Abstract
Background and Objective:
The aim of this study is to determine the effect of educational program based on the extended theory of reasoned action on self-care behaviours in women with type 2 diabetes in Fasa. This quasi-experimental study was performed on 100 women with type 2 diabetes who referred to diabetes clinics in Fasa.
Materials and Methods:
Samples were randomly divided into experimental and control groups. The data were collected using a questionnaire based on the extended theory of reasoned action and self-care behaviours that were completed by both the control and experimental groups before and 3 months after the educational intervention. Data were analysed by SPSS software version 22, descriptive statistics tests, Chi-square test, independent T-test, and paired T-test.
Results:
The results of the study showed that after the educational intervention, the mean scores of all constructs of the extended theory of reasoned action in the experimental group were significantly increased compared to the control group (P <0.05).
Conclusion:
Also, the educational intervention had a significant effect on the promotion of patient's self-care behaviours in the experimental group and the HbA1c level decreased in the experimental group compared to the control group (P <0.05). In addition, it was found that the extended theory of reasoned action could be a suitable framework for designing educational interventions for promoting self-care behaviours in diabetic patients.
Keywords: Education, self-care behavior, the extended theory of reasoned action, type 2 diabetes
INTRODUCTION
Diabetes is a chronic disease caused by abnormalities in carbohydrate, protein, and fat metabolism.[1] As a silent epidemic of the century, it has become one of the biggest health problems all over the world.[2]
Diabetes is divided into two types: type 1 and type 2. Type 1, which accounts for 5% to 10% of the cases, is caused by insulin deficiency and results in autoimmune damage to the cells-producing pancreatic insulin. Type 2 diabetes, which accounts for 90% to 95% of cases of diabetes, is caused by the inability of muscle cells to respond to insulin (insulin resistance) and insufficient compensatory insulin secretion.[3] According to the statistics, in 2016, there were 422 million diabetic adult patients worldwide[4] estimated to reach 552 million by 2030.[5,6,7] According to the latest statistics released by the Iranian Diabetes Society, 7 million of Iranians (8.9%) have diabetes,[8] and it is estimated that in Iran, the number of diabetic patients will reach 6 million by 2030.[9]
The chronic nature of diabetes increases the likelihood of developing chronic complications, such as ocular, cardiorenal, neurological, and vascular problems during the lifetime of diabetics. This leads to many difficulties for diabetics and a heavy economic burden on the health system of the community.[10]
Regarding the high burden of diabetes, behavioral change and improved metabolic control are major goals in controlling the disease, which largely depends on the patient's self-care behavior,[11] because >95% of the care is bound to patient him/herself.[12]
The International Diabetes Federation recommends that patients take appropriate self-care measures, such as a healthy diet, regular use of medications, regular exercise, and blood glucose monitoring.[13]
Recent studies have shown that diabetes and its complications, including ocular, cardiovascular, and renal can be prevented by healthy diet, regular physical activity, blood glucose control, blood pressure control, and cholesterol control.[14] Furthermore, education can play a key role in establishing healthy behaviors, providing a better understanding of the disease, and can prevent or delay complications.[15] Heshmati et al.[16] suggested that along with care, high precision screening, and early diagnosis of diabetes, education, and promotion of patients' knowledge of the disease and its complications are necessary to prevent complications. Self-care education helps patients to make good decisions about their health.[15] Self-care behaviors education for the patients and family increases patient satisfaction, improves the quality of life, reduces patient anxiety, reduces the incidence of disease complications, increases the patients' participation in health-care programs, and increases the patient's autonomy in daily activities.[17] The effectiveness of health education programs mostly depends on the correct use of theories and patterns used in health education. Therefore, the use of theories and models of behavior change is important for health education professionals.[18]
Based on the previous studies,[19] it seems that the theory of reasoned action can be appropriate for promoting self-care behaviors in diabetic patients. One of the theories that have been used effectively in health education programs is the theory of reasoned action. The theory has four constructs, including attitude toward behavior, subjective norms or social pressure, behavioral intention, and self-efficacy. Attitude toward behavior is the person's positive/negative assessment of behavior that involves two factors of behavioral beliefs and evaluation of behavioral outcomes. Abstract norms or social pressure is based on the belief that people affected by different individuals in the community, such as family members, spouse, friends, and health-care providers, are acting through their influence and support. This construct also includes two factors of normative beliefs and an incentive to obey. Behavioral intention is the person's decision and desire to conduct a particular behavior.[20] Another construct of this theory, which was later added, is the self-efficacy that has been emphasized in various studies on its importance in creating self-care behaviors.[21] According to Bandura's theory, self-efficacy involves the trust and confidence of an individual in his/her ability to do his/her affairs with desirable results.[22] This factor is a valuable tool for health-care providers to enhance the patients' motivation for self-care, and consequently, increase their life expectancy and health behaviors.[23]
Therefore, considering the importance of diabetes and its devastating complications in physical, economic, and social dimensions as well as the role of self-care in the treatment and prevention of complications, this study aims to determine the effectiveness of educational program based on the extended theory of reasoned action on self-care behaviors in women with type 2 diabetes in Fasa.
METHODS
The present study is a controlled semi-experimental study that aims to determine the effect of educational programs on self-care behaviors using the extended theory of reasoned action in women with type 2 diabetes in Fasa.
The research community includes patients with type 2 diabetes who referred to the Diabetes Clinic in Shariati Hospital, Fasa, in 2017–2018. The research samples were randomly selected according to the previous study,[19] as follows:
Number of samples according to the relation:
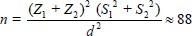
Z1 is the confidence coefficient of 0.95, that is, 1.96
Z2 is the power factor test of 0.80, that is, 0.84
S1 and S2 are the estimates of the standard deviation of knowledge, attitude, and performance scores of up to 16.7 points
d is the least difference in the change of mean score between each of the two groups, which indicate a significant difference of 10 scores. Forty-four cases were obtained in each group (88 in total), which were determined 50 in each group (totaling 100) in the study because of noncooperation or withdrawal of patients.
The criteria for entering the study include reading and writing skills, at least 1 year of diagnosis, age over 30 years, and having no hypertension and mental disorder. In this study, a sample of 170 type 2 diabetic patients who were filed in the diabetes center, were invited to participate in the study program; 35 out of the patients announced their withdrawal from the program. Out of 135 patients, 100 patients were randomly selected and assigned into experimental and control groups (each of 50 patients). The data collection tools in this research include: (a) demographic information questionnaire, including questions about age, level of education, and marital status; (b) to measure the constructs of the theory of reasoned action, we used the questionnaires by Babazadeh et al.[19] and Didarloo et al.,[24] whose validity and reliability had been confirmed. Cronbach's alpha coefficient for attitude toward behavior, abstract norms, behavioral intention, and self-efficacy was 0.88, 0.86, 0.88, and 0.88, respectively. The questionnaire included eight demographic information questions (age, occupation, education, duration of diabetes, marital status, income, background diseases, and family history of diabetes): 12 questions of attitude toward behavior, 12 questions of abstract norms, eight questions of behavioral intention, and 15 questions of self-efficacy. For scoring constructs, based on the Likert scale, five options were used, which varied from score 1 (totally disagree) to score 5 (totally agree); and (c) to measure the self-care behaviors of the patients, 20 questions about physical activity, diet, diabetes drugs, foot and eye care, and self-regulation of blood glucose, and Toobert et al.[25] criterion of summary of the diabetes self-care activities was used, whose validity and reliability had been confirmed. For example, “How many days did you control your blood glucose over the last week?” high average indicated the good performance, and the low average showed the low performance of self-care behaviors, which were reported as percentages. Before the educational intervention, in both experimental and control groups, questionnaires were completed. Then, patients in both groups were referred to unit laboratory (Fatemiyeh Clinic) for hemoglobin A1c (HbA1c) test. Educational intervention was carried out based on the constructs of the theory of reasoned action in the experimental group in the form of ten sessions of lecture (55–60 min), group discussion, practical demonstration, question and answer, and use of educational videos, images, and PowerPoint, which were held at the diabetes center hall.
A session was also held with the presence of the doctor of the diabetes center, staff of the center, and one of the family members as abstract norms. These sessions focused on diabetes, how diabetes affects the eyes and feet, peripheral neuropathy, damage to large and small arteries, various ocular complications, the impact of proper diet and physical activity, drug use, and how to control blood glucose. In the prevention of ocular complications and foot ulcers, the patients were given information and instructions on the importance of exercise in controlling blood glucose, daily care of feet, wearing proper shoes, washing the feet, and the importance of the regular visit to the ophthalmologist.
At the end of the educational sessions, the patients were given a booklet. A WhatsApp group was formed for the exchange of information and a message was sent to them weekly. A monthly follow-up session was also held for them to discuss care-related issues. Three months after the educational intervention, the questionnaire was completed by both the experimental and control groups. Individuals were referred to the laboratory for HbA1c test, and the results were recorded.
Data analysis was performed using SPSS 22 software (IBM Corp, USA). To describe the quantitative and qualitative variables, mean and standard deviation and frequency percentage were used, respectively. Furthermore, the paired t-test was used for the comparison of mean scores of constructs of the extended theory of reasoned action, self-care behaviors, and HbA1c levels in patients before and 3 months after the education in each group; independent t-test was used to compare mean scores of constructs of the extended theory of reasoned action, self-care behaviors, the HbA1c level of patients, and the relative frequency of the two groups.
RESULTS
In Table 1, before intervention, there was no significant difference between the two groups in terms of attitude (P = 0.125), abstract norms (P = 0.292), self-efficacy (P =), behavioral intention (P = 0.26), and self-care behaviors (P = 0.194), but 3 months after the intervention, a significant increase was observed in the experimental group in each of the constructs compared to the control group (P < 0.001) [Table 1]. Paired t-test in the experimental group showed that the mean score of HbA1c decreased significantly 3 months after the intervention (P < 0.001). This test in the control group showed no significant difference between the mean score of HbA1c before and 3 months after the intervention (P < 0.05) [Table 2].
Table 1.
Comparison of the mean score of attitude toward behavior, abstract norms, self-efficacy, and self-care behaviors in the experimental and control group before and 3 months after the intervention
| Variable | Group | Mean±SD | Paired t-test (P) | |
|---|---|---|---|---|
| Before intervention | 3 months after intervention | |||
| Attitude toward behavior | Experimental | 6.68±24.67 | 6.58±69.34 | <0.001 |
| Control | 6.98±25.19 | 6.86±26.90 | 0.228 | |
| Independent t-test | 0.125 | P<0.001 | ||
| Abstract norms | Experimental | 6.53±30.24 | 6.58±67.35 | <0.001 |
| Control | 6.36±32.14 | 6.48±3.393 | 0.132 | |
| Independent t-test | 0.212 | P<0.001 | ||
| Self-efficacy | Experimental | 5.31±33.56 | 5.40±75.96 | <0.001 |
| Control | 5.83±32.85 | 5.10±34.12 | 0.214 | |
| Independent t-test | 0.174 | P<0.001 | ||
| Behavioral intention | Experimental | 27.5±29.94 | 66.5±72.45 | <0.001 |
| Control | 17.5±31.13 | 72.5±32.40 | 0.336 | |
| Independent t-test | 0.26 | P<0.001 | ||
| Self-care behaviors | Experimental | 24.5±26.14 | 12.5±63.39 | <0.001 |
| Control | 58.5±27.19 | 59.5±29.20 | 0.258 | |
| Independent t-test | 0.194 | P<0.001 | ||
SD: Standard deviation
Table 2.
Comparison of mean score of hemoglobin A1c in the experimental and control group before and 3 months after the intervention
| Variable | Group | Mean±SD | Paired t-test (P) | |
|---|---|---|---|---|
| Before intervention | 3 months after intervention | |||
| HbA1c | Experimental | 8.96±1.77 | 7.21±1.26 | <0.001 |
| Control | 8.88±1.85 | 8.83±1.79 | 0.102 | |
| Independent t-test | 0.343 | P<0.001 | ||
SD: Standard deviation; HbA1c: HemoglobinA1c
DISCUSSION
Regarding the comparison of the distribution of the frequency of demographic variables in the two groups, the findings showed that the two groups had the same demographic and background characteristics (age, level of education, and sex), suggesting the homogeneity of the studied groups. The studies by Babazadeh et al.[19] and Shojaeezadeh et al.,[26] consistent with the results of this study, showed that the patient's allocation process was designed, so that both the experimental and control groups were homogeneous in terms of the studied demographic variables. The findings of the study indicated an increase in mean scores of attitude toward self-care behaviors in the experimental group compared to the control group after intervention. This means that when people felt that this behavior led to the positive health outcomes (weight loss, improved fitness, reduced need for diabetes drugs, diabetes control, and improved quality of life), they would adopt and maintain that behavior. These results were supported by the findings of the previous studies regarding the positive attitude toward health behaviors.[27,28]
The results of the study by Didarloo et al.,[24] entitled “Prediction of Self-management Behaviour among Iranian Women with Type 2 Diabetes,” showed a positive significant relationship between attitude and intention to do self-management. It means that the more intense the people's attitude toward the self-care behavior, the more likely their intention to do self-care behaviors. In different studies, the effect of education on the attitude of individuals has been discussed.[29,30,31,32]
Abstract norms or pressures are among the constructs of the theory of reasoned action, which have been proven to be positively correlated with the health behaviors.[33,34] The findings of the present study indicate an increase in the mean score of abstract norms in the experimental group compared to the control group after the intervention. This means that the more pressure from family members, especially spouse, doctors, health caregivers, and friends, to carry out health behaviors by patients, the more health-care behaviors are taken up by the patients. The findings of the studies by Babazadeh et al.,[19] Zendehtalab et al.,[35] and Najimi et al.[36] also suggested the effect of the educational program on important members for patients on improving self-care behaviors. Omondi et al.[34] and Blue[33] also reported that abstract norms have a positive correlation with patients' intention to do self-care behaviors. Therefore, it is suggested that health workers should pay special attention to the important individuals for patients to improve the self-care behaviors in them.
According to the results of this research, the mean score of self-efficacy in the experimental group was increased compared to the control group after the intervention, which was statistically significant. Self-efficacy is one of the components of the lifestyle changes that can improve chronic illness. Individuals with high self-efficacy believe that they can make certain changes to improve their health, while those who have low self-efficacy have little belief in changing their health behavior (limiting the use of salt, physical activity, etc).[37] Along with the present study, Shakibazadeh et al.[13] also emphasized the positive correlation between self-efficacy and self-care in diabetes patients.[38]
High self-efficacy in patients with type 2 diabetes has a positive correlation with diet planning, the implementation of a regular exercise program, and self-care.[39] Findings of the study by Didarloo et al.[24] revealed that self-efficacy was the strongest direct and indirect determinant of physical activity behavior through behavioral intention. The intention to do behavior influenced by self-efficacy, which includes the individual's beliefs in his ability to organize activities, is to successfully carry out the desired behavior to achieve the certain result in a given condition. The more strong these beliefs, the easier the individual does the health behaviors. A study, using constructs of various theories, also shows that the effect of self-efficacy on the desired behavior is stronger than other psychological and social factors.[40] Morovvatisharifabad et al.[41] reported self-efficacy as the most important determinant of self-care behaviors in people with diabetes. Babazadeh et al.[19] also suggested that in designing educational interventions, self-efficacy should be considered as one of the factors influencing self-care behaviors in patients with type 2 diabetes. The results of this study are consistent with the results of Sadeghi et al.,[42] Eftekhar Ardebili et al.,[43] Kim et al.,[44] and Warren-Findlow et al.[45] on increase of self-efficacy by limiting salty foods and increased exercise, and with Park et al.[46] on improvement of self-efficacy in hypertensive patients after intervention.
According to the theory of reasoned action, human behavior is a function of its intention, and the more intense the individual's intention to behavior, the more likely it is to behave; of course, not in the sense that any intention must lead to behavior. In fact, the intention to behavior is a necessary condition but not sufficient, and in this theory, it is considered as the first and strongest construct.[24] The intention to do physical activity behaviors in diabetic patients is influenced by abstract norms, self-efficacy, and their attitude (positive and negative beliefs about behavior and evaluation of behavioral outcomes).[47] Also, since all the constructs of abstract norms, self-efficacy, and attitude were improved in the present study, it was expected that the intention would be improved as well. In the study of Didarloo et al.,[24] there was a positive correlation between intention and physical activity in patients with type 2 diabetes. The findings of the studies by Baum A et al.[48] and Didarloo et al.[24] proved that the individual's intention to perform a particular behavior is the first and best predictor of his/her behavior.
Based on the results of the present study, the mean score of self-care in the experimental group was increased compared to the control group after the intervention, which was statistically significant. This increase in self-care behaviors could be attributed to the patient's participation in the educational sessions that were held for the test group. One of the self-care dimensions studied in this article was dietary observation. The results of Hazavehei et al.[28] and Baghianimoghadam et al.[1] showed that after the intervention, the mean score of behaviors such as walking, exercise, regular use of medications, and the use of a proper diet increased significantly in the intervention group. Furthermore, the studies by Ezadirad et al.,[49] Shojafard et al.,[50] and Jalilian et al.[51] were consistent with the findings of the present study. This findings were also consistent with the results of Oshvandi et al.,[52] Daghio et al.,[53] Babazadeh et al.,[19] and the results of systematic review of Heinrich et al. on the effective role of interventions based on self-care behaviors of patients in nutrition, blood glucose monitoring, patient knowledge and information, and quality of life.[54] These findings suggested that informing patients about the importance of dieting in controlling type 2 diabetes could play an important role in promoting their nutritional behaviors. Health professionals consider physical activity as one of the essential factors for controlling diabetes.[55] One of the self-care dimensions studied in this article was physical activity. The findings of this research indicated that there was a significant difference between the two groups in terms of physical activity after intervention. This means that educational intervention has a significant effect on the improvement of physical activity in patients in the experimental group, which is consistent with the results of studies by Babazadeh et al.[19] and Oshvandi et al.[52]
In the study of Shojaeezadeh et al.,[26] the mean scores of walking performance in the intervention group increased immediately and 3 months later, but no increase was observed in the control group that is consistent with the present study. Park et al. conducted a study aimed at implementing an educational program with exercises in 40 hypertensive patients (18 in the experimental group and 22 in the control group) in Korea. The experimental group received an educational program for 12 weeks based on individual health and self-care behaviors, individual counseling, and appropriate exercise by trained nurses. The results of the study showed that the implementation of an educational program with exercise could be effective in decreasing systolic blood pressure, improving self-efficacy, and quality of life associated with health in people with hypertension.[46]
Jordan reported that 85% of the amputation of lower limbs of diabetic patients could be prevented with proper care. Proper care of diabetic foot, including daily examination of the feet and inside the shoes, daily washing of the feet and its complete drying, avoid walking barefoot, using the shoes that lower the pressure on the sole, avoid cutting the edges of the nails, avoid touching the corns and warts, and referring to the doctor regularly.[56]
One of the self-care dimensions studied in this research was foot care. The findings of this study indicated that there was a significant difference between the two groups regarding foot care after the educational intervention, which was consistent with the results of Shojaeezadeh et al.[26]
In the study of Ghanei et al.,[57] 82% and 76% of diabetic patients performed daily washing and examination of their feet, indicating the desired performance of the studied patients.
According to the results of this study, the mean score of HbA1C in the experimental group was reduced compared to the control group after the intervention, which was statistically significant. The study of Baghianimoghadam et al.[58] in the Yazd diabetes center showed that the mean scores of HbA1C before and after the intervention were 9.84 and 7.28, respectively.
Based on studies, it was estimated that a 1% decrease in hemoglobin glycosylated level is associated with a 35% reduction in the risk of complications of type 2 diabetes[59] and a 20% reduction in the risk of macrovascular complications.[60]
A meta-analysis review study showed that moderate-intensity physical activity can reduce HbA1c up to 6% in people with type 2 diabetes, which reduces the risk of microvascular complications by 22%.[61]
In this regard, Yousefipoor et al.[62] showed that after 8 weeks of physical activity, the level of HbA1c, LDL-c, TG, and fasting blood glucose decreased significantly in the experimental group.[62] In the study of Syrjala on diabetic patients, nutrition education reduced their HbA1c levels.[63] Turner et al.[64] found that the use of therapeutic, diet, and exercise-related activities reduced the amount of HbA1c in patients. All of these studies confirmed the findings of the present study.
CONCLUSION
According to the results of this study, the design and implementation of the educational programs based on the theory of reasoned action play an important role in promoting self-care behaviors in patients with type 2 diabetes. Therefore, it is suggested that health-care providers use this theory in designing and implementing educational programs for diabetic patients at various levels of providing services, including health-care homes, health centers, and diabetes clinics. In the present study, the collection of information through the questionnaire was subject to limitations, because some of the participants may not have provided the correct information. Furthermore, there were problems related to the participation and cooperation of individuals in the study and completion of questionnaires, which were omitted by explaining the objectives of the research plan and confidentiality of the information provided by them. Another limitation of the present study was the impossibility of generalizing the study to the whole society, as samples were selected from individuals referred to the Diabetes Clinic of Shariati Hospital, Fasa, which may well not be representative of the entire community.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Baghianimoghadam M, Afkhami Ardekani M. The effect of educational intervention on quality of life of diabetic patients type 2, referee to diabetic research centre of Yazd. Q Horizon Med Sci. 2008;13:21–8. [Google Scholar]
- 2.Abdoli S, Ashktorab T, Ahmadi F, Parvizy S. Diabetes diagnosis disrupter identity? Iran J Endocrinol Metab. 2011;13:26–35. [Google Scholar]
- 3.Laffel L. Ketone bodies: A review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999;15:412–26. doi: 10.1002/(sici)1520-7560(199911/12)15:6<412::aid-dmrr72>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Diabetes: Global report on diabetes. 2016. [Last accessed on 2016 May 09]. Available from: http://www.who.int/diabetes/global-report/en/
- 5.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 7.Guariguata L. By the numbers: New estimates from the IDF diabetes Atlas update for 2012. Diabetes Res Clin Pract. 2012;98:524–5. doi: 10.1016/j.diabres.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Infectious Disease Society. Diabetes: Global Threat, 2012. Infectious Disease Society. 2012 [Google Scholar]
- 9.World Health Organization. Prevalence of Diabetes in the Eastern Mediterranean Region. Geneva: Diabetes Programme the Institute; 2010. [Google Scholar]
- 10.Antony S. In: Principles of Internal Medicine Harison: Endocrine System Diseases. 1st ed. Zaree SH, Mortazavi M, editors. Tehran: Andishe Rafee; 2009. [Google Scholar]
- 11.Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008;26:77–82. [Google Scholar]
- 12.Noroozi A, Tahmasebi R, Shaybani B. Relationship between personality trait and self-management in diabetic patients referred to Bushehr medical centers in 2012-2013. ISMJ. 2014;16:436–46. [Google Scholar]
- 13.Shakibazadeh E, Rashidian A, Larijani B, Shojaeezadeh D, Forouzanfar MH, Karimi Shahanjarini A. Perceived Barriers and Self-Efficacy: Impact on Self-care Behaviours in Adults with Type 2 Diabetes. Faculty of Nursing and Midwifery. Hayat. 2009;15:69–78. [Google Scholar]
- 14.Shi L, Shu XO, Li H, Cai H, Liu Q, Zheng W, et al. Physical activity, smoking, and alcohol consumption in association with incidence of type 2 diabetes among middle-aged and elderly Chinese men. PLoS One. 2013;8:e77919. doi: 10.1371/journal.pone.0077919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kashfi SM, Jeyhouni AK, Khalili RB, Hatami M. Evaluation of the effects of educating about nutrition and jogging on the blood sugar of type II diabetic patients of a clinic in Shiraz, Iran. Hakim Res J. 2009;12:54–60. [Google Scholar]
- 16.Heshmati HB, Khorasani F, Moghadam Z. Prevalence of chronic complications of diabetes and its related factors in referred type 2 diabetes patients in Freydoonkenar diabetes center. J Neyshabur Univ Med Sci. 2014;1:36–43. [Google Scholar]
- 17.Koshyar H. Nursing Theory and Theorists. 1st edition. Tehran: Andishe Rafi publication; 2009. [Google Scholar]
- 18.Robinson TD. Hypertension Beliefs and Behaviors of African Americans in Seleceted Cleveland Public Housing. Kent State University; 2012 [Google Scholar]
- 19.Babazadeh T, Banaye Jeddi M, Shariat F, Moradil F, Mokammel A. The effect of educational intervention based on the extended theory of reasoned action on self-care behaviors in patients with type 2 diabetes. J Health. 2017;8:256–67. [Google Scholar]
- 20.Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. John Wiley & Sons; 2008. [Google Scholar]
- 21.Mohamadinejad F, Pedram Razi S, Aliasgharpour M, Tabari F, Kazemnejad A. Effect of patient education program on self-efficacy in patients with diabetes. Iran J Nurs Res. 2015;10:35–41. [Google Scholar]
- 22.Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II) Health Promot Pract. 2005;6:148–56. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- 23.Bentsen SB, Wentzel-Larsen T, Henriksen AH, Rokne B, Wahl AK. Self-efficacy as a predictor of improvement in health status and overall quality of life in pulmonary rehabilitation – An exploratory study. Patient Educ Couns. 2010;81:5–13. doi: 10.1016/j.pec.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Didarloo AR, Shojaeizadeh D, Gharaaghaji Asl R, Habibzadeh H, Niknami SH, Pourali R. Prediction of self-management behavior among Iranian women with type 2 diabetes: Application of the theory of reasoned action along with self-efficacy (ETRA) Iran Red Crescent Med J. 2012;14:86–95. [PMC free article] [PubMed] [Google Scholar]
- 25.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 26.Shojaeezadeh D, Tol A, Sharifirad G, Alhani F. Effect of education program based on empowerment model in promoting self-care among type 2 diabetic patients in Isfahan. RJMS. 2013;20:18–31. [Google Scholar]
- 27.Taghdisi M, Borhani M, Solhi M, Afkari M, Hosseini M. Effect of educational program based on PRECED model on quality of life in patients with typeII diabetes. J Gorgan Univ Med Sci. 2011;13:29–36. [Google Scholar]
- 28.Hazavehei SM, Khani JA, Hasanzadeh A, Rashidi M. The effect of educational program based on BASNEF model on diabetic (Type II) eyes care in Kazemi's Clinic, (Shiraz) Iran J Endocrinol Metab. 2008;10:145–54. [Google Scholar]
- 29.Sharifirad G, Rezaeian M, Soltani R, Javaheri S, Mazaheri MA. A survey on the effects of husbands' education of pregnant women on knowledge, attitude, and reducing elective cesarean section. J Educ Health Promot. 2013;2:50. doi: 10.4103/2277-9531.119036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niaki TM, Behmanesh F, Mashmuli F, Azimi H. The effect of prenatal group education on knowledge, attitude and selection of delivery type in primiparous women. Iran J Med Educ. 2010;10:124–30. [Google Scholar]
- 31.Shahraki Sanavi F, Ansari-Moghaddam A, Navabi Rigi S. Two teaching methods to encourage pregnant women for performing normal vaginal delivery. Iran J Med Educ. 2012;12:184–92. [Google Scholar]
- 32.Besharati F, Hazavehei S, Moeini B, Moghimbeigi A. Effect of educational interventions based on theory of planned behavior (TPB) in selecting delivery mode among pregnant women referred to Rasht health centers. J Zanjan Univ Med Sci Health Serv. 2011;19:10. [Google Scholar]
- 33.Blue CL. Does the theory of planned behavior identify diabetes-related cognitions for intention to be physically active and eat a healthy diet? Public Health Nurs. 2007;24:141–50. doi: 10.1111/j.1525-1446.2007.00618.x. [DOI] [PubMed] [Google Scholar]
- 34.Omondi D, Walingo M, Mbagaya G, Othuon L. Understanding physical activity behavior of type 2 diabetics using the theory of planned behavior and structural equation modeling. Int J Hum Soc Sci. 2010;5:160–7. [Google Scholar]
- 35.Zendehtalab H, Vaghei S, Emamimoghadam Z. Effect of intervention based on BASNEF model on quality of life in patients with type 2 diabetes. Evid Based Care. 2013;3:7–16. [Google Scholar]
- 36.Najimi A1, Azadbakht L, Hassanzadeh A, Sharifirad GR. The Effect of Nutritional Education on Metabolic Outcomes Based on BASNEF Model in Elderly Patients with Type 2 Diabetes. J Res Health Sci. 2010;6:549–58. [Google Scholar]
- 37.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 38.Fujiwara Y, Kishida K, Terao M, Takahara M, Matsuhisa M, Funahashi T, et al. Beneficial effects of foot care nursing for people with diabetes mellitus: An uncontrolled before and after intervention study. J Adv Nurs. 2011;67:1952–62. doi: 10.1111/j.1365-2648.2011.05640.x. [DOI] [PubMed] [Google Scholar]
- 39.Boyer BA, Paharia MI, editors. Comprehensive handbook of clinical health psychology. John Wiley & Sons; 2008. [Google Scholar]
- 40.Hanna HH. The Influence of Self-Efficacy and Spirituality on Self-Carebehaviors and Glycemic Control in Older African Americans with Type 2 Diabetes. Barry University School of Nursing; 2006. [Google Scholar]
- 41.Morovvatisharifabad M, Tonekaboni MA. The relationship between perceived benefits/barriers of self-care behaviours and self-management in diabetic patients. Hayat. 2007;13:17–27. [Google Scholar]
- 42.Sadeghi R, Mohseni M, Khanjani N. The effect of an educational intervention according to hygienic belief model in improving care and controlling among patients with hypertension. RafsanjanUniv Med Sci. 2014;13:383–94. [Google Scholar]
- 43.Eftekhar Ardebili H, Moradi H, Mahmoudi M. Effect of educational intervention based on the health belief model in blood pressure control in hypertensive women. J Mazandaran Univ Med Sci. 2014;24:62–71. [Google Scholar]
- 44.Kim KB, Han HR, Huh B, Nguyen T, Lee H, Kim MT, et al. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27:1199–208. doi: 10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37:15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Park YH, Song M, Cho BL, Lim JY, Song W, Kim SH. The effects of an integrated health education and exercise program in community-dwelling older adults with hypertension: A randomized controlled trial. Patient Educ Couns. 2011;82:133–7. doi: 10.1016/j.pec.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 47.Fishbein M, Ajzen I, Flanders NA. Belief, attitude, intention and behaviour: an introduction to theory and research. 1st Edition. Publisher Addison-Wesley: USA; 1975. [Google Scholar]
- 48.Sutton S. Theory of planned behaviour. In: Baum A, Newman S, Weinman J, West R, McManus C, editors. Cambridge handbook of psychology, health and medicine. Cambridge: Cambridge University Press; 1997. [Google Scholar]
- 49.Izadirad H, Masoudi GR, Zareban I, Poor MS, Jadgal K. The Effect of Educational Program Based on BASNEF Model on Women's Blood Pressure with Hypertension. [Last accessed on 2019 Mar 16];Journal of Torbat Heydariyeh University of Medical Sciences. 2013 1:22–31. Available from: http://jms.thums.ac.ir/article-1-40-fa.html . [Google Scholar]
- 50.Shojafard J, Nadrian H, Moghadam MB, Mahmudabad SM, Sanati H, Shahi MA. Effects of an educational program on self-care behaviors and its perceived benefits and barriers in patients with Heart Failure in Tehran. [Last accessed on 2019 Mar 16];payavard. 2009 2:43–55. Available from: http://payavard.tums.ac.ir/article-1-133-en.html . [Google Scholar]
- 51.Jalilian F, Zinat Motlagh F, Solhi M. Effectiveness of education program on increasing self management among patients with type II diabetes. Sci J Ilam Univ Med Sci. 2012;20:26–34. [Google Scholar]
- 52.Oshvandi K, Jokar M, Khatiban M, Keyani J, Yousefzadeh MR, Sultanian AR. The effect of self care education based on teach back method on promotion of self care behaviors in type II diabetic patients: A clinical trial study. Iran J Diabetes Metab. 2014;13:131–43. [Google Scholar]
- 53.Daghio M, Fattori G, Ciardullo A. Use of pictorial advice to promote compliance to diet and drugs among illiterate and migrant patients. J Diabetol. 2010;3:3. [Google Scholar]
- 54.Heinrich E, Schaper NC, de Vries NK. Self-management interventions for type 2 diabetes: A systematic review. Eur Diabetes Nurs. 2010;7:71–6. [Google Scholar]
- 55.Ghazanfari Z, Niknami S, Ghofranipour F, Larijani B. Regular physical activity from perspective of females with diabetes: A qualitative study. Horizon Med Sci. 2009;15:5–14. [Google Scholar]
- 56.Jordan DN, Jordan JL. Foot self-care practices among Filipino American women with type 2 diabetes mellitus. Diabetes Ther. 2011;2:1–8. doi: 10.1007/s13300-010-0016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghanei R, Golkar F, Aminpoor E. Foot care in depressed and non-depressed diabetic patients. Modern Care Journal. 2013;10:124–31. [Google Scholar]
- 58.MH BM. The Study of BASNEF Model Effectiveness in Controlling Yazd Diabetic Patients [Dissertation] Tehran: Tarbiat Modarres Universitys; 2001. [Google Scholar]
- 59.Amini M, Mehr Mohamadi N, Aminoroaya A. Incidence of type 2 diabetes in 25-75 years without diabetes symptom refered to diabetes research center in Isfahan, during 1997-2002. J Zanjan Univ Med Sci Health Serv. 2003;12:33–40. [Google Scholar]
- 60.Sigal RJ, Kenny GP, Boulé NG, Wells GA, Prud'homme D, Fortier M, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: A randomized trial. Ann Intern Med. 2007;147:357–69. doi: 10.7326/0003-4819-147-6-200709180-00005. [DOI] [PubMed] [Google Scholar]
- 61.Nelson KM, Reiber G, Boyko EJ, NHANES III. Diet and exercise among adults with type 2 diabetes: Findings from the third national health and nutrition examination survey (NHANES III) Diabetes Care. 2002;25:1722–8. doi: 10.2337/diacare.25.10.1722. [DOI] [PubMed] [Google Scholar]
- 62.Yousefipoor P, Tadibi V, Behpoor N, Parnow A, Delbari M, Rashidi S. Effects of aerobic exercise on glucose control and cardiovascular risk factor in type 2 diabetes patients. Med J Mashhad Univ Med Sci. 2015;57:976–84. [Google Scholar]
- 63.Syrjälä AM, Niskanen MC, Knuuttila ML. The theory of reasoned action in describing tooth brushing, dental caries and diabetes adherence among diabetic patients. J Clin Periodontol. 2002;29:427–32. doi: 10.1034/j.1600-051x.2002.290507.x. [DOI] [PubMed] [Google Scholar]
- 64.Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: Progressive requirement for multiple therapies (UKPDS 49).UK prospective diabetes study (UKPDS) group. JAMA. 1999;281:2005–12. doi: 10.1001/jama.281.21.2005. [DOI] [PubMed] [Google Scholar]


