Abstract
Background
Uncontrolled blood pressure (BP) is relatively common despite treatment with antihypertensive medication. This study aimed to investigate factors associated with uncontrolled systolic BP (SBP) and diastolic BP (DBP) separately in hypertensive patients with high medication adherence in Korea.
Methods
This population-based cross-sectional study included 3,236 participants in the Korea National Health and Nutrition Examination Survey from 2013 to 2015. Hypertensive patients with high medication adherence were defined when they stated that they were taking antihypertensive medication daily. “Uncontrolled SBP and DBP” were defined as SBP ≥140 mm Hg and DBP ≥90 mm Hg, respectively. Data were analyzed using logistic regression to determine the association between uncontrolled SBP or DBP and various factors.
Results
The prevalence of uncontrolled SBP and uncontrolled DBP was 23.3%, and 9.0%, respectively. In multivariate analysis, uncontrolled SBP was positively associated with older age, female sex, blue-collar occupation or no work (vs. white-collar), presence of a spouse, short sleep duration, frequent heavy alcohol drinking, longer hypertension duration, diabetes, stroke, and missing antihypertensive medication on the examination day, but negatively associated with high stress. Uncontrolled DBP was positively associated with frequent heavy alcohol drinking, but negatively associated with older age, blue-collar occupation or no work (vs. white-collar), and diabetes.
Conclusion
After excluding low medication adherence, we identified various factors associated with uncontrolled SBP or DBP in Korean adults with treated hypertension. There were differences between factors associated with uncontrolled SBP or DBP. Separate analysis of SBP and DBP may help understand the factors involved in BP control.
Keywords: Hypertension, Medication Adherence, Compliance, Blood Pressure
INTRODUCTION
Hypertension, also known as high blood pressure (BP), is a common chronic medical condition in adults and a well-established risk factor for cardiovascular disease, cerebrovascular disease, and kidney disease. It is relatively common for BP to be uncontrolled despite treatment with antihypertensive medication. In a population-based study conducted from 2011 to 2012 in the United States, 30% of the treated adults had uncontrolled systolic BP (SBP) ≥140 mm Hg or diastolic BP (DBP) ≥90 mm Hg [1]. In low- and middle-income countries, the rate of uncontrolled BP has been reported to be over 70% [2].
Various factors are related to uncontrolled BP, including treatmentrelated factors (such as low medication adherence and suboptimal therapy) and other factors (such as patient demographics, socioeconomic status, lifestyle factors, comorbidities, and duration of hypertension) [3,4]. Understanding these factors may help predict difficult-tocontrol hypertension and determine treatment plans. Since low adherence medication is the first factor to be excluded in patients with uncontrolled BP, studies conducted on patients with high medication adherence are needed [5]. In addition, since the physiologies of SBP and DBP are different, separate analysis of these two BPs may help understand the factors involved in BP control [6]. Therefore, this study aimed to investigate factors associated with uncontrolled SBP and DBP separately in hypertensive patients with high medication adherence in the general population of Korean adults.
METHODS
This study followed the tenets of the Declaration of Helsinki, and it was approved by the Institutional Review Board of Dongguk University Ilsan Hospital (IRB approval no., 2018-12-024). Data of the sixth Korea National Health and Nutrition Examination Survey (KNHANES) were used for this study. The data pertained age, sex, residential area, education level, occupation type, house income, spouse status, stress perception level, exercise intensity and frequency, sleep duration, smoke status, alcohol drinking behavior, history of antihypertensive medication, hypertension duration, history of diabetes, myocardial infarction (MI) or angina, stroke, dyslipidemia, thyroid disease, depression, chronic kidney disease, or liver cirrhosis, antihypertensive medication intake status on the day of examination, SBP and DBP, body mass index (BMI), and waist circumference (WC).
1. Study Population
The KNHANES is a nationwide survey administered by the Korea Centers for Disease Control and Prevention (KCDC). The sixth KNHANES was conducted from 2013 to 2015 and included a random sampling of 9,491 households across 576 national districts selected by a panel to represent the South Korean population through a stratified, multistage, clustered sampling method. The survey included a health interview, nutritional survey, physical examination, and blood tests. For the blood test, fasting was instructed after dinner the day before the test.
2. Hypertensive Patients with High Medication Adherence
In the survey, participants were asked how often they took antihypertensive medication to control their BP. Hypertensive patients with high medication adherence were defined as those who answered that they took antihypertensive medication daily. In the present study, participants who took daily antihypertensive medication were included for further analyses.
3. Variable Definitions
A participant was considered to live in an urban residential area if they lived in “dong” of the city administrative district and rural if the participant lived in “eup” or “myeon” of the country’s administrative district. Their educational level was categorized as either lower than middle school graduation (≤9 years) and higher than high school graduation (≥10 years). Occupation was classified according to the Korean Standard Classification of Occupations as follows: group 1 (managers, professionals, and related workers); group 2 (clerks); group 3 (service and sales workers); group 4 (skilled agricultural, forestry, and fishery workers); group 5 (craft, equipment, and machine operating and assembling workers); group 6 (elementary workers); and group 7 (housewives, students, and unemployed). In this study, groups 1 and 2 were merged into white-collar type, groups 3, 4, 5, and 6 were merged into a blue-collar type, and group 7 was classified as “no work” type. The median monthly house income was 1,500,000 Korean won (KRW) in 2013, 1,480,400 KRW in 2014, and 1,575,900 KRW in 2015. The house income was divided into two groups based on median values. Spouse status was considered as ‘no spouse’ in the case of bereavement or divorce, otherwise, it was considered as having a spouse regardless of whether they were living together or not. The stress perception level was classified as “low” if they did not feel any stress or feel a little; otherwise, it was considered as “high” if they felt a lot of stress or felt very much. Regular exercise was defined as walking activity for at least 30 minutes per day for at least 5 days a week. Current smoker was defined if the participant was a current smoker of cigarettes with a total of ≥100 cigarettes during their lifetime. The frequency of alcohol drinking and heavy drinking in the most recent year was surveyed. Heavy alcohol drinking was defined as drinking more than 7 cups of liquor or soju (Korean distilled liquor) or more than 5 cans of beer.
Diabetes, MI or angina, stroke, dyslipidemia, thyroid disease, depression, chronic kidney disease, and liver cirrhosis were defined as self-reported physician’s diagnosis. BP was measured three times by trained nurses with a mercury sphygmomanometer (Baumanometer; Baum, Copiague, NY, USA) in a seated position with arm height adjusted to the heart height after a minimum of 5 minutes of rest. The average of the second and third measurements was used as the final BP value. SBP ≥140 mm Hg and DBP ≥90 mm Hg were defined as “uncontrolled”. Obesity was defined as a BMI ≥25 kg/m2, and abdominal obesity was defined as WC ≥90 cm in men and ≥85 cm in women.
4. Statistical Analyses
Statistical analyses were performed using IBM SPSS software ver. 20.0 (IBM Corp., Armonk, NY, USA). For comparisons between two groups, chi-square analysis or Fisher’s exact test was used for categorical variables. Results are expressed as mean±standard deviation. Logistic regression analysis was used to identify the association between uncontrolled BP and other variables. A stepwise method with iteratively adding and removing predictors to find a subset of variables in a data set was used for multivariate analysis, and the odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. All statistics were twotailed and a P-value of <0.05 was considered significant.
RESULTS
A total of 22,948 Korean subjects participated in the sixth KNHANES from 2013 to 2015 (Figure 1). Of 18,034 subjects aged 19 years or older, 3,360 subjects (18.6%) were taking antihypertensive medication. Of 3,360 subjects, 3,236 subjects (96.3%) were taking medication daily, 85 subjects (2.5%) were taking medication for between ≥20 and <30 days a month, 24 subjects (0.7%) were taking medication for ≥15 and <20 days a month, and 15 subjects (0.4%) were taking medication for <15 days a month. In the present study, 3,236 participants who were taking antihypertensive medication daily were included for further analyses. The mean age of the subjects was 66.2±10.10 years; males accounted for 42.3% and females accounted for 57.7%. The mean hypertension duration was 9.7±8.13 years. The overall BP (SBP and/or DBP) was uncontrolled in 890 (27.5%) of the 3,236 subjects.
Figure. 1.
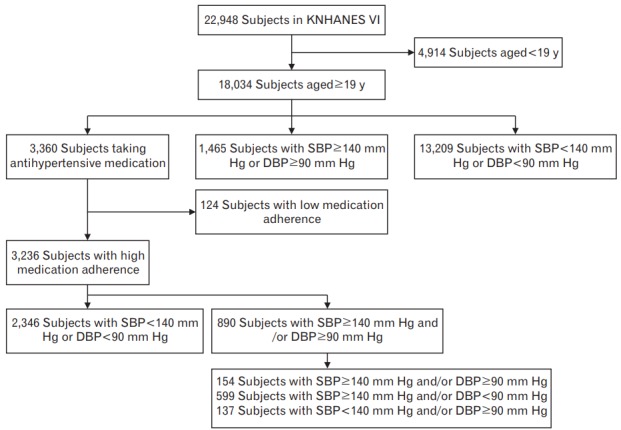
Flowchart showing the selection of study subjects. KNHANES, Korea National Health and Nutrition Examination Survey; SBP, systolic blood pressure; DBP, diastolic blood pressure.
1. Systolic Blood Pressure
SBP was uncontrolled in 753 (23.3%) of the 3,236 subjects. The characteristics of subjects with or without uncontrolled SBP are summarized in Table 1. The rate of uncontrolled SBP was higher in subjects with the following characteristics: older age (29.1% in ≥70 years), female sex (25.9%), low education level (25.9%), blue-collar occupation (21.9%) or no work (25.6% versus 10.5% in white-collar occupation), low house income (25.5%), low stress, short sleep duration (27.6%), non or exsmoker (24.0%), no obesity (25.2%), longer hypertension duration (32.7% in ≥25 years), diabetes (27.0%), stroke (31.8%), and missing antihypertensive medication on the day of examination (23.7%, all P<0.05).
Table 1.
Characteristics of subjects with or without uncontrolled BP
| Characteristic | Uncontrolled systolic BP |
Uncontrolled diastolic BP |
||||
|---|---|---|---|---|---|---|
| No | Yes (%*) | P-value | No | Yes (%*) | P-value | |
| Total | 2,483 | 753 (23.3) | 2,945 | 291 (9.0) | ||
| Age (y) | <0.001 | <0.001 | ||||
| <55 | 398 | 56 (12.3) | 347 | 107 (23.6) | ||
| 55–69 | 1,106 | 296 (21.1) | 1,262 | 140 (10.0) | ||
| ≥70 | 979 | 401 (29.1) | 1,336 | 44 (3.2) | ||
| Sex | <0.001 | 0.001 | ||||
| Male | 1,098 | 270 (19.7) | 1,218 | 150 (11.0) | ||
| Female | 1,385 | 483 (25.9) | 1,727 | 141 (7.6) | ||
| Residential area | 0.352 | 0.150 | ||||
| Rural | 597 | 188 (24.5) | 708 | 59 (7.7) | ||
| Urban | 1,904 | 565 (22.9) | 2,237 | 232 (9.4) | ||
| Education level | <0.001 | <0.001 | ||||
| Middle school or lower | 1,530 | 535 (25.9) | 1,921 | 144 (7.0) | ||
| High school of higher | 900 | 197 (18.0) | 958 | 139 (12.7) | ||
| Occupation type | <0.001 | <0.001 | ||||
| White-collar | 214 | 25 (10.5) | 186 | 53 (22.2) | ||
| Blue-collar | 858 | 240 (21.9) | 977 | 121 (11.0) | ||
| No work | 1,361 | 467 (25.6) | 1,718 | 110 (6.0) | ||
| House income | <0.001 | <0.001 | ||||
| Less than median | 1,540 | 528 (25.5) | 1,916 | 152 (7.4) | ||
| Median or more | 929 | 223 (19.4) | 1,015 | 137 (11.9) | ||
| Spouse | 0.190 | <0.001 | ||||
| No | 722 | 238 (24.8) | 906 | 54 (5.6) | ||
| Yes | 1,758 | 515 (22.7) | 2,036 | 237 (10.4) | ||
| Stress | 0.027 | 0.477 | ||||
| Low | 1,869 | 589 (24.0) | 2,237 | 221 (9.0) | ||
| High | 543 | 135(19.9) | 611 | 67 (9.9) | ||
| Regular exercise | 0.186 | 0.424 | ||||
| No | 1,519 | 476 (23.9) | 1,809 | 186 (9.3) | ||
| Yes | 904 | 252 (21.8) | 1,058 | 98 (8.5) | ||
| Sleep duration (h) | 0.001 | 0.522 | ||||
| ≥6 | 1,878 | 522 (21.8) | 2,175 | 225 (9.4) | ||
| <6 | 531 | 202 (27.6) | 670 | 63 (8.6) | ||
| Smoke | 0.001 | 0.144 | ||||
| Non or ex | 2,082 | 657 (24.0) | 2,496 | 243 (8.9) | ||
| Current | 329 | 66 (16.7) | 351 | 44 (11.1) | ||
| Alcohol drinking (d/wk) | 0.771 | 0.072 | ||||
| ≤3 | 2,226 | 665 (23.0) | 2,634 | 257 (8.9) | ||
| ≥4 | 192 | 60 (23.8) | 221 | 31 (12.3) | ||
| Heavy alcohol drinking (d/wk) | 0.320 | <0.001 | ||||
| <1 | 2,070 | 632 (23.4) | 2,494 | 208 (7.7) | ||
| ≥1 | 345 | 93 (21.2) | 358 | 80 (18.3) | ||
| Hypertension duration (y) | <0.001 | 0.001 | ||||
| <10 | 1,470 | 363 (19.8) | 1,642 | 191 (10.4) | ||
| 10–24 | 862 | 309 (26.4) | 1,081 | 90 (7.7) | ||
| ≥25 | 136 | 66 (32.7) | 195 | 7 (3.5) | ||
| Diabetes | 0.004 | 0.001 | ||||
| No | 1,883 | 531 (22.0) | 2,172 | 242 (10.0) | ||
| Yes | 596 | 220 (27.0) | 767 | 49 (6.0) | ||
| Myocardial infarction or angina | 0.198 | 0.168 | ||||
| No | 2,284 | 679 (22.9) | 2,692 | 271 (9.2) | ||
| Yes | 180 | 65 (26.5) | 229 | 16 (6.5) | ||
| Stroke | 0.001 | 0.878 | ||||
| No | 2,289 | 662 (22.4) | 2,688 | 263 (8.9) | ||
| Yes | 178 | 83 (31.8) | 237 | 24 (9.2) | ||
| Dyslipidemia | 0.345 | 0.173 | ||||
| No | 1,583 | 466 (22.7) | 1,854 | 195 (9.5) | ||
| Yes | 899 | 287 (24.2) | 1,090 | 96 (8.1) | ||
| Thyroid disease | 0.965 | 0.167 | ||||
| No | 2,375 | 717 (23.2) | 2,811 | 281 (9.1) | ||
| Yes | 87 | 26 (23.0) | 107 | 6 (5.3) | ||
| Depression | 0.849 | 0.483 | ||||
| No | 2,311 | 696 (23.1) | 2,735 | 272 (9.1) | ||
| Yes | 151 | 47 (23.7) | 183 | 15 (7.6) | ||
| Chronic kidney disease | 0.708 | 0.176† | ||||
| No | 2,429 | 732 (23.2) | 2,875 | 286 (9.1) | ||
| Yes | 32 | 11 (25.6) | 42 | 1 (2.3) | ||
| Liver cirrhosis | 0.784 | 1.000† | ||||
| No | 2,442 | 738 (23.2) | 2,895 | 285 (9.0) | ||
| Yes | 19 | 5 (20.8) | 22 | 2 (8.3) | ||
| Antihypertensive medication on the day of examination | 0.003 | 0.076 | ||||
| No | 2,358 | 734 (23.7) | 2,808 | 284 (9.2) | ||
| Yes | 125 | 19 (13.2) | 137 | 7 (4.9) | ||
| Obesity | 0.008 | 0.001 | ||||
| BMI <25 kg/m2 | 1,239 | 418 (25.2) | 1,535 | 122 (7.4) | ||
| BMI ≥25 kg/m2 | 1,239 | 335 (21.3) | 1,406 | 168 (10.7) | ||
| Abdominal obesity | 0.145 | 0.939 | ||||
| No | 1,321 | 423 (24.3) | 1,587 | 157 (9.0) | ||
| Yes | 1,161 | 329 (22.1) | 1,357 | 133 (8.9) | ||
BP, blood pressure; BMI, body mass index.
Prevalence of uncontrolled BP in the stated condition.
P-value derived from the chi-square test or Fisher’s exact test.
The ORs for the association between uncontrolled SBP and other factors are shown in Table 2. In multivariate analysis, the variables selected by the stepwise method were age, sex, occupation type, spouse, stress, sleep duration, heavy alcohol drinking, hypertension duration, diabetes, stroke, and missing antihypertensive mediation on the day of examination. Uncontrolled SBP was positively associated with older age (OR, 1.69 in 55–69 years; OR, 2.49 in ≥70 years versus <55 years), female sex (OR, 1.55), blue-collar occupation (OR, 1.81) or no work (OR, 1.68 versus white-collar), presence of a spouse (OR, 1.28), short sleep duration (OR, 1.28), frequent heavy alcohol drinking (≥1 day a week; OR, 1.38), longer hypertension duration (OR, 1.21 in 10–24 years; OR, 1.55 in ≥25 years versus <10 years), diabetes (OR, 1.22), stroke (OR, 1.54), and missing antihypertensive medication on the day of examination (OR, 2.36), but negatively associated with high stress (OR, 0.76; all P<0.05).
Table 2.
Association between uncontrolled systolic blood pressure and other factors
| Factors | Univariate |
Multivariate* |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (y) | ||||
| <55 | 1.00 (ref) | 1.00 (ref) | ||
| 55–69 | 1.90 (1.40–2.59) | <0.001 | 1.69 (1.21–2.35) | 0.002 |
| ≥70 | 2.91 (2.15–3.94) | <0.001 | 2.49 (1.75–3.53) | <0.001 |
| Sex (female) | 1.42 (1.20–1.68) | <0.001 | 1.55 (1.25–1.91) | <0.001 |
| Residential area (urban) | 0.91 (0.76–1.11) | 0.352 | ||
| Education level (high school or higher) | 0.63 (0.52–0.75) | <0.001 | ||
| Occupation type | ||||
| White-collar | 1.00 (ref) | 1.00 (ref) | ||
| Blue-collar | 2.39 (1.55–3.71) | <0.001 | 1.81 (1.15–2.85) | 0.010 |
| No work | 2.94 (1.92–4.50) | <0.001 | 1.68 (1.06–2.66) | 0.026 |
| House income (median or more) | 0.70 (0.59–0.84) | <0.001 | ||
| Spouse (yes) | 0.89 (0.76–1.06) | 0.190 | 1.28 (1.03–1.58) | 0.023 |
| Stress (high) | 0.79 (0.64–0.97) | 0.037 | 0.76 (0.60–0.95) | 0.015 |
| Regular exercise (yes) | 0.89 (0.75–1.06) | 0.186 | ||
| Sleep duration (<6 h) | 1.37 (1.13–1.65) | 0.001 | 1.28 (1.04–1.56) | 0.018 |
| Smoke (current) | 0.64 (0.48–0.84) | 0.001 | ||
| Alcohol drinking (≥4 d/wk) | 1.05 (0.77–1.42) | 0.768 | ||
| Heavy alcohol drinking (≥1 d/wk) | 0.88 (0.69–1.13) | 0.321 | 1.38 (1.03–1.83) | 0.029 |
| Hypertension duration (y) | ||||
| <10 | 1.00 (ref) | 1.00 (ref) | ||
| 10–24 | 1.45 (1.22–1.73) | <0.001 | 1.32 (1.10–1.59) | 0.003 |
| ≥25 | 1.97 (1.43–2.40) | <0.001 | 1.55 (1.11–2.18) | 0.011 |
| Diabetes | 1.31 (1.09–1.57) | 0.004 | 1.22 (1.00–1.49) | 0.046 |
| Myocardial infarction or angina | 1.22 (0.90–1.63) | 0.198 | ||
| Stroke | 1.61 (1.23–2.12) | 0.001 | 1.54 (1.15–2.07) | 0.004 |
| Dyslipidemia | 1.08 (0.92–1.28) | 0.345 | ||
| Thyroid disease | 0.99 (0.63–1.55) | 0.965 | ||
| Depression | 1.03 (0.74–1.45) | 0.847 | ||
| Chronic kidney disease | 1.14 (0.57–2.27) | 0.709 | ||
| Liver cirrhosis | 0.87 (0.32–2.34) | 0.784 | ||
| Antihypertensive medication on the day of examination (no) | 2.05 (1.26–3.34) | 0.004 | 2.36 (1.38–4.05) | 0.002 |
| Obesity (body mass index ≥25 kg/m2) | 0.80 (0.68–0.94) | 0.008 | ||
| Abdominal obesity (yes) | 0.89 (0.75–1.04) | 0.145 | ||
OR, odds ratio; CI, confidence interval; ref, reference.
A stepwise method, iteratively adding and removing predictors to find a subset of variables in a data set, was used with all factors.
2. Diastolic Blood Pressure
DBP was uncontrolled in 291 (9.0%) of 3,236 subjects. The characteristics of subjects with or without uncontrolled DBP are shown in Table 1. The rate of uncontrolled DBP was higher in subjects with the following characteristics: Younger age (23.6% in <55 years), male sex (11.0%), high education level (12.7%), white-collar occupation (22.2%), high house income (11.9%), presence of a spouse (10.4%), frequent heavy alcohol drinking (≥1 day a week, 18.3%), shorter hypertension duration (10.4% in <10 years), no diabetes (10.0%), and obesity (BMI ≥25, 10.7%, all P<0.05).
The ORs for association between uncontrolled SBP and other factors are shown in Table 3. In multivariate analysis, the variables selected by the stepwise method were age, occupation type, heavy alcohol drinking, and diabetes. Uncontrolled DBP was positively associated with frequent heavy alcohol drinking (≥1 day a week; OR, 1.62) but negatively associated with older age (OR, 0.45 in 55–69 years; OR, 0.15 in ≥70 years versus <55 years), blue-collar occupation (OR, 0.66) or no work (OR, 0.55 versus white-collar), and diabetes (OR, 0.71; all P<0.05).
Table 3.
Association between uncontrolled diastolic blood pressure and other factors
| Factors | Univariate |
Multivariate* |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (y) | ||||
| <55 | 1.00 (ref) | 1.00 (ref) | ||
| 55–69 | 0.36 (0.27–0.48) | <0.001 | 0.45 (0.33–0.61) | <0.001 |
| ≥70 | 0.11 (0.07–0.16) | <0.001 | 0.15 (0.10–0.23) | <0.001 |
| Sex (female) | 0.66 (0.52–0.84) | 0.001 | ||
| Residential area (urban) | 1.24 (0.92–1.68) | 0.150 | ||
| Education level (high school or higher) | 1.94 (1.51–2.47) | <0.001 | ||
| Occupation type | ||||
| White-collar | 1.00 (ref) | 1.00 (ref) | ||
| Blue-collar | 0.44 (0.30–0.62) | <0.001 | 0.66 (0.45–0.96) | 0.029 |
| No work | 0.23 (0.16–0.32) | <0.001 | 0.55 (0.37–0.83) | 0.004 |
| House income (median or more) | 1.70 (1.33–2.17) | <0.001 | ||
| Spouse (yes) | 1.95 (1.44–2.65) | <0.001 | ||
| Stress (high) | 1.11 (0.83–1.48) | 0.477 | ||
| Regular exercise (yes) | 0.90 (0.70–1.16) | 0.424 | ||
| Sleep duration (<6 h) | 0.91 (0.68–1.22) | 0.522 | ||
| Smoke (current) | 1.29 (0.92–1.81) | 0.145 | ||
| Alcohol drinking (≥4 d/wk) | 1.44 (0.97–2.14) | 0.073 | ||
| Heavy alcohol drinking (≥1 d/wk) | 2.68 (2.02–3.55) | <0.001 | 1.62 (1.19–2.21) | 0.002 |
| Hypertension duration (y) | ||||
| <10 | 1.00 (ref) | |||
| 10–24 | 0.72 (0.55–0.93) | 0.012 | ||
| ≥25 | 0.31 (0.14–0.67) | 0.002 | ||
| Diabetes | 0.57 (0.41–0.79) | 0.001 | 0.71 (0.51–0.99) | 0.044 |
| Myocardial infarction or angina | 0.69 (0.41–1.17) | 0.170 | ||
| Stroke | 1.04 (0.67–1.61) | 0.876 | ||
| Dyslipidemia | 0.84 (0.65–1.01) | 0.174 | ||
| Thyroid disease | 0.56 (0.24–1.29) | 0.172 | ||
| Depression | 0.82 (0.48–1.42) | 0.484 | ||
| Chronic kidney disease | 0.24 (0.03–1.75) | 0.158 | ||
| Liver cirrhosis | 0.92 (0.22–3.95) | 0.914 | ||
| Antihypertensive medication on the day of examination (no) | 1.98 (0.92–4.27) | 0.082 | ||
| Obesity (body mass index ≥25 kg/m2) | 1.50 (1.18–1.92) | 0.001 | ||
| Abdominal obesity (yes) | 0.99 (0.78–1.26) | 0.940 | ||
OR, odds ratio; CI, confidence interval; ref, reference.
A stepwise method, iteratively adding and removing predictors to find a subset of variables in a data set, was used with all factors.
DISCUSSION
In the present study, we investigated the factors associated with uncontrolled SBP and DBP in hypertensive patients with high medication adherence in the general population of Korean adults. Older age, blue-collar occupation or no work (versus white-collar), and diabetes were positively associated with uncontrolled SBP, but negatively associated with uncontrolled DBP. Female sex, presence of a spouse, short sleep duration, longer hypertension duration, stroke, and missing antihypertensive medication on the day of examination were only positively associated with uncontrolled SBP. High stress was only negatively associated with uncontrolled SBP. Frequent heavy alcohol drinking was positively associated with both uncontrolled SBP and DBP.
In this study, the factors associated with uncontrolled SBP were different from those associated with uncontrolled DBP. SBP is the force that blood exerts on the arterial walls as the heart muscle contracts to propel blood, and DBP is the residual pressure exerted on the artery during heart muscle relaxation between beats [6]. Since the physiology of SBP and DBP is different, the control of SBP and DBP may be influenced by different factors, respectively. Furthermore, demographic factors such as aging, sex, occupation, marital status, lifestyle, and comorbidities affect the control of SBP and DBP through interactions with different factors; the consequences of these seem to be complex and sometimes contradictory.
Few previous studies have analyzed SBP and DBP separately. In one study conducted in the United States, Dave et al. [7] found that older age, African Americans (versus Caucasian), and moderate risk of blood triglyceride levels (versus normal) are positively associated with uncontrolled SBP, while male sex, African Americans, younger age, and no personal history of atrial fibrillation are positively associated with uncontrolled DBP for individuals taking antihypertensive medications. In another study conducted in Lebanon, Farah et al. [8] found that older age, male sex, low and medium medication adherence, and treatment with three or more antihypertensive drugs are positively associated with uncontrolled SBP. They also described that younger age, obesity, and low medication adherence were positively associated with uncontrolled DBP, whereas being married and taking statins were associated with better DBP control.
The association of age with uncontrolled SBP and DBP in this study is consistent with the results of previous studies. The pathophysiology of blood vessels with increasing age supports our findings. When we get older, the elasticity of the blood vessel wall decreases and becomes stiff. As a result, the SBP continues to rise with age, whereas the DBP tends to decline after 50 years of age [9]. Older age may directly contribute to SBP that is difficult to control. Furthermore, the behavioral factors related to hypertension management may affect the intensity of control. Isolated systolic hypertension is more common in old age due to the vascular pathophysiology [10]. Intensive management for systolic hypertension with wide pulse pressure (PP) can increase the risk of cardiovascular disease; hence, controlling systolic hypertension with wide PP is more likely to be carefully controlled than strictly controlled [10].
Occupation type was associated with BP control in the present study. Blue-collar occupation or no work (versus white-collar) was positively associated with uncontrolled SBP but negatively associated with uncontrolled DBP. In a study of male municipal employees, bluecollar workers had a higher risk of uncontrolled hypertension than white-collar workers [11]. A cross-sectional study in the Japanese working population by Tsutsumi et al. [12] indicated that job strain is linearly associated with the prevalence of hypertension in Japanese men with a wide range of occupations and that the strain level is significantly higher in subordinates (versus manager) and blue-collar workers (versus white-collar workers). There is a lack of studies on the relationship between occupational groups and SBP/ DBP, and a causal relationship has yet to be revealed. However, more studies of occupational groups and hypertension-related to factors may explain the findings of our study.
The presence of diabetes can intensely accelerate vascular remodeling, leading to an increase in arterial stiffness [13]. As a result, diabetes may lead to changes in SBP and DBP, like age-related BP changes. This study demonstrated that like older age, diabetes was positively associated with uncontrolled SBP but negatively associated with uncontrolled DBP. In addition, insulin resistance in diabetes can lead to excess circulating insulin in the blood, which can increase BP by stimulating the sympathetic nervous system and increasing sodium reabsorption [14]. Previous studies have reported that people with diabetes are less likely to have BP control [15].
Various results have been reported on the association between sex and BP control. In a study conducted in the United States, Dave et al. [7] reported that male sex is positively associated with uncontrolled DBP in individuals taking antihypertensive medications. In another population-based study of the United States, there was no significant difference in BP control between males and females [16]. However, in the present study, female sex had a higher risk of uncontrolled SBP; this result is consistent with previous studies of Waddell et al. [17] and Berry et al. [18] who demonstrated that postmenopausal women had stiffer larger arteries compared to men. Stiffer large arteries may contribute to a rise in SBP in older women [17,18].
Those who had a spouse were at higher risk of uncontrolled SBP in this Korean population study; however, previous studies have reported diverse results. A study in South Asia has reported that being single has a higher risk of uncontrolled BP compared to being married [19]. In a study on the general population of the United States, the control rate of hypertension was higher in currently or formerly married non-Hispanic whites and Mexican Americans, while hypertension control was not associated with marital status in non-Hispanic blacks [20]. These results seem to reflect different gender roles and cultural differences among race or ethnicity.
The current study showed that those with a short sleep duration had a higher risk of uncontrolled SBP. Zuo et al. [21] reported that sleep for >7 hours is associated with a lower risk of uncontrolled hypertension compared to sleep for <7 hours for middle-aged women with hypertension. The short sleep duration has been assumed to be related to the activation of the sympathetic nervous system [22], and it especially affects nighttime BP levels.
It is well known that long-term hypertension can cause excessive deposition of extracellular matrix (ECM) proteins that are the main structural composition of large blood vessels [23]. Uncontrolled excessive ECM proteins can increase atherogenesis consequentially [24]; this mechanism may explain the positive association with longer hypertension duration and uncontrolled SBP in the present study.
In the present study, stroke was a risk factor of uncontrolled SBP in hypertensive patients with high medication adherence. Previous studies have shown that many patients with post-stoke hypertension have poorly uncontrolled BP [25]. In a cross-sectional study for a cohort with recent lacunar stroke, over half of the participants (52.9%) had uncontrolled SBP 2.5 months after stroke [25]. In addition, moderate-to-severe hypertension and resistant hypertension are related to the occurrence of stroke [26]. With this background, it may be assumed that hypertensive patients with stroke have difficulty in controlling BP. Because uncontrolled BP is the most important risk factor for stroke, BP in hypertensive patients accompanying stroke has to be well controlled for secondary stroke prevention.
In the current study, only 4.4% of subjects took antihypertensive medication on the day of examination. This may be the result of instructing all participants to fast for a blood test. This study showed that missing medication on the day of examination was positively associated with uncontrolled SBP in spite of normally taking regular medication. The medical institution generally recommends fasting on the day of the examination, but it should be necessary to make additional recommendations for taking antihypertensive medication. Not taking antihypertensives on the morning of the examination had a big impact on BP, even if they were normally taken every day. This underlines the importance of taking antihypertensive drugs consistently.
Psychological stress has been proposed as a factor contributing to the development of hypertension [27]. However, hypertensive patients with high stress were more likely to have SBP control in the present study. This result may suggest that stress-induced hypertension is well-controlled by medication.
The association between high alcohol consumption and hypertension has been reported in recent epidemiological and clinical studies [28]. Two cross-sectional studies (the US general population and elderly Greeks) on antihypertensive medication have consistently indicated that heavy alcohol intake is associated with lower control rate of hypertension on medication [20,29]. In this study, heavy alcohol drinking more than once a week was a risk factor for both uncontrolled SBP and DBP. However, there was no association between frequent but not heavy drinking and BP control. The mechanism by which alcohol increases BP is unclear. Several possible mechanisms have been suggested including increased sympathetic activity and cortisol value, stimulation of the endothelium to release factors that lead to vasoconstriction, a loss of relaxation caused by inflammation and oxidative injury of the endothelium, and an influence of the renin-angiotensin-aldosterone system [28]. Husain et al. [28] have proposed that the most effective prevention and treatment of alcohol-induced hypertension is physical exercise and the use of angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers in the clinic.
This study has several limitations. First, the KNHANES Survey evaluated medication adherence in hypertensive patients based on a questionnaire. In the questionnaire, the frequency of taking medication was classified according to the number of days of drug use per month; since this was dependent on their memory, a recall bias may exist. Second, white-coat effects on BP could not be excluded at the time of the examination. Furthermore, information on the type or number of antihypertensive medications could not be obtained from the survey. In addition, we could not assess whether patients were receiving appropriate medication. Third, since this study included only Koreans, it is necessary to consider racial differences when interpreting our results. Finally, the study did not reveal the influence of the doctor’s judgment on BP control depending on individual characteristics. Target BP levels in hypertension control vary depending on the patient’s accompanying disease, risk of adverse drug reactions, and age [30]; these factors may influence the doctor’s perception of BP control depending on individual characteristics. Especially in the elderly, hypertension should be controlled with discretion. Isolated systolic hypertension with wide PP is more common in old age due to the pathophysiology of blood vessels [10]. Therefore, intensive SBP control without consideration of the wide PP may induce extremely low DBP in old age and is associated with a higher risk of cardiovascular hypoperfusion [10]. As a result, it is speculated that hypertension in the elderly may not be strictly controlled. This study did not consider doctor’s behavioral factors that could influence these therapeutic goals. Future studies should consider these aspects when investigating factors related to the control or deregulation of hypertension.
The current study has several strengths. This study is based on nationally representative data from KNHANES. KNHANES contains a large volume of data that allows us to explore various aspects of the health of the Korean population, and the KCDC keeps it as an unbiased source. The current study is the first attempt to investigate factors associated with uncontrolled BP in hypertensive patients with high medication adherence in the general population of Korean adults.
In conclusion, after excluding low medication adherence, we identified various factors associated with uncontrolled SBP or DBP in Korean adults with treated hypertension. There were differences between factors associated with uncontrolled SBP or DBP. A separate analysis of SBP and DBP may help us to predict difficult-to-control hypertension and determine treatment plans.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Yoon SS, Gu Q, Nwankwo T, Wright JD, Hong Y, Burt V. Trends in blood pressure among adults with hypertension: United States, 2003 to 2012. Hypertension. 2015;65:54–61. doi: 10.1161/HYPERTENSIONAHA.114.04012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149:785–94. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 4.De la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz JJ, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30:1211–6. doi: 10.1097/HJH.0b013e328353634e. [DOI] [PubMed] [Google Scholar]
- 5.Matsumura K, Arima H, Tominaga M, Ohtsubo T, Sasaguri T, Fujii K, et al. Impact of antihypertensive medication adherence on blood pressure control in hypertension: the COMFORT study. QJM. 2013;106:909–14. doi: 10.1093/qjmed/hct121. [DOI] [PubMed] [Google Scholar]
- 6.Shahoud JS, Aeddula NR. Physiology, arterial pressure regulation. Treasure Island (FL): StatPearls Publishing; 2019. [PubMed] [Google Scholar]
- 7.Dave GJ, Bibeau DL, Schulz MR, Aronson RE, Ivanov LL, Black A, et al. Predictors of uncontrolled hypertension in the Stroke Belt. J Clin Hypertens (Greenwich) 2013;15:562–9. doi: 10.1111/jch.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farah R, Zeidan RK, Chahine MN, Asmar R, Chahine R, Salameh P, et al. Predictors of uncontrolled blood pressure in treated hypertensive individuals: first population-based study in Lebanon. J Clin Hypertens (Greenwich) 2016;18:871–7. doi: 10.1111/jch.12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure: the Framingham Heart Study. Circulation. 1997;96:308–15. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 10.Pinto E. Blood pressure and ageing. Postgrad Med J. 2007;83:109–14. doi: 10.1136/pgmj.2006.048371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sparacino J, Ronchi D, Bigley TK, Flesch AL, Kuhn JW. Blood pressure of male municipal employees: effects of job status and worksite. Percept Mot Skills. 1982;55:563–78. doi: 10.2466/pms.1982.55.2.563. [DOI] [PubMed] [Google Scholar]
- 12.Tsutsumi A, Kayaba K, Tsutsumi K, Igarashi M; Jichi Medical School Cohort Study Group. Association between job strain and prevalence of hypertension: a cross sectional analysis in a Japanese working population with a wide range of occupations: the Jichi Medical School cohort study. Occup Environ Med. 2001;58:367–73. doi: 10.1136/oem.58.6.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spinetti G, Kraenkel N, Emanueli C, Madeddu P. Diabetes and vessel wall remodelling: from mechanistic insights to regenerative therapies. Cardiovasc Res. 2008;78:265–73. doi: 10.1093/cvr/cvn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–9. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adeniyi OV, Yogeswaran P, Longo-Mbenza B, Ter Goon D. Uncontrolled hypertension and its determinants in patients with concomitant type 2 diabetes mellitus (T2DM) in rural South Africa. PLoS One. 2016;11:e0150033. doi: 10.1371/journal.pone.0150033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 17.Waddell TK, Dart AM, Gatzka CD, Cameron JD, Kingwell BA. Women exhibit a greater age-related increase in proximal aortic stiffness than men. J Hypertens. 2001;19:2205–12. doi: 10.1097/00004872-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Berry KL, Cameron JD, Dart AM, Dewar EM, Gatzka CD, Jennings GL, et al. Large-artery stiffness contributes to the greater prevalence of systolic hypertension in elderly women. J Am Geriatr Soc. 2004;52:368–73. doi: 10.1111/j.1532-5415.2004.52107.x. [DOI] [PubMed] [Google Scholar]
- 19.Jafar TH, Gandhi M, Jehan I, Naheed A, de Silva HA, Shahab H, et al. Determinants of uncontrolled hypertension in rural communities in South Asia-Bangladesh, Pakistan, and Sri Lanka. Am J Hypertens. 2018;31:1205–14. doi: 10.1093/ajh/hpy071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162:1051–8. doi: 10.1001/archinte.162.9.1051. [DOI] [PubMed] [Google Scholar]
- 21.Zuo H, Wang J, Lin Y, Deng L, Su J, Zhang J. Gender-specific associations of sleep duration with uncontrolled blood pressure in middleaged patients. Clin Exp Hypertens. 2016;38:125–30. doi: 10.3109/10641963.2014.995801. [DOI] [PubMed] [Google Scholar]
- 22.Hwang HR, Lee JG, Lee S, Cha KS, Choi JH, Jeong DW, et al. The relationship between hypertension and sleep duration: an analysis of the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-3) Clin Hypertens. 2015;21:8. doi: 10.1186/s40885-015-0020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carlsson AC, Ruge T, Sundstrom J, Ingelsson E, Larsson A, Lind L, et al. Association between circulating endostatin, hypertension duration, and hypertensive target-organ damage. Hypertension. 2013;62:1146–51. doi: 10.1161/HYPERTENSIONAHA.113.02250. [DOI] [PubMed] [Google Scholar]
- 24.Xu J, Shi GP. Vascular wall extracellular matrix proteins and vascular diseases. Biochim Biophys Acta. 2014;1842:2106–19. doi: 10.1016/j.bbadis.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White CL, Pergola PE, Szychowski JM, Talbert R, Cervantes-Arriaga A, Clark HD, et al. Blood pressure after recent stroke: baseline findings from the secondary prevention of small subcortical strokes trial. Am J Hypertens. 2013;26:1114–22. doi: 10.1093/ajh/hpt076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hung CY, Wang KY, Wu TJ, Hsieh YC, Huang JL, Loh el-W, et al. Resistant hypertension, patient characteristics, and risk of stroke. PLoS One. 2014;9:e104362. doi: 10.1371/journal.pone.0104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ushakov AV, Ivanchenko VS, Gagarina AA. Psychological stress in pathogenesis of essential hypertension. Curr Hypertens Rev. 2016;12:203–14. doi: 10.2174/1573402112666161230121622. [DOI] [PubMed] [Google Scholar]
- 28.Husain K, Ansari RA, Ferder L. Alcohol-induced hypertension: mechanism and prevention. World J Cardiol. 2014;6:245–52. doi: 10.4330/wjc.v6.i5.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skliros EA, Papadodima SA, Sotiropoulos A, Xipnitos C, Kollias A, Spiliopoulou CA. Relationship between alcohol consumption and control of hypertension among elderly Greeks: the Nemea primary care study. Hellenic J Cardiol. 2012;53:26–32. [PubMed] [Google Scholar]
- 30.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:1269–324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]


