Abstract
Graves' Orbitopathy (GO) is the most frequent extrathyroidal manifestation of Graves' disease (GD). Its ultimate cause remains unclear, but it is commonly considered an autoimmune disorder due to self recognition of autoantigens constitutively expressed by orbital fibroblasts (OFs), and thyroid epithelial cells. High dose intravenous glucocorticoids (ivGC) are the most commonly used treatment for moderately severe and active GO. However, based on the complex pathogenesis of GO, a number of factors may have a protective and maybe a therapeutic role. The use of other medications improving the effect of GC may increase the overall effectiveness of the therapy and reduce GC doses, thereby limiting side effects. Recently, a possible protective role of 3-hydroxy-3-methylglutaryl-coenzyme reductase inhibitors, the so-called statins, and perhaps of lowering cholesterol levels, has been proposed. Thus, statins have been reported to be associated with a reduced frequency of GO in GD patients and in recent cross-sectional and retrospective studies a significant correlation was found between the occurrence of GO and both total and LDL-cholesterol in patients with a GD of relatively recent onset, suggesting a role of cholesterol in the development of GO. Moreover, a correlation was found between the GO clinical activity score and total as well as LDL-cholesterol in untreated GO patients, depending on GO duration, indicating a role of cholesterol on GO activity. Therefore, statin treatment may be beneficial for GO. Here we review this subject, which offers new therapeutic perspectives for patients with GO.
Keywords: Graves' orbitopathy, Graves' disease, thyroid, autoimmunity, statin, 3-hydroxy-3-methylglutaryl-coenzyme reductase, cholesterol, pleiotropic effects of statins
Introduction
Graves' orbitopathy (GO) is a disfiguring syndrome observed in patients with autoimmune thyroid diseases, especially Graves' disease (GD). Recognized risk factors for GO development are uncontrolled hyperthyroidism, radioiodine (RAI) treatment, and smoking. The pathogenesis of GO is due to a number of complex mechanisms which interplay among each other, namely humoral and cell-mediated immunity, cytokine production, and oxidative stress. Based on this knowledge, a number of factors may have a protective and maybe therapeutic role. Recently, a possible protective role of 3-hydroxy-3-methylglutaryl-coenzyme reductase inhibitors, commonly known as statins, and perhaps of lowering cholesterol levels, has been proposed. Here we review this subject which offers new therapeutic perspectives for patients with GO.
Brief Notes on Go
GO is generally described as an autoimmune disease and it is observed in ~25–30% of patients with Graves' hyperthyroidism and less commonly in patients with hypothyroid autoimmune thyroiditis, or in those without thyroid dysfunction, the so-called euthyroid GO (1–3). Although the ultimate cause of GO remains unclear, some of the molecular mechanisms have been clarified. GO is likely due to an autoimmune reaction against autoantigens constitutively expressed by orbital fibroblasts (OFs) and thyroid epithelial cells, being the TSH-receptor the major autoantigen (1–3). Recently, a major role of the insulin-like growth factor-1 receptor (IGF-1R) has emerged (4). The extent to which IGF-1R has an intrinsic role or its actions are related to its capability of interplaying with the TSH-R has to be clarified (5). Overall, once the autoimmune reaction is started, both B and T cells infiltrate the fibroadipose orbital tissue and, through a number of interconnected events, lead to the cell modifications underlying the connective tissue remodeling typical of GO, with orbital fat expansion and extraocular muscle enlargement, which are ultimately responsible for the clinical manifestations of the disease (1, 2, 6).
The typical clinical features of GO are proptosis, inflammation, and diplopia. Subclinical eye involvement is common, whereas only ~3–5% of patients with GO have a severe disease characterized by corneal ulceration, severe inflammation, or compressive optic neuropathy (2, 7). In addition to genetic and demographical variables (6), the recognized risk factors associated with the development of GO in GD patients are age, sex, hypothyroidism, inadequate control of hyperthyroidism, radioiodine, and cigarette smoking (8–21).
The choice of treatment depends on the extent of GO activity, which is defined by a clinical activity score (1, 22). Patients affected with mild GO can be treated with lubricants and/or selenium (1, 23, 24), whereas, according to the European Group On Graves' Orbitopathy (EUGOGO) guidelines, high dose intravenous glucocorticoids GC (ivGC) are the first line treatment for moderately severe and active GO (1). However, more recently, new medications have been proposed, including rituximab (25), teprotumumab (26, 27), mycophenolate (28), and tocilizumab (29). Finally, orbital decompression, squint or palpebral surgery can be considered in patients with an inactive disease, for therapeutic or rehabilitative purposes (30). The use of systemic GC takes advantage from their immunosuppressive and anti-inflammatory actions, resulting in an overall beneficial effect ranging from ~35 to ~80% of patients (1, 31). Regarding the molecular mechanisms of GC, their actions on genomic and non-genomic pathways may affect the production of cytokines, the distribution of circulating T-cell subsets, the recruitment of monocytes and macrophages, the expression T-lymphocyte adhesion molecules, as well as the production, differentiation and homing of dendritic cells (32–34), thereby blocking the interplay between innate and adaptive immune responses. Unfortunately, patients are often selected to treatment because of the severity of the disease, despite having an inactive GO when immunosuppression is not effective. Thus, when patients with a long standing, still severe, but fibrotic and inactive GO are included in studies on immunosuppressive treatments, the response rate decreases remarkably. These observations may explain why about ~30% of patients do not respond to GC. Another potential explanation for the lack of response to treatment may be the necessity for a stronger immunosuppression. The use of additional medications may in theory improve the effects of GC, possibly increasing the overall effectiveness of the therapy and reducing GC dosage, thereby limiting side effects.
Statins and Go
Clinical Standpoint
Statins are the most commonly used drugs that improve cardiovascular risk by reducing low-density lipoprotein (LDL) cholesterol levels (26, 35). The JUPITER trial assessed the potential benefit of statins in healthy participants (36, 37), which was demonstrated by a significant reduction of markers of systemic inflammation (e.g., C-reactive protein), cholesterol levels, and the number of cardiovascular events (37, 38). The study showed the pleiotropic anti-inflammatory actions of statins, which were not related to their actions in terms of lowering cholesterol, and suggested that statins can be used as a new adjuvant anti-inflammatory therapy, in accordance to various studies (39–50). Statin treatment seems to be linked with the reduced risk of developing GO among patients with GD (51). Stein et al. studied a large cohort of patients with newly-diagnosed GD to identify risk factors associated with the development of GO, indicating that thyroidectomy as the chosen treatment of hyperthyroidism and exposure to statins may lower the risk (51). They investigated whether the administration of drugs with anti-inflammatory actions reduce the risk of GO. In a multivariate regression model, medical therapy with antithyroid medications, regardless of whether it was used alone or followed by RAI, did not modify the risk of GO compared to patients receiving RAI alone. In contrast, thyroidectomy alone or thyroidectomy with antithyroid medications were associated with a significant reduced risk of GO compared to RAI alone. Regarding TSH levels, individuals with TSH >7 μIU/mL had a higher risk of developing GO compared to those with TSH levels ≤7 μIU/mL, but this finding was not statistically significant. Finally, the authors assessed the potential protective effect on GO development of COX-2 inhibitors and statins. The use of statins for at least 60 days during an observation lasting 1 year was followed by a reduction of GO risk by ~40%. In contrast, statistically significant differences in terms of GO risk in patients exposed to non-statin cholesterol lowering medications were not found. Furthermore, in both univariate and multivariate models, no significant differences between subjects treated with COX-2 inhibitors and subjects not receiving these medications were observed (51). The protective action of statins on the risk of GO was considered as a direct effect of the immunomodulatory effects of statins (52).
Molecular Mechanisms
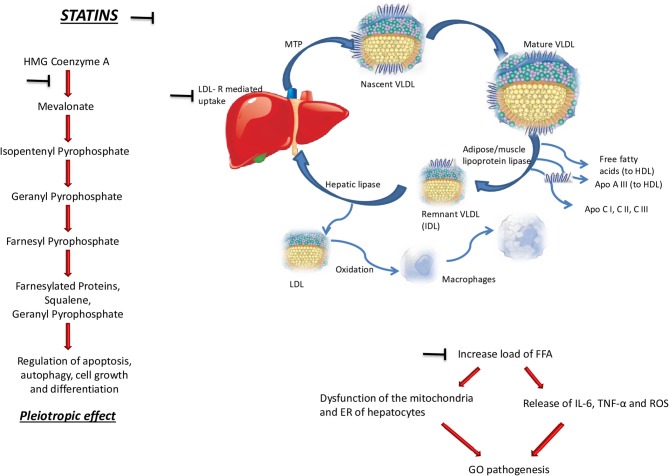
As depicted in Figure 1, several studies reported that statins influence positively tissue remodeling and protect against heart failure (53, 54). The effects of statins are due to the competitive inhibition of 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase, the key-limiting enzyme of cholesterol synthesis in the multistep mevalonate pathway in the liver (36, 37, 55). In addition to the biosynthesis of cholesterol, mevalonate is also a precursor of isoprenoids, namely farnesyl pyrophosphate (FPP) and geranylgeranyl pyrophosphate (GGPP), and the inhibition of the synthesis of isoprenoid intermediates plays a major role in most of the pleiotropic effects of statins (56). The prenyl groups derived by mevalonate are essential for cell activities, such as growth and differentiation, because of their role in the post-translational modification of proteins involved in intracellular signaling (57–59). Thus, it is demonstrated that statins induce cell death in many cell types, including macrophages (60, 61) cardiac myocytes (62), and smooth muscle cells (SMCs) (63–65). Moreover, the apoptosis induced by statins can be totally blocked by the addition of GGPP and partially by FPP, suggesting that geranylgeranylation is a key process for this effect which does not seem to be related with the reduction of cholesterol (66).
Figure 1.
Molecular basis for a role of cholesterol and statins in the pathogenesis of Graves' Orbitopathy (GO). The symbol ⊣ indicates the pathways inhibited by statins, namely its pleiotropic effect in the regulation of apoptosis, autophagy, cell growth, and differentiation (left side of the figure), and the reduced synthesis of free fatty acids (upper sides of the figure). HMG, 3-hydroxy-3-methyl-glutaryl; MTP, microsomal triglyceride transfer protein; VLDL, very low density lipoproteins; HDL, high density lipoproteins; APO, apolipoprotein; LDL-R, low density lipoprotein receptor; FFAl, free fatty acids; TNFα, tumor necrosis factor α; ROS, reactive oxygen species; ER, endoplasmic reticulum.
To investigate the effects of blocking the mevalonate pathway on both extrinsic and intrinsic apoptosis pathways, Ghavami et al. measured cysteine-dependent aspartate-directed proteases (caspase) cleavage in human atrial fibroblast (hATF) following simvastatin treatment for up to 120 h (67). Their data showed that the activation of the intrinsic pathway is selectively due to mevalonate cascade inhibition. In particular, through HMG-CoA inhibition, statins concomitantly induced autophagy, apoptosis, and unfolded protein response (UPR) stress in the endoplasmic reticulum (ER) in hATF (67). The initiation of apoptosis is driven by the disruption of the balance between pro- and anti-apoptotic proteins. HMG-CoA inhibition also promotes UPR/ER stress, as indicated by an increase in the ER of the chaperone and signaling regulator BIP/GRP78, and by the activation of endoplasmic reticulum kinase (PERK) and transcription factor 4 (ATF4), which in turn activate the CCAAT-enhancer-binding protein homologous protein CHOP to support apoptosis. Inhibition of HMG-CoA also leads to leak of cathepsin B (CATH-B) and L (CATH-L) from lysosomes, thereby enhancing apoptosis (67), and inducing the autophagy flux. These findings suggest that statins influence autophagic events acting on the co-regulation of apoptosis and UPR (67). Even if the molecular mechanisms are not fully clarified, the activity of statins on these processes may explain, at least in part, their pleiotropic effects also in GO. Thus, the autophagic and cell death programs, which influence the innate immune signaling pathway, are the key elements of the inflammation balance. The “danger hypothesis” and the intrinsic role of autophagy in GD have been recently described by Kawashima et al. (68), who suggested that autophagic events, through the processing and delivery of cytosolic antigens, enable thyroid cells to present antigens to CD4+ T cells. Furthermore, autophagy may influence the differentiation of OFs into mature adipocytes (69), and the early autophagic flux can also trigger the cell death-cascade in several cell types, including fibroblasts and monocytoid cells (70). Based on these assumptions, the association between statin treatment and an altered autophagy due to a severe reduction of protein prenylation, reflecting blocking of the mevalonate pathway, may be a potential explanation for their protective effect on GO. As reported above, statins induce cell death in human fibroblasts (67), and it would be interesting to investigate whether this effect can also influence the production of glycosaminoglycan by OFs, and their differentiation into adipocytes and myofibroblasts. Recently, Shih et al. reported a direct correlation between mast cells and macrophage infiltration in the Muller's muscle and the extent of the upper lid retraction (71). By Masson's trichrome staining, they evaluated the proportions of fat, muscle, and fibrosis in Muller's muscle specimens. Normal muscle samples had undulating bundles of smooth muscle fibers, a thin layer of connective tissue and small deposits of fat. In contrast, GO Muller's muscles presented a decreased muscle volume and an increase in fat tissue and fibrosis (71). The immunohistochemical study of Muller's muscle showed that normal samples were characterized by mast cells and macrophages infiltrating muscular tissue. In patients with GO the mast cell component was decreased, and the share of macrophages infiltrating Muller's muscle was significantly higher. To investigate to what extent the decrease in muscle reflected an increase in apoptosis, Shih et al. performed an immunohistochemical staining for caspase-3, which was undetectable in all samples, indicating that apoptosis is not increased and that the reduced muscle volume in GO Muller's muscles likely reflects an attenuated myogenesis, augmented adipogenesis, and transdifferentiation of myoblasts into adipocytes (71). The regression models showed that mast cell infiltrating Muller's muscle correlated positively with fractional fat composition, and negatively with fractional fibrosis. Moreover, a direct correlation between macrophage counts and both fibrosis and extent of the upper eyelid retraction was observed. Overall, the findings led to the conclusion that the degree of inflammatory cell infiltration of Muller's muscle is associated with the clinical severity of the upper eyelid retraction (71). Croons et al. demonstrated that statins have the capability of triggering apoptosis in macrophages, at concentrations at which SMCs are in contrast resistant (66). Thus, according to the ability of statins of affecting macrophage viability in vitro by inducing apoptosis, the early autophagic flux induced by statins may explain apoptosis of macrophages infiltrating Muller's muscles in GO patients, suggesting a beneficial effect of these medications.
A recent study by Shahida et al. showed that Simvastatin may inhibit adipogenesis in preadipocytes and human OFs, modulating the expression of early, and late adipogenic genes in both cell types (72). They used 3T3-L1 preadipocytes and human OFs, exposing them to 10% cigarette smoke extract (CSE) with or without Simvastatin, and compared gene expression between these cells and unexposed cells. In 3T3-L1 preadipocytes, Cyr61, Ptgs2, Erg1, and Zfp36 levels were greater in cells exposed to CSE compared with unexposed cells. Interestingly, Simvastatin downregulated the expression of these genes. Moreover, CSE alone did not induce adipogenesis, while Scid1, PPAR-γ, and adipogenesis itself were reduced in preadipocytes treated with Simvastatin compared to untreated cells. Similar effects were seen also in human OFs (72).
In addition to the above-mentioned actions, statins seem to have, at least in vitro and in experimental animal models of autoimmune diseases, an immunoregulatory action (73–76), whereas, to our knowledge, there are no reports on the use of statins in human autoimmune diseases. The main immunoregulatory action of statins seems to be related to tolerogenic dendritic cells (TolDCs), a specialized subset that induces immune tolerance and counteracts autoimmune responses (74). Atorvastatin, has been shown to induce TolDCs, thereby ameliorating experimental autoimmune diseases such as myasthenia gravis and experimental autoimmune encephalomyelitis (74, 75). In addition, statins may exert an inhibitory action on antigen-presenting dendritic cells. Thus, Simvastatin was found to inhibit the maturation of myeloid dendric cells derived from peripheral blood mononuclear cells from patients with autoimmune optic neuritis and to counteract the proliferation of T-cells induced by dendritic cells (76).
Cholesterol and Go
In addition to a possible direct action of statins on the eye by their pleiotropic effects, the effects of these drugs in GO may also reflect lowering of cholesterol serum level (77). In a recent cross-sectional study, a significant correlation was found between the occurrence of GO and both total and LDL-cholesterol, in patients with a GD of relatively recent onset, suggesting a role of cholesterol in the development of GO (77). Moreover, a correlation was found between CAS and total as well as LDL-cholesterol in untreated GO patients depending on GO duration, indicating a role of cholesterol on GO activity. In the former population of patients with a GD of recent onset, based on the presence or absence of GO, cut-off values were established for total cholesterol at 191 mg/dl and for LDL-cholesterol at 118.4 mg/dL (77). Cholesterol levels above these values were associated with a significantly increased risk of GO. Still in the former population, the percentage of patients with high total cholesterol was significantly greater in patients with GO (77). Overall, the fact that the relation between GO and cholesterol was restricted only to patients with GD of recent onset could be somehow anticipated. In GD patients, there is a close temporal relation between the occurrences of hyperthyroidism and GO, and GO only very rarely appears more than 12 months after the onset of hyperthyroidism (78). This implies that risk factors for GO are more readily identified in patients with a GD of recent onset compared to patients with a long-standing disease, in whom GO occurrence is a very rare event (78). In this context, it is interesting to note that the observations of Stein et al., who, as mentioned above, found a protective role of statins in terms of GO development, were obtained in patients with GD of recent onset (51). In patients with GO, the severity and activity of the eye disease appeared to be minimally affected by serum lipids, even though CAS values were significantly higher in GO patients with high total cholesterol. It is possible that the findings may have been compromised by the fact that some patients had undergone intravenous glucocorticoid treatment for GO before enrollment, with a consequent improvement of GO. Therefore, the analysis was restricted to untreated GO patients, and a significant correlation was found by multivariate analysis with adjustment for GO duration (a variable that correlated with CAS by univariate analysis) between CAS and both total and LDL-cholesterol. In this subgroup of patients and in accordance with the findings obtained in the total cohort of GO patients, CAS was significantly higher in those with high total cholesterol (77). Overall, these data suggest the possibility that not only cholesterol is a possible GO risk factor, but also that it may be associated with more active forms of the eye disease.
In confirmation of these data, in a recent retrospective study, it was reported that patients with GO had higher LDL-cholesterol and total cholesterol compared with patients affected with GD without GO. Furthermore, the percentage of patients who had LDL-cholesterol and total cholesterol levels above the upper limit of the normal range was significantly and remarkably greater in patients with GO (79). These observations suggest that cholesterol is indeed a risk factor for GO.
The mechanisms underlying the potential link between GO and cholesterol may reflect the known altered inflammatory state of hypercholesterolemia, as shown in Figure 1. Thus, the disorders of lipid profile are associated with a mild-to-moderate, systemic, chronic inflammation (36, 37). In hepatocytes, the increased load of free fatty acids is followed by an altered function of mitochondria and endoplasmic reticulum, which ultimately causes the release of reactive oxygen species. Moreover, though indirect mechanisms, free fatty acids trigger the release of pro-inflammatory cytokines, in particular interleukin-6 and tumor-necrosis factor-α, which are both involved in the pathogenetic mechanisms of GO. In support of an altered inflammatory state in hypercholesterolemia as the possible cause of the association between GO and high cholesterol, Busnelli et al. reported that statins are protective in terms of systemic inflammation in swine (80). Obviously, these explanations are speculative and further investigations are required.
Strengths and Limitations
The observation of a protective role of statins in developing GO in GD patients as well as the correlation of GO and its activity with serum cholesterol are quite novel, and promising for a possible use of statins in GO. On the other hand, the studies available so fare are quite few, no randomized clinical trial are available, because of which the role of statins, and of cholesterol in GO must be considered still preliminary.
Conclusions
Both basic and clinical findings regarding the effects of statins on GO are encouraging and deserve to be better investigated. Whether statins have an intrinsic role or their effects are related to their capability of lowering cholesterol has to be clarified. Nevertheless, the relation between the presence and the activity of GO and the levels of cholesterol in patients with GD and GO of recent onset may have important clinical implications as they may unravel a new field in GO management, and prompt the necessity for investigating if lowering cholesterol is associated with improved GO outcomes. If the data were confirmed, the use of statins could be considered to improve the efficacy of immunosuppressive therapy, maybe allowing to reduce GC dosage of and consequently limiting their side effects. Clearly, these are just speculations and further, possibly prospective studies are needed.
Author Contributions
GL conceived and wrote the manuscript. GV, II, IC, FS, and EL performed the literature search and revised manuscript critically. MM conceived, revised, and supervised the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. The authors declare that this study received funding from Fullcro S.r.l. The funder had the following involvement with the study: payment of publication costs. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, et al. The 2016 european thyroid association/european group on graves' orbitopathy guidelines for the management of graves' orbitopathy. Eur Thyroid J. (2016) 5:9–26. 10.1159/000443828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piantanida E, Tanda ML, Lai A, Sassi L, Bartalena L. Prevalence and natural history of Graves' orbitopathy in the XXI century. J Endocrinol Invest. (2013) 36:444–9. 10.3275/8937 [DOI] [PubMed] [Google Scholar]
- 3.Leo M, Menconi F, Rocchi R, Latrofa F, Sisti E, Profilo MA, et al. Role of the underlying thyroid disease on the phenotype of Graves' orbitopathy in a tertiary referral center. Thyroid. (2015) 25:347–51. 10.1089/thy.2014.0475 [DOI] [PubMed] [Google Scholar]
- 4.Smith TJ, Janssen JAMJL. Insulin-like growth factor-i receptor and thyroid-associated ophthalmopathy. Endocr Rev. (2019) 40:236–67. 10.1210/er.2018-00066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marinò M, Rotondo Dottore G, Ionni I, Lanzolla G, Sabini E, Ricci D, et al. Serum antibodies against the insulin-like growth factor-1 receptor (IGF-1R) in Graves' disease and Graves' orbitopathy. J Endocrinol Invest. (2019) 42:471–80. 10.1007/s40618-018-0943-8 [DOI] [PubMed] [Google Scholar]
- 6.Marinò M, Latrofa F, Menconi F, Chiovato L, Vitti P. Role of genetic and non-genetic factors in the etiology of Graves' disease. J Endocrinol Invest. (2015) 38:283–94. 10.1007/s40618-014-0214-2 [DOI] [PubMed] [Google Scholar]
- 7.Bahn RS. Current insights into the pathogenesis of Graves' Ophthalmopathy. Horm Metab Res. (2015) 47:773–8. 10.1055/s-0035-1555762 [DOI] [PubMed] [Google Scholar]
- 8.Sisti E, Menconi F, Leo M, Profilo MA, Mautone T, Mazzi B, et al. Long-term outcome of Graves' orbitopathy following high-dose intravenous glucocorticoids and orbital radiotherapy. J Endocrinol Invest. (2015) 38:661–8. 10.1007/s40618-015-0241-7 [DOI] [PubMed] [Google Scholar]
- 9.Bartalena L. Prevention of Graves' ophthalmopathy. Best Pract Res Clin Endocrinol Metab. (2012) 26:371–9. 10.1016/j.beem.2011.09.004 [DOI] [PubMed] [Google Scholar]
- 10.Menconi F. Total thyroid ablation in Graves' orbitopathy. J Endocrinol Invest. (2015) 38:809–15. 10.1007/s40618-015-0255-1 [DOI] [PubMed] [Google Scholar]
- 11.Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, et al. Clinical features of Graves' ophthalmopathy in an incidence cohort. Am J Ophthalmol. (1996) 121:284–90. 10.1016/S0002-9394(14)70276-4 [DOI] [PubMed] [Google Scholar]
- 12.Prummel MF, Wiersinga WM, Mourits MP, Koornneef L, Berghout A, van der Gaag R. Effect of abnormal thyroid function on the severity of Graves' ophthalmopathy. Arch Intern Med. (1990) 150:1098–101. 10.1001/archinte.1990.00390170124027 [DOI] [PubMed] [Google Scholar]
- 13.Bartalena L, Marcocci C, Bogazzi F, Manetti L, Tanda ML, Dell'Unto E, et al. Relation between therapy for hyperthyroidism and the course of Graves' ophthalmopathy. N Engl J Med. (1998) 338:73–7. 10.1056/NEJM199801083380201 [DOI] [PubMed] [Google Scholar]
- 14.Lai A, Sassi L, Compri E, Marino F, Sivelli P, Piantanida E, et al. Lower dose prednisone prevents radioiodine-associated exacerbation of initially mild or absent Graves' orbitopathy: a retrospective cohort study. J Clin Endocrinol Metab. (2010) 95:1333–1337. 10.1210/jc.2009-2130 [DOI] [PubMed] [Google Scholar]
- 15.Watanabe N, Noh JY, Kozaki A, Iwaku K, Sekiya K, Kosuga Y, et al. Radioiodine-associated exacerbation of Graves' orbitopathy in the Japanese population: randomized prospective study. J Clin Endocrinol Metab. (2015) 100:2700–8. 10.1210/jc.2014-4542 [DOI] [PubMed] [Google Scholar]
- 16.Tra..isk F, Tallstedt L, Abraham-Nordling M, Andersson T, Berg G, Calissendorff J, et al. Thyroid-associated ophthalmopathy after treatment for Graves' hyperthyroidism with antithyroid drugs or iodine-131. J Clin Endocrinol Metab. (2009) 94:3700–007. 10.1210/jc.2009-0747 [DOI] [PubMed] [Google Scholar]
- 17.Wiersinga WM. Smoking and thyroid. Clin Endocrinol. (2013) 79:145–51. 10.1111/cen.12222 [DOI] [PubMed] [Google Scholar]
- 18.Khong JJ, Finch S, De Silva C, Rylander S, Craig JE, Selva D, et al. Risk factors for Graves' orbitopathy; the Australian Thyroid-Associated Orbitopathy Research (ATOR) study. J Clin Endocrinol Metab. (2016) 101:2711–20. 10.1210/jc.2015-4294 [DOI] [PubMed] [Google Scholar]
- 19.Anagnostis P, Boboridis K, Adamidou F, Kita M. Natural course of mild Graves' orbitopathy: is it a chronic remitting or a transient disease? J Endocrinol Invest. (2017) 40:257–61. 10.1007/s40618-016-0555-0 [DOI] [PubMed] [Google Scholar]
- 20.Bartalena L, Masiello E, Magri F, Veronesi G, Bianconi E, Zerbini F, et al. The phenotype of newly diagnosed Graves' disease in Italy in recent years is milder than in the past: results of a large observational longitudinal study. J Endocrinol Invest. 39:1445–51. 10.1007/s40618-016-0516-7 [DOI] [PubMed] [Google Scholar]
- 21.Bartalena L, Chiovato L, Vitti P. Management of hyperthyroidism due to Graves' disease: frequently asked questions and answers (if any). J Endocrinol Invest. (2016) 39:1105–14. 10.1007/s40618-016-0505-x [DOI] [PubMed] [Google Scholar]
- 22.Mourits MP, Prummel MF, Wiersinga WM, Koornneef L. Clinical activity score as a guide in the management of patients with Graves' ophthalmopathy. Clin Endocrinol. (1997) 47:632. 10.1046/j.1365-2265.1997.2331047.x [DOI] [PubMed] [Google Scholar]
- 23.Marcocci C, Kahaly GJ, Krassas GE, Bartalena L, Prummel M, Stahl M, et al. Selenium and the course of mild Graves' orbitopathy. N Engl J Med. (2011) 364:1920–31. 10.1056/NEJMoa1012985 [DOI] [PubMed] [Google Scholar]
- 24.Marinò M, Dottore GR, Leo M, Marcocci C. Mechanistic pathways of selenium in treatment for Graves' disease and Graves' orbitopathy. Horm Metabol Res. (2018) 50:887–93. 10.1055/a-0658-7889 [DOI] [PubMed] [Google Scholar]
- 25.Stan MN, Salvi M. Management of endocrine disease: rituximab therapy for Graves' orbitopathy - lessons from randomized control trials. Eur J Endocrinol. (2016) 176:R101–9. 10.1530/EJE-16-0552 [DOI] [PubMed] [Google Scholar]
- 26.Smith TJ, Kahaly GJ, Ezra DG, Fleming JC, Dailey RA, Tang RA, et al. Teprotumumab for thyroid-associated ophthalmopathy. N Engl J Med. (2017) 376:1748–61. 10.1056/NEJMoa1614949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piantanida E, Bartalena L. Teprotumumab: a new avenue for the management of moderate-to-severe and active Graves' orbitopathy? J Endocrinol Invest. (2017) 40:885–7. 10.1007/s40618-017-0717-8 [DOI] [PubMed] [Google Scholar]
- 28.Kahaly GJ, Riedl M, König J, Pitz S, Ponto K, Diana T, et al. Combined mycophenolate + prednisolone therapy is more effective than prednisolone in active and moderate-to-severe Graves' Orbitopathy – a randomized, observer blind, multicenter trial. Lancet Diabetes Endocrinol. (2018) 6:287–98. 10.1016/S2213-8587(18)30020-2 [DOI] [PubMed] [Google Scholar]
- 29.Pérez-Moreiras JV. Treatment of active corticosteroid-resistant Graves' Orbitopathy. Ophthalmic Plast. Reconstr. Surg. (2014) 30:162–7. 10.1097/IOP.0000000000000037 [DOI] [PubMed] [Google Scholar]
- 30.Sellari-Franceschini S, Rocchi R, Marinò M, Bajraktari A, Mazzi B, Fiacchini, et al. Rehabilitative orbital decompression for Graves' Orbitopathy: results of a randomized clinical trial. J Endocrinol Invest. (2018) 41:1037–42. 10.1007/s40618-018-0847-7 [DOI] [PubMed] [Google Scholar]
- 31.Tu X, Dong Y, Zhang H, Su Q. Corticosteroids for Graves' Ophthalmopathy: systematic review and meta-analysis. Biomed Res Int. (2018) 2018:4845894. 10.1155/2018/4845894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hart RH, Kendall-Taylor P, Crombie A, Perros P. Early response to intravenous glucocorticoids for severe thyroid-associated ophthalmopathy predicts treatment outcome. J Ocul Pharmacol Ther. (2005) 21:328–36 10.1089/jop.2005.21.328 [DOI] [PubMed] [Google Scholar]
- 33.Zang S, Ponto KA, Kahaly GJ. Intravenous glucocorticoids for Graves' orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab. (2011) 96:320–32. 10.1210/jc.2010-1962 [DOI] [PubMed] [Google Scholar]
- 34.Salvi M, Campi I. Medical treatment of Graves' orbitopathy. Horm Metab Res. (2015) 47:779–88. 10.1055/s-0035-1554721 [DOI] [PubMed] [Google Scholar]
- 35.Goldstein JL, Brown MS. A century of cholesterol and coronaries: from plaques to genes to statins. Cell. (2015) 161:161–72. 10.1016/j.cell.2015.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ridker PM, Group JS. Rosuvastatin in the primary prevention of cardiovascular disease among patients with low levels of low-density lipoprotein cholesterol and elevated high-sensitivity C-reactive protein: rationale and design of the JUPITER trial. Circulation. (2003) 108:2292–7. 10.1161/01.CIR.0000100688.17280.E6 [DOI] [PubMed] [Google Scholar]
- 37.Fonseca FA, Izar MC. Primary prevention of vascular events in patients with high levels of C-reactive protein: the JUPITER study. Expert Rev Cardiovasc Ther. (2009) 7:1041–56. 10.1586/erc.09.93 [DOI] [PubMed] [Google Scholar]
- 38.Verma A, Lavie CJ, Milani RV. C-reactive protein: how has JUPITER impacted clinical practice? Ochsner J. (2009) 9:204–10. [PMC free article] [PubMed] [Google Scholar]
- 39.Chang JW, Yang WS, Min WK, Lee SK, Park JS, Kim SB. Effects of simvastatin on high-sensitivity C-reactive protein and serum albumin in hemodialysis patients. Am J Kidney Dis. (2002) 39:1213–7. 10.1053/ajkd.2002.33393 [DOI] [PubMed] [Google Scholar]
- 40.McKay A, Leung BP, McInnes IB, Thomson NC, Liew FY. A novel anti-inflammatory role of simvastatin in a murine model of allergic asthma. J Immunol. (2003) 172:2903–8. 10.4049/jimmunol.172.5.2903 [DOI] [PubMed] [Google Scholar]
- 41.Stuve O, Prod'homme T, Slavin A, Youssef S, Dunn S, Steinman L, et al. Statins and their potential targets in multiple sclerosis therapy. Expert Opin Ther Targets. (2003) 7:613–22. 10.1517/14728222.7.5.613 [DOI] [PubMed] [Google Scholar]
- 42.Stuve O, Youssef S, Steinman L, Zamvil SS. Statins as potential therapeutic agents in neuroinflammatory disorders. Curr Opin Neurol. (2003) 16:393–401. 10.1097/01.wco.0000073942.19076.d1 [DOI] [PubMed] [Google Scholar]
- 43.Walsh GM. Statins as emerging treatments for asthma and chronic obstructive pulmonary disease. Expert Rev Respir Med. (2008) 2:329–35. 10.1586/17476348.2.3.329 [DOI] [PubMed] [Google Scholar]
- 44.Huang CC, Chan WL, Chen YC, Chen TJ, Chou KT, Lin SJ, et al. Statin use in patients with asthma: a nationwide population-based study. Eur J Clin Invest. (2011) 41:507–12. 10.1111/j.1365-2362.2010.02434.x [DOI] [PubMed] [Google Scholar]
- 45.Paul F, Waiczies S, Wuerfel J, Bellmann-Strobl J, Dörr J, Waiczies H, et al. Oral high-dose atorvastatin treatment in relapsing-remitting multiple sclerosis. PLoS ONE. (2008) 3:e1928. 10.1371/journal.pone.0001928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vollmer T, Key L, Durkalski V, Tyor W, Corboy J, Markovic-Plese S, et al. Oral simvastatin treatment in relapsing-remitting multiple sclerosis. Lancet. (2004) 363:1607–8. 10.1016/S0140-6736(04)16205-3 [DOI] [PubMed] [Google Scholar]
- 47.Semb AG, Holme I, Kvien TK, Pedersen TR. Intensive lipid lowering in patients with rheumatoid arthritis and previous myocardial infarction: an explorative analysis from the incremental decrease in endpoints through aggressive lipid lowering (IDEAL) trial. Rheumatology. (2011) 50:324–9. 10.1093/rheumatology/keq295 [DOI] [PubMed] [Google Scholar]
- 48.McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, et al. Trial of Atorvastatin in rheumatoid arthritis (TARA): double-blind, randomised placebo-controlled trial. Lancet. (2004) 363:2015–21. 10.1016/S0140-6736(04)16449-0 [DOI] [PubMed] [Google Scholar]
- 49.Hu Y, Tong G, Xu W, Pan J, Ryan K, Yang R, et al. Anti-inflammatory effects of simvastatin on adipokines in type 2 diabetic patients with carotid atherosclerosis. Diab Vasc Dis Res. (2009) 6:262–8. 10.1177/1479164109339966 [DOI] [PubMed] [Google Scholar]
- 50.Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. (2005) 4:977–87. 10.1038/nrd1901 [DOI] [PubMed] [Google Scholar]
- 51.Stein JD, Childers D, Gupta S, Talwar N, Nan B, Lee BJ, et al. Risk factors for developing thyroid-associated ophthalmopathy among individuals with Graves Disease. JAMA Ophthalmol. (2015) 133:290–6. 10.1001/jamaophthalmol.2014.5103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bifulco M, Ciaglia E. Statin reduces orbitopathy risk in patients with Graves' disease by modulating apoptosis and autophagy activities. Endocrine. (2016) 53:649–50. 10.1007/s12020-015-0762-z [DOI] [PubMed] [Google Scholar]
- 53.Correale M, Brunetti ND, Totaro A, Montrone D, Russo AR, Fanigliulo AM, et al. Statin therapy blunts inflammatory activation and improves prognosis and left ventricular performance assessed by tissue doppler imaging in subjects with chronic ischemic heart failure: results from the Daunia Heart Failure Registry. Clinics. (2011) 66:777–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang L, Zhang L, Sun A, Jiang H, Qian J, Ge J, et al. Effects of statin treatment on cardiac function in patients with chronic heart failure: a meta-analysis of randomized controlled trials. Clin Cardiol. (2011) 34:117–23. 10.1002/clc.20821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Piepoli M.F, Hoes AW, Brotons C, Hobbs RFD, Corra U. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2016) 38:2739–91. 10.1080/13814788.2017.1398320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol. (2001) 21:1712–9. 10.1161/hq1101.098486 [DOI] [PubMed] [Google Scholar]
- 57.Buhaescu I, Izzedine H. Mevalonate pathway: a review of clinical and therapeutical implications. Clin Biochem. (2007) 40:575–84. 10.1016/j.clinbiochem.2007.03.016 [DOI] [PubMed] [Google Scholar]
- 58.Dai Y, Khanna P, Chen S, Pei XY, Dent P, Grant S. Statins synergistically potentiate 7-hydroxystaurosporine (UCN-01) lethality in human leukemia and myeloma cells by disrupting Ras farnesylation and activation. Blood. (2007) 109:4415–23. 10.1182/blood-2006-09-047076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hamada M, Khanna P, Chen S, Pei XY, Dent P, Grant S. Involvement of RhoA and RalB in geranylgeranyltransferase I inhibitor-mediated inhibition of proliferation and migration of human oral squamous cell carcinoma cells. Cancer Chemother Pharmacol. (2011) 68:559–69. 10.1007/s00280-010-1520-9 [DOI] [PubMed] [Google Scholar]
- 60.Vamvakopoulos JE, Green C. HMG-CoA reductase inhibition aborts functional differentiation and triggers apoptosis in cultured primary human monocytes: a potential mechanism of statin-mediated vasculoprotection. BMC Cardiovasc Disord. (2003) 3:6. 10.1186/1471-2261-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim YC, Song SB, Lee MH, Kang KI, Lee H, Paik SG, et al. Simvastatin induces caspaseindependent apoptosis in LPS-activated RAW264.7 macrophage cells. Biochem Biophys Res Commun. (2006) 339:1007–14. 10.1016/j.bbrc.2005.11.099 [DOI] [PubMed] [Google Scholar]
- 62.Demyanets S, Kaun C, Pfaffenberger S, Hohensinner PJ, Rega G, Pammer J. Hydroxymethylglutarylcoenzyme A reductase inhibitors induce apoptosis in human cardiac myocytes in vitro. Biochem Pharmacol. (2006) 71:1324–30. 10.1016/j.bcp.2006.01.016 [DOI] [PubMed] [Google Scholar]
- 63.Martinet W, Schrijvers DM, Timmermans JP, Bult H. Interactions between cell death induced by statins and 7-ketocholesterol in rabbit aorta smooth muscle cells. Br J Pharmacol. (2008) 154:1236–46. 10.1038/bjp.2008.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baetta R, Donetti E, Comparato C, Calore M, Rossi A, Teruzzi C, et al. Proapoptotic effect of atorvastatin on stimulated rabbit smooth muscle cells. Pharmacol Res. (1997) 36:115–21. 10.1006/phrs.1997.0211 [DOI] [PubMed] [Google Scholar]
- 65.Guijarro C, Blanco-Colio LM, Ortego M, Alonso C, Ortiz A, Plaza JJ, et al. 3-Hydroxy-3-methylglutaryl coenzyme a reductase and isoprenylation inhibitors induce apoptosis of vascular smooth muscle cells in culture. Circ Res. (1998) 83:490–500. 10.1161/01.RES.83.5.490 [DOI] [PubMed] [Google Scholar]
- 66.Croons V, De Meyer I, Houten SM, Martinet W, Bult H, Herman AG, et al. Effect of Statins on the viability of macrophages and smooth muscle cells. J. Cardiovasc Pharmacol. (2010) 55:269–75. 10.1097/FJC.0b013e3181d0bec3 [DOI] [PubMed] [Google Scholar]
- 67.Ghavami S, Yeganeh B, Stelmack GL, Kashani HH, Sharma P, Cunnington R, et al. Apoptosis, autophagy and ER stress in mevalonate cascade inhibition-induced cell death of human atrial fibroblasts. Cell Death Dis. (2012) 3:e330. 10.1038/cddis.2012.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kawashima A, Tanigawa K, Akama T, Yoshihara A, Ishii N, Suzuki K. Innate immune activation and thyroid autoimmunity. J Clin Endocrinol Metab. (2011) 96:3661–71. 10.1210/jc.2011-1568 [DOI] [PubMed] [Google Scholar]
- 69.Yoon JS, Lee HJ, Chae MK, Lee EJ. Autophagy is involved in the initiation and progression of Graves' orbitopathy. Thyroid. (2015) 25:445–54. 10.1089/thy.2014.0300 [DOI] [PubMed] [Google Scholar]
- 70.Maiuri MC, Zalckvar E, Kimchi A, Kroemer G. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat Rev Mol Cell Biol. (2007) 8:741–52. 10.1038/nrm2239 [DOI] [PubMed] [Google Scholar]
- 71.Shih M-J, Liao SL, Kuo KT, Smith TJ, Chuang LM. Molecular pathology of muller's muscle in Graves' ophthalmopathy. JCEM. (2006) 91:1159–67 10.1210/jc.2005-1877 [DOI] [PubMed] [Google Scholar]
- 72.Shahida B, Johnson PS, Jain R, Brorson H, Åsman P, Planck T, et al. Simvastatin downregulates adipogenesis in 3T3-L1 preadipocytes and orbital fibroblasts from Graves' ophthalmopathy patients. Endocr Connect. (2019). 10.1530/EC-19-0319. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mira E, Manes S. Immunomodulatory and anti-inflammatory activities of statins. Endocr Metab Immune Disord Drug Targets. (2009) 9:237–47. 10.2174/187153009789044383 [DOI] [PubMed] [Google Scholar]
- 74.Chen Z, Yang D, Peng X, Lin J, Su Z, Li J, et al. Beneficial effect of atorvastatin-modified dendritic cells pulsed with myelin oligodendrocyte glycoprotein autoantigen on experimental autoimmune encephalomyelitis. Neuroreport. (2018) 29:317–27. 10.1097/WNR.0000000000000962 [DOI] [PubMed] [Google Scholar]
- 75.Li H, Wang CC, Zhang M, Li XL, Zhang P, Yue LT, et al. Statin-modified dendritic cells regulate humoral immunity in experimental autoimmune myasthenia gravis. Mol Cell Neurosci. (2015) 68:284–92. 10.1016/j.mcn.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 76.Tsakiri A, Tsiantoulas D, Frederiksen J, Svane IM. Increased immunopotency of monocyte derived dendritic cells from patients with optic neuritis is inhibited in vitro by simvastatin. Exp Neurol. (2010) 221:320–8. 10.1016/j.expneurol.2009.11.014 [DOI] [PubMed] [Google Scholar]
- 77.Sabini E, Mazzi B, Profilo MA, Mautone T, Casini G, Rocchi R, et al. High serum cholesterol is a novel risk factor for Graves' orbitopathy: results of a Cross-Sectional Study. Thyroid. (2018) 28:386–94. 10.1089/thy.2017.0430 [DOI] [PubMed] [Google Scholar]
- 78.Wiersinga WM, Smit T, Van der Gaag R, Koornneef L. Temporal relationship between onset of Graves' ophthalmopathy and onset of thyroidal Graves' disease. J Endocrinol Invest. (1988) 11:615–9. 10.1007/BF03350193 [DOI] [PubMed] [Google Scholar]
- 79.Lanzolla G, Sabini E, Profilo MA, Mazzi B, Sframeli A, Rocchi R, et al. Relationship between serum cholesterol and Graves' orbitopathy (GO): a confirmatory study. J Endocrinol Invest. (2018) 41:1417–23. 10.1007/s40618-018-0915-z [DOI] [PubMed] [Google Scholar]
- 80.Busnelli M, Manzini S, Froio A, Vargiolu A, Cerrito MG, Smolenski RT, et al. Diet induced mild hypercholesterolemia in pigs: local and systemic inflammation, effects on vascular injury - rescue by high-dose statin treatment. PLoS ONE. (2013) 8:e80588. 10.1371/journal.pone.0080588 [DOI] [PMC free article] [PubMed] [Google Scholar]