faqs/. Published 2015. Accessed November 30, 2018. [Google Scholar]
- 12.The Joint Commission. Facts about federal deemed status and state recognition | Joint Commission. https://www.jointcommission.org/facts_about_federal_deemed_status_and_state_recognition/. Published 2017. Accessed November 30, 2018. [Google Scholar]
- 13.Stevenson D, Grabowski D, Coots L. Nursing home divestiture and corporate restructuring:Final report. Washington, DC US Dep Heal Hum Serv. 2006. http://aspe.hhs.gov/_/office_specific/daltcp.cfm. Accessed November 30, 2018. [Google Scholar]
- 14.Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Serv Res. 2008;43(4):1184–1203. doi: 10.1111/j.1475-6773.2008.00841.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bishop CE. Where Are The Missing Elders? The Decline In Nursing Home Use, 1985 And 1995. Health Aff. 1999;18(4):146–155. doi: 10.1377/hlthaff.18.4.146 [DOI] [PubMed] [Google Scholar]
- 16.Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. Growth Of Racial And Ethnic Minorities In US Nursing Homes Driven By Demographics And Possible Disparities In Options. Health Aff. 2011;30(7):1358–1365. doi: 10.1377/hlthaff.2011.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevenson D, Grabowski D. Sizing Up The Market For Assisted Living. https://doi.org/101377/hlthaff20090527. August 2010. doi: 10.1377/HLTHAFF.2009.0527 [DOI] [PubMed] [Google Scholar]
- 18.Silver BC, Grabowski DC, Gozalo PL, Dosa D, Thomas KS. Increasing Prevalence of Assisted Living as a Substitute for Private-Pay Long-Term Nursing Care. Health Serv Res. 2018;53(6):4906–4920. doi: 10.1111/1475-6773.13021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khatutsky G, Ormond C, Wiener J, et al. Residential Care Communities and Their Residents in 2010: A National Portrait. DHHS Publ No 2016–1041 Hyattsville, MD Natl Cent Heal Stat. 2016. http://www.cdc.gov/nchs/govdelivery.htm. Accessed December 5, 2018. [Google Scholar]
- 20.Thomas KS, Keohane L, Mor V. Local Medicaid Home- and Community-Based Services Spending and Nursing Home Admissions of Younger Adults. Am J Public Health. 2014;104(11):e15–e17. doi: 10.2105/AJPH.2014.302144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas KS, Mor V. The Relationship between Older Americans Act Title III State Expenditures and Prevalence of Low-Care Nursing Home Residents. Health Serv Res. 2013;48(3):1215–1226. doi: 10.1111/1475-6773.12015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas KS, Mor V. Providing More Home-Delivered Meals Is One Way To Keep Older Adults With Low Care Needs Out Of Nursing Homes. Health Aff. 2013;32(10):1796–1802. doi: 10.1377/hlthaff.2013.0390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas KS. The Relationship Between Older Americans Act In-Home Services and Low-Care Residents in Nursing Homes. J Aging Health. 2014;26(2):250–260. doi: 10.1177/0898264313513611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hahn EA, Thomas KS, Hyer K, Andel R, Meng H. Predictors of Low-Care Prevalence in Florida Nursing Homes: The Role of Medicaid Waiver Programs. Gerontologist. 2011;51(4):495–503. doi: 10.1093/geront/gnr020 [DOI] [PubMed] [Google Scholar]
- 25.Grabowski DC, Afendulis CC, McGuire TG. Medicare prospective payment and the volume and intensity of skilled nursing facility services. J Health Econ. 2011;30(4):675–684. doi: 10.1016/J.JHEALECO.2011.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feng Z, Grabowski DC, Intrator O, Mor V. The Effect of State Medicaid Case-Mix Payment on Nursing Home Resident Acuity. Health Serv Res. 2006;0(0):060720074824042-??? doi: 10.1111/j.1475-6773.2006.00545.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qian X, Russell LB, Valiyeva E, Miller JE. “Quicker and sicker” under Medicare’s prospective payment system for hospitals: new evidence on an old issue from a national longitudinal survey. Bull Econ Res. 2011;63(1):1–27. http://www.ncbi.nlm.nih.gov/pubmed/21141646. Accessed May 14, 2019. [DOI] [PubMed] [Google Scholar]
- 28.Potthoff S, Kane RL, Franco SJ. Improving hospital discharge planning for elderly patients. Health Care Financ Rev. 1997;19(2):47–72. http://www.ncbi.nlm.nih.gov/pubmed/10345406. Accessed May 14, 2019. [PMC free article] [PubMed] [Google Scholar]
- 29.Konetzka RT, Stearns SC, Park J. The staffing-outcomes relationship in nursing homes. Health Serv Res. 2008;43(3):1025–1042. doi: 10.1111/j.1475-6773.2007.00803.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hyer K, Thomas KS, Branch LG, Harman JS, Johnson CE, Weech-Maldonado R. The Influence of Nurse Staffing Levels on Quality of Care in Nursing Homes. Gerontologist. 2011;51(5):610–616. doi: 10.1093/geront/gnr050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hyer K, Thomas KS, Johnson CE, Harman JS, Weech-Maldonado R. Do Medicaid Incentive Payments Boost Quality? Florida’s Direct Care Staffing Adjustment Program. J Aging Soc Policy. 2013;25(1):65–82. doi: 10.1080/08959420.2012.705629 [DOI] [PubMed] [Google Scholar]
- 32.Werner R, Stuart E, Polsky D. Public Reporting Drove Quality Gains At Nursing Homes. Health Aff. 2010;29(9):1706–1713. doi: 10.1377/hlthaff.2009.0556 [DOI] [PubMed] [Google Scholar]
- 33.Castle NG, Mor V. Physical Restraints in Nursing Homes: A Review of the Literature Since the Nursing Home Reform Act of 1987. Med Care Res Rev. 1998;55(2):139–170. doi: 10.1177/107755879805500201 [DOI] [PubMed] [Google Scholar]
- 34.Lane C, Harrington A. The factors that influence nurses’ use of physical restraint: A thematic literature review. Int J Nurs Pract. 2011;17(2):195–204. doi: 10.1111/j.1440-172X.2011.01925.x [DOI] [Google Scholar]
- 35.Wagner LM, McDonald SM, Castle NG. Nursing Home Deficiency Citations for Physical Restraints and Restrictive Side Rails. West J Nurs Res. 2013;35(5):546–565. doi: 10.1177/0193945912437382 [DOI] [PubMed] [Google Scholar]
- 36.Castle NG. Mental Health Outcomes and Physical Restraint Use in Nursing Homes. Adm Policy Ment Heal Ment Heal Serv Res. 2006;33(6):696–704. doi: 10.1007/s10488-006-0080-0 [DOI] [PubMed] [Google Scholar]
- 37.Hofmann H, Hahn S. Characteristics of nursing home residents and physical restraint: a systematic literature review. J Clin Nurs. 2014;23(21–22):3012–3024. doi: 10.1111/jocn.12384 [DOI] [PubMed] [Google Scholar]
- 38.Jalbert JJ, Eaton CB, Miller SC, Lapane KL. Antipsychotic Use and the Risk of Hip Fracture Among Older Adults Afflicted With Dementia. J Am Med Dir Assoc. 2010;11(2):120–127. doi: 10.1016/j.jamda.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 39.Gill SS, Bronskill SE, Normand S-LT, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007;146(11):775–786. http://www.ncbi.nlm.nih.gov/pubmed/17548409. Accessed November 30, 2018. [DOI] [PubMed] [Google Scholar]
- 40.Maust DT, Kim HM, Chiang C, Kales HC. Association of the Centers for Medicare & Medicaid Services’ National Partnership to Improve Dementia Care With the Use of Antipsychotics and Other Psychotropics in Long-term Care in the United States From 2009 to 2014. JAMA Intern Med. 2018;178(5):640. doi: 10.1001/jamainternmed.2018.0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dorsey ER, Rabbani A, Gallagher SA, Conti RM, Alexander GC. Impact of FDA Black Box Advisory on Antipsychotic Medication Use. Arch Intern Med. 2010;170(1):96–103. doi: 10.1001/archinternmed.2009.456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lucas JA, Bowblis JR. CMS Strategies To Reduce Antipsychotic Drug Use In Nursing Home Patients With Dementia Show Some Progress. Health Aff. 2017;36(7):1299–1308. doi: 10.1377/hlthaff.2016.1439 [DOI] [PubMed] [Google Scholar]
- 43.Chatterjee S, Mehta S, Sherer JT, Aparasu RR. Prevalence and Predictors of Anticholinergic Medication Use in Elderly Nursing Home Residents with Dementia. Drugs Aging. 2010;27(12):987–997. doi: 10.2165/11584430-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 44.Kok JS, Berg IJ, Scherder EJA. Special care units and traditional care in dementia: relationship with behavior, cognition, functional status and quality of life - a review. Dement Geriatr Cogn Dis Extra. 2013;3(1):360–375. doi: 10.1159/000353441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rahman M, Grabowski DC, Intrator O, Cai S, Mor V. Serious Mental Illness and Nursing Home Quality of Care. Health Serv Res. 2013;48(4):1279. doi: 10.1111/1475-6773.12023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grabowski DC, Aschbrenner KA, Rome VF, Bartels SJ. Quality of mental health care for nursing home residents: a literature review. Med Care Res Rev. 2010;67(6):627–656. doi: 10.1177/1077558710362538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ouslander JG, Schnelle JF, Uman G, et al. Predictors of successful prompted voiding among incontinent nursing home residents. JAMA. 1995;273(17):1366–1370. http://www.ncbi.nlm.nih.gov/pubmed/7715062. Accessed November 30, 2018. [PubMed] [Google Scholar]
- 48.Schnelle JF, Ouslander JG, Simmons SF. Predicting nursing-home resident responsiveness to a urinary incontinence treatment protocol. Int Urogynecol J. 1993;4(2):89–94. doi: 10.1007/BF00376418 [DOI] [Google Scholar]
- 49.Leung FW, Schnelle JF. Urinary and fecal incontinence in nursing home residents. Gastroenterol Clin North Am. 2008;37(3):697–707, x. doi: 10.1016/j.gtc.2008.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mor V, Thomas KS, Rahman M. Defining and Measuring Nursing Home Placement. J Am Geriatr Soc. 2018;66(10):1866–1868. doi: 10.1111/jgs.15546 [DOI] [PMC free article] [PubMed] [Google Scholar]