Abstract
Objectives. To examine the association between family member incarceration, psychological stress, and subclinical cardiovascular disease (CVD).
Methods. Between 2012 and 2016, 1849 CVD-free women from the Mexican Teachers’ Cohort responded to questions on family incarceration from the Life Stressor Checklist. Perceived stress and hair cortisol levels were measured in a subset of participants. Carotid intima-media thickness was measured, and carotid atherosclerosis was determined in all participants. We used multivariable quantile, linear, and logistic regression models to evaluate the association between family member incarceration, stress, and subclinical CVD.
Results. Among women with a mean age of 49.7 years (SD ±5.2), 15.3% reported family member incarceration. We found that both perceived stress and hair cortisol levels were significantly higher in women with an incarcerated family member relative to women without one. After multivariable adjustment, women who reported family member incarceration had 41% (95% confidence interval = 1.04, 2.00) higher odds of carotid atherosclerosis compared with those who did not.
Conclusions. Family member incarceration was associated with robust markers of stress and cardiovascular risk. Mass incarceration may have a long-lasting impact on physical health of affected families.
Mass incarceration is increasingly recognized as an emerging public health concern that drives health inequalities in the United States.1 The Americas have the highest imprisonment rate in the world (400 incarcerated people per 100 000), with the United States leading globally as a country with more than 2 million incarcerated people.2,3 Relative to other nations, Mexico′s prison population rate (163 incarcerated people per 100 000) is close to the global median.3 However, the prison population has steadily increased over past decades (see Appendix A, available as a supplement to the online version this article at http://www.ajph.org for details). And while recent changes in pretrial detention policies lowered the number of incarcerated individuals (currently at 198 475), this year’s constitutional reforms are likely to result in a new spike in incarceration rates.4
Increasing incarceration in the United States and Mexico has had a disproportionate impact on disadvantaged and marginalized individuals who have measurably been found to have poorer health statuses before, during, and after incarceration.1,5 Incarceration not only affects those incarcerated but may also negatively affect the well-being of their family and community. For example, parental incarceration appears to affect child and adolescent health.6,7 Initial evidence suggests that incarceration may also negatively influence the mental and physical health8–10 of adult family members who provide care for incarcerated people and their families during prison terms. Losing a family member to incarceration may represent a highly stressful life event that may affect cardiovascular health through altered metabolic responses and unhealthy lifestyle behaviors.11,12
Even though social context and prison conditions differ between the United States and Mexico, understanding the health consequences of incarceration on adult family members in Mexico may elucidate health disparities in the United States. We sought to gain insight on the public health impact of mass incarceration by uniquely assessing perceived and biological measures of stress in women living in Mexico and investigating the relation between family member incarceration, stress, and cardiovascular disease (CVD).
METHODS
We conducted a cross-sectional analysis in women from the Mexican Teachers’ Cohort (MTC), a prospective study of 115 314 female teachers living in Mexico that began in 2006 to 2008.13 At baseline and every 3 years, participants responded to questionnaires on lifestyle and health. Between September 2012 and June 2016, a random sample of teachers from 3 states (Chiapas, Yucatán, and Nuevo León) was invited to take part in an ancillary study on CVD. Close to 70% (n = 2390) of those invited chose to participate. Characteristics of attendees and nonattendees were similar (Table A, available as a supplement to the online version of this article at http://www.ajph.org). We excluded women with prevalent myocardial infarction and stroke (n = 13) and those with missing information on family member incarceration (n = 322) and carotid intima-media thickness (IMT; n = 206). The current analysis included 1849 women.
Assessment of Family Member Incarceration
We evaluated stressful life events by using the Life Stressor Checklist–Revised (LSC-R).14 Study participants responded to the LSC-R in a protected, private environment during the clinical evaluation. One of the questions addressed whether the respondent has or ever had a family member incarcerated. Women were asked to provide details on their age when the incarceration started and ended and on “How much do you consider this event to have affected your life in the past year?” (using a 5-point Likert scale from “not at all” to “extremely” affected). We did not assess LSC-R’s validity; however, we previously used the instrument in the MTC to evaluate exposure–disease relations.15
Psychological Stress and Hair Cortisol Levels
Participants responded to the Perceived Stress Scale-10 (PSS-10)16 at the same time as the LSC-R. The PSS-10 attempts to measure “the degree to which life in the past month has been experienced as unpredictable, uncontrollable and overwhelming” (e.g., “in the last month, how often have you felt nervous and stressed?”) on a 5-point response (from 0 = “never” to 4 = “very often”). We obtained a score by following standard practice.16 We found the internal consistency of the score to be high (r = 0.83) in a sample of 1310 MTC participants from Chiapas and Yucatán.
In Nuevo León, (n = 631) participants provided hair samples to measure cortisol levels, a biomarker of exposure to chronic stress.17 Hair was cut as close as possible to the scalp from the posterior vertex by study personnel and stored in aluminum foil. Cortisol concentrations were determined by C. K. at a specialized laboratory from the 3-centimeter proximal hair segment (representing 3-month period before sampling) following a standardized procedure.17 We excluded women with hair cortisol plus or minus 3 SD away from the mean (n = 1) as well as those with an cortisol-to-cortisone ratio of greater than 3, which was considered implausible (n = 15).
Subclinical Cardiovascular Disease
Vascular neurologists used a SonoSite MicroMaxx ultrasound and Asus laptop with M’AthStd Software (Intelligence in Medical Technologies, Paris, France) to measure carotid IMT and to detect atherosclerotic plaques following international guidelines.18 IMT was measured between the lumen–intima and media–adventitia interfaces on the far wall of the common carotid artery, at least 5 millimeters below its end where the carotid bifurcation was visible. Images of a 10-millimeter arterial segment were used to measure the mean IMT for each common carotid artery from which the overall mean was calculated. When neurologists were unable to obtain an adequate image, they repeated this procedure on the near wall. Structures protruding into the arterial lumen by 0.5 millimeters or more or 50% of the surrounding IMT or IMT greater than 1.5 millimeters were considered plaque. We assessed the reproducibility of IMT measurement (n = 147) and found it to be high—r = 0.89 (95% confidence interval [CI] = 0.84, 0.93) for Chiapas and r = 0.92 (95% CI = 0.86, 0.96) for Yucatán.
Covariates
The 2008 (baseline) MTC questionnaire included information on indigenous background (participant or her parents spoke an indigenous language), education (last completed degree), main health care provider used for important medical conditions, marital status, and smoking. We created a socioeconomic status score based on responses to owning 7 key household items.19 We updated self-reported covariates by using the 2011 MTC questionnaire whenever possible. At study sites, standardized study personnel measured weight with an electronic digital scale (Tanita Corp, Arlington Heights, IL) to the nearest 0.1 kilogram and height with a wall stadiometer (Seca Corp, Hamburg, Germany) to the nearest millimeter. We calculated body mass index (BMI) as the weight in kilograms over height in meters squared. For diabetes, hypertension, and hypercholesterolemia, we used self-reported diagnosis and treatment from questionnaires and updated this information from interviews at the clinical site.
We also used clinical information obtained at study sites for diagnosis. Blood pressure measurements were collected automatically by placing the cuffs on 4 extremities (VaSera VS-1000, Fukuda Denshi, Tokyo, Japan), and fasting blood samples (25 mL) were drawn through venipuncture and processed within 30 minutes. Women with a systolic blood pressure of 140 millimeters of mercury or higher or diastolic pressure of 90 millimeters of mercury or higher were considered hypertensive. Plasma concentrations of glucose, total cholesterol, triglycerides, and high-density lipoprotein cholesterol were measured at the clinical laboratory in each site with standard assays. Women were classified as having diabetes when the fasting plasma glucose levels were 126 milligrams per deciliter or higher. We used fasting plasma total cholesterol of 240 milligrams per deciliter or higher or low-density lipoprotein cholesterol of 160 milligrams per deciliter or higher to determine if the participant had hypercholesterolemia. We used 5 violence-related questions from the LSC-R (physical or observed violence) to assess exposure to a violent environment.
Statistical Analysis
We categorized participant exposure as having or ever having an incarcerated family member and classified exposed women according to the duration of the family member’s incarceration in 2 categories based on the median duration of incarceration in this population (≤ 1 or > 1 year; we imputed missing values to the median; n = 14). We categorized participants’ experience of family incarceration according to perceived effect on daily life in low or high severity (< 3 or ≥ 3 points) based on the median Likert scale responses.
We used directed acyclic graphs20 (Figures A and B, available as supplements to the online version of this article at http://www.ajph.org) to articulate our research questions and guide our analytical strategies (i.e., variable selection to adjust for confounding, mediation analyses). First, we compared PSS-10 scores in women with and without a history of family member incarceration. We used age-, site-, and multivariable-adjusted linear regression models to assess the adjusted mean difference in PSS-10 scores and 95% CIs. We included age (continuous), health care provider (public, private, or other), indigenous background, education (high school, bachelors, or masters), marital status (single, together, or divorced or widowed), socioeconomic status score (tertiles), and exposure to violence. We selected variables used to adjust for confounding based on risk factors for cardiovascular disease, previous stress–CVD literature,21 and proposed frameworks for studying stress and disease in human populations.22
Second, we evaluated hair cortisol levels according to family member incarceration exposure. Hair cortisol residuals were not normally distributed even after log-transformation (P < .001 for the Shapiro–Wilk test). Thus, we fit age- and multivariable-adjusted quantile regression models to determine the adjusted median difference and 95% CIs in hair cortisol levels.
Finally, we compared log-transformed IMT values23 and carotid atherosclerosis (mean left or right IMT ≥ 0.8 mm or plaque) in women with and without family member incarceration. We estimated percentage differences in mean IMT by using age-, site-, and multivariable-adjusted linear regression models and odds ratios (ORs) for carotid atherosclerosis by using similarly adjusted logistic regression models.
We explored effect measure modification by including a cross-product term of family incarceration and median age (< 49 or ≥ 49 years), state of residence, and ethnicity as the effect on CVD may vary depending on these factors. We compared models with and without the cross-product term by using a likelihood ratio test. Perceived stress, cortisol levels, smoking, BMI, diabetes, hypertension, and hypercholesterolemia may mediate the impact of family member incarceration on cardiovascular health (Figure A).11 For carotid atherosclerosis, we used the counterfactual approach to conduct a mediation analysis24 to estimate the natural direct and indirect effects for each potential mediator independently and calculated the proportion mediated for those suggesting significant effects. We repeated analyses in which smoking, BMI, diabetes, hypertension, and hypercholesterolemia were included in the model to adjust for confounding (Figure B). We performed post hoc analyses exploring results of women classified according to recentness of exposure (current or less-recent incarceration). All statistical tests were 2-sided using a P value of less than .05, and we performed analyses with SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
The mean age of study participants was 49.7 years (SD ±5.2) and median age was 49 years (interquartile range = 46–53 years). The prevalence of family member incarceration was 15.3% (n = 283). Of exposed women, 65.8% reported that their family member was either currently or recently (< 1 year) incarcerated, and 40.0% perceived that the event had a severe effect on their life. Women with an incarcerated family member were more often indigenous, divorced, and had a lower socioeconomic status than women without one. Exposed women were also more likely to smoke, be obese, and have diabetes, and were more frequently exposed to violence relative to their unexposed counterparts (Table 1).
TABLE 1—
Distribution of Study Covariates Among 1849 Mexican Women According to Family Member Incarceration: Mexico, 2012–2016
| Incarceration of a Family Member |
||
| Yes (n = 283), Mean ±SD or No. (%) | No (n = 1566), Mean ±SD or No. (%) | |
| Age, y | 49.5 ±4.8 | 49.7 ±5.2 |
| Study sites | ||
| Chiapas | 104 (36.8) | 538 (34.4) |
| Yucatán | 97 (34.3) | 395 (25.2) |
| Nuevo León | 82 (29.0) | 633 (40.4) |
| Indigenous | 48 (17.0) | 211 (13.5) |
| Graduate education | 51 (18.0) | 270 (17.2) |
| Private health care provider | 54 (19.1) | 293 (18.7) |
| High socioeconomic status | 131 (46.3) | 816 (52.1) |
| Divorced, separated, or widowed | 52 (18.4) | 218 (14.0) |
| Violent environment | 134 (47.4) | 535 (34.2) |
| Potential mediatorsa | ||
| Current smokers | 26 (9.2) | 102 (6.5) |
| Obesity | 114 (40.3) | 581 (37.1) |
| Diabetes | 27 (9.5) | 111 (7.1) |
| Hypertension | 63 (22.3) | 341 (21.8) |
| Hypercholesterolemia | 89 (31.5) | 509 (32.5) |
| Perceived stress, PSS-10 scoreb | 14.4 ±5.9 | 12.8 ±5.9 |
Note. PSS-10 = Perceived Stress Scale 10.
These variables serve as potential mediators in the association between family member incarceration and cardiovascular disease.
PSS-10 was only available for 1690 participants from this population.
Table B (available as a supplement to the online version of this article at http://www.ajph.org) compares study participants with those excluded from the analysis because of missing information. We observed slight differences in characteristics between groups (except women with missing data were less likely to be from Nuevo León). We observed a difference in women with and without hair cortisol that is likely driven by location (hair cortisol was measured only in Nuevo León; Table C, available as a supplement to the online version of this article at http://www.ajph.org). This subgroup had a higher educational level and socioeconomic status (and only a few were indigenous) and were more likely to be obese and more frequently exposed to violence.
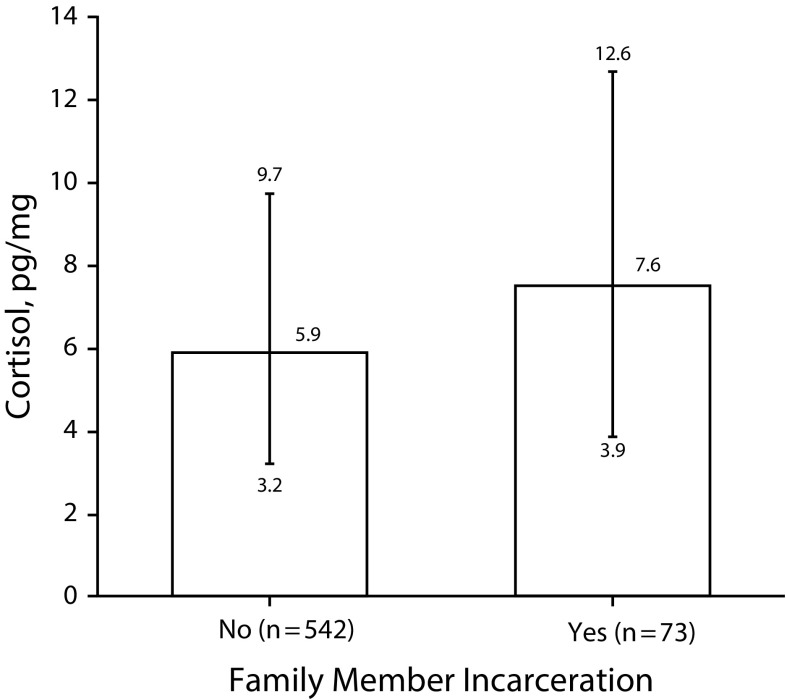
The subgroup for whom PSS-10 was available did not differ from the full study population (Table D, available as a supplement to the online version of this article at http://www.ajph.org). Among the 1690 (91.4%) women who completed the PSS-10, the mean score for those with family member incarceration was 15.6 (SD ±6.0) whereas the corresponding score for women without one was 12.5 (SD ±5.8). After multivariable adjustment, we found a statistically significant difference in mean PSS-10 scores comparing exposed and unexposed women (1.4; 95% CI = 0.6, 2.1; Table 2). We observed a suggestion that the difference may be slightly stronger in women who reported a shorter duration of incarceration and those who reported a high versus low effect on their daily life. Among the 615 women with valid cortisol levels, those with an incarcerated family member had significantly higher median cortisol levels than women without one (Figure 1). The multivariable-adjusted median difference was 1.40 picograms per milligram (95% CI = 0.30, 2.50).
TABLE 2—
Adjusted Difference in Perceived Stress Scores According to Family Member Incarceration Among 1690 Women: Mexico, 2012–2016
| No. | Age-and-Site–Adjusted Difference (95% CI) | Multivariable Differencea (95% CI) | |
| Family incarceration | |||
| No | 1431 | 0 (Ref) | 0 (Ref) |
| Yes | 259 | 1.5 (0.8, 2.3) | 1.4 (0.6, 2.1) |
| Duration of incarceration | |||
| No incarceration | 1431 | 0 (Ref) | 0 (Ref) |
| ≤ 1 y | 180 | 1.7 (0.8, 2.4) | 1.6 (0.7, 2.5) |
| > 1 y | 79 | 1.2 (–0.1, 2.5) | 1.0 (–0.3, 2.3) |
| Effect on daily life | |||
| No incarceration | 1431 | 0 (Ref) | 0 (Ref) |
| Low severity | 155 | 1.4 (0.4, 2.3) | 1.3 (0.3, 2.2) |
| High severity | 104 | 1.8 (0.6, 2.9) | 1.6 (0.4, 2.7) |
Note. CI = confidence interval.
Multivariable analysis refers to adjusting for age, site (Chiapas, Yucatán, or Nuevo León), health care provider (public, private, or other), indigenous background (yes or no), education (high school, bachelors, or masters), marital status (single, together, or divorced or widowed), socioeconomic status (low, middle, or high), and violence (yes or no).
FIGURE 1—
Median and Interquartile Ranges of Cortisol Levels According to Family Member Incarceration: Mexico, 2012–2016
Note. Wilcoxon 2-sample difference in median test P = .017.
We observed no association between family member incarceration and mean IMT (% difference = 0.6; 95% CI = −1.0, 2.2; Table 3). However, women who reported exposure to family member incarceration had 41% higher odds of carotid atherosclerosis relative to those who did not (multivariable-adjusted OR = 1.41; 95% CI = 1.04, 2.00). The magnitude of the association appeared to be higher for women with a longer duration of family member incarceration. In a post hoc analysis, differences in PSS-10 appeared to be lower but IMT percent differences higher in women with a currently incarcerated family member compared with women without family member incarceration (Table E, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 3—
Adjusted Percentage Differences of Mean Intima-Media Thickness and Odds Ratios for Carotid Atherosclerosis According to Family Member Incarceration: Mexico, 2012–2016
| Difference of Mean IMT, % (95% CI) |
ORs for Carotid Atherosclerosis (95% CI) |
|||||
| No. | Age-and-Site–Adjusted Difference | Multivariable Differencea | No. Cases/Noncases | Age-and-Site–Adjusted Difference | Multivariable Differencea | |
| Family member incarceration | ||||||
| No | 1566 | 0 (Ref) | 0 (Ref) | 325/1241 | 1 (Ref) | 1 (Ref) |
| Yes | 283 | 1.2 (−0.4, 2.8) | 0.6 (−1.0, 2.2) | 80/203 | 1.54 (1.14, 2.08) | 1.41 (1.04, 2.00) |
| Duration of incarceration | ||||||
| No incarceration | 1566 | 0 (Ref) | 0 (Ref) | 325/1241 | 1 (Ref) | 1 (Ref) |
| ≤ 1 y | 191 | 1.0 (−0.9, 2.9) | 0.4 (−1.5, 2.3) | 51/140 | 1.42 (1.00, 2.03) | 1.24 (0.89, 1.86) |
| > 1 y | 92 | 1.6 (−1.0, 4.2) | 1.0 (−1.6, 3.7) | 29/63 | 1.82 (1.13, 2.92) | 1.68 (1.03, 2.74) |
| Effect on daily life | ||||||
| No incarceration | 1566 | 0 (Ref) | 0 (Ref) | 325/1241 | 1 (Ref) | 1 (Ref) |
| Low severity | 171 | 0.3 (−1.7, 2.3) | −0.2 (−2.1, 1.8) | 46/125 | 1.50 (1.02, 2.16) | 1.38 (0.94, 2.29) |
| High severity | 112 | 2.6 (0.2, 5.0) | 1.8 (−0.6, 4.2) | 34/78 | 1.63 (1.05, 2.53) | 1.46 (0.94, 2.02) |
Note. CI = confidence interval; IMT = intima-media thickness; OR = odds ratio.
Multivariable analysis refers to adjusting for age, site (Chiapas, Yucatán, or Nuevo León), health care provider (public, private, or other), indigenous background (yes or no), education level (high school, bachelors, or masters), marital status (single, together, or divorced or widowed), socioeconomic status (low, middle, or high), and violence (yes or no).
The impact of family incarceration on carotid atherosclerosis appeared to differ across states and ethnicity, but tests for heterogeneity were not statistically significant (Table F, available as a supplement to the online version of this article at http://www.ajph.org). The OR for carotid atherosclerosis in Chiapas was 1.64 (95% CI = 0.98, 2.73) while the corresponding estimate in Nuevo León was 1.13 (95% CI = 0.64, 2.00; P value for interaction = 0.58). Similarly, the association appeared to be stronger in indigenous (OR = 1.96; 95% CI = 0.86, 4.50) relative to nonindigenous women (OR = 1.32; 95% CI = 0.94, 1.84; P value for interaction = 0.17).
We performed an additional sensitivity analysis adjusting for CVD risk factors that may be intermediates: smoking, BMI, diabetes, hypertension, and hypercholesterolemia. The adjusted median difference for cortisol was minimally affected and remained significantly different (1.48 pg/mg; 95% CI = 0.22, 2.74) and our results for perceived stress did not change (Table G, available as a supplement to the online version of this article at http://www.ajph.org). However, controlling for CVD risk factors slightly attenuated the association between family member incarceration, IMT, and carotid atherosclerosis (Table H, available as a supplement to the online version of this article at http://www.ajph.org).
We considered potential confounders of the exposure–outcome or mediator–outcome association in the mediation analysis, and we included exposure–mediator interaction for perceived stress based on the literature22 and because it meaningfully changed the estimate for the natural indirect effect. Our results suggested that both perceived stress and BMI might mediate the association between family incarceration and carotid atherosclerosis (Table I, available as a supplement to the online version of this article at http://www.ajph.org). The proportion mediated by perceived stress was 21.3% (95% CI = –2.2, 25.8) and that for BMI was 18.8% (95% CI = 0.00, 19.3). We explored the mediating effect of cortisol levels in women with available measurements but chose not to report results because of imprecision attributable to a small sample size.
DISCUSSION
In this sample of Mexican women, family member incarceration was significantly associated with perceived stress scores, hair cortisol, and subclinical carotid atherosclerosis (even after adjustment for factors that may be intermediates). Participants who reported family member incarceration had characteristics that may reflect unhealthy behaviors. Our results indicate that the association between family member incarceration and CVD may in part be mediated by stress and unhealthy lifestyle choices.
Chronic stressors result in an abnormal activation of the hypothalamic–pituitary–adrenal axis and the autonomic nervous system.12,22 The release of cortisol and catecholamines from the adrenal glands increases heart rate and blood pressure and, when sustained, this activation may result in inflammation, atherosclerosis, and CVD.25,26 Physiological reactions are often combined with coping mechanisms such as smoking, unhealthy diets, lack of physical activity, and weight gain which may further negatively affect cardiovascular health.25 Our results are consistent with emerging literature on the physiological, behavioral, and long-term effects of stressful experiences on cardiovascular health.27–29
Incarceration is recognized as a highly stressful event for families.30 Previous research into the family consequences of incarceration has often focused on financial and nonphysical health outcomes and on the health of children of incarcerated parents.1,6 Our study makes an important contribution to the limited literature on the cardiovascular health impact of incarceration on adult family members. Only 2 previous studies have documented that family member incarceration was associated with self-reported cardiovascular disease.9,10
We explored different aspects of the family member incarceration including duration, recentness, and the incarceration’s impact on current life with perceived stress and CVD. For stress, estimates were slightly higher among women with a family member who was incarcerated for 1 year or less versus more than 1 year. By contrast, the association between family incarceration and carotid atherosclerosis appeared to be stronger among women reporting a longer duration of incarceration. These results were unexpected. We hypothesized that longer duration of family member incarceration would be more strongly associated with perceived stress and CVD.31 However, the stress score only captured stress levels over the past month so there may be some variability over time, whereas atherosclerosis reflects a slower progressive process.
In a post hoc exploration of the impact of less-recent versus current incarceration, we found slightly higher stress scores in women reporting less-recent incarceration and no differences in the odds of carotid atherosclerosis. The associations did not differ according to the impact of incarceration on daily life. Duration, recentness, and the incarceration’s impact on current life are distinct aspects of stressful experiences that are often correlated. We were limited by sample size in our ability to evaluate these aspects independently. We observed much higher odds of carotid atherosclerosis in indigenous relative to nonindigenous women and a suggestion of heterogeneity across states (with a stronger association in states with more indigenous women). These findings may represent differences in the experience of incarceration attributable to discrimination or prison conditions.32
Strengths and Limitations
Our study has important strengths, including its population-based design, the use of a valid measure of psychological stress, and a novel, reliable biomarker for stress, in addition to our high-quality standardized assessment of subclinical CVD and our mediation analyses.
However, several limitations must be considered. First, in this cross-sectional study we cannot exclude reverse causation. Poor health and stress may affect the recall of details regarding the incarceration (e.g., duration). However, it is unlikely that these factors resulted in overreporting of incarceration.
Second, underreporting of family incarceration because of stigma is possible. Interestingly, the prevalence of family member incarceration in our study population was almost 2 times what was observed in a similar study in the United States (15% vs 8%).9 The incorrect classification of individuals according to carotid atherosclerosis is unlikely to differ because women were unaware of outcome measures. If this had occurred, this misclassification would have resulted in an underestimation of the strength of the association.
Third, like any observational study, the concern that cardiovascular risk factors associated with family incarceration may explain the association cannot be eliminated. In our main analyses, we adjusted for several sociodemographic characteristics and uniquely included exposure to violence. However, there is a possibility that lifestyle and proximal cardiovascular risk factors (e.g., obesity) may be associated with family member incarceration through an unmeasured variable (Figure B, available as a supplement to the online version of this article at http://www.ajph.org). We evaluated the impact of considering lifestyle and proximal risk factors for CVD confounders and our conclusions remained the same.
Fourth, hair cortisol was available only in women from Nuevo León. The impact of family incarceration on stress may differ across states. It is possible that the magnitude of the family incarceration–hair cortisol association may be even stronger in the states that did not have hair cortisol levels as was suggested by our analysis on carotid atherosclerosis.
Fifth, the instrument used to assess family member incarceration did not capture important details. For example, we cannot differentiate which family member was incarcerated or understand imprisonment conditions.
Sixth, our mediation results should be interpreted with caution because they rely on strong assumptions that are difficult to test.24
Finally, our results may not be generalizable to men. Women generally shoulder most of the burden of care for incarcerated people and may be more vulnerable than men to the consequences of family incarceration.
Public Health Implications
Mass incarceration may have a long-lasting impact on physical health of affected families and may play a role in health disparities. This study in Mexico provides unique evidence on the potential role of stress–disease pathways in the cardiovascular consequences of mass incarceration on families. Even though the United States and Mexican prison systems differ, extortion of incarcerated people, lack of resources, and poor living conditions of incarcerated people are common in both contexts.1,33 These 2 contexts likely present similarities in the stress of caretaking for incarcerated people while handling the consequences of their incarceration.
Elucidating family member incarceration-related stress and specific physiological pathways (e.g., inflammation, endothelial function) that link this experience to CVD will require long-term longitudinal studies with repeated biomarker measurements and clinical cardiovascular outcomes (e.g., myocardial infarction). Future studies should also seek to capture important details to make distinctions on which family member was incarcerated (e.g., sibling), nature of the crime (violent vs nonviolent), type of incarceration (e.g., pretrial), and length of sentencing. Also, evaluating emotional distress, loss of income, and financial burden as well as stigma may provide opportunities for interventions to lower the burden of incarceration on families. Addressing stress-related symptoms could mitigate their cardiovascular impact.31 While enhancing perception of social support and reducing negative thinking on single mothers has shown to reduce or improve stress management,34 developing effective family-focused interventions to lower stress on caregivers of children with incarcerated parents is necessary.35 Beyond reevaluating incarceration policies contributing to mass incarceration and ensuring adequate living conditions for incarcerated people, primary care providers in affected communities need to address family member incarceration in clinical practice.
ACKNOWLEDGMENTS
This work was supported by CONACyT (SALUD 161786 and FOINS 214145), an investigator–initiated unrestricted grant from AstraZeneca (ISSNPCV0022), and an institutional grant support by Tecnológico de Monterrey, Escuela de Medicina y Ciencias de la Salud. D. Stern and M. Lajous were partially supported by the Bernard Lown Scholars in Cardiovascular Health Program at the Harvard T. H. Chan School of Public Health.
We thank all study participants for their time and continued support of the Mexican Teachers’ Cohort. We thank the leadership at the office for Regulation at Carrera Magisterial (now Servicio Profesional Docente) in Mexico’s Ministry of Education as well as state coordinators in Chiapas, Yucatán, and Nuevo León for their support in contacting Mexican Teachers’ Cohort participants and assisting with operations during the clinical visits. We would like to acknowledge the commitment to the study by Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado’s Prevention and Health Protection area within the Medical Sub-Directorate by providing technical and logistical support in data collection and hosting clinical visits in their facilities in Chiapas and Yucatán. For clinical data collection in Nuevo León, we thank Tecnologico de Monterrey’s Escuela de Medicina y Ciencias de la Salud and Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado de Nuevo León for hosting our research team.
CONFLICTS OF INTEREST
R. Lopez-Ridaura and M. Lajous have received limited salary support from an institutional grant provided by The Bloomberg Family Foundation. The other authors have nothing to declare.
HUMAN PARTICIPANT PROTECTION
All study participants provided informed consent. The study was approved by institutional review boards at the Instituto Nacional de Salud Pública (National Institute of Public Health) and Tecnologico de Monterrey, Escuela de Medicina y Ciencias de la Salud.
REFERENCES
- 1.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389(10077):1464–1474. doi: 10.1016/S0140-6736(17)30259-3. [DOI] [PubMed] [Google Scholar]
- 2.Coyle A, Fair H, Jacobson J, Walmsley R. Imprisonment Worldwide: The Current Situation and an Alternative Future. Bristol, England: Policy Press; 2016. [Google Scholar]
- 3.International Centre for Prison Studies. World Prison Brief. Available at: https://www.prisonstudies.org/highest-to-lowest/prison_population_rate?field_region_taxonomy_tid=All. Accessed November 25, 2019.
- 4.Office of the High Commissioner for Human Rights. UN rights experts urge Mexico to drop automatic pre-trial detention. 2018. Available at: https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=24010&LangID=E. Accessed November 25, 2019.
- 5.Silverman-Retana O, Lopez-Ridaura R, Servan-Mori E, Bautista-Arredondo S, Bertozzi SM. Cross-sectional association between length of incarceration and selected risk factors for non-communicable chronic diseases in two male prisons of Mexico City. PLoS One. 2015;10(9):e0138063. doi: 10.1371/journal.pone.0138063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wildeman C, Goldman AW, Turney K. Parental incarceration and child health in the United States. Epidemiol Rev. 2018;40(1):146–156. doi: 10.1093/epirev/mxx013. [DOI] [PubMed] [Google Scholar]
- 7.Lee RD, Fang X, Luo F. The impact of parental incarceration on the physical and mental health of young adults. Pediatrics. 2013;131(4):e1188–e1195. doi: 10.1542/peds.2012-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wildeman CS, Turney JK. Despair by association? The mental health of mothers with children by recently incarcerated fathers. Am Sociol Rev. 2012;77(2):216–243. [Google Scholar]
- 9.Lee H, Wildeman C, Wang EA, Matusko N, Jackson JS. A heavy burden: the cardiovascular health consequences of having a family member incarcerated. Am J Public Health. 2014;104(3):421–427. doi: 10.2105/AJPH.2013.301504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeHart D, Shapiro C, Hardin JW. The impact of incarceration on families: a single-jurisdiction pilot study using triangulated administrative data & qualitative interviews. Washington, DC: Office of Justice Programs’ National Criminal Justice Reference Service; 2017.
- 11.Edmondson D, von Kanel R. Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry. 2017;4(4):320–329. doi: 10.1016/S2215-0366(16)30377-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McEwen BS. Allostasis and the epigenetics of brain and body health over the life course: the brain on stress. JAMA Psychiatry. 2017;74(6):551–552. doi: 10.1001/jamapsychiatry.2017.0270. [DOI] [PubMed] [Google Scholar]
- 13.Lajous M, Ortiz-Panozo E, Monge A et al. Cohort profile: The Mexican Teachers’ Cohort (MTC) Int J Epidemiol. 2017;46(2):e10. doi: 10.1093/ije/dyv123. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe J, Kimerling R, Brown PJ, Chrestman KR, Levin K. Psychometric review of the life stressor checklist–revised. In: Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press; 1996. pp. 198–201. [Google Scholar]
- 15.Flores‐Torres MH, Lynch R, Lopez‐Ridaura R et al. Exposure to violence and carotid artery intima‐media thickness in Mexican women. J Am Heart Assoc. 2017;6(8):e006249. doi: 10.1161/JAHA.117.006249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 17.Stalder T, Steudte S, Miller R, Skoluda N, Dettenborn L, Kirschbaum C. Intraindividual stability of hair cortisol concentrations. Psychoneuroendocrinology. 2012;37(5):602–610. doi: 10.1016/j.psyneuen.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Touboul P-J, Hennerici M, Meairs S et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011) Cerebrovasc Dis. 2012;34(4):290–296. doi: 10.1159/000343145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirko KA, Lajous M, Ortiz-Panozo E et al. Socioeconomic position and markers of adiposity among female teachers in Mexico. J Epidemiol Community Health. 2017;71(10):999–1004. doi: 10.1136/jech-2017-209179. [DOI] [PubMed] [Google Scholar]
- 20.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48. [PubMed] [Google Scholar]
- 21.Rosengren A, Hawken S, Ôunpuu S et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 22.Epel ES, Crosswell AD, Mayer SE et al. More than a feeling: a unified view of stress measurement for population science. Front Neuroendocrinol. 2018;49:146–169. doi: 10.1016/j.yfrne.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleinbaum DG, Kupper LL, Nizam A, Rosenberg ES. Applied regression analysis and other multivariable methods. Boston, MA: Cengage Learning; 2013.
- 24.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150. doi: 10.1037/a0031034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 27.Gallo LC, Roesch SC, Fortmann AL et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Psychosom Med. 2014;76(6):468–475. doi: 10.1097/PSY.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sumner JA, Chen Q, Roberts AL et al. Posttraumatic stress disorder onset and inflammatory and endothelial function biomarkers in women. Brain Behav Immun. 2018;69:203–209. doi: 10.1016/j.bbi.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sumner JA, Kubzansky LD, Elkind MS et al. Trauma exposure and posttraumatic stress disorder symptoms predict onset of cardiovascular events in women. Circulation. 2015;132(4):251–259. doi: 10.1161/CIRCULATIONAHA.114.014492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chui WH. Incarceration and family stress as understood through the family process theory: evidence from Hong Kong. Front Psychol. 2016;7:881. doi: 10.3389/fpsyg.2016.00881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gilsanz P, Winning A, Koenen KC et al. Post-traumatic stress disorder symptom duration and remission in relation to cardiovascular disease risk among a large cohort of women. Psychol Med. 2017;47(8):1370–1378. doi: 10.1017/S0033291716003378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prison Insider. Prisons in Mexico. 2015. Available at: https://www.prison-insider.com/countryprofile/prisonsofmexico#. Accessed November 25, 2019.
- 33.Comisión de Derechos Humanos del Distrito Federal. Special report on the situation of the detention centers of the Federal District [in Spanish] 2005. Available at: https://piensadh.cdhdf.org.mx/index.php/informe-especial-2/informe-especial-sobre-la-situacion-de-los-centros-de-reclusion-del-distrito-federal. Accessed November 25, 2019.
- 34.Taylor ZE, Conger RD. Promoting strengths and resilience in single-mother families. Child Dev. 2017;88(2):350–358. doi: 10.1111/cdev.12741. [DOI] [PubMed] [Google Scholar]
- 35.Miller AL, Perryman J, Markovitz L, Franzen S, Cochran S, Brown S. Strengthening incarcerated families: evaluating a pilot program for children of incarcerated parents and their caregivers. Fam Relat. 2013;62(4):584–596. doi: 10.1111/fare.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]