Abstract
Background
Cardiovascular disease remains a leading cause of death among women. Despite improvements in the management of patients with acute coronary syndrome (ACS), women with an ACS remain at higher risk.
Methods and Results
We performed a time‐dependent analysis of the management and outcomes of women admitted with ACS who enrolled in the prospective biennial ACS Israeli Surveys between 2000 and 2016. Surveys were divided into 3 time periods (2000‐2004, 2006‐2010, and 2013‐2016). Outcomes included 30‐day major adverse cardiac events (death, myocardial infarction, stroke, unstable angina, stent thrombosis, urgent revascularization) and 1‐year mortality. Overall, 3518 women were admitted with an ACS. Their mean age (70±12 years) was similar among the time periods. Over the time course of the study, more women were admitted with non–ST‐elevation ACS (51.9%, 59.6%, and 66.1%, respectively; P<0.001), and statins and percutaneous coronary intervention were increasingly utilized (66%, 91%, 93%, and 42%, 60%, and 68%, respectively; P<0.001 for each). Among women with ST‐segment–elevation myocardial infarction, more primary percutaneous coronary interventions were performed (48.5%, 84.7%, and 95.3%, respectively; P<0.001). The rate of 30‐day major adverse cardiac events has significantly decreased over the years (24.6%, 18.6%, and 13.5%, respectively; P<0.001). However, 1‐year mortality rates declined only from 2000 to 2004 (16.9%, 12.8%, and 12.3%; P=0.007 for the overall difference), and this change was not significant after propensity matching or multivariate analysis.
Conclusions
Over more than a decade, 30‐day major adverse cardiac events have decreased among women with ACS. Advances in pharmacological treatments and an early invasive approach may have accounted for this improvement. However, the lack of further reduction in 1‐year mortality rates among women suggests that more measures should be provided in this high‐risk population.
Keywords: acute coronary syndrome, sex, temporal trends
Subject Categories: Mortality/Survival, Quality and Outcomes, Acute Coronary Syndromes
Clinical Perspective
What Is New?
Utilization of guideline‐recommended therapies, both pharmacological and invasive, in women with acute coronary syndrome has significantly improved during the years.
The short‐term clinical outcome of women with acute coronary syndrome has significantly improved over the years, both in ST‐segment–elevation myocardial infarction and non–ST‐elevation acute coronary syndrome and in younger and older women.
However, 1‐year mortality rates of women admitted with an acute coronary syndrome have overall remained unchanged during the past 2 decades.
What Are the Clinical Implications?
The lack of reduction in mortality rates among women over time suggests that more measures should be provided in this high‐risk population.
Introduction
The prognosis of women with ischemic heart disease has dramatically improved over the past 4 decades. Yet, sex‐based differences in outcomes still exist, and women presenting with acute coronary syndrome (ACS) exhibit higher in‐hospital and 1‐year mortality compared with men.1, 2, 3
Increased awareness, improvement in diagnosis, implementation of evidence‐based drug therapies, and percutaneous coronary intervention (PCI) in patients with ST‐segment–elevation myocardial infarction (STEMI) and non–ST‐elevation ACS (NSTE‐ACS), have resulted in a reduction in short‐ and long‐term morbidity and mortality.4, 5, 6 Similar trends have been reported also in women, yet reports are conflicting.7, 8, 9, 10, 11, 12 Young women with ACS, for example, are a particularly high‐risk group with worse outcomes compared with young men.8, 9, 10 In addition, it is not clear whether the prognosis of women admitted with STEMI and NSTE‐ACS have improved in a similar extent.
We aimed to examine temporal trends in major adverse cardiovascular events (MACE) and mortality among women admitted with an ACS (STEMI and NSTE‐ACS). We hypothesized that, during the years, the utilization of evidence‐based therapies in women has increased, and this would translate into a reduction in recurrent cardiovascular ischemic events and mortality.
Methods
Data Sharing
The data that support the findings of this study are available from the corresponding author on reasonable request.
Study Population
ACSIS (the ACS Israeli Survey) is a biennial prospective national registry of all patients with ACS hospitalized in 25 coronary care units and cardiology departments in all general hospitals in Israel over a 2‐month period (March and April).7, 10 It is governed and coordinated by the Working Group on Acute Cardiovascular Care, part of the Israel Heart Society, in participation with the Israeli Association for Cardiovascular Trials. Demographic, historic, and clinical data were recorded on prespecified forms for all patients. Patient management was at the discretion of the attending physicians. Admission and discharge diagnoses were recorded as determined by the attending physicians based on clinical, electrocardiographic, and biochemical criteria. Definitions of type of myocardial infarction (ST‐elevation versus non–ST‐elevation) and unstable angina were homogeneous and based on prespecified criteria according to accepted definitions in the specific survey period. All patients signed an informed consent for participating in the ACSIS registry in each medical center, and each institution received the approval of its institutional review board.7, 10
The current study population comprises all women with ACS (either STEMI, non–ST‐segment–elevation myocardial infarction, or unstable angina) enrolled in the ACSIS registry between 2000 and 2016 (8 consecutive registries). Comparisons were made using data from all 8 surveys separately (2000, 2002, 2004, 2006, 2008, 2010, 2013, 2016) and by trichotomizing the survey period into 3 prespecified time intervals defined as early (2000‐2004), middle (2006‐2010), and late (2013‐2016) time periods. The reason for this categorization was mainly the management of ACS at each time interval: in the early period, primary PCI was introduced and was increasingly utilized; in the middle period the use of potent P2Y12 inhibitors was introduced; and in the late period more contemporary guideline‐recommended therapies were utilized including the radial approach in coronary angiography, early invasive strategy, and the common use of high‐potency statins.
Clinical Outcomes
Clinical outcomes included 30‐day MACE, which included death, MI, stroke, unstable angina, stent thrombosis, and urgent revascularization. One‐year mortality was examined as well. Data on 30‐day MACE were ascertained by hospital chart review, telephone contact, and clinical follow‐up data. Mortality data at 30 days were determined for all patients from hospital charts and by matching identification numbers of patients with the Israeli National Population Registry. One‐year mortality data were ascertained through the use of the Israeli National Population Registry.
Statistical Analyses
The groups were compared with χ2 for categorical/nominal variables and with t test for continuous variables. ANOVA or Kruskal‐Wallis tests were used for nonnormally distributed variables. Temporal trends in characteristics and treatment were compared using the χ2 test for trend. Survival analysis between the groups was performed using the Kaplan‐Meier method and compared using the Log Rank test. In order to examine the effect of study groups on survival, we performed multivariable analysis (Cox proportional hazard) adjusted for covariates based on univariate analysis of baseline characteristics. To examine the effect of study groups on other outcomes, multivariable analysis was performed, adjusted for covariates based on univariate analysis of baseline characteristics. To reduce bias among the time periods, a propensity score matching was performed. A 1‐to‐1 matching was conducted, based on statistical significant differences among the groups, with a caliper of 0.07. All analyses were performed by the Israeli Association for Cardiovascular Trials using R software (R Development Core Team, R version 3.6.1 [2019‐07‐05], Vienna, Austria). A 2‐sided P<0.05 was used for declaring statistical significance.
Results
Baseline Characteristics
A total of 15 211 patients with ACS were enrolled in the 8 surveys (ACSIS 2000 through 2016), of whom 3518 (23%) were women who were included in the study. During those years there was a decrease in the relative percentage of women among all patients with ACS (from 25% in 2000 to 21% in 2016, P<0.001).
The mean age (70±12 years) has not changed among the 3 time periods. Baseline characteristics and outcomes are depicted in Table 1. Cardiovascular risk factors including dyslipidemia, hypertension, current smoking, family history of coronary artery disease, obesity, and chronic renal failure were more common among women enrolled in the late time periods as compared with the early time period (P<0.001 for each). In addition, women in the late time periods had undergone more PCI than those in the early time period (23.3% versus 16.1%, P<0.001). Prior use of β‐blockers and statins was also more common in the middle and late time periods.
Table 1.
Baseline Characteristics of Women Admitted With ACS
| Years | P Value | |||
|---|---|---|---|---|
| 2000‐2004 (n=1480) | 2006‐2010 (n=1229) | 2013‐2016 (n=809) | ||
| Characteristics | ||||
| Mean age, y (SD) | 70.3 (11.9) | 70.3 (12.5) | 70.2 (12.3) | 0.97 |
| Dyslipidemia | 819 (55.6) | 924 (75.4) | 618 (76.9) | <0.001 |
| Hypertension | 1018 (69.0) | 938 (76.3) | 612 (75.9) | <0.001 |
| Current smokers | 240 (16.4) | 227 (18.8) | 174 (21.5) | 0.01 |
| Diabetes mellitus | 621 (42.2) | 538 (43.9) | 357 (44.3) | 0.50 |
| Family history of CAD | 206 (14.1) | 244 (21.6) | 168 (25.6) | <0.001 |
| BMI (kg/m2) (mean, SD) | 27.6 (4.9) | 28.2 (5.5) | 29.2 (14.9) | 0.002 |
| Prior MI | 367 (24.9) | 324 (26.4) | 203 (25.2) | 0.60 |
| Prior CABG | 117 (8.0) | 91 (7.4) | 55 (6.8) | 0.60 |
| Prior PCI | 237 (16.1) | 298 (24.3) | 188 (23.3) | <0.001 |
| Chronic renal failure | 127 (8.7) | 172 (14.1) | 105 (13.0) | <0.001 |
| PVD | 8 (0.27) | 8 (0.27) | 6 (0.24) | 0.24 |
| Prior CVA/TIA | 155 (10.6) | 130 (10.6) | 81 (10.0) | 0.90 |
| History of CHF | 158 (10.7) | 126 (10.3) | 75 (9.3) | 0.50 |
| Prior medications | ||||
| Aspirin | 467 (45.6) | 656 (53.9) | 375 (48.3) | <0.001 |
| Clopidogrel | 36 (3.5) | 115 (9.4) | 97 (12.4) | <0.001 |
| Statins | 371 (36.2) | 694 (56.9) | 432 (60.9) | <0.001 |
| β‐Blockers | 410 (39.9) | 574 (47.0) | 336 (44.6) | 0.003 |
| ACE‐I | 177 (33.1) | 318 (42.2) | 233 (30.9) | <0.001 |
| ARB | 57 (10.7) | 95 (12.6) | 161 (21.6) | <0.001 |
| Hypoglycemic agents | 228 (27.2) | 344 (28.1) | 221 (27.6) | 0.90 |
Data are n (%) unless otherwise specified. ACE‐I indicates angiotensin‐converting enzyme inhibitors; ACS, acute coronary syndrome; ARB, angiotensin receptor blockers; BMI, body mass index; CABG, coronary artery bypass graft; CAD, coronary artery disease; CHF, congestive heart failure; CVA, cerebrovascular accident; MI, myocardial infarction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; TIA, transient ischemic attack.
Clinical Presentation and Management
Over the years, more women were admitted with NSTE‐ACS (51.9%, 59.6%, and 66.1%, respectively; P<0.001; Figure 1). Time from symptom onset to ECG has significantly decreased over the years, although it was still long in the late period (median 139 [67, 301] minutes) (Table 2). In addition, in STEMI patients, door‐to‐balloon time has significantly decreased to a median of 60 (30, 110) minutes (Table 2). The proportion of women with a Global Registry of Acute Coronary Events score >140 significantly decreased from the early to the late time periods (34.8%, 32.7%, and 27.9%, respectively; P=0.013), as did the Killip class at presentation (Table 2).
Figure 1.

Type of acute coronary syndrome in women by survey year. ACSIS indicates Acute Coronary Syndrome Israeli Survey; NSTEMI, non–ST‐segment–elevation myocardial infarction; STEMI, ST‐segment–elevation myocardial infarction; UAP, unstable angina pectoris.
Table 2.
Clinical Presentation and Hospital Management
| Years | P Value | |||
|---|---|---|---|---|
| 2000‐2004 (n=1480) | 2006‐2010 (n=1229) | 2013‐2016 (n=809) | ||
| STEMI | 711 (48.1) | 496 (40.4) | 274 (33.9) | <0.010 |
| Admission Killip class | <0.001 | |||
| I | 1061 (71.9) | 956 (77.8) | 648 (84.4) | |
| II | 226 (15.3) | 153 (12.4) | 749 (9.6) | |
| III | 157 (10.6) | 94 (7.6) | 329 (4.2) | |
| IV | 31 (2.1) | 269 (2.1) | 14 (1.8) | |
| GRACE score >140 | 213 (34.8) | 280 (32.7) | 174 (27.4) | 0.01 |
| Sinus rhythm | 908 (87.9) | 1058 (86.1) | 670 (82.8) | 0.008 |
| AF/SVT | 55 (5.3) | 52 (6.8) | 73 (9.0) | 0.008 |
| Laboratory tests | ||||
| Peak troponin I | 305 (72.8) | 488 (74.8) | 340 (72.8) | 0.60 |
| Peak troponin T | 177 (66.8) | 359 (74.6) | 348 (75.2) | 0.03 |
| Total cholesterol (mg/dL), [median, IQR] | 194.00 [168.00, 226.00] | 177.00 [152.00, 206.75] | 178.00 [149.00, 214.00] | <0.001 |
| LDL cholesterol (mg/dL) [median, IQR] | 116.00 [91.00, 141.00] | 101.00 [77.00, 128.00] | 102.00 [77.00, 134.00] | <0.001 |
| Triglycerides (mg/dL) [median, IQR] | 139.00 [103.50, 189.00] | 130.00 [94.00, 184.00] | 127.50 [88.12, 181.75] | 0.003 |
| Coronary angiography | 376 (69.0) | 982 (79.9) | 721 (89.1) | <0.001 |
| PCI | 623 (42.0) | 732 (59.5) | 551 (68.2) | <0.001 |
| Primary PCI (in STEMI) | 188 (48.5) | 244 (84.7) | 201 (95.3) | <0.001 |
| Radial vascular access | NA | 24 (25.3) | 128 (62.1) | NA |
| TIMI grade flow following procedure, mean (SD) | NA | 2.82 (0.64) | 2.71 (0.81) | NA |
| Time from symptoms onset to ECG, min [median, IQR] | 165 [98, 291] | 150 [80, 303] | 139 [67, 301] | 0.027 |
| Door to balloon time (STEMI), min [median, IQR] | 80 [42, 144] | 77 [40, 128] | 60 [30, 110] | 0.021 |
| Discharge medication | ||||
| Aspirin | 1267 (88.4) | 1124 (94.1) | 721 (90.8) | <0.001 |
| P2Y12 | 596 (42.5) | 869 (73.0) | 664 (83.6) | <0.001 |
| Statins | 928 (65.7) | 1082 (90.5) | 715 (92.6) | <0.001 |
| ACE‐I/ARB | 964 (65.1) | 900 (74.4) | 600 (74.2) | <0.001 |
| β‐Blockers | 1059 (74.4) | 962 (80.5) | 592 (77.1) | 0.001 |
| Cardiac rehabilitation (referral) | NA | 396 (35.0) | 276 (45.5) | NA |
Data are n (%) unless otherwise specified. ACE‐I indicates angiotensin‐converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin receptor blocker; GRACE, Global Registry of Acute Coronary Events; IQR, interquartile range; LDL, low‐density lipoprotein; NA, not applicable; PCI, percutaneous coronary intervention; STEMI, ST‐segment–elevation myocardial infarction; SVT, supraventricular tachycardia; TIMI, thrombolysis in myocardial infarction.
During the years studied, more women had undergone coronary angiography and PCI (42%, 60%, and 68%, P<0.001; Table 2). Specifically, 95.3% of women admitted with STEMI in the late time period had undergone primary PCI (Table 2). Radial access was increasingly utilized. Evidence‐based medications at discharge, such as aspirin, P2Y12 inhibitors, statins, and β‐blockers, had also been increasingly utilized during the study years (Table 2). In the late time period nearly 50% of the women with an ACS were referred to cardiac rehabilitation at discharge.
Clinical Outcomes
The rate of 30‐day MACE has significantly decreased over the years (24.6%, 18.6%, and 13.5% in the early, middle, and late time periods, respectively; P<0.001; Table 3). The absolute rate of 1‐year mortality has significantly decreased since the early period but has remained unchanged during the past decade (16.9%, 12.8%, and 12.3% in the early, middle, and late time periods, respectively, P=0.002; Table 3, Figure 2). After propensity matching (Tables S1 and S2), 1‐year mortality did not change significantly during the study period (Figure 3). These results were also consistent on multivariate analysis (Figure 4).
Table 3.
In‐Hospital Complications, 30‐Day MACE, 30‐Day and 1‐Year Mortality Rates
| Years | P Value | |||
|---|---|---|---|---|
| 2000‐2004 (n=1480) | 2006‐2010 (n=1229) | 2013‐2016 (n=809) | ||
| In‐hospital complications | ||||
| CHF mild‐moderate (Killip‐2) | 207 (14.1) | 166 (13.6) | 60 (7.4) | <0.001 |
| Pulmonary edema (Killip‐3) | 206 (14.0) | 132 (10.8) | 40 (5.0) | <0.001 |
| Cardiogenic shock (Killip‐4) | 89 (6.0) | 57 (4.7) | 32 (4.0) | 0.07 |
| Post‐MI angina/reischemia | 149 (10.2) | 64 (5.2) | 10 (1.2) | <0.001 |
| Acute renal failure | 157 (10.7) | 82 (6.7) | 45 (5.6) | <0.001 |
| All patients | ||||
| 30‐d mortality | 141 (9.5) | 85 (6.9) | 53 (6.6) | 0.01 |
| 30‐d MACEa | 364 (24.6) | 229 (18.6) | 109 (13.5) | <0.001 |
| 1‐y mortality | 249 (16.9) | 156 (12.8) | 98 (12.3) | 0.002 |
| STEMI | ||||
| 30‐d mortality | 104 (14.6) | 48 (9.7) | 30 (11.0) | 0.029 |
| 30‐d MACEa | 207 (29.1) | 105 (21.2) | 44 (16.1) | <0.001 |
| 1‐y mortality | 143 (20.2) | 74 (15.0) | 43 (16.1) | 0.053 |
| NSTE‐ACS | ||||
| 30‐d mortality | 37 (4.8) | 37 (5.1) | 23 (4.3) | 0.836 |
| 30‐d MACEa | 157 (20.5) | 124 (16.9) | 65 (12.1) | <0.001 |
| 1‐y mortality | 105 (13.7) | 82 (11.2) | 55 (10.4) | 0.146 |
Data are n (%) unless otherwise specified. ACS indicates acute coronary syndrome; CHF, congestive heart failure; MACE, major adverse cardiovascular events; MI, myocardial infarction; NSTE, non–ST‐segment–elevation; STEMI, ST‐segment–elevation myocardial infarction.
Thirty‐day MACE include 30‐day mortality, unstable angina, myocardial infarction, cerebrovascular event, stent thrombosis, and urgent revascularization.
Figure 2.
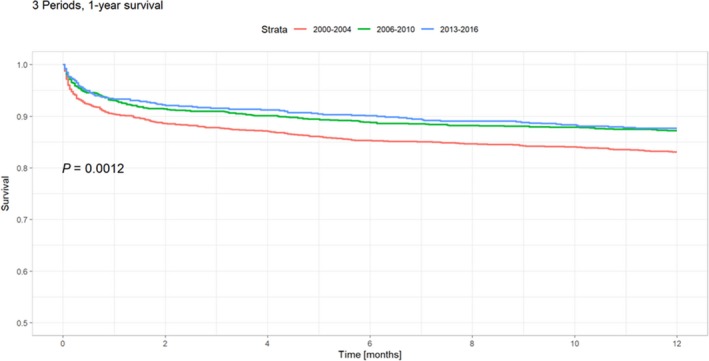
Kaplan‐Meier curves for 1‐year mortality according to the early (2000‐2004), middle (2006‐2010), and late (2013‐2016) time periods.
Figure 3.

Kaplan‐Meier curve for 1‐year mortality after propensity matching: (A) early vs middle time period; (B) early vs late time period.
Figure 4.
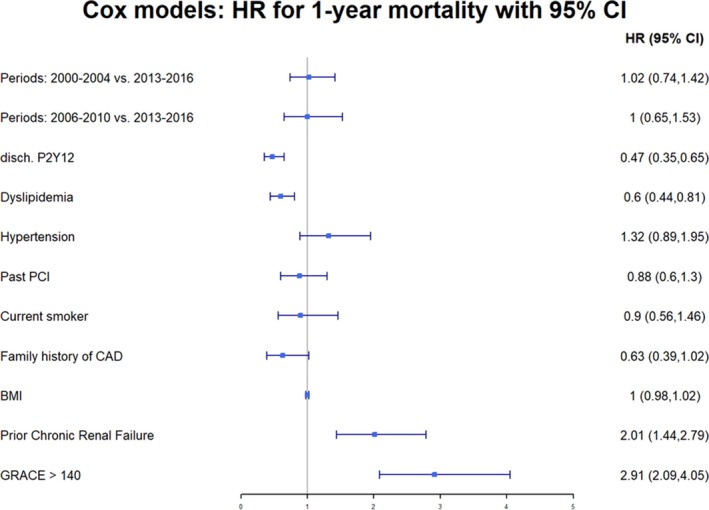
Multivariable analysis for 1‐year mortality. GRACE indicates Global Registry of Acute Coronary Events; HR, hazard ratio; PCI, percutaneous coronary intervention.
During the study years, the rates of 30‐day MACE decreased both in women with STEMI and in those with NSTE‐ACS (Table 3). Interestingly, the rates of 30‐day and 1‐year mortality numerically decreased in women with STEMI but remained unchanged in women with NSTE‐ACS (Table 3). In‐hospital complications such as heart failure, post‐ACS angina/ischemia, and renal failure have also significantly decreased over the years (Table 3).
When the women were stratified by age (<55, ≥55 years), 30‐day MACE decreased during the years in both age groups, yet the mortality rates numerically decreased especially among women aged ≥55 years, whereas the mortality rates of younger women remained unchanged (Table 4).
Table 4.
Thirty‐Day MACE, 30‐Day and 1‐Year Mortality Rates in Women Aged <55 and ≥55 Years
| Age <55 years | Age ≥55 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Time Period | Time Period | |||||||
| 2000‐2004 (n=86) | 2006‐2010 (n=69) | 2013‐2016 (n=36) | P Value | 2000‐2004 (n=625) | 2006‐2010 (n=427) | 2013‐2016 (n=238) | P Value | |
| STEMI | ||||||||
| MACE | 12 (14.0) | 8 (11.6) | 1 (2.8) | 0.194 | 195 (31.2) | 97 (22.7) | 43 (18.1) | <0.001 |
| 30‐d mortality | 1 (1.2) | 3 (4.3) | 0 (0.0) | 0.249 | 103 (16.5) | 45 (10.6) | 30 (12.7) | 0.021 |
| 1‐y mortality | 6 (7.1) | 3 (4.4) | 2 (5.7) | 0.789 | 137 (22.0) | 71 (16.7) | 41 (17.7) | 0.082 |
| Time Period | Time Period | |||||||
|---|---|---|---|---|---|---|---|---|
| 2000‐2004 (n=79) | 2006‐2010 (n=75) | 2013‐2016 (n=57) | P Value | 2000‐2004 (n=688) | 2006‐2010 (n=658) | 2013‐2016 (n=478) | P Value | |
| Non–ST‐elevation ACS | ||||||||
| MACE | 20 (25.3) | 10 (13.3) | 6 (10.5) | 0.044 | 137 (19.9) | 114 (17.3) | 59 (12.3) | 0.003 |
| 30‐d mortality | 2 (2.5) | 1 (1.4) | 3 (5.3) | 0.402 | 35 (5.1) | 36 (5.5) | 20 (4.2) | 0.629 |
| 1‐y mortality | 3 (3.8) | 3 (4.1) | 3 (5.3) | 0.912 | 102 (14.9) | 79 (12.0) | 52 (11.0) | 0.117 |
Data are n (%) unless otherwise specified. ACS indicates acute coronary syndrome; MACE, major adverse cardiovascular events; STEMI, ST‐segment–elevation myocardial infarction.
Discussion
This study, from a prospective biennial national registry in women with ACS, has several findings. Several characteristics of women admitted with ACS have become more common (eg, dyslipidemia, hypertension) during the years of the study, while some have remained unchanged (eg, age). NSTE‐ACS has become increasingly common among women and represents about two thirds of all ACS in women. Utilization of guideline‐recommended therapies, both pharmacological and invasive, in women with ACS has significantly improved during the years. Finally, the short‐term clinical outcome of women with ACS has significantly improved over the years, both in STEMI and NSTE‐ACS and in younger and older women. However, 1‐year mortality rates of women admitted with an ACS have overall remained unchanged during the past 2 decades.
Our data demonstrate a steady decline over the years in the relative representation of women admitted with an ACS, out of all ACS events. This finding is in contrast with previous reports that show an increase in the number of women admitted with an ACS.4, 13 This difference may be explained in part by the population of the ACSIS registry, which included only patients with ACS hospitalized in coronary care units and cardiology departments.
Better adherence to contemporary evidence‐based therapies, including higher rates of revascularization and secondary prevention drug therapies, have been previously related to improved outcomes in ACS in both sexes 14, 15, 16 and might explain the improvement in short‐term outcomes observed in our study during the years. Despite more utilization of guideline‐based therapies during time, 1‐year mortality rates of women admitted with an ACS have remained almost unchanged. Although this finding is likely to be multifactorial, several possible reasons may be suggested. First, our data show that mortality rates have slightly decreased in STEMI but have remained unchanged in NSTE‐ACS, which represents the leading type of ACS in women. Second, although the age of women with an ACS over the years has not changed, lack of improvement in mortality after ACS in young women even in the modern era may have contributed to the overall results. In this context, several studies have shown higher rates of in‐hospital mortality among young woman with ACS.15, 16, 17, 18 Third, the clinical profile of women admitted with ACS has changed during the years. Compared with the earlier period, women in the past decade have a higher burden of risk factors and comorbidities, including hypertension, dyslipidemia, renal failure, obesity, and smoking. The deleterious effect of the last factor has been consistently shown across a wide range of medical conditions and is considered a major risk factor for the development of ischemic heart disease and MI.19, 20 Studies have demonstrated that smoking is particularly harmful among women with a dose‐dependent effect.21 Indeed, the multivariate analysis that accounted for differences in baseline characteristics among the time periods, demonstrated that the latest period was not associated with a reduction in 1‐year mortality. Fourth, the overall unchanged mortality rates in the past decade may reflect the change in the pathophysiology of ACS in women during those years. More women were admitted with NSTE‐ACS in the last decades. About a third of these women have nonobstructive coronary artery disease,22, 23, 24 which may include microvascular disease, endothelial dysfunction, and vasospastic angina. Although the prognosis after ACS in the setting of nonobstructive epicardial coronary artery disease is better than that of obstructive disease, it is not benign.24 Importantly, the impact of evidence‐based therapies of ACS in this population is less robust, explaining in part the lack of improvement in mortality in the past decade despite better use of modern treatments.
In the United States as well as in Israel, longevity has improved during the years.25, 26 According to data from the Israel Central Bureau of Statistics, in the last decade (2006‐2016), longevity of women has increased by 1.7 years.26 In addition, in the past 30 years, longevity has improved by 7.4 years among women. Thus, in the last decade, there is only a modest increase in longevity, and this rate is smaller than those of prior decades. Interestingly, the rates of cardiovascular mortality have decreased during the years (from 550 cases per 100 000 in 1980 to 95 cases per 100 000 in 2014). Nevertheless, since 2010, the decline in cardiovascular mortality has plateaued and remained nearly unchanged. Similar data have been reported by the American Heart Association in the 2019 heart disease and stroke statistics in which cardiovascular mortality has declined in the past 3 decades but remained unchanged in the last decade.25 These data are consistent with data from the ACSIS registry presented herein in women with ACS, for whom, although there was a decline in mortality during the years studied, only a small change, if any, was observed in the last decade. Thus, the improvement in longevity during the years studied is presumably multifactorial. Possible explanations include advanced screening modalities, early diagnosis of disease, and an improvement in the management of chronic diseases such as ischemic heart disease, diabetes mellitus, cancer, and heart failure.
Our study has several limitations. Results are derived from the ACSIS registry, which comprises a population admitted to cardiology wards and intensive cardiac care units nationwide with the diagnosis of ACS. Patients with less typical symptoms, which are more common among women, although ultimately diagnosed as ACS, may have been managed in the internal medicine wards and therefore are not represented in the current study. This may partially explain the decrease in the relative percentage of women among all patients with ACS. In addition, the ACSIS registry has limited follow‐up data beyond the index hospitalization with respect to long‐term medical treatment, adherence to treatment, and additional interventions. Therefore, the long‐term outcomes may be significantly influenced by these and other postdischarge intervening factors. Due to a decrease in mortality rates during the years, a β‐2 error cannot be ruled out. Finally, data regarding cardiac versus noncardiac causes of death are not available in the ACSIS registry.
Conclusions
During more than a decade, 30‐day MACE has significantly decreased among women admitted with an ACS. Advances in contemporary pharmacological treatments and an early invasive approach may have accounted for this improvement. However, the lack of reduction in mortality rates among women over time suggests that more measures should be provided for this high‐risk population.
Disclosures
None.
Supporting information
Table S1. Baseline Characteristics After Propensity Matching: Early (2000‐2004) Versus Middle (2006‐2010) Time Periods
Table S2. Baseline Characteristics After Propensity Matching: Early (2000‐2004) Versus Late (2013‐2016) Time Periods
(J Am Heart Assoc. 2020;9:e014721 DOI: 10.1161/JAHA.119.014721.)
References
- 1. Jneid H, Fonarow GC, Cannon CP, Hernandez AF, Palacios IF, Maree AO, Wells Q, Bozkurt B, Labresh KA, Liang L, Hong Y, Newby LK, Fletcher G, Peterson E, Wexler L; Get With the Guidelines Steering Committee and Investigators . Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;118:2803–2810. [DOI] [PubMed] [Google Scholar]
- 2. Shaw LJ, Shaw RE, Merz CN, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKay CR, Block PC, Hewitt K, Weintraub WS, Peterson ED. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in‐hospital mortality in the American College of Cardiology‐National Cardiovascular Data Registry. Circulation. 2008;117:1787–1801. [DOI] [PubMed] [Google Scholar]
- 3. Kunadian V, Qiu W, Lagerqvist B, Johnston N, Sinclair H, Tan Y, Ludman P, James S, Sarno G; National Institute for Cardiovascular Outcomes Research and Swedish Coronary Angiography and Angioplasty Registries . Gender differences in outcomes and predictors of all‐cause mortality after percutaneous coronary intervention (data from United Kingdom and Sweden). Am J Cardiol. 2017;119:210–216. [DOI] [PubMed] [Google Scholar]
- 4. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. [DOI] [PubMed] [Google Scholar]
- 5. Rogers WJ, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, Pollack CV Jr, Gore JM, Chandra‐Strobos N, Peterson ED, French WJ. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non‐ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1026–1034. [DOI] [PubMed] [Google Scholar]
- 6. McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sabbag A, Matetzky S, Gottlieb S, Fefer P, Kohanov O, Atar S, Zahger D, Porter A, Koifman B, Goldenberg I, Segev A. Recent temporal trends in the presentation, management, and outcome of women hospitalized with acute coronary syndromes. Am J Med. 2015;128:380–388. [DOI] [PubMed] [Google Scholar]
- 8. Bucholz EM, Strait KM, Dreyer RP, Lindau ST, D'Onofrio G, Geda M, Spatz ES, Beltrame JF, Lichtman JH, Lorenze NP, Bueno H, Krumholz HM. Editor's choice‐sex differences in young patients with acute myocardial infarction: a VIRGO study analysis. Eur Heart J Acute Cardiovasc Care. 2017;6:610–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gupta M, Singh N, Verma S. South Asians and cardiovascular risk: what clinicians should know. Circulation. 2006;113:e924–e929. [DOI] [PubMed] [Google Scholar]
- 10. Sabbag A, Matetzky S, Porter A, Iakobishvili Z, Moriel M, Zwas D, Fefer P, Asher E, Beigel R, Gottlieb S, Goldenberg I, Segev A. Sex differences in the management and 5‐year outcome of young patients (<55 years) with acute coronary syndromes. Am J Med. 2017;130:1324. [DOI] [PubMed] [Google Scholar]
- 11. Leifheit‐Limson EC, D'Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Canto JG, Rogers WJ, Goldberg RJ, Peterson ED, Wenger NK, Vaccarino V, Kiefe CI, Frederick PD, Sopko G, Zheng ZJ. Association of age and sex with myocardial infarction symptom presentation and in‐hospital mortality. JAMA. 2012;307:813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roger VI, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence severity and outcome of hospitalized myocardial infarction. Circulation. 2010;121:853–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex‐based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341:217–225. [DOI] [PubMed] [Google Scholar]
- 16. Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age‐specific gender differences in in‐hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109:1097–1103. [DOI] [PubMed] [Google Scholar]
- 17. Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med. 2009;169:1767–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sabbag A, Matetzky S, Porter A, Iakobishvili Z, Moriel M, Zwas D, Fefer P, Asher E, Beigel R, Gottlieb S, Goldenberg I, Segev A. Sex differences in the management and 5 year outcomes of young patients (<55 years) with acute coronary syndromes. Am J Med. 2017;130:1324.e15–1324.e22. [DOI] [PubMed] [Google Scholar]
- 19. Doll R, Peto R, Sutherland I. Mortality in relation to smoking; 50 years observation on male British doctors. BMJ. 2004;325:1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Njølstad I, Arnsen E, Lound‐Larsen PG. Smoking, serum lipids, blood pressure and sex differences in myocardial infarction. Circulation. 1996;93:450–456. [DOI] [PubMed] [Google Scholar]
- 21. Grundtvig M, Hagen TP, German M, Reikvam A. Sex‐based differences in premature first myocardial infarction caused by smoking: twice as many years lost by women as by men. Eur J Cardiovasc Prev Rehabil. 2009;16:174–179. [DOI] [PubMed] [Google Scholar]
- 22. Gehrie E, Raynolds HR, Chen AY, Neelon BH, Ohman EM, Newby LK, Peterson A, Hochman J. Characterization and outcomes of women and men with non–ST‐segment elevation myocardial infarction and nonobstructive coronary artery disease: results from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) Quality Improvement Initiative. Am Heart J. 2009;158:688–694. [DOI] [PubMed] [Google Scholar]
- 23. Ouellette ML, Loffler AI, Beller GA, Workman VK, Holland EA, Bourque JM. Clinical characteristics, sex differences, and outcomes in patients with normal or near‐normal coronary arteries, non‐obstructive or obstructive coronary artery disease. J Am Heart Assoc. 2018;7:e007965 DOI: 10.1161/JAHA.117.007965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pepine CJ, Ferdinand KC, Shaw LJ, Light‐McGroary KA, Shah RU, Gulati M, Duvenray C, Walsh MM, Bairey‐Merz N. Emergence of non obstructive coronary artery disease. J Am Coll Cardiol. 2015;66:1918–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 26. The Israeli Central Bureau of Statistics . Life expectancy in Israel, 2016. Available at: https://www.cbs.gov.il/he/mediarelease/DocLib/2017/362/05_17_362b.pdf. Accessed November 15, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline Characteristics After Propensity Matching: Early (2000‐2004) Versus Middle (2006‐2010) Time Periods
Table S2. Baseline Characteristics After Propensity Matching: Early (2000‐2004) Versus Late (2013‐2016) Time Periods


