Abstract
Background:
Psychiatric comorbidity with diabetes mellitus is common. Comorbidity of diabetes and psychiatric disorders can present in different patterns, which are associated with impaired quality of life, increased cost of care, poor treatment adherence, poor glycaemia control and increased emergency room visits. The present study was planned to assess the psychiatric comorbidity in type 2 diabetic patients at tertiary care hospital in a hilly state of North India.
Objectives:
To study the prevalence of psychiatric comorbidity among patients of type 2 diabetes mellitus and to study the association between psychiatric comorbidity, sociodemographic and clinical variables in such patients.
Materials and Methods:
A cross-sectional study was conducted after enrolling the eligible diabetic patients attending outpatient department services of medicine department, Indira Gandhi Medical College, Shimla. The Brief Illness Perception Questionnaire was used to assess the cognitive and emotional aspects of illness, Hamilton Depression Rating Scale for assessment of depression, Hamilton Anxiety Rating Scale for assessing severity of anxiety and Mini-International Neuropsychiatric Interview 6.0 for screening all major Axis I disorders.
Results:
Out of 320 patients of type 2 diabetes mellitus screened, 202 eligible patients were enrolled. Depression was the most common psychiatric comorbid illness present in (41.9%) patients. Depression was slightly higher in female patients and persons aged >50 years. Greater prevalence of depressive episodes was there in people with longer duration of diabetes.
Conclusion:
There were a significant percentage of diabetic patients having psychiatric illnesses. Their attitude towards these comorbidities may be changed by psychiatric counselling at regular intervals.
Keywords: Comorbidity, depression, diabetes, quality of life
INTRODUCTION
Diabetes mellitus (DM) comprises a group of common metabolic disorders that share the phenotype of hyperglycaemia. Widespread metabolic deregulation imposes tremendous physical and psychological burden.[1] Prevalence of diabetes in India ranges from 2.7% to 15.1%. As per the International Diabetic Federation 2013, 9.1% of the adult population may be suffering from diabetes in India.[2]
Diabetic patients are twice as likely as the general population to suffer from depression, with higher risk in women. During a 5-year follow up, 80% of diabetic patients have recurrence of depressive episodes.[3] Depression and anxiety in particular are more frequent in diabetic patients. Patients with DM suffering from depression have a higher incidence of suicidal ideations. Psychological stress factors play an active role in both aetiology and the metabolic control of DM. Other contributing factors in the pathogenesis of type 2 diabetes mellitus (T2DM) include environmental and lifestyle factors, family history, ethnicity and genetics.[4] Psychological distress can occur when DM is first diagnosed: Denial, anger, guilt, reactive depression and finally acceptance are the reactions, which are anticipated and take months to resolve.[5] Patients with mental health disorders receive less medical care for DM. The quality of life of the patient is adversely affected due to the knowledge about the course of illness, restriction of diet and activity, closely monitored management schedules and the continued risk of acute and chronic life-threatening complications.[6] “Diabetes burnout” and “Diabetes overwhelmus” are the words used often to describe the distress experienced by diabetic patients. Comorbidity of diabetes and psychiatric disorders can present in different patterns. First, the two can present as independent conditions with no apparent direct connection. Second, the course of diabetes can be complicated by emergence of psychiatric disorders. Third, certain psychiatric disorders like depression and schizophrenia act as significant independent risk factors for development of diabetes. Fourth, there could be an overlap between the clinical presentations of hypoglycaemic or ketoacidosis episodes and conditions such as panic attacks. Fifth, impaired glucose tolerance and diabetes could emerge as a side effect of the medications used for psychiatric disorders. Biochemical changes due to the mental and treatment with second-generation (atypical) antipsychotic agents may actually increase the risk of diabetes.[7]
Psychiatric disorders in patients with diabetes lead to increase cost of care, poor treatment adherence, poor glycaemia control, increased emergency room visits, hospitalization higher rate of absenteeism and increased diabetes-specific mortality.[8]
Fragmentation of medical and psychiatric treatment further complicates the management of comorbid diabetes and psychosis. The low quality of medical care for patients with diabetes and psychosis should be deemed a modifiable risk factor for poor diabetes outcomes. Research specifically on patients with comorbid diabetes and psychotic disorders is scarce, and patients with serious mental illness have typically been excluded from large clinical trials of medications and interventions for diabetes.[9,10] Indians are more susceptible for diabetes because of increased insulin resistance, abdominal obesity, decreased adiponectin and increased C-reactive protein levels.[11] Keeping above facts in view, the present study was planned to assess the psychiatric comorbidity in T2DM patients.
AIMS AND OBJECTIVES
To study the prevalence of psychiatric comorbidity among patients of T2DM
To study the association between psychiatric comorbidity and sociodemographic and clinical variables in patients with T2DM.
MATERIAL AND METHODS
Study setting
The study was conducted at Indira Gandhi Medical College, Shimla, which is a Tertiary Care Centre of hilly state of Himachal Pradesh catering majority of the population of the state.
Study design
Descriptive cross-sectional study.
Study population and sample size
All the patients attending outpatient department (OPD) services of medicine department, who were diagnosed with T2DM, were screened for enrolment in the study during August 2016 to July 2017. The eligible patients who fulfilled following inclusion and exclusion criteria and gave written informed consent were enrolled in the study.
Inclusion criteria
Patients within the age group of 18-60 years diagnosed with T2DM
Willingness to participate in the study.
Exclusion criteria
Patients with history of epilepsy, mental retardation and neurocognitive disorders
Patients with any chronic medical illness other than DM and on long-term treatment for any other medical and psychiatric illness
Patients having chronic DM with complications such as renal cardiovascular system and neuropathy.
Tools
Sociodemographic Profile Sheet: This semi-structured, pretested proforma was used to record information regarding sociodemographic variables
Case Record Form: Self-devised, semi-structured and pretested proforma used to record historical and clinical details
The Brief Illness Perception Questionnaire (B-Ipq):[12] The B-IPQ, a nine-item scale designed to rapidly assess the cognitive and emotional representations of illness
The International Classification Of Diseases, Tenth Revision (ICD-10):[13] Diagnosis of psychiatric disorders was made according to ICD-10
Hamilton Depression Rating Scale (HAM-D):[14] The HAM-D is the most widely used clinician-administered depression assessment scale. The original version contains 17 items (HAM-D17) pertaining to symptoms of depression experienced over the past week. Internal consistency was assessed using Cronbach's α. A “receiver operating characteristics” curve was obtained and the sensitivity, specificity, positive and negative predictive values were calculated for different cut-off points of the HAMD-17, illustrating the discriminative properties of the scale in the selected patient population. It is a valid and reliable tool to assess the severity of depression
Hamilton Anxiety Rating Scale (HAM-A):[15] The HAM-A was one of the first rating scales developed to measure the severity of anxiety symptoms. The scale consists of 14 items, each defined by a series of symptoms, and measures both psychic anxiety and somatic anxiety. It is a valid and reliable tool
Mini-International Neuropsychiatric Interview 6.0 (Mini 6.0):[16] The MINI 6.0 screens for all major Axis I disorders, including schizophrenia, anxiety, mood disorders, eating disorders, and substance dependence. There is also a brief screen for suicidality. It is available in multiple languages, for children, and other populations, and is easy to administer, with good reliability and validity.
Data collection
After obtaining a written informed consent from all eligible patients a detailed history from the patient and/or a reliable person who knows the patient well was taken. Sociodemographic and clinical data were obtained from the patients, relatives and recorded using semi-structured formats. The Brief Illness Perception Questionnaire (B-IPQ) was used to assess the cognitive and emotional representations of illness. Diagnosis of psychiatric disorders was made according to The International Classification of Diseases, Tenth Revision (ICD-10). Psychiatric symptoms were also assessed by using Mini-International Neuropsychiatric Interview 6.0 (M.I.N.I.6.0). If the patient was found to have anxiety or depressive disorder, the severity of the same was assessed by using appropriate scales Hamilton Depression Rating Scale (HAM-D), or Hamilton Anxiety Rating Scale (HAM-A) as per the psychiatric diagnosis.
Routine blood investigations like FPG\PPG, HbA1c, complete haemogram, ESR, T3\T4\TSH, serum urea/creatinine, lipid profile, SGOT\SGPT\serum total and direct bilirubin, serum electrolytes and X-ray chest were carried out as per need of the patient.
Statistical analysis
Data was entered into Microsoft Excel. Data were analysed using statistical software Epi Info version 7.2.0.1. The categorical variables and continuous variables reported as percentages and mean ± standard deviation respectively.
RESULTS
A total of 320 patients of T2DM were screened, out of which 202 eligible patients were enrolled in the study. The age of the patients ranged from 24 years to 60 years with mean age of 50.63 ± 09.37 years. Females comprised 48% of study population. Most of the patients (64%) belonged to rural area and 95% were married [Figures 1 and 2]. Majority 187 (92.5%) of patients were either matriculate or graduate and more than half of the patients 129 (63.9%) were farmers [Figures 3 and 4]. Maximum number of 162 (80.2%) patients belonged to joint families and only 40 (19.8%) patients belonged to nuclear families. Out of 202 patients, most of the 146 (72.3%) patients belonged to middle socioeconomic class and 56 (27.7%) patients belonged to lower socioeconomic class [Figure 5]. Out of the 202 patients, 118 (58.4%) patients had psychiatric comorbidity. Depression was the most common psychiatric comorbid illness present in 85 (41.9%) patients [Figure 6].
Figure 1.
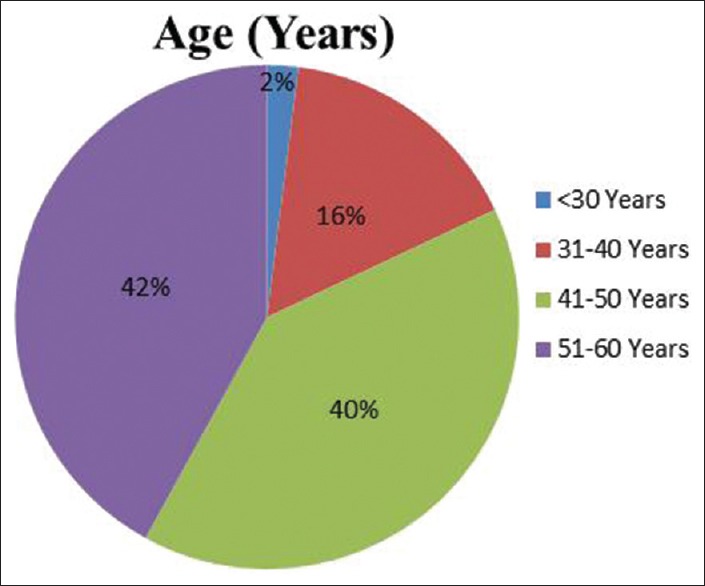
Age distribution
Figure 2.
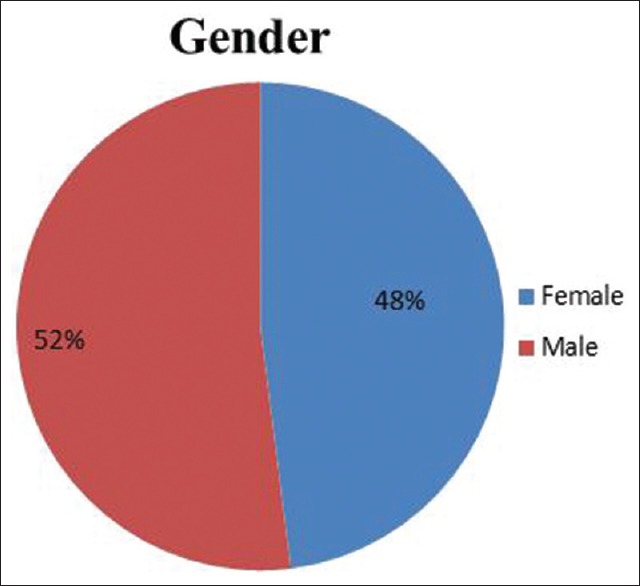
Gender distribution
Figure 3.
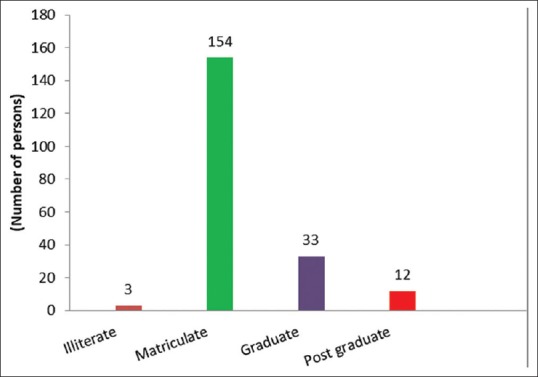
Educational status
Figure 4.
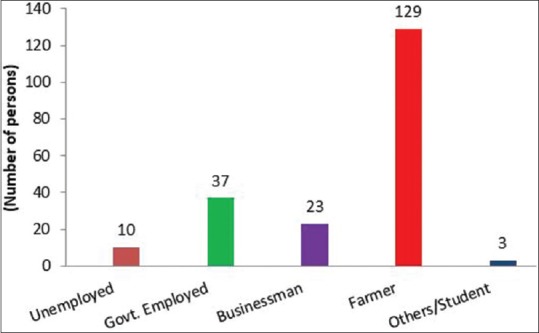
Occupational status
Figure 5.
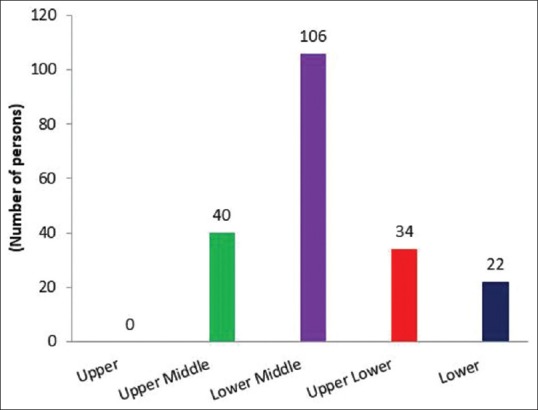
Socioeconomic Status
Figure 6.
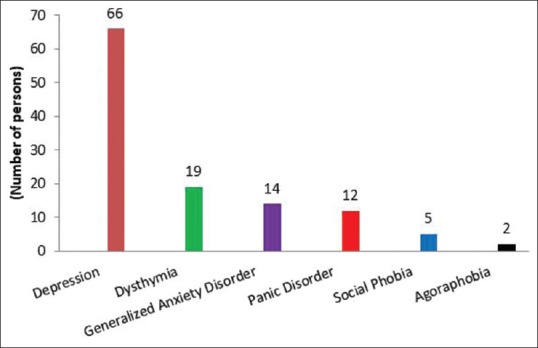
Types of psychiatric morbidity
In present study, the crude prevalence of psychiatric comorbidity especially depression was higher in the higher age group (>50 years = 20.5%, Table 1); however, it was not statistically significant (P-value >0.05). Various psychiatric morbidities were higher in females as compared to males [Table 2], similar trend was seen in farmers as well [Table 3] but were statistically not significant. There was no significant relation between psychiatric illness and marital status [Table 4].
Table 1.
Relationship between psychiatric comorbidity and age
| Psychiatric comorbidity | Number of patients (n) | Percentage | Chi square | P |
|---|---|---|---|---|
| Depressive episode | >50 years=42 | 20.5 | 2.3 | 0.07 |
| <50 years=24 | 12.0 | |||
| Dysthymia | >50 years=12 | 5.8 | 3.5 | 0.25 |
| <50 years=7 | 3.6 | |||
| Generalized anxiety disorder | >50 years=8 | 3.8 | 0.6 | 0.82 |
| <50 Years=6 | 3.0 | |||
| Panic Disorder | >50 years=7 | 3.4 | 1.7 | 1.25 |
| <50 years=5 | 2.6 | |||
| Social Phobia | >50 years=3 | 1.5 | 0.3 | 0.9 |
| <50 years=2 | 1.0 | |||
| Agoraphobia | >50 years=2 | 0.9 | 0.2 | 0.76 |
| <50 years=0 | 0 |
Table 2.
Relationship between psychiatric comorbidity and gender
| Psychiatric comorbidity | Number of patients (n) | Percentage (%) | Chi square | P |
|---|---|---|---|---|
| Depressive episode | Male=28 | 14.0% | 4.2 | 0.55 |
| Female=38 | 18.5% | |||
| Dysthymia | Male=8 | 4.0% | 2.4 | 0.86 |
| Female=11 | 5.4% | |||
| Generalized anxiety disorder | Male=7 | 3.2% | 0.8 | 0.91 |
| Female=7 | 3.6% | |||
| Panic Disorder | Male=6 | 3.2% | 1.2 | 0.32 |
| Female=6 | 2.8% | |||
| Social Phobia | Male=3 | 1.5% | 0.3 | 0.9 |
| Female=2 | 1.0% | |||
| Agoraphobia | Male=2 | 0.9% | 0.2 | 0.76 |
| Female=0 | 0% |
Table 3.
Relationship of psychiatric comorbidity with occupation
| Psychiatric comorbidity | Number of patients (n) | Percentage | Chi square | P |
|---|---|---|---|---|
| Depressive episode | UE=5 GE=6 BM=18 F=35 Others=2 |
2.5 3.0 9.0 17.0 1.0 |
5.2 | 0.38 |
| Dysthymia | UE=2 GE=2 BM=5 F=10O thers=0 |
0.9 1.0 2.5 5.0 0 |
4.3 | 0.12 |
| Generalized Anxiety Disorder | UE=1 GE=2 BM=5 F=6 Others=0 |
0.3 1.0 2.5 3.0 0 |
3.7 | 0.93 |
| Panic Disorder | UE=0 GE=3 BM=3 F=6 Others=0 |
0 1.5 1.5 3.0 0 |
1.2 | 0.32 |
| Social Phobia | UE=0 GE=2 BM=0 F=3 Others=0 |
0 1.2 1.0 1.5 0 |
0.3 | 0.90 |
| Agoraphobia | UE=0 GE=0 BM=0 F=2 Others=0 |
0 0 0 1.2 0 |
0.2 | 0.76 |
Table 4.
Relationship of psychiatric comorbidity with marital status
| Psychiatric comorbidity | Number of Patients (n) | Percentage | Chi square | P |
|---|---|---|---|---|
| Depressive episode | Single=8 | 4.0% | 3.6 | 0.06 |
| Married=55 | 27.0% | |||
| Divorced=3 | 1.5% | |||
| Dysthymia | Single=0 | 0.0% | 1.6 | 0.34 |
| Married=16 | 7.9% | |||
| Divorced=3 | 1.5% | |||
| Generalized Anxiety Disorder | Single=0 | 0.0% | 2.3 | 0.45 |
| Married=11 | 5.3% | |||
| Divorced=3 | 1.5% | |||
| Panic Disorder | Single=0 | 0.0% | 1.2 | 0.32 |
| Married=6 | 3.2% | |||
| Divorced=6 | 2.8% | |||
| Social Phobia | Single=0 | 0.0% | 0.3 | 0.9 |
| Married=3 | 1.5% | |||
| Divorced=2 | 1.0% | |||
| Agoraphobia | Single=0 | 0.0% | 0.2 | 0.76 |
| Married=2 | 0.9% | |||
| Divorced=0 | 0.0% |
In the present study, the prevalence of psychiatric comorbidity especially depression was higher in patients who suffered from DM for a longer duration (>10 years) compared to other patients (<10 years, Table 5).
Table 5.
Relationship between psychiatric comorbidity and clinical variables
| Psychiatric comorbidity | Number of patients (n) | Percentage | 95% Confidence Interval (CI) |
|---|---|---|---|
| Depressive episode | >10 years (40) | 19.5% | 12-24 |
| <10 years (26) | 13.0% | 10-15 | |
| Dysthymia | >10 years (13) | 6.4% | 4-8 |
| <10 years (6) | 3.0% | 2-4 | |
| Generalized Anxiety Disorder | >10 years (8) | 4.0% | 2-6 |
| <10 years (6) | 2.8% | 2-4 | |
| Panic Disorder | >10 years (8) | 4.0% | 1-3 |
| <10 years (4) | 2.0% | 1-2 | |
| Social Phobia | >10 years (3) | 1.5% | 1-2 |
| <10 years (2) | 1.0% | 1-2 | |
| Agoraphobia | >10 years (2) | 0.9% | 0.2-1 |
| <10 years (0) | 0.01% | 0 |
In the current study, psychiatric comorbidity especially depression was higher in patients having uncontrolled DM (HbA1c > 9) and also who were on insulin along with oral hypoglycemic medications Table 6.
Table 6.
Relationship with HbA1c and type of treatment
| Psychiatric comorbidity | Number of Patients (n) | Percentage | Number of Patients (n) | Percentage |
|---|---|---|---|---|
| Depressive episode | HbA1c >9=44 HbA1c <9=22 |
21.4% 11.0% |
Insulin + Oral hypoglycemic=36 Oral hypoglycaemic only=30 |
17.4% 15.0% |
| Dysthymia | HbA1c >9=12 HbA1c <9=7 |
6.0% 3.4% |
Insulin + Oral hypoglycemic=11 Oral hypoglycaemic only=8 |
5.4% 4.0% |
| Generalized Anxiety Disorder | HbA1c >9=9 HbA1c <9=5 |
3.9% 2.9% |
Insulin + Oral hypoglycemic=10 Oral hypoglycaemic only=4 |
4.6% 2.2% |
| Panic Disorder | HbA1c >9=8 HbA1c <9=4 |
4.0% 2.0% |
Insulin + Oral hypoglycemic=8 Oral hypoglycaemic only=4 |
4.0% 2.0% |
| Social Phobia | HbA1c >9=3 HbA1c <9=2 |
1.5% 1.0% |
Insulin + Oral hypoglycemic=3 Oral hypoglycaemic only=2 |
1.5% 1.0% |
| Agoraphobia | HbA1c >9=2 HbA1c <9=0 |
0.9% 0% |
Insulin + Oral hypoglycemic=2 Oral hypoglycaemic only=0 |
0.9% 0% |
DISCUSSION
The present study was the first of its kind in our state. A total of 320 patients were screened, out of which only 202 were eligible for the study. Mean age of patients in our study was 50.63 ± 09.37 years, which is similar to what has been observed in the prior studies.[17,18] Majority of patients being in age group 40–60 years in several studies including our study can be explained by the fact that T2DM is very common in this age group. Similar to the previous studies from other parts of country, males (52.5%) and females (47.5%) were almost equally distributed.[19] Since majority of patients in our state hail from rural background,[20] our study also showed a similar pattern, 64.4% patients in the present study belonged to the rural background. Most of the patients (76.2%) were matriculate. Only three patients (1.5%) were illiterate. Similar patterns of literacy have been observed in the prior studies.[19,21]
In our study, 63.9% patients were farmers and 5.0% patients were unemployed. Higher prevalence of diabetes in the farmers in our study sample as compared to that seen in previous studies from India[19] may be due the fact that agriculture is the main occupation in our state. In the present study, 95.5% of the patients were married. In various studies from the subcontinent, 78%-92% patients were married which is comparable to the present study.[12,13] Vast majority (80.2%) of the patients in our study lived in joint families which is comparable to other studies, where 60.3% to 73.6% patients lived in joint families. In the state of Himachal Pradesh majority families are still following the culture of joint families. Owing to the low rate of unemployment in our study, most of the patients (72.3%) belonged to middle socioeconomic class (including upper middle and lower middle) as measured by modified Kuppuswamy's Socioeconomic Scale[17] and only 10.9% belonged to lower socioeconomic class. The crude prevalence of the psychiatric comorbidity in T2DM patients was found to be around 58.4%. Most common psychiatric comorbid illness found was depression which was present in 85 patients (41.9%). Out of these, 9.4% patients were diagnosed as cases of dysthymia. Majority of the patients were suffering from mild depression. Second most common psychiatric comorbid illness found was generalized anxiety disorder which was present in (6.8%). Most of the patients had mild degree of anxiety according to the Hamilton Anxiety scale. Panic disorder was present in almost 12 patients (6.0%). Social phobia was present in (2.6%) and agoraphobia was seen in two patients (0.9%). Shoib S, et al.[22] had observed depression in 13.5%, generalized anxiety disorder in 5.5%, panic disorder in 6%, social phobia in 1%, and agoraphobia in 1.5% of their patients. Chaudhry R, et al.[23] observed that overall 84% of the patients with diabetes had comorbid depression. They noted that generalized anxiety disorder was present in 9.5%, panic disorder in 6%, and social phobia in 1% of the patients. Tawfik EA, et al.[24] had observed depression in 30.7%, generalized anxiety disorder in 10.7%, panic disorder in 10%, social phobia in 5.7%, and agoraphobia in 10% of the patients. Prevalence of comorbid depression has varied across studies probably due to different ethnic groups. In the present study, the prevalence of depression was slightly higher in female patients as compared to that in males (23.9% vs 18.0%), respectively. Prevalence of anxiety and panic disorders were almost similar in both the sexes. Social phobia and agoraphobia also had no significant difference in the prevalence in both the sexes. Patients above 50 years of age had higher prevalence (26.3%) of depressive episodes as compared to that of younger patients (15.6%). Although, the patients with broken families were not in higher proportion in our study, most of them (9.0%) were diagnosed to have one or more psychiatric comorbidity with their primary illnesses. This demonstrates that the patients who were divorced or separated were emotionally more vulnerable to have psychiatric illnesses. In this study, the higher prevalence of psychiatric comorbidity was associated with the longer duration of DM in the patients. It was also observed that the patients having higher blood sugar levels or uncontrolled DM (HbA1c > 9) were also having statistically insignificant higher prevalence of depressive episodes (27.4%) in comparison to those having lower blood sugar levels (14.4%). Patients who were on insulin along with oral hypoglycemic medications also exhibited higher prevalence of the psychiatric illnesses (22.8% vs 19.0%).
CONCLUSION
Prevalence of the psychiatric comorbidity in T2DM patients was found to be 58.4% and the most common comorbid psychiatric illness was depression followed by generalized anxiety disorder. Depression was slightly higher in female patients and person aged >50 years. Greater prevalence of depressive episodes was there in people with longer duration of diabetes and uncontrolled diabetes.
Limitations
Due to a relatively small sample size, the findings of this study need to be corroborated with larger sample size studies
A prospective study design needs to be planned to see the better association of psychiatric comorbidities with T2DM.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
All patients who participated in this study.
REFERENCES
- 1.Pouwers A. Diabetes mellitus. In: Kasper DL, Braunwald E, Fauci A, Hauser C, Longo D, Jameson JL, editors. Harrison's Principles of Internal Medicine. New York: McGraw Hill; 2005. p. 2158. [Google Scholar]
- 2.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 3.Balhara YPS. Diabetes and psychiatric disorders. Indian J Endocrinol Metab. 2011;15:274–83. doi: 10.4103/2230-8210.85579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown ES, Varghese FP, McEwan BS. Association of depression with medical illness: Does cortisol play a role? Biol Psychiatry. 2004;55:1–9. doi: 10.1016/s0006-3223(03)00473-6. [DOI] [PubMed] [Google Scholar]
- 5.Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta- analysis. Diabetologia. 2006;49:837–45. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 6.Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: A meta-analysis. Diabetes Care. 2008;31:2383–90. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanz BJ, Rensch-Riemann BS, Fritz-Sigmund DI, Schmidt MH. IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care. 1993;16:1579–87. doi: 10.2337/diacare.16.12.1579. [DOI] [PubMed] [Google Scholar]
- 8.Chaudhry R, Mishra P, Mishra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: A hospital-based study. Ind Psychiatry J. 2010;19:47–9. doi: 10.4103/0972-6748.77637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson N, Fuller JH, Edmeades SP. Depression and Diabetes. Diabet Med. 1988;5:268–74. doi: 10.1111/j.1464-5491.1988.tb00983.x. [DOI] [PubMed] [Google Scholar]
- 10.Geffken G, Ward H, Staab J, Carmichael S, Evans D. Psychiatric morbidity in endocrine disorders. Psychiatric Clin North Am. 1998;21:473–89. doi: 10.1016/s0193-953x(05)70017-4. [DOI] [PubMed] [Google Scholar]
- 11.Robinson DJ, Luthra M, Vallis M, Psych R. Diabetes and Mental Health. [Last accessed on 2017 Oct 21];Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. doi: 10.1016/j.jcjd.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 12.Broadbenta E, Petriea KJ, Maina J, Weinmanb J. The brief illness perception questionnaire. J of Psychosomatic Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organisation. ICD-10 Classification of Mental and Behavioural Disorders: Clinical Description and Diagnostic Guidelines. Geneva: World Health Organisation; 1992. [Google Scholar]
- 14.Hamilton M. A rating scale depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 16.Sheehan D, Janavas J, Harnett-Sheehan K, Sheehan M, Gray C. International Neuropsychiatric Interview, English version 6.0.0. January 1. 2010 [Google Scholar]
- 17.Kumar BPR, Dudala SR, Rao AR. Kuppuswamy's socioeconomic status scale-A revision of economic parameter for 2012. Int J Res Dev Health. 2013;1:2–4. [Google Scholar]
- 18.Taneja N, Adhikary M, Chandramouleeswaan S, Kapoor SK. Prevalence of common mental disorders among patients with diabetes mellitus and hypertension in an urban east Delhi slum – A cross sectional study. Telangana J Psych. 2015;1:27–32. [Google Scholar]
- 19.Singh H, Raju MSVK, Dubey V, Kurrey R, Bansal S, Malik M. A study of sociodemographic clinical and glycaemic control factors associated with co-morbid depression in type 2 diabetes mellitus. Ind Psychiatry J. 2014;23:134–42. doi: 10.4103/0972-6748.151687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahajan K, Negi PC, Merwaha R, Mahajan N, Chauhan V, Asotra S. Gender differences in the management of acute coronary syndrome patients: One year results from HPIAR (HP-India ACS Registry) Int J Cardiol. 2017;248:1–6. doi: 10.1016/j.ijcard.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Amin G, Shah S, Vankar GK. The prevalence and recognition of depression in primary care. Indian J Psych. 1998;40:364–69. [PMC free article] [PubMed] [Google Scholar]
- 22.Stojanović-Tasić M, Grgurević A, Cvetković J, Grgurević U, Trajković G. Association between somatic diseases and symptoms of depression and anxiety among Belgrade University students. Med Glas (Zenica) 2014;11:373–8. [PubMed] [Google Scholar]
- 23.Chaudhry R, Mishra P, Mshra J, Parminder S, Mishra BP. Psychiatric morbidity among diabetic patients: A hospital based study. Ind Psychiatry J. 2010;19:47–9. doi: 10.4103/0972-6748.77637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tawfik EA, Talaat A, Elsayed O, Shahda M, Neamatallah M. Psychiatric morbidity and glycemic control in type 2 non obese diabetic Egyptian patients. Life Sci J. 2013;10:1071–8. [Google Scholar]


