Abstract
Background
Obesity and atrial fibrillation (AF) frequently coexist and independently increase mortality. We sought to assess the association between obesity and adverse events in patients receiving oral anticoagulants for AF.
Methods and Results
Consecutive AF outpatients receiving anticoagulant agents (both vitamin K antagonists and direct oral anticoagulants) were recruited into the FANTASIIA (Atrial fibrillation: influence of the level and type of anticoagulation on the incidence of ischemic and hemorrhagic stroke) registry. This observational, multicenter, and prospective registry of AF patients analyzes the quality of anticoagulation, incidence of events, and differences between oral anticoagulant therapies. We analyzed baseline patient characteristics according to body mass index, normal: <25 kg/m2, overweight: 25–30 kg/m2, and obese: ≥30 kg/m2), assessing all‐cause mortality, stroke, major bleeding and major adverse cardiovascular events (a composite of ischemic stroke, myocardial infarction, and total mortality) at 3 years’ follow‐up. In this secondary prespecified substudy, the association of weight on prognosis was evaluated. We recruited 1956 patients (56% men, mean age 73.8±9.4 years): 358 (18.3%) had normal body mass index, 871 (44.5%) were overweight, and 727 (37.2%) were obese. Obese patients were younger (P<0.01) and had more comorbidities. Mean time in the therapeutic range was similar across body mass index categories (P=0.42). After a median follow‐up of 1070 days, 255 patients died (13%), 45 had a stroke (2.3%), 146 a major bleeding episode (7.5%) and 168 a major adverse cardiovascular event (8.6%). Event rates were similar between groups for total mortality (P=0.29), stroke (P=0.90), major bleeding (P=0.31), and major adverse cardiovascular events (P=0.24). On multivariate Cox analysis, body mass index was not independently associated with all‐cause mortality, cardiovascular mortality, stroke, major bleeding, or major adverse cardiovascular events.
Conclusions
In this prospective cohort of patients anticoagulated for AF, obesity was highly prevalent and was associated with more comorbidities, but not with poor prognosis.
Keywords: atrial fibrillation, mortality, obesity, prognosis, risk factors
Subject Categories: Atrial Fibrillation, Cardiovascular Disease, Epidemiology, Obesity, Risk Factors
Clinical Perspective
What Is New?
Obesity is not associated with prognosis in patients anticoagulated for atrial fibrillation.
What Are the Clinical Implications?
While obesity is one of the main risk factors we target to prevent and treat cardiovascular disease, in the setting of atrial fibrillation obese patients show similar incidence of mortality and nonfatal adverse clinical outcomes.
Introduction
Obesity and atrial fibrillation (AF) are increasing in epidemic proportions worldwide, and both increase the incidence of cardiovascular events.1, 2 AF has long been recognized as a risk factor for stroke, and its association with all‐cause mortality is also widely acknowledged.3 While obesity significantly increases the risk of many metabolic and cardiovascular diseases,1, 2, 3 it is also associated with a lower incidence of events once the cardiovascular disease has been established, as has been proven with conditions such as diabetes mellitus, chronic kidney disease, stroke, dementia, coronary artery disease, and heart failure.4, 5, 6, 7, 8 This phenomenon is known as the “obesity paradox.”
Obesity has been related to the incidence and progression of AF,9, 10 but its effect on prognosis in AF patients is controversial.11 Two subanalyses from randomized clinical trials have shown lower rates of adverse events in patients with higher body mass index (BMI), the AFFIRM (Atrial Fibrillation Follow‐Up Investigation of Rhythm Management)12 and ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trials,13 but this observation has not been confirmed in observational registries with real‐world data.14 Some authors have proposed that obese patients may have a more favorable prognosis because of better anticoagulation control or to a more complete pharmacological treatment compared with nonobese patients, but results have not been consistent among different studies.12, 14
We sought to assess the role of obesity and BMI on prognosis in real‐world patients receiving oral anticoagulants for AF.
Methods
The FANTASIIA (Spanish acronym for “Atrial fibrillation: influence of the level and type of anticoagulation on the incidence of ischemic and hemorrhagic stroke”) registry design is described in detail elsewhere.15 In brief, this is an observational, prospective, national, and multicenter study of clinical and demographic characteristics of Spanish patients with AF. Its main objective is to assess the incidence of thromboembolic and bleeding events in an unselected population of patients with AF, assessing the type of oral anticoagulant (ie, vitamin K antagonists (VKA) or direct oral anticoagulants) used, and the quality of anticoagulation with VKA. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Population
Between June 2013 and March 2014, outpatients with confirmed diagnosis of paroxysmal, persistent, or permanent AF were prospectively enrolled. All patients included had been receiving oral anticoagulation for at least 6 months at the time of recruitment. By design, each investigator included 16 patients taking VKA and 4 patients who were taking direct oral anticoagulants. Eighty investigators, working in 50 outpatient clinics, performed the study. Exclusion criteria were as follows: patients with valvular heart disease (rheumatic valve disease, moderate–severe valve disease, and prosthesis or valve repair surgery), age younger than 18 years, or with recent hospital admission. The study aimed to assess the influence of the anticoagulant treatment in prognosis; thus, patients admitted or with an admission in the prior 3 months were excluded. All patients provided signed informed consent.
The study complied with the ethical principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. It was approved by the Spanish Agency of Medicine and Health Products as a prospective follow‐up postauthorization study (approval number SEC‐ACO‐2012–01) and by the Ethics Committee of the Hospital Universitario San Juan de Alicante.
Study Variables and Data Collection
Clinical and demographic data for all AF patients were collected in a detailed medical history. We defined previous heart disease as the composite of coronary artery disease, heart failure, and other structural cardiomyopathies (such as hypertrophic cardiomyopathy, chronic pericardial disease, or congenital diseases). Coagulation status was determined by the international normalized ratio values at 6 months before study entry and at 1 year of follow‐up. The estimated time spent in the therapeutic range was assessed by the Rosendaal method. Stroke risk was calculated using the CHADS2 and CHA2DS2‐VASc scores,16, 17 bleeding risk using the HAS‐BLED score,18 and comorbidity according to the Charlson index. Serum creatinine levels were collected at baseline and the estimated glomerular filtration rate was calculated using the Cockcroft‐Gault formula: ([140–age] ×[weight in kg]×[0.85 if female]/[72×creatinine]). Obesity was assessed at baseline by means of BMI and stratified as normal weight (<25 kg/m2), overweight (25 to <30 kg/m2), and obese (≥30 kg/m2).
At 3 years, we assessed incidence of stroke, major bleeding, all‐cause mortality, cardiovascular mortality, and major adverse cardiovascular events (MACE, defined as the composite of ischemic stroke, myocardial infarction, and cardiovascular and all‐cause mortality). Thromboembolic events were defined as stroke or transient ischemic attack and peripheral artery embolism. All strokes were evaluated by computed tomography or magnetic resonance imaging according to the neurologist's criteria. Bleeding events were assessed according to the 2005 International Society of Thrombosis and Haemostasis criteria.19 All‐cause and cardiovascular mortality were also recorded. Death was classified as cardiovascular when caused by acute coronary syndrome, heart failure, lethal arrhythmia or sudden death, artery aneurysm rupture, or stroke. An external event assignment committee evaluated all adverse events.
Statistical Analyses
The Kolmogorov‐Smirnov method was used to test the normality of continuous variables, which were reported as mean±SD or median (interquartile range), as appropriate. Categorical variables were expressed as relative frequencies (%). We used the ANOVA test to compare continuous variables across BMI categories and the post hoc Tukey test to assess intergroup differences. Qualitative variables were compared using the χ2 test. Cox regression analyses were used to test the associations between BMI and mortality, bleeding, and cardiovascular events. The independent effect of clinical variables on adverse clinical outcomes was calculated using a Cox proportional hazards regression; the multivariate model included variables yielding a P<0.15 on univariable analysis. The models included BMI, age, sex, hypertension, dyslipidemia, diabetes mellitus, coronary artery disease, heart failure, aortic or peripheral artery disease, chronic kidney disease, Charlson index, history of stroke, and CHA2DS2‐VASc and HAS‐BLED scores. Differences in event‐free survival were examined with the log‐rank test, and Kaplan‐Meier curves were drafted accordingly. To test nonlinear association between the continuous variable BMI and the events, analyses of restricted cubic splines were performed by generating restricted cubic splines for 4 knots and adjusting the Cox multivariate model for each event, including splines as covariates. P<0.05 were considered statistically significant. All statistical analyses were performed with Stata version 12 (Stata Corporation, College Station, TX).
Results
The final study sample comprised 1956 patients (56% men, mean age 73.8±9.4 years). Table 1 shows the baseline characteristics of the study population. BMI was in the normal range in 358 (18.3%) patients, while 871 (44.5%) patients were overweight and 727 (37.2%) were obese. Obese patients were significantly younger and showed a higher prevalence of comorbidities such as hypertension, diabetes mellitus, previous heart failure, and pulmonary disease compared with normal weight and overweight patients.
Table 1.
Baseline Characteristics Stratified by BMI
| All Patients | Normal Weight (BMI<25 kg/m2) | Overweight (BMI 25–30 kg/m2) | Obese (BMI≥30 kg/m2) | P Value | |
|---|---|---|---|---|---|
| N | 1956 | 358 | 871 | 727 | |
| Demographic data | |||||
| Age (y, mean±SD) | 73.8±9.4 | 75.3±9.5 | 74.5±9.5 | 72.1±9.2 | <0.01 |
| Women, % | 44.0 | 46.7 | 40.6 | 46.6 | 0.03 |
| Comorbidities and cardiovascular risk factors | |||||
| Arterial hypertension, % | 80.4 | 69.8 | 79.7 | 86.5 | <0.01 |
| Dyslipidemia, % | 52.2 | 48.6 | 51.8 | 54.5 | 0.18 |
| Diabetes mellitus, % | 29.4 | 24.3 | 25.5 | 36.5 | <0.01 |
| Smoking habit, % | 5.1 | 5.6 | 3.9 | 6.2 | 0.10 |
| CODP/OSAS, % | 17.5 | 14.5 | 13.9 | 23.4 | <0.01 |
| Chronic kidney failure, % | 19.3 | 22.6 | 19.5 | 17.3 | 0.11 |
| Liver dysfunction, % | 1.2 | 1.1 | 1.2 | 1.4 | 0.90 |
| Cancer | 8.6 | 9.8 | 8.2 | 8.5 | 0.65 |
| Aortic or peripheral artery disease | 6.0 | 6.7 | 6.4 | 5.2 | 0.51 |
| History of stroke | 17.0 | 20.7 | 17.6 | 14.4 | 0.03 |
| History of systemic embolism | 2.2 | 1.1 | 1.5 | 3.6 | <0.01 |
| Thyroid dysfunction | 11.1 | 12.0 | 11.7 | 10.0 | 0.49 |
| Alcohol abuse | 3.7 | 3.9 | 2.3 | 5.2 | <0.01 |
| Charlson index | 1.14±1.16 | 1.16±1.20 | 1.04±1.14 | 1.26±1.15 | <0.01 |
| Previous cardiac disease | |||||
| AF, % | 100 | 100 | 100 | 100 | |
| Cardiac disease, % | 48.0 | 44.1 | 45.6 | 52.7 | <0.01 |
| Heart failure, % | 28.9 | 28.2 | 25.8 | 32.9 | <0.01 |
| Coronary artery diseases, % | 18.2 | 16.2 | 19.4 | 17.7 | 0.39 |
| Acute coronary syndrome, % | 13.8 | 12.6 | 14.6 | 13.5 | 0.62 |
| Coronary revascularization, % | 11.5 | 10.9 | 12.2 | 10.9 | 0.67 |
| Coronary stent, % | 9.4 | 6.9 | 10.5 | 9.4 | 0.17 |
| Dilated cardiomyopathy or LVEF <45% (%) | 11.7 | 13.1 | 10.6 | 12.2 | 0.37 |
| Hypertrophic cardiomyopathy, % | 2.6 | 2.8 | 2.9 | 2.2 | 0.68 |
| Congenital heart disease, % | 0.6 | 1.1 | 0.2 | 0.8 | 0.13 |
| Aortic valve disease, % | 3.2 | 6.2 | 2.4 | 2.8 | <0.01 |
| Left ventricular hypertrophy, % | 15.6 | 10.3 | 15.6 | 18.3 | <0.01 |
| Atrial flutter, % | 4.4 | 5.6 | 3.8 | 4.5 | 0.37 |
| Sinus node dysfunction, % | 2.6 | 3.1 | 2.8 | 2.1 | 0.54 |
| Pacemaker | 6.5 | 7.8 | 6.9 | 5.4 | 0.25 |
| Bleeding episodes in the last 6 mo | |||||
| Major bleeding episodes, % | 4.1 | 5.6 | 4.1 | 3.3 | 0.20 |
| Bleeding requiring transfusion (% within bleedings) | 32.5 | 35.0 | 38.9 | 20.8 | 0.33 |
| Bleeding requiring surgery (% within bleedings) | 8.8 | 10.0 | 5.6 | 12.5 | 0.63 |
| Type of AF | |||||
| Paroxysmal, % | 29.1 | 32.7 | 31.0 | 25.2 | 0.14 |
| Persistent, % | 16.8 | 16.8 | 15.9 | 17.7 | |
| Longstanding persistent, % | 4.7 | 4.2 | 4.4 | 5.2 | |
| Permanent, % | 49.4 | 46.4 | 48.7 | 51.9 | |
| Previous electrical cardioversion, % | 18.1 | 14.3 | 17.3 | 20.9 | 0.02 |
| Previous pharmacological cardioversion, % | 21.8 | 21.8 | 20.8 | 22.9 | 0.57 |
| Previous AF ablation, % | 4.3 | 4.5 | 4.6 | 3.9 | 0.76 |
| Control strategy in the baseline visit | 0.79 | ||||
| Rhythm control, % | 38.2 | 39.7 | 37.6 | 38.2 | |
| Rate control, % | 61.8 | 60.3 | 62.5 | 61.8 | |
| CHADS2 (mean±SD) | 2.25±1.24 | 2.23±1.34 | 2.22±1.21 | 2.31±1.24 | 0.37 |
| CHA2DS2‐VASc (mean±SD) | 3.71±1.59 | 3.73±1.64 | 3.67±1.53 | 3.74±1.62 | 0.79 |
| HAS‐BLED (mean±SD) | 2.01±1.05 | 2.03±1.10 | 1.98±1.02 | 2.02±1.05 | 0.72 |
| Physical examination | |||||
| Systolic blood pressure (mm Hg, mean±SD) | 132.1±18.5 | 127.1±17.4 | 132.5±17.7 | 134.2±19.5 | <0.01 |
| Diastolic blood pressure (mm Hg, mean±SD) | 75.9±11.5 | 72.2±11.0 | 75.8±11.1 | 77.97±11.7 | <0.01 |
| Heart rate (bpm, mean±SD) | 72.7±15.1 | 71.8±16.0 | 71.8±14.2 | 74.1±15.5 | <0.01 |
| Weight (kg, mean±SD) | 78.5±14.4 | 63.4±8.8 | 75.0±8.4 | 90.2±13.1 | <0.01 |
| Height (cm, mean±SD) | 164.5±8.9 | 164.7±9.0 | 165.4±8.5 | 163.3±9.1 | <0.01 |
| BMI (kg/m2, mean±SD) | 28.9±4.9 | 23.0±2.6 | 27.4±1.4 | 33.8±3.7 | <0.01 |
| Complementary examinations | |||||
| Rhythm at baseline | 0.05 | ||||
| Sinus, % | 33.0 | 35.8 | 35.3 | 29.0 | |
| AF, % | 60.6 | 57.3 | 57.9 | 65.5 | |
| Pacemaker, % | 5.7 | 5.9 | 6.2 | 4.9 | |
| Other, % | 0.7 | 1.1 | 0.6 | 0.6 | |
| LVEF (%, mean±SD) | 58.6±11.4 | 57.8±12.3 | 59.1±11.2 | 58.3±11.1 | 0.09 |
| Left ventricular hypertrophy, % | 40.0 | 33.0 | 38.1 | 45.7 | <0.01 |
| Hemoglobin (g/dL, mean±SD) | 13.7±1.7 | 13.4±1.7 | 13.7±1.7 | 13.7±1.8 | <0.01 |
| Serum creatinine (mg/dL, mean±SD) | 1.1±0.5 | 1.1±0.8 | 1.0±0.4 | 1.0±0.4 | 0.05 |
| Glomerular filtration rate (mL/min per 1.73 m2, mean±SD) | 66.2±22.9 | 60.9±20.3 | 64.5±20.7 | 70.8±25.8 | <0.01 |
| Total cholesterol (mg/dL, mean±SD) | 177.1±38.6 | 179.8±40.8 | 177.2±36.5 | 175.6±39.9 | 0.10 |
| Glucose (mg/dL, mean±SD) | 108.6±31.6 | 103.2±27.8 | 106.3±29.5 | 114.1±34.8 | <0.01 |
| HBA1C (%, mean±SD) | 6.2±1.3 | 5.9±1.2 | 6.2±1.1 | 6.3±1.6 | <0.01 |
AF indicates atrial fibrillation; BMI, body mass index; bpm, beats per minute; COPD, chronic obstructive pulmonary disorder; HBA1C, hemoglobin A1c; LVEF, left ventricular ejection fraction; OSAS, obstructive sleep apnea syndrome.
Pharmacological Treatment
There were significant differences in most cardiovascular medications (Table 2), but not in the quality of anticoagulation control with VKA according to BMI. Mean time in the therapeutic range was similar across BMI categories (normal weight: 61.1% versus overweight: 62.5% versus obese: 63.1%; P=0.42). No significant differences were found in the percentage of VKA patients achieving <65% or 70% of their time in the therapeutic range (Table S1).
Table 2.
Pharmacological Treatment at Baseline Stratified by BMI
| Normal Weight (BMI<25 kg/m2) | Overweight (BMI 25–30 kg/m2) | Obese (BMI≥30 kg/m2) | P Value | |
|---|---|---|---|---|
| N | 358 | 871 | 727 | |
| Diuretics, % | 48.9 | 54.9 | 64.5 | <0.01 |
| Aldosterone antagonists, % | 16.2 | 11.3 | 16.1 | <0.01 |
| ACE inhibitors, % | 26.8 | 31.7 | 31.8 | 0.19 |
| Angiotensin receptor blockers, % | 32.4 | 39.5 | 46.2 | <0.01 |
| Statins, % | 46.1 | 55.6 | 58.7 | <0.01 |
| Antiplatelets, % | 9.5 | 11.6 | 9.9 | 0.42 |
| β‐Blockers, % | 55.9 | 58.1 | 65.2 | <0.01 |
| Digoxin, % | 20.9 | 16.9 | 18.3 | 0.24 |
| Antiarrhythmic drugs, % | 25.4 | 25.7 | 22.9 | 0.42 |
ACE indicates angiotensin‐converting enzyme; BMI, body mass index.
Events During Follow‐Up
After a median of 1070 (interquartile range 750–1110) days of follow‐up, 255 (13.04%) patients had died, including 107 (5.47%) from cardiovascular causes. Forty‐five (2.30%) patients had suffered a stroke, 48 (2.45%) a systemic embolism, 146 (7.46%) a major bleeding episode, and 168 (8.59%) a MACE. Annual event rates were similar across BMI groups for total mortality (normal weight: 4.84% versus overweight: 4.55% versus obese: 3.85%; P=0.29), cardiovascular mortality (normal weight: 1.51% versus overweight: 2.18% versus obese: 1.63%; P=0.26), stroke (normal weight: 0.85% versus overweight: 0.74% versus obese: 0.79% P=0.90), systemic embolism (normal weight: 0.85% versus overweight: 0.84% versus obese: 0.79%; P=0.96), major bleeding (normal weight: 2.18% versus overweight: 2.91% versus obese: 2.24%; P=0.31), and MACE (normal weight: 2.27% versus overweight: 3.27% versus obese: 2.79%; P=0.24) (Table 3 and Figure 1).
Table 3.
Events During Follow‐Up, Stratified by BMI
| Normal Weight (BMI<25 kg/m2) N=358 | Overweight (BMI 25–30 kg/m2) N=871 | Obese (BMI≥30 kg/m2) N=727 | P Value | ||||
|---|---|---|---|---|---|---|---|
| n | Annual Rate (%/year) | n | Annual Rate (%/year) | n | Annual Rate (%/year) | ||
| All‐cause mortality | 52 | (4.84) | 119 | (4.55) | 84 | (3.85) | 0.29 |
| Cardiovascular mortality | 16 | (1.51) | 56 | (2.18) | 35 | (1.63) | 0.26 |
| Stroke | 9 | (0.85) | 19 | (0.74) | 17 | (0.79) | 0.90 |
| Systemic embolism | 9 | (0.85) | 22 | (0.84) | 17 | (0.79) | 0.96 |
| Major bleeding | 23 | (2.18) | 75 | (2.91) | 48 | (2.24) | 0.22 |
| MACE | 24 | (2.27) | 84 | (3.27) | 60 | (2.79) | 0.24 |
BMI indicates body mass index; MACE, major adverse cardiovascular event (composite of ischemic stroke, myocardial infarction, and cardiovascular and total mortality).
Figure 1.
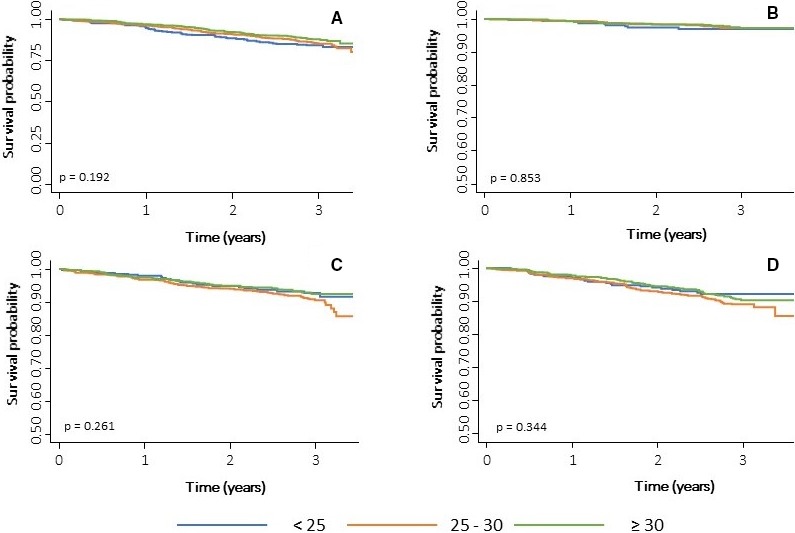
Kaplan–Meier survival estimates. A, Mortality, (B) stroke, (C) major bleeding, and (D) MACE (composite of ischemic stroke, myocardial infarction, and cardiovascular and total mortality). MACE indicates major adverse cardiovascular events.
On univariable analysis, obesity was not statistically related to all‐cause mortality (odds ratio [OR] 1.24, 95% CI 0.94–1.64; P=0.14, cardiovascular mortality OR 1.23, 95% CI 0.81–1.86; P=0.33), stroke (OR 0.97, 95% CI 0.53–1.79; P=0.93), systemic embolism (OR 1.08, 95% CI 0.59–1.97; P=0.80), major bleeding (OR 1.23, 95% CI 0.86–1.75; P=0.27), or MACE (OR 1.07, 95% CI 0.77–1.49; P=0.68) (Table S2).
Subgroup Analyses
The event rates were analyzed in prespecified subgroups. We did not find significant differences between sexes or age groups. Event rates for death or MACE are shown in Table S2. Only 7 patients in our population were underweight (BMI<18.5 kg/m2), precluding further analyses in this category (Table S3).
Multivariate Analysis
In the multivariate Cox analysis performed to adjust for confounding variables, BMI was not independently associated with all‐cause mortality, cardiovascular mortality, stroke, major bleeding, or MACE (Table 4). The restricted cubic splines analyses showed nonlinear relationship between BMI and events (Figure 2).
Table 4.
Multivariate Cox regression
| HR | 95% CI | P Value | ||
|---|---|---|---|---|
| Total mortality | ||||
| BMI (reference <30 kg/m2) | 0.94 | 0.71 | 1.25 | 0.69 |
| Age, per y | 1.09 | 1.07 | 1.11 | <0.01 |
| Heart failure | 1.72 | 1.26 | 2.36 | <0.01 |
| Charlson index | 1.33 | 1.15 | 1.54 | <0.01 |
| CHA2DS2‐VASc | 0.81 | 0.69 | 0.95 | 0.01 |
| HAS‐BLED | 1.34 | 1.16 | 1.55 | <0.01 |
| Stroke | ||||
| BMI (reference <30 kg/m2) | 1.17 | 0.62 | 2.22 | 0.63 |
| Cerebrovascular disease | 2.54 | 1.10 | 5.88 | 0.03 |
| Major bleeding | ||||
| BMI (reference <30 kg/m2) | 0.88 | 0.61 | 1.28 | 0.51 |
| Dyslipidemia | 0.57 | 0.41 | 0.81 | 0.01 |
| Chronic kidney failure | 1.50 | 1.01 | 2.23 | 0.04 |
| HAS‐BLED | 1.29 | 1.08 | 1.55 | <0.01 |
| MACE | ||||
| BMI (reference <30 kg/m2) | 1.00 | 0.72 | 1.41 | 0.98 |
| Age, per y | 1.06 | 1.03 | 1.09 | <0.01 |
| Coronary artery disease | 1.99 | 1.26 | 3.13 | <0.01 |
| Heart failure | 2.01 | 1.27 | 3.16 | <0.01 |
| HAS‐BLED | 1.21 | 1.01 | 1.44 | 0.04 |
Model adjustment: The models included BMI, age, sex, hypertension, dyslipidemia, diabetes mellitus, coronary artery disease, heart failure, aortic or peripheral artery disease, chronic kidney disease, Charlson index, history of stroke, CHA2DS2‐VASc and HAS‐BLED scores. BMI indicates body mass index; HR, hazard ratio; MACE, major adverse cardiovascular event (composite of ischemic stroke, myocardial infarction, and cardiovascular and total mortality).
Figure 2.
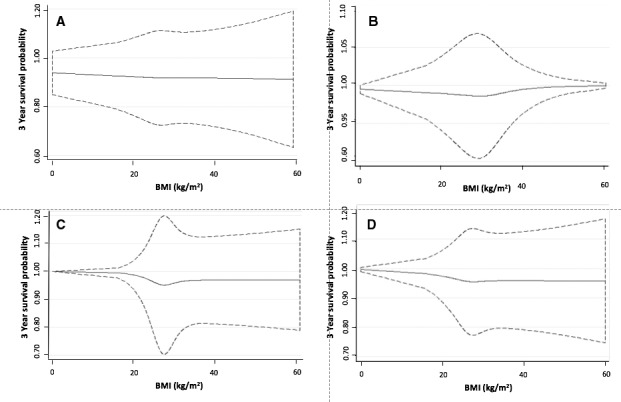
Association between BMI and the estimated 3‐year survival probability including BMI as a continuous variable using restricted cubic splines with 3 degrees of freedom. The dotted lines represent the 95% CI. (A) Mortality, (B) stroke, (C) major bleeding, and (D) MACE (composite of ischemic stroke, myocardial infarction, and cardiovascular and total mortality). The models were adjusted by age, sex, hypertension, diabetes mellitus, dyslipidemia, coronary artery disease, heart failure, aortic artery disease, chronic kidney disease, Charlson index, previous stroke, CHA 2 DS 2‐VASc, and HAS‐BLED. BMI indicates body mass index; MACE, major adverse cardiovascular events.
An additional model including only BMI and age was performed in order to further study the effect of age in the relationship between BMI and events (Figure 3).
Figure 3.
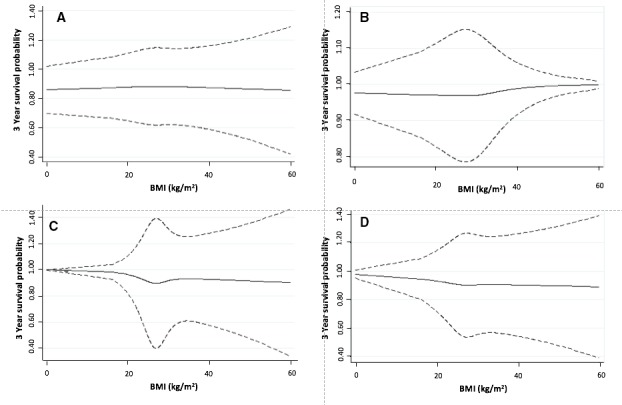
Association between BMI and the estimated 3‐year survival probability including BMI as a continuous variable using restricted cubic splines with 3 degrees of freedom. The dotted lines represent the 95% CI. A, Mortality, (B) stroke, (C) major bleeding, and (D) MACE (composite of ischemic stroke, myocardial infarction, and cardiovascular and total mortality). The models were adjusted by age. BMI indicates body mass index; MACE, major adverse cardiovascular events.
Discussion
In a real‐world cohort of patients receiving oral anticoagulant therapy for AF, half of the patients were overweight and a third were obese. Despite the higher prevalence of cardiovascular risk factors in overweight and obese patients, there were no significant differences in adverse events between normal and obese patients. Moreover, higher BMI was not independently associated with a higher risk of mortality or adverse outcomes in multivariate analysis.
Whether obesity is a protective factor or has no effect is a matter of debate. In 2 substudies of the ARISTOTLE trial, overweight and obesity were associated with lower risk of all‐cause mortality, cardiovascular mortality, and stroke even after adjusting for biomarkers of cardiac and renal dysfunction and inflammatory activity.13, 20 A large meta‐analysis and systematic review evaluated the relationship between BMI and clinical outcomes in AF patients, finding that the risk of stroke, death, and cardiovascular death were lower in overweight and obese patients compared with patients with a normal BMI,21 but other studies, such as the EORP‐AF (EURObservational Research Programme‐Atrial Fibrillation),22 did not find significant differences.
Studies including clinical trial data show reduced events among obese patients (the so‐called “obesity paradox”), while most observational registries report similar event rates between obese and normal weight patients, suggesting that comorbidities have an important role in determining outcomes.22 Proietti et al23 performed a systematic review studying the relationship between overweight or obesity and cardiovascular prognosis and observed an obesity paradox for adverse events only in clinical trials cohorts, whereas observational studies fail to show this relationship, in accordance with our results in the FANTASIIA registry. Indeed, in our study, the Charlson index was significantly higher among obese patients, and in the multivariate analyses it was an independent predictor of mortality, while obesity did not show significant association. While clinical trials are considered to provide the highest grade of evidence, observational registries are better suited for studying broader populations without strict inclusion criteria, obtaining information more representative of real‐life daily clinical practice.
Obesity has been shown to be an independent risk factor for thromboembolic events in the general population with no AF,14, 24 but the relationship between stroke and BMI in patients with AF is debated. Indeed, scores to predict stroke do not include BMI, and the 2 variables (stroke and obesity) are not associated in observational studies.17, 25 Our results corroborate these observations. Although most studies in patients with AF show neutral or protective effects for higher BMI, overweight and obesity were associated with a worse prognosis in the Danish Diet, Cancer, and Health study of incident AF, a prospective nationwide study.26 The protection conferred by obesity seems more evident in patients with established cardiovascular disease, and the selection of patients with incident AF could result in a lower‐risk population. In fact, in heart failure—the paradigm of advanced cardiac disease—the obesity paradox is more pronounced.27
The risk of bleeding has scarcely been studied. Our results suggest that obesity does not modify bleeding risk in patients anticoagulated for AF, and other studies have shown only that underweight could be associated with increased bleeding risk,25, 28 but not overweight or obesity. Again, obesity is not included in any bleeding risk score: neither HAS‐BLED nor ATRIA, HAEMORR2HAGES, or ORBIT include weight among the variables that predict bleeding episodes.29
Age is one of the strongest predictors of mortality. In our study, mean age decreased as BMI increased, and this finding is consistent with other studies.13, 20, 30 In the subanalysis including only age and BMI, BMI still did not show a significant relationship with events in the follow‐up.
The higher risk of developing a cardiovascular disease caused by obesity is probably not as strong as the effect of cachexia worsening prognosis in any chronic disease. We speculate that obesity increases the probability of developing cardiovascular diseases, but it also helps patients survive their complications. Underweight patients have an increased mortality risk21, 31 and are more prone to have diseases as a result of poor nutritional status, whereas obesity confers metabolic reserves that may help to cope with heart disease. Our results support this hypothesis. Figure 2 shows that rather than a decrease of risk for obesity, there is an increase of risk for BMI values <25.
Finally, obese patients may have better tolerance for cardiovascular drugs with proven prognostic benefits. In our study, obese patients received a significantly higher proportion of renin‐angiotensin system blockers, diuretics, statins, and β‐blockers. This finding is consistent with previous reports and could explain, at least in part, the good prognosis associated with obesity. In agreement with other groups, we found similar international normalized ratio control among BMI categories,25 but the effect of overweight and obesity on prognosis did not change after adjustment for these potential confounders. A nonlinear relationship between BMI and events was also tested (Figure 2) and we did not find significant changes in the event rates through all the spectrum of BMI of our population, reinforcing the lack of association between weight and prognosis in this scenario.
Limitations
This study has some limitations. BMI was collected only at baseline, so we could not assess the associations between long‐term changes in BMI over time on outcomes. The measurement of obesity by means of BMI is a limited approach, because it does not assess the distribution of fat, the amount of lean body weight, body fat, fat‐free mass, or fat composition.32 While most studies assess obesity with BMI, results are similar in studies evaluating it by waist circumference.13, 20 The lack of more detailed information about the type of bleeding or the cause of cardiovascular death prevented further analyses. The Cockcroft‐Gault formula tends to overestimate creatinine clearance in obese patients. Although multivariate adjustment was performed, the effects of residual confounding cannot be fully excluded. A propensity‐score matched analysis would have reinforced the strength of the findings, but the limited sample size of our study prevented us from performing this analysis. On the other hand, the observational nature of our study provides real‐world data.
In conclusion, in this prospective cohort of real‐world patients anticoagulated for AF, obesity was highly prevalent but was not associated with poor prognosis. In contrast to clinical trial cohorts, the obesity paradox does not appear to be evident in real‐world studies.
Sources of Funding
The FANTASIIA registry was funded by an unconditional grant from Pfizer/Bristol‐Myers‐Squibb and by grants from the Instituto de Salud Carlos III (Madrid)‐FEDER (RD16/11/00420, RD12/0042/0068, RD12/0042/0010, RD12/0042/0069, and RD12/0042/0063). The authors are supported by RD12/0042/0049 (RETICS) from ISCIII and PI13/00513/FEDER from ISCIII. Fundación Séneca (19245/PI/14), Instituto Murciano de Investigación Biosanitaria (IMIB16/AP/01/06).
Disclosures
None.
Supporting information
Appendix S1. FANTASIIA Registry Investigators.
Table S1. Quality of Anti‐Vitamin K Control Stratified by BMI
Table S2. Univariate Cox Regression
Table S3. Event Rates for Subgroups, Stratified by BMI
(J Am Heart Assoc. 2020;9:e013789 DOI: 10.1161/JAHA.119.013789.)
References
- 1. Börschel CS, Schnabel RB. The imminent epidemic of atrial fibrillation and its concomitant diseases—Myocardial infarction and heart failure—a cause for concern. Int J Cardiol. 2019;287:162–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ricci G, Tomassoni D, Pirillo I, Sirignano A, Sciotti M, Zaami S, Grappasonni I. Obesity in the European region: social aspects, epidemiology and preventive strategies. Eur Rev Med Pharmacol Sci. 2018;22:6930–6939. [DOI] [PubMed] [Google Scholar]
- 3. Ruddox V, Sandven I, Munkhaugen J, Skattebu J, Edvardsen T, Erik Otterstad J. Atrial fibrillation and the risk for myocardial infarction, all‐cause mortality and heart failure: a systematic review and meta‐analysis. Eur J Prev Cardiol. 2017;24:1555–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Han SJ, Boyko EJ. The evidence for an obesity paradox in type 2 diabetes mellitus. Diabetes Metab J. 2018;42:179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mohebi R, Simforoosh A, Tohidi M, Azizi F, Hadaegh F. Obesity paradox and risk of mortality events in chronic kidney disease patients: a decade of follow‐up in Tehran lipid and glucose study. J Ren Nutr. 2015;25:345–350. [DOI] [PubMed] [Google Scholar]
- 6. Andersen KK, Olsen TS. The obesity paradox in stroke: lower mortality and lower risk of readmission for recurrent stroke in obese stroke patients. Int J Stroke. 2015;10:99–104. [DOI] [PubMed] [Google Scholar]
- 7. Wang ZJ, Zhou YJ, Galper BZ, Gao F, Yeh RW, Mauri L. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: a systematic review and meta‐analysis. Heart. 2015;101:1631–1638. [DOI] [PubMed] [Google Scholar]
- 8. Fitzpatrick AL, Kuller LH, Lopez OL, Diehr P, O'Meara ES, Longstreth WT, Luchsinger JA. Midlife and late‐life obesity and the risk of dementia: cardiovascular health study. Arch Neurol. 2009;66:336–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang TJ, Parise H, Levy D, D'Agostino RB, Wolf PA, Vasan RS, Benjamin EJ. Obesity and the risk of new‐onset atrial fibrillation. JAMA. 2004;292:2471. [DOI] [PubMed] [Google Scholar]
- 10. Tsang TSM, Barnes ME, Miyasaka Y, Cha SS, Bailey KR, Verzosa GC, Seward JB, Gersh BJ. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: a longitudinal cohort study of 21 years. Eur Heart J. 2008;29:2227–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, Milani RV. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61:142–150. [DOI] [PubMed] [Google Scholar]
- 12. Badheka AO, Rathod A, Kizilbash MA, Garg N, Mohamad T, Afonso L, Jacob S. Influence of obesity on outcomes in atrial fibrillation: yet another obesity paradox. Am J Med. 2010;123:646–651. [DOI] [PubMed] [Google Scholar]
- 13. Sandhu RK, Ezekowitz J, Andersson U, Alexander JH, Granger CB, Halvorsen S, Hanna M, Hijazi Z, Jansky P, Lopes RD, Wallentin L. The ‘obesity paradox’ in atrial fibrillation: observations from the ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial. Eur Heart J. 2016;37:2869–2878. [DOI] [PubMed] [Google Scholar]
- 14. Mitchell AB, Cole JW, McArdle PF, Cheng Y‐C, Ryan KA, Sparks MJ, Mitchell BD, Kittner SJ. Obesity increases risk of ischemic stroke in young adults. Stroke. 2015;46:1690–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bertomeu‐González V, Anguita M, Moreno‐Arribas J, Cequier Á, Muñiz J, Castillo‐Castillo J, Sanchis J, Roldán I, Marin F, Bertomeu‐Martínez V; FANTASIIA Study Investigators . Quality of anticoagulation with vitamin K antagonists. Clin Cardiol. 2015;38:357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–2870. [DOI] [PubMed] [Google Scholar]
- 17. Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. [DOI] [PubMed] [Google Scholar]
- 18. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJGM, Lip GYH. A novel user‐friendly score (HAS‐BLED) to assess 1‐year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. [DOI] [PubMed] [Google Scholar]
- 19. Schulman S, Anger SU, Bergqvist D, Eriksson B, Lassen MR, Fisher W. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010;9:202–204. [DOI] [PubMed] [Google Scholar]
- 20. Roopinder D, Sandhu K, Sandhu RK, Ezekowitz JA, Hijazi Z, Westerbergh J, Aulin J, Alexander JH, Granger CB, Halvorsen S, Hanna MS, Lopes RD, Siegbahn A, Wallentin L. Obesity paradox on outcome in atrial fibrillation maintained even considering the prognostic influence of biomarkers: insights from the ARISTOTLE trial. Open Heart. 2018;5:e000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhu W, Wan R, Liu F, Hu J, Huang L, Li J, Hong K. Relation of body mass index with adverse outcomes among patients with atrial fibrillation: a meta‐analysis and systematic review. J Am Heart Assoc. 2016;5:004006 DOI: 10.1161/JAHA.116.004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Boriani G, Laroche C, Diemberger I, Fantecchi E, Meeder J, Kurpesa M, Baluta MM, Proietti M, Tavazzi L, Maggioni AP; Lip GYH, EORP‐AF General Pilot Registry Investigators . Overweight and obesity in patients with atrial fibrillation: Sex differences in 1‐year outcomes in the EORP‐AF General Pilot Registry. J Cardiovasc Electrophysiol. 2018;29:566–572. [DOI] [PubMed] [Google Scholar]
- 23. Proietti M, Guiducci E, Cheli P, Lip GYH. Is there an obesity paradox for outcomes in atrial fibrillation? Stroke. 2017;48:857–866. [DOI] [PubMed] [Google Scholar]
- 24. Guo Y, Yue X, Li H, Song Z, Yan H, Zhang P, Gui Y, Chang L, Li T. Overweight and obesity in young adulthood and the risk of stroke: a meta‐analysis. J Stroke Cerebrovasc Dis. 2016;25:2995–3004. [DOI] [PubMed] [Google Scholar]
- 25. Inoue H, Kodani E, Atarashi H, Okumura K, Yamashita T, Origasa H; J‐RHYTHM Registry Investigators . Impact of body mass index on the prognosis of Japanese patients with non‐valvular atrial fibrillation. Am J Cardiol. 2016;118:215–221. [DOI] [PubMed] [Google Scholar]
- 26. Overvad TF, Rasmussen LH, Skjøth F, Overvad K, Lip GYH, Larsen TB. Body mass index and adverse events in patients with incident atrial fibrillation. Am J Med. 2013;126:640.e9–640.e17. [DOI] [PubMed] [Google Scholar]
- 27. Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61:151–156. [DOI] [PubMed] [Google Scholar]
- 28. Eikelboom JW, Wallentin L, Connolly SJ, Ezekowitz M, Healey JS, Oldgren J, Yang S, Alings M, Kaatz S, Hohnloser SH, Diener H‐C, Franzosi MG, Huber K, Reilly P, Varrone J, Yusuf S. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation. Circulation. 2011;123:2363–2372. [DOI] [PubMed] [Google Scholar]
- 29. Rivera‐Caravaca JM, Roldán V, Esteve‐Pastor MA, Valdés M, Vicente V, Lip GYH, Marín F. Importance of time in therapeutic range on bleeding risk prediction using clinical risk scores in patients with atrial fibrillation. Sci Rep. 2017;7:12066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang J, Yang YM, Zhu J, Zhang H, Shao XH, Tian L, Huang B, Yu LT, Gao X, Wang M. Overweight is associated with improved survival and outcomes in patients with atrial fibrillation. Clin Res Cardiol. 2014;103:533–542. [DOI] [PubMed] [Google Scholar]
- 31. Simoons ML, Bonneux L. Obesity, cardiology, and beyond. J Am Coll Cardiol. 2008;52:986–987. [DOI] [PubMed] [Google Scholar]
- 32. Alagiakrishnan K, Banach M, Ahmed A, Aronow WS. Complex relationship of obesity and obesity paradox in heart failure—higher risk of developing heart failure and better outcomes in established heart failure. Ann Med. 2016;48:603–613. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. FANTASIIA Registry Investigators.
Table S1. Quality of Anti‐Vitamin K Control Stratified by BMI
Table S2. Univariate Cox Regression
Table S3. Event Rates for Subgroups, Stratified by BMI


